Abstract
Background
Point-of-care ultrasound (POCUS) education has become an essential component of medical school curricula. Ultrasound represents a highly effective teaching modality to reinforce anatomical knowledge gained during cadaveric dissections. At Texas Tech University Health Sciences Center-School of Medicine (TTUHSC-SOM), POCUS was incorporated into the pre-clerkship curriculum especially during the first year of medical school anatomy course.
Methods
Pre- and post-ultrasound quizzes and summative exam performance were used to evaluate ultrasound session effectiveness. Post-block survey results were utilized to assess students’ perception of these sessions.
Results
A significant increase in post-quiz scores compared to pre-quiz scores (p < 0.0001) was observed in all three ultrasound sessions. Students ranked the overall experience with ultrasound sessions highly with 86% indicating ultrasound training was valuable in understanding human anatomy. Additionally, 92% indicated being more at ease in acquiring ultrasound images as the block progressed.
Conclusions
First-year medical students perceived ultrasound training as valuable in enhancing their understanding of human anatomy and became more proficient acquiring ultrasound images as the block progressed. Early introduction of POCUS in the pre-clerkship curriculum helps build foundational knowledge and skills that support students in developing competency in image acquisition and interpretation.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06483-y.
Keywords: Point of Care Ultrasound, anatomy laboratory education, technology-based learning
Introduction
Point of Care Ultrasonography (POCUS) is a diagnostic tool used by physicians in various specialties. Ultrasound’s utility in the rapid diagnosis of various medical conditions has resulted in its widespread incorporation in clinical practice by physicians, especially in the field of emergency medicine [1]. Current advancements in POCUS and the safety, portability, and effectiveness of this modality have resulted in expansion of POCUS to fields outside of traditional specialists using ultrasound, such as radiologists, cardiologists, obstetrics-gynecologists, and plastic surgeons [2, 3]. Clinical adoption of POCUS has outpaced education and training, resulting in the need to introduce education on this technology earlier within the pre-clerkship medical school curriculum [4, 5].
Ultrasound proficiency requires practice and repetition to become facile in image acquisition. In keeping with this, the American College of Emergency Physicians published clinical ultrasound guidelines in 2017 recommending a minimum of 150 ultrasound examinations (or 25–50 for each type) for general competence [6]. Incorporating ultrasound education and training into undergraduate medical education is highly beneficial to ensure students develop increased proficiency in image acquisition and overall comfort with this diagnostic tool [7, 8]. Accordingly, many institutions began implementing POCUS training into their undergraduate medical curriculum as early as 2006. The American Institute of Ultrasound in Medicine hosts a self-reported list of medical schools that have incorporated ultrasound into their medical school curricula. It reports 81 of 221 Liaison Committee on Medical Education-accredited schools to have some level of structured ultrasound instruction [9]. However, based on a recent survey of institutions, adoption of ultrasound in the curriculum of accredited United States medical schools is even more widespread [10]. Currently, 72.6% (168/200) of the medical schools that responded to the survey indicated having an ultrasound curriculum. Ultrasound was listed as a mandatory activity by majority of the survey respondents, with instruction primarily being integrated into existing courses (73.8% in basic science courses, 66.2% in clinical skills courses, and 35.4% in clinical rotations). Incorporation of ultrasound into undergraduate medical school curricula has generally been favorably received by the students as determined by a high level of satisfaction, as well as interest in obtaining additional ultrasound training [5, 11].
The use of ultrasound imaging can aid in connecting students’ comprehension of anatomy in the preclinical phase and their subsequent evaluation of patient anatomy and pathology in the clinical setting. An extensive review published in 2017 highlights that POCUS introduced during anatomy, complements anatomical knowledge learned during cadaveric dissections and fosters development of clinical skills [12]. While incorporating ultrasound as an educational tool for anatomy presents a boon for students, feasibility is limited by lack of resources required to effectively implement these sessions. Some of the significant hurdles preventing implementation of POCUS into the pre-clerkship curriculum include lack of trained faculty, curricular time limitations, and a lack of proper equipment/funding.11,13,14 The purpose of this study was twofold. First, we describe our experience with the implementation of POCUS into the pre-clerkship curriculum gross anatomy course at Texas Tech University Health Sciences Center School of Medicine (TTUHSC-SOM). Our secondary aim was to evaluate the effectiveness of formal ultrasound sessions, their impact on first-year medical students’ ability to read and acquire images, and their perceptions of the value of POCUS in the first-year gross anatomy course. Finally, we describe the successful navigation of commonly cited barriers to implementation.
Materials and methods
Ethics
This project has been approved by the TTUHSC-Quality Improvement Review Board (QIRB). Protocol number: QI-22091.
Study design
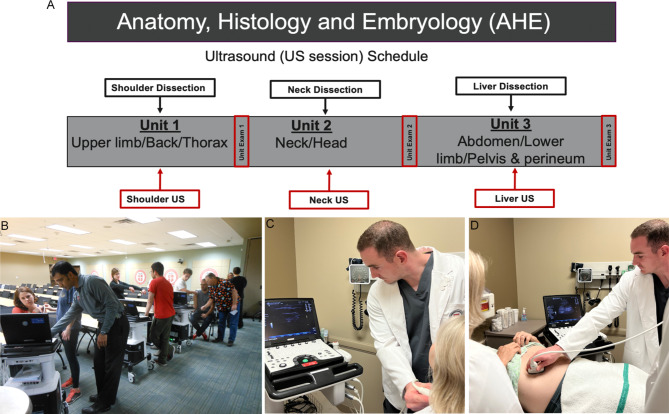
The Phase 1 medical school curriculum at TTUHSC begins with the 10-week Anatomy, Histology and Embryology (AHE) block. During this course, first-year medical students learn about human anatomy through lectures, cadaveric laboratory dissection, basic tissue histology, and embryology. The AHE block is divided into 3 units- upper limb, back and thorax (unit 1); head and neck (unit 2); and abdomen, lower limb, pelvis, and perineum (unit 3) (Fig. 1A). Ultrasound sessions were fully incorporated into the first-year anatomy block during the 2016–2023 academic year. This consisted of a 50-minute introductory lecture given by a clinician familiarizing the students with ultrasound physics, definitions/terms, “knobology”, transducer types, screen orientation and various artifacts. Additionally, three hands-on ultrasound sessions were integrated with the existing dissection activities for specific anatomical regions typically completed by our first-year medical students. These included the shoulder, neck, and abdomen (right upper quadrant) (Table 1).
