Abstract
Introduction
The utilization of maternal health services is vital to prevent maternal and child health problems. However, there is limited evidence as to why rural women have lower utilization and educational inequality in maternal health services utilization in Ethiopia. Identifying the causes is the first step to achieving maternal and child health initiatives.
Objective
The objective of this study was to decompose the urban-rural disparities and educational inequalities in maternal health care utilization in Ethiopia.
Methods
The study used the 2019 Ethiopian Demography Health Survey. Blinder-Oaxaca decomposition and multivariate decomposition analyses were done on a weighted 3,926.7 women to see the urban-rural differences in maternal health service utilization by using Stata 17.0. For the educational inequality of maternal health service utilization, concentration curve and concentration index were used by using conindex. P value < 0.005 was used to declare association.
Result
84.89% of urban and 70.75% of rural residents use antenatal care and 73% of urban and 44% rural use institutional delivery. There was no urban-rural difference in postnatal care utilization. There was educational inequality in antenatal care (CIx 0.0926; p < 0.001), delivery care (CIx 0.2137; p < 0.001 and postnatal care (CIx 0.1272; p < 0.001) utilization in Ethiopia. 83.3% of antenatal care urban-rural difference was explained by women’s characteristics difference. Secondary (16.51%) and higher (23.01%) educational level difference of urban and rural women widening antenatal care utilization. Living regions (-1.33%) difference of urban and rural women mitigated antenatal care utilization. About 76.07% of the urban-rural difference in institutional delivery was explained by differences in the characteristics of women. Attending primary (3.76%), secondary (11.83%), and higher (8.44%) education, antenatal care (15.81%) difference of urban and rural women were widening institutional delivery utilization.
Conclusion
The urban-rural disparity in antenatal care and delivery care utilization is significant in the country. There were educational inequalities in maternal health service utilization. Attending, Secondary, higher, educational levels widening antenatal care and institutional delivery care utilization. Living regions mitigated antenatal care utilization. Antenatal care utilization widening institutional delivery utilization. Special attention is needed for rural women to improve maternal health service utilization through health extension workers and the women’s developmental army.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20689-1.
Keywords: Maternal health services, Urban-rural disparities, Educational inequality, Blinder-Oaxaca decomposition
Introduction
Maternal mortality is a global public health problem [1–5]. Globally, maternal mortality is decline in the last 25 years [4, 6–9]. But the burden is high in low income countries [2, 4, 6–9] including Ethiopia, where maternal health service coverage is a public health problem [10–13]. The burden would be potentially high in the third world for the next 10 years [6, 14, 15].
Pregnant women suffer from pregnancy-related complications [16–22]. Reproductive health is a global agendum for the last 50 years [23–26]. Despites the global efforts, reproductive health problems of women are not addressed [4, 16, 20, 27–32].
Improving maternal health is among the targets of the third Sustainable Development Goal (SDG) adopted by the international community [6]. Maternal health service is among the meanness to reduce maternal mortality ratio below 70 per 100,000 live births. But 295,000 maternal deaths were recorded due to pregnancy and child birth by the year 2017 [33]. In 2016, maternal death is the first cause of death among 15–29 years women and the second cause among reproductive age women [34].
Maternal health service includes antenatal care utilization, institutional delivery and post natal care utilization [35, 36]. Maternal health services are the corner stones to mitigate maternal and child mortality and morbidity [4, 8].
In Ethiopia, maternal mortality ratio is high (412 per 100,000 life birth) [37]. The country has reproductive strategy for the last 20 years. Maternal health services are available to the country side and included in health extension package. In the last 2 decades, maternal health service utilizations are increased in the country. But it still low [38].
Antenatal care is among the most effective interventions to mitigate maternal mortality and morbidity [39–41]. It is an entry point for delivery care, postnatal care, child, makes link between the health provider and, the client for further interventions [41–45]. During ANC pregnancy related complications, pre-existing health conditions are screened, diagnosed and appropriate interventions are delivered for pregnant women. Behavioral change communication on personal hygiene, utilization of available services and interventions are provided for the women and the family at large [39, 41, 43, 46–48].
Even though, the coverage of ANC, institutional utilization increased for the last 20 years, still it the services are public health problems [49, 50]. Although the research was conducted in the country, all the studies were done at the local level, used a small sample size, and did not consider the urban-rural difference in a country where81% of the general and 80% of female populations live in rural part of the country and 24.1% and 54.4% of urban and rural women did not attend education at all respectively. The educational inequality of maternal health service utilization is not evidenced in the country. There was trend analysis on optimal antenatal care utilization which is different from antenatal care utilization. The decomposition analysis helps to decompose inequalities in maternal health service utilization in urban-rural settings. The findings might be used to develop effective strategies to minimize the urban-rural difference in the utilization of maternal health services and to reduce educational inequalities in accessing the services. So, the study aimed to identify urban-rural variation, and educational inequalities of maternal health service utilization in Ethiopia a by using decomposition analysis.
Method
Study setting and period
This research was carried out in Ethiopia, situated in the North-eastern region of Africa. The study utilized the intermediate dataset of the Ethiopian Demographic and Health Survey (EDHS) 2019, conducted by the Central Statistical Agency in collaboration with the Federal Ministry of Health (FMoH) and the Ethiopian Public Health Institute. Data were obtained through www.dhsprogram.com after a formal request, and access was granted following approval via email. The study employed a cross-sectional design, utilizing secondary data from the 2019 intermediate Ethiopian Demography and Health Survey.
Sampling procedure
The sample for the intermediate Ethiopian Demographic and Health Survey (EDHS) 2019 underwent a two-stage stratified selection process. Initially, regions were stratified, and within each region, further stratification occurred based on urban and rural distinctions, resulting in 21 sampling strata. A total of 305 enumeration areas (94 urban and 211 rural) were chosen with a probability proportional to Enumeration Area (EA) size within each stratum. In the second stage, households were systematically sampled in proportion to each EA. The analysis included a weighted total of 3,926.7 women, as illustrated in Fig. 1.
Fig. 1.
