Abstract
Background
Depression is the most common psychological phenomenon among caregivers of children with Cleft Lip and/or Palate and affects the quality of life, treatment satisfaction, children’s self-esteem and parent–child relationship. However, Existing studies have limited explanations for the mechanisms that lead to depression in caregivers of children with Cleft Lip and/or Palate. The present study aimed to identify factors influencing depression among caregivers of children with Cleft Lip and/or Palate and to provide a reference point and new ideas for future research.
Methods
This cross-sectional study investigated 248 caregivers at two Cleft Lip and/or Palate treatment centers in China, spanning from April 2019 to July 2020. The diathesis-stress model was used to construct the model, and data analysis was conducted using SPSS 26.0 and AMOS 25.0. Path analysis was employed to test the hypothetical model, and the fit of the model was evaluated using Chi-Square/degree of freedom, Goodness-of-Fit Index, Normed Fit Index, Relative Fit Index, Incremental Fit Index, Tacker-Lewis Index, Comparative Fit Index and Root Mean Square Error of Approximation.
Results
The study found that the average level of depression among caregivers of children with Cleft Lip and/or Palate was 4.83 (4.79). Additionally, 43.5% of caregivers exhibited depressive symptoms. The fit of the modified path model was found to be satisfactory, with the following indices: Chi-Square/degree of freedom = 1.881, Goodness-of-Fit Index = 0.986, Normed Fit Index = 0.973, Relative Fit Index = 0.919, Incremental Fit Index = 0.987, Tucker-Lewis Index = 0.960, Comparative Fit Index = 0.987, and Root Mean Square Error of Approximation (RMSEA) = 0.060. The results indicated that parenting stress had the greatest direct impact on depression, followed by hope. Indirect effects on depression were observed for optimism, resilience, and coping, which were mediated through perceived social support and parenting stress.
Conclusions
This study suggests that depression in caregivers of children with Cleft Lip and/or Palate was leadingly influenced by parenting stress and hope. Strategies aimed at the key factors are expected to decrease depression.
Keywords: Depression, Parenting stress, Path analysis, Cleft lip and/or palate, Caregivers
Background
Cleft Lip and/or Palate (CL/P) is the most common congenital developmental defect of the oral and maxillofacial region, which is caused by pathogenic factors that lead to the failure of embryonic development to form normal physiological structures of the lip and palate, thus manifesting as unilateral or bilateral cleft upper lip and palate, nasal collapse, alveolar bone loss, tooth and jaw misalignment and craniomaxillofacial deformities [1]. Statistics show that the average incidence of CL/P worldwide is 1 per 1,000 [2, 3]. China has one of the largest numbers of children with CL/P in the world, with an incidence of 1.4‰ [4]. CL/P not only affects the child’s appearance, swallowing and voice functions [5], but also causes low self-esteem, loneliness, anxiety and depression, affecting the child’s quality of life [6].
Caregivers, as key roles in parenting, are involved in the entire process of treating children with CL/P. Caregivers need assistance with biomedical, physical development, rehabilitation, psychological and family issues, as well as managing the social, economic and emotional challenges that accompany cleft lip disease [7]. Heavy childcare tasks create a wide range of psychological problems for caregivers of children with CL/P. The treatment process for CL/P patients is closely related to the psychological adjustment and adaptation of the parents, and the influence of the caregiver on the child is unquestionable. Studies have shown that the mental health of caregivers directly affects the physical and mental health, social behavior, educational achievement, and personality formation of children with CL/P [8], as well as the harmony and family functioning of the entire family [9]. Therefore, the mental health status of caregivers of children with CL/P cannot be ignored.
Caregivers raising a child with CL/P are often accompanied by psychological phenomena such as self-blame, guilt, sadness, worry, anxiety, depression, panic, anger, and feelings of insanity [10]. Studies show that depression and anxiety are among the most common psychological consequences [11, 12], ranging from 52 to 94% among family caregivers [13]. Even caregivers may have higher levels of depression than the patients themselves [14]. As one of the most common psychological problems among caregivers of children with CL/P, depression has a significant impact on caregivers’ quality of life, treatment satisfaction, children’s self-esteem, gender identity, and parent–child relationship building [15, 16].
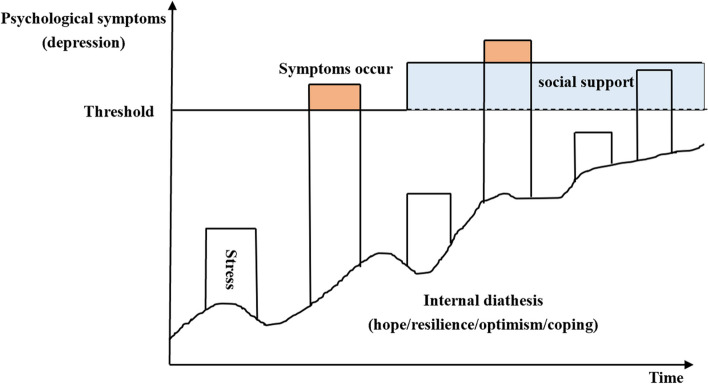
Based on the diathesis-stress theoretical model (Fig. 1), the arisen of depression consists of two main components: internal diathesis and stressful events. Internal diathesis is stable, developmental, foundational and implicit, mainly referring to perceptions, hopes, attribution styles, coping styles, etc. In the process of depression, there are three relationships between stress and diathesis in this model. First, diathesis and stress together constitute the necessary conditions for depression to arise. Intrinsic diathesis increases the likelihood of stress generation. The second relationship is that diathesis is the only necessary condition for depression. Stress is a less influencing factor and is a consequence of diathesis. The third relationship is that the only necessary condition for depression to occur is stress. It is worth noting, the threshold of psychological symptoms in the diathesis-stress model is also influenced by the received support and resources [17]. The loss or acquisition of resources is an important mechanism that drives the stress response [18]. In the study of parents of children with intellectual disabilities, it was found that perceived social support was a protective factor for reduced parenting stress [19] and depression [20]. However, the relationship between internal diathesis, stress and support in the depressive symptoms of caregivers of children with CL/P has not been proven, and the current research is still heavily patient-centered. Hope, resilience, optimism and coping are fundamental source of strength and inner guidance for caregivers [21]. Therefore, it was hypothesized in this study that caregiver-specific internal diathesis (including hope, optimism, resilience, and coping), parenting stress, and perceived social support of children with CL/P would influence caregiver depressive symptoms, while internal diathesis and perceived social support would in turn influence caregiver parenting stress.
Fig. 1.
The diathesis-stress model in this study
Reviewing previous studies, the interactions between each internal diathesis (including hope, optimism, resilience and coping style) and support among caregivers of children with CL/P were also hypothesized and refined in this study. In a survey of mother caregivers of individual with Down syndrome, it was noted that hope and resilience were positively associated to social support [22]. Slattery, McMahon [23] indicated that higher levels of optimism predicted greater positive reappraisal and social support parents of children with developmental disabilities. The level of optimism in caregivers of people with Alzheimer also affects social support [24]. Hope is negatively correlated with coping dysfunctions [21] and coping increased as hope increased in family caregivers of persons living with chronic illness [25]. The level of resilience in primary caregivers of elderly maintenance hemodialysis can affect their positive coping style [26]. Caregiver resilience also has a direct impact on hope levels [27, 28]. In a study of fathers and mothers of children with CL/P, optimism and hope were positively correlated [29], with optimists seizing all potential opportunities and working hard with hope and confidence. Peer and Hillman [30] conducted a systematic review of research article databases and found optimism as resilience factors for parents of children with intellectual and/or developmental disabilities.
