Abstract
Background
Following the latest war in 2023, over nine million people have been internally displaced, of which White Nile State received over 50,000. They lived in different camps and moved to big cities. This study assessed the scope of mental and physical concerns among the IDPs to identify important healthcare needs.
Methods
This is a cross-sectional survey of four localities of internally displaced persons in White Nile state, Sudan. Between December 4th and December 14th, 2023, 800 directly interviewed participants were randomly selected using a face-to-face semi-structured interview. Potential participants were determined using a stratified simple random method.
Results
The findings revealed that 45% of IDPs experienced poor physical health, with prevalent ailments among adults including minor colds (67%), respiratory infections (43%), prolonged flu episodes (36%), insomnia (38%), headaches (42%), gastric upset (44%), nausea (35%), and gastrointestinal issues (40%). Depression, PTSD, and anxiety were prevalent among adults at rates of 18%, 20%, and 14% respectively. Moreover, a staggering 72% of children under five suffered from malnutrition, with males accounting for 44% and females 56%.
Conclusion
Alarming numbers of IDPs in White Nile State face significant physical and mental health problems, warranting urgent interventions from local and international relief agencies.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20972-1.
Keywords: Conflict, Internally displaced persons, Physical health, Mental health, Malnutrition, Health Management, Displacement camps, Sudan
Introduction
Large-scale population displacement often arises from conflicts and natural disasters due to environmental degradation, political persecution, or economic hardships [1]. In contrast to refugees, internally displaced people (IDPs), or those who have been forced to leave their homes but are still inside their country’s borders, face particular difficulties since they are unlikely to receive the same level of aid from international organisations unless their home country specifically requests it [2]. The consequences of violent conflicts, wars, and displacement events are well-documented, leading to complex humanitarian crises with profound impacts on the well-being of affected populations [3]. These impacts manifest both directly, through violence and physical harm, and indirectly, resulting in increased rates of infectious diseases and malnutrition [4]. Sudan, marked by a history of conflict and instability, experienced another wave of violence since the conflict between the Sudanese Armed Forces and the Rapid Support Forces began on April 15, 2023. Sudan currently has the highest number of displaced individuals worldwide. By the end of 2023, 7.6 million people have been internally and externally displaced within and outside of Sudan [5], resulting in many internally displaced individuals seeking refuge in camps and settlements across the nation [6].
According to the Internal Displacement Monitoring Centre (IDMC), Sudan ranked eighth globally in terms of the number of internally displaced people due to conflict and violence in 2020 [7]. About one in every eight IDPs around the world is from Sudan, which represents 13% of all IDPs worldwide.9 The regions in Sudan with the largest percentage of internally displaced people (IDPs) were South Darfur (12%), River Nile (11%), East Darfur (11%), White Nile (8%), Al Jazirah (8%), and North Darfur (8%) [5]. Access to medical care in IDP camps is often limited, leading to preventable deaths and increased morbidity, particularly among women and children [8]. Malnutrition prevails in such settings and significantly elevates the risks of short- and long-term morbidity and mortality [9]. Additionally, conflict-induced displacement increases the risk of mental health disorders, including depression and post-traumatic stress disorder (PTSD), among affected populations [10, 11]. The psychological distress stemming from conflicts may also contribute to the adoption of unhealthy behaviours such as hazardous drinking and smoking, leading to a higher burden of non-communicable diseases [12]. The humanitarian, development, health, and mental health sectors must emphasise the provision of mental health services in conflict and post-conflict situations due to the high and persistent rates of mental disorders in conflict-affected nations [13]. The prevalence of mental health problems among conflict-affected individuals is more than twice that of the general population, and the rates of PTSD and depression vary widely across studies. The variation in prevalence rates can be attributed to methodological factors and differences between conflict-affected IDPs and refugee populations [14]. This is assumed to be due to prolonged displacement, food insecurity, and exposure to traumatic experiences [15]. Stressors such as unemployment, low socioeconomic status, and social isolation can exacerbate pre-existing mental health disorders and raise the chance of acquiring new disorders [16]. According to a meta-analysis of the prevalence of major depressive disorder and PTSD in the adult population of war survivors worldwide, 238 million and 242 million of them, respectively, suffer from these conditions [17]. Psychiatric diagnoses were found in 62.2% of the subjects in another study conducted in South Darfur. With 14.9% of individuals reporting PTSD, depression (13.5%), and comorbid PTSD and depression (8.1% of participants), PTSD was the most frequently reported condition [18]. Armed conflict has an indirect impact on mental health in addition to its direct effects. The loss of houses and other sources of support, the breakdown of social networks, and displacement can all exacerbate feelings of loneliness, hopelessness, and anxiety. These indirect impacts worsen the mental health problems that conflict-affected persons are facing [19]. A study conducted in Uganda among South Sudanese citizens shows the detrimental substantial effects of war-related trauma on mental health [20, 21].
The Sudan armed conflict of 2023 resulted in a substantial number of IDPs in the country. Despite the evident need, comprehensive data on the prevalence of both physical and mental health problems among Sudanese IDPs in White Nile State following the ongoing war are lacking. In order to evaluate and address the health issues facing IDPs, we conducted a cross-sectional study to determine the prevalence of physical and mental health disorders, assess the association between displacement status and mental disorders, and identify the prevalence and associated factors of malnutrition among Sudanese IDPs.
Methods
Sample selection and study setting
Government statistics indicate that there are over 400 IDP camps in the state, with around 50,000 inhabitants in total. Approximately 30% of the camp population is under five years old. The state is made up of eight localities, and a sample of 800 IDPs was selected for this study and has been calculated using a definite population equation as follows:
 |
 |
 |
 |
 |
 |
 |
.