Fig. 1.
Integration of ultrasound sessions into Phase 1 curriculum and in-person ultrasound sessions layout. A) The AHE block consists of 10 weeks and 3 units. Unit 1 focuses on the upper limb, back and thorax. After students complete the shoulder cadaveric dissection, in-person shoulder ultrasound session is incorporated into this unit. Unit 2 covers head and neck and students perform neck and thyroid ultrasound. Unit 3 focuses on abdomen, lower limb, pelvis, and perineum. In this unit students perform the liver and gallbladder ultrasound. B and C) For ultrasound sessions 1 (shoulder) and 2 (neck and thyroid), medical students perform ultrasound on each other (2 students/ultrasound machine) during practice sessions. D) For abdomen (liver and gallbladder) ultrasound, medical students perform ultrasound on a standardized patient. For this session students are grouped based on their cadaveric tank groups (3 students/standardized patient)
Table 1.
Ultrasound curriculum for first year medical students during anatomy lab dissections
| Session | Objectives |
|---|---|
| Shoulder (session 1) | Obtain an image of the musculoskeletal structures of the shoulder and wrist. Specifically, identify median nerve, arteries (radial and ulnar), tubercles/tuberosity (greater and lesser) and tendons (flexors at the wrist level, long head of the biceps, supraspinatus, infraspinatus, teres minor and subscapularis). |
| Neck and thyroid (session 2) | Identify carotid artery, jugular vein, thyroid gland, thyroid isthmus, trachea, strap muscles and measure the thyroid lobes. |
| Abdomen (session 3) | Identify relationship and orientation of liver and gallbladder. Obtain a view of the left lobe of the liver, caudate lobe, inferior vena cava, ligamentum venosum, and hepatic vein. |
Participants
All first-year medical students enrolled at TTUHSC-SOM (2016–2019, 2021–2023) were eligible for inclusion (n = 1,260) in this study. Due to COVID-19 restrictions, ultrasound sessions were not offered in the academic year 2019–2020. Ultrasound sessions and the associated quizzes were mandatory for the medical students; however, students were given the opportunity to select the time for the in-person ultrasound session to allow for flexibility in scheduling. All the participants were included in the pre-quiz analysis, but only the participants who attended in-person ultrasound sessions were included in the post analysis. Additionally, despite the mandatory nature of the quizzes, some students fail to complete the quizzes on time, resulting in missing data. This discrepancy may be reflected in the differences between the number of quiz takers and ultrasound attendance.
Facilitator training
To ensure consistency among facilitators, a 2-hour facilitator training was provided to the anatomy faculty and the teaching assistants (Graduate Medical Education Sciences Program, GMES) prior to each ultrasound session. Additionally, the teaching assistants participated in a total of 5 h of ultrasound training during the GMES orientation, prior to start of the AHE block. During this training, the teaching assistants engage in hands-on practice sessions under the supervision of experienced faculty members to ensure they feel comfortable facilitating the sessions. The trainers included the medical education anatomy faculty who are well-versed with ultrasonography. For the musculoskeletal ultrasound (session 1) the clinicians, together with fellows, from the Department of Family Medicine Sports Medicine Fellowship, participated in training the faculty and medical students. The medical education anatomy faculty and the clinicians remained consistent throughout the study.
In-person ultrasound session structure
Prior to each session, students were provided online learning modules (the Society of Ultrasound in Medical Education (SUSME) modules) with stepwise instructions for performing the ultrasound evaluation of specific structures within each region (Supplemental File 1). To optimize time utilization, each ultrasound education session was strategically consolidated into a single day, further organized into 30-minute intervals for student sign-ups. For these sessions, students paired up and worked to image the region of interest using either themselves (shoulder and neck ultrasound, Fig. 1B C) or a standardized patient (abdomen, Fig. 1D). This approach enhanced scheduling flexibility for students, mitigating disruptions to the curriculum while ensuring ample time for skills practice and achievement of educational objectives. The learning objectives for each session were developed in alignment with the core clinical ultrasound milestones proposed by Dinh et al. [13] To further aid in learning, students were guided by the facilitators and the student-to-facilitator ratio was kept low (~ 2:1). The facilitators ensured proper student understanding of the material covered in the session, contextualized the concepts with regards to clinical applications and embryology within the anatomy curriculum, and moved students through the sessions in a timely manner.