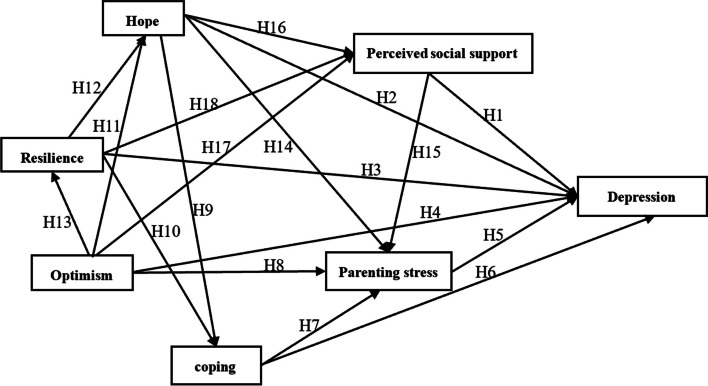
In summary, based on the diathesis-stress model and previous studies, this research aimed to identify factors influencing the depression of caregivers of children with CL/P, and the detailed hypothetical paths and initial model were illustrated in Fig. 2.
Fig. 2.
Path diagram for the hypothetical model. H1: perceived social support decrease depression; H2: hope decrease depression; H3: resilience decrease depression; H4: optimism decrease depression; H5: parenting stress increase depression; H6: coping decrease depression; H7: coping decrease parenting stress; H8: optimism decrease depression; H9: hope increase coping; H10: resilience increase coping; H11: optimism increase hope; H12: resilience increase hope; H13: optimism increase resilience; H14: hope decrease parenting stress; H15: perceived social support decrease parenting stress; H16: hope increase social support; H17: optimism increase perceived social support; H18: resilience increase perceived social support
Methods
Study design and participants
This study employed a cross-sectional design and utilized pathway analysis. It was conducted at two CL/P treatment centers in China, spanning from April 2019 to July 2020. Path analysis is a form of structural equation model that utilizes a path diagram to evaluate the causal relationship between a dependent variable and two or more dependent variables. The main purpose of path analysis is to assess the accuracy and reliability of a hypothetical causal model, as well as to quantify the strength of the causal relationship between variables. Primary caregivers of children with CL/P receiving management in two Chinese hospitals were recruited and interviewed using a convenience sampling method. The specific inclusion criteria were as follows: (1) caregivers referred to fathers or mothers who have taken care of the child with CL/P for at least 3 months. (2) Primary caregivers of children under 18 years of age with non-syndromic cleft lip and/or palate. (2) Children were being managed at the treatment centers including surgery, voice training, orthodontic treatment, etc., with no other serious medical conditions. (3) Caregivers were able to understand and cooperate with the completion of the questionnaire. Caregivers with other care assignments and comorbid other serious illnesses were excluded. This study adhered to the guidelines for Strengthening the Reporting of Observational Studies in Epidemiology.
Two methods were used to determine the sample size in this study. (1) According to the calculation formula of cross-sectional study:
To calculate the final sample size, we can use the following formula: α = 0.05; Zα = 1.96; σ = 15.39; δ = 2. By substituting these values into the formula, we get n = 1.962*15.392/22 = 227.47. Therefore, to account for a no-response rate of 10% ~ 20%, the recommended sample size should be 248–270. (2) Based on the number of free estimated parameter: Jackson [31] and Bentler and Chou [32] stated that to avoid overfitting due to a small sample size, structural equation modeling should require a sample size of at least 10 times the estimated parameters. According to the hypothetical model of this study, there were 18 free parameters that need to be estimated. Therefore, a minimum sample size of 180 was required. Also considering a 10%-20% non-response rate, the sample size should be between 198–216. Combining the above two methods, the sample size is taken to be the larger range of 248 ~ 270.
Data collection
This study used a questionnaire method to collect data. Trained investigators used uniform instruction to detail the content and purpose of this study to participants. Information received for this study was strictly confidential. After the caregiver agreed to participate in the study and signed the informed consent form, the investigator distributed the questionnaire on the spot. Each participant took 20 ~ 30 min to complete the questionnaires. Participants can always ask questions during the questionnaire response, and the respondent will answer them immediately. After filling out the questionnaire, investigators checked whether there were any missing items and ensured that the questionnaires were returned after the answers were complete.
Measures
Demographic characteristics
Demographic material included caregiver personal information: caregiver category, age, and education level; general information about the child: gender, age, developmental condition, types of diseases, and family profile: family history, income monthly.
Patient Health Questionnaire (PHQ-9)
The PHQ-9 was developed by Columbia University in the mid-1990s based on the DSM-IV. This scale has been translated into multiple languages and has demonstrated good reliability and validity across various populations [33, 34]. The depression status of caregivers of children with CL/P was assessed using the Chinese version of the PHQ-9 in this study [35]. The scale consists of nine items, each scored on a scale of 0 (not at all) to 3 (almost every day). The total score can range from 0 to 27 points, and the severity of depression is classified as none (1–4 points), mild (5–9 points), moderate (10–14 points), moderately severe (15–19 points), and severe (20–27 points). In the current study, the Cronbach’s α coefficient was found to be 0.893.
Herth Hope Index (HHI)
This study utilized the Chinese version of the HHI [36] evaluate the hope level of caregivers of children with CL/P. The scale comprises of 12 items categorized into 3 dimensions: temporality and future, positive readiness and expectancy, and interconnectedness. A 4-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree’ with scores of 1 to 4 was employed. The total score ranges from 12 to 48 points, with higher scores indicating a higher level of hope. The Chinese version of the HHI is widely utilized within the caregiver community and demonstrates good reliability and validity [37]. In this study, the Cronbach’s α coefficient was calculated to be 0.854.
Revised Life Orientation Test (LOT-R)
The Life Orientation Test-Revised (LOT-R) [38] was utilized to evaluate the optimistic personality traits of caregivers responsible for children with CL/P. The scale consists of a total of 10 items, comprising 3 items related to positive expectations, 3 items related to negative expectations, and 4 other questions that are somewhat ambiguous. Each item is rated on a scale ranging from ‘strongly disagree (1 point)’ to ‘strongly agree (5 points)’. The overall score of the scale falls within the range of 10 to 50 points, with a higher score indicating a greater degree of optimism. The LOT-R has demonstrated good reliability and validity within the Chinese population [39]. In the present study, the Cronbach’s α coefficient was calculated to be 0.600, indicating an acceptable level of internal consistency.
Resilience Scale-14 (RS-14)
The resilience of caregivers of children with CL/P was assessed using the RS-14 scale [40], which consists of two dimensions: ‘personal ability’ (10 items) and ‘positive cognition’ (4 items), making a total of 14 items. Each item is rated on a 7-point scale, ranging from 1 (not at all) to 7 (completely). The total score of the scale ranges from 14 to 98 points, with higher scores indicating greater levels of resilience in caregivers. The RS-14 scale has demonstrated good reliability and validity in the Chinese population [41], with a Cronbach’s α coefficient of 0.901 in this study.