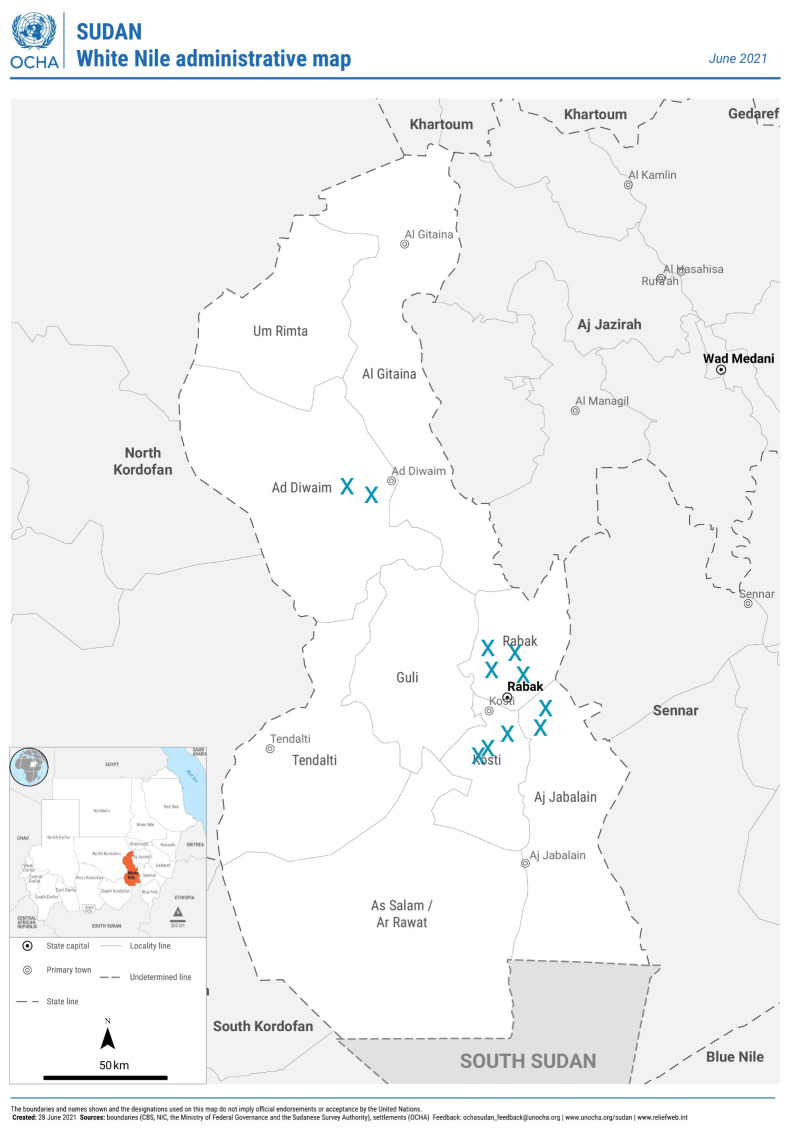
The first calculation predicted a sample size of 397 people. We doubled the number, setting a target of 794 participants to improve accuracy, decrease potential bias, and allow for non-responses, bringing the overall sample size to 800. This distribution was guided by White Nile State’s government data on IDPs. Given that 30% of the IDP population was under five years old, we divided the sample size into two groups: 226 participants under five and 574 people aged five and up. A consistent sample size was necessary due to practical restrictions, even though having a varied sample size estimate for nutrition for children under five would have been preferable. There was enough representation of both groups in the final sample to ensure that the results appropriately represent health concerns across age groups. These participants were from eleven camps located in the four largest localities: Rabak (41%), Kosti (20.5%), Aljabaleen (16.25%), and Aldweem (22.25%). The first two localities contained half of the total camps in the state (Fig. 1).
Fig. 1.
The distribution of the selected IDP camps in White Nile state
Participants
The participants in this study were individuals who had been forcibly displaced from their homes due to violent conflict following events in April 2023. They were residing in officially recognised Internally Displaced Persons (IDP) camps in White Nile State. To participate, individuals needed to be physically and cognitively capable of completing the questionnaire. Additionally, participants had to be at least 10 years old to participate in the physical and mental health questionnaires or under 5 years old to participate in the malnutrition questionnaire. Individuals who had been diagnosed with a mental disorder before April 15th, 2023, were excluded from the study to ensure that the mental health conditions measured were directly associated with displacement-related factors and recent traumatic events rather than long-standing psychiatric conditions. This exclusion principle was intended to determine the effect of recent displacement on mental health.
Stratified random sampling method was used to ensure a representative sample of IDPs across White Nile State. Camps were first stratified by locality and geographical division of localities (Rabak, Kosti, Aljabaleen, and Aldweem). Based on government data and participants, the camps were randomly selected within each locality. A simple random method was used with every fourth tent in the Camp chosen as a potential participant. This approach allowed us to capture a broad cross-section of the IDP population while ensuring logistical feasibility and data reliability. We also noted an extremely high level of interest and cooperation among the camp residents, as IDPs supported the study and could not wait to express their experiences. Such openness to share information with IDPs supported the recruitment and the questionnaire completion process, which subsequently made the data collection proceed smoothly and systematically from those selected. This method enabled us to identify the general perimeter of the IDP population. At the same time, on the operational level, we could carry out the survey without problems and had reliable data. All participants were Muslim and displaced from Khartoum State. Although 226 children under five were evaluated for malnutrition, 574 participants over ten filled out physical and mental health questionnaires. However, given the logistical limitations of the study, the sample size for children under five was deemed sufficient, and it offers crucial preliminary information about the nutritional status and related health issues of young children in the IDP camps in White Nile State.
Ethical approval
was granted by the health research ethical committee of the Ministry of Health, White Nile State, before the onset of the study. Participants were approached in their tents and were required to provide informed consent before participating in the study. Confidentiality of information was guaranteed, and all potential subjects were provided with detailed explanations about the study, its purpose, and their rights as participants. This included the right to confidentiality and the right to withdraw from the study at any time. No names were collected or recorded, and no financial incentives were offered to any participant.
Materials
In 2023, the authors and four trained medical student interviewers conducted a cross-sectional survey to gather data from IDPs. A total of 800 interviews were conducted using a face-to-face semi-structured interview method between December 4th and December 14th, 2023. To ensure confidentiality, the interviews took place in private outdoor spaces in the camps where the respondents lived. Each interview lasted approximately 20 min on average. This method allowed respondents to freely discuss sensitive topics without fear of judgment or influence from group dynamics. Unlike group discussions, individual interviews provided a more private and secure environment for participants to express their thoughts and experiences. This approach aimed to capture a more authentic representation of the participants’ perspectives on various issues related to their displacement. Data were collected digitally in the field using an interview questionnaire, and the data was entered directly via Google Forms by the interviewers themselves. The responses were pooled into a digital database, almost eliminating potential input errors. Moreover, the digital data validation embedded in the form ensured that the correct entries were made.
Participants above 10
IDPs above 10 responded to three sets of questionnaires -back-translated from English into Arabic- to generate diagnoses of physical and mental health disorders among them. The first questionnaire consisted of 6 questions to gather demographic information and details about their displacement history. The second questionnaire utilised was the Physical Health Questionnaire (PHQ), a modified version of Spence et al.’s (1987) measure of health [22]. This scale included 14 items that assessed the frequency of symptoms such as sleep disturbances, headaches, respiratory infections, and gastrointestinal problems. Responses were rated on a 7-point frequency scale, with higher scores indicating better somatic health. The total score ranged from 14 to 82, with a mean score of 38.86 (SD 13.32). Participants scoring below 40 were considered to have poor physical health. The third questionnaire was the MINI (Mini International Neuropsychiatric Interview), developed by a team of psychiatrists and clinicians led by Dr. Sheehan and Dr. Lecrubier [23]. The MINI, which is frequently utilised in clinical and research contexts, has been validated across a variety of demographics, including conflict-affected people, with reliability coefficients more than 0.75 for key modules included in this study (depression, PTSD, and anxiety). This comprehensive method fully assessed physical and emotional disorders among individuals older than 10 in the study population.
Although this study managed to account for a range of confounding factors such as age, gender, and marital status, there might still be other additional potential confounding factors that could affect the observable associations between relocation and health outcomes. Significantly, pre-displacement socioeconomic status, historical trauma exposure, and levels of social support may have an impact on both mental and physical health, regardless of recent displacement. For example, individuals from lower socioeconomic origins may have had weaker baseline health or fewer resources to deal with displacement-related stressors, which could impact their health. Similarly, prior trauma exposure may predispose people to mental health issues, whilst strong social support may operate as a protective factor. Although these variables were not directly measured, future studies should better consider a more comprehensive set of covariates to isolate the specific impacts of displacement on health. Incorporating these additional factors would strengthen the analysis and provide a clearer understanding of the unique health needs of internally displaced persons.
