Abstract
Central pancreatectomy (CP) is a viable option for low malignant tumors located in the neck or proximal body of the pancreas. This procedure has the advantage of minimizing impairment to pancreatic function. However, it is technically challenging and carries a relatively high risk of postoperative pancreatic fistula. Recently, minimally invasive CP surgery has gained popularity, with evidence supporting its safety and efficacy. Nevertheless, conventional laparoscopic CP presents technical difficulties, while robot-assisted CP is associated with higher costs. ArtiSential (LivsMed Inc.) is a device that has been successfully utilized in various surgical procedures, offering the ergonomic advantages of robotic surgery within a laparoscopic setting. In this article, we share our successful experience of performing laparoscopic CP using ArtiSential in a patient with intraductal papillary mucinous neoplasm.
Keywords: Laparoscopy, Pancreas, Pancreatectomy, Minimally invasive surgical procedures
INTRODUCTION
Recently, interest in preserving endocrine and exocrine functions of the pancreas after pancreatic surgery has increased. Parenchyma-sparing pancreatectomies such as enucleations, resections of the uncinate process, and central pancreatectomies (CPs) for benign to low-grade pancreatic tumors have attracted attention. Examples of these low-grade tumors include solitary pancreatic tumors and intraductal papillary mucinous neoplasms (IPMNs) [1]. Among the procedures, CP was first performed by Dagradi and Serio in 1982 for insulinoma patients and can be performed in patients with tumors that meet previously established criteria [1,2]. CP offers several advantages, including the preservation of pancreatic parenchyma, which helps prevent endocrine and exocrine dysfunction [3]. It also reduces the morbidity associated with the biliary and gastric anastomoses required in pancreatoduodenectomy (PD) [2] and avoids the need for splenectomy, often performed alongside distal pancreatectomy (DP), thereby preserving the spleen [1]. However, CP also has disadvantages, such as the technical difficulty associated with two cutting surfaces after segmental resection of the pancreas and the increased risk of postoperative pancreatic fistula (POPF) [1–3].
The proportion of minimally invasive surgeries (MISs) of the pancreas is increasing [4]. In pancreatic surgery, MIS has similar oncologic outcomes compared to open surgery and offers clear advantages in terms of faster postoperative recovery and cosmesis for patients [5]. MIS has been attempted in CPs, and its safety and feasibility have been demonstrated in several cases. However, laparoscopic CP has the disadvantage of being technically challenging due to the limited intracorporeal motion of laparoscopic instruments, and robot-assisted CP is often cost-prohibitive.
ArtiSential (LivsMed Inc.) is a newly developed multi–degree-of-freedom (DOF) articulating laparoscopic instrument that brings the ergonomic benefits of robotic surgery to laparoscopic surgery [6]. This instrument overcomes the spatial limitations of laparoscopic surgery and has been used in surgeries such as appendectomy, gastrectomy, colorectal surgery, and even pediatric surgery.
In this report, we present a case of laparoscopic CP using ArtiSential in a patient with low-grade IPMN in the neck of the pancreas.
METHODS
Patient information
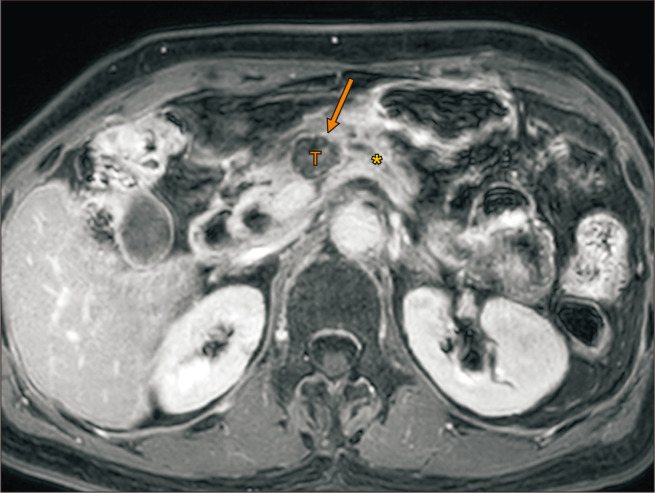
The patient is an 80-year-old female patient who underwent laparoscopic anterior resection for colon cancer in 2017. Her body mass index was 24.6 kg/m², she had no other medical history, including diabetes mellitus (DM), and there was no weight loss prior to her visit. During follow-up computed tomography (CT), a 2.8-cm cystic IPMN of branch duct type with high stigmata was observed in the pancreas body. The pancreatic duct was mildly dilatated to 3 mm (Fig. 1). Laboratory tests including tumor marker, amylase, and lipase levels were normal. Further ultrasound endoscopy showed a well-enhanced, 2.5-cm cystic lesion with a 1.8-cm mural nodule in the neck portion of the pancreas.