Multidimensional Scale of Perceived Social Support (MSPSS)
The MSPSS [42] is a self-report questionnaire used to measure the social support functions. In this study, the Chinese version of MSPSS was employed to assess the perceived social support among caregivers of children with cleft lip and/or palate. The scale comprises three dimensions: family support, friend support, and other support, with a total of 12 items. A 7-point Likert scale ranging from ‘strongly disagree’ (1 point) to ‘strongly agree’ (7 points) was used. The total score of the scale ranges from 12 to 84 points, with a higher score indicating a higher level of social support. The MSPSS has demonstrated good reliability and validity among the Chinese population [39, 43]. In the current study, the Cronbach’s α coefficient was found to be 0.928.
Coping Health Inventory for Parents (CHIP)
The CHIP (Coping Health Inventory for Parents) [44] is a tool used to measure the coping methods employed by parents in maintaining a normal family life when they have a child with a chronic disease. In this study, the Chinese version of the CHIP was utilized to assess the coping styles of caregivers of children with CL/P (cleft lip and/or palate). The scale consists of 45 items divided into 3 dimensions, and each item is rated on a 5-point Likert scale. The total score on the scale ranges from 45 to 225, with higher scores indicating a more positive caregiver coping style. The Chinese version of the CHIP has been widely used among caregivers [45]. In this particular study, the Cronbach’s α coefficient was calculated to be 0.940.
Parenting Stress Index-Short Form (PSI-SF)
The parenting stress of caregivers was assessed using the Chinese version of the PSI-SF [46]. The scale comprises three dimensions: parenting distress, parent–child dysfunctional interaction, and difficult child, with a total of 36 items. A 5-point Likert scale ranging from ‘strongly disagree (1)’ to ‘strongly agree (5)’ was used. The total score of the scale ranges from 36 to 180 points, with higher scores indicating more stressful childcare. The Cronbach’s α coefficient for this study was calculated as 0.940.
Statistical analysis
Descriptive statistics and Pearson correlation analysis were conducted using SPSS 26.0 to examine the relationship between demographic variables and scale scores. A significance level of 0.05 (2-tailed) was used for all statistical tests. Path analysis was performed using Amos 25.0 to verify the hypothetical model. The standardization coefficient greater than 1 in the path analysis indicates the collinearity. Mahalanobis distance and the chi-square critical value were used to assess outliers. The normality of the major variables in the study model was confirmed by examining skewness and kurtosis coefficients. Shapiro–Wilk test (S-W test) was used to perform multivariate normal distribution with the help of Normaltest_v1.0 (SPSS 26.0 macro for univariate and multivariate normality test). Associations and predictions were validated through maximum likelihood estimates (MLE). Additionally, a good model was indicated by the following criteria: Chi-Square/degree of freedom (χ2/df) < 2, Goodness-of-Fit Index (GFI) > 0.9, Normed Fit Index (NFI) > 0.9, Relative Fit Index (RFI) > 0.9, Incremental Fit Index (IFI) > 0.9, Tacker-Lewis Index (TLI) > 0.9, Comparative Fit Index (CFI) > 0.9, and Root Mean Square Error of Approximation (RMSEA) < 0.08.
Results
General characteristics of participants
A total of 262 questionnaires were distributed, and 255 of them were returned, with a recovery rate of 97.33%. Among them, 248 questionnaires were considered valid with an effective recovery of 97.25%. Demographic characteristics of caregivers and children with CL/P were showed in Table 1. In the final data obtained, caregivers of children with cleft lip and palate were all fathers or mothers. The primary caregivers were mothers (n = 179; 72.2%). A majority of caregivers were 26 ~ 45 years old, accounting for 81.5%. More than half of the caregivers have junior high school and below (n = 130; 52.4%). The mean age of children with CL/P was 7.70 (5.76), with 136 males (52.4%) and 112 females (45.2%). Most of children had normal development condition (n = 202; 81.5%) and nearly half of children were diagnosed as cleft lip and palate. Only 13 cases (5.2%) had family history and less than one-third of households had an average monthly income of more than 5,000 yuan.
Table 1.
Characteristics of caregivers and children with CL/P (N = 248)
| Characteristic | Group | n (%) or Mean (SD) |
|---|---|---|
| Primary caregivers | Fathers | 67 (27.8) |
| Mothers | 179 (72.2) | |
| Age of caregivers (years) | < 25 | 13 (5.2) |
| 26–45 | 202 (81.5) | |
| > 46 | 33 (13.3) | |
| Education of caregivers | Junior high school and below | 130 (52.4) |
| High school or junior college | 56 (22.6) | |
| University and above | 62 (25.0) | |
| Sex of children | Male | 136 (54.8) |
| Female | 112 (45.2) | |
| Age of children (years) | 7.70(5.76) | |
| Development of children | Slower | 37 (14.9) |
| Normal | 202 (81.5) | |
| Faster | 9 (3.6) | |
| Types of diseases | Cleft lip | 53 (21.4) |
| Cleft palate | 77 (31.0) | |
| Cleft lip and palate | 118 (47.6) | |
| Family history | Yes | 13 (5.2) |
| No | 235 (94.8) | |
| Income monthly (¥) | < 3000 | 95 (38.3) |
| 3000–5000 | 101 (40.7) | |
| > 5000 | 52 (21.0) |
Descriptive statistics, correlations, normality and multi-normality of study variables
In this study, the standardized coefficients were all less than 1, so there was no collinearity. The Mahalanobis distance were all less than the chi-square critical value of 18.55 (fx = CHIINV(0.005,6)) and there were no outliers. The scores of hope, optimistic, resilience, social support, coping and depression, correlation, kurtosis, skewness and S-W test were shown in Table 2. The average score of depression for caregivers of children with CL/P was 4.83 (4.79). Among the 248 caregivers, 108 (43.5%) had depressive symptoms (≥ 5 points). Mildly depressed ((5 ~ 9points) caregivers were 78 (31.5%). There was a significant positive correlation (p < 0.001) between parenting stress and depression. Among caregivers of children with CL/P, hope, resilience, optimism, social support, and coping showed significant negative correlations (p < 0.001) with depression. According to Kline’s criteria [47], the absolute value of the skewness coefficient for each variable in this study is less than 3, and the absolute value of the kurtosis coefficient is less than 8. This indicates that the variables follow a normal distribution. The S-W statistical test showed an MVW value of 0.9665 and a P-value of 0.9997 (> 0.05). This suggested that the multivariable data conformed to a multivariate normal distribution which is a prerequisite for constructing the path model.
Table 2.
