Abstract
目的
通过生物力学试验探讨下胫腓联合损伤重建术中螺钉理想植入角度。
方法
选取24个成年尸体踝关节标本制备下胫腓联合损伤模型后,根据螺钉植入角度随机分为A(0°)、B(10°~15°)、C(20°~25°)、D(30°~35°)组,分别在离踝关节近端2 cm水平处植入螺钉。采用生物力学试验机,在中立、背伸(10°)、跖屈(15°)、内翻(10°)和外翻(15°)位,施加0~700 N轴向载荷,测量腓骨位移(压力分离试验);在中立位以内旋和外旋施加0~5 N·m扭矩载荷,测量腓骨位移(扭矩分离试验)。
结果
压力分离试验中,不同体位及载荷条件下,C组位移均最小。中立位时,A组300~700 N载荷条件下、B组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05);背伸位时,A组500~700 N载荷下、B组及D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05),而A组各载荷条件下位移均小于B组(P<0.05);跖屈位时,D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05);外翻位时,A组400~700 N载荷条件下、B组及D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05)。扭矩分离试验中,不同载荷条件下C组位移最小、B组最大。内旋时,B组各载荷条件下、D组3~5 N·m载荷条件下位移与C组比较,差异有统计学意义(P<0.05);外旋时,B组和D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05)。其余条件下各组间差异均无统计学意义(P>0.05)。
结论
下胫腓联合损伤重建术中螺钉植入理想角度为20°~25°,以该角度植入螺钉固定后腓骨位移更小。
Keywords: 下胫腓联合损伤, 螺钉固定, 植入角度, 生物力学
Abstract
Objective
To investigate ideal screw implant angle in reconstruction of tibiofibular syndesmosis injury by using a biomechanical test.
Methods
A total of 24 ankle specimens from adult cadavers were used as the tibiofibular syndesmosis injury model. According to the angle of screw placement, the tibiofibular syndesmosis injury models were randomly divided into groups A (0°), B (10°-15°), C (20°-25°), and D (30°-35°), and the screws were placed at a level 2 cm proximal to the ankle joint. The displacement of fibula was measured by biomechanical testing machine at neutral, dorsiflexion (10°), plantar flexion (15°), varus (10°), and valgus (15°) positions, with axial load of 0-700 N (pressure separation test). The displacement of fibula was also measured at neutral position by applying 0-5 N·m torque load during internal and external rotation (torsional separation test).
Results
In the pressure separation test, group C exhibited the smallest displacement under different positions and load conditions. At neutral position, significant differences were observed (P<0.05) between group A and group C under load of 300-700 N, as well as between group B and group C under all load conditions. At dorsiflexion position, significant differences were observed (P<0.05) between group A and group C under load of 500-700 N, as well as between groups B, D and group C under all load conditions, and the displacements under all load conditions were significantly smaller in group A than in group B (P<0.05). At plantar flexion position, significant differences were observed (P<0.05) between group D and group C under all load conditions. At valgus position, significant differences were observed (P<0.05) between group A and group C under load of 400-700 N, as well as between groups B, D and group C under all load conditions. In the torsional separation test, group C exhibited the smallest displacement and group B had the largest displacement under different load conditions. During internal rotation, significant differences were observed (P<0.05) between group B and group C under all load conditions, as well as between group D and group C at load of 3-5 N·m. During external rotation, significant differences were observed between groups B, D and group C under all load conditions (P<0.05). No significant difference was detected between groups at the remaining load conditions (P>0.05).
Conclusion
The ideal screw implant angle in reconstruction of tibiofibular syndesmosis injury was 20°-25°, which has a small displacement of fibula.
