Abstract
Rapid diagnostic tests (RDTs) are crucial for diagnosing malaria in resource-limited settings. These tests, which detect the histidine-rich protein 2 (PfHRP2) and its structural homologue PfHRP3, are specifically designed to identify Plasmodium falciparum. Deletion of the Pfhrp2 gene in parasite has been reported in India and other malaria-endemic countries. Therefore, periodic surveillance of Pfhrp2 and Pfhrp3 genetic deletions is crucial. We conducted a study to examine these gene deletions in P. falciparum isolates from nine malaria-endemic states in India. In this study, we analyzed 1,558 samples that were microscopically confirmed to be P. falciparum positive. We isolated genomic DNA from all the aforementioned samples, followed by PCR amplification of the Pfhrp2/3 gene. The results showed that the deletion rates for Pfhrp2 and Pfhrp3 genes were 0.44% and 1.47%, respectively. These findings indicate that the gene deletions in all nine states are at low level. Despite these low deletion rates, continuous surveillance is crucial to monitor the efficiency of HRP2 based malaria RDTs. It is recommend that conducting large-scale studies which include other endemic states in India to gain a more comprehensive understanding of the prevalence and impact of these gene deletions over time. This ongoing surveillance will ensure that diagnostic strategies remain effective and that any emerging trends in gene deletions are promptly addressed to achieve the malaria control and elimination.
Introduction
Malaria is at the forefront of the World Health Organization’s (WHO) disease elimination programs, given its significant global mortality rates each year. In 2022, India contributed about 65.7% of all malaria cases in the WHO South-East Asia region, with P. falciparum accounting for nearly 54% of these cases [1]. Despite a substantial reduction in malaria cases in 2023, there were still 0.22 million reported cases, compared to 214 million cases in 2015 [2]. These cases predominantly come from rural parts of India, particularly in areas with limited resources and insufficient medical infrastructure [3]. Malaria diagnosis in these regions relies mainly on microscopy and rapid diagnostic test (RDT) kits, each with its own advantages and limitations [3, 4]. Histidine-rich protein II (HRP2), a protein produced exclusively by P. falciparum, enables HRP2 RDTs to exhibit high specificity and sensitivity for detecting this parasite compared to other malaria RDTs [5]. The genes encoding HRP2 and its analogue protein, HRP3 (Pfhrp2 and Pfhrp3), are located in the sub-telomeric regions of Plasmodium chromosomes 8 and 13, respectively [5]. These regions are known for extensive genetic diversity and frequent changes during recombination events [6, 7]. HRP3 shares repeat motifs with HRP2, allowing antibodies against HRP2 to cross-react with HRP3. The failure of RDTs to detect P. falciparum infections can often be attributed to the absence of detectable HRP2 antigen levels. This may result from genetic variability and deletions at the hrp2 and hrp3 loci, along with other factors such as misinterpretation of RDT results, the prozone effect, and Pfhrp2/3 gene deletions [5]. Recognizing the significant implications of these false negatives, the WHO has recommended revising testing strategies if the local prevalence of false-negative HRP2 RDTs due to gene deletions reaches 5% [8]. Initial evidence of widespread Pfhrp2 and Pfhrp3 gene deletions emerged from studies in Peru [9]. In India, Bharti et al. reported low-level deletions of the hrp2 gene across eight highly endemic states, raising concerns about the reliability of HRP2 RDTs in these regions and underscoring the need for continuous monitoring and surveillance [10]. Given the critical role of accurate diagnosis in malaria control and elimination efforts, this study further investigates the prevalence of Pfhrp2 and Pfhrp3 gene deletions in parasites from nine malaria-endemic states in India. The aim is to determine whether there have been changes in the prevalence of these deletions, which could impact the effectiveness of current diagnostic tools. By focusing on these gene deletions, the study seeks to enhance our understanding of the genetic dynamics of Pfhrp2 in India and improve diagnostic accuracy.
Methods
Study site and sample collection
The present study utilized stored blood samples collected by the ICMR-NIRTH in 2014, 2017 2019, and 2020 as part of an Therapeutic efficacy study (TES) [11, 12] (Table 2). A total of 1558 samples (microscopically confirmed P. falciparum) were collected from the nine malaria endemic states of India (Fig 1), were used for the detection of Pfhrp2 and Pfhrp3 gene deletion. The study was approved by ICMR-NIRTH Institutional Ethics Committee to utilise the archived samples in the current study (NIRTH/IEC/01/3162/2020).