Correlation relationships, normality, multi-normality and scores between hope, optimistic, resilience, social support, coping and parenting stress
| Variable | Mean (SD) | Kurtosis | Skewness | Depression | Hope | Optimistic | Resilience | Social support | Coping |
|---|---|---|---|---|---|---|---|---|---|
| Depression | 4.83 (4.79) | 2.299 | 1.443 | 1 | |||||
| Hope | 39.04 (4.68) | -0.144 | 0.062 | -0.435*** | 1 | ||||
| Optimistic | 16.60 (2.72) | -0.116 | 0.154 | -0.221*** | 0.376*** | 1 | |||
| Resilience | 75.42 (14.34) | 1.310 | -0.764 | -0.339*** | 0.479*** | 0.236*** | 1 | ||
| Social support | 64.04 (12.49) | 0.114 | -0.428 | -0.341*** | 0.490*** | 0.318*** | 0.397*** | 1 | |
| Coping | 168.54 (25.10) | -0.325 | 0.224 | -0.252** | 0.477*** | 0.186** | 0.387*** | 0.390*** | 1 |
| Parenting stress | 84.37 (21.67) | -0.412 | 0.010 | 0.544*** | -0.542*** | -0.373*** | -0.360*** | -0.455*** | -0.401*** |
| S-W test | MVW | P | |||||||
| 0.9665 | 0.9997 |
**P < 0.01
***P < 0.001
Path analysis
Modified fitting results and evaluation
According to diathesis-stress model and previous studies, hope, optimism, resilience, perceived social support, coping and parenting stress among caregivers of children with CL/P were considered into path analysis to further explore the role path and effectiveness of each variable to depression. The fit index of the hypothetical path model (Fig. 2) was as follow: χ2/df = 2.698, GFI = 0.991, NFI = 0.983, RFI = 0.884, IFI = 0.990, TLI = 0.924, CFI = 0.989, RMSEA = 0.083. The significance of regression coefficients and Modification Index (MI) were initially considered to modify this model. The MI (> 4) showed that it is needed to establish the correlation of residuals among coping and perceived social support. However, one of the assumptions underlying structural equation model is that residuals are independent, and it is not possible to connect residual correlations arbitrarily. Therefore, this study finally relies on the significance of regression coefficient to modify.
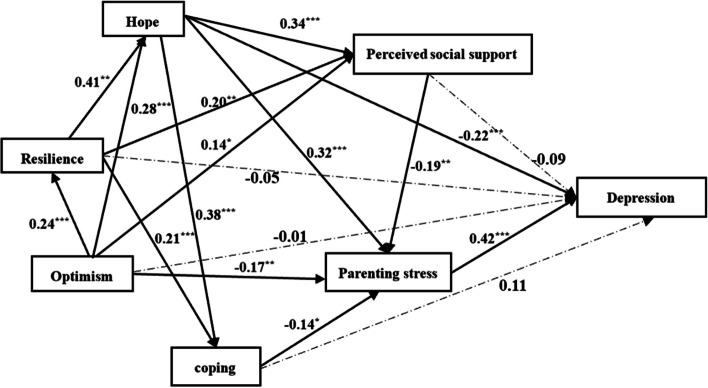
The regression coefficients between perceived social support, resilience, coping, optimism and depression were not significant in the path model (p > 0.05). To improve clarity and flow without changing the meaning or adding more content, the model was progressively modified to remove insignificant pathways leading to depression from social support, resilience, coping, and optimism. The fit of the modified path model was re-evaluation as follows: χ2/df = 1.881, GFI = 0.986, NFI = 0.973, RFI = 0.919, IFI = 0.987, TLI = 0.960, CFI = 0.987, RMSEA = 0.060. All of the fit indices met the recommended levels, confirming the modified model as the final model (Fig. 3).
Fig. 3.
Path diagram for the modified model. Numbers on the solid line are standard estimate. *P < 0.05, **P < 0.01, ***P < 0.001
Standardized direct, indirect and total effect of modified model
In the modified model, 14 pathways were statistical significance in total. Parenting stress and hope showed a direct effect on depression in caregivers of children with CL/P. Hope had a negative effect (-0.217), and parenting stress had a positive effect (0.416). Optimism (-0.237), resilience (-0.194), hope (-0.182), perceived social support (-0.080) and coping (-0.060) had an indirect effect on depression. The overall effects of different variables on depression from large to small were as follows: parenting stress (0.416), hope (0.400), optimism (-0.237), resilience (-0.194), perceived social support (-0.800), coping (-0.600). The details of standardized direct, indirect and total effect between variables were displayed in Table 3.
Table 3.
Standardized direct, indirect and total effect between variables in pathways of modified model
| Dependent variables | Effect size | Independent variables | |||||
|---|---|---|---|---|---|---|---|
| Optimistic | Resilience | Hope | Social support | Coping | Parenting stress | ||
| Resilience | Direct | 0.236 | - | - | - | - | - |
| Indirect | - | - | - | - | - | - | |
| Total | 0.236 | - | - | - | - | - | |
| Hope | Direct | 0.279 | 0.414 | - | - | - | - |
| Indirect | 0.098 | - | - | - | - | - | |
| Total | 0.376 | 0.414 | - | - | - | - | |
| Social support | Direct | 0.143 | 0.200 | 0.341 | - | - | - |
| Indirect | 0.175 | 0.141 | - | - | - | - | |
| Total | 0.318 | 0.341 | 0.341 | - | - | - | |
| Coping | Direct | - | 0.206 | 0.379 | - | - | - |
| Indirect | 0.191 | 0.157 | - | - | - | - | |
| Total | 0.191 | 0.363 | 0.379 | - | - | - | |
| Parenting stress | Direct | -0.166 | - | -0.319 | -0.191 | -0.145 | - |
| Indirect | -0.208 | -0.250 | -0.120 | - | - | - | |
| Total | -0.375 | -0.250 | -0.439 | -0.191 | -0.145 | ||
| Depression | Direct | - | - | -0.217 | - | - | 0.416 |
| Indirect | -0.237 | -0.194 | -0.182 | -0.080 | -0.060 | - | |
| Total | -0.237 | -0.194 | -0.400 | -0.080 | -0.060 | 0.416 | |
Discussion
It is worth mentioning that caregivers of children with CL/P in this study are all fathers or mothers, which is consistent with China’s basic national conditions. In the two CL/P treatment centers in China, parents are still the main caregivers of children with CL/P. This is because parents bear the initial responsibility for their children’s health. Additionally, children with CL/P in China predominantly come from remote rural areas [48] where access to advanced medical facilities is limited. Consequently, they must rely on higher-level hospitals for CL/P treatments. In this context, parents remain the primary drivers in seeking medical treatment from distant hospitals and managing the associated financial expenses.
In this study, the mean score of depression among caregivers of children with CL/P was 4.83 (4.79), which was lower than the depression score of 7.10 (6.24) among caregivers with dementia [49]; mildly depressed caregivers were nearly 1/3 (n = 78; 31.5%), which was lower than the proportion of mildly depressed caregivers of children with cancer (47.8%) [50]. Reasons for this discrepancy may be that: on the one hand, a holistic sequential treatment model integrating orthodontics, surgical repair, speech, psychology and care has been developed for CL/P [51], and most children can return to normal life through aggressive surgical treatment and rehabilitation [52]. This gives caregivers a lot of confidence and hope. However, dementia is a progressive disease, current medications and other interventions can only mitigate the progression of the disease but not restore the patient’s cognitive function. Therefore, caregivers of children with CL/P may develop fewer depressive symptoms compared to caregivers of patients with dementia. On the other hand, compared to childhood cancer, the CL/P has a low lethality rate, a high survival rate, and a manageable disease progression. This may also reduce the frustration of caregivers of children with CL/P. In addition, many support measures have been developed in China for CL/P families including Smile Train, Operation Rebirth, Yan Ran Angel Fund, Operation Smile and other public welfare programs [53, 54], which alleviate the financial pressure and maintain the psychological health of the caregivers. Finally, the maintenance of their psychological well-being has become an important part of the sequential treatment of CL/P, and psychological interventions for caregivers of children with CL/P are constantly being developed [55]. Therefore, caregivers in this study had lower levels of depression. However, it should not be overlooked that nearly half of the caregivers in this study had depressive symptoms (n = 108; 43.5%). This suggests that researchers still need to focus on the mental health of caregivers of children with CL/P.
