ABSTRACT
BACKGROUND:
Emotional distress increases, also affected by the setting.
OBJECTIVE:
To estimate changes in prevalence of severe anxiety and depressive symptoms and associated factors.
DESIGN AND SETTING:
This cross-sectional study included adults living in Manaus selected through a three-stage probability sampling in 2015 and 2019.
METHODS:
This is an analysis of two surveys conducted. The outcomes were assessed by Generalized Anxiety Disorder 7-item (≥ 15 points) and Patient Health Questionnaire 9-item (≥ 20), and changes were tested by chi-square goodness-of-fit. Prevalence ratios (PR) with 95% confidence intervals (95%CI) were calculated by Poisson regression.
RESULTS:
Severe anxiety symptoms increased from 3.3% (95%CI = 2.7–3.9) in 2015 (n = 3,479) to 8.7% (95%CI = 7.5–9.8) in 2019 (n = 2,321); severe depressive symptoms changed from 2.5% (95%CI = 2.0–3.0) to 8.5% (95%CI = 7.3–9.6). Variations were more pronounced in social vulnerability (P < 0.05). Outcomes were higher in women (anxiety: PR = 1.27; 95%CI = 1.20–1.34, depression: PR = 1.35; 95%CI = 1.27–1.44), low-income individuals (anxiety: PR = 1.90; 95%CI = 1.20–3.00, depression: PR = 1.98; 95%CI = 1.22–3.19), less educated individuals (anxiety: PR = 2.20; 95%CI = 1.16–4.18, depression: PR = 2.37; 95%CI = 1.23–4.60), and individuals with poor health status (anxiety: PR = 9.06; 95%CI = 6.72–12.21, depression: PR = 8.99; 95%CI = 6.67–12.12).
CONCLUSION:
Severe anxiety and depression tripled in Manaus, potentially reflecting Brazilian socioeconomic crises.
KEYWORDS (MeSH terms): Anxiety., Depression., Prevalence., Socioeconomic factors., Cross-sectional studies.
AUTHOR KEYWORDS: Mental health., Mental suffering., Austerity., Survey., Amazonas., Brazil.
INTRODUCTION
Mental health is influenced by social, economic, cultural, racial, psychological, and behavioral factors, which mediate suffering and can trigger disorders such as anxiety and depression. 1 From the onset of symptoms to the treatment of these conditions, individuals encounter numerous challenges, including limited access to specialists, a constrained therapeutic arsenal, and inadequate social care. These barriers can contribute to the chronicity of symptoms associated with anxiety and depression. 2
The global prevalence of affective disorders is rising, with depressive states increasing by approximately 50% since the 1990s, predominantly affecting women. 3 In Brazil, depressive symptoms are associated with a high prevalence of non-communicable chronic diseases, as the daily limitations imposed by chronically ill exacerbate mental suffering, leading to depressive symptoms. 4
Since 2016, Brazil has been experiencing increases in unemployment rate, income inequality, and reductions in public support for basic social programs due to ongoing economic and political crises. 5 These measures included reforms in the healthcare system and reductions in social spending. 6 In this social insecurity setting, stress and fear, among other feelings of restlessness, impair mental health at the individual and collective levels. 7
The Brazilian Amazon is one of the country’s least developed regions, with significant income inequality and limited research on mental health and its social effects. 8 In 2015, a survey was carried out in the Manaus Metropolitan Region. 9 In 2019, another population-based survey was conducted exclusively in Manaus. 10 Anxiety and depressive symptoms affected over 20% of Manauaras adults in 2019. 11 Meanwhile, the prevalence was < 10% in the whole metropolitan area in 2015, 12,13 indicating an increase in mental suffering in this population. Comparing the population of the same city in these two periods would help identify the predictors of mental health disorders and assess the effects of the social context in the Brazilian Amazon.
OBJECTIVE
This study aimed to estimate the changes in the prevalence of severe anxiety and depressive symptoms from 2015 to 2019 and identify the factors associated with severe symptomatology among adults living in Manaus.
METHODS
Study design
Two cross-sectional population-based studies conducted in adults (≥ 18 years old) living in Manaus, Brazil, in 2015 and 2019 were analyzed. The 2015 survey examined the metropolitan area of Manaus and seven other cities. In the present analysis, the sample was restricted to adults residing in Manaus to enable comparison with the results of the 2019 survey, which focused exclusively in the capital. 14
Setting
This study was conducted in Manaus, the capital of the state of Amazonas, which is the most economically and densely populated city in the state, housing over half of its inhabitants in 2018. In the same year, the state ranked fourth in terms of income inequality (Gini index 0.523) and had a high percentage of public healthcare demand (84%). 14 Manaus is one of the Brazilian cities with the largest gross domestic product (78 billion Brazilian reais, accounting for 1% of the gross national product in 2018). However, this wealth is unevenly distributed, resulting in significant social inequalities. 14
Participants
Probabilistic sampling was conducted in three stages to select participants for both surveys. In the first stage, census tracts were randomly selected. In the second stage, households were chosen through systematic sampling. A number from 1 to 20 was randomly assigned to determine the first household to be visited, ensuring that 1 out of every 20 households was visited. All residents present in the household were registered in the electronic devices used for the interview. One participant was selected based on predefined quotas for age and sex according to the proportions estimated by the Brazilian Institute of Geography and Statistics for each time point to ensure population representativeness. 9,10
Variables
The primary outcomes were the prevalence and severity of anxiety and depressive symptoms. The independent variables were sex (men or women), pregnancy (yes or no), age (18–24, 25–34, 35–44, 45–59, or ≥ 60 years), ethnicity (White [White and Asian] or Black [Black, Brown, and Indigenous]), the presence of a partner (yes or no), education (higher education or above, high school, elementary school, or less than elementary school), occupation (formal worker, informal worker, retired, student, or unemployed/housewife), social class (A/B, C, or D/E, where A refers to the wealthiest and E refers to the poorest based on the Brazilian Economic Classification Criteria of each year), 15,16 and self-reported health status (good, fair, or poor).