Participants under-five
To collect nutritional data for their children, mother-child pairs were chosen at random from each camp. To obtain a wider range of nutritional data within resource limits, up to two children per mother were included if a home had more than one child under five. Restricting each home to two children helped strike a compromise between the requirement for thorough data and preventing over-representation from any single household. This method enabled us to collect detailed data on each child’s nutritional status while maintaining consistency across households. The mothers provided oral informed consent for their children to participate in the study, which included a clinical examination for signs of malnutrition such as oedema. The presence of oedema was determined by applying pressure to the feet and checking for a shallow imprint that persisted after the pressure was removed.
The primary method for assessing children’s nutrition status under five is a self-administered standardised questionnaire that includes questions about dietary intake, general health, and access to essential services such as sanitation, healthcare, and food security. As far as feasible, caregivers were encouraged to bring in recent clinic documentation, and answers were checked for accuracy. The questionnaire was designed to capture the perceived availability of water, sanitation, healthcare, and food, and so was intrinsically self-reported in the IDP setting. Malnutrition in the children under study was discovered and classified using the GLIM (Global Leadership Initiative on Malnutrition) criteria [24]. According to those criteria, a malnutrition diagnosis is established through one phenotypic criterion (such as weight-for-age or muscle wasting) and one etiologic criterion (such as nutritional intake or overall health condition). This method offers a trustworthy framework for evaluating malnutrition in environments with limited resources, such as IDP camps. In this study, the assessment of malnutrition considered factors such as nutritional intake, muscle wasting, oedema, weight-for-height, and weight-for-age. Muscle wasting implies malnutrition and was detected during a physical examination. Oedema is indicative of severe malnutrition and protein deficit. Dietary intake is critical since insufficient consumption can lead to nutritional deficiencies. General health status encompasses medical history and physical well-being, influencing nutritional status. These indicators allowed for a more comprehensive assessment of malnutrition risk factors among the children investigated.
This study used the Statistical Package for Social Sciences (SPSS26) to analyse the collected quantitative data. Descriptive statistics, such as frequencies and percentages, were calculated for all variables in the questionnaire. Chi-squared tests were then employed to explore the relationships between various factors, including physical and mental illnesses, health problems and displacement status, malnutrition, and environmental factors. A statistical significance level of p < 0.05 was used to determine the significance of these associations. Furthermore, Odds ratios and risk estimates were used to analyze the links and comorbidities of mental health problems, specifically depression, anxiety, and PTSD. By this method we were able to assess the risk that patients with one mental condition (e.g., depression) would also display symptoms of another disorder (e.g., anxiety or PTSD). Odds ratios gives information about the intensity and direction of these associations, whereas risk estimates let us calculate the likelihood of co-occurrence among the illnesses in our sample population. This method allowed us to investigate the potential impact of these mental health conditions on individuals within our study population.
Results
Participants above 10
Of the 574 participants above ten who completed physical and mental health questionnaires, male participants comprised 30% of the sample, while female participants comprised 70%. Among these participants, approximately 48.6% were married, 45.5% were single, 1.4% were divorced, and 4.5% were widowed. Additionally, 226 participants under five completed a malnutrition questionnaire, with male participants representing 45.5% of the sample and female participants representing 54.5% (Table 1).
Table 1.
Socio-demographic characteristics of internally displaced persons in White Nile state, Sudan
| Characteristics | N | % |
|---|---|---|
| Age (years) | ||
| 11–18 | 179 | 31 |
| 19–35 | 199 | 35 |
| > 35 | 196 | 34 |
| Gender | ||
| Male | 172 | 30 |
| Female | 402 | 70 |
| Employment status | ||
| Full-time | 30 | 5 |
| Part-time | 35 | 6 |
| Unemployed | 325 | 57 |
| Self-employed | 31 | 5 |
| Student | 153 | 27 |
| Displacement period (months) | ||
| < 1 | 13 | 2 |
| 1–3 | 55 | 10 |
| 4–6 | 173 | 30 |
| > 6 | 333 | 58 |
| Marital status | ||
| single | 261 | 46 |
| married | 279 | 49 |
| divorced | 8 | 1 |
| widowed | 26 | 4 |
| Educational level | ||
| Non-formal | 63 | 11 |
| primary | 210 | 37 |
| secondary | 174 | 30 |
| Vocational training | 6 | 1 |
| university or higher | 121 | 21 |
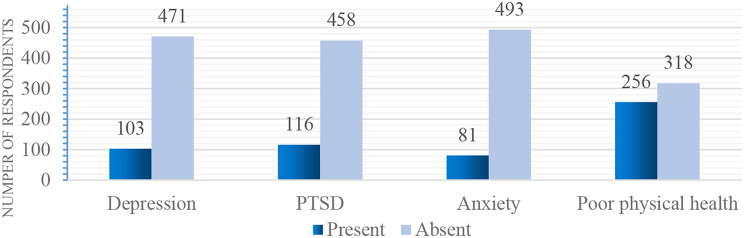
When using a cut-off point of 40 in the physical health questionnaire, our study found that 45% of internally displaced persons (IDPs) were classified as having poor physical health. The most prevalent physical health issues among adults included minor colds (67%), respiratory infections (43%), long-lasting colds or flu (36%), insomnia and disturbed sleep (38%), headaches (42%), upset stomach (44%), nausea (35%), and diarrhoea or constipation (40%). Additionally, the reported cases of depression, PTSD, and anxiety among the participants was 18%, 20%, and 14%, respectively (Fig. 2). These findings suggest that IDPs are experiencing a high burden of both physical and mental health issues, highlighting the importance of providing comprehensive healthcare services to this vulnerable population.
Fig. 2.
Distribution of depression, anxiety, PTSD and poor physical health among Internally displaced people in White Nile State
Regarding age distribution, the respondents in our study were almost equally divided among three age categories: 31% were aged 11–18 years, 35% were aged 19–35 years, and 34% were above 35 years old (Table 1). To investigate the relationship between age and physical and mental health problems among internally displaced persons (IDPs), we conducted Chi-square tests. (Tables 2 and 3) show a significant association between age and poor physical health as well as (PTSD) with a chi-square value of 12.779, df (2) and a P value of 0.002; 9.229, df (2) and a P value of 0.010, respectively. This indicates a statistically significant relationship between age and poor physical health and PTSD, at a significance level of p < 0.05. However, we found that age was insignificantly associated with depression and anxiety among the IDPs (Table 4) and (Table 5).
Table 2.