Parenting stress and hope showed direct effect on depression among caregivers of children with chronic diseases. Optimism, resilience, coping and perceived social support indirectly influence depression through parenting stress and/or hope. Parenting stress is the variable with the largest effect size for depression. Parenting stress in caregivers of children with CL/P is a psychological response in the parenting process, a stressful reaction that manifests when caregivers do not have sufficient resources to meet the needs [56]. Many studies show that caregivers of children with CL/P experience high levels of parenting stress [57–59]. Caregiver stress in childcare is significantly and positively associated with depression levels and is a risk factor for psychological problems [60, 61]. Current research suggests that parenting stress leads to depressive symptoms mainly due to a decreased ability to expect, seek and feel pleasure, which is closely related to a neurotransmitter called dopamine in the nucleus acumens region of the brain [62, 63]. Specifically, when parenting stress arises in the caregiver of a child with CL/P, neurotransmitters in the brain directly evoke the hypothalamic–pituitary–adrenal axis [64], affecting the hypothalamus and pituitary gland to secrete dopamine, leading to depressive symptoms. Fang et al. [65] noted that chronic stress significantly upregulates the expression of lipopolysaccharide/endotoxin binding protein (LBP), which inhibits dopamine decarboxylase (DDC) and dopamine beta hydroxylase (DBH), key enzymes in monoamine synthesis, resulting in depression. In addition to direct effects on depressive symptoms in caregivers of children with CL/P, there is also an interaction between parenting stress and internal diathesis (hope, optimism, resilience, coping), and perceived social support. Path analysis verified the effect of hope, optimism, coping and perceived social support on depression among caregivers of children with CL/P in this study, which is consistent with previous research findings [66–69]. While resilience has no direct impact on parenting stress, it is to reduce parenting stress by increasing perceived social support. Resilience is an inherent psychological potential of individuals to mobilize all their own protective resources to achieve good adaptation in the pursuit of their own harmonious development under frustrating situations. To some extent, perceived social support is part of the inner resources mobilized by resilience and resilience influences perceived social support [70, 71]. A domestic research identified perceived social support as an important stress coping resource [72]. Good perceived social support can lead to higher self-efficacy [73]. In particular, perceived social support can lead to a lower assessment of stress when individuals are faced with stressful situations [18].
The study also showed that hope is another directly influential variable on depression among caregivers of children with CL/P. Hope is a positive perception and belief that leads people to believe in a positive and desirable goal that can be achieved in the future [36]. Higher levels of caregiver hope can reduce depressive symptoms [74, 75]. Caregivers of children with CL/P who have a strong sense of hope are more likely to have positive “converging” goal [76], which can be to help the child heal, return their child to a normal life or resolve their own difficulties. Goal generation facilitates the generation of behavioral routes for caregivers of children with CL/P. Those with high levels of hope formed more specific and feasible routes than those with low hope, and were also adept at forming alternative routes [76]. This also fits with the hope of being able to influence coping styles in this study. Resilience and optimism can act on hope to indirectly influence depression levels in caregivers of children with CL/P. Resilience, hope, and optimism are collectively referred to as the three major psychological capitals, and each variable has commonalities and characteristics that cannot be ignored. Unlike hope, optimism tends to be more of a stable personality trait, is not context-specific [77], and favors an attributional approach. Optimistic people make lasting, general and internal attributions to positive events and transient, specific and external attributions to negative events. Caregivers with optimistic characteristics are more likely to view the current dilemma as solvable and hopeful when faced with raising a child with CL/P. In short, an individual’s ability to generate hope in the face of setbacks is influenced by the trait of optimism [30]. Resilience positively affects sense of hope [78, 79]. Higher levels of resilience in caregivers of children with cleft lip and palate represent a weaker vulnerability to be able to cope with problems and a greater sense of hope to overcome adversity.
There are also some limitations in this study. First, cross-sectional studies cannot determine the causal relationship between the study variables. Future longitudinal designs are needed to further depict this relationship. Second, we used self-report scales which was also prone to social desirability response bias although measures were taken to overcome such bias (e.g., anonymity and confidentiality). Third, caregivers (fathers and mothers) of children with CL/P were analyzed as a whole in this study. However, different roles of parents have different emotional responses and behaviors. Future research could explore and compare the depression pathways of fathers and mothers separately. At the same time, it is undeniable that intellectual and developmental disabilities, along with behavioral issues in children with CL/P, affect parenting stress and well-being. In the future, consider incorporating developmental challenges in children with CL/P into theory-driven analyses. Finally, only caregivers of children with CL/P in two Chinese hospitals were investigated in this study, which may limit the broad representativeness of the findings. Validation of the study results in other Chinese regions or abroad is warranted.
Conclusions
In summary, we explored the factors that might be associated with depression among caregivers of children with CL/P in the context of China based on the diathesis-model and previous research. The most significant discovery was that caregivers’ depression could be influenced by hope, optimism, resilience, coping, perceived social support and parenting stress. Among these factors, parenting stress and hope are the most important. In particular, parenting stress is a major determinant because of its direct effect on depression. Targeted parenting stress interventions should be performed to decrease depression including cognitive-behavioral interventions, psychosocial interventions and provide available support and resources.
Acknowledgements
The authors would like to thank all participating caregivers of children with CL/P for their contributions to this study and also like to thank colleagues at the Maxillofacial Surgery Department of School and Hospital of Stomatology of China Medical University and West China School/ Hospital of Stomatology Sichuan University for their help with data collection.
Abbreviations
- CL/P
Cleft lip and/or palate
- PHQ-9
Patient Health Questionnaire
- HHI
Herth Hope Index
- LOT-R
Revised Life Orientation Test
- RS-14
Resilience Scale-14
- MSPSS
Multidimensional Scale of Perceived Social Support
- CHIP
Coping Health Inventory for Parents
- PSI-SF
Parenting Stress Index-Short Form
- S-W test
Shapiro–Wilk test
- MLE
Maximum likelihood estimation
- χ2/df
Chi-Square/degree of freedom
- GFI
Goodness-of-Fit Index
- NFI
Normed Fit Index
- RFI
Relative Fit Index
- IFI
Incremental Fit Index
- TLI
Tacker-Lewis Index
- CFI
Comparative Fit Index
- RMSEA
Root-Mean-Square Error of Approximation
- MI
Modification Index
Authors’ contributions
JRY proposed the study hypothesis, performed the data analysis, wrote and revised the manuscript. XHL, YQG, CXG and RZW supervised this study and provide available resources. WRW, JYW, YJW and RZW collected, analyzed and interpreted the data. LLY developed study proposal, administrated the funding project and revised the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the project of Education Department of Liaoning Province (LJKR0281).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All methods were conducted in accordance with relevant guidelines and regulations or declaration of Helsinki. Eligible participants signed an informed consent form before being included in this study and were informed of their right to withdraw at any time during the survey. All information provided in the questionnaire was kept confidential. This study was approved by the Ethical Committee of China Medical University (Approval number: 2018–27).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Runzi Wang and Lulu Yuan share the correspondence authorship on this work.