Ultrasound questions and student feedback
Twenty-four hours prior to each ultrasound session, a short multiple-choice pre-quiz was administered via Examplify (web-based testing application) to collect data on baseline familiarity and understanding of the principles of ultrasound and identification of various structures on a static ultrasound image of the region of interest (Supplemental File 2). Following completion of an ultrasound session, a post-quiz containing questions relevant to the learning session was assigned to the students. The focus of the post-quiz was to determine whether in-person ultrasound sessions improved ultrasound familiarity and image interpretation. To obtain this goal, different post-quiz questions were given as compared to pre-quiz, but tested concepts were the same. To assess retention of knowledge gained from these sessions, 2 image interpretation questions were included in the unit exams. The image interpretation questions included on exams consisted of images that students had previously seen. However, students were tasked with identifying an alternative structure within the same image, challenging their comprehension in a novel way. An End-of-Block survey was given to the students after completion of AHE block to assess student attitudes. For the academic year 2022–2023, both pre-quiz 1 and post-quiz 3 also contained questions to gauge student perception of ultrasound and confidence in usage of ultrasound.
Statistical analysis
De-identified student assessment scores were obtained through the TTUHSC- Office of Curriculum. Data are expressed as the mean ± standard deviation. A student’s paired t-test was used to compare the pre- and post-quiz scores. For multiple comparisons, a one-way or two-way analysis of variance (ANOVA) was performed using GraphPad Prism version 4.03 software. When significance was observed, comparisons between groups were made using Bonferroni or Tukey’s post-hoc test. A p-value of ≤ 0.05 was considered significant.
Results
Student performance on the ultrasound quizzes
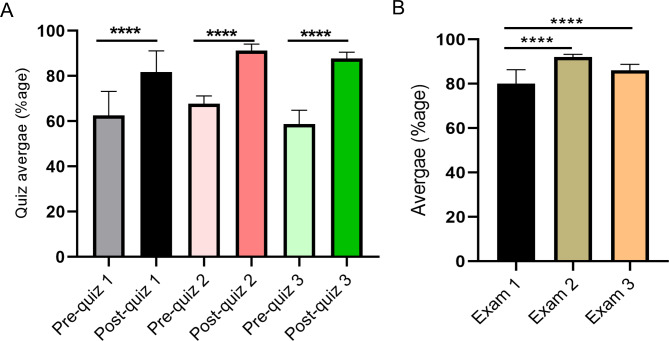
Student performance on pre- and post-quizzes for the shoulder, neck and thyroid, and abdomen sessions were analyzed. Each class for the academic years presented had between 168 and 189 participants on the pre- and post-ultrasound quizzes (Tables 2, 3 and 4). Student post-quiz scores improved significantly relative to their pre-quiz scores for shoulder, neck, thyroid, and abdomen ultrasound sessions across all academic years (Fig. 2A and Tables 2, 3 and 4). Additionally, student performance on subsequent pre- and post-quizzes improved significantly from session 1. Pre- and post-quiz session 2 scores (67.6% and 90.9% respectively) were significantly higher than corresponding pre- and post-quiz performance from session 1 (59.8% and 82.6% respectively) (p < 0.001) (Fig. 2A). In contrast, performance on pre-quiz 3 (60.2%) was significantly lower compared to prior pre-quiz 2 (60.2% and 67.6% respectively) (p < 0.001). However, performance on post-quiz 3 (87.4%) was significantly improved as compared to post-quiz 1 (82.6%) (p < 0.001) (Fig. 2A).
Table 2.
Student performance on ultrasound quizzes for the shoulder session
| Ultrasound session 1 | Quiz average (%age) | SD (±) | Number of participants (quizzes) | Number of participants (US session) | Score range | p-value | |
|---|---|---|---|---|---|---|---|
| AY 2016–2017 | Pre-quiz | 64 | 1.13 | 180 | 182 | 20–100 | < 0.0001 |
| Post-quiz | 89 | 0.72 | 182 | 40–100 | |||
| AY 2017–2018 | Pre-quiz | 65 | 1.3 | 186 | 186 | 0-100 | < 0.0001 |
| Post-quiz | 85 | 0.80 | 178 | 40–100 | |||
| AY 2018–2019 | Pre-quiz | 65 | 1.18 | 185 | 184 | 0-100 | < 0.0001 |
| Post-quiz | 88 | 0.75 | 181 | 40–100 | |||
| AY 2019–2020 | Pre-quiz | 62 | 1.19 | 187 | 188 | 0-100 | < 0.0001 |
| Post-quiz | 87 | 0.86 | 185 | 20–100 | |||
| AY 2021–2022 | Pre-quiz | 43 | 1.2 | 189 | 187 | 0-100 | < 0.0001 |
| Post-quiz | 65 | 0.80 | 178 | 20–100 | |||
| AY 2022–2023 | Pre-quiz | 76 | 1.1 | 180 | 184 | 44–100 | < 0.0001 |
| Post-quiz | 77 | 0.89 | 168 | 20–100 | |||
AY- academic year, %age- percentage, SD- standard deviation
Table 3.
Student performance on ultrasound quizzes for the neck and thyroid session
| Ultrasound session 2 | Quiz average (%age) | SD (±) | Number of participants (quizzes) | Number of participants (US session) | Score range | p-value | |
|---|---|---|---|---|---|---|---|
| AY 2016–2017 | Pre-quiz | 69 | 1.41 | 188 | 181 | 0-100 | < 0.0001 |
| Post-quiz | 91 | 0.68 | 181 | 40–100 | |||
| AY 2017–2018 | Pre-quiz | 67 | 1.45 | 185 | 183 | 0-100 | < 0.0001 |
| Post-quiz | 93 | 0.72 | 174 | 0-100 | |||
| AY 2018–2019 | Pre-quiz | 71 | 1.38 | 181 | 183 | 0-100 | < 0.0001 |
| Post-quiz | 94 | 0.53 | 177 | 60–100 | |||
| AY 2019–2020 | Pre-quiz | 69 | 1.45 | 189 | 188 | 0-100 | < 0.0001 |
| Post-quiz | 93 | 0.59 | 188 | 40–100 | |||
| AY 2021–2022 | Pre-quiz | 69 | 1.51 | 188 | 181 | 0-100 | < 0.0001 |
| Post-quiz | 90 | 0.68 | 181 | 40–100 | |||
| AY 2022–2023 | Pre-quiz | 61 | 1.4 | 184 | 181 | 0-100 | < 0.0001 |
| Post-quiz | 86 | 0.82 | 179 | 20–100 | |||
AY- academic year, %age- percentage, SD- standard deviation
Table 4.