Data sources and measurement
A team of trained and experienced interviewers collected data from the participants using questionnaires preconfigured in the SurveyToGo software, with the aid of electronic devices (Tab3 SM-T110 Samsung® Galaxy, in 2015 and Intel TabPhone 710 Pro, in 2019). Data were collected offline and subsequently transmitted to a research database via the Internet.
Anxiety symptoms were assessed using the validated version of the Generalized Anxiety Disorder 7-item (GAD-7). 17,18 The questionnaire comprises seven items that assess the symptoms observed in the last two weeks, with a total score ranging from 0 to 21. The anxiety symptoms were categorized as minimal or none (0–4), mild (5–9), moderate (10–14), or severe (15–21). 19 A cutoff value of ≥ 10 points was used to indicate the presence of anxiety symptoms, with sensitivity and specificity greater than 80% compared with the mental health professionals’ clinical diagnosis. Severe anxiety was defined as a GAD-7 score of ≥ 15. 20
The validated version of the nine-item Patient Health Questionnaire 9-item (PHQ-9) was used to assess depressive symptoms. 21 Based on the instrument’s nine questions, depressive symptoms were categorized as minimal or none (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), or severe (20–27), with the total scores ranging from 0 to 27. A score of ≥ 10 points indicated the presence of depressive symptoms, with a sensitivity of 78% and a specificity of 87% (compared to the clinical diagnosis made by a psychiatrist). 22 Severe depressive symptoms were considered present if the final score of PHQ-9 was ≥ 20. 23
Bias
To avoid biases related to the research instrument, several precautions were taken. The data were automatically tabulated by transmitting the questionnaires completed on the tablets to the online database. Face-to-face interviews were conducted using validated instruments to measure the main outcomes and variables, which increased the response rate and data reliability. The questionnaire was pre-tested with 150 participants from various social levels to ensure comprehension. To allow reliability of data collection, part of interviews were audio recorded by the electronic device and 20% of interviews were audited by telephone.
Study size
The sample size was determined based on the population estimates for each period. In the 2015 survey, 4,000 of the 2,106,322 adult inhabitants were planned to be interviewed across the Manaus Metropolitan Region. This estimate was based on an anticipated 50% healthcare service usage, 95% confidence level, 2% absolute accuracy, and a design effect of 1.5. 9 In 2019, 2,300 interviews were planned considering the results of the previous study, which found that 20% of the participants reported seeking health services in the last 15 days, 2,145,444 adults living in Manaus and similar parameters to the previous survey. 10
Statistical methods
The prevalence of severe anxiety and depressive symptoms and the corresponding 95% confidence intervals (95%CI) were estimated and described according to the independent variables. The differences in absolute (Δ) and relative (ratio) frequencies from 2015 to 2019 were calculated, and significance was assessed using the chi-square goodness-of-fit test. The outcomes were stratified by year, sex, and health status, and the Pearson’s correlation coefficient (r) was estimated to examine the relationship between the GAD-7 and PHQ-9 scores.
A Poisson regression with robust variance was performed to assess the factors associated with severe anxiety and depressive symptoms. Prevalence ratios (PR) and 95%CI of severe anxiety and depression symptoms were calculated and adjusted for year of research, sex, and age, in separate models. All analyses employed a complex sampling design (svy command) and were performed using the Stata statistical package (version 12.4).
Ethics
Both surveys were approved by the Universidade Federal do Amazonas Research Ethics Committee (opinion letter No. 974,428 of March 3, 2015, and Certificate of Presentation for Ethical Assessment [CAAE]: 42203615.4.0000.5020; 2019: opinion letter No. 3,102,942 on December 28, 2018, and CAAE: 04728918.0.0000.5020). All participants signed an informed consent form prior to the interviews.
RESULTS
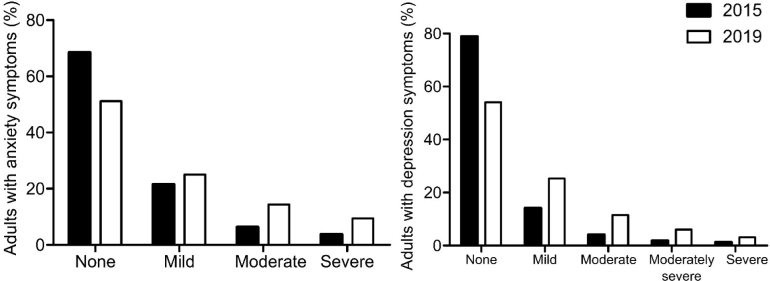
We included 5,800 participants (3,479 in 2015 and 2,321 in 2019). The prevalence of severe anxiety symptoms were 3.3% (95%CI = 2.7%–3.9%) in 2015 and 8.7% (95%CI = 7.5%–9.8%) in 2019. Similarly, the prevalence of severe depressive symptoms increased from 2.5% (95%CI = 2.0%–3.0%) in 2015 to 8.5% (95%CI = 7.3%–9.6%) in 2019. Comparisons between the 2019 with 2015 survey results suggested a relative increase in the prevalence of both severe anxiety and depressive symptoms ( Figure 1 ).
Figure 1. Distribution of anxiety and depression symptoms in adults living in Manaus, according to the severity, in 2015 (n = 3,479) and 2019 (n = 2,321).