Contributor Information
Runzi Wang, Email: 277507000@qq.com.
Lulu Yuan, Email: 18040229859@sina.cn.
References
- 1.Zhang Z. Oral and maxillofacial surgery. 7th ed. Beijing: People’s Medical Publishing House; 2012. [Google Scholar]
- 2.Kadir A, Mossey PA, Blencowe H, Moorthie S, Lawn JE, Mastroiacovo P, et al. Systematic review and meta-analysis of the birth prevalence of orofacial clefts in low- and middle-income countries. Cleft Palate Craniofac J. 2017;54(5):571–81. 10.1597/15-221. [DOI] [PubMed] [Google Scholar]
- 3.Mossey PA, Modell B. Epidemiology of oral clefts 2012: an international perspective. Front Oral Biol. 2012;16:1–18. 10.1159/000337464. [DOI] [PubMed] [Google Scholar]
- 4.Wang M, Yuan Y, Wang Z, Liu D, Wang Z, Sun F, et al. Prevalence of orofacial clefts among live births in China: a systematic review and meta-analysis. Birth Defects Res. 2017;109(13):1011–9. 10.1002/bdr2.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang JN, Song FQ, Zhou SN, Zheng H, Peng LY, Zhang Q, et al. Analysis of single-nucleotide polymorphism of Sonic hedgehog signaling pathway in non-syndromic cleft lip and/or palate in the Chinese population. Beijing Da Xue Xue Bao Yi Xue Ban. 2019;51(3):556–63. 10.19723/j.issn.1671-167X.2019.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou W, Xu Z, Zhang L, Zhang X. Psychological status investigation and psychological nursing of parents of children with cleft lip and palate. Lab Med Clin. 2014;11(09):1273–4. 10.3969/j.issn.1672-9455.2014.09.059. [Google Scholar]
- 7.Toledano-Toledano F, Moral de la Rubia J. Factors associated with anxiety in family caregivers of children with chronic diseases. BioPsychoSoc Med. 2018;12:20. 10.1186/s13030-018-0139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelson P, Glenny AM, Kirk S, Caress AL. Parents’ experiences of caring for a child with a cleft lip and/or palate: a review of the literature. Child. 2012;38(1):6–20. 10.1111/j.1365-2214.2011.01244.x. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Zhai D, Xin Y, Ma J, Huang Y, Xin X. A study on the psychosomatic states of parents of children with cleft lip / palate. J Pract Stomatol. 2012;28(04):505–8. 10.3969/j.issn.1001-3733.2012.04.022. [Google Scholar]
- 10.Given BA, Given CW, Sherwood P. The challenge of quality cancer care for family caregivers. Semin Oncol Nurs. 2012;28(4):205–12. 10.1016/j.soncn.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Baker JK, Seltzer MM, Greenberg JS. Longitudinal effects of adaptability on behavior problems and maternal depression in families of adolescents with autism. J Fam Psychol. 2011;25(4):601–9. 10.1037/a0024409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallagher S, Phillips AC, Oliver C, Carroll D. Predictors of psychological morbidity in parents of children with intellectual disabilities. J Pediatr Psychol. 2008;33(10):1129–36. 10.1093/jpepsy/jsn040. [DOI] [PubMed] [Google Scholar]
- 13.Thrush A, Hyder AA. The neglected burden of caregiving in low- and middle-income countries. Disabil Health J. 2014;7(3):262–72. 10.1016/j.dhjo.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 14.KarimiMoghaddam Z, Rostami M, Zeraatchi A, MohammadiBytamar J, Saed O, Zenozian S. Caregiving burden, depression, and anxiety among family caregivers of patients with cancer: an investigation of patient and caregiver factors. Front Psychol. 2023;14:1059605. 10.3389/fpsyg.2023.1059605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu L, Liu X, Zhang G, Su H. Psychological health instruction of parents of 230 children with cleft lip and/or palate. Nurs Res. 2010;24(36):3333–4. 10.3969/j.issn.1009-6493.2010.36.026. [Google Scholar]
- 16.Mank A, van Maurik IS, Rijnhart JJM, Rhodius-Meester HFM, Visser LNC, Lemstra AW, et al. Determinants of informal care time, distress, depression, and quality of life in care partners along the trajectory of Alzheimer’s disease. Alzheimers Dement (Amst). 2023;15(2):e12418. 10.1002/dad2.12418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wen H, Hu S. Stress symptoms of social workers and their resolution from the perspective of the diathesis-stress model–an analysis based on data from the China Survey of Social Work Dynamics (CSWLS2019). J Soc Work. 2022;03:85-99–109-10. 10.3969/j.issn.1672-4828.2022.03.009. [Google Scholar]
- 18.Zaidman-Zait A, Mirenda P, Duku E, Vaillancourt T, Smith IM, Szatmari P, et al. Impact of personal and social resources on parenting stress in mothers of children with autism spectrum disorder. Autism. 2017;21(2):155–66. 10.1177/1362361316633033. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Wu J, Yao Y, Liu Y, Ren J, Chen S. The relationship between behavioral problems and parental anxiety in children with autism and intellectual disability: the mediating role of parenting stress and the moderating role of appreciative social support. Psychol Dev Educ. 2023;39(01):77–84. 10.16187/j.cnki.issn1001-4918.2023.01.09. [Google Scholar]
- 20.McCloskey RJ, Pei F. The role of parenting stress in mediating the relationship between neighborhood social cohesion and depression and anxiety among mothers of young children in fragile families. J Community Psychol. 2019;47(4):869–81. 10.1002/jcop.22160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eche IJ, Eche IM, Pires C, Isibor C, Achibiri A, Aronowitz T. A systematic mixed-studies review of hope experiences in parents of children with cancer. Cancer Nurs. 2022;45(1):E43-e58. 10.1097/ncc.0000000000000841. [DOI] [PubMed] [Google Scholar]
- 22.Chiracu A, Cosma GA, Stepan AR, Cosma MA, Corlaci I, Călugăru EDC, et al. Psychological capital, quality of life, and well-being in mother caregivers of individuals with down syndrome. Front Psychol. 2023;14:1145104. 10.3389/fpsyg.2023.1145104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slattery É, McMahon J, Gallagher S. Optimism and benefit finding in parents of children with developmental disabilities: the role of positive reappraisal and social support. Res Dev Disabil. 2017;65:12–22. 10.1016/j.ridd.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Díaz A, Ponsoda JM, Beleña A. Optimism as a key to improving mental health in family caregivers of people living with Alzheimer’s disease. Aging Ment Health. 2020;24(10):1662–70. 10.1080/13607863.2020.1715342. [DOI] [PubMed] [Google Scholar]
