ABSTRACT
This study analyzed 1432 questions asked in 19 surveys (N = 43,014) on COVID-19 vaccines between January 2020 and August 2022 using dimensions including (1) information sources about COVID-19 vaccine, (2) information about the access, effectiveness, and side effects of COVID-19 vaccine, (3) COVID-19 vaccine hesitancy (i.e. false perception, skepticism, and vaccine refusal), (4) motivations to get the COVID-19 vaccine (i.e. to perform routine activities, convenience, incentives, influences, and travel requirement), (5) false perceptions caused vaccine refusal, and (6) intentions to get vaccinated. Our results show that vaccine refusal was rampant throughout the pandemic and mostly attributed to the rush in the vaccine development process and perceived safety risks. Additionally, our analysis indicates that people’s motivation to get vaccinated came from varied sources such as doctors, family members, and politicians. Lastly, mandating vaccines during the pandemic did not significantly increase uptake among individuals who were initially skeptical, and concerns about the rapid development of the vaccine were a major cause of vaccine hesitancy. Findings were discussed and interpreted using the information deficit model, the two-step flow theory, and the reactance theory. This research provides valuable insights and practical implications, along with significant theoretical contributions and policy recommendations.
KEYWORDS: COVID-19 vaccine, information deficit model, public opinion, global pandemic, vaccine acceptance, vaccine refusal
Introduction
COVID-19 has dramatically influenced the world socially, politically, economically, psychologically, and emotionally.1 The COVID-19 pandemic has taken millions of lives across the world, caused widespread suffering, and had serious debilitating long-term physical and mental health effects on many of the people who survived the virus. Since the beginning of this health crisis, much global discussion has revolved around how to stop the spread of the virus and end the pandemic to save human lives. Issues related to COVID-19 vaccines have been at the center of the discussion. Besides concerns about the rapid development of the vaccines,2 which raised questions about the effectiveness and safety of vaccines, politicization and misinformation concerning COVID-19 vaccines has had led to vaccine hesitance, slowing vaccine uptake among the public.3–7 In the U.S., for example, more than three years after the first COVID-19 case was detected in the country, less than 70% of eligible Americans completed a primary series of vaccination.8 More troubling, recent vaccine tracking data show that only about 15% of eligible Americans received their recommended updated COVID-19 booster shots, even though the booster shots were shown to extend protection against even the most recent virus variants, and were widely available free of charge.8 Vaccine hesitancy posed as one of the most challenging barriers to curbing the pandemic.9
Multiple efforts have been made to understand public opinion about COVID-19 which plays a key role to vaccine acceptance and public health policies regarding the global pandemic. In the US, polls and surveys have been distributed to garner information from Americans on their attitudes, expectations, and acceptance of COVID-19 vaccines. Some of the most frequently asked poll questions include those about vaccine hesitancy, reasons for hesitancy, information sources about COVID-19 vaccines, and perceptions of COVID-19 vaccines for children. COVID-19 is, indeed, one of the biggest and longest global public health crises.10 Previous studies have explored various dimensions of vaccine hesitancy and acceptance. These include the effectiveness of financial incentives for COVID-19 vaccination,11,12 the ethics of offering benefits to vaccine recipients,13 resistance to the COVID-19 vaccine in the U.S.,3 willingness to be vaccinated,14 overall vaccine acceptance in the U.S.,1 and the influence of vaccine knowledge, risk perception, and doctor-patient communication on vaccination intentions.15 However, these studies focus on specific topics within the broader debate on public attitudes toward COVID-19 vaccines. This leaves a significant gap in research that could provide a comprehensive overview of public opinion on vaccines in the U.S., using COVID-19 as a case study. We argue that public opinion regarding the pandemic might also have changed over time. Therefore, providing a comprehensive overview of public polls or surveys on COVID-19 vaccines is important to understanding public attitude and behavior about COVID-19 vaccines. The findings of this study may be useful for government agencies, state and local health departments, policy institutes, and vaccine development companies by providing insights on how to promote the effectiveness and importance of vaccines during health crises. Additionally, these findings can help mainstream and social media messaging in improving public knowledge, promoting health literacy, and reducing misinformation about vaccines.
In this paper, we acquired data from the Roper Center for Public Opinion Research and extracted all surveys (i.e., 19 in total) conducted by various media, academic, and nonprofit organizations. We organized the themes based on questions throughout the course of almost three years. The themes include: (1) information sources about the COVID-19 vaccine, (2) information about the access, effectiveness, and side effects of the COVID-19 vaccine, (3) COVID-19 vaccine hesitancy (i.e., false perception, skepticism, and vaccine refusal), (4) motivations to get the COVID-19 vaccine (i.e., to perform routine activities, convenience, incentives, influences, and travel requirement), (5) false perceptions that caused vaccine refusal, (6) and intentions to get vaccinated.
Theoretically, findings from this study highlight the importance of several factors in effective health communication concerning COVID vaccination. They indicate that a more proactive approach is needed to address the vaccine hesitancy issue in the US, rather than over-reliance on the information deficit explanatory model. Findings from this research offer theoretical, practical, and policy implications for strategic public health policies and vaccine communication campaigns to encourage COVID vaccination.
Literature review
COVID-19 vaccine hesitancy
COVID-19 vaccine hesitancy, defined as reluctance or refusal to accept vaccination despite availability, has been a significant obstacle to achieving global immunity against COVID-19. Extant research suggests that hesitancy is influenced by a complex interplay of cognitive, social, political, and historical factors, with common concerns including vaccine safety, efficacy, and trust in healthcare systems.16,17 Pourrazavi et al.16 explain that the “5C” model – confidence, complacency, constraints, calculation, and collective responsibility – captures many of the socio-psychological drivers of hesitancy.18 Low confidence in vaccine safety and efficacy is often cited as a primary concern, exacerbated by fears of side effects, which are particularly pronounced among individuals who feel the vaccine development process was rushed.19 This hesitation is more evident within communities that have experienced medical exploitation or discrimination in the past, such as Black and Hispanic populations in the U.S., who often cite medical mistrust as a barrier.20 Geographically, hesitancy also varies, with regions like the U.S. Northeast and South showing lower acceptance rates compared to the Midwest, illustrating the impact of localized cultural and demographic factors on vaccine receptivity.17,21
Public opinion polls provide useful insights into these complex patterns, revealing notable demographic and socioeconomic disparities in vaccine hesitancy. For example, Yasmin et al.17 reported acceptance rates ranging from 12% in certain religious and minority communities to over 90% among medical center employees and healthcare workers, highlighting how occupational exposure and perceived risk influenced attitudes. Additionally, hesitancy rates were higher among younger adults, women, and individuals with lower education or income levels, with Szilagyi et al.22 finding that financial insecurity and limited access to reliable health information contributed to skepticism about the vaccine’s safety and necessity. These polls also captured psychological factors, with individuals who believed in alternative forms of immunity or who expressed distrust in mainstream healthcare being more likely to refuse vaccination.17 Shifts in public opinion over time, such as increasing acceptance after the initial rollout, underscored the importance of responsive public health messaging that addresses evolving concerns and builds trust through consistent, transparent communication.16,22
Social influences and misinformation further fueled COVID-19 vaccine hesitancy, as social media platforms often served as channels for conspiracy theories and unverified claims about vaccine safety.23–26 Pourrazavi et al. noted that misinformation and social norms – such as the opinions of family members and peer groups – played a major role in shaping individual decisions about vaccination, with studies showing that individuals whose close networks expressed skepticism were more likely to be hesitant.19,27 Public opinion polls have consistently highlighted this pattern, indicating that exposure to vaccine-related misinformation and conspiracy theories correlated strongly with hesitancy, particularly among those who relied on non-medical sources of information.20 Therefore, the insights from public opinion data can guide the development of communication strategies that promote vaccine acceptance by identifying and addressing social and psychological barriers to vaccination.
Public opinion polls and vaccines
A public opinion poll or survey is a systematic effort to collect information about the attitudes, beliefs, perceptions, behaviors, or preferences of a specific population on topics such as politics, energy, climate change, science, health, social issues, or consumer preferences.28 Polls generally involve asking a representative sample of people questions to gauge their opinions, and the results can provide insights into trends and public sentiments. These polls are often used by politicians, policy institutes, policymakers, researchers, governments, and businesses to inform decisions and strategies. SteelFisher et al.29 analyzed 21 nationally representative public opinion polls conducted between 2015 and 2023, focusing on childhood vaccination during the COVID-19 pandemic. Their study addressed three key public health issues: perceptions of vaccine safety and risk, trust in the public health institutions that promote vaccines, and support for school vaccination requirements. The findings indicated that 35–42% of the U.S. public considered COVID-19 vaccines “very safe” for most children, while approximately 70% believed routine childhood vaccines were “very safe.” Additionally, about 54% expressed strong trust in public health agencies to provide accurate information about the safety of routine childhood vaccines. Regarding school vaccine requirements, public opinion was divided before the 2022–23 school year, with 47% to 52% opposing the mandate for students to receive a COVID-19 vaccine to attend in person. In a separate study, Blendon et al.30 examined public opinion related to COVID-19. Their findings revealed that the public prioritized four major issues during the pandemic: passing a relief bill, expanding federal support for COVID-19 testing, vaccination, and personal protective equipment, passing an economic stimulus bill, and increasing eligibility for food stamps.