The prevalence of severe anxiety symptoms was higher in women (4.8% in 2015 and 11.6% in 2019), those belonging to the lower social classes (4.3% in 2015 and 9.6% in 2019), and those with poor health (16.7% in 2015 and 31.7% in 2019). Severe depressive symptoms were more frequent in women (4.2% in 2015; 11.0% in 2019), individuals from the lower social classes (3.7% in 2015; 9.6% in 2019), and individuals with poor health (13.9% in 2015; 31.4% in 2019) ( Table 1 ). Higher absolute changes (Δ) in the prevalence of severe anxiety and depressive symptoms were observed among women (anxiety and depression: 6.8%), individuals with lower educational levels (5.9% and 7.3%, respectively), and those with poor health status (15.0% and 17.5%). Conversely, the highest ratio of prevalence between 2015 and 2019 was observed in the youngest adults (5.8 and 6.6; Table 1 ). The prevalence rates of anxiety symptoms (of any severity) were 9.1% (95%CI = 8.2%–10.1%) in 2015 and 22.4% (95%CI = 20.7%–24.1%), in 2019. Meanwhile, depressive symptoms affected 6.3% (95%CI = 5.5%–7.1%) of the adults in 2015 and 19.9% (95%CI = 18.2%–21.5%) in 2019.
Table 1. Main characteristics of the participants, prevalence, absolute and relative differences of severe anxiety and depression symptoms in Manaus, 2015 (n = 3,479) and 2019 (n = 2,321).
| Variables | Total, n (%) | Severe anxiety symptoms, n (%) | Severe depressive symptoms, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2019 | 2015 | 2019 | Δ | Ratio | 2015 | 2019 | Δ | Ratio | |
| Sex | ||||||||||
| Men | 1,623 (47.9) | 1,088 (47.8) | 26 (1.6) | 59 (5.4) | 3.8 | 3.4 | 11 (0.7) | 61 (5.6) | 5.0 | 8.4 |
| Women | 1,856 (52.2) | 1,233 (52.2) | 88 (4.8) | 144 (11.6) | 6.8 | 2.4 | 77 (4.2) | 137 (11.0) | 6.8 | 2.6 |
| Pregnant | ||||||||||
| No | 1,657 (89.9) | 1,091 (88.3) | 79 (4.9) | 131 (11.9) | 7.1 | 2.4 | 66 (4.1) | 125 (11.4) | 7.3 | 2.8 |
| Yes | 199 (10.1) | 142 (11.7) | 9 (4.5) | 13 (9.3) | 4.8 | 2.1 | 11 (5.5) | 12 (8.4) | 2.9 | 1.5 |
| Age group (years) | ||||||||||
| 18–24 | 716 (19.6) | 405 (19.3) | 11 (1.5) | 35 (8.5) | 7.0 | 5.8 | 10 (1.4) | 37 (9.0) | 7.7 | 6.6 |
| 25–34 | 1,010 (27.5) | 586 (25.1) | 29 (2.8) | 41 (7.0) | 4.2 | 2.5 | 28 (2.7) | 44 (7.5) | 4.8 | 2.8 |
| 35–44 | 744 (22.4) | 553 (22.9) | 24 (3.2) | 53 (9.5) | 6.3 | 3.0 | 13 (1.7) | 52 (9.3) | 7.6 | 5.4 |
| 45–59 | 674 (20.2) | 526 (21.2) | 31 (4.6) | 53 (10.0) | 5.4 | 2.2 | 24 (3.6) | 48 (9.1) | 5.5 | 2.5 |
| ≥ 60 | 335 (10.3) | 251 (11.6) | 19 (5.7) | 21 (8.4) | 2.8 | 1.5 | 13 (3.9) | 17 (6.8) | 2.9 | 1.8 |
| Ethnicity | ||||||||||
| White | 674 (19.3) | 349 (15.1) | 19 (2.8) | 34 (9.6) | 6.8 | 3.4 | 17 (2.5) | 28 (8.0) | 5.5 | 3.2 |
| Black | 2,805 (80.7) | 1,972 (85.0) | 95 (3.4) | 169 (8.5) | 5.1 | 2.5 | 71 (2.5) | 170 (8.5) | 6.0 | 3.4 |
| Marital status | ||||||||||
| Without partner | 1,636 (47.0) | 1,005 (44.1) | 43 (2.7) | 89 (8.7) | 6.0 | 3.2 | 40 (2.5) | 99 (9.7) | 7.2 | 4.0 |
| With partner | 1,843 (53.0) | 1,316 (56.0) | 71 (3.8) | 114 (8.6) | 4.8 | 2.2 | 48 (2.6) | 99 (7.5) | 4.9 | 2.9 |
| Educational level | ||||||||||
| Higher education or above | 131 (3.8) | 153 (6.5) | 2 (1.5) | 8 (5.3) | 3.8 | 3.5 | 3 (2.2) | 7 (4.7) | 2.5 | 2.2 |
| High school | 1,695 (48.3) | 1,171 (50.4) | 37 (2.2) | 91 (7.7) | 5.5 | 3.5 | 28 (1.6) | 89 (7.6) | 5.9 | 4.6 |
| Elementary school | 562 (16.0) | 432 (18.9) | 20 (3.6) | 41 (9.4) | 5.8 | 2.6 | 16 (2.8) | 38 (8.8) | 6.0 | 3.1 |
| Less than elementary | 1,091 (31.9) | 565 (24.2) | 55 (5.0) | 63 (10.9) | 5.9 | 2.2 | 41 (3.8) | 64 (11.1) | 7.3 | 2.9 |
| Economic classification | ||||||||||
| A/B | 555 (16.0) | 282 (12.2) | 8 (1.4) | 14 (5.0) | 3.6 | 3.5 | 6 (1.0) | 14 (5.0) | 3.9 | 4.8 |