Table 2. Distribution of hrp2/3 deletion cases across Indian states/year wise within the total sample population.
| Parameters | Total no. of samples (N) | hrp2 deletion | hrp3 deletion | hrp2 deleted % | hrp3 deleted % |
|---|---|---|---|---|---|
| 2014 | 627 | 3 | 7 | 0.47 | 1.11 |
| 2017 | 569 | 3 | 11 | 0.52 | 0.70 |
| 2019 | 233 | 0 | 3 | 0 | 0.19 |
| 2020 | 129 | 1 | 2 | 0.77 | 0.12 |
| Madhya Pradesh | 470 | 1 | 3 | 0.2 | 0.6 |
| Chhattisgarh | 370 | 4 | 9 | 1.1 | 2.4 |
| Jharkhand | 166 | 1 | 2 | 0.6 | 1.2 |
| Maharashtra | 118 | 0 | 2 | 0.0 | 1.7 |
| Odisha | 141 | 1 | 4 | 0.7 | 2.8 |
| Assam | 74 | 0 | 1 | 0.0 | 1.4 |
| Meghalaya | 60 | 0 | 1 | 0.0 | 1.7 |
| Mizoram | 99 | 0 | 1 | 0.0 | 1.0 |
| Telangana | 60 | 0 | 0 | 0.0 | 0 |
| Total | 1558 | 7 | 23 | 0.44 | 1.47 |
Fig 1. Map of India highlighting the nine malaria-endemic states.

Genomic DNA extraction
Whole blood samples were obtained from patients. Subsequently, 200 μl of blood was utilized for isolation, and DNA extraction was performed using a Qiagen DNA Blood Mini Kit (Qiagen-51306, Hilden, Germany) as per the manufacturer’s protocol. The DNA sample was stored at -80°C for long term storage, and at -20°C during the molecular biology analyses.
Amplification of histidine-rich protein 2 and 3 (hrp2/3)
Two step PCR amplification (primary and nested) method was used to amplify a segment encompassing exon 2 of Pfhrp2 and Pfhrp3 gene to carried out the gene deletions prevalence, PCR product of Pfhrp2 and Pfhrp3 gene resulted in a 222 bp and 216 bp respectively. Sample with Pfhrp2 and Pfhrp3 negative results were confirmed using 18S rRNA, msp1 and msp2 markers. For the primary PCR, 5 μL of genomic DNA was used as the template, while for the nested PCR, 2 μL of a 1:10 diluted primary PCR product served as the template. The PCR reaction was conducted in a 25 μL mixture containing 10X buffer, 1 mM MgCl₂, 0.2 mM of each dNTP, 0.4 μM of each primer, and 0.2 units of Taq polymerase (Invitrogen, Life Technologies). All PCR products were analyzed on a 1.2% agarose gel, and images were captured using a GelDoc-It2 imager. The details regarding primers and PCR cycling parameters employed for the amplification of Pfhrp2 and Pfhrp3 are described in Table 1.
Table 1. Details of primers used in the study.