Ho et al.31 analyzed poll data on several health threats, including avian flu, severe acute respiratory syndrome (SARS), West Nile virus, and anthrax. Their findings revealed that Americans’ perceptions of these threats were the highest during the early stages of major outbreaks, with public concerns decreasing once the situations appeared to be under control. Similarly, international studies have examined public opinion about COVID-19 vaccines. For example, Gagneux-Brunon et al.32 investigated attitudes toward mandatory COVID-19 vaccination in France prior to its official announcement, as well as the factors influencing opposition to such a policy among both young and older populations. They found that 43% of participants supported mandatory vaccination, 41.9% opposed it, and 15.1% were undecided. Among those opposed to mandatory vaccination for the general public, 30.05% supported its implementation for healthcare workers. Some scholars have also examined public opinion through social media platforms. For instance, Featherstone et al.33 examined childhood vaccination themes on Twitter (currently known as X) using semantic network analysis. Their results suggested that the most prominent theme was HPV vaccination as a disease preventative. The MMR vaccine autism link was the second major theme, followed by measles outbreak rates. These themes reflect public opinions on popular vaccine topics and current issues on social media.
Public opinion polls during COVID-19 reveal a growing gap between public views on vaccines and attitudes toward vaccine policies worldwide. Public sentiment regarding vaccine safety, necessity, trust, and support remains critically important. However, it is important to note that polls collect public opinion at a single point in time, and these views can evolve due to various factors, as mentioned earlier. While these polls provide valuable insights, they also help public health organizations advocate for protective measures and tailor health messaging to persuade the public on vaccine issues. This suggests that public health officials must focus on addressing concerns about vaccine safety, effectiveness, and benefits. Finally, understanding the nuanced shifts in public opinion on vaccination, along with adapting communication strategies in response, can help policymakers and public health leaders ensure that vaccination remains a cornerstone of public health policy both today and in the future.29
Method
Data acquisition
For this study, we used data from the Roper Center for Public Opinion Research hosted by Cornell University. We used three key search terms: “COVID-19 vaccine” OR “coronavirus vaccine” OR “corona vaccine” to acquire data. Data were collected between January 2020 and August 2022. The total number of survey questions examined was 1,432 from several different survey organizations such as Gallup, Ipsos, SSRS, and the Eagleton Center for Public Opinion Polling (ECPOP). In terms of sample size, the minimum number of participants in the surveys analyzed in this study was 419 and the maximum was 12,649. The median number of participants were 1,203. The surveys included a substantial total number of participants, with a sample size of (N = 43,014). The first survey to examine public opinion on COVID-19 was conducted in March 2020 and the latest was in August 2022.
Demographic characteristics of participants
In terms of survey populations, 70.2% of the surveys were conducted with a national sample of adults, 11.54% with a national sample of adults including oversampling of minority populations such as Black and Hispanic individuals, 6.6% with likely voters, 6.16% with parents of young children, and 5.5% with residents from various states. Survey organizations employed various methods to collect data. Specifically, 48.1% of the surveys were web-based, 25.4% were conducted via telephone, 16% used a combination of web and telephone methods, and 11.5% utilized more than two methods, such as computer-assisted surveys.
Data cleaning
After downloading the survey datasets, data cleaning was performed. During this process, we removed eight questions because they did not have any option for participants to choose. First, we also excluded questions that were too general, such as “What is the biggest challenge Americans are facing right now?” In some cases, participants mentioned issues like “immigration,” “inflation,” or “unemployment,” which appeared in the results because some respondents wrote “vaccines.” Second, we removed open-ended survey questions, some of which had more than 100 possible responses, which could complicate analysis. Third, we removed questions that showed total percentages exceeding 100 or falling below 100. Fourth, we excluded questions that were asked at different points in time using different scales, as the variation in options and scales could make it difficult to draw meaningful conclusions. These questions were ultimately excluded from the analysis as they were not directly related to vaccines or COVID-19. By following these steps, the final number of survey questions in this study was 1,432. The data cleaning was performed by using Microsoft Excel.
Data analysis
Once the data were cleaned, we used Microsoft Excel to organize the questions into major themes. Prior research suggests that themes are general propositions that emerge from the data and “provide recurrent and unifying ideas regarding the subject of inquiry”34 p. 1766). We combined both inductive and deductive approaches to code the data. This approach is useful because it allows researchers to generate new coded themes instead of forcing data only into existing themes, and eventually providing a list of new themes with new insights.34 For the inductive method, the researchers identified keywords in the question statements and grouped them based on similarities in wording. A detailed description of this process is provided below. For the deductive approach, when researchers were uncertain about the question statements, they consulted prior studies that had analyzed public opinion polls (see29,31,31). This helped ensure more accurate coding of the data.
The data were coded by the first and third author. Initially, we generated 10 major themes. To identify the 10 major themes, we followed a systematic process. First, we grouped questions related to information sourcing, usually indicated by keywords in the question statements. These questions were combined regardless of their scale or when they were asked. We repeated this process for each emerging theme, such as vaccine safety, vaccine refusal, and motivations to get vaccinated. Once we had grouped the questions based on key terms, we examined their scales. If the scale of questions within the same theme matched, we consolidated them to form the major themes. Additionally, we looked for questions that had been asked over time to show variations in public opinion about the COVID-19 vaccine. This process allowed us to refine our themes and ensure a comprehensive analysis of public opinion on vaccines. Finally, we used peer debriefing sessions during the coding process to finalize our themes. We had multiple meetings to address queries regarding the coding process and naming themes.35 These sessions were conducted not only within the research team but also with a qualitative data analyst from the first author’s institution who is an expert in qualitative research methods. The agreement in data coding between the two research team members ranged between 85% to 90% for all themes.
Results
Information sources about COVID-19 vaccine
In this dimension, there was only one survey in January 2021 that asked the public about the media source of their COVID-19 vaccine information. Results showed that social media were important sources about COVID-19 vaccines, with Facebook dominating the scene. More than one third (38%) of Americans said they got their information about COVID-19 vaccines from Facebook. YouTube was the second most popular social media platform used, with nearly one fifth (18%) of Americans seeking for COVID-19 vaccine information from this platform. Twitter and Instagram were third (14%) and fourth (12%) in popularity was TikTok, which, despite being new to the social media landscape, has emerged as a considerably important source on COVID-19 vaccines for some Americans (5%), leaving Reddit (3%), and WhatsApp (2%) trailing behind as sources used to access COVID-19 vaccine information.
Of the mainstream media sources, CNN was the most popular, with 30% of Americans saying they received information on COVID-19 vaccines from this source, followed by Fox News (23%), MSNBC (21%), and One America News (11%). While some conservative mainstream media (e.g., Fox News) have consistently received higher viewership,36 liberal outlets seem to be sought out more often with regards to COVID-19 vaccine information (see Table 1). Zheng et al.37 suggested that there is a positive relationship between online COVID-19 vaccine information seeking and vaccination intention. Liberal media outlets might have been popular sources for COVID-19 vaccine information due to the political polarization that has developed in the US concerning the pandemic between conservative and liberal segments of the public.38 Since liberals are more likely than conservatives to see the pandemic as a serious threat, they are also most likely to actively seek COVID-19 vaccination information4 and liberals tend to gravitate toward using liberal media outlets.39,40
Table 1.
Information sources i.e., mainstream media, social media, and interpersonal sources and percentage of participants who reported to have received information about COVID-19 (coronavirus) vaccine from these sources.
| Information Sources | Percent |
|---|---|
| Mainstream Media* | |
| CNN Fox News MSNBC One America News Some other cable news channels Newsmax Telemundo or Univision |
30 23 21 11 8 6 1 |
| Social Media* | |
| Facebook YouTube Some other social media sites or app TikTok |
38 18 14 12 9 5 3 2 |
| Interpersonal Sources** | |
| A doctor, nurse, or other health care provider A pharmacist A religious leader Family or friends Centers for Disease Control and Prevention State or local public health department |
79 44 17 48 60 58 |
N = 1563, January 2021, SSRS.
*Percentage of participants who responded yes in response to “In the past two weeks, did you get information about the COVID-19 (coronavirus) vaccine from … or not?”
**Percentage of participant who responded very likely or somewhat in response to “When deciding whether to get a COVID-19 vaccine, how likely are you to turn to … for information?”
In terms of the use of interpersonal sources of information related to COVID-19 vaccines, according to the results from SSRS’s survey conducted in January 2021, the majority of people said that they would be very likely to turn to healthcare professionals (e.g., doctors, nurses, or other healthcare workers (46%); CDC (31%), state or local public health departments (26%), or pharmacists (22%)) to get information. Family and friends also played an important role in giving advice to some people with about half of the respondents (48%) saying they were somewhat likely or very likely to seek advice from family or friends, while only 6% said they would go to a religious leader for information. This highlights the importance of information sources in issues related to COVID-19 vaccines for some people (see Table 1).
Over the last two decades, people have increasingly turned to social media to receive health information, especially during the COVID-19 pandemic.41 Moreover, studies have found that social media (i.e., Facebook, YouTube), mainstream media (i.e., CNN, Fox News), and interpersonal sources (i.e., doctors, family and friends), and health organizations (i.e., CDC, local health departments) have been primary sources of health information.42,43 Studies suggest that individuals who rely on non-traditional news sources or alternative guidance, rather than traditional news outlets or official government recommendations, tend to have lower perceptions of COVID-19 severity and are less likely to get vaccinated.44 Another study found that higher levels of vaccine hesitancy were a strong predictor of individuals choosing alternative sources of information.45 Other studies show that participants who trusted social media for its diverse range of views and perceived authenticity often expressed distrust toward traditional media, citing concerns about biases and agendas.46 Finally, it is possible that individuals who distrust traditional news sources may turn to social media platforms for information about vaccines.