The association between demographic factors and physical health status among internally displaced persons in White Nile State, Sudan
| Poor physical health | Chi-square | P-value | |||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Age (years) | 11–18 | 118 (66%) | 61 (34%) | 12.779 | 0.002 |
| 19–35 | 106 (53%) | 93 (47%) | |||
| > 35 | 94 (48%) | 102 (52%) | |||
| Gender | Male | 124 (72%) | 48 (28%) | 27.695 | 0.000 |
| Female | 194 (48%) | 208 (52%) | |||
| Employment status | Full-time | 17 (57%) | 13 (43%) | 19.853 | 0.001 |
| Part-time | 14 (40%) | 21 (60%) | |||
| Unemployed | 162 (50%) | 163 (50%) | |||
| Self-employed | 19 (61%) | 12 (39%) | |||
| Student | 106 (69%) | 47 (31%) | |||
| Displacement period (months) | < 1 | 9 (69%) | 4 (31%) | 5.924 | 0.0115 |
| 1–3 | 35 (64%) | 20 (36%) | |||
| 4–6 | 103 (60%) | 70 (40%) | |||
| > 6 |
171 (51%) |
162 (49%) | |||
| Total | 318 (55%) |
256 (45%) |
|||
*p < 0.05, Pearson Chi-Square test
Table 3.
The association between demographic factors and PTSD among internally displaced persons in White Nile state, Sudan
| PTSD | Chi-square | P-value | |||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Age (years) | 11–18 | 154 (91%) | 25 (9%) | 9.229 | 0.010 |
| 19–35 | 160 (80%) | 39 (20%) | |||
| > 35 | 144 (73%) | 52 (27%) | |||
| Gender | Male | 153 (89%) | 19 (11%) | 12.786 | 0.000 |
| Female | 305 (76%) | 97 (24%) | |||
| Employment status | Full-time | 22 (73%) | 8 (27%) | 10.552 | 0.032 |
| Part-time | 30 (86%) | 5 (14%) | |||
| Unemployed | 254 (78%) | 71 (22%) | |||
| Self-employed | 20 (65%) | 11 (35%) | |||
| Student | 132 (86%) | 21 (14%) | |||
| Displacement period (months) | < 1 | 11(85%) | 2 (15%) | 0.721 | 0.868 |
| 1–3 | 45 (82%) | 10 (18%) | |||
| 4–6 | 140 (81%) | 33 (19%) | |||
| > 6 | 262 (79%) | 71 (21%) | |||
| Total | 458 (80%) | 116 (20%) | |||
*p < 0.05, Pearson Chi-Square test
Table 4.
The association between demographic factors and depression among internally displaced persons in White Nile state, Sudan
| Depression | Chi-square | P-value | |||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Age (years) | 11–18 | 152 (85%) | 27 (15%) | 1.480 | 0.477 |
| 19–35 | 160 (80%) | 39 (20%) | |||
| > 35 | 159 (80%) | 37 (20%) | |||
| Gender | Male | 145 (66%) | 76 (34%) | 0.842 | 0.359 |
| Female | 326 (92%) | 27 (8%) | |||
| Employment status | Full-time | 23 (76%) | 7 (24%) | 19.853 | 0.001 |
| Part-time | 24 (69%) | 11 (31%) | |||
| Unemployed | 268 (82%) | 57 (18%) | |||
| Self-employed | 19 (61%) | 12 (39%) | |||
| Student | 137 (90%) | 16 (10%) | |||
| Displacement period (months) | < 1 | 12 (92%) | 1 (8%) | 1.498 | 0.683 |
| 1–3 | 47 (85%) | 8 (15%) | |||
| 4–6 | 141 (82%) | 32 (18%) | |||
| > 6 | 271 (81%) | 62 (19%) | |||
| Total | 471 (82%) | 103 (18%) | |||
*p < 0.05, Pearson Chi-Square test
Table 5.
The association between demographic factors and anxiety among internally displaced persons in White Nile state, Sudan
| Anxiety | Chi-square | P-value | |||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Age (years) | 11–18 | 158 (88%) | 21 (12%) | 2.709 | 0.258 |
| 19–35 | 173 (87%) | 26 (13%) | |||
| > 35 | 162 (83%) | 34 (17%) | |||
| Gender | Male | 157 (91%) | 15 (9%) | 5.888 | 0.015 |
| Female | 336 (84%) | 66 (16%) | |||
| Employment status | Full-time | 26 (87%) | 4 (13%) | 10.777 | 0.029 |
| Part-time | 27 (77%) | 8 (23%) | |||
| Unemployed | 274 (84%) | 51 (16%) | |||
| Self-employed | 24 (77%) | 7 (23%) | |||
| Student | 142 (93%) | 11 (7%) | |||
| Displacement period (months) | < 1 | 12 (92%) | 1 (8%) | 1.827 | 0.609 |
| 1–3 | 50 (91%) | 5 (9%) | |||
| 4–6 | 148 (86%) | 25 (14%) | |||
| > 6 | 283 (85%) | 50 (15%) | |||
| Total | 493 (86%) | 81(14%) | |||
*p < 0.05, Pearson Chi-Square test
In terms of educational level, our study found that 11% of respondents had not attended any formal education, while 36.6%, 30.6%, 21.1%, and 1% had education levels of primary, secondary, above educational status, and vocational training, respectively. Upon conducting chi-square tests, the results indicated an insignificant association between educational level and poor physical health, depression, anxiety, and PTSD among the internally displaced persons (IDPs) studied.
We found that male participants accounted for 30% of the sample, while female participants made up 70% of the total participants. The chi-square test results revealed a significant relationship between gender and anxiety, as well as gender and poor physical health, with chi-square values of 27.695, df (1) and P value 0.000; 5.888, df (1) and P value.015, respectively which is significant at P < 0.05. However, we did not find statistically significant differences between gender and depression or PTSD in this population (p > 0.05).
In our study on marital status among IDPs, we found that 48.6% of participants were married, 45.5% were single, 1.4% were divorced, and 4.5% were widowed. Upon conducting statistical analysis using Pearson’s chi-square tests, we discovered a direct relationship between being married and experiencing poor physical health and PTSD among the IDPs. Specifically, the results indicated significant associations between marital status and poor physical health and PTSD, with Pearson’s chi-square value of 12.779, df (2) and P value 0.002; 9.229, df (2) and P value 0.010, respectively, which is significant at P < 0.05. However, we did not observe statistically significant associations between marital status and depression or anxiety in this population.
In our study examining the relationship between displacement period and mental health outcomes among IDPs, we found that the majority of participants, 58%, had been displaced for more than 6 months. A smaller proportion of participants were displaced for 4–6 months (30.1%), 1–3 months (9.6%), and less than one month (2.3%). Interestingly, even though around two-thirds of IDPs experiencing depression, PTSD, anxiety, and poor physical health had been displaced for more than 6 months, our analysis did not detect a statistically significant difference in these health outcomes based on the duration of displacement.
In our investigation into the relationship between employment status and the mental and physical well-being of IDPs, we found that the majority of participants (56%) were unemployed. There were also smaller proportions of participants who were students (26.7%), self-employed (5.4%), part-time employees (6.1%), and full-time employees (5.2%). We observed a direct relationship between employment status and poor physical health, depression, PTSD, and anxiety, as indicated by Pearson’s chi-square values. The results showed significant relationships with Pearson’s chi-square values of 19.803, df (4) and P value 0.001; 19.853, df (4) and P value 0.001; 10.552, df (4) and P value 0.032; 10.777, df (4) and P value 0.029, respectively which is significant at P < 0.05.