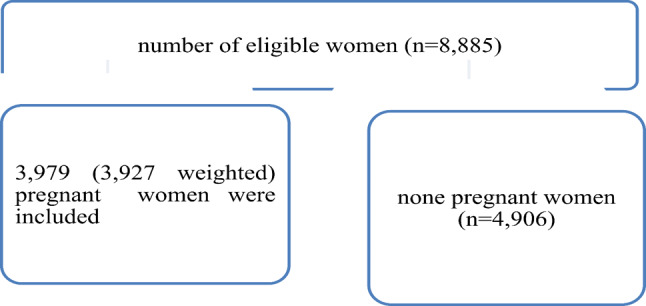
Sampling and exclusion procedures to identify the final sample size in intermediate 2019 EDHS
Study variables
The outcome variables of this study were urban-rural differences in maternal (Antenatal care, institutional delivery and postnatal care) health service utilization and educational inequality of maternal health care services utilization in Ethiopia. The independent variables include; women’s age, religion, current marital status, educational level, household wealth index, region and number of children.
Variable measurement: If a woman visited at least one ANC during her pregnancy, she was considered as having ANC follow-up and if a woman visited a health facility for follow-up within 42 days after delivery, she was considered as having postnatal follow-up [51]. Respondent’s education categorized into (no education, primary, secondary and higher education), Wealth index was classified as (poorest, poor, middle, richer and richest), parity (1, 2–4 and 5 and above), region (developed and developing). Amhara, Oromia, Tigray, SNNP, Addis Ababa and Dire Dawa are considered as developed and others as developing regions [52, 53].
Data management and analysis
Data management and statistical analyses were done by using Stata 17.0 software. Mean, median and percentages were used to describe the characteristics of the study population by area. The Pearson chi-square was used to examine whether ANC, Institutional delivery and postnatal care utilization was different in urban and rural women in Ethiopia. To explain the urban-rural disparities of ANC, institutional delivery and postnatal care among reproductive-age women, the Blinder-Oaxaca decomposition analysis was used [54]. This technique decomposes the differences in an outcome for two groups can be explained by differences in the level or distribution of the determinants of the outcome, differences in the impact of these determinants on the outcome and/or the interaction of the two [55]. The Oaxaca decomposition utilizes the high group (urban women in this study) as the reference group, weighting contrasts in attributes by the coefficients of urban women and contrasts in coefficients by the covariates of rural women. Regressions were performed for urban and rural women independently and afterward the assessed coefficients and covariates were utilized to compute the decompositions [56]. Consistent results using the different weights were thought to represent the robustness of the study outcome. The extension of the Oaxaca-Blinder method for non-linear dependent variables, Multivariate decomposition (mvdcmp) was used for detailed decomposition [57]. It is primarily intended for use in nonlinear decomposition and convenient methods for dealing with path dependency, as well as overcoming the identification problem associated with the selection of a reference category when dummy variables are included as Oaxaca. Mvdcmp determines the high-outcome group automatically and uses the low-outcome group as a reference [58].
Concentration curve and concentration index
We examined education-related inequality in ANC, institutional delivery and postnatal care utilization in Ethiopia using both concentration curve and concentration index methods. Concentration curves were used to illustrate the extent to which ANC, institutional delivery and postnatal care utilization were unequally distributed across educational levels. The concentration curve plots the cumulative percentage of the outcome variables (y-axis) against the cumulative percentage of the population, ranked by educational level, beginning with the uneducated and ending with the highest educational level (x-axis). We used three separate concentration curves to visualize the distribution of ANC, institutional delivery and postnatal care utilization by educational status. A concentration curve below the diagonal line also called the line of perfect equality indicates that outcome variables are concentrated among the highly educated, also called pro-educated inequality, whereas a curve above the diagonal line indicates that they are concentrated among the uneducated, also called pro-uneducated inequality. Furthermore, we calculated the concentration index, a summary measure of the magnitude of educational-related inequality. The concentration index ranges from − 1 to 1, with zero indicating perfect equality, negative values indicating that the outcome variable is concentrated among the uneducated and positive values indicating that it is concentrated among the educated group [59]. The concentration indices were calculated using the conindex command in Stata version17.0.
Results
Characteristics of the respondents
A total of 3,927 women participated in the analysis, comprising 1,004 from urban areas and 2,923 from rural regions. In the urban cohort, the mean age was 28.42 years (± 6.19 standard deviation), while rural dwellers had a mean age of 28.73 years (± 6.88 standard deviation). The average age at the first birth for urban participants was 20.24 years (± 4.63 standard deviation), contrasting with rural residents at 18.17 years (± 3.95 standard deviation). In terms of educational attainment, 304 individuals (29.66%) in urban areas and 1,710 individuals (58.96%) in rural areas did not receive any formal education, as indicated in Table 1.
Table 1.
Socio-demographic characteristics of pregnant women in Ethiopia, intermediate EDHS 2019
| Variable | Urban | Rural |
|---|---|---|
| Current age in years (mean) | 28.42 | 28.73 |
| Age at first birth (mean) | 20.24 | 18.17 |
| Religion | ||
| Orthodox | 396 (38.59) | 1,045 (36.02) |
| Muslim | 304 (29.59) | 1,036 (35.72) |
| Others* | 327(31.82) | 819 (28.25) |
| Educational status | ||
| No education | 304 (29.66) | 1,710 (58.96) |
| Primary | 424 (41.32) | 991 (34.16) |
| Secondary | 179 (17.46) | 165 (5.70) |
| Higher | 119 (11.56) | 34 (1.18) |
| Household Wealth index | ||
| poor | 123 (12.02) | 1524 (52.54) |
| middle | 60 (5.85) | 701 (24.18) |
| rich | 843 (82.13) | 675(23.28) |
| Marital status | ||
| Never married | 5 (0.53) | 15 (0.53) |
| Married | 933 (90.9) | 2,752 (94.88) |
| Widowed/ divorced | 88 (8.57) | 133 (4.59) |
| Parity | ||
| 1 | 281 (27.33) | 545 (18.78) |
| 2–4 | 520 (50.62) | 1,218 (41.99) |
| 5 and above | 226 (22.05) | 1,138 (39.22) |
| Region | ||
| Developing | 106 (10.35) | 229 (8.54) |
| Developed | 920 (89.65) | 2,671 (91.46) |
Urban-rural differences in the utilization of maternal health services
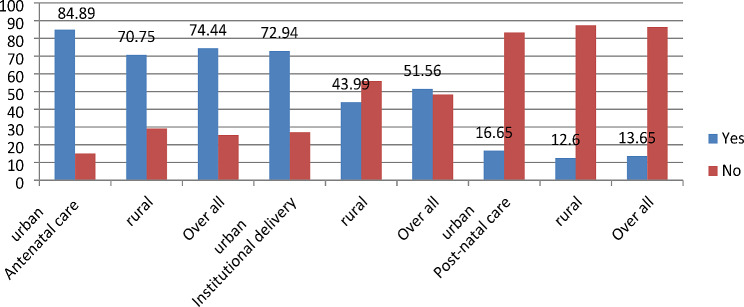
In Fig. 2, the utilization of antenatal, delivery care, and post-natal care in both urban and rural settings, as well as overall utilization in Ethiopia, is presented. The overall utilization of antenatal care stood at approximately 75%. Notably, urban residents exhibited a higher uptake at 84.89%, surpassing the 70.75% observed among rural residents. Institutional delivery accounted for 52% of births in Ethiopia, with a significant disparity between urban (73%) and rural (44%) residents (Fig. 2). The overall utilization of post-natal care in the country was approximately 14%. Chi square test indicates, both antenatal care and institutional delivery showed statistically significant differences between urban and rural dwellers, at (p-value < 0.001).