Information about the access, effectiveness, and side effects of COVID-19 vaccine
Between January and August 2021, several surveys asked Americans about access to COVID-19 vaccines. Access to COVID-19 vaccines was asked multiple times during the first half of 2021, when vaccination campaigns were rolled out. Clearly, Americans’ information efficacy regarding access to COVID-19 vaccines saw mixed results. In January 2021 more than half of the respondents (55%) said they had enough information about who was prioritized to get COVID-19 vaccines. In May 2021, 78% said they had enough information about who would be able to get a COVID-19 vaccine. However, in terms of accessing the vaccine, only 38% said that they had enough information in August 2021. Overall, in January and February 2021, most people said that they did not have enough information about where to get COVID-19 vaccines (Table 2). In March, April, and May 2021, most participants responded that they had enough information about where they could get COVID-19 vaccines.
Table 2.
The percentage of participants who responded to have enough information when asked “do you feel you have enough information about the availability and effectiveness of the COVID-19 (coronavirus) vaccine?” based on nine different parameters.
| Survey Date | Who gets priority for vaccine | You get a covid vaccine | Where you will be able to get a COVID-19 vaccine | Access to vaccines | Effectiveness of the vaccine | Effectiveness of vaccine in children | Potential side effects | Side effects in children | Safety for children |
|---|---|---|---|---|---|---|---|---|---|
| Jan–21 (N = 1563) |
55 | 37 | – | – | 52 | – | 45 | – | – |
| Feb–21 (N = 1874) |
– | – | 55 | – | – | – | 51 | – | – |
| Mar–21 (N = 1862) |
– | – | 67 | 53 | – | – | – | – | – |
| Apr–21 (N = 1001) |
– | – | 75 | 66 | – | – | – | – | – |
| May–21 (N = 2097) |
– | – | 78 | 69 | – | – | – | – | – |
| Aug–21 (N = 1259) |
– | – | – | 38 | 42 | – | – | 38 | – |
| Dec–21 (N = 1196) |
– | – | – | – | – | 41 | – | 37 | 39 |
During the pandemic, many people had problems accessing accurate and timely information about the COVID-19 vaccines. In addition, countries prioritized different populations as COVID-19 vaccine rollouts started after the emergency authorization. In this regard, the WHO noted that COVID-19 vaccine inequity and accessibility was not only a moral but also a human rights issue. Thus, the rights-based approach was essential to making the COVID-19 vaccines easily accessible to all.47 Table 2 indicates that in April and May 2021, most respondents did not have enough information about when they would be able to get COVID-19 vaccines.
The American public, however, did not have enough information regarding effectiveness of the COVID-19 vaccines.15, 48 A little more than half of the respondents were confident about the “effectiveness of the vaccine” (52% - January 2021). Interestingly, the American public perceived that they did not have enough information about the effectiveness of the COVID-19 vaccine (57%) in August 2021 and 58% said in December 2021 that they did not have enough information about the effectiveness of the COVID-19 vaccines for children (see Table 2).
In January 2021, more than half of Americans believed they did not have enough information on the “potential side effects” (54%) of COVID-19 vaccines. Similarly, when asked about the information about side effects in children, more than 60% respondents said that they did not have enough information in August and December 2021. Only 37% people in December 2021 said they have enough information about the side effects of COVID-19 vaccine in children (Table 2). All in all, the levels of COVID-19 vaccine information efficacy were low among Americans, painting a poor picture of the COVID-19 vaccine communication landscape in the country (Table 2). During COVID-19, health organizations, medical professionals, scientists, and governments faced several challenges about the science of COVID-19 vaccination, social distancing, and face masking. These findings are consistent with other empirical studies which suggest that people expressed concerns about COVID-19 vaccine side effects. For instance, Latkin et al.’s49 study found that 64% people strongly agreed that they could get side effects of the COVID-19 vaccines. This perception perhaps could be explained by insufficient information about the effects of the COVID-19 vaccines in early 2021, about a year into the pandemic.
To contextualize our results, it is important to note that while governments initially focused on providing information about where to get the vaccine, this emphasis shifted over time to address issues of efficacy and side effects. However, these findings highlight the need for further empirical research to understand why people feel they did not receive sufficient information about vaccine efficacy, its effectiveness for children, its side effects for children, and its overall safety. Furthermore, the rapidly changing situation with multiple information policy updates during the COVID-19 pandemic made it difficult for both federal and local governments to keep pace with the changes. In the U.S. health system, information typically flows from federal to local levels, but in many cases, local and state health departments were unable to provide the public with timely or comprehensive information about the COVID-19 vaccine because they had not received sufficient guidance from federal health agencies.50 At times, information from federal agencies was also retracted. For example, the CDC initially overstated the efficacy of vaccines in preventing COVID-19 infections and focused on vaccination to the near exclusion of other mitigation measures. In 2021, CDC Director Walensky announced that vaccinated individuals could not transmit COVID-19, a statement she later retracted after widespread criticism).51
COVID-19 vaccine hesitancy
Within this dimension, we divided COVID-19 vaccine hesitancy into three sub-themes: (1) false perception, (2) skepticism, and (3) COVID-19 vaccine refusal. Many of the survey questions were included to understand the reasons why Americans refuse to get COVID-19 vaccines. In this theme, two main pollsters, Ipsos and ECPIP, deployed multiple surveys to collect public opinions on COVID-19 vaccine hesitancy. Table 3 shows that in March 2021, 42% Americans believed they did not need the vaccine, while 61% reported that cost was not a factor in their decision not to get vaccinated.
Table 3.
Percentage of respondents who reported it to be a major reason while responding to “what is the major or minor reason that you would not get agree to receive a coronavirus/COVID-19 vaccine?”.
| Survey Date | False Perception | Skepticism | Vaccine Refusal | ||||||
|---|---|---|---|---|---|---|---|---|---|
| |
It would cost too much |
You do not think you need it |
Do not think I need it |
You want to know more about how well it works |
Have seen too many mistakes from the medical care system in the past |
The vaccines were developed and tested too quickly |
Want to know more about how well they work |
Concern about side effects |
Do not get vaccines in general |
| Nov-20* (N = 1001) |
15 | 25 | - | 82 | - | - | 51 | - | - |
| Mar-21** (N = 10121) |
- | - | 42 | - | 46 | 67 | 61 | 72 | 36 |
*ECPIP.
**IPSOS.
Between November 2020 and March 2021, Ipsos and ECPIP surveys revealed that 82% of Americans expressed a desire to learn more about the vaccines and their effectiveness. False perceptions about the vaccines were a major factor contributing to vaccine hesitancy, with Ipsos surveys highlighting the significant role played by false perceptions in why people were reluctant to get vaccinated. For example, in March 2021, nearly half (46%) of Americans said they had “seen too many mistakes from the medical care system in the past.” In the same survey, a larger share of the American population (67%) attributed a major reason they did not get vaccinated was because “the vaccines were developed and tested too quickly.” More than half (61%) said they wanted “to know more about how they (the vaccines) work.” Lastly, Table 3 shows that 72% of Americans said “concerns about the side effects” of the COVID-19 vaccines were a major reason for them to consider whether to get vaccinated.
During the pandemic, Ipsos asked Americans in March 2021 about the reasons why they would receive a COVID-19 vaccine. Results demonstrated that 36% of Americans attributed the reason for their COVID-19 vaccine refusal to the fact that they did not “get vaccines in general” (Table 3). COVID-19 vaccine skepticism arose even before the vaccines were developed. Two important drivers for such skepticism among members of the public, according to Boyd52 p. 1), were “witnessing fallibility of the scientific process play out in real time, and a perceived breakdown of the distinction between experts and non-experts” (p. 1). Refusal, skepticism, and false perceptions of vaccines in general are not new. However, in the context of a global pandemic, getting the public to vaccinate is still the most effective way to stop the spread of COVID-19. Understanding vaccine skepticism and its drivers is, therefore, important to successfully convincing them to get vaccinated, hence preventing the spread of the virus. Survey results presented here indicate a dire need for better communication about the vaccines to the American public. Experts noted that the “volume and velocity of information during the COVID-19 pandemic have made it difficult for people to assess the accuracy of information”48 p. 335).
Prior studies have revealed many reasons behind vaccine hesitancy. For instance, Anas et al.53 suggest that trust in institutions, and cultural and religious beliefs influences people’s vaccination decisions in a significant manner. A systematic review of 15 studies conducted by Troiano and Nardi,54 explored the reasons behind COVID-19 vaccine hesitancy. The reasons include but are not limited to being against vaccines in general, concerns about safety/thinking that a vaccine produced in a rush is too dangerous, considering the vaccine useless because of the harmless nature of COVID-19, general lack of trust, doubts about the efficiency of the vaccine, belief to be already immunized, evidence about the vaccine. Our study also identified similar reasons for refusing the COVID-19 vaccine.