Fig. 1.
Preoperative magnetic resonance imaging. Cystic lesions are observed in the pancreas body (arrow), and the pancreatic duct (asterisk) is dilated in areas more distal than the tumor (T).
Surgical technique
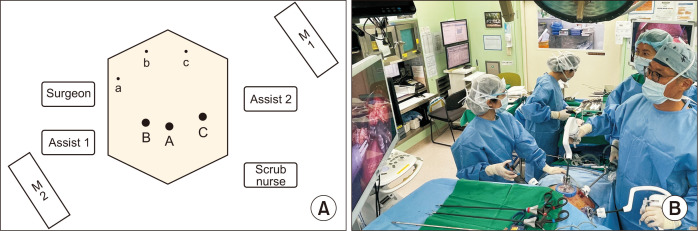
The patient underwent ArtiSential-assisted CP on April 21, 2023. She was originally scheduled for DP, but CP was attempted because the malignancy was low-grade and the case met established CP criteria [1,2]. The surgery was divided into two stages, the laparoscopic resection stage and the ArtiSential-assisted reconstruction stage. The trocar position was consistent with that in laparoscopic PD [7]. Six trocars were used in total: three 5-mm trocars and three 12-mm trocars. The surgeon was positioned to the right of the patient and did not change position during the surgery. The placement of the trocars and the layout of the operating room are shown in Fig. 2.
Fig. 2.
Schematic diagram showing the trocar position and operator position, and the actual surgical field. The surgeon stands on the right side of the patient during the entire surgical procedure. A total of six ports approach was performed: three 5-mm ports (A–C) and three 12-mm ports (a–c). The scope held by assist 1 alternates between ports A and B depending on the surgical procedure; and during the anastomosis phase, the scope is placed in port B and the ArtiSential instruments (LivsMed Inc.) are placed in ports A and a to perform anastomosis. Assist 2 uses ports C and c to properly expose the surgical field. Two monitors (M1, M2) show the surgical field of the surgeon and assistants on opposite sides.
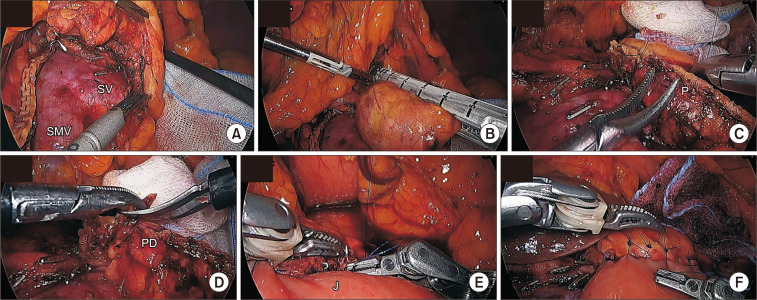
First, the gastrocolic ligament was divided with a SONICBEAT (Olympus) a few centimeters from the gastroepiploic arcade of the stomach body. Next, the stomach was lifted by an assistant at the 12 o’clock position to expose the pyloric area; and the anterosuperior part of the pancreas head and the inferior part of the pylorus were separated to fully expose the pancreatic neck. The superior and inferior borders of the pancreas were then mobilized to create a tunnel between the superior mesenteric vein and the pancreas. An endo-GIA (Medtronic) stapler was inserted along the tunnel, and the proximal part of the pancreas was resected. To ensure a sufficient resection margin, the distal part of the pancreas was further mobilized using an energy device and clips (Fig. 3A). The distal margin was also resected with an endo-GIA stapler (Fig. 3B), and the resected pancreas was placed in a retrieval bag and removed from the abdominal cavity. A prolene 5-0 reinforcement suture was placed along the stapler line at the distal margin (Fig. 3C). The pancreatic duct area at the distal margin was cut with laparoscopic scissors to expose a duct approximately 5 mm in diameter (Fig. 3D). To perform pancreatojejunostomy (PJ), the jejunum was transected approximately 50 cm distal to the ligament of Treitz to approach the distal Roux-en-Y limb through the retromesenteric window to the distal pancreatic resection margin.
Fig. 3.