(Table 6) shows the co-existence between physical and mental health problems and the Chi-Square test results indicated a significant direct association between depression, PTSD, anxiety with poor physical health. The chi-square values for depression, PTSD, and anxiety were 12.355, 42.742, and 51.921 respectively, all with a P value of 0.000 which is considered statistically significant at P < 0.05. Furthermore, the odds ratios between depression and anxiety, depression and PTSD, as well as between PTSD and anxiety were calculated to be (OR = 0.513, 95% CI: 0.349–0.753), (OR = 0.492, 95% CI: 0.346–0.701), and 6(OR = 0.235, 95% CI: 0.160–0.346) respectively (Table 7).
Table 6.
Exploring the co-existence of physical and mental health problems among internally displaced persons in White Nile state, Sudan
| Disorders | Depression | Anxiety | PTSD | ||||
|---|---|---|---|---|---|---|---|
| Absent | Present | Absent | Present | Absent | Present | ||
| Physical Health | Good | 277 (87%) | 41 (13%) | 303 (61%) | 190 (39%) | 285 (90%) | 33 (10%) |
| Poor | 194 (76%) | 62 (24%) | 190 (74%) | 66 (26%) | 173 (68%) | 83 (32%) | |
| Depression | Absent | ------ | 415 (84%) | 78 (16%) | 390 (85%) | 68 (15%) | |
| Present | 56 (69%) | 25 (31%) | 81 (70%) | 35 (30%) | |||
| Anxiety | Absent | ------ | ------ | 419 (91%) | 39 (9%) | ||
| Present | 74 (64%) | 42 (36%) | |||||
Table 7.
Risk of depression and anxiety following PTSD among internally displaced persons in White Nile state, Sudan
| Disorders | Odds ratio | Upper value | Lower value | P- value |
|---|---|---|---|---|
| Depression | 0.492 | 0.701 | 0.346 | 0.000 |
| Anxiety | 0.235 | 0.346 | 0.160 | 0.000 |
*p < 0.05, Pearson Chi-Square test
The gender distribution among children under five was roughly equal (Table 8), with a male-to-female ratio of nearly 1:1. Three-quarters were not breastfed, indicating a marginally significant relationship with health outcomes (Chi-square = 3.699, p = 0.054). Food insecurity was widespread and substantially linked with health status (Chi-square = 20.056, p = 0.000), and over half did not have access to healthcare, which was also significant (Chi-square = 6.833, p = 0.009). Over one-third reported poor water and sanitation conditions, while no significant connection was found (Chi-square = 4.183, p = 0.242). Approximately half of the children indicated low socioeconomic position, indicating a considerable connection (Chi-square = 14.038, p = 0.003) (Table 9).
Table 8.
Health-related factors among children under five in IDP camps: a sociodemographic overview
| Characteristics | N | % |
|---|---|---|
| Gender | ||
| Male | 101 | 46 |
| Female | 121 | 54 |
| Breastfeeding | ||
| Yes | 63 | 28 |
| No | 163 | 72 |
| Food Security | ||
| very insecure | 13 | 6 |
| Insecure | 89 | 39 |
| Moderately insecure | 113 | 50 |
| Secure | 11 | 5 |
| Access to Healthcare | ||
| Yes | 116 | 51 |
| NO | 110 | 49 |
| Water and Sanitation | ||
| Very poor | 7 | 3 |
| poor | 76 | 33 |
| Faire | 137 | 61 |
| Excellent | 6 | 3 |
| Socioeconomic Status | ||
| Very poor | 12 | 5 |
| Poor | 91 | 40 |
| Average | 117 | 52 |
| Good | 6 | 3 |
*p < 0.05, Pearson Chi-Square test
Table 9.
Association between socioeconomic and environmental factors and malnutrition in children under five
| Malnutrition | Chi-square | P-value | |||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Gender | Male | 31(30%) | 72(70%) | 0.314 | 0.575 |
| Female | 33(27%) | 90(73%) | |||
| Breastfeeding | Yes | 52(32%) | 111(68%) | 3.699 | 0.054 |
| No | 12(19%) | 51(81%) | |||
| Food Security | very insecure | 8(62%) | 5(38%) | 20.056 | 0.000 |
| Insecure | 34(38%) | 55(62%) | |||
| Moderately insecure | 22(19%) | 91(81%) | |||
| Secure | 0(0%) | 11(100%) | |||
| Access to Healthcare | Yes | 40(36%) | 70(64%) | 6.833 | 0.009 |
| NO | 24(21%) | 92(79%) | |||
| Clinical Signs | Yes | 39(23%) | 134(77%) | 12.121 | 0.000 |
| NO | 25(47%) | 28(53%) | |||
| Water and Sanitation | Very poor | 4(57%) | 3(43%) | 4.183 | 0.242 |
| poor | 24(32%) | 52(68%) | |||
| Faire | 35(26%) | 102(74%) | |||
| Excellent | 1(16%) | 5(84%) | |||
| Socioeconomic Status | Very poor | 7(58%) | 5(42%) | 14.038 | 0.003 |
| Poor | 33(36%) | 58(64%) | |||
| Average | 24(21%) | 93(79%) | |||
| Good | 0(0%) | 6(100%) | |||
| Total | 64 (28%) | 162 (72%) | |||
*p < 0.05, Pearson Chi-Square test
Etiologic and phenotypic criteria for malnutrition revealed substantial needs: 45 participants had poor general health, and 153 had a low diet. Muscle wasting (16 participants), low weight-for-height (41 participants), and low weight-for-age (121 participants) were all phenotypic indicators of substantial malnutrition in the group (Fig. 3). These findings underscore young children’s critical dietary and health needs in displacement camps.
Fig. 3.
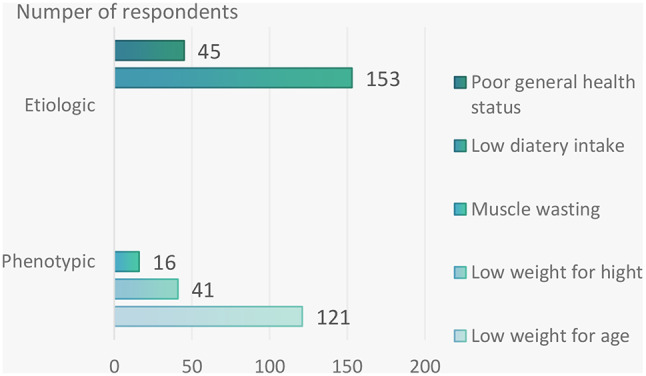
Comparison of etiologic vs. phenotypic malnutrition criteria in children under five
Discussion
Given the rising numbers of internally displaced persons (IDPs) in Sudan and their heightened susceptibility to a range of infectious and chronic diseases, it is crucial to thoroughly document the prevalence of various health issues within these communities. This study represents a pioneering effort in examining the physical and mental health challenges faced by IDPs residing in camps in Sudan. The findings of our study shed light on the intricate relationship between the displacement experience and the health outcomes of IDPs in our study area. Our investigation reveals a concerning prevalence of new cases of both physical and mental health issues among this vulnerable population. Although there have been no recent outbreaks of communicable diseases in the State, we found that a substantial proportion of IDPs exhibited signs of poor physical well-being, with 45% meeting the criteria for classifying poor physical health symptoms. These issues have far-reaching socioeconomic implications for displaced individuals, impacting their health, mental well-being, and ability to reintegrate into society. Among adults’ most commonly reported physical health issues were minor colds, respiratory infections, prolonged cold or flu symptoms, insomnia, headache, upset stomach, nausea, and diarrhoea or constipation. These findings underscore the multifaceted challenges faced by IDPs, ranging from infectious diseases to sleep disturbances and gastrointestinal problems.