Motivations to get the COVID-19 vaccine
In this dimension, we divided the survey results into five sub-themes including (1) daily routine, (2) convenience, (3) incentives, (4) influences, and (5) travel requirement. In the first sub-theme, the survey questions focused on the public support for policies on where proof of vaccination should be shown in their everyday life activities. The second sub-theme was about the public’s willingness to get vaccinated based on how easy they could get access to the vaccines. The third sub-theme asked about incentive to get vaccinated. The fourth sub-theme was concerned with sources of influence that may motivate Americans to get vaccinated. They included endorsements from celebrities, family members, or friends. Lastly, the public was polled about whether they would get vaccinated if that was a requirement to attend sporting events, to travel, or to go to office.
In May and June 2021, poll results indicated that the American public was torn about requiring a proof of vaccination to do many daily activities, with mandating showing a proof of vaccination to “attend a sporting event” receiving slightly higher support (32% chose strongly support in May and 26% in June) (Figure 1). Opposition to this requirement, however, was stronger for shopping at “non-grocery stores” (35% in May and 34% in June). This demonstrates that although sporting events are important in the American culture, perhaps, the American public saw it as less essential compared to other daily activities (e.g., going to a salon, barber shop, returning to work, or shopping at non-grocery stores).
Figure 1.
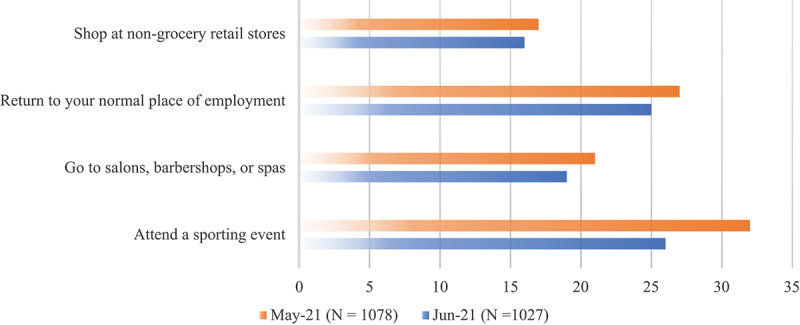
Percentage of the respondents who expressed strong support when asked “do you support or oppose having to show proof of a COVID-19 (coronavirus) vaccine to do each of the following?” May 2021 (N = 1078, IPSOS) June 2021 (N = 2288, NORC).
Between July and August 2021, participants were asked if they would be willing to get vaccinated if the vaccines were offered by mobile clinics, doctor or primary care offices, and their offices or workplaces. Most said they would not at all be likely to get vaccinated at any of these places (Table 4). This is in line with results from Dorman et al.’s14 study, which found that convenience was not a strong predictor for the public’s willingness to get vaccinated.
Table 4.
Percentage of the participants who responded very likely or somewhat likely while responding to “if each of the following were to happen, how likely, if at all, would you be to get the COVID-19 (coronavirus) vaccine?”.
| Scenarios | Jul–21 (N = 1048) | Aug-21 (N = 999) | Sep-21 (N = 1065) |
|---|---|---|---|
| Convenience to get vaccinated | |||
| You could get the vaccine at a mobile clinic that was at a convenient location for you. You could get the vaccine at your doctor or primary care provider’s office. You could get the vaccine at your office or workplace |
21 26 21 |
--18 | - |
| Incentives to get vaccinated | - | ||
| You were given paid time off by your employer to get the vaccine. You were given paid time off by your employer to get the vaccine. Your employer gave you a raise or a bonus for getting vaccinated. |
24-- | -15 25 |
- |
| Influences to get vaccinated | - | ||
| A celebrity or public figure you like endorses getting the vaccine. A friend or family member got the vaccine and talked to you about it. A friend or family member got the vaccine and talked to you about it. |
14 23- |
--21 | ---- |
| COVID-19 vaccination requirement for travel | - | ||
| If it was a requirement to travel on an airplane or by train. If it was a requirement to travel on an airplane or by train. |
-- | 23- | -22 |
Based on different types of incentives, several surveys conducted by Ipsos examined people’s willingness to get a COVID-19 vaccination. Table 4 indicates that 63% people were not at all likely to get vaccinated against COVID-19 if their employer offered paid time off in July 2021. More than half (54%) of the participants said in August 2021 that they were not at all likely to get vaccinated if their employer gave them a bonus or a raise. The pandemic continued to hinder the ability of businesses to operate at full capacity. The COVID-19 vaccine could offer a path for employees to return to work safely while protecting themselves and their fellow workers. However, employers were reluctant to mandate vaccination for their employees and considered different ways to increase employee vaccination rates.55 Investigating different vaccination motivational strategies, Berry et al.56 suggest that organizations can offer t-shirts, merchandise, or other gifts to encourage their employees to get a vaccine.
Identifying drivers for the public’s vaccination through different sources of influences is important to increase vaccine uptakes. For instance, a survey conducted by Ipsos in July 2021 shows that 70% of people said that they were not at all likely to get vaccinated even if a celebrity or a public figure endorsed the vaccine. Only 8% people were very likely to get vaccinated if their family members got it and talked about it with them (Table 4).57 study examined the effectiveness of prestige-based incentives and found that the most effective incentive was “vaccination of an expert scientist, followed by vaccination of friends and family members and knowing someone dying from the disease” (p. 1).
Poll results from August and September 2021 showed that only 10% Americans agreed that they would be very likely to get vaccinated to travel by plane or train if it was required. However, most were not at all likely to get vaccinated against COVID-19. Previous studies have identified various motivations for getting the COVID-19 vaccine. For example, Moore et al.58 highlighted several extrinsic (e.g., protecting one’s community, family, and friends), intrinsic (e.g., the desire to protect oneself from COVID-19), and structural (e.g., vaccine mandates) factors that influence people’s decision to get vaccinated. Our study found two similar motivations, but one key contrast: vaccine mandates do not appear to be effective in motivating Americans. A comparative study across four countries also found that 80% of participants who received the COVID-19 vaccine cited public health recommendations and trust in vaccine safety as the primary reasons for their decision.59
False perceptions caused vaccine refusal
Despite being recognized as one of the most successful public health achievements, vaccination is still perceived as unnecessary by many individuals.60 Prior research suggests that vaccine-hesitant individuals may refuse vaccines but agree with others; they may delay getting vaccinated or accept vaccines according to a physician-recommended schedule but may also be unsure in doing so. Therefore, vaccine hesitancy should be discussed and understood in a broader socio-political cultural context.61 However, some may still refuse vaccines without any reason.
In this study, results from different surveys on COVID-19 vaccines indicated that most people who did not plan to get vaccinated cited inaccurate information about the vaccines. For instance, AP-NORC Center for Public Affairs asked people why they did not need a COVID-19 vaccine in February 2021. Table 5 reveals that 19% believe that they did not need it because they were not a member of a high-risk group followed by 16% that they were using masks and taking precautions instead of getting vaccinated. They also believed that they did not need it because they did not belong to the group which were recommended to get it, or that COVID-19 was not a “serious illness” 14%.
Table 5.
The percentage of respondents who said yes while answering “why do you believe that you don’t need a COVID-19 (coronavirus) vaccine?”.
| Reasons | Percent |
|---|---|
| AP-NORC Center for Public Affairs* | |
| I already had COVID-19. I am not a member of a high-risk group. I am not a member of the groups currently recommended to get the COVID-19 vaccine. I do not spend time with any high-risk people. I don’t believe COVID-19 is a serious illness. I don’t think vaccines are beneficial. I plan to use masks or other precautions instead. Other |
5 19 14 15 14 10 16 5 |
| SRSS** | |
| I don’t trust the government. I don’t trust the scientists and companies that make the vaccine. I had coronavirus/COVID-19, so I think I’m immune now. I never get vaccines, generally. I’m just not concerned about coronavirus/COVID-19. I’m worried about allergies and side effects. It’s still too untested/I’m waiting to see what happens. Other |
18 17 5 9 9 16 20 5 |
| IPSOS*** | |
| COVID-19 doesn’t seriously hurt kids. COVID-19 isn’t that dangerous. My parents don’t want me to. None of my friends are getting the vaccine. None of these Skipped Something else The vaccine hasn’t been tested enough. The vaccine isn’t safe. |
11 8 16 5 8 4 8 26 15 |
*N = 1055; **N = 1669; ***N = 572.
A survey was conducted by Ipsos with 1002 registered voters in December 2020 on why people were not planning to get a COVID-19 vaccine. About 21% of the respondents said that they were not planning because they did not “trust the vaccine will work.” In addition, 13% said that they were generally against vaccines; followed by distrust of the government 10%. About 23% of the respondents did not plan to get vaccinated because the vaccine development was rushed, or they wanted more data before getting it (Figure 2).
Figure 2.
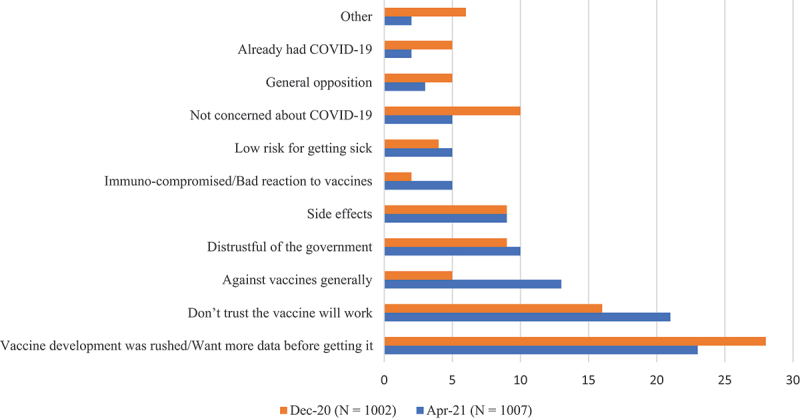
Percentage of the respondents distributed across a spectrum of reasons why they do not plan on getting a COVID (coronavirus) vaccine.