- 25.Duggleby W, Lee H, Nekolaichuk C, Fitzpatrick-Lewis D. Systematic review of factors associated with hope in family carers of persons living with chronic illness. J Adv Nurs. 2021;77(8):3343–60. 10.1111/jan.14858. [DOI] [PubMed] [Google Scholar]
- 26.Yang Y, Gao H, Shang C, Song G, Li H, Chen L. Frailty and resilience on coping styles of middle-aged and elderly maintenance hemodialysis patients and caregivers: an Actor Partner Interdependence Model analysis. Nurs Res. 2022;36(20):3619–23. 10.12102/j.issn.1009-6493.2022.20.009. [Google Scholar]
- 27.Cao N, Li H, Zhao Y. Study on influencing factors of level of hope in caregiversfor patients with esophageal cancer. Tianjin J Nurs. 2021;29(01):9–13. 10.3969/j.issn.1006-9143.2021.01.003. [Google Scholar]
- 28.Anderson MI, Daher M, Simpson GK. A predictive model of resilience among family caregivers supporting relatives with traumatic brain injury (TBI): a structural equation modelling approach. Neuropsychol Rehabil. 2020;30(10):1925–46. 10.1080/09602011.2019.1620787. [DOI] [PubMed] [Google Scholar]
- 29.Yuan L, Gao Y, Pan B, Wang J, Wang Y, Gong C, et al. Resilience and related factors: a comparison of fathers and mothers of patients with Cleft Lip and/or Palate in China. Front Psych. 2021;12:791555. 10.3389/fpsyt.2021.791555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peer JW, Hillman SB. Stress and resilience for parents of children with intellectual and developmental disabilities: a review of key factors and recommendations for practitioners. J Policy Pract Intel Disabil. 2014;11(2):92–8. [Google Scholar]
- 31.Jackson DL. Revisiting sample size and number of parameter estimates: some support for the N:q hypothesis, structural equation modeling. Multidiscip J. 2003;10(1):128–41. [Google Scholar]
- 32.Bentler P, Chou CP. Practical issues in structural modeling. Sociol Methods Res. 1987;16(1):78–117. [Google Scholar]
- 33.Chen S, Chiu H, Xu B, Ma Y, Jin T, Wu M, et al. Reliability and validity of the PHQ-9 for screening late-life depression in Chinese primary care. Int J Geriatr Psychiatry. 2010;25(11):1127–33. 10.1002/gps.2442. [DOI] [PubMed] [Google Scholar]
- 34.Chagas MH, Tumas V, Rodrigues GR, Machado-de-Sousa JP, Filho AS, Hallak JE, et al. Validation and internal consistency of Patient Health Questionnaire-9 for major depression in Parkinson’s disease. Age Ageing. 2013;42(5):645–9. 10.1093/ageing/aft065. [DOI] [PubMed] [Google Scholar]
- 35.Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–44. 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 36.Herth K. Development and refinement of an instrument to measure hope. Sch Inq Nurs Pract. 1991;5(1):39–51 discussion 3-6. [PubMed] [Google Scholar]
- 37.Wang Y. Study on feasibility of Chinese version of Herth hope index for cancer patients. Chin Nurs Res. 2010;24(01):20–1. 10.3969/j.issn.1009-6493.2010.01.008. [Google Scholar]
- 38.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–78. 10.1037/0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 39.Yang YL, Liu L, Li MY, Shi M, Wang L. Psychological disorders and psychosocial resources of patients with newly diagnosed bladder and kidney cancer: a cross-sectional study. PLoS ONE. 2016;11(5):e0155607. 10.1371/journal.pone.0155607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1(2):165–78. [PubMed] [Google Scholar]
- 41.Gao Y, Yuan L, Pan B, Wang L. Resilience and associated factors among Chinese patients diagnosed with oral cancer. BMC Cancer. 2019;19(1):447. 10.1186/s12885-019-5679-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dahlem NW, Zimet GD, Walker RR. The multidimensional scale of perceived social support: a confirmation study. J Clin Psychol. 1991;47(6):756–61. 10.1002/1097-4679(199111)47:6%3c756::aid-jclp2270470605%3e3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 43.Liu L, Yang YL, Wang ZY, Wu H, Wang Y, Wang L. Prevalence and positive correlates of posttraumatic stress disorder symptoms among Chinese patients with hematological malignancies: a cross-sectional study. PLoS ONE. 2015;10(12):e0145103. 10.1371/journal.pone.0145103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mccubbin HI, Mccubbin MA, Patterson JM, Cauble AE, Warwick WW. CHIP—Coping Health Inventory for Parents: an assessment of parental coping patterns in the care of the chronically ill child. J Marriage Fam. 1983;45(2):359–70. 10.2307/351514. [Google Scholar]
- 45.Li Y, Wei M. Study of application of the Chinese version of CHIP for parents of children with chronic disease. Chin J Nurs. 2007;11:972–5. [Google Scholar]
- 46.Abidin RR. Parenting stress index-professional manual, 3rd. Odessa: Psychological Assessment Resource; 1995. p. 9–13. [Google Scholar]
- 47.Kline RB. Principles and practice of structural equation modeling. New York: The Guilford Press; 1998. [Google Scholar]
- 48.Zhou X, Jiang Y, Fang J, Wang H, Xie D, Kuang H, et al. Incidence of cleft lip and palate, and epidemiology of perinatal deaths related to cleft lip and palate in Hunan Province, China, 2016–2020. Sci Rep. 2023;13(1):10304. 10.1038/s41598-023-37436-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tan KP, Ang JK, Koh EBY, Pang NTP, Mat Saher Z. Relationship of psychological flexibility and mindfulness to caregiver burden, and depressive and anxiety symptoms in caregivers of people with dementia. Int J Environ Res Public Health. 2023;20(5):4232. 10.3390/ijerph20054232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alaqeel M, Alkhathaami F, Alshangiti A, Alanazi A, Alothri MA, Alqarni AT, et al. Depression and quality of life among caregivers of pediatric cancer patients. Cureus. 2022;14(4):e24256. 10.7759/cureus.24256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shi B, Li C, Li J, Yang C, Yin H, Jia Z, et al. Research and treatment of cleft lip and palate in China: review of 30 years. China J Oral Maxillofac Surg. 2016;14(05):385–96. [Google Scholar]
- 52.Shi B, Fu Y, Yin N, Huang H, Liu J, Chen R, et al. Application of team approach and key techniques of cleft lip and palate. West China J Stomatol. 2017;35(01):8–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shi B, Peng Z, Ma Y, Dong X. A study on the accessibility of welfare in the implementation of medical aid policy: an example of the “Operation Rebirth” project for children with cleft lip and palate. China Soc Work Res. 2014;01:64–103. [Google Scholar]
- 54.Feng Y. The power behind the smile - Remembering Mr. Charles Wang, the founder and chairman of the Smile Train Foundation of America. China Med Pharm. 2012;2(02):4–5. [Google Scholar]