Fig. 2.
utilization antenatal care, institutional delivery and post-natal care services in Ethiopia stratified by their residency, 2019
As maternal age advances, the disparity between urban and rural areas in the utilization of antenatal care, institutional delivery, and postnatal care widens. The most substantial difference, at 36.34%, in institutional delivery was noted among women aged 35–49 years. With increasing educational attainment, the urban-rural differences in the utilization of antenatal care, institutional delivery, and postnatal care generally decrease, except for the highest educational level. Notably, the most significant difference (8.31) in postnatal care utilization was observed among women with higher educational levels, as outlined in Table 2.
Table 2.
Urban-rural difference on antenatal care, institutional delivery and postnatal care utilization in Ethiopia, 2019
| Variables | % of Antenatal care utilization | % of institutional delivery | % of post-natal care utilization | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | Deference | Urban | Rural | Deference | Urban | Rural | Deference | |
| Current age | |||||||||
| 15–19 | 69.05 | 69.12 | -0.07 | 57.62 | 56.83 | 0.79 | 21.28 | 15.43 | 5.85 |
| 20–34 | 92.00 | 70.49 | 21.51 | 74.02 | 45.65 | 28.37 | 15.64 | 12.30 | 3.34 |
| 35–49 | 85.03 | 61.93 | 23.1 | 72.78 | 36.44 | 36.34 | 19.29 | 12.75 | 6.54 |
| Age at 1st birth | |||||||||
| <= 19 | 84.92 | 68.06 | 16.86 | 65.65 | 42 | 23.65 | 13.15 | 13.73 | -0.58 |
| > 19 | 94.23 | 69.03 | 25.2 | 81.16 | 48.13 | 33.03 | 20.6 | 10.23 | 10.37 |
| Religion | |||||||||
| Orthodox | 97.83 | 82.01 | 15.82 | 85.65 | 49.99 | 35.66 | 21.42 | 15.16 | 6.26 |
| Muslim | 84.41 | 58.95 | 25.46 | 83.72 | 40.69 | 43.03 | 15.46 | 11.47 | 3.99 |
| Others* | 86.56 | 70.01 | 16.55 | 47.52 | 40.50 | 7.02 | 11.91 | 10.78 | 1.13 |
| Educational status | |||||||||
| No education | 77.94 | 59.23 | 18.71 | 53.65 | 33.28 | 20.37 | 13.44 | 10.99 | 2.45 |
| Primary | 89.59 | 79.38 | 10.21 | 74.53 | 54.25 | 20.28 | 15.59 | 13.85 | 1.74 |
| Secondary | 98.45 | 92.31 | 6.14 | 90.52 | 82.41 | 8.11 | 23.32 | 22.30 | 1.02 |
| Higher | 98.84 | 96.61 | 2.23 | 90.24 | 96.27 | -6.03 | 18.45 | 10.14 | 8.31 |
| Household Wealth index | |||||||||
| poor | 69.89 | 58.23 | 11.66 | 45.15 | 30.90 | 14.25 | 21.12 | 10.07 | 11.05 |
| middle | 60 | 79.14 | -19.14 | 23.09 | 48.48 | -25.39 | 15.35 | 15.03 | 0.32 |
| rich | 92.85 | 87.19 | 5.66 | 80.56 | 68.85 | 11.71 | 16.08 | 15.77 | 0.31 |
| Marital status | |||||||||
| Currently not married | 81.90 | 70.74 | 11.16 | 65.23 | 44.39 | 20.84 | 13.53 | 20.00 | -6.47 |
| Currently Married | 90.66 | 68.21 | 22.45 | 73.72 | 43.96 | 29.76 | 16.96 | 12.20 | 4.76 |
| Parity | |||||||||
| 1 | 92.9 | 77.45 | 15.45 | 87.90 | 66.54 | 21.36 | 12.75 | 16.79 | -4.04 |
| 2–4 | 92.13 | 71.08 | 21.05 | 72.78 | 44.01 | 28.77 | 22.00 | 11.55 | 10.45 |
| 5 and above | 76.88 | 61.2 | 15.68 | 54.78 | 33.16 | 21.62 | 9.15 | 11.72 | -2.57 |
| Region | 0 | ||||||||
| Developed | 92.49 | 75.63 | 16.86 | 74.21 | 45.78 | 28.43 | 17.38 | 13.22 | 4.16 |
| Developing | 81.78 | 57.36 | 24.42 | 61.94 | 23.05 | 38.89 | 10.44 | 5.43 | 5.01 |
| Attending antenatal care | |||||||||
| No | 25.83 | 11.32 | 14.51 | 2.59 | 3.08 | -0.49 | |||
| Yes | 81.33 | 57.49 | 23.84 | 19.11 | 16.54 | 2.57 | |||
| Institutional delivery | |||||||||
| No | 10.47 | 7.47 | 3 | ||||||
| Yes | 18.88 | 18.83 | 0.05 | ||||||
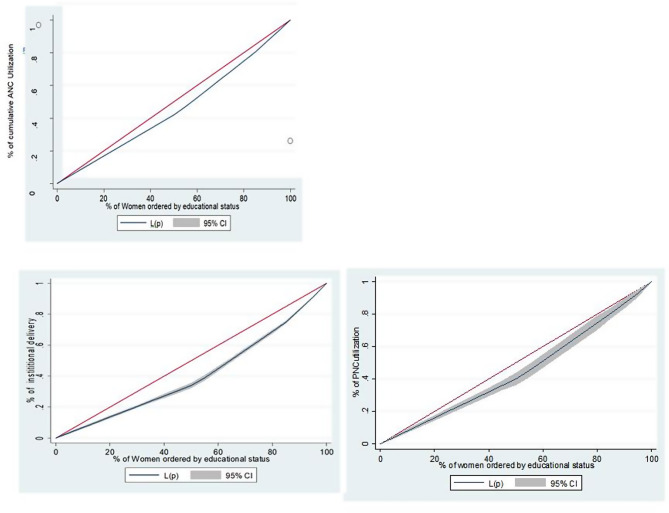
Educational inequality of maternal health service utilization
Figure 3 displays the concentration curve elucidating the distribution of antenatal care (ANC) service utilization in Ethiopia. The curve notably positions below the equality line (red dashed line), indicating a disproportionately high concentration of ANC service utilization among highly educated women. The Concentration Index (CIx) for ANC service utilization was calculated at 0.0926 (standard error: 0.0053; p < 0.00), affirming this uneven distribution of ANC utilization with educational status. Similarly, the concentration curves are situated beneath the equality line for institutional delivery and postnatal care utilization, signaling an unevenly high concentration of these services among highly educated women. The CIx values for institutional delivery and post-natal care service utilizations were 0.2137 (standard error: 0.0082; p < 0.00) and 0.1272 (standard error: 0.0232; p < 0.00), respectively.