The COVID-19 vaccine hesitancy did not improve over time. Results from a survey conducted by Beacon Research in April 2021 revealed that 28% of Americans believed the vaccine development was rushed, or they needed to see more data. Another 16% said that they did not trust that vaccines would work, and 10% said that they were not concerned about COVID-19. Only 5% said that they were generally against the vaccine, already had COVID-19, and showed general opposition to the COVID-19 vaccines (Figure 2). Half a year later, according to an Ipsos survey in November 2021, 20% of Americans were still waiting to see what happens; 18% did not trust the government; Another 17% did not trust the scientists or the companies who developed the vaccines; and 16% were worried about side effects or allergic reactions from the vaccines (Table 5). Another survey showed that 26% of Americans did not plan to get vaccinated because the vaccines had “not been tested enough;” their parents did not want them to (16%); The vaccines were “not safe” (15%); or COVID-19 did “not seriously hurt kids” (Table 5).
Misinformation and fake news have played a significant role in vaccine rejection. Health literacy may also be a crucial factor in determining whether individuals choose to get vaccinated. Montagni et al.62 found that individuals who received the COVID-19 vaccine demonstrated a high ability to detect fake news and had good health literacy. Similarly, Neely and Witkowski63 discovered that belief in misinformation was associated with a statistically significant decrease in the likelihood of receiving COVID-19 vaccine boosters. Additionally, based on an analysis of over 40 countries, Singh et al.64 found a strong correlation between the perceived believability of COVID-19 misinformation and vaccine hesitancy.
Intentions to get vaccinated
Multiple surveys were deployed to measure the public’s intention to get vaccinated based on vaccine availability and a few other scenarios. For instance, SSRS conducted a survey in February 2021 about people’s intention to get vaccinated based on availability. Table 6 shows that 75% people would be very likely to get vaccinated if the vaccines were available in their doctor’s office, followed by 61% at a local pharmacy, 55% at hospital, 49% at their community clinic, and 48% at their workplace. It also indicates that 27% of people responded that they were not at all likely to get vaccinated even if it was available at a grocery store, followed by 20% at their workplace, 18% at a local school or a vaccination site run by the government, and 11% at a local community clinic. These findings suggest that traditional vaccination places like doctor offices, pharmacies, and hospitals were not among the most popular choices where American would prefer to go to for vaccination. Newly set-up vaccination sites were, however, most picked by Americans, demonstrating that offering COVID-vaccines at a convenient place was, indeed, an effective way to make the vaccines more accessible to people.
Table 6.
The percentage of respondents who responded very likely or somewhat likely when asked which scenario of vaccine availability or endorsement could likely lead to their decision to get a vaccination.
| Reasons | Percent |
|---|---|
| Intention to get a vaccination if available at* | |
| A community health clinic A grocery store A hospital A large vaccination site run by the government A local church or religious center A local pharmacy A local school Your own doctor’s office Your workplace |
78 53 81 67 64 86 68 89 63 |
| Intention to get vaccinated based on scenario** | |
| If President (Donald) Trump said it was safe If the cost were completely covered by insurance If the FDA (Food and Drug Administration) said it was safe If you could get it easily, from a walk-in or drive-thru clinic If you had to make an appointment and get it at a hospital If it cost you $100 If you were paid $100 to receive the vaccine |
19 56 54 50 37 26 26 |
*N = 1874, February 2021, SSRS.
**N = 1075, September 2020, IPSOS.
Another way to measure intention to get vaccinated is based on different scenarios. For instance, IPSIS conducted a survey in September 2020 when the vaccine was only authorized for emergency use only. It is called first-generation vaccine. The survey shows that 59% of people said that they would not be at all likely to get vaccinated if President Trump said it was safe, followed by 49% if they were paid $100 to receive it, and 48% if it cost them $100 to get it. Since it was a first-generation vaccine, people were not sure if the cost of it was going to be covered by the government or their insurance company. When asked by Ipsos in September 2020, 25% said that they would be very likely to get it if the cost was covered by their insurance, followed by 20% if they could get it from a drive-thru clinic, and 17% said they would get it only if the FDA said it was safe (Table 6). Money incentives were a strong driver for vaccination among Americans. Results in Table 6 reveals that only 11% of respondents said they would get vaccinated if they got paid $100. Findings from previous research show that monetary incentives did not work in other countries. For example, a randomized controlled trial conducted in Sweden suggested that paying $24 only increased the vaccination rate by 4.2%.11 In the US, however, several experimental studies65–67 confirmed the influence of financial incentives on willingness to get vaccinated by members of the American public.
The intention to get vaccinated for COVID-19 is a key predictor of actual vaccination uptake. Some surveys have reported lower intentions to receive the COVID-19 vaccine among women.68 Others like Yasmin et al.17 suggested a strong correlation between being a member of a racial minority, such as African American, and a lower intention to get vaccinated. They also identified sex, race, age, education level, and income status as significant factors influencing vaccination intentions. Overall, vaccination intentions were lowest among Black/African American individuals, as well as pregnant or breastfeeding women. Similarly, Yenew et al.69 found that higher levels of perceived susceptibility to and severity of COVID-19, as well as perceived vaccine benefits and cues to action, positively predicted the intention to receive the vaccine. In contrast, higher perceived barriers to vaccination were negatively associated with vaccination intention. Our study found both similar and contrasting results.
Discussion
This systematic review of public opinion about COVID-19 vaccines reported results from multiple polls in the US. It provides a comprehensive understanding of Americans’ opinion about COVID-vaccines during nearly three years when the pandemic was raging across the US and in other parts of the world. This review yielded several important practical, policy, and theoretical implications. First, COVID vaccine refusal was common. A frequently attributed reason was based upon the perception that the vaccine development was rushed and that members of the public needed more information. However, as the pandemic went by months later, when information about the vaccine development became available, the public’s COVID-19 vaccine skepticism saw very little change. This shows that transparency and effective communication with the public about science is becoming fundamentally important and needs to be provided properly from the beginning of a health crisis.48,70 It could also be explained by the likelihood that vaccine skeptics were hard to sway by simply providing them with more information. This raises a noteworthy theoretical point about the appropriateness of using the information deficit model,71 especially with regards to vaccine hesitancy. That is, providing accurate information alone is not enough in vaccination campaigns. Other factors need to be considered to successfully persuade members of the public to get vaccinated.
These findings have broad international relevance in understanding vaccine hesitancy and public attitudes toward vaccination. Previous research suggests that vaccine acceptance levels tend to remain stable across Western countries, with few exceptions. In a survey of vaccine acceptance conducted across 23 countries, Lazarus et al.72 observed a similar pattern of COVID-19 vaccine hesitancy in several developed nations. For instance, in 2022, the United States had a vaccine hesitancy rate of 19.8%, similar to other developed countries – such as the United Kingdom (19.6%), France (18.3%), Germany (21.9%), and Sweden (20.8%) that reported comparable levels of hesitancy. These findings highlight that the issue of vaccine hesitancy is widespread and increasingly urgent on a global scale, underscoring the need for developing comprehensive communication strategies to address this growing public health concern across many countries. Other studies provide valuable insights concerning vaccine confidence. Larson et al.73 found that the European region has the lowest levels of confidence in vaccine safety, with France being the least confident country globally. While vaccine confidence is low in parts of Europe, countries like Bangladesh, Ecuador, and Iran reported the highest levels of agreement that vaccines are important. Our study observed similar trends, with the general public in the United States expressing significant concerns about vaccine safety.
Practical implications
Practically, our findings are helpful for public health scholars and practitioners, health communication scholars, health organizations such as the CDC, state and local health departments, and research organizations that examine public opinion concerning vaccine-related issues among various populations. For instance, results from our poll crosstabulations corroborated this conclusion and suggested that trust is key to convincing the public to take preventive measures for battling health crises. This includes trust in various types of social, political, and scientific institutions and authorities. Gaining public trust is not easy and may not be dependent only on providing sufficient information. Perhaps, health communication campaign messages need to devise plans to consider the factors that influence earning trust from different audiences when approaching members of the public. For example, using persuasive techniques like the two-step flow theory which emphasizes the role of key opinion leaders or social media influencers could be helpful in gaining trust from members of different population groups and swaying their attitudes and opinions on vaccine, a deeply polarized issue.
Influence on members of the public concerning the issue of vaccination may come from various sources. Some people may be more influenced by doctors; others might listen to family or friends. Identifying influential sources to use when providing vaccination information is, therefore, important to the success of vaccination campaigns. Perhaps, campaigns can emulate the information dissemination successes of the current fragmented media environment, where mass communication is segmented to target smaller groups of populations, reducing the gap between mass and individualized communication. Interestingly, Table 1 highlights the importance of different social, mainstream, and interpersonal sources of health information about vaccines. The results may be helpful to health organizations in disseminating their messages through popular channels. In addition, health information seeking is important to decision-making on health treatments.74 It is evident that there is no one-message-that-fits-all, even if the message is about a global pandemic that has affected everyone. This finding highlights the importance of interpersonal communication in conveying health messages. Interestingly, it is in line with the second finding of this study which emphasizes trust as an important aspect in persuading the public to get vaccinated. Effective interpersonal communication can be used help restore trust in science and institutions among the public.