Furthermore, our study underscores the rate of mental health concerns among IDPs. We found that depression impacted 18% of respondents, indicating a substantial burden of depressive symptoms within the population. Additionally, post-traumatic stress disorder (PTSD) and anxiety were reported by 20% and 14% of individuals, respectively. These findings underscore the significant psychological distress experienced by IDPs, likely stemming from the trauma of displacement, loss of home and community, and exposure to ongoing stressors. The observed rate of PTSD among IDPs in Sudan, at 20%, is notably higher compared to rates found in similar studies involving Guatemalan refugees (11.2%) and Bosnian refugees (5.6%) [25]. Additionally, the challenging living conditions within the camps, coupled with high rates of unemployment among the IDPs, likely contributed to the elevated prevalence of PTSD. These results echo previous research findings [26], emphasising the profound impact of conflict-related trauma on the mental health of displaced populations.
Our analysis delved into age distribution among IDPs, revealing intriguing trends across various age groups. Notably, respondents were relatively evenly spread among three age brackets: 11–18 years, 19–35 years, and above 35 years. We found that older age cohorts exhibited a higher propensity to report poor physical health and PTSD compared to their younger counterparts. This observed link suggests that older individuals may encounter challenges in adapting to the new social dynamics brought about by displacement. Older IDPs may struggle to re-establish their social status and roles in their previous communities, where responsibilities were clearly defined. This difficulty in adjusting to a changed social environment could contribute to the heightened somatic symptoms and PTSD experienced by older IDPs.
Interestingly, our findings did not show any gender differences in depression and PTSD among IDPs. This lack of distinction may be because both men and women in our study were equally susceptible to mental health issues, given the traumatic experiences they had endured. However, previous research suggested that female participants in their study were more vulnerable to developing PTSD due to experiences such as rape, violent loss of family members, and widowhood [27].
To a certain degree, we anticipated similar rates of anxiety in females compared to males based on the relatively similar rates of depression and PTSD between genders. However, our findings revealed that females reported higher levels of anxiety than expected. This suggests that women may be at a heightened risk for developing anxiety disorders, potentially due to a lower threshold for anxiety in females compared to males. This disparity in anxiety levels could be influenced by factors such as the targeted nature of violence against women, specifically in cases of sexual assault. Conversely, the lack of statistically significant differences in depression and PTSD between genders suggests that the manifestation of these conditions may not be solely determined by gender among IDPs. This underscores the complexity of mental health dynamics within displaced communities and calls for comprehensive assessments that consider multifaceted determinants beyond gender alone.
The significant gender imbalance in the sample, with females comprising 70% of participants compared to 30% of males, reflects the demographic composition of the camps, where women and children constitute a larger proportion of displaced populations. However, this imbalance was due to the role of men as the breadwinners and maybe participants in outdoor activities who did not stay in the camps. Yet, previous research suggests that women are more vulnerable to displacement-related psychological distress due to higher exposure to specific risks, including gender-based violence and caregiving responsibilities. As such, our findings may overrepresent the prevalence of certain health issues, such as anxiety and PTSD. Future studies with balanced gender representation are necessary to assess the full spectrum of health outcomes among displaced individuals. We carried out multi-regression to gauge the effects of covariates and risk factors in the primary outcome.
The study underscores a notable association between unemployment and adverse health outcomes among IDPs. We found that a significant proportion of IDPs were unemployed, and this status was linked to higher rates of depression, PTSD, anxiety, and poor physical health. Addressing employment challenges within displaced populations may, therefore, be crucial in mitigating the burden of mental and physical health issues in such contexts. These findings suggest a significant impact of employment status on the health outcomes of individuals living in camps and heightened vulnerability among the unemployed populace to mental health disorders and physical health issues compared to their employed counterparts.
Although a majority of participants experienced displacement for more than six months, no statistically significant correlation was found between the duration of displacement and the rate of depression, PTSD, anxiety, or poor physical health- contrary to common beliefs and previous research findings [28]. This implies that factors beyond displacement duration may exert greater influence on IDPs’ mental and physical well-being. This unexpected result underscores the complexity of factors influencing health outcomes beyond just the length of displacement. It challenges the notion that longer displacement periods directly correlate with poorer health outcomes. This can reflect the resilience techniques IDPs employ to cope with protracted hardship. IDPs actively develop resilience through social support networks, community structures, and health management — even in cases of prolonged migration. Regardless of the duration of displacement, these adaptive methods may act as a buffer against the anticipated decline in mental health, indicating that resilience may be essential to IDPs’ psychological well-being [29]. It is possible that other factors, such as the quality of living conditions, access to healthcare, and social support networks, may play a more influential role in determining the mental and physical well-being of displaced individuals. Further research could explore these non-temporal factors to better understand the complexities of the relationship between displacement period and health outcomes in IDP populations.
Furthermore, our study contributes valuable insights into the nexus between educational attainment and health outcomes among IDPs. While a substantial proportion of participants had only completed primary education, with a smaller segment having no formal education background, we found no significant correlation between educational level and physical and mental health status. These results suggest that factors beyond education might wield greater influence over mental health outcomes in this vulnerable population.
The discrepancy in the levels of PTSD and somatic symptoms between married and single IDPs contradicts findings from previous research that show single individuals tend to experience higher levels of psychological distress [30]. Our study reveals a higher occurrence of PTSD and somatic symptoms among married IDPs. This unexpected result may be attributed to the unique challenges faced by married IDPs, who often bear the responsibility of protecting their families amid threats and dangers. The additional pressure on married individuals to ensure the safety and well-being of their loved ones, coupled with difficulties in forming new social networks, could contribute to their heightened levels of distress. While marriage is typically considered a protective factor against psychiatric issues in normal circumstances, the demands of conflict situations or natural disasters may reverse this trend, placing greater burdens on married IDPs [26]. These findings suggest that the context in which individuals live plays a crucial role in determining the impact of marital status on mental health outcomes, highlighting the complex interplay between personal relationships and environmental stressors. Our findings revealed an unexpected link between marital status and mental health, with married persons reporting greater rates of PTSD and somatic symptoms than single participants. A potential reason is that married people may feel more stressed because they have responsibilities to protect and provide for their families in stressful camp conditions. Furthermore, the disruption of typical family structures and societal duties may cause significant psychological suffering in married IDPs. These findings are consistent with conflict studies highlighting the special constraints married people encounter in displacement situations.