Operative images. (A) Distal pancreas mobilization with energy device. (B) Distal margin resection with endo-GIA (Medtronic). (C) Distal margin reinforcement prolene 5-0 suturing. (D) Identification of pancreatic duct with laparoscopic scissors. (E) Duct-to-mucosa suture with ArtiSential (LivsMed Inc.). (F) Anterior layer suture with ArtiSential. SMV, superior mesenteric vein; SV, splenic vein; P, remnant pancreas; PD, pancreatic duct; J, jejunum.
After the resection stage, PJ was performed using two ArtiSential instruments, a fenestrated grasper, and a needle holder. First, an interrupted suture was positioned from the superior to the inferior part of the pancreas using prolene 5-0 for the posterior layer to approximate the pancreas and jejunum. During suturing, the needle was directed towards the pancreas, passing through the jejunum first, then the pancreas, followed by the tie. Then, a duct-to-mucosa anastomosis was performed. A silicone catheter was inserted during the anastomosis, and seven interrupted prolene 5-0 sutures completed the anastomosis (Fig. 3E). Again, the needle passed through the jejunal opening first, followed by the pancreatic duct. After the duct-to-mucosa anastomosis, interrupted prolene 5-0 sutures were placed from the superior to the inferior pancreas to complete the PJ (Fig. 3F). To complete the Roux-en-Y PJ, the jejunojejunostomy was performed with a hand-sewn side-to-side anastomosis extra-corporeally through the umbilical wound. The proximal margin of the pancreas and the PJ site were covered with polyglycolic acid sheets (Neoveil, GUNZE Ltd.) patch to prevent POPF. The surgical procedure is shown in the Supplementary Video 1.
RESULTS
The operative time was 242 minutes, and the blood loss was 50 mL. Sips of water were started on postoperative day (POD) 1, and the patient was started on a liquid diet on POD 2. The patient had flatulence on POD 3 and no POPF. The drain was removed on POD 5, and the follow-up CT on POD 6 was unremarkable except for mild fluid collection around the pancreas. The patient was discharged on POD 7 without any special events. Pathology showed that the resected 1.7 × 1.6-cm tumor had a safety margin of 0.5 cm. Histologic findings were a branch duct-type IPMN with low-grade dysplasia. There was no evidence of DM or exocrine insufficiency postoperatively. The patient has been followed up on an outpatient basis for 6 months without recurrence.
DISCUSSION
Robotics are being used increasingly for pancreatic surgeries worldwide [8]. However, despite the many advantages of robotic surgery, its high cost limits accessibility. Therefore, various laparoscopic articulated tools have been developed to reproduce the articulated and wristed features of robotic surgery. ArtiSential is one of those recently developed, multi-DOF articulated instruments. Our center has demonstrated its safety and feasibility by applying ArtiSential to laparoscopic cholecystectomy and laparoscopic PD [9].
The efficacy of CP compared to PD or DP for pancreatic tumors has been studied, but the issue is still controversial. Compared to PD or DP, CP preserves the parenchyma of the pancreas and prevents impairment of exocrine and endocrine functions but has the disadvantage of increased complications such as POPF [1–3]. Improving the quality of life by preventing exocrine and endocrine impairment has clear long-term benefits, especially in cases with long residual life expectancy such as those with low-grade malignancies. In our case, the patient did not develop DM or exocrine insufficiency after surgery.
CP is difficult with the conventional laparoscopic approach for several reasons. The remnant pancreas tends to be relatively soft, the pancreatic duct is smaller, and the cut surface of the pancreas is larger. In addition, as shown in Fig. 3 and Supplementary Video 1, during PJ in CP, the resection margin of the pancreas is skewed toward the patient’s left side, and the anastomosis direction is nearly perpendicular to the axis of the laparoscopic instrument. This presents a significant challenge with conventional laparoscopic instruments, which have limited articulation, making precise suturing in these difficult orientations extremely challenging. Moreover, the placement of the Roux-en-Y limb into the resected space further obscures the view of the distal pancreas, complicating the suturing process [10].
ArtiSential addresses these limitations by offering wrist-like articulation, similar to robotic instruments, enabling precise and intuitive movements, even in complex and awkward positions. The multidirectional articulation of the ArtiSential instruments allows surgeons to place sutures more easily at difficult angles, especially during the delicate PJ. The wristed motion facilitates accurate needle placement and secure knot tying, reducing the strain on the surgeon and improving overall ergonomics. In this case, the use of ArtiSential during PJ proved particularly beneficial in navigating the intricate spatial relationships. Its articulation allowed for precise needle manipulation in both horizontal and vertical planes, resulting in smoother suturing and minimizing the risk of tension or misalignment at the anastomosis site. This flexibility is a significant advantage, particularly when the PJ site is tilted or positioned away from the surgeon’s usual operating axis.