Fig. 3.
Concentration curve of antenatal care institutional deliver and post natal care by educational status
Detailed decomposition
Statistical variations were observed in antenatal care and institutional delivery between urban and rural residents in Ethiopia, while no such disparity was found in postnatal care utilization. Of the urban-rural difference in antenatal care utilization, 83.3% could be attributed to divergences in women’s characteristics. Educational status, religion, marital status, and geographical arrangement significantly contributed to the difference in antenatal care utilization. Positive coefficients widened the gap, while negative coefficients mitigated it. Disparities in secondary and higher educational levels contributed to a 16.51% and 23.01% widening of antenatal care utilization, respectively. Urban-rural differences in marital status and living regions mitigated antenatal care utilization by -2.6% and − 1.33%, respectively. Difference in the behavior of the rural and urban women accounts about 16.7% of disparities in antenatal care utilization. However, this effect did not demonstrate statistical significance between urban and rural women.
About 76.07% of the urban-rural difference on institutional delivery was due to differences in characteristics of women. The difference of institutional delivery was significantly attributed to attending primary (3.76%), secondary (11.83%), and higher (8.44%) educational status of women, having 2 to 4 children (-6.1%), following Muslim religion (-3.62) and attending antenatal care (15.81%). Difference in the behavior of the rural and urban women accounts about 23.93% of disparities in institutional delivery utilization. However, the effect had no statistical difference between urban and rural women (Table 3).
Table 3.
Detailed decomposition antenatal care, institutional delivery and postnatal care by place of residence in Ethiopia, 2019
| Utilization of services | ANC | Delivery care | Postnatal care | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | P value | % | Coefficient | P value | % | Coefficient | P value | % | |
| Decomposition | |||||||||
| Row difference | 0.14 | < 0.001 | 0.29 | < 0.001 | 0.04 | 0.057 | |||
| Explained | 0.12 | 0.001 | 83.3 | 0.22 | < 0.001 | 76.07 | -0.05 | 0.352 | -112.37 |
| Unexplained | 0.02 | 0.623 | 16.7 | 0.07 | 0.341 | 23.93 | 0.09 | 0.128 | 212.37 |
| Endowment (Explained component) = difference in characteristics (E) | |||||||||
| Current age | |||||||||
| 15–19 | |||||||||
| 20–34 | 0.005 | 0.37 | 3.32 | 0.002 | 0.851 | 0.69 | -0.021 | 0.524 | -50.85 |
| 35–49 | 0.001 | 0.968 | 0.15 | -0.009 | 0.371 | -2.96 | 0.011 | 0.637 | 27.03 |
| Age at 1st birth | |||||||||
| <= 19 | |||||||||
| > 19 | 0.008 | 0.07 | 6.14 | 0.001 | 0.992 | 0.03 | 0.016 | 0.440 | 39.47 |
| Religion | |||||||||
| Orthodox | |||||||||
| Muslim | 0.003 | 0.215 | 2.37 | -0.01 | 0.017* | -3.62 | 0.001 | 0.961 | 0.79 |
| Others* | -0.005 | 0.001* | -3.48 | -0.009 | 0.001* | -3.14 | -0.002 | 0.577 | -5.77 |
| Educational status | |||||||||
| No education | Reference | ||||||||
| Primary | 0.002 | 0.329 | 1.52 | 0.011 | 0.028* | 3.76 | 0.002 | 0.801 | 5.09 |
| Secondary | 0.023 | 0.002* | 16.51 | 0.034 | 0.001* | 11.83 | 0.015 | 0.536 | 36.58 |
| Higher | 0.035 | < 0.001* | 23.01 | 0.024 | 0.036* | 8.44 | 0.004 | 0.793 | 9.58 |
| Household Wealth index | |||||||||
| poor | |||||||||
| middle | 0.004 | 0.656 | 2.94 | 0.01 | 0.469 | 6.89 | 0.01 | 0.767 | 25.79 |
| rich | 0.041 | 0.103 | 28.78 | 0.104 | 0.146 | 35.97 | -0.204 | 0.288 | -503.93 |
| Marital status | |||||||||
| Currently not married | Reference | ||||||||
| Currently Married | -0.003 | 0.048* | -2.60 | -0.007 | 0.068 | -2.35 | -0.001 | 0.905 | -1.42 |
| Parity | |||||||||
| 1 | Reference | ||||||||
| 2–4 | -0.005 | 0.176 | -3.79 | -0.018 | 0.014* | -6.1 | 0.022 | 0.425 | 53.86 |
| 5 and above | 0.005 | 0.566 | 3.67 | 0.032 | 0.067 | 11.28 | 0.002 | 0.958 | 4.02 |
| Region | |||||||||
| Developed | Reference | ||||||||
| Developing | -0.002 | 0.005* | -1.33 | -0.001 | 0.499 | -0.45 | -0.004 | 0.299 | -10.7 |
| Attending antenatal care | |||||||||
| No | Reference | ||||||||
| Yes | 0.045 | 0.001* | 15.81 | 0.081 | 0.502 | 200.23 | |||
| Institutional delivery | |||||||||
| No | |||||||||
| Yes | 0.027 | 0.608 | 66.08 | ||||||
| Due to Difference in Coefficients (C) | |||||||||
| Current age | |||||||||
| 15–19 | |||||||||
| 20–34 | 0.031 | 0.662 | 22.025 | 0.05 | 0.66 | 17.22 | -0.175 | 0.343 | -432.75 |
| 35–49 | -0.006 | 0.84 | -4.23 | 0.038 | 0.391 | 13.37 | -0.058 | 0.413 | -144.39 |
| Age at 1st birth | |||||||||
| <= 19 | |||||||||
| > 19 | 0.022 | 0.232 | 16.1 | -0.001 | 0.951 | -0.46 | 0.057 | 0.12 | 141.92 |
| Religion | |||||||||
| Orthodox | |||||||||
| Muslim | -0.002 | 0.908 | -1.57 | 0.05 | 0.056 | 17.42 | -0.002 | 0.955 | -4.01 |
| Others* | -0.028 | 0.259 | -19.83 | -0.051 | 0.03 | -17.73 | -0.002 | 0.934 | -5.04 |
| Educational status | |||||||||
| No education | Reference | ||||||||
| Primary | -0.015 | 0.551 | -6.75 | 0.027 | 0.288 | 9.21 | 0.006 | 0.831 | 14.99 |
| Secondary | 0.004 | 0.427 | 3.09 | 0.005 | 0.363 | 1.89 | 0.001 | 0.931 | 1.28 |
| Higher | -0.001 | 0.690 | -0.39 | -0.002 | 0.396 | -0.67 | 0.001 | 0.508 | 3.16 |
| Household Wealth index | |||||||||
| poor | |||||||||
| middle | -0.019 | 0.342 | -13.47 | -0.04 | 0.27 | -13.93 | -0.014 | 0.686 | -35.44 |