| Primer name | Primer sequence | Denaturation | Annealing | Elongation | No of cycles |
|---|---|---|---|---|---|
| Pfhrp2 (exon 2) primary |
GGTTTCCTTCTCAAAAAATAAAG
TCTACATGTGCTTGAGTTTCG |
94 °C, 1 min | 58°C, 45 sec | 72 °C, 1 min | 35 |
| Pfhrp2 (exon 2) nested |
GTATTATCCGCTGCCGTTTTTGCC
CTACACAAGTTATTATTAAATGCGGAA |
94 °C, 1 min | 63°C, 45 sec | 72 °C, 1 min | 25 |
| Pfhrp3 (exon 2) primary |
GGTTTCCTTCTCAAAAAATAAAA
CCTGCATGTGCTTGACTTTA |
94 °C, 45 sec | 53 °C, 1 min | 72 °C, 1 min | 30 |
| Pfhrp3 (exon 2) nested |
ATATTATCGCTGCCGTTTTTGCT
CTAAACAAGTTATTGTTAAATTCGGAG |
94 °C, 45 sec | 62 °C, 1 min | 72 °C, 1 min | 25 |
| MSP1 (primary) |
CTAGAAGCTTTAGAAGATGCAGTATTG
CTTAAATAGTATTCTAATTCAAGTGGATCA |
94°C, 1 min | 61°C, 2 min | 72°C, 1 min | 25 |
| MSP1 (Nested) |
AAATGAAGGAACAAGTGGAACAGCTGTTAC
ATCTGAAGGATTTGTACGTCTTGAATTACC |
94°C, 1 min | 61°C, 2 min | 72°C, 1 min | 30 |
| MSP2 (primary) |
ATGAAGGTAATTAAAACATTGTCTATTATA
CTTTGTTACCATCGGTACATTCTT |
94°C, 1 min | 61°C, 1 min | 72°C, 1 min | 25 |
| MSP2 (Nested) |
AGAAGTATGGCAGAAAGTAAKCCTYCTACT
GATTGTAATTCGGGGGATTCAGTTTGTTCG |
94°C, 1 min | 61°C, 1 min | 72°C, 1 min | 30 |
| 18s rRNA Plasmodium (Genus) |
TCAAAGATTAAGCCATGCAAGTGA
CCTGTTGTTGCCTTAAACTTC |
95°C, 30 sec | 54°C, 45 sec | 72°C, 1 min 30 sec | 35 |
| P. falciparum (nested) |
TTAAACTGGTTTGGGAAAACCAAATATATT
ACACAATGAACTCAATCATGACTACCCGTC |
95°C, 30 sec | 58°C, 1 min | 72°C, 1 min | 30 |
Amplification of 18s rRNA, merozoite surface protein 1 and 2 (msp1 and msp2)
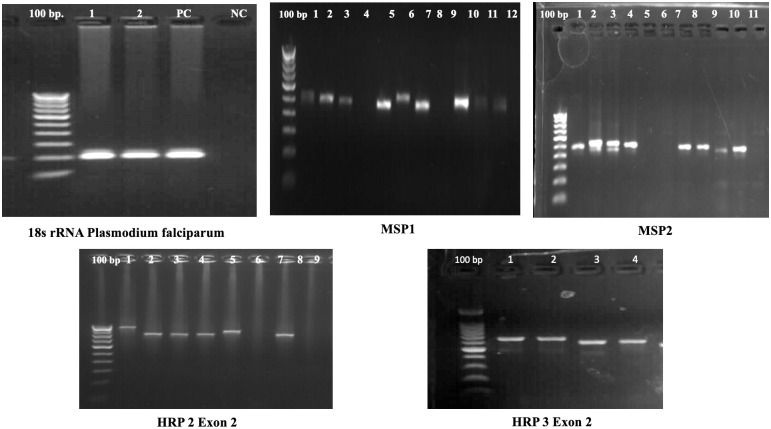
To assess DNA integrity, samples that were not amplified for the HRP2/3 gene were tested for 18S rRNA, msp1, and msp2 to confirm the presence of genuine HRP2/3 gene deletions. Details regarding the primers and PCR cycling parameters used for amplifying 18S rRNA, msp1, and msp2 are provided in Table 1. The PCR amplified gel images are shown in Fig 2.
Fig 2. PCR gel images showing the amplification of hrp2/3, 18s rRNA, msp1, msp2 genes.
Data analysis
The results of the Pfhrp2/3 gene deletion were recorded in a Microsoft Excel sheet to estimate the prevalence of gene deletions by state.
Results
Gene deletion in Pfhrp2
The overall rate of Pfhrp2 deletion in nine malaria-endemic states is 0.44% (7 out of 1,558). Among these states, Chhattisgarh has the highest level of Pfhrp2 deletion at 1.1% (4 out of 370), followed by Odisha at 0.7% (1 out of 141), Jharkhand at 0.6% (1 out of 166), and Madhya Pradesh at 0.2% (1 out of 470). No Pfhrp2 deletion cases were found in Maharashtra, Assam, Meghalaya, Mizoram, and Telangana. In 2020, Pfhrp2 deletion was reported at a higher rate of 0.77% (1 out of 129), followed by 0.52% (3 out of 569) in 2017, and 0.47% (3 out of 627) in 2014 (Table 2). Interestingly, no cases of deletion were found in 2019. In order to assess the DNA quality of the deleted sample showing Pfhrp2 deletion, msp1, and msp2 marker genes were amplified, as recommended for evaluating DNA integrity. Interestingly, both marker genes showed successful amplification in this particular sample, while repeated attempts also did not amplify the Pfhrp2 gene, confirming the Pfhrp2 deletion (Figs 2 and 3).
