Abstract
Background
Patient experience of care surveys are an important component of performance improvement and clinical effectiveness because they serve as a good proxy for patient’s satisfaction and the quality of care. The purpose of this study was to assess patients’ experience of care in four referral hospitals in two of South Africa’s rural provinces.
Methods
A cross-sectional study was conducted in four public hospitals in Eastern Cape (Nelson Mandela Academic (NMAH) and St. Elizabeth (SEH)) and Mpumalanga provinces (Rob Ferreira (RFH) and Themba) for two weeks in July 2022. Systematic random sampling was used to select 662 outpatients. A validated patient experience of care questionnaire measuring demographics, access to care, availability of medicines, cleanliness, staff attitudes and waiting times was used. The level of statistical significance was p-value ≤ 0.05.
Results
Females accounted for 71.6% (474/662) of participants; the median age was 47 years and 20.2% (133/657) required assistance with a disability. Only 19.0% (31/659) of patients had been turned away from hospital previously; one hospital was reported to not be clean (68.5%, 111/162); more than two-thirds of Mpumalanga province participants (223/329, 67.8%) reported absence of drinking water (p-value < 0.0001); 68.5% (111/162) of Themba participants did not think that the hospital was clean compared to NMAH’s 82.2% (134/163) who thought it was clean (p-value < 0.0001). At least 70% of participants in each of the hospitals found the health professionals to be respectful towards patients (p-value < 0.0001). In all hospitals, at least half of the participants did not know the processes to be followed when lodging a complaint (p-value = 0.002). None of the four hospitals met all the national targets. And only two out of 28 potential domains exceeded 80% or the cut-off score for satisfaction.
Conclusions
Whilst hospitals have been implementing various quality measures to improve patient’s experience of care, there are a few concerns such as non-availability of drinking water, lack of knowledge of complaints processes and waiting times that were mostly reported to be unacceptable. Efforts should be made to address the highlighted areas that affect patient experiences to continue improving patient care.
Trial registration
The study forms part of a clinical trial which was registered on 19 May 2022 in the South African National Clinical Trial Registry with ref: DOH-27-052022-6854. The URL of trial registry record is: https://sanctr.samrc.ac.za/.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-12002-y.
Keywords: Patient satisfaction, Patient experience of care, Referral hospital
Introduction
The global concern for healthcare quality necessitates a prompt response from the health sector to meet the growing needs and demands of patients [1, 2]. Ensuring high-quality healthcare involves consistently satisfying patients through the provision of effective, efficient, and successful healthcare services that adhere to current clinical norms and standards [3]. Patient satisfaction serves as a crucial measure of how well an individual’s needs and desires are met [4]. Various tools are available to address deficiencies in the delivery of quality care, including Root Cause Analysis [5], Continuous Quality Improvement Methods [6, 7], and Patient Experience of Care (PEC) [8]. The selection of appropriate tools depends on the specific context, goals, and resources available. For instance, PEC can create a platform for patients to share their experiences and utilise this feedback for appropriate interventions [8, 9].
PEC encompasses all the observable processes that patients encounter throughout their care journey and significantly influence their perception of the received care [10]. It involves parts of healthcare delivery that patients value highly when seeking and receiving care, including getting timely appointments, easy access to information, good communication with health providers, etc [11]. PEC has become a critical domain of quality that is used to evaluate hospital performance and assess the quality of care provided to patients [9, 12–14]. As advised by the South African National Department of Health (NDoH), information from PEC should be used by leaders to improve care [8]. PEC surveys complement evaluations of clinical performance by identifying key areas for improvement throughout the patient’s hospital journey [15, 16]. Patients’ experiences can be used to assess structures and processes of treatment [14].
In South Africa, it is mandatory for the government to deliver quality healthcare to all citizens through the publicly-funded health sector [17]. However, South Africa’s public health sector continues to face resource limitations, which negatively affect access to quality hospital care and overall hospital performance [18–20]. Despite significant efforts by the government to improve healthcare delivery, there remains a wide variation in the quality of care within and between provinces, posing a significant challenge to the country’s health sector [21, 22]. These variations may, among others, perpetuate inequities in healthcare access and outcomes [23, 24], erode patient trust and satisfaction and complicate the monitoring and evaluation of healthcare programs [25]. Public healthcare facilities exhibit poor performance in various quality indicators, including prolonged waiting time because of a shortage of human resources, adverse events, poor hygiene, and poor infection control measures, increased litigation due to avoidable errors, shortage of medicine and equipment, poor record-keeping, poor-quality healthcare delivery and, old and poorly maintained infrastructure [26, 27]. All these contribute to the rising levels of patients’ dissatisfaction with the quality of healthcare received in hospitals [28]. This is because customer satisfaction is impacted by service quality [29].
A 2018 South African public healthcare facilities survey found that almost 50% of patient participants were dissatisfied with the service they received [22]. Long patient waiting times and staff attitudes have been reported as two major factors influencing the level of patient satisfaction [30]. Patients who waited less than half an hour before being examined by a doctor reported higher levels of satisfaction compared to those who waited for longer than 30 min. Non-availability of prescribed medication was found to be associated with bad patient experience of care [31]. It was also observed that the type of facility that patients had attended created a false association between their area of residence and their overall experience [32].
Patient safety remains a concern in health facilities, dating back to the principle of “first do no harm” [33]. This concern is partly due to a lack of utilisation of the patient safety incidents (PSI) reporting system by health professionals as they are afraid of litigation and disciplinary action [34]. In 2017, the NDoH introduced the national PEC assessment guideline [8] in addition to Batho Pele principles (1997) [35], Patients’ Rights Charter for South Africa (1999) [36], and National Core Standards for Establishments in South Africa (2013) [37]. The PEC guideline focuses on six priority areas of care which are used as predictors and dimensions that inform the level of patient satisfaction: access to care, availability and use of medicines, patient safety, cleanliness, and infection and prevention and control, values and attitudes of staff, and patient waiting time for care [8].
Despite the various government initiatives implemented to enhance healthcare efficiency, safety, quality, and accessibility in South Africa, the problem of unequal access to quality healthcare services persists [38]. Patients from most South African rural areas are compelled to travel long distances to urban tertiary and quaternary health centres to access specialist healthcare services [39]. To address these challenges, South Africa is currently in the process of implementing the national health insurance (NHI), which aims to provide universal high-quality care for all South Africans, regardless of their ability to pay [40].
This study forms part of an ongoing cluster Randomised Controlled trial (RCT) titled “Exploring the feasibility of improving the performance of public hospitals through a focused implementation of clinical governance interventions in South Africa’s Eastern Cape and Mpumalanga Provinces”. Both provincial health departments consist of a network of hospitals ranging from district hospitals to tertiary hospitals in Mpumalanga and up to a central hospital in the Eastern Cape province. Regional hospitals are not developed enough to provide first-line general medical specialist services and do not have adequate capacity to provide reasonable access to specialist hospital care, thus protecting tertiary and central hospitals from unnecessary referrals. Strong district and regional hospitals provide an important foundation for a sustainable referral network. Both provinces have emerging tertiary hospital services, which provide tertiary care for the public sector-dependent majority population.
PECs are a critical component of clinical governance. However, no research studies have been conducted to solicit feedback from healthcare service users in the selected hospitals. Specifically, this study focuses on assessing patients’ experiences of care in four referral hospitals located in two rural provinces of South Africa.
These findings will shed light on specific service delivery challenges unique to each hospital, providing valuable guidance for improving the quality and overall performance of their services.
Methods
Study design
This study aimed to assess patients’ experience of care in four referral hospitals in two of South Africa’s rural provinces. An analytic cross-sectional design was used to collect data as part of an ongoing cluster Randomised Controlled trial (RCT).
Study setting
The study was conducted in four public hospitals in the Eastern Cape (Nelson Mandela Academic (NMAH) and St. Elizabeth (SEH)) and Mpumalanga (Rob Ferreira Hospital (RFH) and Themba Hospital) provinces. The Eastern Cape and Mpumalanga provinces have the fourth largest and sixth largest populations in South Africa, respectively [41]. The two provinces have a high proportion of rural populations [41]. Most of the people rely on public health facilities for healthcare.