The decision to receive a vaccination can be influenced by individuals’ reliance on different health information sources. These sources can shape public attitudes and beliefs about vaccination,75 which in turn impact vaccine uptake. Hwang76 explored how health information sources are linked to perceived vaccine efficacy and safety, which then affect influenza vaccine uptake. The study suggested that individuals who valued medical professionals, medical journals, and newspaper articles were more likely to perceive vaccines as effective and, consequently, more likely to receive the influenza vaccine. In contrast, individuals who relied more on social media were less likely to perceive vaccine efficacy and, as a result, were less likely to get vaccinated. Similarly, Park et al.44 examined how the source of COVID-19 information influenced perceptions of COVID-19 severity and the likelihood of getting vaccinated among Medicare beneficiaries. They found that individuals who relied on non-traditional sources, compared to those who trusted traditional news outlets or guidance from government officials, had lower perceptions of COVID-19 severity and were less likely to get the vaccine. Those relying on social media had the lowest levels of agreement on key measures, including the belief that COVID-19 is more contagious than the flu, more deadly than the flu, that everyone should take precautions, and that they would get the COVID-19 vaccine. Our study found that social media was also the primary source of information related to COVID-19 for many participants (see Table 1). These findings suggest that governments should leverage social media platforms to disseminate messages during health crises. Additionally, they highlight the growing reliance on social media as a primary source of information, with many people moving away from traditional media channels. While trust in media plays a significant role in this shift, traditional media sources still hold greater influence when it comes to decisions about vaccination.
Policy implications
The findings of this study are also useful to policy makers who work to reduce COVID-19-related morbidity and mortality by suggesting solutions they might adopt related to promoting the safety of social gatherings, sports events, travel, and work. Results from multiple surveys indicated that mandating vaccination, even during a global pandemic, is never a good solution. As findings from this study demonstrate, policies to require members of the public to show proof of vaccination to access various settings, including sporting events, barber shops, grocery stores, traveling, or work would have been met with strong resistance. This is understandable since members of the American public are known to react negatively to policies that may infringe on their individual rights. Reactance theory can provide valuable insights for informing the development and implementation of COVID-19 related policies. Reactance theory suggests individuals have a natural inclination to resist attempts to limit their freedom or control their behavior. In addition, this theory posits that when people perceive a threat to their freedom, they experience reactance, which can manifest as increased motivation to restore or assert their autonomy. In the context of COVID-19 related policies, reactance theory can help scholars and practitioners understand how individuals may react when faced with regulations or restrictions.77 Further, this also presents a dilemma concerning how to deal with a contagious health crisis that requires curbing human mobility. In addition, a lengthy and complex pandemic like COVID-19 inevitably exposes social and economic inequality, where those with lower income may not be able to afford to follow lockdown guidelines or to stay at home. Policies that limit mobility freedom are not likely to work if existing inequalities are not addressed in any solution plan.78
Furthermore, this study also found that besides accurate information, transparency about vaccine development, trust, and interpersonal communication, the convenience of vaccination sites and financial incentives can help boost vaccination rates among members of the American public. This finding is in line with results from experimental research conducted in the US which found a statistically significant surge in participants’ intention to get vaccinated if financial incentives were offered.65–67 The cross-sectional results from analyzing public opinion polls present a viable solution to curbing the pandemic if vaccinate rates are low. It is important to note that this solution may not work in other countries as members of the public in other cultures may not be swayed by financial incentives as indicated in previous research.11 During the COVID-19 pandemic, the US erected many drive-through clinics and vaccination sites across the country. Results from our analysis indicated that this is a very effective strategy to help boost vaccination among the American public.
Theoretical implications
Our findings contribute to the existing literature on vaccine hesitancy, vaccine confidence, vaccine safety, health information sources, motivations to get vaccinated, message design, and COVID-19 related policies. In addition, there is an agreement (range, 88–100%) among the global experts that communication issues remain an important area of risk and opportunity for ending COVID-19 as a public health threat globally. “Policymakers and public health agencies should have taken special care when communicating the causation of and continuing accountability for the pandemic”48 p. 334). Indeed, COVID-19 vaccines are effective and safe against all variants, however, often research findings do not reach ordinary people in society to provide enough about the efficacy of vaccines. Such a disconnection between science and the public eventually leads to information deficits among members of the public.70,79 Theoretically, this study adds caution to the overreliance on using the information deficit model in communicating science. While providing sufficient accurate information is necessary, over relying on that ignores the information consumption process, which drives (in)actions among members of the public, especially when communicating complex scientific issues like the COVID-19 vaccines. Thus, more comprehensive theoretical frameworks are needed to understand the COVID-19 vaccine hesitancy issue, especially in the context of increasing politicization of scientific issues and rampant misinformation being circulated online. As the polls included in this study indicate trust in and concerns around vaccine developments and effectiveness play major roles in the public’s acceptance of COVID-19 vaccines, in addition to the information deficit model, trust in science, persuasion theories, and opinion leading are a few important theoretical concepts and frameworks in explaining the broad vaccine hesitancy issue. Our results challenge the argument that simply providing accurate information is sufficient to convince the public about a scientific issue. Our findings can also help in designing communication programs and messages to tackle vaccine hesitancy.
Limitations and future research
This study has several limitations. First, the data exclusively originate from the Roper Center for Public Opinion Research, without inclusion of other datasets encompassing various polls conducted throughout the COVID-19 pandemic. Future studies should incorporate global surveys such as those from the Pew Research Center, the World Values Survey, and Eurobarometer to track how public opinion about vaccines changes over time. Additionally, including individual-level data could enhance the replicability and reproducibility of the findings. While we have discussed the generalizability of our results, it is important to exercise caution when applying these findings to low-income countries, as contextual differences may affect vaccine perceptions and behaviors. Second, this study is descriptive and exploratory in nature, precluding the establishment of causal relationships based on its findings. Future studies should also test these findings using nationally representative samples to validate the results of these public opinion polls. Finally, the research did not account for sample characteristics such as age, gender, education, and personal health, which could provide valuable context for interpreting the results. Future studies should consider demographic characteristics to better interpret these findings and inform targeted health communication strategies. Since surveys are often cross-sectional, caution is needed when making broad claims about public opinion on any public health issue, as these opinions may change over time. Despite these limitations, this research represents a pioneering effort in systematically analyzing public opinion polls on COVID-19 vaccines in the US, thereby advancing scholarly understanding of the public’s attitudes toward COVID-19 vaccines. Finally, these findings offer valuable insights into various aspects of COVID-19 vaccine hesitancy, with implications that extend beyond the U.S. context. Throughout the results and discussion sections, we have also outlined strategies for addressing vaccine hesitancy in the U.S. to help guide future public health efforts
Biographies
Muhammad Ittefaq is an assistant professor in the School of Communication Studies at James Madison University. He has published in numerous journal articles in top communication journals such as Health Communication, Environmental Communication, Journal of Science Communication, and International Journal of Communication. Dr. Ittefaq’s research examines the ways in which people consume and interact with information through mainstream and social media, including how they interpret scientific messages, make decisions related to climate and health, and support policies related to science.
Hong Tien Vu is an associate professor in William Allen White School of Journalism and Mass Communications at University of Kansas. Dr. Vu’s research focuses on global/development communication and digital media, with other interests including communication for global change.
Ali Zain is an assistant professor in strategic communication in Walter Cronkite School of Journalism and Mass Communication at Arizona State University. His research focuses on studying strategic message features that drive public perception, engagement, and behavioral outcomes in a range of contexts including health and science communications, misinformation, information processing, and societal disparities.
Tayyeb Ramazan is a lecturer at University of Lahore. Currently, he is finishing his PhD in the School of Communication Studies at University of Punjab Pakistan.
Gary L. Kreps serves as a Distinguished University Professor of Communication and Founding Director of the Center for Health and Risk Communication at George Mason University. His research examines the influences of strategic evidence-based communication programs and practices on reducing health risks and enhancing health outcomes, with a focus on promoting health equity in society.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Authors’ contributions
MI, HV, TR, GK, and AZ participated in the conception and design of the paper. MI collected the data and AZ analyzed the data. HV and GK edited and critically reviewed the manuscript. All authors read and approved the final manuscript.