Fig 3. Year-wise distribution of (A) hrp2 gene deletions and (B) hrp3 gene deletions across Indian states.
Gene deletion in Pfhrp3
The overall rate of Pfhrp3 deletion in nine malaria-endemic states is 1.47% (23 out of 1,558). Among these states, Odisha has the highest level of hrp3 deletion at 2.8% (4 out of 141), followed by Chhattisgarh at 2.4% (9 out of 370). Meghalaya (1 out of 60) and Maharashtra (2 out of 118) each have a deletion rate of 1.7%, Assam has 1.4% (1 out of 74), Jharkhand has 1.2% (2 out of 166), and Madhya Pradesh has 0.6% (3 out of 470). No Pfhrp3 deletion cases were found in Telangana. In 2014, Pfhrp3 deletion was reported at the highest rate of 1.11%, followed by 0.70% in 2017, 0.19% in 2019, and 0.12% in 2020. Population genetic marker genes (msp1, and msp2) showed successful amplification in these samples, while repeated attempts to amplify the Pfhrp3 gene failed to amplify the gene confirming Pfhrp3 deletion (Figs 2 and 3).
Dual deletion of Pfhrp2 and Pfhrp3 genes
Dual deletion of both Pfhrp2 and Pfhrp3 genes was found in Madhya Pradesh at 0.21% (1 out of 470), followed by Chhattisgarh at 1.08% (4 out of 370), Jharkhand at 0.60% (1 out of 166), and Odisha at 0.70% (1 out of 141). However, no dual gene deletions were found in Assam, Meghalaya, Mizoram, Maharashtra, and Telangana.
Discussion
Malaria diagnosis is vital for timely treatment and transmission prevention. In India, RDTs are preferred in resource-limited settings. RDTs have delivered 3.9 billion tests globally since 2010 [1]. The states of Madhya Pradesh, Chhattisgarh, Jharkhand, Maharashtra, Odisha, Assam, Meghalaya, Mizoram, and Telangana, account for nearly 65% of malaria cases in 2023 [2]. These states exhibit varying intensities of malaria transmission due to differences in environmental, socioeconomic, and epidemiological factors (Table 3). This study conducted across nine malaria-endemic states in India have identified low levels of Pfhrp2 deletions (0.44%) in P. falciparum populations. Samples were assessed for ‘real’ Pfhrp2/3 deletions, to accurately interpret test results, we used additional markers, such as the 18S ribosomal RNA gene or msp1, and msp2 genes, as controls. The presence of these genes confirms the integrity of the sample and the efficacy of the PCR process. If the 18S or msp1/2 testing is positive while hrp2 is not amplified, it is more likely indicative of a genuine deletion. Conversely, if all markers fail to amplify, it may point to a procedural error rather than a true genetic absence. During the analyses of msp1 and msp2, multiclonal infections were also observed, as indicated by multiple bands in the isolates (data not shown). In a 2013 study in Chhattisgarh, a 4% deletion rate of the Pfhrp2 gene was reported, alongside partial gene deletions for Pfhrp2 and Pfhrp3 [13, 14]. In 2017–18, Nema et al. observed a 3.8% deletion rate of the Pfhrp2 gene in Chhattisgarh (unpublished). Similarly, findings in Kolkata indicated a 2.17% deletion rate for both genes [15]. However, Odisha showed a higher incidence of Pfhrp2 deletion at approximately 17% [16]. A systematic review and meta-analysis by kojom et al. shown that pooled prevalence of Pfhrp2 deletions was 5% in India. For pfhrp3 deletions, the prevalence was 4% in India [17]. While our study suggests that the prevalence of Pfhrp2 deletion has not substantially increased compared to previous reports, the WHO recommends baseline surveys in countries with documented Pfhrp2/3 deletions, and neighboring regions. These surveys are crucial to assess if deletion prevalence surpasses the threshold requiring RDT changes. WHO’s response plan includes actions such as identifying new biomarkers, enhancing non-HRP2 RDT performance, market forecasting, and bolstering laboratory networks for molecular characterization [8, 18]. Studies are underway to explore alternative biomarkers like hemozoin [19], heme detoxification proteins (HDP) [20], and Glutamate dehydrogenase (GDH) [21] for developing next-generation RDTs. Continuous surveillance, as recommended by WHO, is essential to ensure the reliability of HRP2-based RDTs. Based on current data, HRP2-based RDTs remain suitable for use in these states. One limitation of the study is that we did not perform PfLDH-based RDT detection according to the hrp2 gene deletion estimation protocol. Accurate detection is essential for effective malaria treatment and management, especially in high-transmission areas. This study enhances global knowledge and informs local health policies to reduce the malaria burden and advance elimination efforts.