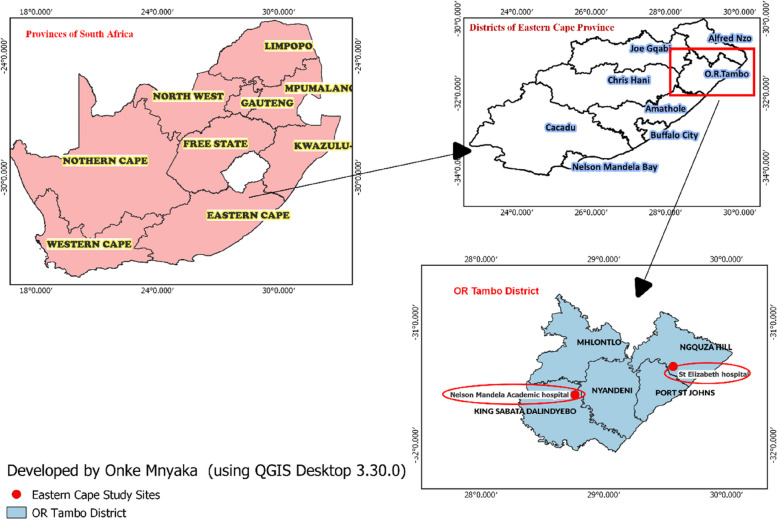
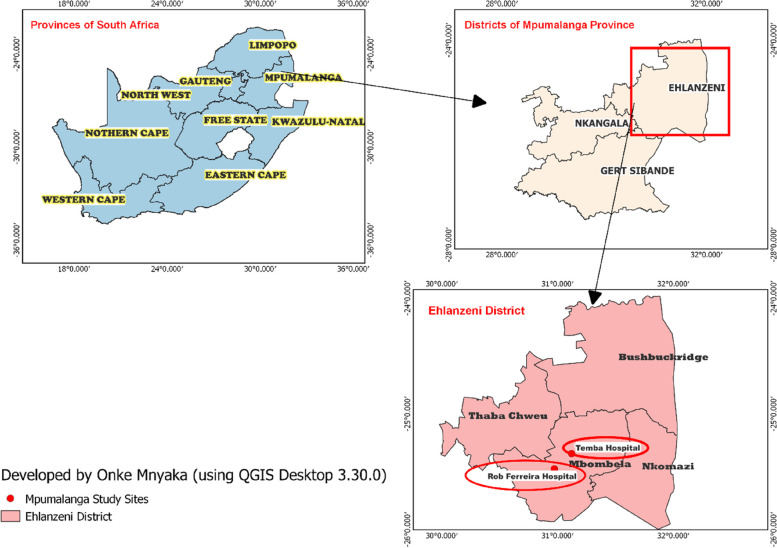
The participating hospitals in the OR Tambo health district, Eastern Cape Province are highlighted in Fig. 1 and those in the Ehlanzeni health district, Mpumalanga Province are highlighted in Fig. 2. The two districts are classified among regions with suboptimal healthcare delivery in South Africa [42].
Fig. 1.
Study area Map, Eastern Cape Province
Fig. 2.
Study area Map, Mpumalanga Province
Population and sampling
All patients receiving healthcare services in the four hospitals constituted the population for this study.
A systematic random sampling of patients attending the outpatient department (general, discipline specific outpatient departments and outpatient pharmacy services) was conducted by approaching every fifth patient in the outpatient waiting area or pharmacy queues until the sample size was reached. A total combined sample size for all four hospitals was calculated using the equation, for a one-sided 95% confidence interval and a 5% significance level (z = 1.96). Because the proportion (p) of patients who were either satisfied or not satisfied with the quality of care received was not known, this (p) was set at 50% and the desired precision (d) was set at 4%. These assumptions yielded a total minimum sample size of 600, and a further 10% (60) was added to factor in data entry errors. A total sample size of 660 participants was then distributed proportionally across all four sites (based on the number of beds). The study considered the following categories of patients for participation: (i) patients able to give informed consent, (ii) patients with unimpaired decision-making capacity and (iii) designated representatives for patients unable to participate. Patients excluded from the study include (i) individuals lacking decision-making capacity, (ii) those whose health condition affects clear thinking unless they insist, (iii) those mentally unfit to understand and respond, and (iv) those too ill to participate without family members [8].
Data collection
Data were collected over a two-week period in July 2022. The NDoH recommends that the PEC survey should be conducted during July, August and September each year. The NDoH suggests that there is an increase in care-seeking behaviour during this recommended period [8]. Data were collected in line with the guideline for conducting PEC which is outlined as follows: (i) patients were notified about the data collection by the hospital staff as part of general announcements to patients, (ii) no hospital staff members were involved in the collection of data. The research team was divided into teams who collected the data over five working days in each hospital as recommended by the NDoH [8]. The standardised and validated quantitative survey tool1 on patient experience of outpatients used by the South African Department of Health (Appendix A) [8] was adopted and used for data collection. This tool asks questions on biographical data; access to care; availability and use of medicines; patient safety; cleanliness; values and attitudes; and waiting times. The research team hired two language translators fluent in English and three local languages (isiXhosa, siSwati, and isiZulu). The first translator translated the data collection tools, and the second translator back-translated the data collection tools. The translators were chosen based on their proficiency and experience in translating health-related materials to ensure accuracy and cultural relevance for the participants. The questionnaire was translated into isiXhosa, siSwati, and isiZulu to accommodate participants who were not comfortable with English.
Data management and analysis
Upon completion of data collection, questionnaires were checked for completeness and consistency before data was entered into a Microsoft Excel spreadsheet. Data validation settings were used to prevent and/or minimise erroneous entries. The complete case analysis method was employed to handle missing data.
Data were analysed using STATA version 17.0 (STATA Corp, College Station, Texas, USA). Categorical variables were compared using frequencies, percentages, and graphs. The Shapiro-Wilk test was used to determine the distribution of numerical data. Numerical variables are presented using the median and interquartile range (IQR) as they were not normally distributed. Categorial data were summarised using frequency tables and graphs. The Kruskal-Wallis test was used to compare the median ages of participants in the four hospitals. According to the National Guideline for PEC surveys, the scoring process involves coding the survey responses and calculating individual scores for each domain [8]. This scoring is achieved by aggregating the scores of individual survey questions pertaining to a specific domain. Weighted averages are then computed, considering the assigned importance of each item as assigned by the NDoH [8]. An aggregate score of 80% or higher indicates satisfaction, while any score below this threshold indicates dissatisfaction [8]. This criterion serves as a benchmark for assessing the level of satisfaction based on the calculated scores. The level of statistical significance was set at p-value ≤ 0.05.
Results
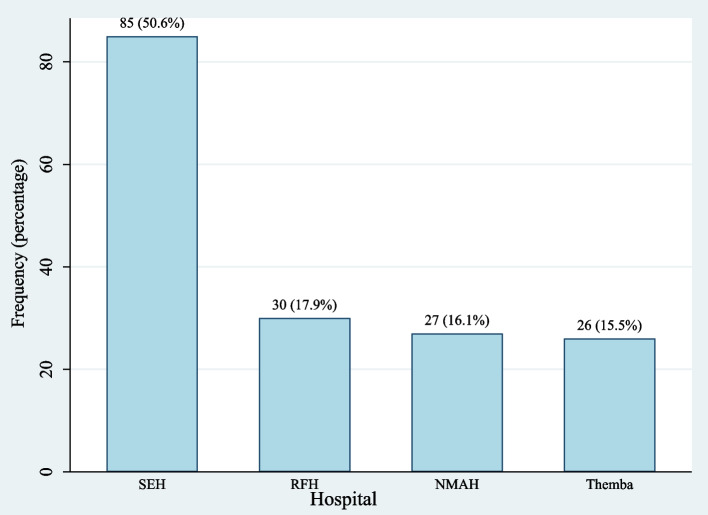
Participants were almost equally distributed between the four hospitals (± 25%). A total of 662 (92.2%) patients were surveyed between the four hospitals, out of 718 patients approached. Reasons for refusal to participate were not sought. The demographic characteristics are summarised in Table 1, where females accounted for 71.6% of participants (474/662); the median age was 47 years, and just over a third of participants (250/662, 37.8%) were younger than 40 years but at least 18 years old, and 20.2% (133/657) had a disability that required assistance. Of the 133 individuals with a disability, 86.5% (115/133) received hospital assistance with their disability. For example, patients who were in wheelchairs would ask for assistance to navigate the hospital. The 18/133 (13.5%) who reported having not received assistance on their disability were at TH (10/18, 55.6%), RFH (33.3%, 6/18) and NMAH (11.1%, 2/18).