Our study did reveal a strong association between depression, PTSD, and anxiety among IDPs, The odds ratio between depression and anxiety (OR = 0.513, 95% CI: 0.349–0.753) implies a high likelihood of co-occurrence, and may suggest that these two conditions overlap in conflict-affected populations. The risk estimates between depression and PTSD (OR = 0.492, 95% CI: 0.346–0.701) indicates a high likelihood of co-occurrence, highlighting the emotional and psychological load associated with trauma and displacement. The decreased odds ratio found between PTSD and anxiety (OR = 0.235, 95% CI: 0.160–0.346) suggests that PTSD and anxiety can coexist, but they may have different triggers or manifestations. PTSD is frequently associated with specific trauma-related symptoms, whereas anxiety may indicate a broader response to displacement stressors. This interconnectedness highlights the complex relationship between these mental health disorders in displaced populations.
Turning to the findings concerning children under five, malnutrition emerged as this demographic’s predominant physical health issue. The disparities observed in malnutrition rates underscore the multifaceted nature of the problem, with factors such as access to healthcare, food security, and socioeconomic status playing pivotal roles. Notably, the absence of a significant disparity in malnutrition rates between boys and girls in this age group highlights the universal impact of malnutrition across genders.
The data show that children under the age of five in displacement camps have considerable health and nutritional issues, indicating their vulnerability. Despite gender equality, a sizable proportion lacked breastfeeding, food security, and access to healthcare, with statistically significant connections shown for food security and healthcare access. These inadequacies underscore the additional hazards that IDP children face, as insufficient resources directly affect their physical health.
Malnutrition has emerged as a major concern, with a significant proportion of children fitting both causal and phenotypic criteria. Poor general health and a low nutritional intake were frequently recorded, whereas phenotypic signs such as low weight-for-height and weight-for-age indicated significant growth deficits. The existence of muscle wasting and these nutritional indicators reflect the severe living conditions in IDP camps, where inadequate nutrition and healthcare pose long-term dangers to physical and cognitive development.
Our research findings indicate a concerning trend, showing that out of every ten children surveyed, seven were found to have malnutrition. This represents a significant increase in the prevalence of malnutrition compared to previous studies. Despite the potential availability of food, several factors may explain these troubling results, including elevated food prices that exceed normal levels. Research conducted among suddenness refugees has demonstrated a concerning association between the prevalence of communicable diseases such as malaria, diarrhoea, and pneumonia and an increased risk of malnutrition [31, 32]. Malnutrition remains a significant public health issue in Africa, with alarming statistics indicating that 38.6% of children under five years old are stunted, 28.4% are underweight, and 7.2% are wasted [33]. Globally, the prevalence rates of stunting, underweight, and wasting are estimated at 39.1%, 22.8%, and 4.1%, respectively [34]. These findings underscore the urgent need for targeted interventions to address malnutrition among vulnerable populations, particularly in regions affected by conflict and displacement. These children are particularly susceptible to malnutrition, making them a key target for interventions to improve overall nutritional status and health outcomes in these communities. The prevalence of malnutrition in young children can serve as an important indicator of the general population’s nutritional status, providing valuable data for health education and treatment initiatives. Addressing the underlying factors contributing to malnutrition, such as inadequate food aid and poor access to essential nutrients, is crucial for improving the health and well-being of refugees and displaced populations, particularly children who are most at risk.
Malnutrition in IDPs can lead to significant adverse effects on both their physical and mental health. Physically, malnutrition can result in nutritional deficiencies, gastrointestinal problems, weakness, and fatigue. Mentally, it can cause cognitive impairment, emotional distress, and social isolation. Nutritional status serves as a critical public health indicator for refugees and displaced populations, as it is closely linked to the risk of short-term mortality. A combination of dietary and environmental factors influences the complex causes of malnutrition in these vulnerable groups. Research focusing on IDPs has highlighted ongoing issues of under-nutrition, characterised by inadequate intake of both macro and micro-nutrients. While definitive causation has not been established, there is a strong likelihood that the insufficient food aid supplies provided during this period have contributed to the high rates of malnutrition, poor health outcomes, and increased mortality among displaced populations.
The study emphasises the urgent need for targeted health interventions for internally displaced persons in Sudan, highlighting the importance of addressing social determinants of health, providing gender-sensitive approaches, and improving access to mental health services. Recommendations include tailored interventions to mitigate anxiety and promote physical well-being among female IDPs, improving access to affordable and nutritious food and healthcare services for children, implementing psycho-social interventions, establishing mental health clinics in camps, increasing financing for healthcare programs, training more healthcare workers, improving accessibility to healthcare facilities, encouraging breastfeeding and maternal nutrition, and continuously monitoring mortality and malnutrition. Collaborative efforts from various stakeholders are essential in providing adequate care for IDPs. Prioritising the physical health of IDPs is crucial for promoting their long-term health outcomes and successful integration into society. Addressing malnutrition comprehensively can enhance the resilience and recovery of displaced populations. Tailored interventions for diverse healthcare needs within different age groups and genders among displaced populations are necessary to address mental and physical health needs, create employment opportunities, and improve the nutritional status of young children.
Limitation
This study has several limitations. First, its cross-sectional design limits the generalizability of findings to other regions of Sudan and prevents the assessment of causal relationships. Second, the study’s focus on mental health and exclusion of physical health assessments narrows its scope. Third, social desirability bias, where participants may overreport symptoms to receive aid, is a potential concern despite efforts to reduce it. Fourth, the significant gender imbalance in the sample reflects the demographic composition of the camps, with 70% of female participants making findings, particularly mental health, are women-related disorders. Fifth, while the study controlled for certain variables, unmeasured factors like pre-displacement socioeconomic status, trauma exposure, and social support could still influence the results. Sixth, the reliance on caregiver-reported data for under-five malnutrition, while practical in the field, limits the precision of the findings. Finally, excluding individuals with pre-existing mental health conditions while focusing on the specific impacts of recent trauma may have resulted in conservative estimates of mental health prevalence. Overall, these limitations emphasise the need for a more comprehensive approach to understanding the complex health needs of conflict-affected populations.
Conclusion
In conclusion, our study highlights the significant impact of internal displacement on the health of internally displaced people (IDPs) in Sudan, particularly in White Nile State. The high prevalence of mental illnesses, poor physical health, and malnutrition in IDP camps underscores the urgent need for comprehensive healthcare services, psycho-social support programs, and improvements to living conditions. Addressing these issues is crucial for the well-being of individual IDPs and public health in Sudan as a whole. Recommendations include increased funding for healthcare services, implementation of psycho-social support programs, improvements to living conditions in IDP camps, collaboration between government agencies and organisations, and redistributing displaced individuals to reduce crowding. Future research should continue to explore the relationships between displacement and health disparities through longitudinal studies, gender-specific studies, and resilience research to promote better health outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are grateful to A&A Research Consultations for providing analysis services and reviewing the manuscript. We are especially thankful to Altahir, Abubakar, Majda, and Hibat, who assisted in data collection. We appreciate the support provided during the study by the White Nile State Ministry of Health. We thank the leaders of the IDP camps for helping the research team. We gratefully acknowledge the cooperation and involvement of the IDP camp residents and the parents of the children in the study. Lastly, we would like to express our gratitude to Kenana Sugar Company for providing funding for this research.