- 55.Wang Y, Xin Y, Ma J, Xin X, Shi B, Huang Y. Effects of an early psychological intervention on parents of children with cleft lip/palate. West China J Stomatol. 2013;31(04):372–6. 10.7518/hxkq.2013.04.011. [PubMed] [Google Scholar]
- 56.Holly LE, Fenley AR, Kritikos TK, Merson RA, Abidin RR, Langer DA. Evidence-base update for parenting stress measures in clinical samples. J Clin Child Adolesc Psychol. 2019;48(5):685–705. 10.1080/15374416.2019.1639515. [DOI] [PubMed] [Google Scholar]
- 57.Lentge K, Lentge F, Zeller AN, Gellrich NC, Tavassol F, Korn P, et al. Cleft lip and palate: the psychological burden of affected parents during the first three years of their children’s lives. Int J Oral Maxillofac Surg. 2022;51(11):1462–8. 10.1016/j.ijom.2022.04.003. [DOI] [PubMed] [Google Scholar]
- 58.Boztepe H, Çınar S, ÖzgürMd FF. Parenting stress in Turkish mothers of infants with Cleft Lip and/or Palate. Cleft Palate Craniofac J. 2020;57(6):753–61. 10.1177/1055665619898592. [DOI] [PubMed] [Google Scholar]
- 59.Xun Y, Wang J, Yuan L, Gong C, Gao Y. Status quo and influencing factors of parental stress among parents of children with cleft lip andpalate. Nurs Res. 2022;36(20):3598–603. [Google Scholar]
- 60.Foody C, James JE, Leader G. Parenting stress, salivary biomarkers, and ambulatory blood pressure: a comparison between mothers and fathers of children with autism spectrum disorders. J Autism Dev Disord. 2015;45(4):1084–95. 10.1007/s10803-014-2263-y. [DOI] [PubMed] [Google Scholar]
- 61.Wang J, Hu Y, Wang Y, Qin X, Xia W, Sun C, et al. Parenting stress in Chinese mothers of children with autism spectrum disorders. Soc Psychiatry Psychiatr Epidemiol. 2013;48(4):575–82. 10.1007/s00127-012-0569-7. [DOI] [PubMed] [Google Scholar]
- 62.Al-Hasani R, Gowrishankar R, Schmitz GP, Pedersen CE, Marcus DJ, Shirley SE, et al. Ventral tegmental area GABAergic inhibition of cholinergic interneurons in the ventral nucleus accumbens shell promotes reward reinforcement. Nat Neurosci. 2021;24(10):1414–28. 10.1038/s41593-021-00898-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dormegny-Jeanjean LC, Mainberger OAE, de Crespin de Billy C, Obrecht A, Danila V, Erb A, et al. Safety and tolerance of combination of monoamine oxidase inhibitors and direct dopamine agonists in adults and older adults with highly resistant depression. L'Encephale. 2023. 10.1016/j.encep.2023.01.011. [DOI] [PubMed]
- 64.Kanes SJ, Dennie L, Perera P. Targeting the Arginine Vasopressin V(1b) receptor system and stress response in depression and other neuropsychiatric disorders. Neuropsychiatr Dis Treat. 2023;19:811–28. 10.2147/ndt.s402831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fang M, Li Y, Liao Z, Wang G, Cao Q, Li Y, et al. Lipopolysaccharide-binding protein expression is increased by stress and inhibits monoamine synthesis to promote depressive symptoms. Immunity. 2023;56(3):620-34.e11. 10.1016/j.immuni.2023.02.002. [DOI] [PubMed] [Google Scholar]
- 66.Wang Y, Chung MC, Wang N, Yu X, Kenardy J. Social support and posttraumatic stress disorder: a meta-analysis of longitudinal studies. Clin Psychol Rev. 2021;85:101998. 10.1016/j.cpr.2021.101998. [DOI] [PubMed] [Google Scholar]
- 67.Zhang Y, Cui C, Wang L, Yu X, Wang Y, Wang X. The Mediating role of hope in the relationship between perceived stress and post-traumatic stress disorder among Chinese patients with oral cancer: a cross-sectional study. Cancer Manag Res. 2021;13:393–401. 10.2147/cmar.s281886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li L, Ai H, Gao L, Zhou H, Liu X, Zhang Z, et al. Moderating effects of coping on work stress and job performance for nurses in tertiary hospitals: a cross-sectional survey in China. BMC Health Serv Res. 2017;17(1):401. 10.1186/s12913-017-2348-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kimhi S, Eshel Y, Shahar E. Optimism as a predictor of the effects of laboratory-induced stress on fears and hope. Int J Psychol. 2013;48(4):641–8. 10.1080/00207594.2012.676181. [DOI] [PubMed] [Google Scholar]
- 70.Liu Q, Yu X, Fei Y, Qiu C, Zhu X. Gratitude and health promotion behaviors among patients with first-ever ischemic stroke: the mediating role of resilience and perceived social support. Nurs J Chin PLA. 2021;38(11):12–6. 10.3969/ji.ssn.1008-9993.2021.11.004. [Google Scholar]
- 71.Salces-Cubero IM, Ramírez-Fernández E, Ortega-Martínez AR. Strengths in older adults: differential effect of savoring, gratitude and optimism on well-being. Aging Ment Health. 2019;23(8):1017–24. 10.1080/13607863.2018.1471585. [DOI] [PubMed] [Google Scholar]
- 72.Chang PY, Chang TH, Yu JM. Perceived stress and social support needs among primary family caregivers of ICU Patients in Taiwan. Heart Lung. 2021;50(4):491–8. 10.1016/j.hrtlng.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 73.Zhao Y, Huang L, Li Y. Influence of physical exercises on pilot students’ emotional stability: Chain mediation effects of perceived social support and self-efficacy. Chin J Health Psychol. 2023;31(03):446–51. 10.13342/j.cnki.cjhp.2023.03.024. [Google Scholar]
- 74.Chow EO, Fung SF, Singh H. Actor-partner effects of wellbeing, hope and self-esteem on depression in stroke survivor-caregiver dyads: a randomized controlled trial. Clin Rehabil. 2023;37(3):394–406. 10.1177/02692155221128758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rumpold T, Schur S, Amering M, Ebert-Vogel A, Kirchheiner K, Masel E, et al. Hope as determinant for psychiatric morbidity in family caregivers of advanced cancer patients. Psychooncology. 2017;26(5):672–8. 10.1002/pon.4205. [DOI] [PubMed] [Google Scholar]
- 76.Liu M, Huang X. Hope: a review of research in psychology. Adv Psychol Sci. 2013;21(03):548–60. 10.3724/SP.J.1042.2013.00548. [Google Scholar]
- 77.Scheier MF, Weintraub JK, Carver CS. Coping with stress: divergent strategies of optimists and pessimists. J Pers Soc Psychol. 1986;51(6):1257–64. 10.1037/0022-3514.51.6.1257. [DOI] [PubMed] [Google Scholar]
- 78.Gandeng A, Chao L, Wang S. The relationship between career exploration, mental toughness, and sense of hope among first-year freshmen. Ment Health Educ Prim Second Schl. 2019;22:12–7. [Google Scholar]
- 79.Gu J, Tao L, He J, Dai J, Li S. Study on the relationship between professional identity, resilience and hope of nurses in the outbreak of new coronavirus pneumonia. J Clin Nurs. 2020;19(05):2–5. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.