Table 1.
Summary of demographic characteristics
| Characteristics | Overall | NMAH | RFH | SEH | TH | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | 662 | (100.0) | 163 | (24.6) | 167 | (25.2) | 166 | (25.1) | 166 | (25.1) |
| Sex; n (%) | ||||||||||
| Female | 474 | (71.6) | 113 | (69.3) | 120 | (71.9) | 109 | (65.7) | 132 | (79.5) |
| Male | 188 | (28.4) | 50 | (30.7) | 47 | (28.1) | 57 | (34.3) | 34 | (20.5) |
| Agea, years; med (IQR) | 47 | (27.0) | 53 | (27.0) | 42 | (26.0) | 50 | (29.0) | 40 | (28.0) |
| Agea, years; n (%) | ||||||||||
| 18–29 | 123 | (18.7) | 12 | (7.4) | 38 | (22.8) | 26 | (15.7) | 47 | (28.8) |
| 30–39 | 127 | (19.3) | 30 | (18.4) | 35 | (21.0) | 31 | (18.7) | 31 | (19.0) |
| 40–49 | 117 | (17.8) | 30 | (18.4) | 30 | (18.0) | 25 | (15.1) | 32 | (19.6) |
| 50–69 | 216 | (32.8) | 62 | (38.0) | 52 | (31.1) | 55 | (33.1) | 47 | (28.8) |
| 70–90 | 76 | (11.5) | 29 | (17.8) | 12 | (7.2) | 29 | (17.5) | 6 | (3.7) |
| Requires assistance with disabilityb, x; n (%) | ||||||||||
| Yes | 133 | (20.2) | 38 | (23.3) | 36 | (21.6) | 18 | (10.9) | 41 | (25.3) |
| No | 524 | (79.8) | 125 | (76.7) | 131 | (78.4) | 147 | (89.1) | 121 | (74.7) |
| Previous visits to this health facility; n (%) | ||||||||||
| Yes | 518 | (78.5) | 148 | (91.4) | 125 | (74.9) | 125 | (75.3) | 120 | (72.7) |
| No | 142 | (21.5) | 14 | (8.6) | 42 | (25.2) | 41 | (24.7) | 45 | (27.3) |
| More than 2-hours to get to hospital; n (%) | ||||||||||
| Yes | 350 | (52.9) | 107 | (65.6) | 82 | (49.1) | 67 | (40.4) | 94 | (56.6) |
| No | 312 | (47.1) | 56 | (34.4) | 85 | (50.9) | 99 | (59.6) | 72 | (43.4) |
NMAH Nelson Mandela Academic Hospital, RFH Rob Ferreira Hospital, SEH St. Elizabeth Hospital, TH Themba Hospital
aTH has 3 participant responses with missing age; bSEH has 1 participant response missing; xTH has 4 participant response missing
Further shown in Table 1 is that 65.6% (107/163) and 56.6% (94/166) of participants from NMAH and TH, respectively, travelled for more than two hours to get to the hospital, either when using a private vehicle or public transport (taxi or bus). More than three-quarters of the patients (78.5%, n = 518/662) had received health services from the same facility within the 12-months prior to the survey. Figure 3 shows that patients from RFH and TH were statistically younger than those from NMAH and SEH (p-value < 0.0001).
Fig. 3.
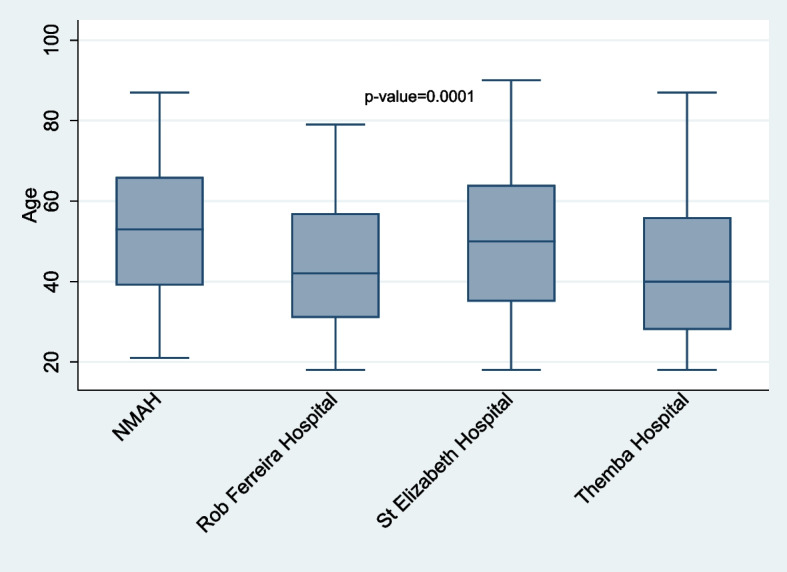
Median age comparisons of participants
Table 2 shows a statistically significant difference between participants reporting to have been previously turned away from the hospitals (p-value < 0.0001). RFH participants reported 33.6% (42/125) and NMAH participants reported 7.4% (11/148) of previously turned away participants. While service times were reported to be acceptable by 71.2% (116/163) of NMAH participants, 50.3% (84/167) and 51.2% (84/164) of RFH and TH participants respectively found the service times unacceptable. This finding was statically significant (p-value < 0.0001). Majority of the participants in all hospitals did not expect to be transferred to another hospital. More than 70% of the participants in three of the four hospitals reported that warning signage was present in the hospital walkways except for TH (34.6%, 55/159) reported (p-value < 0.0001). More than 80% of participants reported having their identities confirmed in each hospital, with all SEH’s participants reporting positively (p-value < 0.0001). Similarly, all SEH’s participants reported being informed of the treatment plan by doctors and nurses (p-value = 0.028) and being informed about their health condition in detail (p-value < 0.0001).
Table 2.
Access to care and communication
| Characteristic | Hospital | p-value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NMAH | RFH | SEH | TH | |||||||
| Previously turned away from this hospitala; n (%) | < 0.0001 | |||||||||
| Yes | 11 | (7.4) | 42 | (33.6) | 12 | (9.6) | 23 | (19.3) | ||
| No | 137 | (92.6) | 83 | (66.4) | 113 | (90.4) | 96 | (80.7) | ||
| Acceptable service timesb; n (%) | < 0.0001 | |||||||||
| Yes | 116 | (71.2) | 83 | (49.7) | 94 | (56.6) | 80 | (48.8) | ||
| No | 47 | (28.8) | 84 | (50.3) | 72 | (43.4) | 84 | (51.2) | ||
| Expectation of being referred to another hospitalc; n (%) | 0.007 | |||||||||
| Yes | 78 | (47.9) | 54 | (32.3) | 53 | (31.9) | 68 | (41.2) | ||
| No | 85 | (52.2) | 113 | (67.7) | 113 | (68.1) | 97 | (58.8) | ||
| Presence of warning signage in the hospital walkwaysd; n (%) | < 0.0001 | |||||||||
| Yes | 102 | (62.6) | 117 | (70.9) | 17 | (94.4) | 55 | (34.6) | ||
| No | 61 | (37.4) | 48 | (29.1) | 1 | (5.6) | 104 | (65.4) | ||
| Identity confirmatione; n (%) | 0.029 | |||||||||
| Yes | 134 | (82.2) | 152 | (91.0) | 18 | (100.0) | 138 | (84.7) | ||
| No | 29 | (17.8) | 15 | (9.0) | 0.0 | (0.0) | 25 | (15.3) | ||
| Informed of health conditionf; n (%) | < 0.0001 | |||||||||
| Yes | 154 | (94.5) | 140 | (83.8) | 18 | (100.0) | 124 | (77.0) | ||
| No | 9 | (5.5) | 27 | (16.2) | 0.0 | (0.0) | 37 | (23.0) | ||
| Informed of Treatment planf; n (%) | 0.028 | |||||||||
| Yes | 139 | (85.3) | 138 | (82.6) | 18 | (100.0) | 123 | (76.4) | ||
| No | 24 | (14.7) | 29 | (17.4) | 0.0 | (0.0) | 38 | (23.6) | ||
NMAH Nelson Mandela Academic Hospital, RFH Rob Ferreira hospital, SEH St. Elizabeth Hospital, TH Themba Hospital
an = 517; bn = 660; cn = 661); dn = 505; en = 511; fn = 509
More than two-thirds (67.8%, 223/329) of Mpumalanga province’s (FRH & TH) participants reported the absence of drinking water (p-value < 0.0001). Majority of the participants (68.5%, 111/162) of TH did not think that the hospital was clean compared to NMAH’s (82.2%,134/163) (p-value < 0.0001). 59.8% (98/164) and 43.7% (73/167) of TH and RFH’s participants respectively had not seen waste disposal bins in the corridors; 75.3% (125/166) of SEH’s participants reported seeing pests like cockroaches in the hospital compared to 15.4% (23/149) by RFH participants (Table 3).