| rich | 0.001 | 0.987 | 0.11 | 0.001 | 0.976 | 0.28 | -0.056 | 0.188 | -137.71 |
| Marital status | |||||||||
| Currently not married | Reference | ||||||||
| Currently Married | -0.003 | 0.334 | -2.72 | 0.126 | 0.171 | 43.49 | -0.007 | 0.299 | -16.24 |
| Parity | |||||||||
| 1 | Reference | ||||||||
| 2–4 | -0.033 | 0.310 | -23.64 | -0.03 | 0.426 | -10.31 | 0.104 | 0.167 | 257.28 |
| 5 and above | -0.01 | 0.708 | -7.19 | -0.016 | 0.702 | -5.7 | 0 0.023 | 0.649 | 57.1 |
| Region | |||||||||
| Developed | Reference | ||||||||
| Developing | -0.001 | 0.913 | -0.24 | -0.001 | 0.9 | -0.28 | -0.004 | 0.674 | -8.76 |
| Attending antenatal care | |||||||||
| No | |||||||||
| Yes | -0.01 | 0.885 | -3.47 | 0.091 | 0.619 | 223.73 | |||
| Institutional delivery | |||||||||
| No | |||||||||
| Yes | -0.018 | 0.68 | -43.96 | ||||||
Discussion
The objective of this study was to examine the urban-rural disparities and educational inequalities in maternal health care service utilization in Ethiopia by using mini EDHS 2019.
There was a statistical disparity in urban-rural ANC utilization in Ethiopia. The finding was supported by findings from Ethiopia [60] and Indonesia [61]. Even though the prevalence of ANC is low, the utilization is higher in urban residents than rural residents in Ethiopia. The urban-rural discrepancy might be due to the availability of health facilities in urban areas [62–66], Health care facilities in rural areas are usually located centrally, making it difficult for many women in such areas to access them easily, thereby causing a low use of such services, more experts are found in urban areas [64, 67, 68]. Moreover, urban women have good knowledge and information about ANC [65, 69].
83.3% of the urban-rural difference in antenatal care utilization was due to differences in the characteristics of women. In the decomposition analysis, marital status, region, and educational level of mothers, contributed to the urban–rural disparity in antenatal care use. The finding is supported by previous findings [70, 71]. Among the compositional factors, a very significant contribution to the positive disparities of urban-rural ANC utilization was due to maternal educational status. 17.46% and 11.56% of urban residents were attending secondary and higher education, and 5.7% and 1.18% of rural residents were attending secondary and higher education respectively (Table 1). A higher proportion of women attending secondary and higher education in urban areas increase the gap in ANC utilization. The result implies that to reduce the urban rural difference, education is very important on which Ethiopia launches universal educational coverage for the last 3 decades. In comparison to urban areas, where educational opportunities may be more readily available, rural areas often face challenges in providing access to education. This can result in lower levels of education among women in rural areas, which in turn can contribute to disparities in ANC utilization. There is educational inequality (CIx = 0.0926, p < 0.001) of using ANC in Ethiopia. The finding is in line with previous findings [9, 61]. The result implies, to improve as well as to reduce inequalities of ANC utilization, education is crucial.
Marital status mitigates urban rural difference of ANC by -2.6%. That is being married increases ANC utilization. This finding is significant as it highlights the importance of addressing urban-rural disparities in marital status in order to improve access to antenatal care services. Unmarried women were less likely to utilize antenatal care services compared to married women [66, 72]. This suggests that addressing urban-rural differences in marital status could indeed have a significant impact on improving access to antenatal care.
About 76.07% of the urban-rural difference on institutional delivery was due to differences in characteristics of women. The finding is in line with [73]. Difference due to coefficients accounts for about 23.93% of disparities in institutional delivery. However, the effect had no statistical difference between urban and rural women. The variation in delivery care utilization between urban and rural areas in Ethiopia may be attributed to factors such as the lower socioeconomic status of rural women, limited access to ANC services, and limited access to media. The descriptive statistics reveal that nearly a third (71%) of pregnant women in rural areas did not receive any ANC. In contrast, 85% of women in urban areas receive at least one ANC follow-up. It is evident that wealthier women in urban areas have better access to information on maternal and child health through various media channels, which facilitates their utilization of ANC services and ultimately leads to giving birth at a healthcare facility.
Educational status difference increases the gap on institutional delivery utilization among urban and rural women in Ethiop. If rural women attend primary (3.76%)/ secondary (11.83%) and higher (8.44%) education the gap might be reduced by 3.76%, 11.83% and 8.44%. respectively the result is similar with previous study [73]. In Ethiopia, 11.56% of urban women and 1.18 of rural women were attending higher educational status (Table 1) There is educational inequality (CIx = 0.2137, p < 0.001) of using institutional delivery in Ethiopia.