| C | 2,006 (57.4) | 1,244 (53.6) | 66 (3.4) | 112 (8.9) | 5.6 | 2.7 | 47 (2.4) | 106 (8.5) | 6.1 | 3.6 |
| D/E | 918 (26.5) | 795 (34.1) | 40 (4.3) | 77 (9.6) | 5.2 | 2.2 | 35 (3.7) | 78 (9.6) | 5.9 | 2.6 |
| Occupation | ||||||||||
| Formal job | 651 (18.8) | 419 (17.9) | 13 (2.0) | 36 (8.6) | 6.6 | 4.3 | 7 (1.1) | 30 (7.2) | 6.1 | 6.7 |
| Informal job | 978 (28.5) | 661 (28.1) | 27 (2.7) | 39 (5.8) | 3.1 | 2.2 | 18 (1.8) | 48 (7.3) | 5.5 | 4.1 |
| Retired | 271 (8.2) | 162 (7.2) | 20 (7.5) | 18 (10.9) | 3.5 | 1.5 | 14 (5.2) | 13 (7.8) | 2.6 | 1.5 |
| Student | 315 (8.7) | 124 (5.7) | 5 (1.6) | 9 (7.1) | 5.5 | 4.5 | 5 (1.5) | 9 (7.2) | 5.6 | 4.7 |
| Unemployed/housewife | 1,264 (35.7) | 955 (41.0) | 49 (3.9) | 101 (11.0) | 7.0 | 2.8 | 44 (3.5) | 98 (10.2) | 6.6 | 2.9 |
| Health status | ||||||||||
| Good | 2,243 (64.1) | 1,498 (64.8) | 33 (1.5) | 53 (3.5) | 2.0 | 2.4 | 21 (0.9) | 60 (4.0) | 3.1 | 4.5 |
| Fair | 1,012 (29.3) | 671 (28.8) | 44 (4.3) | 102 (15.1) | 10.9 | 3.5 | 36 (3.5) | 90 (13.3) | 9.8 | 3.8 |
| Poor | 224 (6.6) | 152 (6.5) | 37 (16.7) | 48 (31.7) | 15.0 | 1.9 | 31 (13.9) | 48 (31.4) | 17.5 | 2.3 |
| Total | 3,479 (100) | 2,321 (100) | 114 (22.5) | 203 (50.3) | 27.9 | 7.8 | 88 (18.3) | 198 (48.7) | 30.4 | 10.6 |
After adjustment, the prevalence of severe anxiety and depressive symptoms was significantly higher in 2019 in women (anxiety: PR = 1.27; 95%CI = 1.20–1.34, depression: PR = 1.35; 95%CI = 1.27–1.44), individuals with lower income (anxiety: PR = 1.90; 95%CI=1.20–3.00, depression: PR = 1.98; 95%CI = 1.22–3.19), and less educated individuals (anxiety: PR = 2.20; 95%CI = 1.16–4.18, depression: PR = 2.37; 95%CI = 1.23–4.60), and in those with worse health status (anxiety: PR = 9.06; 95%CI = 6.72-12.21, depression: PR = 8.99; 95%CI = 6.67–12.12) ( Table 2 ). The prevalence of severe anxiety was also higher in individuals who only finished elementary education (PR = 1.96; 95%CI = 1.01–3.79) compared with those who achieved a higher education. Age, pregnancy in the previous year, ethnicity, the presence of a partner, and occupation were not associated with the outcomes ( Table 2 ).
Table 2. Unadjusted and adjusted prevalence ratios (PR) with 95% confidence intervals (95%CI) of severe anxiety and depression symptoms by independent variables.
| Variables | Severe anxiety symptoms | Severe depressive symptoms | ||||||
|---|---|---|---|---|---|---|---|---|
| PR unadjusted (95%CI) | P value | PR adjusted (95%CI) | P value | PR unadjusted (95%CI) | P value | PR adjusted (95%CI) | P value | |
| Year | ||||||||
| 2015 | 1.00 | < 0.001 | 1.00 | < 0.001 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| 2019 | 2.63 (2.09–3.28) | 1.27 (1.20–1.34) | 3.35 (2.62–4.30) | 1.35 (1.27–1.44) | ||||
| Age group (years) | ||||||||
| 18–24 | 1.00 | 0.045 | 1.00 | 0.094 | 1.00 | 0.733 | 1.00 | 0.733 |
| 25–34 | 0.95 (0.66–1.39) | 0.96 (0.66–1.39) | 0.95 (0.66–1.38) | 0.96 (0.67–1.38) | ||||
| 35–44 | 1.27 (0.89–1.83) | 1.25 (0.87–1.78) | 1.07 (0.74–1.56) | 1.05 (0.73–1.51) | ||||
| 45–59 | 1.46 (1.02–2.08) | 1.42 (1.00–2.02) | 1.22 (0.85–1.75) | 1.18 (0.82–1.69) | ||||
| ≥ 60 | 1.40 (0.92–2.14) | 1.30 (0.85–1.97) | 1.03 (0.65–1.62) | 0.94 (0.60–1.49) | ||||
| Sex | ||||||||
| Men | 1.00 | < 0.001 | 1.00 | < 0.001 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Women | 2.32 (1.81–2.98) | 2.31 (1.81–2.95) | 2.38 (1.83–3.09) | 2.38 (1.83–3.09) | ||||
| Pregnant | ||||||||
| No | 1.00 | 0.431 | 1.00 | 0.905 | 1.00 | 0.661 | 1.00 | 0.940 |
| Yes | 0.84 (0.54–1.30) | 0.97 (0.62–1.53) | 0.91 (0.59–1.40) | 0.98 (0.62–1.55) | ||||
| Ethnicity | ||||||||
| White | 1.00 | 0.862 | 1.00 | 0.767 | 1.00 | 0.401 | 1.00 | 0.815 |
| Black | 1.03 (0.77–1.38) | 0.96 (0.72–1.28) | 1.15 (0.83–1.58) | 1.04 (0.76–1.42) | ||||