Author contributions
A.M.A.A. interpreted the data and wrote the first manuscript. A.M.A.A., O.A.M.A., S.E.M.S., S.H.I.H., N.E.M.A., H.M.A.A., A.A.M.A., H.A.M.A., A.I.A., M.E.E.Y., F.E.A.A., O.A.O.A., S.B.M.A., S.A.A.E., contributed to the literature review, data collection, and editing of the manuscript and approved the final manuscript. A.H.O. contributed to editing the questionnaires and the manuscript.
Funding
Funded by Kenana Sugar Company.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
According to the Declaration of Helsinki, ethical approval was granted by the health research ethical committee of the Ministry of Health, White Nile State, before the onset of the study. Participants were approached in tents and required to provide informed consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferris EG. The politics of Protection: the limits of Humanitarian Action. Brookings Institution; 2018.
- 2.IDMC. Global Report on Internal Displacement; 2020.
- 3.Rubenstein LS. Humanitarianism and Social movements: lessons from the Global South. University of California Press; 2018.
- 4.Toole MJ, Waldman RJ. Refugees and displaced persons: war, hunger, and public health. JAMA. 1990;263(24):3286–8. [PubMed] [Google Scholar]
- 5.ReliefWeb. Sudan humanitarian update (21 January 2024) [EN/AR] - Sudan. https://reliefweb.int/report/sudan/sudan-humanitarian-update-21-january-2024-enar. Accessed January 27, 2024.
- 6.Smith J. Conflict dynamics in Sudan: a comprehensive analysis. J Confl Stud. 2021;25(2):45–67. [Google Scholar]
- 7.IDMC. Global Report on Internal Displacement; 2023.
- 8.Sphere Project. The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response; 2018.
- 9.UNICEF. The State of the World’s Children 2019; 2019.
- 10.Mollica RF, et al. The Harvard Trauma Questionnaire: validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in indochinese refugees. J Nerv Ment Dis. 1998;180(2):111–6. [PubMed] [Google Scholar]
- 11.Porter M, Haslam N. Predisplacement and post displacement factors associated with the mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294(5):602–12. [DOI] [PubMed] [Google Scholar]
- 12.Charlson FJ, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. 2016;44(6):1195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charlson F, Van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. Articles New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. 2019;394. 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed]
- 14.Mental health conditions in conflict situations are much more widespread than we thought. https://www.who.int/news-room/commentaries/detail/mental-health-conditions-in-conflict-situations-are-much-more-widespread-than-we-thought. Accessed January 27, 2024.
- 15.Expert opinion. https://www.internal-displacement.org/expert-opinion/5-key-findings-on-internal-displacement-and-mental-health. Accessed January 27, 2024.
- 16.Mental health and forced displacement. https://www.who.int/news-room/fact-sheets/detail/mental-health-and-forced-displacement. Accessed April 23, 2024.
- 17.Hoppen TH, Morina N. The prevalence of PTSD and major depression in the global population of adult war survivors: a meta-analytically informed estimate in absolute numbers. Eur J Psychotraumatol. 2019;10(1). 10.1080/20008198.2019.1578637. [DOI] [PMC free article] [PubMed]
- 18.Elhabiby MM, Radwan DN, Okasha TA, El-Desouky ED. Psychiatric disorders among a sample of internally displaced persons in South Darfur. Int J Soc Psychiatry. 2015;61(4):358–62. 10.1177/0020764014547061. [DOI] [PubMed] [Google Scholar]
- 19.Makwana N. Disaster and its impact on mental health: a narrative review. J Family Med Prim care. 2019;8(10):3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dev D. (2022). Addressing the state of mental health in South Sudanese refugees across Uganda. Can J Undergrad Res 7(1).
- 21.Mohammed Bilal M, Moawia Balla Elnour S, Mohamed Elmahdi ZZ, Mustafa Mudawi Ahmed E. Mental health consequences among Sudanese due to the armed conflicts and civil unrest of 2023: a cross-sectional study. Int J Soc Psychiatry. 2024;70(3):563–73. 10.1177/00207640231221101 [DOI] [PubMed]
- 22.Spence JT, Helmreich RL, Pred RS. Impatience versus achievement strivings in the type A pattern: Differential effects on students’ health and academic performance. J Appl Psychol. 1987;72(4):522–8. [PubMed] [Google Scholar]
- 23.Salah TT, Abdelrahman A, Lien L, Eide AH, Martinez P, Hauff E. The mental health of internally displaced persons: an epidemiological study of adults in two settlements in Central Sudan. Int J Soc Psychiatry. 2013;59(8):782–8. 10.1177/0020764012456810. Epub 2012 Sep 13. PMID: 22982816. [DOI] [PubMed] [Google Scholar]
- 24.Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition – A consensus report from the global clinical nutrition community. Clin Nutr. 2019;38(1):1–9. [DOI] [PubMed] [Google Scholar]
- 25.Sabin M, Lopes Cardozo B, Nackerud L, Kaiser R, Varese L. Factors associated with poor mental health among Guatemalan refugees living in Mexico 20 years after civil conflict. JAMA 2003;290(5):635–42. [DOI] [PubMed]
- 26.Hamid AA, Musa SA. Mental health problems among internally displaced persons in Darfur. Int J Psychol. 2010;45(4):278 – 85. doi: 10.1080/00207591003692620. PMID: 22044013. [DOI] [PubMed]
- 27.Ekblad S, Prochazka H, Roth G. Psychological impact of torture: a 3-month follow-up of mass-evacuated kosovan adults in Sweden. Lessons learnt for prevention. Acta Psychiatry Scand. 2002;106:30–7. [DOI] [PubMed] [Google Scholar]
- 28.Kira IA, Shuwiekh HA, Rice KG, Ashby JS, Elwakeel SA, Sous MS, Alhuwailah A. The dynamics of post-disaster recovery among displaced and nondisplaced persons in Gaza Strip: a comparative study. Psychol Trauma. 2018;10(6):665–74. [Google Scholar]
- 29.Ekezie W. Resilience actions of Internally Displaced Persons (IDPs) living in camp-like settings: a Northern Nigeria case study. Journal of Migration and Health. 2022;6:100115. 10.1016/j.jmh.2022.100115 [DOI] [PMC free article] [PubMed]
- 30.Roberto SB, Chaaya M, Fares JE, Abi Khirs J. Psychological distress after the occupation: a community cross-sectional survey from Lebanon. Br J Health Psychol. 2006;11:695. [DOI] [PubMed] [Google Scholar]
- 31.Shears P, Berry AM, Murphy R, Nabil MA. Epidemiological assessment of the health and nutrition of Ethiopian refugees in emergency camps in Sudan1985.BMJ. (Clin Res Ed. 1987;295:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orach GC. Morbidity and mortality amongst southern Sudanese in Koboko Refugee camps, Arua district, Uganda. East Afr Med J. 1999;74:195–1999. [PubMed] [Google Scholar]
- 33.Hendrickse RG, Barr DGD. Matthews TS.Paediatrics in the tropics. Oxford Blackwell Scientific Publication; 1991.
- 34.Uganda Demographic Health Survey (UDHS).Preliminary Report2006/2007pp22-23.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.