Table 3. Parasite density and transmission intensity by year and state.
| Year | States | Parasite density/μL Geometric mean (Range) |
Transmission setting |
|---|---|---|---|
| 2014 | Jhabua, Madhya Pradesh | 6868 (5755.9–8195.9) | High |
| Anuppur, Madhya Pradesh | 2518 (2015.3–3146.4) | Moderate | |
| Bastar, Chhattisgarh | 7869 (6430.5–9629.2) | High | |
| Simdega, Jharkhand | 3032 (2086.4–4405.1) | High | |
| 2017 | Balaghat, Madhya Pradesh | 5262.6 (1000–99240) | High |
| Jagdalpur, Chhattisgarh | 14044 (1080–98200) | High | |
| Kilepal, Chhattisgarh | 10015 (1130–88765) | High | |
| Koraput, Odisha | 7380.8 (1053–98746) | High | |
| Gondia, Maharashtra | 6770.8 (1200–92280) | Moderate | |
| 2019 | Udalguri, Assam | 3266 (1270–68955) | Low |
| South Garo hills, Meghalaya | 3567 (1510–91057) | High | |
| Lunglei, Mizoram | 5474 (1020–96000) | High | |
| 2020 | Khammam, Telangana | 5580 (1090–28570) | Low |
| Kalahandi, Odisha | 12150 (2200–67102) | High |
Conclusion
HRP2-based RDT kits have proven immensely beneficial in rural and tribal regions of India, where malaria prevalence is notably high. The current study presents genetic diversity data of Pfhrp2 and Pfhrp3 genes across nine malaria-endemic states of India. Results confirm a low prevalence of gene deletion in these regions. Among microscopically confirmed samples, only 0.44% exhibited Pfhrp2 deletion, while 1.47% had Pfhrp3 deletion across the nine states. This data will aid in comprehending the evolutionary mechanisms linked to the emergence and dissemination of Pfhrp2/3 deletions.
Acknowledgments
The authors would like to thank the study participants and field staff. The manuscript was approved by the Publication Screening Committee of ICMR-NIRTH Jabalpur.
Data Availability
All relevant data are within the manuscript and its supporting information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.World malaria report 2023. https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023
- 2.Malaria:: National Center for Vector Borne Diseases Control (NCVBDC). https://nvbdcp.gov.in/index1.php?lang=1&level=1&sublinkid=5784&lid=3689
- 3.Nema S, Ghanghoria P, Bharti PK. Malaria Elimination in India: Bridging the Gap Between Control and Elimination. Indian Pediatr. 2020;57(7):613–7. doi: 10.1007/s13312-020-1888-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nema S, Verma AK, Bharti PK. Strengthening diagnosis is key to eliminating malaria in India. Lancet Infect Dis. 2019. Dec;19(12):1277–8. doi: 10.1016/S1473-3099(19)30544-4 [DOI] [PubMed] [Google Scholar]
- 5.Poti KE, Sullivan DJ, Dondorp AM, Woodrow CJ. HRP2: Transforming Malaria Diagnosis, but with Caveats. Trends Parasitol. 2020. Feb 1;36(2):112–26. doi: 10.1016/j.pt.2019.12.004 [DOI] [PubMed] [Google Scholar]
- 6.Figueiredo LM, Freitas-Junior LH, Bottius E, Olivo-Marin JC, Scherf A. A central role for Plasmodium falciparum subtelomeric regions in spatial positioning and telomere length regulation. EMBO J. 2002. Feb 15;21(4):815–24. doi: 10.1093/emboj/21.4.815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ribacke U, Mok BW, Wirta V, Normark J, Lundeberg J, Kironde F, et al. Genome wide gene amplifications and deletions in Plasmodium falciparum. Mol Biochem Parasitol. 2007. Sep;155(1):33–44. doi: 10.1016/j.molbiopara.2007.05.005 [DOI] [PubMed] [Google Scholar]
- 8.Response plan to pfhrp2 gene deletions. https://www.who.int/publications-detail-redirect/WHO-CDS-GMP-2019.02