Table 3.
Cleanliness, sanitation and water availability in hospitals
| Characteristic | Hospital | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| NMAH | RFH | SEH | TH | ||||||
| Availability of drinking waterd; n (%) | < 0.0001 | ||||||||
| Yes | 111 | (68.1) | 56 | (33.5) | 94 | (56.6) | 50 | (30.9) | |
| No | 52 | (31.9) | 111 | (66.5) | 72 | (43.4) | 112 | (69.1) | |
| Cleanliness of the hospitald; n (%) | < 0.0001 | ||||||||
| Yes | 134 | (82.2) | 94 | (56.3) | 134 | (80.7) | 51 | (31.5) | |
| No | 29 | (17.8) | 73 | (43.7) | 32 | (19.3) | 111 | (68.5) | |
| Availability of waste disposal bins in corridorsb; n (%) | < 0.0001 | ||||||||
| Yes | 116 | (71.2) | 94 | (56.3) | 160 | (96.4) | 66 | (40.2) | |
| No | 47 | (28.8) | 73 | (43.7) | 6 | (3.6) | 98 | (59.8) | |
| Presence of pestse; n(%) | |||||||||
| Yes | 56 | (34.4) | 23 | (15.4) | 125 | (75.3) | 52 | (36.4) | < 0.0001 |
| No | 107 | (65.6) | 126 | (84.6) | 41 | (24.7) | 91 | (63.6) | |
| Use of toiletsb; n (%) | < 0.0001 | ||||||||
| Yes | 125 | (76.7) | 137 | (82.0) | 165 | (99.4) | 122 | (74.4) | |
| No | 38 | (23.3) | 30 | (18.0) | 1 | (0.6) | 42 | (25.6) | |
| Toilets are in good conditiong; n (%) | |||||||||
| Yes | 103 | (82.4) | 91 | (66.9) | 128 | (77.6) | 52 | (43.7) | < 0.0001 |
| No | 22 | (17.6) | 45 | (33.1) | 37 | (22.4) | 67 | (56.3) | |
| Availability of toilet paper; n (%) | < 0.0001 | ||||||||
| Yes | 55 | (44.0) | 65 | (47.8) | 95 | (57.6) | 30 | (25.0) | |
| No | 70 | (56.0) | 71 | (52.2) | 70 | (42.4) | 90 | (75.0) | |
| Availability of running tap water in toiletc; n (%) | < 0.0001 | ||||||||
| Yes | 119 | (95.2) | 117 | (86.0) | 122 | (73.9) | 70 | (57.4) | |
| No | 6 | (4.8) | 19 | (14.0) | 43 | (26.1) | 52 | (42.6) | |
| Availability of hand wash basin in toiletc; n(%) | 0.046 | ||||||||
| Yes | 103 | (82.4) | 108 | (79.4) | 120 | (72.7) | 84 | (68.9) | |
| No | 22 | (17.6) | 28 | (20.6) | 45 | (27.3) | 38 | (31.2) | |
| Availability of liquid soap dispensera; n(%) | |||||||||
| Yes | 57 | (45.6) | 40 | (29.6) | 75 | (45.5) | 24 | (19.8) | < 0.0001 |
| No | 68 | (54.4) | 95 | (70.4) | 90 | (54.6) | 97 | (80.2) | |
| Availability of disposable paper towelf; n(%) | |||||||||
| Yes | 52 | (41.6) | 27 | (19.9) | 7 | (4.2) | 19 | (16.4) | < 0.0001 |
| No | 73 | (58.4) | 109 | (80.2) | 158 | (95.8) | 102 | (84.3) | |
| Availability of waste disposal bins with lid in toileta; n (%) | |||||||||
| Yes | 105 | (84.7) | 71 | (52.2) | 152 | (92.1) | 38 | (31.4) | < 0.0001 |
| No | 19 | (15.3) | 65 | (47.8) | 13 | (7.9) | 83 | (68.6) | |
NMAH Nelson Mandela Academic Hospital, RFH Rob Ferreira hospital, SEH St. Elizabeth Hospital, TH Themba Hospital
an = 546; bn = 660; cn = 548; dn = 658; en = 621; fn = 547; gn = 545
Most (71.5%, 473/662) participants were surveyed at pharmacy after receipt of prescriptions. While 94.3% (446/473) of these participants had received their prescribed medication, 5.3% (25/473) did not receive all their prescribed medication. The 25 patients who had not received all their prescribed medication were from RFH (56.0%, 14/25), TH (32.0%, 8/25) and SEH (12.0%, 3/25). Even though 94.9% (449/473) of patients with prescriptions recalled receiving information on how to take medication, only 64.5% recalled being given information on the side effects of the prescribed medication. More than half of the patients (51.2%, 85/166) who reported not being given information on the side effects of the medication were from SEH (Fig. 4).
Fig. 4.
Information on prescribed medication side effects (NMAH = Nelson Mandela Academic Hospital, RFH = Rob Ferreira hospital; SEH = St. Elizabeth Hospital; TH = Themba Hospital)
More than 70% of participants had used the hospital toilets and they reported that the toilets were generally in a good condition at NMAH (82.4%, 103/125), SEH (77.58%, 128/165) and RFH (66.9%, 91/136) but not at TH (56.3%, 67/119), toilet paper was reported to be unavailable by 75.0% (90/120), 56.0% (70/125) and 52.2% (71/136) of TH, NMAH and RFH participants respectively. Most (95.2%, 119/125) participants at NMAH participants reported the availability of running tap water in the toilet compared to 57.4% (70/122) of participants from TH. More than two-thirds of each of the hospitals’ participants reported the availability of a hand wash on the toilet sink basin. More than half of each of the hospitals’ participants reported the absence of a liquid soap dispenser in toilets, and TH had the highest such participants (80.2%, 97/121). Paper towels were reported to be available by 4.2% (7/165) and 41.6% (52/125) of participants at SEH and NMAH, respectively (Table 3). Most participants at SEH (92.1%, 152/165) and NMAH (84.7%, 105/124) reported availability of waste disposal bins with lids in the toilets, while only 31.4% (38/121) of TH’s participants were positive on this measure. All these differences (Table 3) were statistically significant (p-value < 0.05).
More than 50% of three of the four hospitals’ participants reported that health workers had introduced themselves, while only 32.7% (54/165) of SEH’s participants had a health worker introducing themselves (p-value < 0.0001). Majority of participants across all hospitals reported that consultations were mostly in private; and at least 70% of participants in each of the hospitals found the health professionals to be respectful towards them and other patients (p-value < 0.0001) (Table 4). Two-thirds (66.7%, 108/162) of NMAH’s participants were not asked for permission before being treated participants or not afforded an opportunity to ask questions (63.8%, 104/163). In comparison, 91.6% (152/166) and 81.4% (136/167) of participants from SEH and RFH respectively, were offered that opportunity (p-value < 0.0001).
Table 4.