Student performance on ultrasound quizzes for the abdomen session
| Ultrasound session 3 | Quiz average (%age) | SD (±) | Number of participants (quizzes) | Number of participants (US session) | Score range | p-value | |
|---|---|---|---|---|---|---|---|
| AY 2016–2017 | Pre-quiz | 57 | 1.38 | 182 | 182 | 0-100 | < 0.0001 |
| Post-quiz | 90 | 0.79 | 182 | 20–100 | |||
| AY 2017–2018 | Pre-quiz | 68 | 1.33 | 179 | 186 | 0-100 | < 0.0001 |
| Post-quiz | 92 | 0.61 | 171 | 40–100 | |||
| AY 2018–2019 | Pre-quiz | 58 | 1.37 | 180 | 184 | 0-100 | < 0.0001 |
| Post-quiz | 85 | 1.05 | 177 | 20–100 | |||
| AY 2019–2020 | Pre-quiz | 59 | 1.45 | 188 | 188 | 0-100 | < 0.0001 |
| Post-quiz | 87 | 0.84 | 187 | 20–100 | |||
| AY 2021–2022 | Pre-quiz | 61 | 1.5 | 183 | 189 | 0-100 | < 0.0001 |
| Post-quiz | 85 | 1.01 | 189 | 20–100 | |||
| AY 2022–2023 | Pre-quiz | 49 | 1.33 | 180 | 183 | 0-100 | < 0.0001 |
| Post-quiz | 87 | 1.02 | 173 | 56–100 | |||
AY- academic year, %age- percentage, SD- standard deviation
Fig. 2.
Student performance on the ultrasound quizzes and summative exams. (A) Student average performance on the pre- and post-ultrasound quizzes (3 pre- and 3 post-quizzes) over the years was shown as a bar graph. (B) Student performance on static ultrasound image interpretation questions on summative exams was shown as a bar graph. Data are expressed as the mean ± standard deviation. A one-way Analysis of Variance (ANOVA) followed by Tukey’s post-hoc test was performed using GraphPad Prism software. A p ≤ 0.05 was considered significant (**** p < 0.0001)
Student performance on summative written exam ultrasound questions
To assess retention of knowledge gained from in-person ultrasound sessions, image interpretation questions were included in unit exams specific to the ultrasound session corresponding with that unit. Following ultrasound session 1, 80% of the students correctly identified the long head of the biceps tendon on the summative unit 1 exam with a point biserial (PBS) of 0.38 (Fig. 2B). Similarly, 92% and 86% of the students correctly identified the internal jugular vein and the inferior vena cava (IVC) on the unit 2 (PBS-0.19) and unit 3 (PBS-0.22) exams (Fig. 2B). Student performance on units 2 and 3 ultrasound exam questions was significantly increased as compared to unit 1 (p < 0.001) (Fig. 2B). In academic year 2020–2021, in-person ultrasound sessions were not provided to the students due to COVID restrictions but the didactic introductory lecture familiarizing the students with ultrasound physics, definitions/terms, “knobology”, transducer types, screen orientation and various artifacts was given. During COVID year, performance on a question requiring identification of nerves versus muscle tendons based on anisotropy was only successfully answered by 34% of the students.
Student survey
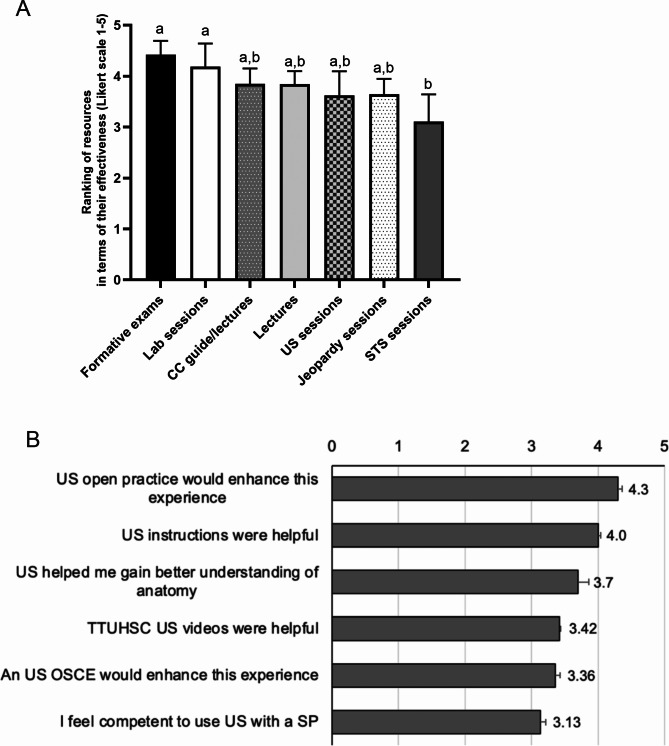
Prior to participating in the in-person AHE ultrasound sessions, 38% of the students were familiar (somewhat or extremely) with techniques and imaging, 65% were comfortable with visualizing anatomy in a 3D space and 26% were comfortable with acquiring ultrasound images (Table 5). After completion of 3 hands-on ultrasound sessions in AHE, 99% of the students said they were familiar with ultrasound techniques and imaging, 86% felt comfortable visualizing anatomy in a 3D space and 94% felt comfortable with acquiring ultrasound images (Table 5). In the End-of-Block AHE surveys (n = 161–186), the ultrasound sessions were rated equivalent to other sessions/activities offered within the block, such as anatomy lab sessions, formative exams, clinical correlation lectures, and jeopardy sessions (Fig. 3A). Students indicated that ultrasound sessions were beneficial to their better understanding of anatomy (Fig. 3B). Students also endorsed a strong desire for more time in the curriculum to practice and learn ultrasound skills (Fig. 3B).