However, there are some drawbacks to ArtiSential. A long learning curve for surgeons is one limitation. Surgeons are often confused at first by the combination of the fulcrum principle of laparoscopic surgery and the intuitive movements of robotic surgery in one instrument. The size and weight of the instruments can also make them difficult for surgeons with small hands or weakness to use effectively. However, the advantages outweigh these disadvantages. Once the surgeon becomes accustomed to using ArtiSential, he/she will be able to effectively perform the CP reconstruction stage anastomosis. The cost concerns of robotic surgery can be avoided.
In conclusion, this case report is the first of ArtiSential-assisted CP and demonstrates that ArtiSential features can be used to perform surgery safely and effectively in cases that are difficult to perform with conventional laparoscopic instruments. The rarity of tumors that meet the criteria for CP precludes collection of many cases in a short time period; but as more cases are collected, quantifiable comparison of surgical outcomes of conventional laparoscopic CP and ArtiSential-assisted CP will be possible, as will derivation of the objective advantages of ArtiSential-assisted CP.
Supplementary materials
Supplementary materials can be found via https://doi.org/10.7602/jmis.2024.27.4.227
Notes
Ethics statements
The Institutional Review Board of Severance Hospital provided approval for this study and granted a waiver of informed consent after determining that the video footage is devoid of any identifying information (No. 4-2023-0547). This measure aligns with ethical standards by ensuring that the data is entirely non-identifiable and that participants’ privacy is maintained.
Authors’ contributions
Conceptualization, Funding acquisition: CMK
Investigation: JHJ
Methodology, Visualization: All authors
Writing–original draft: JHJ
Writing–review & editing: CMK
All authors read and approved the final manuscript.
Conflict of interest
All authors have no conflicts of interest to declare.
Funding/support
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C0767).
Data availability
The data presented in this study are available upon reasonable request to the corresponding author.
References
- 1.Kang CM, Lee JH, Lee WJ. Minimally invasive central pancreatectomy: current status and future directions. J Hepatobiliary Pancreat Sci. 2014;21:831–840. doi: 10.1002/jhbp.143. [DOI] [PubMed] [Google Scholar]
- 2.Iacono C, Bortolasi L, Facci E, et al. The Dagradi-Serio-Iacono operation central pancreatectomy. J Gastrointest Surg. 2007;11:364–376. doi: 10.1007/s11605-007-0095-1. [DOI] [PubMed] [Google Scholar]
- 3.Dragomir MP, Sabo AA, Petrescu GED, Li Y, Dumitrascu T. Central pancreatectomy: a comprehensive, up-to-date meta-analysis. Langenbecks Arch Surg. 2019;404:945–958. doi: 10.1007/s00423-019-01829-3. [DOI] [PubMed] [Google Scholar]
- 4.Deichmann S, Wellner U, Bolm L, et al. Minimally invasive approaches in pancreatic cancer surgery. Eur Surg. 2024;56:76–85. doi: 10.1007/s10353-023-00812-z. [DOI] [Google Scholar]
- 5.van Hilst J, de Rooij T, Klompmaker S, et al. Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): A pan-European propensity score matched study. Ann Surg. 2019;269:10–17. doi: 10.1097/SLA.0000000000002561. [DOI] [PubMed] [Google Scholar]
- 6.Min SH, Cho YS, Park K, et al. Multi-DOF (Degree of Freedom) articulating laparoscopic instrument is an effective device in performing challenging sutures. J Minim Invasive Surg. 2019;22:157–163. doi: 10.7602/jmis.2019.22.4.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Navarro JG, Kang CM. Pitfalls for laparoscopic pancreaticoduodenectomy: need for a stepwise approach. Ann Gastroenterol Surg. 2019;3:254–268. doi: 10.1002/ags3.12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright GP, Zureikat AH. Development of minimally invasive pancreatic surgery: an evidence-based systematic review of laparoscopic versus robotic approaches. J Gastrointest Surg. 2016;20:1658–1665. doi: 10.1007/s11605-016-3204-1. [DOI] [PubMed] [Google Scholar]
- 9.Kang CM. Technical note safe and effective laparoscopic cholecystectomy. Special ed. Biomedbook; 2023. [Google Scholar]
- 10.Chong EH, Jang JY, Choi SH. Robotic central pancreatectomy: a surgical technique. J Minim Invasive Surg. 2023;26:155–161. doi: 10.7602/jmis.2023.26.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.