Staff attitudes, courtesy, waiting time, and complaints management
| Characteristic | Hospital | p-value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NMAH | RFH | SEH | TH | |||||||
| Health workers introduced themselvesa; n(%) | < 0.0001 | |||||||||
| Yes | 99 | (60.7) | 96 | (57.5) | 54 | (32.7) | 85 | (53.1) | ||
| No | 64 | (39.3) | 71 | (42.5) | 111 | (67.3) | 75 | (46.9) | ||
| Permission asked before being treateda; n(%) | < 0.0001 | |||||||||
| Yes | 54 | (33.3) | 110 | (65.9) | 124 | (74.7) | 95 | (59.4) | ||
| No | 108 | (66.7) | 57 | (34.1) | 42 | (25.3) | 65 | (40.6) | ||
| Provided opportunity to ask questionsb; n(%) | < 0.0001 | |||||||||
| Yes | 59 | (36.2) | 136 | (81.4) | 152 | (91.6) | 109 | (69.4) | ||
| No | 104 | (63.8) | 31 | (18.6) | 14 | (8.4) | 48 | (30.6) | ||
| Consultation was in a private spaceb; n(%) | < 0.0001 | |||||||||
| Yes | 141 | (87.0) | 139 | (83.2) | 166 | (100.0) | 115 | (71.9) | ||
| No | 21 | (13.0) | 28 | (16.8) | 0 | (0.0) | 45 | (28.1) | ||
| Health workers generally respectful towards patientsb; n (%) | 0.003 | |||||||||
| Yes | 128 | (78.5) | 149 | (89.2) | 128 | (77.1) | 117 | (73.6) | ||
| No | 35 | (21.5) | 18 | (10.8) | 38 | (22.9) | 42 | (26.4) | ||
| Knowledge of how to lodge a complaintc; n (%) | 0.002 | |||||||||
| Yes | 50 | (30.7) | 72 | (43.1) | 83 | (50.0) | 57 | (35.2) | ||
| No | 113 | (69.3) | 95 | (56.9) | 83 | (50.0) | 105 | (64.8) | ||
| Queues are monitored by health workersd; n(%) | < 0.0001 | |||||||||
| Yes | 126 | (77.3) | 83 | (49.7) | 134 | (80.7) | 73 | (44.8) | ||
| No | 37 | (22.7) | 84 | (50.3) | 32 | (19.3) | 90 | (55.2) | ||
| Communication on expected waiting timesc; n (%) | < 0.0001 | |||||||||
| Yes | 90 | (55.6) | 55 | (32.9) | 108 | (65.1) | 64 | (39.3) | ||
| No | 72 | (44.4) | 112 | (67.1) | 58 | (34.9) | 99 | (60.7) | ||
| Acceptability of waiting timesc; n (%) | < 0.0001 | |||||||||
| Yes | 86 | (52.8) | 55 | (32.9) | 108 | (65.1) | 45 | (27.6) | ||
| No | 77 | (47.2) | 112 | (67.1) | 58 | (34.9) | 118 | (72.4) | ||
NMAH Nelson Mandela Academic Hospital, RFH Rob Ferreira Hospital, SEH St Elizabeth Hospital, TH Themba Hospital
an = 655; bn = 653; cn = 658; dn = 659
The highest proportion of participants who said they knew how to lodge a complaint were from SEH (50.0%, 83/166. The differences between the four hospitals were statistically significant (p = 0.002) (Table 4). While more than 75% of both Eastern Cape’s hospitals’ (NMAH and SEH) participants observed queues being monitored by health workers, this was far less at RFH (49.7%, 83/167) and TH (44.8%,73/163) (p-value < 0.0001). Furthermore, more than 60% of each of RFH and THs participants felt that there had been no communication on the expected waiting times (p-value < 0.0001). The waiting times were reported as unacceptable by 72.4% (118/163) and 67.1% (112/167) of TH’s and RFH’s participants respectively (p-value < 0.0001).
Table 5 shows the overall performance of hospitals against the national targets for patients’ experience of care domains. All hospitals scored below the national targets on overall patient satisfaction, values and attitudes of staff, access to care, cleanliness, and waiting times. TH did not meet any of the national targets. All the hospitals, except TH, met the patient safety target, but only NMAH met the target on availability and use of medicines.
Table 5.
Overall scores of hospitals against the national targets for patients’ experience of care domains
| Domain | National target (%) | Hospital score | |||
|---|---|---|---|---|---|
| NMAH (%) | RFH (%) | SEH (%) | TH (%) | ||
| Access to care | 100 | 59.3 | 54.0 | 70.5 | 52.4 |
| Availability and use of medicines | 95 | 95.1 | 68.8 | 85.7 | 70.3 |
| Patient safety | 65 | 76.5 | 72.7 | 84.2 | 60.5 |
| Cleanliness of the hospital | 74 | 67.6 | 54.0 | 68.4 | 40.6 |
| Values and attitudes of staff | 74 | 54.4 | 70.1 | 71.0 | 60.4 |
| Waiting times | 74 | 61.9 | 38.5 | 70.3 | 37.2 |
|
Overall patient experience of care survey results |
80 | 69.1 | 59.7 | 75.0 | 53.6 |
NMAH Nelson Mandela Academic Hospital, RFH Rob Ferreira hospital, SEH St. Elizabeth Hospital, TH Themba Hospital
Discussion
This study assessed participants’ experiences of care in four referral hospitals in two of South Africa’s rural provinces.
The sample population in this study mostly consisted of females. A significant number of participants were below 40 years of age. Some participants had to travel for at least two hours to reach the hospital, regardless of their mode of travel. This is expected as these hospitals primarily serve geographically dispersed areas in two largely rural provinces. This study found poor patient satisfaction results, low access to care and prolonged waiting times. Some patients reported hospitals to be unclean without clean drinking water; and, a significant proportion of participants reporting poor safety in hospitals, and most patients did not know the process that is followed for lodging a complaint in the hospital. However, there were some positive findings, with most participants expressing satisfaction with the staff attitudes across all hospitals. Additionally, most participants reported being content with service times, and the majority noted the presence of visible signage in the hospitals.
The majority of patients in two hospitals travelled at least two hours to get to the hospital, irrespective of the mode of travel. This finding was expected because one of the two hospitals (NMAH) is a referral hospital that covers a wide area that is sparsely populated [43]. A small proportion of patients reported being turned away in all the hospitals. However, the reasons for these were not explored. It is likely that patients tried to access the referral hospitals without a referral from a primary or lower level of care and were turned away as a result [44]. In some healthcare systems, patients are sometimes turned away from hospitals, a practice known as “gatekeeping.” This happens when patients are required to seek care at primary or lower-level facilities before they can access higher-level hospitals. The South African Human Rights Commission reported that patients in both urban and rural areas have been turned away from hospitals for various reasons, including issues with the referral system [45]. The gatekeeping process is intended to reduce the burden on hospitals and ensure that only cases requiring specialized care are referred to tertiary hospitals [46]. A second explanation could be that patients did not come on their pre-arranged date of visit [47]. The problem of patients being turned away from hospitals can be minimised by strengthening primary care and level 1 hospitals (district hospitals), and patients being turned away should be triaged appropriately and advised on an alternative place of care [47]. Furthermore, community engagement should be strengthened to offer the general public a clear understanding of the services offered at different levels of care and the challenges experienced in meeting the minimum requirements. These challenges include staff shortages, infrastructure limitations, and financial constraints [48–50].
The provision of high-quality services enhances the satisfaction and overall experience of patients receiving care [51]. Surveys measuring patients’ experiences are critical in informing clinical decision-making by gathering feedback from individuals utilising healthcare services [52]. This feedback assists decision makers in evaluating whether user expectations are being met or not. In this study, participants from one of the Eastern Cape hospitals (NMAH), reported that health professionals did not seek their permission before administering treatment. This highlights the significance of ongoing education for all staff members, emphasising the importance of respecting patient autonomy and stating that patients should be fully informed about their treatment options and involved in decision-making as much as possible [53].
Of the four hospitals, only one achieved the national target on the availability of medicine. Overall, the four hospitals achieved an average of 80.0% for this target. This finding is comparable to those reported in a study that was conducted in another South African province (Free State), where the availability of medicine averaged between 75% and 95% [54]. Availability of medicines in public health facilities is impacted by different factors including, poor medicine stock management, late deliveries from the medical depot, poor communication amongst the role players, lack of electronic ordering system, duplication of patients in the system, medicine theft, transport, department red tape [54] and insufficient availability of pharmacy personnel [55]. Shortages of medicine have also been reported in other African countries [51, 56–59].