References
- 1.Malik AA, McFadden SM, Elharake J, Omer SB.. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sah P, Vilches TN, Moghadas SM, Fitzpatrick MC, Singer BH, Hotez PJ, Galvani AP. Accelerated vaccine rollout is imperative to mitigate highly transmissible COVID-19 variants. EClinicalMedicine. 2021;35:100865. doi: 10.1016/j.eclinm.2021.100865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolsen T, Palm R. Politicization and COVID-19 vaccine resistance in the U.S. Prog Mol Biol Transl Sci. 2022;188(1):81–15. doi: 10.1016/bs.pmbts.2021.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen X, Ariati J, Li M, Kreps GL. Examining the influences of COVID-19 information avoidance and uncertainty on perceived severity of the pandemic: applications from the health belief model and Weick’s model of organizing. Health Behav Res. 2022;5(3). doi: 10.4148/2572-1836.1151. [DOI] [Google Scholar]
- 5.Hotez PJ, Nuzhath T, Colwell B. Combating vaccine hesitancy and other 21st century social determinants in the global fight against measles. Curr Opin Virol. 2020;41:1–7. doi: 10.1016/j.coviro.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Kamboh SA, Ittefaq M, Sahi AA. Journalistic routines as factors promoting COVID-19 vaccine hesitancy in Pakistan. Third World Q. 2022;43(1):278–287. doi: 10.1080/01436597.2021.1995713. [DOI] [Google Scholar]
- 7.Li M, Yang B-K, Yu Z, Kreps X, Chen GL, Kansangra R, Kansangra R. Exploring factors associated with Chinese-Americans’ willingness to receive an additional hypothetical annual dose of the COVID-19 vaccine. Vaccines. 2023;11(1):11. doi: 10.3390/vaccines11010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC . COVID data tracker. Centers for Disease Control and Prevention. 2023. https://covid.cdc.gov/covid-data-tracker.
- 9.Fisk RJ. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Global Health J. 2021;5(1):51–55. doi: 10.1016/j.glohj.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson D, Bradbury‐Jones C, Baptiste D, Gelling L, Morin K, Neville S, Smith GD. Life in the pandemic: some reflections on nursing in the context of COVID‐19. J Clin Nurs. 2020;29(13–14):2041–2043. doi: 10.1111/jocn.15257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campos-Mercade P, Meier AN, Schneider FH, Meier S, Pope D, Wengström E. Monetary incentives increase COVID-19 vaccinations. Science. 2021;374(6569):879–882. doi: 10.1126/science.abm0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khazanov GK, Stewart R, Pieri MF, Huang C, Robertson CT, Schaefer KA, Ko H, Fishman J. The effectiveness of financial incentives for COVID-19 vaccination: a systematic review. Preventative Med. 2023;172:107538–107538. doi: 10.1016/j.ypmed.2023.107538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Persad G, Emanuel EJ. Ethical considerations of offering benefits to COVID-19 vaccine recipients. JAMA : The J Am Med Assoc. 2021;326(3):221–222. doi: 10.1001/jama.2021.11045. [DOI] [PubMed] [Google Scholar]
- 14.Dorman C, Perera A, Condon C, Chau C, Qian J, Kalk K, DiazDeleon D. Factors associated with willingness to be vaccinated against COVID-19 in a large convenience sample. J Community Health. 2021;46(5):1013–1019. doi: 10.1007/s10900-021-00987-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng H, Jiang S, Rosenthal S. Linking online vaccine information seeking to vaccination intention in the context of the COVID-19 pandemic. Sci Commun. 2022;44(3):320–346. doi: 10.1177/10755470221101067. [DOI] [Google Scholar]
- 16.Pourrazavi S, Fathifar Z, Sharma M, Allahverdipour H. COVID-19 vaccine hesitancy: a systematic review of cognitive determinants. Health Promot Perspectives. 2023;13(1):21–35. doi: 10.34172/hpp.2023.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yasmin F, Najeeb H, Moeed A, Naeem U, Asghar MS, Chughtai NU, Yousaf Z, Seboka BT, Ullah I, Lin CY, et al. COVID-19 vaccine hesitancy in the United States: a systematic review. Front Public Health. 2021;9:770985. doi: 10.3389/fpubh.2021.770985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Betsch C, Korn L, Sprengholz P, Felgendreff L, Eitze S, Schmid P, Böhm R. Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proc Natl Acad Sci - PNAS. 2020;117(36):21851–21853. doi: 10.1073/pnas.2011674117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freeman D, Loe BS, Yu L-M, Freeman J, Chadwick A, Vaccari C, Shanyinde M, Harris V, Waite F, Rosebrock L, et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): a single-blind, parallel-group, randomised controlled trial. The Lancet. Public Health. 2021;6(6):e416–e427. doi: 10.1016/S2468-2667(21)00096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jamison AM, Quinn SC, Freimuth VS. “You don’t trust a government vaccine”: narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sciamp; Med. 2019;221:87–94. doi: 10.1016/j.socscimed.2018.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parente DJ, Ojo A, Gurley T, LeMaster JW, Meyer M, Wild DM, Mustafa RA. Acceptance of COVID-19 vaccination among health system personnel. The J Am Board of Fam Med. 2021;34(3):498–508. doi: 10.3122/jabfm.2021.03.20054. [DOI] [PubMed] [Google Scholar]
- 22.Szilagyi PG, Thomas K, Shah MD, vizueta N, Cui Y, Vangala S, Kapteyn a national trends in the US Public’s likelihood of getting a COVID-19 vaccine—April 1 to December 8. JAMA: The J Am Med Assoc. 2020;325(4):396–398. doi: 10.1001/jama.2020.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baines A, Ittefaq M, Abwao M. #scamdemic, #plandemic, or #scaredemic: what parler social media platform tells us about COVID-19 vaccine. Vaccines. 2021;9(5):421–. doi: 10.3390/vaccines9050421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y, Long J, Jun J, Kim S, Zain A, Piacentine C. Anti-intellectualism amid the COVID-19 pandemic: the discursive elements and sources of anti-Fauci tweets. Public Underst Sci. 2023;32(5):641–657. doi: 10.1177/09636625221146269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ittefaq M, Hussain SA, Fatima M. COVID-19 and social-politics of medical misinformation on social media in Pakistan. Media Asia. 2020;47(1–2):75–80. doi: 10.1080/01296612.2020.1817264. [DOI] [Google Scholar]
- 26.Seo H, Liu Y, Ittefaq M, Shayesteh F, Kamanga U, Baines A. International migrants and coronavirus disease 2019 vaccinations: social media, motivated information management, and vaccination willingness. Digit Health. 2022;8:205520762211259. doi: 10.1177/20552076221125972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hossain MB, Alam MZ, Islam MS, Sultan S, Faysal MM, Rima S, Hossain MA, Mamun AA. Health belief model, theory of planned behavior, or psychological antecedents: what predicts COVID-19 vaccine hesitancy better among the Bangladeshi adults?. Front Public Health. 2021;9. doi: 10.3389/fpubh.2021.711066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freeland EP. Public opinion: social attitudes. In: Smelser NJ, and Baltes PB, editors. International encyclopedia of the social & behavioral sciences. 2nd ed. Oxford, England: Elsevier; 2015. p. 562–568. [Google Scholar]
- 29.SteelFisher GK, Findling MG, Caporello HL, Stein RI. Has COVID-19 threatened routine childhood vaccination? Insights from US public opinion polls. Health Aff Forefr. 2023; doi: 10.1377/forefront.20230605.570346. [DOI] [Google Scholar]
- 30.Blendon RJ, Benson JM, Schneider EC. The future of health policy in a partisan United States: insights from public opinion polls. Jama. 2021;325(13):1253–1254. doi: 10.1001/jama.2021.1147. [DOI] [PubMed] [Google Scholar]
- 31.Ho SS, Brossard D, Scheufele DA. Trends: public reactions to global health threats and infectious diseases. Public Opin Q. 2007;71(4):671–692. doi: 10.1093/poq/nfm041. [DOI] [Google Scholar]
- 32.Gagneux-Brunon A, Botelho-Nevers E, Bonneton M, Peretti-Watel P, Verger P, Launay O, Ward JK. Public opinion on a mandatory COVID-19 vaccination policy in France: a cross-sectional survey. Clin Microbiol Infect. 2022;28(3):433–439. doi: 10.1016/j.cmi.2021.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Featherstone JD, Ruiz JB, Barnett GA, Millam BJ. Exploring childhood vaccination themes and public opinions on twitter: a semantic network analysis. Telematics and Inf. 2020;54:101474–. doi: 10.1016/j.tele.2020.101474. [DOI] [Google Scholar]
- 34.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahmadian S, Khaghanizadeh M, Khaleghi E, Zarghami MH, Ebadi A. Stressors experienced by the family members of brain-dead people during the process of organ donation: a qualitative study. Death Stud. 2020;44(12):759–770. doi: 10.1080/07481187.2019.1609137. [DOI] [PubMed] [Google Scholar]
- 36.The Associated Press . Ratings show fox news viewers tuning out Jan. 6 hearings. 2022. https://apnews.com/article/jan-6-hearings-fox-news-ratings-c898174e44e9a2e342c87ed084c9f699.