The number of children mitigates the urban rural difference in institutional delivery utilization. If the number of children, the urban women had the number of rural women, institutional delivery gap might be widening by 6.1% [73, 74]. Similarly if rural women attend ANC like urban women the gap in institutional delivery might be reduced by 15.81% [73, 74]. ANC empowers women on knowledge, risk recognition and institutional delivery utilization [75–77].
Even though there was no significant urban rural difference on postnatal care utilization. There is educational inequality (CIx = 0.1272, p < 0.001) of post natal care utilization in Ethiopia. The finding is supported with previous researches [78–81]. This low utilization adversely affects maternal and child health by increasing the risk of infections, hemorrhage, and insufficient support for breastfeeding, which can lead to failure to thrive and higher neonatal mortality rates. Additionally, it can contribute to postpartum depression and other mental health challenges, resulting in prolonged suffering. Furthermore, inadequate postnatal care limits essential education on family planning, nutrition, and immunizations. Therefore, enhancing access to and the quality of postnatal care services is vital for reducing morbidity and mortality rates among mothers and infants [82].
The result of this study was more representative than other studies and the analysis shows the urban-rural difference and the source of difference on utilization of maternal health services. Despite this strength, the result may be prone to recall bias because the data were collected from a history of the event and some variables were missed since the data set was intermediate. Due to the nature of the data set, quality related data, previous exposure variables, paternal and institutional variables were not included.
Conclusion: ANC utilization and institutional delivery had a significant discrepancy in urban-rural women (urban women use the services better than the rural women). Maternal characteristics contribute more than 75% of the urban-rural difference on ANC and institutional delivery utilization. But postnatal care utilization was similarly low in urban and rural areas. There was educational inequality on ANC, institutional and postnatal care utilization in Ethiopia.
Attending, Secondary, higher, educational levels widening and living regions mitigated antenatal care utilization. Primary, secondary and higher education and antenatal care utilization were widening institutional delivery utilization. Advocacy and behavioral change communication should be area of attention for rural women to improve maternal health service utilization through health extension workers and women developmental army. Further, research is needed to have information on the effect of quality of service on maternal health service utilization.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
MA: initiated the research concept, analyze and interpreted the data; AM, AAT, AK, NK, YT AE, SDK, KM, ETA, EB, CD, LA and FDB: wrote the manuscript; all authors: critically revise, read and approved the final manuscript. All authors have equal participation.
Abbreviations
- ANC
Antenatal Care
- CSA
Central Statistics Agency
- EA
Enumeration Area
Author contributions
MA: initiated the research concept, analyze and interpreted the data; AM, AAT, AK, NK, YT AE, SDK, KM, ETA, EB, CD, LA and FDB: wrote the manuscript; all authors: critically revise, read and approved the final manuscript. All authors have equal participation.
Funding
There is no specific funding for this study.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval and consent to participate
Ethical clearance was obtained from Ethical Review Committee of Wollo University College of Medicine and Health Science. An authorization letter to download EDHS-2019 data set was also obtained from CSA after requesting www.measuredhs.comwebsite. The requested data were treated strictly confidential and was used only for the study purpose. Complete information regarding the ethical issue was available in the EDHS-2019 report.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cross S, Bell JS, Graham WJ. What you count is what you target: the implications of maternal death classification for tracking progress towards reducing maternal mortality in developing countries. Bull World Health Organ. 2010;88:147–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kassebaum NJ, Barber RM, Bhutta ZA, Dandona L, Gething PW, Hay SI, et al. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet. 2016;388(10053):1775–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNICEF, UNFPA, World Bank Group. Trends in maternal mortality: 1990–2015: estimates from WHO. and the United Nations Population Division: World Health Organization; 2015. [Google Scholar]
- 4.UNICEF, UNFPA. Trends in maternal mortality 2000 to 2017: estimates by WHO. World Bank Group and the United Nations Population Division; 2019.
- 5.Paxton A, Wardlaw T. Are we making progress in maternal mortality? Proc Natl Acad Sci USA. 2010;107(5587). [DOI] [PubMed]
- 6.Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-agency Group. Lancet. 2016;387(10017):462–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Douthard RA, Martin IK, Chapple-McGruder T, Langer A, Chang S. US maternal mortality within a global context: historical trends, current state, and future directions. J Women’s Health. 2021;30(2):168–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okonofua F. Maternal mortality in developing countries. Contemporary obstetrics and gynecology for developing countries. Springer; 2021. pp. 13–22.
- 9.Yaya S, Anjorin SS, Adedini SA. Disparities in pregnancy-related deaths: spatial and bayesian network analyses of maternal mortality ratio in 54 African countries. BMJ Global Health. 2021;6(2):e004233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayele AA, Getaye Tefera Y, East L. Ethiopia’s commitment towards achieving sustainable development goal on reduction of maternal mortality: there is a long way to go. Women’s Health. 2021;17:17455065211067073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haregu T, Alemayehu YK, Alemu YA, Medhin G, Woldegiorgis MA, Fentaye FW et al. Disparities in the implementation of the Health Extension Program in Ethiopia: doing more and better towards universal health coverage. 2021. [DOI] [PMC free article] [PubMed]
- 12.Kiross GT, Chojenta C, Barker D, Loxton D. Optimum maternal healthcare service utilization and infant mortality in Ethiopia. BMC Pregnancy Childbirth. 2021;21(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsegaye S, Yibeltal K, Zelealem H, Worku W, Demissie M, Worku A, et al. The unfinished agenda and inequality gaps in antenatal care coverage in Ethiopia. BMC Pregnancy Childbirth. 2022;22(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molokoane F, editor. Editor maternal mortality: an overview. Obstetrics and Gynaecology Forum. In House; 2021.
- 15.Ward ZJ. Computational epidemiology: methods and applications for Global Health. 2021.