Despite most participants reporting satisfaction with the communication by health professionals on matters concerning their illness and treatment plans, it is of concern that some participants (42%) reported that they were not asked for verbal consent before being examined or treated. This finding is in contrast to a Nigerian study, where 90.6% of patients felt listened to by doctors, and 74.1% always received an explanation for the tests ordered by doctors [51]. The reported lack of communication by health professionals is a concern as this power imbalance can be associated with patients’ withdrawal or inability to freely engage with the health professional [60]. Patients’ poor understanding of the procedures undertaken or the treatment care plan are associated with litigation when the unexpected happens [61]. Despite this, healthcare workers in resource-limited settings, such as South African public hospitals, often face significant constraints. These include heavy patient loads and limited time to engage in thorough informed consent processes. This can hinder proper engagement with patients due to health workforce shortages and the high volume of patients that the health system needs to address [49].
Safer and higher quality care are prevalent in facilities that provide better experiences for patients [62, 63]. Safety is also critical for securing patient loyalty because negative perceptions or disliked previous experiences of safety encourages patients to bypass those facilities and put pressure on others [63]. Even though three of the hospitals performed above the national target of 65% for the safety domain [8], the target performance is 100%, as one safety concern could cause the loss of life of a patient, increase mistrust of communities in the hospital and result in a cascade of late diagnoses in the community whilst they seek alternative care [64–66].
The two hospitals from Mpumalanga recorded scores that are below 55% for cleanliness, whilst their Eastern Cape counterparts obtained a minimum score of 67%. As one of the measures that contribute to overall patient satisfaction, hospital cleanliness has a significant influence on the overall patient satisfaction [43, 64–67]. This is evident in the current study where both Mpumalanga hospitals recorded the highest overall patient experience of care score of 60%, which is very far from the national target of at least 80% [8]. This finding is concerning because hospitals are supposed to have higher hygiene standards than non-health organisations [68]. The findings are, however, consistent with previous studies in South Africa, which found some hospital sections had an unacceptable physical environment including toilets [69]. Contrasting findings have been reported in a study conducted in Nigeria where a slight majority (51.8%) agreed that the hospital environment was clean [51]. It is of further concern that some participants (mostly those from Mpumalanga) reported non-availability of drinking water. Similar findings were reported by Obi et al. where only a minority of participants expressed satisfaction about aspects of the hospital environment, like availability of potable water (18.8%), cleanliness of bathrooms and toilets (14.7%) [51].
The positive finding from this study is that participants generally expressed satisfaction with staff attitudes in all the participating hospitals. This finding aligns with a study by Harrichandparsad & Mahomed [32] conducted in eThekwini, KwaZulu-Natal, South Africa, who reported a satisfaction level of 92%. Patients in Nigeria reported that believed that nurses treated them with respect (51.4%), were approachable (52%) and polite and courteous (51.4%) [70]. Furthermore, according to a study conducted by Obi et al. [51] it was found that most participants acknowledged the courteous and professional behaviour of doctors (90%), nurses (64.1%), and records staff (60.6%). However, this finding deviates from other literature that have documented negative staff attitudes. For instance, Mokgoko [68] found that participants reported being spoken to by healthcare workers in a condescending manner, as if they were children. Moreover, nurses were reported by a significant majority (70%) of the patients to have a rude attitude towards them [70]. Satisfaction levels were also low when it came to the attitudes of pharmacy staff (41.8%) and the medical laboratory staff (43.5%) [51]. The South African National Department of Health has identified negative staff attitudes as one of the major challenges in the health system [71].
Patient waiting time is a critical factor that influences the overall satisfaction of patients [72]. Long waiting times are associated with patient dissatisfaction, delayed access to treatments, poor clinical outcomes, increased costs, patient inequality, and patient anxiety [73]. All South African health establishments are compelled by the National Department of Health to have a standard patient waiting time that emphasises a culture of proactive patient notification of expected waiting times for service [8]. The findings of this study revealed waiting times that were deemed unacceptable by the participants. Likewise, additional studies carried out in South Africa by Young, and Klitzman [26, 74] identified prolonged waiting times as a significant drawback in public healthcare, attributing it to various factors. Similarly, a study conducted in Nigeria reported that patients were not satisfied with clinic waiting time (44.7%), laboratory waiting time (31.8%), and pharmacy waiting time (42.9%) [51]. Factors that have a negative impact on waiting times include, poor record keeping [75], human resource shortages, physical space limitations, a high patient volume [76], waiting for administration staff draw clinical records, and pharmacy-related delays [68]. Sometimes patients are not properly orientated on where to go upon arrival at the hospital [76], and in one study almost a quarter (23%) of the participants were observed to lack proper orientation on the hospital. Future studies should explore if this lack of orientation cannot perhaps be mitigated by the presence of marshals and signage from the main entrance. Security personnel who are usually the most accessible persons and a service that is often outsourced to private companies, need to also be orientated on the service points at the hospital so that they can direct patients and their families accordingly.
Our findings highlight areas where these hospitals are doing well and where there are service quality difficulties that need to be addressed to improve service delivery. The findings will guide or enable relevant stakeholders to contextualise quality improvement intervention strategies. Moreover, this study enables hospitals to evaluate acceptance of their services by patients and to some extent understand existing challenges.
This study used a standardised tool for conducting patients’ experiences of care surveys in South Africa which limited probing in instances where the situation demanded as such. Furthermore, findings may not be generalised to the entire patient population because this study was limited to outpatients. However, the use of a standardised tool makes it easier to compare these findings with other South African hospitals’ findings that are assessed using this tool in outpatient settings. The use of a cross-sectional design also eliminated the possibility of corroborating the patients’ responses. However, these findings have provided insights into patients’ perceptions on their experience of care.
This study also provides an opportunity for the participating hospitals to use patients’ feedback to compare their service delivery against other hospitals within and between provinces.
Conclusion
Whilst hospitals have been implementing various quality measures to improve patient’s experience of care, there are a few concerns such as non-availability of drinking water, lack of knowledge of complaints processes and waiting times that were mostly reported to not be acceptable. Furthermore, none of the four hospitals met all the national targets. And only two out of 28 potential domains exceeded 80% or the cut-off score for satisfaction. These are concerns which calls for active interventions in at least these four public hospitals. Efforts to address the highlighted areas which affect patient experiences should be made to continue improving patient care.
Supplementary Information
Acknowledgements
The work reported herein was made possible through funding by the South African Medical Research Council via its Division of Research Capacity Development under the Mid-Career Scientist Programme. The content hereof is the sole responsibility of the authors and does not necessarily represent the official views of the SAMRC. The authors would also like to thank the officials of the participating hospitals and provinces for their support and assistance.
Abbreviations
- DOH
Department of Health
- EC
Eastern Cape province
- HOD
Head of Department
- IQR
Interquartile Range
- MP
Mpumalanga province
- NDOH
National Department of Health
- NHI
National Health Insurance
- NMAH
Nelson Mandela Academic Hospital
- PEC
Patient Experience of care
- PSI
Patient Safety Incidents
- RCT
Randomised Control Trial
- RFH
Rob Ferreira Hospital
- SEH
St Elizabeth Hospital
- TH
Themba Hospital
- UHC
Universal Health Coverage
- WHO
World Health Organisation
Authors’ contributions
WWC conceived the research, sourced funding, engaged stakeholders, completed the first draft of the proposal and manuscript, edited versions of the manuscript, and signed off on the final manuscript for submission. ORM facilitated ethics, provided the software that was used for map developing, created the maps for the study sites and research site access approvals. ORM and AN edited and commented on versions of the manuscript and incorporated and addressed feedback from the co-authors. SAM (senior author) undertook statistical analysis, edited versions of the manuscript, and provided methodological strategy. SCN monitored implementation of the protocol, and edited versions of the manuscript. TM, KM, OG, SCN, IF, VE, XN, KM, NS, NK, MaM, ZN, MuM, BM, SS, BS, and GM collected data and edited versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the South African Medical Research Council Grant number: 57035. The SAMRC only provides financial support for the research programme while, the content is solely the responsibility of the authors and does not necessarily represent the official views of the funder.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study forms part of a registered RCT that was approved by the Research Ethics Committee of the University of the Witwatersrand (Ref: M210939) and Walter Sisulu University (Ref: 040/21). Approvals to access the research sites were granted by the Provincial Health Research Committees of the Eastern Cape (EC_202106_019) and Mpumalanga (MP_202106_009). Written informed consent was obtained from study participants. The study was registered as a clinical trial on 19 May 2022 in the South African National Clinical Trial Registry with ref: DOH-27-052022-6854. The URL of trial registry record is: https://sanctr.samrc.ac.za/. To ensure clear, complete, and transparent reporting, this study is written in accordance with the Standard Protocol items: Recommendations for Interventional trials (SPIRIT) 2013 statement. Furthermore, all methods were carried out in accordance with relevant institutional guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors would like to declare that Sikhumbuzo A. Mabunda who is one of the co-authors of this manuscript is an “Associate Editor” of the BMC Health Services Researcher. Otherwise, the authors declare that they have no other competing interests.