Table 5.
Student perception of basic familiarity with ultrasound techniques and confidence in acquiring ultrasound images
| Ultrasound session 1 pre-quiz (n = 193) | Ultrasound session 3 post-quiz (n = 186) | |
|---|---|---|
| How familiar are you with ultrasound techniques and imaging? | ||
| Extremely familiar | 4.15% | 11.29% |
| Somewhat familiar | 33.68% | 87.63% |
| Not familiar | 24.87% | 2.15% |
| Somewhat unfamiliar | 19.17% | 2.15% |
| Extremely unfamiliar | 18.13% | 0.54% |
| How comfortable are you with visualizing anatomy in a 3D space? | ||
| Extremely comfortable | 5.70% | 15.05% |
| Somewhat comfortable | 59.07% | 70.97% |
| Not comfortable | 22.28% | 16.13% |
| Somewhat uncomfortable | 11.92% | 1.08% |
| Extremely uncomfortable | 1.04% | 0.54% |
| How comfortable are you with acquiring ultrasound images? | ||
| Extremely comfortable | 3.63% | 12.90% |
| Somewhat comfortable | 22.80% | 79.57% |
| Not comfortable | 42.49% | 9.14% |
| Somewhat uncomfortable | 22.28% | 2.15% |
| Extremely uncomfortable | 8.81% | 0.54% |
Fig. 3.
Student perception of ultrasound sessions. An End-of-Block survey was given to the first-year medical students after the completion of AHE block. An average of 169 (range- 160–181) students participated in the survey. (A) Effectiveness of various resources in enhancing student learning experience was analyzed on a 5-point Likert scale. Formative exams and lab sessions were significantly different from student-teaching-student (STS) sessions as indicated by different letters. A one-way Analysis of Variance (ANOVA) followed by Tukey’s post-hoc test was performed using GraphPad Prism software. A p ≤ 0.05 was considered significant. CC- clinical correlation; US- Ultrasound, STS- student-teaching-student. (B) Student perception regarding ultrasound sessions was analyzed based on a 5-point Likert scale
Discussion
Early introduction of POCUS in the medical school curriculum can provide numerous benefits for medical students [5, 7, 14–16]. Due to the complex anatomical relationships and spatial orientation, many aspects of clinical and regional anatomy can be difficult to comprehend based on using 2D models or cadaveric study alone. Incorporating ultrasound has been shown to provide benefits as an additional tool to help understand these complex concepts [7, 17–20]. It also increases competency and confidence in image acquisition and interpretation. Guided POCUS sessions allow for greater confidence in clinical decision-making during clerkships and when performing physical exams [5, 7, 15, 16]. A study by Liu et al. found that students who participated in a longitudinal POCUS program scored significantly higher on the Clinical Skills portion of the United States Medical Licensing Exam than non-participating students [21]. The aim of this study is to describe the authors’ experience in the implementation of POCUS into the pre-clerkship curriculum during the anatomy block at TTUHSC-SOM over a six-year period. Primary outcomes were evaluated through descriptive data using pre- and post-quiz performance, summative exam data, and survey responses from End-of-Block surveys.
At TTUHSC-SOM, ultrasound sessions (didactic and 3 in-person sessions) were fully incorporated into first-year anatomy in the AHE block. Each in-person session was focused on imaging structures corresponding to the cadaveric dissection occurring at the time of the ultrasound instruction. This allowed not only for a demonstration of the pertinent clinical applications, but also afforded students the opportunity to explore concepts that were presented during the anatomy lectures and laboratory. The first two sessions (musculoskeletal system and neck) were performed in groups of two students to one ultrasound machine, providing more opportunity and time to practice their skills on themselves or their partner and allowing for a more personalized experience. Peer interaction and active learning allowed students to learn from and teach one another, which is an effective learning modality [22–24]. Performing the abdominal ultrasound (session 3) on standardized patients also introduced the students to skills required for patient interactions.
There was a significant increase in post-quiz scores compared to pre-quiz scores in all three ultrasound sessions of the AHE block. An increase in post-quiz performance was also observed as students progressed through the block. For instance, post-quiz 2 had significantly higher scores than post-quiz 1 (p < 0.0001). This finding could be explained by students becoming more comfortable with the ultrasound sessions, allowing them greater success. Performance on post-quiz 3 showed significant improvement compared to post-quiz 1 but not relative to post-quiz 2. This finding can be attributed to the comparatively increased difficulty of the third ultrasound session (liver and gallbladder) as compared to the second session. Additionally, student performance on questions on summative exams involving ultrasound image recognition further shows the effectiveness of this learning modality in understanding human anatomy. Students performed well on questions with low levels of difficulty, such as identification of the internal jugular vein on an ultrasound image. However, questions that required greater effort regarding orientation and differentiation, such as identifying the IVC on a liver ultrasound, presented more of a challenge. Despite this challenge, the performance on exam 3 questions was significantly improved as compared to exam 1 questions, suggesting hands-on experience translated into increased familiarity with usage of ultrasound by the end of AHE course. These findings align with current literature showing similar results [7, 25–30].