- 16.Cirelli JF, Surita FG, Costa ML, Parpinelli MA, Haddad SM, Cecatti JG. The Burden of Indirect causes of maternal morbidity and mortality in the Processof Obstetric Transition: a cross-sectional Multicenter Study. Revista Brasileira De Ginecol E Obstetrícia. 2018;40(3):106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.England N, Madill J, Metcalfe A, Magee L, Cooper S, Salmon C, et al. Monitoring maternal near miss/severe maternal morbidity: a systematic review of global practices. PLoS ONE. 2020;15(5):e0233697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Filippi V, Chou D, Barreix M, Say L, Group WMMW, Barbour K, et al. A new conceptual framework for maternal morbidity. Int J Gynecol Obstet. 2018;141:4–9. [Google Scholar]
- 19.Geller SE, Koch AR, Garland CE, MacDonald EJ, Storey F, Lawton B. A global view of severe maternal morbidity: moving beyond maternal mortality. Reproductive Health. 2018;15(1):31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Say L, Chou D, Group WMMW, Barbour K, Barreix M, Cecatti JG, et al. Maternal morbidity: time for reflection, recognition, and action. Wiley Online Library 2018. [DOI] [PMC free article] [PubMed]
- 21.Small MJ, Allen TK, Brown HL, editors. Global disparities in maternal morbidity and mortality. Seminars in perinatology. Elsevier; 2017. [DOI] [PMC free article] [PubMed]
- 22.Tura AK, Trang TL, Van Den Akker T, Van Roosmalen J, Scherjon S, Zwart J, et al. Applicability of the WHO maternal near miss tool in sub-saharan Africa: a systematic review. BMC Pregnancy Childbirth. 2019;19(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yamey G, Shretta R, Binka FN. The 2030 sustainable development goal for health. British Medical Journal Publishing Group; 2014. [DOI] [PubMed]
- 24.Organization WH. Millennium development goals. 2008.
- 25.Cohen SA, Richards CL. The Cairo consensus: population, development and women. Fam Plan Perspect. 1994;26(6):272–7. [PubMed] [Google Scholar]
- 26.WHO. Department of Reproductive Health and Research, including UNDP/UNFPA/WHO/World. Bank Special Programme of Research, Development and Research Training in Human Reproduction annual technical report. World Health Organization, 2001.
- 27.Boerma T, Requejo J, Victora CG, Amouzou A, George A, Agyepong I, et al. Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet. 2018;391(10129):1538–48. [DOI] [PubMed] [Google Scholar]
- 28.Chowdhury MAB, Adnan MM, Hassan MZ. Trends, prevalence and risk factors of overweight and obesity among women of reproductive age in Bangladesh: a pooled analysis of five national cross-sectional surveys. BMJ open. 2018;8(7):e018468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wirth JP, Woodruff BA, Engle-Stone R, Namaste SM, Temple VJ, Petry N, et al. Predictors of anemia in women of reproductive age: biomarkers reflecting inflammation and nutritional determinants of Anemia (BRINDA) project. Am J Clin Nutr. 2017;106(suppl1):S416–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woog V, Kågesten A. The sexual and reproductive health needs of very young adolescents aged 10–14 in developing countries: what does the evidence show. New York: Guttmacher Institute; 2017. [Google Scholar]
- 31.WHO. Maternal mortality measurement: guidance to improve national reporting. World Health Organization; 2022.
- 32.Ozimek JA, Kilpatrick SJ. Maternal mortality in the twenty-first century. Obstet Gynecol Clin. 2018;45(2):175–86. [DOI] [PubMed] [Google Scholar]
- 33.WHO. World health statistics 2019: monitoring health for the SDGs. sustainable development goals: World Health Organization; 2019. [Google Scholar]
- 34.Organization WH. World health statistics 2016: monitoring health for the SDGs sustainable development goals. World Health Organization; 2016.
- 35.Banke-Thomas A, Ayomoh FI, Abejirinde I-OO, Banke-Thomas O, Eboreime EA, Ameh CA. Cost of utilising maternal health services in low and middle-income countries: a systematic review. Int J Health Policy Manage. 2021;10(9):564–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, McLemore MR, Neilson E, Wallace M. Social and structural determinants of health inequities in maternal health. J Women’s Health. 2021;30(2):230–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tamirat KS, Sisay MM. Full immunization coverage and its associated factors among children aged 12–23 months in Ethiopia: further analysis from the 2016 Ethiopia demographic and health survey. BMC Public Health. 2019;19(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tekile AK, Woya AA, Basha GW. Prevalence of malnutrition and associated factors among under-five children in Ethiopia: evidence from the 2016 Ethiopia demographic and Health Survey. BMC Res Notes. 2019;12(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Masi S, Bucagu M, Tunçalp Ö, Peña-Rosas JP, Lawrie T, Oladapo OT, et al. Integrated person-centered health care for all women during pregnancy: implementing World Health Organization recommendations on antenatal care for a positive pregnancy experience. Global Health: Sci Pract. 2017;5(2):197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Langlois EV, Tunçalp Ö, Norris SL, Askew I, Ghaffar A. Qualitative evidence to improve guidelines and health decision-making. Bull World Health Organ. 2018;96(2):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO. WHO recommendations on intrapartum care for a positive childbirth experience. World Health Organization; 2018. [PubMed]
- 42.Haddad SM, Souza RT, Cecatti JG, Barreix M, Tamrat T, Footitt C, et al. Building a Digital Tool for the Adoption of the World Health Organization’s Antenatal Care recommendations: methodological intersection of evidence, clinical logic, and Digital Technology. J Med Internet Res. 2020;22(10):e16355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehl G, Tunçalp Ö, Ratanaprayul N, Tamrat T, Barreix M, Lowrance D, et al. WHO SMART guidelines: optimising country-level use of guideline recommendations in the digital age. Lancet Digit Health. 2021;3(4):e213–6. [DOI] [PubMed] [Google Scholar]
- 44.Noij F. UNFPA CAMBODIA Country Programme Review Fifth Programme Cycle, 2016–2018 Review Report. September 2017.
- 45.WHO. WHO antenatal care recommendations for a positive pregnancy experience: nutritional interventions update: vitamin D supplements during pregnancy. 2020. [PubMed]
- 46.Homer CS, Oats J, Middleton P, Ramson J, Diplock S. Updated clinical practice guidelines on pregnancy care. Med J Aust. 2018;209(9):409–12. [DOI] [PubMed] [Google Scholar]
- 47.Sudfeld CR, Smith ER. New evidence should inform WHO guidelines on multiple micronutrient supplementation in pregnancy. J Nutr. 2019;149(3):359–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Waller A, Bryant J, Cameron E, Galal M, Symonds I, Sanson-Fisher R. Screening for recommended antenatal risk factors: how long does it take? Women Birth. 2018;31(6):489–95. [DOI] [PubMed] [Google Scholar]
- 49.Muluneh AG, Kassa GM, Alemayehu GA, Merid MW. High dropout rate from maternity continuum of care after antenatal care booking and its associated factors among reproductive age women in Ethiopia, evidence from demographic and Health Survey 2016. PLoS ONE. 2020;15(6):e0234741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Worku D, Teshome D, Tiruneh C, Teshome A, Berihun G, Berhanu L, et al. Antenatal care dropout and associated factors among mothers delivering in public health facilities of dire Dawa Town, Eastern Ethiopia. BMC Pregnancy Childbirth. 2021;21(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.WHO. Global guidance on criteria and processes for validation: elimination of mother-to-child transmission of HIV and Syphilis. World Health Organization; 2017.