| Marital status | ||||||||
| Without partner | 1.00 | 0.336 | 1.00 | 0.747 | 1.00 | 0.178 | 1.00 | 0.045 |
| With partner | 1.12 (0.89–1.39) | 1.04 (0.83–1.30) | 0.85 (0.68–1.07) | 0.78 (0.62–0.99) | ||||
| Educational level | ||||||||
| Higher education or above | 1.00 | 0.006 | 1.00 | 0.007 | 1.00 | 0.014 | 1.00 | 0.002 |
| High school | 1.29 (0.68–2.45) | 1.51 (0.80–2.84) | 1.27 (0.66–2.42) | 1.48 (0.78–2.82) | ||||
| Elementary school | 1.71 (0.88–3.33) | 1.96 (1.01–3.79) | 1.64 (0.83–3.22) | 1.85 (0.94–3.63) | ||||
| Less than elementary | 1.93 (1.02–3.66) | 2.20 (1.16–4.18) | 1.87 (0.97–3.58) | 2.37 (1.23–4.60) | ||||
| Economic classification | ||||||||
| A/B | 1.00 | < 0.001 | 1.00 | 0.021 | 1.00 | < 0.001 | 1.00 | 0.019 |
| C | 2.04 (1.30–3.19) | 1.81 (1.16–2.82) | 1.94 (1.21–3.10) | 1.71 (1.07–2.73) | ||||
| D/E | 2.44 (1.54–3.86) | 1.90 (1.20–3.00) | 2.54 (1.57–4.09) | 1.98 (1.22–3.19) | ||||
| Occupation | ||||||||
| Formal job | 1.00 | < 0.001 | 1.00 | 0.115 | 1.00 | 0.002 | 1.00 | 0.482 |
| Informal job | 0.81 (0.56–1.16) | 0.72 (0.50–1.04) | 1.10 (0.74–1.64) | 1.00 (0.67–1.49) | ||||
| Retired | 1.71 (1.13–2.59) | 1.58 (0.96–2.60) | 1.55 (0.95–2.53) | 1.60 (0.88–2.88) | ||||
| Student | 0.73 (0.40–1.32) | 0.74 (0.39–1.41) | 0.93 (0.50–1.73) | 0.87 (0.46–1.65) | ||||
| Unemployed/housewife | 1.42 (1.03–1.95) | 1.00 (0.72–1.39) | 1.73 (1.21–2.47) | 1.19 (0.82–1.72) | ||||
| Health status | ||||||||
| Good | 1.00 | < 0.001 | 1.00 | < 0.001 | 1.00 | < 0.001 | 1.00 | < 0.001 |
| Fair | 3.92 (3.01–5.11) | 3.79 (2.90–4.96) | 3.37 (2.55–4.45) | 3.37 (2.56–4.44) | ||||
| Poor | 9.64 (7.25–12.82) | 9.06 (6.72–12.21) | 9.02 (6.72–12.11) | 8.99 (6.67–12.12) | ||||
PR = prevalence ratios; CI = confidence interval.
Comparison between the 2019 and 2015 survey results revealed an increase in the prevalence of severe anxiety and depression symptoms, with a moderate to high correlation between the GAD-7 and PHQ-9 scores in 2015 (r = 0.726) and 2019 (r = 0.732; Figure 2 ).
Figure 2. Depression and anxiety symptom scores from the Generalized Anxiety Disorder 7-item (GAD-7) and Patient Health Questionnaire 9-item (PHQ-9), for each year, according to sex.
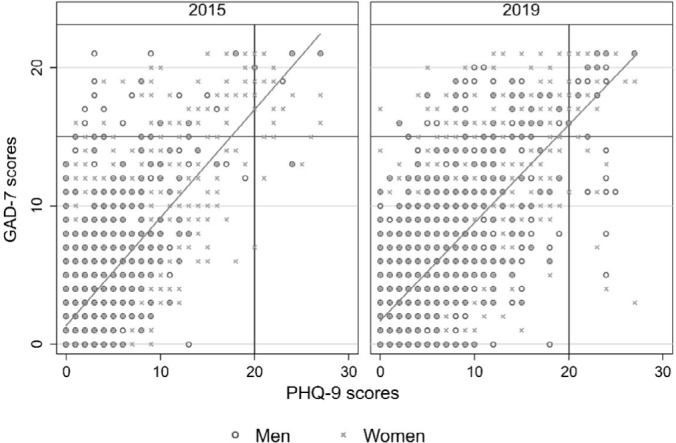
Vertical and horizontal lines indicate the threshold for severe symptoms for each outcome.
DISCUSSION
In 2019, the prevalence of severe anxiety and depression increased from 3% in 2015 to 9%. This increase was more pronounced in socioeconomically disadvantaged individuals, such as those with lower educational levels. The prevalence of severe anxiety and depressive symptoms was notably higher in 2019 among women, individuals with poor health status, and middle-class people. Pregnant women and informal workers had a lower prevalence of severe anxiety.
Our study was not primarily designed as a comparative analysis between the two surveys. The similar methodologies employed in each year enabled us to compare the changes in the study’s outcomes in these two distinct periods. Probabilistic sampling was adopted in both surveys to minimize selection bias, but all measurements were based on self-reports. Anxiety and depressive symptoms were assessed using two validated tools with strong psychometric properties that allow reliability when measuring these outcomes. 18,21 Conservative cut-off points with higher sensitivity and specificity were used to determine the presence of anxiety and depressive symptoms. 20,24,25 The present study reflects the status before the COVID-19 pandemic, which has since had a significant impact on mental health. 26 Despite these limitations, our analysis provides valuable insights into the early effects of austerity measures on mental health in Manaus.