Medical students strongly favor inclusion of POCUS sessions as they recognize the benefits of this early exposure and training. Numerous studies report student feedback on their experiences with ultrasound sessions through survey responses indicating that ultrasound training and educational sessions are well received by students and viewed favorably [5, 7, 11, 17, 31]. In an article by Minardi et al., West Virginia University School of Medicine, the authors described their experience implementing an ultrasound curriculum in 2012. Following the four-year curriculum, survey results showed that 93% of students viewed the curriculum favorably [11]. Other institutions, such as the University of South Carolina and Harvard Medical School, also shared their experiences implementing ultrasound into their curriculum. Both studies reported positive feedback, with over 75% of students wanting to see further incorporation of ultrasound into the curriculum [5, 17]. Similarly, at TTUHSC, AHE End-of-Block survey showed over two-thirds of responses indicating students value ultrasound sessions, as these sessions were ranked on par with other sessions provided within the block. Students also indicated a desire for increased time and opportunities dedicated to ultrasound sessions. In addition, 92% of the students indicated that they are comfortable with acquiring ultrasound images and 86% indicated that they are comfortable with visualizing anatomy in 3D space after completion of ultrasound sessions. These results are on par with previously published literature. For instance, a study reported that 93% of students reported favorably on the ultrasound experience after incorporation of ultrasound within a gross anatomy course for second-year medical students. In addition, approximately 90% felt strongly that ultrasound used in practical self-study was complementary to the anatomy learning [11].
Although ultrasound implementation into medical school curricula is becoming more common, the number of medical schools with a formal ultrasound curriculum is still low [9]. Reasons for this include the hurdles many institutions face in incorporating formal ultrasound sessions into the medical school curriculum. These barriers include cost and lack of funding, time constraints, physical space constraints, and lack of trained faculty [4, 11, 31, 32]. Russell et al. surveyed 122 clinical ultrasound directors and curricular deans at United States medical schools. They found that 94% of these programs encountered some or many of these barriers, with lack of trained faculty being the highest reported [32]. Although this is a significant issue, previous studies have shown successful implementation of ultrasound with limited clinically trained faculty through the help of residents, upper-level medical students, and peer-led instruction [4, 23, 24, 30, 32, 33]. At TTUHSC-SOM, a combination of anatomy faculty (n = 6), clinical faculty (n = 2), residents (n = 2), who are well-versed in ultrasound, and ultrasound-trained teaching assistants (n = 12–15) facilitate these sessions. Teaching assistants having limited background experience with POCUS were trained to facilitate POCUS sessions through a 2-hour facilitator training session prior to each ultrasound session. Additionally, the teaching assistants participated in a total of 5 h of ultrasound training one week before the start of the AHE block. Training sessions involved dividing teaching assistants into small groups and practicing skills pertaining to the upcoming session on standardized patients or each other. This allowed for quick training of graduate students, who were then able to assist in facilitating the teaching sessions. The TTUHSC-SOM gross anatomy class size has an average of 200 students and includes first year medical students and a small group of Graduate Medical Education Sciences students. Notably, this class size surpasses the national average of 155 among U.S. medical schools [34]. Despite the large class size, the student-to-facilitator ratio remains low (~ 2:1) in these sessions due to the availability of teaching assistants. Efficient scheduling plays a pivotal role in optimizing these sessions, with students offered multiple sign-up opportunities on the session date. This approach not only maintains a balanced instructor-student ratio but also accommodates students’ diverse schedules. The success of incorporating ultrasound sessions and integrating image interpretation into exams hinged significantly on the support and commitment of key stakeholders, including students and block directors. Their buy-in was integral to seamless implementation and effectiveness of these educational initiatives.
As ultrasound becomes more prevalent in different medical specialties and clinical settings, it is crucial to prepare medical students with the skills and knowledge they need to use POCUS effectively. Common barriers to implementation including limited trained facilitators can be navigated through invoking the assistance of graduate students or upper-level medical students with short training sessions prior to the teaching session. Early exposure to POCUS in the pre-clerkship curriculum provides students with foundational knowledge and skills, ultimately helping them achieve proficiency in using ultrasound as a diagnostic tool during clerkship rotations, residency training, and future clinical practice. In addition, investigating the feasibility of incorporating POCUS education into the medical school curriculum is an essential step toward ensuring that future clinicians are well-prepared to use this valuable technology.
Limitations of the study
Although this study adds to the literature describing the successful incorporation of POCUS into the medical school curriculum, it does have some limitations. The primary limitation is that this study only involved first-year medical students. Therefore, future studies should include a more diverse group of medical students from different academic years to determine if early ultrasound training improves their competency and proficiency in ultrasound imaging as they progress through their medical education. Secondly, the trainers facilitating the ultrasound sessions had varying levels of expertise in POCUS, and the training sessions attended by teaching assistants were relatively brief. Consequently, the variability in trainer experience may have influenced the consistency and quality of the learning experience for students. Furthermore, the assessment methods utilized in this study are limited. The missing quiz data due to students not completing mandatory quizzes or in-person sessions could introduce a potential bias in the analysis of quiz results. To mitigate the impact of missing quiz data, we analyzed the number of students who did not complete the quizzes. On average, 20 or fewer students missed quizzes, indicating that while missing data may slightly affect overall scores, the impact is minimal when examining broader trends in a large same size (n ≥ 160) rather than individual quiz performance. The effectiveness of early intervention on better student outcomes should be explored through longitudinal assessments in future cohorts.