Footnotes
For guidance on how to conduct the PEC survey, please refer to the guideline created by the NDoH –National Guideline On Conducting Patient Experience Of Care Survey- is provided below: https://www.idealhealthfacility.org.za/App/Document/Download/58.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Smith MD, Rabbitt MP, Coleman- Jensen A. Who are the world’s food insecure? New evidence from the food and agriculture organization’s food insecurity experience scale. World Dev. 2017;93:402–12. [Google Scholar]
- 2.Asamrew N, Endris AA, Tadesse M. Level of patient satisfaction with inpatient services and its determinants: a study of a specialized hospital in Ethiopia. J Environ Public Health. 2020;2020:2473469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mosadeghrad AM. Healthcare service quality: towards a broad definition. Int J Health Care Qual Assur. 2013;26:203–19. [DOI] [PubMed] [Google Scholar]
- 4.Bahari BM, Yip B, Ling W. Factors contributing to customer satisfaction with community pharmacies in Malaysia. J Public Health (Bangkok). 2010;18:35–41. [Google Scholar]
- 5.South African National Department of Health. National Guideline for Patient Safety Incident Reporting and Learning in the Health Sector of South Africa. 2021. Available from: https://knowledgehub.health.gov.za/system/files/elibdownloads/2022-03/National%20Guideline%20for%20Patient%20Safety%20Incident%20Reporting%20and%20Learning%20in%20South%20Africa%20Version%202_2022.pdf.
- 6.DoH. A policy on quality in health care for South Africa. Department of Health, Republic of South Africa. 2007. p. 1–24.
- 7.South African National Department of Health. Continuous quality improvement. 2022. Available from: https://knowledgehub.health.gov.za/elibrary/continuous-quality-improvement-cqi-teams-improve-south-africas-vmmc-programme.
- 8.National Department of Health. National Guideline on conducting Patient Experience of Care Surveys in Public Health Establishments OCTOBER 2017. Health Policy (New York). 2017; October:1–35.
- 9.Mid Staffordshire NH. Report of the Mid Staffordshire NHS Foundation trust public inquiry. Stationery Office; 2013. Available from: https://assets.publishing.service.gov.uk/media/5a7ba0faed915d13110607c8/0947.pdf.
- 10.Fernandes ÓB, Netshiombo M, Gulácsi L, Klazinga NS, Pentek M, Baji P. Patient experiences in a public primary health care clinic: a South African case study. Soc Econ. 2020;42:333–47. [Google Scholar]
- 11.Internet Citation: What Is Patient Experience?. Content last reviewed October 2024. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html.
- 12.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fan B, Imeokparia F, Ludwig K, Korff L, Hunter-Squires J, Chandrasekaran B, et al. Patient experience ratings: what do breast surgery patients care about? Cureus. 2022;14:e28846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molla M, Sisay W, Andargie Y, Kefale B, Singh P. Patients’ satisfaction with outpatient pharmacy services and associated factors in Debre Tabor comprehensive specialized hospital, Northwest Ethiopia: a cross-sectional study. PLoS ONE. 2022;17(1 January):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Price RA, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, et al. Examining the role of patient experience surveys in measuring health care quality. 2014;71:522–54. 10.1177/1077558714541480. [DOI] [PMC free article] [PubMed]
- 16.Gualandi R, Masella C, Piredda M, Ercoli M, Tartaglini D. What does the patient have to say? Valuing the patient experience to improve the patient journey. BMC Health Serv Res. 2021;21:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stuckler D, Basu S, McKee M. Health care capacity and allocations among South Africa’s provinces: infrastructure-inequality traps after the end of apartheid. Am J Public Health. 2011;101:165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Health ND. of. Government notices • GoewermentskennisGewinGs. 2017.
- 19.Malakoane B, Heunis JC, Chikobvu P, Kigozi NG, Kruger WH. Public health system challenges in the free state, South Africa: a situation appraisal to inform health system strengthening. BMC Health Serv Res. 2020;20:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chitha WW, Mnyaka OR, Hongoro DJ, Swartbooi B, Williams N, Masemola MA et al. Protocol for exploring effective clinical governance strategies in South Africa’s Eastern Cape and Mpumalanga provinces. 2021. 10.21203/rs.3.rs-1041055/v1
- 21.Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res. 2009. 10.1186/1472-6963-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Redda EH, Surujla J. Assessing the level of patient satisfaction on Public Healthcare Facilities in South Africa. Hum Soc Sci Rev. 2020;8:172–81.
- 23.Matsoso MP, Fryatt R. National health insurance: the first 16 months. South Afr Med J. 2013;103:156. [DOI] [PubMed]
- 24.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374:817–34. [DOI] [PubMed] [Google Scholar]
- 25.Setswe G, Muyanga S, Witthuhn J, Nyasulu P. Public awareness and knowledge of the National Health Insurance in South Africa. 2015. 10.11604/pamj.2015.22.19.6131 [DOI] [PMC free article] [PubMed]
- 26.Young M. Private vs. Public Healthcare in South Africa. Honors Theses. 2741. 2016. https://scholarworks.wmich.edu/honors_theses/2741.
- 27.Rattan R, Chambers R, Wakley G. The challenges of quality improvement. Clin Govern Gen Dental Pract. 2019;10440:233–40. [Google Scholar]
- 28.Burger R, Christian C. Access to health care in post-apartheid South Africa: availability, affordability, acceptability. Health Econ Policy Law. 2018;15:43–55. [DOI] [PubMed] [Google Scholar]
- 29.Felix R. Service quality and customer satisfaction in selected banks in Rwanda. J Bus Financial Affairs. 2017;06:1–11. [Google Scholar]
- 30.Xie Z, Or C. Associations between waiting times, service times, and patient satisfaction in an endocrinology outpatient department: a time study and questionnaire survey. Inquiry (United States). 2017;54:46958017739527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Devi YN, Laishram J, Singh TG, Devi HS. Patients ’ satisfaction study in the out-patient departments of the two tertiary government hospitals in Manipur. 2020;19:5–9. [Google Scholar]
- 32.Harrichandparsad A, Mahomed OH. Patient and health system determinants of experiences of care at primary health care clinics in eThekwini, KwaZulu-Natal, 2018. Afr J Prim Health Care Fam Med. 2021;13:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Assembly, 72. Global action on patient safety. World Health Organization. 2019. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R6-en.pdf.
- 34.Gqaleni TM, Bhengu BR. Analysis of patient safety incident reporting system as an indicator of quality nursing in critical care units in Kwazulu-Natal, South Africa. Health SA Gesondheid. 2020;25:0–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Health Professions Council of South Africa. Batho Pele Principles. Communications. 2018;2. Available from: https://www.hpcsa-blogs.co.za/wp-content/uploads/2017/04/2017-IN-Handbook-Annexure-G.pdf.
- 36.South African National Department of Health. The Patients’ Rights Charter Participation in decision-making. 2007:1–3. Available from: http://www.doh.gov.za/docs/legislation/patientsright/chartere.html.
- 37.National Department of Health South Africa. “Towards Quality Care for Patients” National Core Standards for Health Establishments in South Africa. 2011. Available from: http://www.doh.gov.za/docs/legislation/patientsright/chartere.html.