- 52.Kefale B, Damtie Y, Yalew M, Adane B, Arefaynie M. Predictors of comprehensive knowledge of HIV/AIDS among people aged 15–49 years in Ethiopia: a multilevel analysis. HIV/AIDS-Research and Palliative Care. 2020:449 – 56. [DOI] [PMC free article] [PubMed]
- 53.The Federal Democratic Republic of Ethiopia. Council of Ministers Regulation 103/2004. The Council of Ministers Regulation for the establishment of Federal Board to provide affirmative support for less developed regions. Fed Negarit Gazeta. 2004; 2634–5.
- 54.Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev. 1973:693–709.
- 55.Reimers CW. Labor market discrimination against Hispanic and black men. The review of economics and statistics. 1983:570-9.
- 56.Powers DA, Yoshioka H, Yun M-S, mvdcmp. Multivariate decomposition for nonlinear response models. Stata J. 2011;11(4):556–76. [Google Scholar]
- 57.Yun M-S. Decomposing differences in the first moment. Econ Lett. 2004;82(2):275–80. [Google Scholar]
- 58.Yun M-S. Identification problem and detailed Oaxaca decomposition: a general solution and inference. J Econ Soc Meas. 2008;33(1):27–38. [Google Scholar]
- 59.Wagstaff A, O’Donnell O, Van Doorslaer E, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation. World Bank; 2007.
- 60.Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2019;14(4):e0214848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wulandari RD, Laksono AD, Rohmah N. Urban-rural disparities of antenatal care in South East Asia: a case study in the Philippines and Indonesia. BMC Public Health. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Woldemichael A, Takian A, Akbari Sari A, Olyaeemanesh A. Availability and inequality in accessibility of health centre-based primary healthcare in Ethiopia. PLoS ONE. 2019;14(3):e0213896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Damtew D, Worku F, Tesfaye Y, Jemal A. Availability of lifesaving maternal and child health commodities and associated factors in public and private health facilities of Addis Ababa, Ethiopia. Health Serv Res Managerial Epidemiol. 2019;6:2333392819892350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Defar A, Getachew T, Taye G, Tadele T, Getnet M, Shumet T, et al. Quality antenatal care services delivery at health facilities of Ethiopia, assessment of the structure/input of care setting. BMC Health Serv Res. 2020;20:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Basha GW. Factors affecting the utilization of a minimum of four antenatal care services in Ethiopia. Obstetrics and Gynecology International. 2019;2019. [DOI] [PMC free article] [PubMed]
- 66.Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cameron L, Contreras Suarez D, Cornwell K. Understanding the determinants of maternal mortality: an observational study using the Indonesian Population Census. PLoS ONE. 2019;14(6):e0217386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dahab R, Sakellariou D. Barriers to accessing maternal care in low income countries in Africa: a systematic review. Int J Environ Res Public Health. 2020;17(12):4292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tiruaynet K, Muchie KF. Determinants of utilization of antenatal care services in Benishangul Gumuz Region, Western Ethiopia: a study based on demographic and health survey. BMC Pregnancy Childbirth. 2019;19(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Samuel O, Zewotir T, North D. Decomposing the urban–rural inequalities in the utilisation of maternal health care services: evidence from 27 selected countries in Sub-saharan Africa. Reproductive Health. 2021;18(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mahabub-Ul-Anwar, Rob U, Talukder N. Inequalities in maternal health care utilization in rural Bangladesh. Int Q Community Health Educ. 2008;27(4):281–97. [DOI] [PubMed] [Google Scholar]
- 72.Tsegaye B, Ayalew M. Prevalence and factors associated with antenatal care utilization in Ethiopia: an evidence from demographic health survey 2016. BMC Pregnancy Childbirth. 2020;20(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mesfin M, Farrow J. Determinants of antenatal care utilization in Arsi Zone, Central Ethiopia. Ethiop J Health Dev. 1996;10(3).
- 74.Abosse Z, Woldie M, Ololo S. Factors influencing antenatal care service utilization in hadiya zone. Ethiop J Health Sci. 2010;20(2). [DOI] [PMC free article] [PubMed]
- 75.Odo D, Shifti D. Institutional delivery service utilization and associated factors among child bearing age women in Goba Woreda, Ethiopia. J Gynecol Obstet. 2014;2(4):63–70. [Google Scholar]
- 76.Rurangirwa AA, Mogren I, Nyirazinyoye L, Ntaganira J, Krantz G. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregnancy Childbirth. 2017;17(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sharma A, Thakur PS, Tiwari R, Sharma R. Utilization of antenatal care services in tribal area of Madhya Pradesh: a community based cross sectional study. Int J Community Med Public Health. 2019;6(6):2465. [Google Scholar]
- 78.Tesfaye G, Chojenta C, Smith R, Loxton D. Application of the Andersen-Newman model of health care utilization to understand antenatal care use in Kersa District, Eastern Ethiopia. PLoS ONE. 2018;13(12):e0208729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Terefe AN, Gelaw AB. Determinants of antenatal care visit utilization of child-bearing mothers in Kaffa, Sheka, and Bench Maji Zones of SNNPR, Southwestern Ethiopia. Health Serv Res Managerial Epidemiol. 2019;6:2333392819866620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tsegay Y, Gebrehiwot T, Goicolea I, Edin K, Lemma H, San Sebastian M. Determinants of antenatal and delivery care utilization in Tigray region, Ethiopia: a cross-sectional study. Int J Equity Health. 2013;12(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tegegne TK, Chojenta C, Getachew T, Smith R, Loxton D. Antenatal care use in Ethiopia: a spatial and multilevel analysis. BMC Pregnancy Childbirth. 2019;19(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shirina Akter Mosa M, Al A, Pasa M, Bharati P, Hossain M. Factors associated with utilization of antenatal care service in Bangladesh: a country based cross-sectional study. Genus. 2021;5.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.