Conclusions
This manuscript highlights the successful implementation of formal ultrasound training sessions into the pre-clerkship medical school curriculum. The incorporation of ultrasound into medical education is becoming increasingly important, and this study contributes to the growing body of literature on this topic. Overall, the results of this study suggest formal ultrasound training in medical school can provide valuable clinical skills and knowledge to future physicians, which may contribute to improved patient care and outcomes. The authors of this study aim to inspire other institutions to consider implementing similar programs and continue advancing the integration of ultrasound into medical education.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank TTUHSC anatomy faculty and the Graduate Medical Education Sciences teaching assistants who facilitated these ultrasound sessions. Specifically, Drs. Dixon Santana and Samuel J. Campbell who initially trained the faculty and medical students. This work was presented at the following conferences: (1) Society of Teachers of Family Medicine (2023, Lecture-based discussion), (2) American Association of Clinical Anatomists (2022, Tech Fair presentation), (3) Sixth World Congress Ultrasound in Medical Education (2018, abstract accepted but meeting was canceled due to Hurricane Florence).
Abbreviations
- POCUS
Point of Care Ultrasound
- TTUHSC-SOM
Texas Tech University Health Sciences Center-School of Medicine
- AHE
Anatomy, Histology and Embryology
- SUSME
Society of Ultrasound in Medical Education
- PBS
Point Biserial
- IVC
Inferior Vena Cava
Author contributions
FZ, CM, MB, GK: data collection, data analysis, literature review and manuscript writing; GB, AH, JM, DE: literature review and critical reading of the manuscript; VL, JK: protocol development and manuscript writing. All authors reviewed the manuscript and approved the final version.
Funding
This work did not receive any external funding.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This project has been approved by the TTUHSC-QIRB (Protocol number: QI-22091) as a quality improvement project. As the project involved the systematic collection and analysis of data to enhance the quality of an educational program, consent to participate was waived in accordance with TTUHSC QIRB guidelines and approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hashim A, Tahir MJ, Ullah I, Asghar MS, Siddiqi H, Yousaf Z. The utility of point of care ultrasonography (POCUS). Ann Med Surg (Lond) Nov. 2021;71:102982. 10.1016/j.amsu.2021.102982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB. Point-of-Care Ultrasound in General Practice: A Systematic Review. Ann Fam Med Jan. 2019;17(1):61–9. 10.1370/afm.2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aravind P, Tiongco RFP, McNichols CH, Williams EH. Ultrasound as a Useful Tool for a Peripheral Nerve Surgeon: Examples in Clinical Practice. J Reconstr Microsurg Jul. 2023;39(6):405–12. 10.1055/s-0042-1759526. [DOI] [PubMed] [Google Scholar]
- 4.Bahner DP, Adkins EJ, Hughes D, Barrie M, Boulger CT, Royall NA. Integrated medical school ultrasound: development of an ultrasound vertical curriculum. Crit Ultrasound J Jul. 2013;2(1):6. 10.1186/2036-7902-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rempell JS, Saldana F, DiSalvo D, et al. Pilot Point-of-Care Ultrasound Curriculum at Harvard Medical School: Early Experience. West J Emerg Med Nov. 2016;17(6):734–40. 10.5811/westjem.2016.8.31387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College of Emergency Physicians. Ultrasound Guidelines: Emergency, Point-of-Care and Clinical Ultrasound Guidelines in Medicine. Ann Emerg Med. May 2017;69(5):e27–54. 10.1016/j.annemergmed.2016.08.457. [DOI] [PubMed]
- 7.Khoury M, Fotsing S, Jalali A, Chagnon N, Malherbe S, Youssef N. Preclerkship Point-of-Care Ultrasound: Image Acquisition and Clinical Transferability. J Med Educ Curric Dev Jan-Dec. 2020;7:2382120520943615. 10.1177/2382120520943615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rao S, van Holsbeeck L, Musial JL, et al. A pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine: a pioneer year review. J Ultrasound Med. 2008;27(5):745–9. 10.7863/jum.2008.27.5.745. [DOI] [PubMed] [Google Scholar]
- 9.AIUM. Ultrasound in Medicine Education Portal: Medical Schools. American Institute of Ultrasound in Medicine. Accessed April. 1st, 2023. http://meded.aium.org/medical-schools
- 10.Nicholas E, Ly AA, Prince AM, Klawitter PF, Gaskin K, Prince LA. The Current Status of Ultrasound Education in United States Medical Schools. J Ultrasound Med Nov. 2021;40(11):2459–65. 10.1002/jum.15633. [DOI] [PubMed] [Google Scholar]
- 11.Minardi J, Ressetar H, Foreman T, et al. Longitudinal Ultrasound Curriculum Incorporation at West Virginia University School of Medicine: A Description and Graduating Students’ Perceptions. J Ultrasound Med Jan. 2019;38(1):63–72. 10.1002/jum.14662. [DOI] [PubMed] [Google Scholar]
- 12.So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: Impact on learning anatomy and physical diagnosis. Anat Sci Educ Mar. 2017;10(2):176–89. 10.1002/ase.1630. [DOI] [PubMed] [Google Scholar]