- 38.Mogashoa PM, Pelser GPJ. An analysis of the implementation of the national core standards in public hospitals | Africa Insight. 2014. https://journals.co.za/doi/pdf/10.10520/EJC164279. Accessed 10 Apr 2023.
- 39.Chitha W, Jafta Z, Mnyaka OR, Hongoro D, Godlimpi L, Swartbooi B, et al. Protocol of mixed-methods assessment of demographic, epidemiological and clinical profile of decentralised patients with cancer at Nelson Mandela Academic Hospital and Rob Ferreira Hospital, South Africa. BMJ Open. 2022;12:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Department of Health. National Health Insurance Bill [B 11-2019]. 2019. Available from: https://www.gov.za/sites/default/files/gcis_document/201908/national-health-insurance-bill-b-11-2019.pdf.
- 41.Department Statistics South Africa. StatsSA. (2021) mid-year population estimates. 2021. Available from: https://www.statssa.gov.za/publications/P0302/P03022021.pdf.
- 42.StatsSA. CS_2016_profile_Mpumalanga. 2016. Available from: https://cs2016.statssa.gov.za/wp-content/uploads/2018/11/CS_2016_profile_Mpumalanga.pdf.
- 43.Sukwana A, Mrara B, Oladimeji O. Prevalence and causes of elective surgical cancellations: findings from a rural Tertiary Hospital in the Eastern Cape, South Africa. Healthc (Switzerland). 2023;11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eskandari M, Abbaszadeh A, Borhani F. Barriers of referral system to health care provision in rural societies in Iran. J Caring Sci. 2013;2:229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.South African Human Rights Commission. FINAL access to health care educational booklet. 2019. Available from: https://www.sahrc.org.za/home/21/files/FINAL%20Access%20to%20Health%20Care%20Educational%20Booklet.pdf.
- 46.Chimbindi N, Newell M-L. Patient satisfaction with HIV and TB treatment in a public programme in rural KwaZulu-Natal: evidence from patient-exit interviews. 2014. [DOI] [PMC free article] [PubMed]
- 47.Adeniji AA, Mash B. Patients’ perceptions of the triage system in a primary healthcare facility, Cape Town, South Africa. Afr J Prim Health Care Fam Med. 2016;8:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lazar M, Davenport L. Barriers to health care access for low income families: a review of literature. J Community Health Nurs. 2018;35:28–37. [DOI] [PubMed] [Google Scholar]
- 49.Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: a critical review. Curationis. 2019;42:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Doherty J. Strengthening clinical leadership in hospitals: a review of the international and South African literature. 2013. 10.13140/RG.2.1.1273.0725.
- 51.Obi IE, Ndu AC, Agu KA, Omotowo BI, Agunwa CC, Idoko AC. Patient satisfaction with services at a tertiary hospital in south-east Nigeria. Malawi Med J. 2018;30:270–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rand L, Dunn M, Slade I, Upadhyaya S, Sheehan M. Understanding and using patient experiences as evidence in healthcare priority setting. Cost Eff Resource Allocation. 2019;17:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Entwistle VA, Carter SM, Cribb A, McCaffery K. Supporting patient autonomy: the importance of clinician-patient relationships. J Gen Intern Med. 2010;25:741–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zuma, Sibusiso Memory. The factors affecting availability of medicines in the Free State District Health Services, University of South Africa, Pretoria. 2013. Available from: http://hdl.handle.net/10500/13331.
- 55.Zuma SM. Pharmacist Assistants ’ role in medicine supply management at a primary healthcare setting. 2022:1–7. [DOI] [PMC free article] [PubMed]
- 56.Elfatih Ibrahim Elamin, Izham Mohamed Ibrahim M. Availability of essential medicines in Sudan. Sudan J Public Health. 2010;5:32–7.
- 57.Modisakeng C, Matlala M, Godman B, Meyer JC. Medicine shortages and challenges with the procurement process among public sector hospitals in South Africa; findings and implications. BMC Health Serv Res. 2020;20:1–0. [DOI] [PMC free article] [PubMed]
- 58.Shukar S, Zahoor F, Hayat K, Saeed A. Drug Shortage: Causes, Impact, and Mitigation Strategies. 2021;12:1–18. [DOI] [PMC free article] [PubMed]
- 59.Adebisi YA, Nwogu IB, Alaran AJ, Badmos AO, Bamgboye AO, Rufai BO, et al. Revisiting the issue of access to medicines in Africa: challenges and recommendations. Public Health Chall. 2022;1:e9. [Google Scholar]
- 60.PatientEngagementHIT. Understanding the Power Hierarchy in Patient-Provider Relationships. The Xtelligent Healthcare Media network. 2018. https://patientengagementhit.com/news/understanding-the-power-hierarchy-in-patient-provider-relationships. Accessed 2 June 2023.
- 61.Raveesh BN, Nayak RB, Kumbar SF. Preventing medico-legal issues in clinical practice. Ann Indian Acad Neurol. 2016;19(Suppl 1):S15–S20. 10.4103/0972-2327.192886. [DOI] [PMC free article] [PubMed]
- 62.The Leapfrog Group. Part Two: Adult Inpatient Care. 2022:1–7. Available from: https://www.leapfroggroup.org/sites/default/files/Files/Patient%20Experience%20Report_HCAHPS_Final_5.5.pdf.
- 63.Gandhi T. Patient Safety and Patient Experience in the Ambulatory Setting. 2022:1–1. https://info.pressganey.com/press-ganey-blog-healthcare-experience-insights/safety-and-patient-experience-in-the-ambulatory-setting. Accessed 4 Apr 2023.
- 64.Jha AK, Larizgoitia I, Audera-Lopez C, Prasopa-Plaizier N, Waters H, Bates DW. The global burden of unsafe medical care: Analytic modelling of observational studies. BMJ Qual Saf. 2013;22:809–15. [DOI] [PubMed] [Google Scholar]
- 65.Singh H, Meyer AND, Thomas EJ. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. BMJ Qual Saf. 2014;23:727–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.WHO Fact sheets/Detail/Patient Safety. Patient Safety. 2023. https://www.who.int/news-room/fact-sheets/detail/patient-safety. Accessed 2 June 2023.
- 67.Adhikary G, Shawon SR, Ali W, Ahmed S, Shackelford KA, Woldeab A et al. Factors influencing patient’s satisfaction at Different Levels of Health Facilities in Bangladesh: results from patient exit interviews. PLoS ONE. 2018:1–13. [DOI] [PMC free article] [PubMed]
- 68.Mokgoko MM. Health care users’ experiences and perceptions of waiting time at a diabetes clinic in an academic hospital. 2013. Available from: http://hdl.handle.net10539/14496.
- 69.Nevhutalu HK, Hattingh J. Patients rights in South Africas public health system: Moral-critical perspectives. 2016. [Google Scholar]
- 70.Garba SN, Ibrahim AH. Perception of patients towards nurses ’ attitudes: implication on the Public. Image Nurs. 2021;3:758–64. [Google Scholar]
- 71.South African National Department of Health. Government Notices - National Health Insurance Policy. 2017. Available from: https://www.gov.za/sites/default/files/gcis_document/201707/40955gon627.pdf.
- 72.Liang H, Xue Y, Zhang ZR. Patient satisfaction in China: a national survey of inpatients and outpatients. BMJ Open. 2021;11:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mcintyre D, Ataguba J. Access to quality health care in South Africa: is the health sector contributing to addressing the inequality challenge? Health Econ Policy Law. 2015;9:179–93. [Google Scholar]
- 74.Klitzman R. Patient-time, doctor-time, and institution-time: perceptions and definitions of time among doctors who become patients. Patient Educ Couns. 2007;66:147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kama ZS. An evaluation of access to health care: Gugulethu community health clinic by Zukiswa Shirley Kama Thesis submitted in fulfilment of the requirements for the degree Master of technology : Public Management In the Faculty of Business at the Cape Peninsula. 2017. Available from: http://hdl.handle.net/20.500.11838/2456.
- 76.Mabunda GS. An investigation into waiting time in public health care facilities in the Capricorn district, Limpopo Province (Doctoral dissertation). 2018. Available from: http://ulspace.ul.ac.za/handle/10386/2366.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.