- 9.Gamboa D, Ho MF, Bendezu J, Torres K, Chiodini PL, Barnwell JW, et al. A large proportion of P. falciparum isolates in the Amazon region of Peru lack pfhrp2 and pfhrp3: implications for malaria rapid diagnostic tests. PloS One. 2010. Jan 25;5(1):e8091. doi: 10.1371/journal.pone.0008091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bharti PK, Chandel HS, Ahmad A, Krishna S, Udhayakumar V, Singh N. Prevalence of pfhrp2 and/or pfhrp3 Gene Deletion in Plasmodium falciparum Population in Eight Highly Endemic States in India. PLOS ONE. 2016. Aug 12;11(8):e0157949. doi: 10.1371/journal.pone.0157949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bharti PK, Shukla MM, Ringwald P, Krishna S, Singh PP, Yadav A, et al. Therapeutic efficacy of artemether–lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria from three highly malarious states in India. Malar J. 2016. Oct 13;15:498. doi: 10.1186/s12936-016-1555-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krishna S, Mishra S, Tiwari P, Vishwakarma AK, Khandai S, Shrivastava S, et al. Therapeutic efficacy of artemether-lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in four malaria endemic states of India. Malar J. 2021. May 21;20(1):229. doi: 10.1186/s12936-021-03762-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar N, Pande V, Bhatt RM, Shah NK, Mishra N, Srivastava B, et al. Genetic deletion of HRP2 and HRP3 in Indian Plasmodium falciparum population and false negative malaria rapid diagnostic test. Acta Trop. 2013. Jan;125(1):119–21. doi: 10.1016/j.actatropica.2012.09.015 [DOI] [PubMed] [Google Scholar]
- 14.Kumari MS, Sharma S, Bhardwaj N, Kumar S, Ahmed MdZ, Pande V, et al. Pfhrp2/3 gene deletion and genetic variation in PfHRP2-based RDTs with P. falciparum positive samples from India and its implication on malaria control. Infect Genet Evol. 2022. Apr 1;99:105232. [DOI] [PubMed] [Google Scholar]
- 15.Acharya A, Saha P, Chaudhury A, Guha SK, Maji AK. Prevalence of histidine-rich protein 2 deletion among the Plasmodium falciparum isolates from Kolkata. Trop Parasitol. 2023;13(1):16–21. doi: 10.4103/tp.tp_19_22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pati P, Dhangadamajhi G, Bal M, Ranjit M. High proportions of pfhrp2 gene deletion and performance of HRP2-based rapid diagnostic test in Plasmodium falciparum field isolates of Odisha. Malar J. 2018. Oct 29;17(1):394. doi: 10.1186/s12936-018-2502-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kojom LP, Singh V. Prevalence of Plasmodium falciparum field isolates with deletions in histidine-rich protein 2 and 3 genes in context with sub-Saharan Africa and India: a systematic review and meta-analysis. Malar J. 2020. Jan 28;19(1):46. doi: 10.1186/s12936-019-3090-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nema S, Kumari M, Ghosh SK. Automation Techniques in Infectious Diseases. In: Kumar S, Kumar A, editors. Automated Diagnostic Techniques in Medical Microbiology. Singapore: Springer Nature; 2024. [cited 2024 Jun 6]. p. 145–60. [Google Scholar]
- 19.Nema S. Malaria hemozoin: A target for point-of-care diagnosis. Indian J Public Health. 2022. Oct 1;66(4):522. doi: 10.4103/ijph.ijph_1646_21 [DOI] [PubMed] [Google Scholar]
- 20.Nema S, Krishna S, Tiwari A, Bharti PK. Limited genetic diversity and expression profile of Plasmodium falciparum haem detoxification protein: a possible diagnostic target. Trans R Soc Trop Med Hyg. 2022. Jun 20;trac055. doi: 10.1093/trstmh/trac055 [DOI] [PubMed] [Google Scholar]
- 21.Kori LD, Valecha N, Anvikar AR. Glutamate dehydrogenase: a novel candidate to diagnose Plasmodium falciparum through rapid diagnostic test in blood specimen from fever patients. Sci Rep. 2020. Apr 14;10(1):6307. doi: 10.1038/s41598-020-62850-x [DOI] [PMC free article] [PubMed] [Google Scholar]