- 37.Zheng H, Jiang S, Wu Q. Factors influencing COVID-19 vaccination intention: the roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Educ Couns. 2022;105(2):277–283. doi: 10.1016/j.pec.2021.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kerr J, Panagopoulos C, van der Linden S. Political polarization on COVID-19 pandemic response in the United States. Pers Individ Differ. 2021;179:110892. doi: 10.1016/j.paid.2021.110892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blank G, Reisdorf B. Digital inequalities and public health during COVID-19: media dependency and vaccination. Inf, Commun Soc. 2023;26(5):1045–1065. doi: 10.1080/1369118X.2023.2166356. [DOI] [Google Scholar]
- 40.Lueck JA, Callaghan T. Inside the ‘black box’ of COVID-19 vaccination beliefs: revealing the relative importance of public confidence and news consumption habits. Soc Sciamp Med. 2022;298:114874. doi: 10.1016/j.socscimed.2022.114874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neely S, Eldredge C, Sanders R. Health information seeking behaviors on social media during the COVID-19 pandemic among American social networking site users: survey study. J Med Internet Res. 2021;23(6):e29802. doi: 10.2196/29802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Geana MV, Kimminau KS, Greiner KA. Sources of health information in a multiethnic, underserved, urban community: does ethnicity matter? J Health Commun. 2011;16(6):583–594. doi: 10.1080/10810730.2011.551992. [DOI] [PubMed] [Google Scholar]
- 43.Jacobs W, Amuta AO, Jeon KC, Alvares C. Health information seeking in the digital age: an analysis of health information seeking behavior among US adults. Cogent Soc Sci. 2017;3(1):1302785. doi: 10.1080/23311886.2017.1302785. [DOI] [Google Scholar]
- 44.Park S, Massey PM, Stimpson JP. Primary source of information about COVID-19 as a determinant of perception of COVID-19 severity and vaccine uptake. J GEN Intern MED. 2021;36(10):3088–3095. doi: 10.1007/s11606-021-07080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bellomo RK, Cerabona V, Massimi A, Migliara G, Sparano M, Novello F, Schilirò T, Siliquini R, Villari P, De Vito C. Who chooses alternative sources of information about childhood vaccinations? A cross-sectional study. Front Public Health. 2023;11:11. doi: 10.3389/fpubh.2023.1225761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Newman N, Fletcher R. Bias, bullshit and lies: audience perspectives on low trust in the media. SSRN J. [Report]. 2017; doi: 10.2139/ssrn.3173579. [DOI] [Google Scholar]
- 47.Torreele E, Amon JJ. Equitable COVID-19 vaccine access. Health Hum Rights. 2021;23(1):273–288. [PMC free article] [PubMed] [Google Scholar]
- 48.Lazarus JV, Romero D, Kopka CJ, Karim SA, Abu-Raddad LJ, Almeida G, Baptista-Leite R, Barocas JA, Barreto ML, Bar-Yam Y, et al. A multinational delphi consensus to end the COVID-19 public health threat. Nature. 2022;611(7935):332–345. doi: 10.1038/s41586-022-05398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Latkin CA, Dayton L, Miller JR, Yi G, Jaleel A, Nwosu CC, Yang C, Falade-Nwulia O. Behavioral and attitudinal correlates of trusted sources of COVID-19 vaccine information in the US. Behavioral Sci. 2021;11(4):56. doi: 10.3390/bs11040056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ittefaq M. “Beating your head against the wall”: burnout on the rise among local health department communication officials. Health Secur. 2023;21(6):44–449. doi: 10.1089/hs.2023.0002. [DOI] [PubMed] [Google Scholar]
- 51.Haroun A, Brueck H. CDC director says data ‘suggests that vaccinated people do not carry the virus’. Business insider. 2021. https://www.businessinsider.com/cdc-director-data-vaccinated-people-do-not-carry-covid-19-2021-3.
- 52.Boyd K. Beyond politics: additional factors underlying skepticism of a COVID-19 vaccine. HPLS. 2021;43(1):12–12. doi: 10.1007/s40656-021-00369-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Anas AL, Salifu M, Zakaria HL. COVID-19 pandemic and vaccination skepticism. Hum Arenas. 2023; doi: 10.1007/s42087-023-00334-w. [DOI] [Google Scholar]
- 54.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Berkman BE, Miner SA, Wendler DS, Grady C. The ethics of encouraging employees to get the COVID-19 vaccination. J Public Health Pol. 2022;43(2):311–319. doi: 10.1057/s41271-022-00347-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berry SD, Baier RR, Syme M, Gouskova N, Bishnoi C, Patel U, Leitson M, Gharpure R, Stone ND, Link‐Gelles R, et al. Strategies associated with COVID-19 vaccine coverage among nursing home staff. J Am Geriatrics Soc. 2022;70(1):19–28. doi: 10.1111/jgs.17559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salali GD, Uysal MS. Effective incentives for increasing COVID-19 vaccine uptake. Psychol Med. 2023;53(7):3242–3244. doi: 10.1017/S0033291721004013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moore R, Purvis RS, Hallgren E, Willis DE, Hall S, Reece S, CarlLee S, Judkins H, McElfish PA. Motivations to vaccinate among hesitant adopters of the COVID-19 vaccine. J Community Health. 2021;47(2):237–245. doi: 10.1007/s10900-021-01037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leung J, Price D, McClure-Thomas C, Bonsaksen T, Ruffolo M, Kabelenga I, Lamph G, Geirdal AØ. Motivation and hesitancies in obtaining the COVID-19 vaccine—A cross-sectional study in Norway, USA, UK, and Australia. Vaccines. 2023;11(6):1086. doi: 10.3390/vaccines11061086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: an overview. Hum Vaccines Immunotherapeutics. 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Streefland P, Chowdhury AMR, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sciamp Med. 1999;49(12):1705–1716. doi: 10.1016/S0277-9536(99)00239-7. [DOI] [PubMed] [Google Scholar]
- 62.Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health. 2021;43(4):695–702. doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Neely SR, Witkowski K. Belief in misinformation and acceptance of COVID-19 vaccine boosters: a survey analysis. PEC Innov. 2024;4:100261. doi: 10.1016/j.pecinn.2024.100261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Singh K, Lima G, Cha M, Cha C, Kulshrestha J, Ahn Y, Varol O, Cresci S. Misinformation, believability, and vaccine acceptance over 40 countries: takeaways from the initial phase of the COVID-19 infodemic. PLOS ONE. 2022;17(2):e0263381. doi: 10.1371/journal.pone.0263381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Andresen JA, Harris JN, Mauro C, Zimet GD, Rosenthal SL. The impact of financial incentives on COVID-19 vaccination intention among a sample of US adults. Preventative Med Rep. 2022;29:101962. doi: 10.1016/j.pmedr.2022.101962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carpio CE, Coman IA, Sarasty O, García M. COVID-19 vaccine demand and financial incentives. Appl Health Econ Health Policy. 2021;19(6):871–883. doi: 10.1007/s40258-021-00687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fishman J, Salmon MK, Scheitrum D, Schaefer KA, Robertson CT. Comparative effectiveness of mandates and financial policies targeting COVID-19 vaccine hesitancy: a randomized, controlled survey experiment. Vaccine. 2022;40(51):7451–7459. doi: 10.1016/j.vaccine.2022.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Berg MB, Lin L. Predictors of COVID-19 vaccine intentions in the United States: the role of psychosocial health constructs and demographic factors. Transl Behavioral Med. 2021;11(9):1782–1788. doi: 10.1093/tbm/ibab102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yenew C, Dessie AM, Gebeyehu AA, Genet A. Intention to receive COVID-19 vaccine and its health belief model (HBM)-based predictors: a systematic review and meta-analysis. Hum Vaccines Immunotherapeutics. 2023;19(1). doi: 10.1080/21645515.2023.2207442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guenther L, Ruhrmann G. Scientific evidence and mass media: investigating the journalistic intention to represent scientific uncertainty. Public Underst Sci. 2016;25(8):927–943. doi: 10.1177/0963662515625479. [DOI] [PubMed] [Google Scholar]
- 71.Allum N, Sturgis P, Tabourazi D, Brunton-Smith I. Science knowledge and attitudes across cultures: a meta-analysis. Public Underst Sci. 2008;17(1):35–54. doi: 10.1177/0963662506070159. [DOI] [Google Scholar]
- 72.Lazarus JV, Wyka K, White TM, Picchio CA, Gostin LO, Larson HJ, Rabin K, Ratzan SC, Kamarulzaman A, El-Mohandes A. A survey of COVID-19 vaccine acceptance across 23 countries in 2022. Nat Med. 2023;29(2):366–375. doi: 10.1038/s41591-022-02185-4. [DOI] [PubMed] [Google Scholar]
- 73.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12(C):295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jia X, Pang Y, Liu LS. Online health information seeking behavior: a systematic review. Healthcare. 2021;9(12):1740. doi: 10.3390/healthcare9121740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gargano LM, Underwood NL, Sales JM, Seib K, Morfaw C, Murray D, Hughes JM. Influence of sources of information about influenza vaccine on parental attitudes and adolescent vaccine receipt. Hum Vaccines Immunotherapeutics. 2015;11(7):1641–1647. doi: 10.1080/21645515.2015.1038445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hwang J. Health information sources and the influenza vaccination: the mediating roles of perceived vaccine efficacy and safety. J Health Commun. 2020;25(9):727–735. doi: 10.1080/10810730.2020.1840675. [DOI] [PubMed] [Google Scholar]
- 77.Kriss LA, Quick BL, Rains SA, Barbati JL. Psychological reactance theory and COVID-19 vaccine mandates: the roles of threat magnitude and direction of threat. J Health Commun. 2022;27(9):654–663. doi: 10.1080/10810730.2022.2148023. [DOI] [PubMed] [Google Scholar]
- 78.Hall MA, Studdert DM. “Vaccine passport” certification—policy and ethical considerations. N Engl J Med. 2021;385(11):e32. doi: 10.1056/NEJMp2104289. [DOI] [PubMed] [Google Scholar]
- 79.Ghalavand H, Panahi S, Sedghi S. How social media facilitate health knowledge sharing among physicians. Behaviour Inf Technol. 2022;41(7):1544–1553. doi: 10.1080/0144929X.2021.1886326. [DOI] [Google Scholar]