The prevalence of severe anxiety and depressive symptoms in our study, particularly in the 2019 survey, was higher than that reported in other countries. For example, a 2011–2014 study of 5,355 German adults reported a prevalence of severe anxiety symptoms of 4%. 27 Similarly, an analysis of 13,829 adults living in Australia in 2020 showed a lower prevalence of severe depressive symptoms (4.5%). 28,29 A representative survey from the United Kingdom (n = 17,152), conducted in 2014, reported severe depressive symptoms in only 3.3% of the population. 30
The increase in the prevalence of severe anxiety and depressive symptoms was more pronounced among vulnerable individuals. In 2018, a cross-sectional study conducted in the United States with 22,682 adults found that financial concerns exacerbated mental health issues, particularly among the unemployed and low-income families due to daily exposure to stressors and the higher vulnerability of this group to stress. 31
Our findings also indicate a higher prevalence of severe anxiety and depression in women than in men. Globally, women have consistently shown a higher prevalence and burden of depression and anxiety from 1990 to 2019. 32 The psychosocial risk factors that can contribute to anxiety and depression are more frequent in women, such as domestic violence, gender harassment, employment and income inequalities, educational disparities, which increases stress. 33,34
Symptom reporting is closely associated with the perception of poor health status, with a higher prevalence of symptoms correlating with greater dissatisfaction with one’s health conditions. 35 Severe anxiety and depressive symptoms were higher among individuals with poorer self-reported health. A study of 1,241 patients from 28 primary care units in Spain in 2014–2017, using the same assessment tools as our research, found that anxiety and depressive symptoms were associated with lower quality of life. 36 The overlapping diagnoses of mental disorders significantly worsens the quality of life. 37 In a South Korean cohort including 1,204 community-dwelling older adults with anxiety and depression followed from 2001 to 2003, both conditions were associated with a higher incidence of comorbidities. 38 The simultaneous presence of anxiety and depression exacerbated the physical disorders and disabilities after a 2-year follow-up period. 38
Middle-class individuals exhibited a high prevalence of severe anxiety and depression. However, the poorest individuals had a higher probability of experiencing these conditions. A 2013 study conducted in 2,229 German adults found a significant correlation between socioeconomic status and clinically significant anxiety and severe anxiety. 39 Another German cohort study that followed 12,484 adult individuals for 2.5 years identified socioeconomic status as a strong predictor of elevated depressive symptoms among individuals without these conditions at baseline. 40 Depression and anxiety may also result in economic consequences and financial burdens. Individuals with lower socioeconomic status experience more depression- and anxiety-related absences from work. 41 This mental distress can amplify social disadvantage, creating a vicious cycle where poorer individuals experience limited access to better employment opportunities and higher incomes, thus exacerbating the burden of mental disorders. 42
Informal employment does not necessarily result in worse health outcomes but can expose underlying vulnerabilities. 43 Informal workers have a lower prevalence of severe anxiety than formal workers. These results contrast with previous analyses, which suggest that informal work is associated with poorer health outcomes compared with formal work, particularly in low- and middle-income countries. 44,45 A cross-sectional study of 8,680 non-agricultural workers from Spanish-speaking Central American countries, conducted in 2011, found a significant association between informal work and poor mental health. 46 A previous analysis of the 2015 survey in the Manaus Metropolitan Region indicated that the health-related quality of life (measured using the European Quality of Life 5-Dimensions 3-Level instrument, which includes an anxiety/depression dimension) was lower among informal workers than among formal workers. 47 The lack of labor and social protections may lead to poor working conditions, irregular income opportunities, barriers to healthcare access, and vulnerability to serious health shocks. 48
CONCLUSIONS
The prevalence of severe anxiety and depression symptoms tripled during the study period. The observed increase in mental distress may reflect the contextual changes, such as rising unemployment and difficulties in accessing health services. Positive variations in both outcomes were particularly pronounced among the most vulnerable individuals, underscoring the pivotal influence of social inequalities on the prevalence of mental disorders in the region. Ideally, further research should prospectively investigate the incidence of these outcomes and triggering factors that may increase mental distress in Manaus. Societal and health services improvements are also needed to address mental health comprehensively.