- 13.Dinh VA, Lakoff D, Hess J, et al. Medical Student Core Clinical Ultrasound Milestones: A Consensus Among Directors in the United States. J Ultrasound Med Feb. 2016;35(2):421–34. 10.7863/ultra.15.07080. [DOI] [PubMed] [Google Scholar]
- 14.Hoppmann RA, Rao VV, Poston MB, et al. An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J. 2011;3(1):1–12. 10.1007/s13089-011-0052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zoll K, Kondrashov P, Pazdernik V et al. Medical Student Perception of the Impact of Early Ultrasonography Education on Experiences during Clinical Rotations. Medical Science Educator. 2017/06/01 2017;27(2):273–280. 10.1007/s40670-017-0394-4
- 16.Wong CK, Hai J, Chan KYE, et al. Point-of-care ultrasound augments physical examination learning by undergraduate medical students. Postgrad Med J Jan. 2021;97(1143):10–5. 10.1136/postgradmedj-2020-137773. [DOI] [PubMed] [Google Scholar]
- 17.Hoppmann RA, Rao VV, Bell F, et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J Dec. 2015;7(1):18. 10.1186/s13089-015-0035-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steinmetz P, Oleskevich S, Lewis J. Acquisition and Long-term Retention of Bedside Ultrasound Skills in First-Year Medical Students. J Ultrasound Med Sep. 2016;35(9):1967–75. 10.7863/ultra.15.09088. [DOI] [PubMed] [Google Scholar]
- 19.Kondrashova T, Kondrashov P. Integration of Ultrasonography into the Undergraduate Medical Curriculum: Seven Years of Experience. Mo Med Jan-Feb. 2018;115(1):38–43. [PMC free article] [PubMed] [Google Scholar]
- 20.Zawadka M, Graczyńska A, Janiszewska A, et al. Lessons Learned from a Study of the Integration of a Point-of-Care Ultrasound Course into the Undergraduate Medical School Curriculum. Med Sci Monit Jun. 2019;2:25:4104–9. 10.12659/msm.914781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu RB, Suwondo DN, Donroe JH, Encandela JA, Weisenthal KS, Moore CL. Point-of-Care Ultrasound: Does it Affect Scores on Standardized Assessment Tests Used Within the Preclinical Curriculum? J Ultrasound Med Feb. 2019;38(2):433–40. 10.1002/jum.14709. [DOI] [PubMed] [Google Scholar]
- 22.Burgess A, McGregor D, Mellis C. Medical students as peer tutors: a systematic review. BMC Med Educ Jun. 2014;9:14:115. 10.1186/1472-6920-14-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Celebi N, Griewatz J, Ilg M, et al. Three different ways of training ultrasound student-tutors yield significant gains in tutee’s scanning-skills. GMS J Med Educ. 2019;36(6):Doc77. 10.3205/zma001285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodcoff A, Keane D, Bialczak A, Ziner E, Hanna JB. Point-of-Care Ultrasonography Integration in Undergraduate Medical Education: A Student-Driven Approach. J Am Osteopath Assoc. Mar 2019;1(3):e11–6. 10.7556/jaoa.2019.033. [DOI] [PubMed] [Google Scholar]
- 25.Tshibwabwa ET, Groves HM. Integration of ultrasound in the education programme in anatomy. Med Educ Nov. 2005;39(11):1148. 10.1111/j.1365-2929.2005.02288.x. [DOI] [PubMed] [Google Scholar]
- 26.Fernández-Frackelton M, Peterson M, Lewis RJ, Pérez JE, Coates WC. A bedside ultrasound curriculum for medical students: prospective evaluation of skill acquisition. Teach Learn Med Winter. 2007;19(1):14–9. 10.1080/10401330709336618. [DOI] [PubMed] [Google Scholar]
- 27.Wright SA, Bell AL. Enhancement of undergraduate rheumatology teaching through the use of musculoskeletal ultrasound. Rheumatol (Oxford) Oct. 2008;47(10):1564–6. 10.1093/rheumatology/ken324. [DOI] [PubMed] [Google Scholar]
- 28.Brown B, Adhikari S, Marx J, Lander L, Todd GL. Introduction of ultrasound into gross anatomy curriculum: perceptions of medical students. J Emerg Med Dec. 2012;43(6):1098–102. 10.1016/j.jemermed.2012.01.041. [DOI] [PubMed] [Google Scholar]
- 29.Kondrashov P, Johnson JC, Boehm K, Rice D, Kondrashova T. Impact of the clinical ultrasound elective course on retention of anatomical knowledge by second-year medical students in preparation for board exams. Clin Anat Mar. 2015;28(2):156–63. 10.1002/ca.22494. [DOI] [PubMed] [Google Scholar]
- 30.Oberoi MK, Perera NC, Reynaga J, et al. Students Teaching Students: Student-Led Ultrasound Curriculum in Medical School Education. Cureus Nov. 2021;13(11):e19332. 10.7759/cureus.19332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dinh VA, Frederick J, Bartos R, Shankel TM, Werner L. Effects of ultrasound implementation on physical examination learning and teaching during the first year of medical education. J Ultrasound Med Jan. 2015;34(1):43–50. 10.7863/ultra.34.1.43. [DOI] [PubMed] [Google Scholar]
- 32.Russell FM, Zakeri B, Herbert A, Ferre RM, Leiser A, Wallach PM. The State of Point-of-Care Ultrasound Training in Undergraduate Medical Education: Findings From a National Survey. Acad Med. May 1. 2022;97(5):723–727. 10.1097/acm.0000000000004512 [DOI] [PubMed]
- 33.Boivin Z, Carpenter S, Lee G, et al. Evaluation of a Required Vertical Point-of-Care Ultrasound Curriculum for Undergraduate Medical Students. Cureus Oct. 2022;14(10):e30002. 10.7759/cureus.30002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Association of American Medical Colleges. Data from: Total Enrollment by U.S. MD-Granting Medical School and Gender, 2018–2019 through 2022–2023. 2022. https://www.aamc.org/media/6101/download
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.