Acknowledgments
The authors would like to thank Espaço da Escrita and Pró-Reitoria de Pesquisa-Unicamp for providing language services
Biographies
MSc. Pharmacist, PhD candidate
PhD. Pharmacist
PhD. Pharmacist
PhD. Pharmacist
Funding Statement
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) [grant numbers: 404990/2013-4 and 448093/2014-6] and the Fundação de Amparo à Pesquisa do Estado de São Paulo [grant number: 166710/2022]. Galvao TF received a productivity scholarship from CNPq [grant number: 313431/2023-0]
Footnotes
Sources of funding: This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) [grant numbers: 404990/2013-4 and 448093/2014-6] and the Fundação de Amparo à Pesquisa do Estado de São Paulo [grant number: 166710/2022]. Galvao TF received a productivity scholarship from CNPq [grant number: 313431/2023-0]
REFERENCES
- 1.Moitra M, Owens S, Hailemariam M, et al. Global Mental Health: Where We Are and Where We Are Going. Curr Psychiatry Rep. 2023;25(7):301–11. doi: 10.1007/s11920-023-01426-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lancet. Brain health and its social determinants. Lancet. 2021;398(10305):1021. doi: 10.1016/s0140-6736(21)02085-7. [DOI] [PubMed] [Google Scholar]
- 3.Dias MK, Ferigato SH, Fernandes A. Attention to the crisis in mental health: centralization and decentralization of practices. Cien Saude Colet. 2020;25(2):595–602. doi: 10.1590/1413-81232020252.09182018. [DOI] [PubMed] [Google Scholar]
- 4.Sousa NFS, Barros MBA, Medina LPB, Malta DC, Szwarcwald CL. Association of major depressive disorder with chronic diseases and multimorbidity in Brazilian adults, stratified by gender: 2019 National Health Survey. Rev Bras Epidemiol. 2021;24(suppl 2):e210015. doi: 10.1590/1980-549720210015.supl.2. [DOI] [PubMed] [Google Scholar]
- 5.Paes-Sousa R, Schramm JMA, Mendes LVP. Fiscal austerity and the health sector: the cost of adjustments. Cien Saude Colet. 2019;24(12):4375–84. doi: 10.1590/1413-812320182412.23232019. [DOI] [PubMed] [Google Scholar]
- 6.Aragão ES, Funcia FR. Fiscal austerity and its effects on the Brazilian Health Economic-Industrial Complex in the context of the COVID-19 pandemic. Cad Saude Publica. 2021;37(9):e00100521. doi: 10.1590/0102-311x00100521. [DOI] [PubMed] [Google Scholar]
- 7.Hamm AO. Fear, anxiety, and their disorders from the perspective of psychophysiology. Psychophysiology. 2020;57(2):e13474. doi: 10.1111/psyp.13474. [DOI] [PubMed] [Google Scholar]
- 8.Garnelo L. Specificities and challenges of public health policies in the Brazilian Amazon. Cad Saude Publica. 2019;35(12):e00220519. doi: 10.1590/0102-311x00220519. [DOI] [PubMed] [Google Scholar]
- 9.Silva MT, Galvao TF. Use of health services among adults living in Manaus Metropolitan Region, Brazil: population-based survey, 2015. Epidemiol Serv Saude. 2017;26(4):725–34. doi: 10.5123/s1679-49742017000400005. [DOI] [PubMed] [Google Scholar]
- 10.Silva MT, Nunes BP, Galvao TF. Use of health services by adults in Manaus, 2019: Protocol of a population-based survey. Medicine. 2019;98(21):e15769. doi: 10.1097/md.0000000000015769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tiguman GMB, Silva MT, Galvão TF. Prevalence of depressive and anxiety symptoms and their relationship with life-threatening events, tobacco dependence and hazardous alcohol drinking: a population-based study in the Brazilian Amazon. J Affect Disord. 2022;298(Pt A):224–31. doi: 10.1016/j.jad.2021.10.059. [DOI] [PubMed] [Google Scholar]
- 12.Silva MT, Caicedo Roa M, Martins SS, da Silva ATC, Galvao TF. Prevalence and correlates of depressive symptoms among adults living in the Amazon, Brazil: a population-based study. J Affect Disord. 2017;222:162–8. doi: 10.1016/j.jad.2017.06.053. [DOI] [PubMed] [Google Scholar]
- 13.Silva MT, Caicedo Roa M, Martins SS, da Silva ATC, Galvao TF. Generalized anxiety disorder and associated factors in adults in the Amazon, Brazil: A population-based study. J Affect Disord. 2018;236:180–6. doi: 10.1016/j.jad.2018.04.079. [DOI] [PubMed] [Google Scholar]
- 14.Instituto Brasileiro de Geografia e Estatística. Manaus, panorama, economia. Rio de Janeiro: IBGE; 2023. [Accessed in 2024 (July 19)]. Available from: https://cidades.ibge.gov.br/brasil/am/manaus/panorama. [Google Scholar]
- 15.Associação Brasileira de Empresas de Pesquisa. Critério de Classificação Econômica Brasil. 2015. [Accessed in 2024 (July 19)]. Available from: https://www.abep.org/criterio-brasil.
- 16.Associação Brasileira de Empresas de Pesquisa. Critério de Classificação Econômica Brasil. 2018. [Accessed in 2024 (July 19)]. Available from: https://www.abep.org/criterio-brasil.
- 17.Sousa TV, Viveiros V, Chai MV, et al. Reliability and validity of the Portuguese version of the Generalized Anxiety Disorder (GAD-7) scale. Health Qual Life Outcomes. 2015;13:50. doi: 10.1186/s12955-015-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monteiro RP, Nascimento BS, Monteiro TMC, da Silva PDG, Ferreira AJC. Psychometric Evidence of the 7-Item Generalized Anxiety Disorder Questionnaire in Brazil. Int J Ment Health Addiction. 2022;20(2):1023–34. doi: 10.1007/s11469-020-00423-9. [DOI] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–25. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 21.de Lima Osório F, Vilela Mendes A, Crippa JA, Loureiro SR. Study of the discriminative validity of the PHQ-9 and PHQ-2 in a sample of Brazilian women in the context of primary health care. Perspect Psychiatr Care. 2009;45(3):216–27. doi: 10.1111/j.1744-6163.2009.00224.x. [DOI] [PubMed] [Google Scholar]
- 22.Santos IS, Tavares BF, Munhoz TN, et al. Sensitivity and specificity of the Patient Health Questionnaire-9 (PHQ-9) among adults from the general population. Cad Saude Publica. 2013;29(8):1533–43. doi: 10.1590/0102-311x00144612. [DOI] [PubMed] [Google Scholar]
- 23.Ettman CK, Abdalla SM, Cohen GH, et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costantini L, Pasquarella C, Odone A, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. 2021;279:473–83. doi: 10.1016/j.jad.2020.09.131. [DOI] [PubMed] [Google Scholar]
- 26.COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12. doi: 10.1016/s0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hinz A, Esser P, Friedrich M, et al. Changes in anxiety in the general population over a six-year period. PLoS One. 2023;18(9):e0291206. doi: 10.1371/journal.pone.0291206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stocker R, Tran T, Hammarberg K, et al. Patient Health Questionnaire 9 (PHQ-9) and General Anxiety Disorder 7 (GAD-7) data contributed by 13,829 respondents to a national survey about COVID-19 restrictions in Australia. Psychiatry Res. 2021;298:113792. doi: 10.1016/j.psychres.2021.113792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shim RS, Baltrus P, Ye J, Rust G. Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005-2008. J Am Board Fam Med. 2011;24(1):33–8. doi: 10.3122/jabfm.2011.01.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arias de la Torre J, Vilagut G, Ronaldson A, et al. Prevalence and age patterns of depression in the United Kingdom. A population-based study. J Affect Disord. 2021;279:164–72. doi: 10.1016/j.jad.2020.09.129. [DOI] [PubMed] [Google Scholar]
- 31.Ryu S, Fan L. The Relationship Between Financial Worries and Psychological Distress Among U.S. Adults. J Fam Econ Issues. 2022;44(1):16–33. doi: 10.1007/s10834-022-09820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang X, Fang Y, Chen H, et al. Global, regional and national burden of anxiety disorders from 1990 to 2019: results from the Global Burden of Disease Study 2019. Epidemiol Psychiatr Sci. 2021;30:e36. doi: 10.1017/s2045796021000275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tseng H, Lee JI, Geng JH, Chen SC. Sex difference in the associations among risk factors with depression in a large Taiwanese population study. Front Public Health. 2023;11:1070827. doi: 10.3389/fpubh.2023.1070827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vinogradova VV, Kivite-Urtane A, Vrublevska J, Rancans E. Point prevalence and sex-specific associated factors of depression in Latvian general population. Front Psychiatry. 2023;14:1065404. doi: 10.3389/fpsyt.2023.1065404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kjeldsberg M, Tschudi-Madsen H, Bruusgaard D, Natvig B. Factors related to self-rated health: a survey among patients and their general practitioners. Scand J Prim Health Care. 2022;40(2):320–8. doi: 10.1080/02813432.2021.2022341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.González-Blanch C, Hernández-de-Hita F, Muñoz-Navarro R, et al. The association between different domains of quality of life and symptoms in primary care patients with emotional disorders. Sci Rep. 2018;8(1):11180. doi: 10.1038/s41598-018-28995-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith L, Shin JI, Butler L, et al. Physical multimorbidity and depression: A mediation analysis of influential factors among 34,129 adults aged ≥ 50 years from low- and middle-income countries. Depress Anxiety. 2022;39(5):376–86. doi: 10.1002/da.23250. [DOI] [PubMed] [Google Scholar]
- 38.Kang HJ, Bae KY, Kim SW, et al. Impact of Anxiety and Depression on Physical Health Condition and Disability in an Elderly Korean Population. Psychiatry Investig. 2017;14(3):240–8. doi: 10.4306/pi.2017.14.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adolph D, Schneider S, Margraf J. German Anxiety Barometer-Clinical and Everyday-Life Anxieties in the General Population. Front Psychol. 2016;7:1344. doi: 10.3389/fpsyg.2016.01344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schlax J, Junger C, Beutel ME, et al. Income and education predict elevated depressive symptoms in the general population: results from the Gutenberg health study. BMC Public Health. 2019;19(1):430. doi: 10.1186/s12889-019-6730-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Linder A, Gerdtham UG, Trygg N, Fritzell S, Saha S. Inequalities in the economic consequences of depression and anxiety in Europe: a systematic scoping review. Eur J Public Health. 2020;30(4):767–77. doi: 10.1093/eurpub/ckz127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rathod S, Pinninti N, Irfan M, et al. Mental Health Service Provision in Low- and Middle-Income Countries. Health Serv Insights. 2017;10:1178632917694350. doi: 10.1177/1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee J, Di Ruggiero E. How does informal employment affect health and health equity? Emerging gaps in research from a scoping review and modified e-Delphi survey. Int J Equity Health. 2022;21(1):87. doi: 10.1186/s12939-022-01684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alfers L, Rogan M. Health risks and informal employment in South Africa: does formality protect health? Int J Occup Environ Health. 2015;21(3):207–15. doi: 10.1179/2049396714y.0000000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lopez-Ruiz M, Artazcoz L, Martinez JM, Rojas M, Benavides FG. Informal employment and health status in Central America. BMC Public Health. 2015;15:698. doi: 10.1186/s12889-015-2030-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lopez-Ruiz M, Benavides FG, Vives A, Artazcoz L. Informal employment, unpaid care work, and health status in Spanish-speaking Central American countries: a gender-based approach. Int J Public Health. 2017;62(2):209–18. doi: 10.1007/s00038-016-0871-3. [DOI] [PubMed] [Google Scholar]
- 47.Tiguman GMB, Caicedo-Roa M, Silva MT, Galvao TF. Occupational exposures and health-related quality of life in the Manaus Metropolitan Region, Amazonas State, Brazil: a cross-sectional study. Cad Saude Publica. 2020;36(12):e00074520. doi: 10.1590/0102-311x00074520. [DOI] [PubMed] [Google Scholar]
- 48.Ko Ko T, Dickson-Gomez J, Yasmeen G, et al. Informal workplaces and their comparative effects on the health of street vendors and home-based garment workers in Yangon, Myanmar: a qualitative study. BMC Public Health. 2020;20(1):524. doi: 10.1186/s12889-020-08624-6. [DOI] [PMC free article] [PubMed] [Google Scholar]