Keywords: Tibiofibular syndesmosis injury, screw fixation, implant angle, biomechanics
下胫腓联合包括下胫腓前、后韧带和骨间韧带,是维持踝关节稳定性的重要解剖结构[1]。下胫腓联合损伤是常见踝关节损伤类型之一,通常是踝关节于背伸位下胫腓联合过度外旋导致,最终出现踝关节不稳定、慢性疼痛等[2-5]。螺钉固定是治疗此类损伤的一种简单方法,能够提供关节即刻稳定性,这对于早期恢复踝关节功能至关重要;而且与其他固定方式相比,其成本通常较低,患者经济负担较小[6]。目前,螺钉固定于胫距关节上方2~5 cm处已达成共识[5, 7],但是植入角度仍存在争议。通常通过螺钉固定踝关节始终保持在中立位[1, 8-9],但在负重过程中由于腓骨试图纵向移动产生剪切应力,故常发生螺钉严重损坏情况[10]。Laflamme等[11]的研究也显示将螺钉放置在不合适位置可能导致活动过程中过度磨损;严重时需行二次手术且手术风险大大增加[7, 12]。因此,有必要找到螺钉最合适植入角度。本研究采用尸体标本建立下胫腓联合损伤模型,将皮质骨螺钉以不同角度植入固定,测试不同负荷模式下生物力学特性,为临床选择合适的螺钉植入角度提供参考。
1. 材料与方法
1.1. 试验标本
成年尸体踝关节标本24个(左、右足各12个),由西南医科大学解剖教研室提供。标本外观完整,均排除先天性发育不良或其他肌肉、骨骼疾病。标本均于−24℃储存,测试前置于室温解冻12 h。
1.2. 试验方法
1.2.1. 下胫腓联合损伤模型制备
于标本胫骨上方8 cm至距下关节和舟骨关节范围,清除皮肤、筋膜及下胫腓联合周围软组织,最大程度减少相邻组织牵拉对生物力学测试的影响;切除伸肌腱,显露局部其他肌肉、肌腱;再切断腓骨肌腱,剥离附着于腓骨的腓骨短肌并拉至一边暴露外踝。切断下胫腓联合,制备下胫腓联合损伤模型。
1.2.2. 螺钉内固定模型及分组
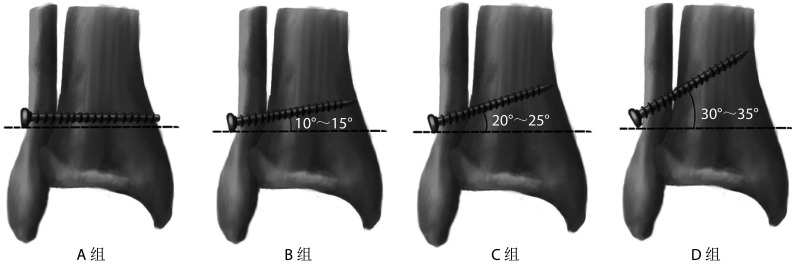
研究采用北京德益达美医疗科技有限公司皮质骨螺钉。将制备的下胫腓联合损伤模型随机分为A、B、C、D组,每组6个标本。各组模型固定于背伸5° 位,在离踝关节近端2 cm水平作直径3.5 mm钻孔,建立不同角度皮质骨螺钉固定模型,A~D组分别以与水平面成0°、10°~15°、20°~25°、30°~35° 植入皮质骨螺钉(图1)。建模完成后,使用量角器测量以确保植入角度准确。
图 1.
Schematic diagram of cortical bone screw implant angle for each group
各组皮质骨螺钉植入角度示意图
1.2.3. 生物力学测试
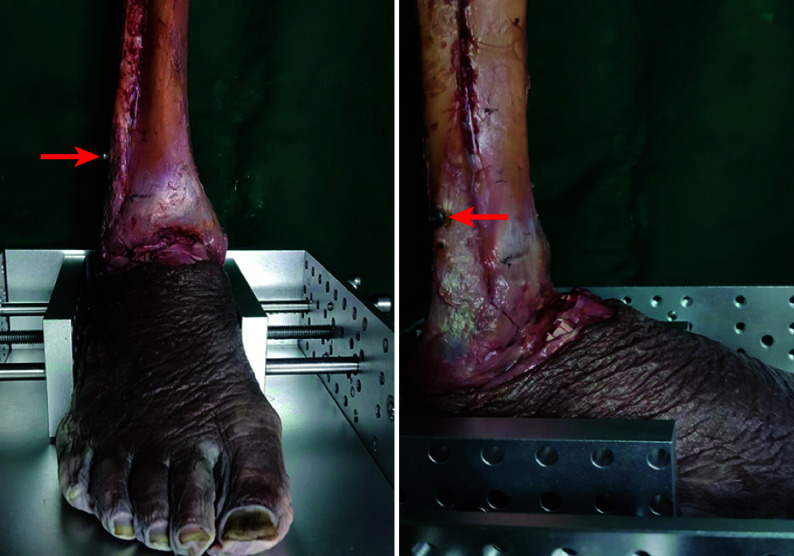
采用美国Bose公司生物力学试验机(Power 3520-AT)进行生物力学测试。测试期间将标本放置在夹具中,以确保模型稳定(图2)。
图 2.
Schematic diagram of specimen fixation on biomechanical testing machine
标本固定于生物力学试验机示意图
箭头示皮质骨螺钉固定
Arrow for the cortical bone screw fixation
① 压力分离试验:将标本连接至固定装置,一端绑定于生物力学试验机动态单元,另一端连接并固定于固定单元。分别将标本固定于中立、背伸(10°)、跖屈(15°)、内翻(10°)和外翻(15°)位进行测试。轴向载荷设定为0~700 N,以100 N/s恒定速度施加载荷,加载间隔2 min。记录100、200、300、400、500、600、700 N载荷下腓骨位移,重复测量3次,取均值。
② 扭转分离试验:将标本固定于中立位进行内、外旋扭转分离试验。扭转载荷0~5 N·m,转矩速度0.1 (N·m)/s,加载间隔2 min。记录1、2、3、4、5 N·m扭转载荷下腓骨位移,重复测量3次,取均值。
1.3. 统计学方法
采用SPSS22.0统计软件进行分析。计量资料经Shapiro-Wilk检验均符合正态分布,数据以均数±标准差表示,组间比较采用单因素方差分析,两两比较采用Tukey检验。检验水准取双侧α=0.05。
2. 结果
2.1. 压力分离试验
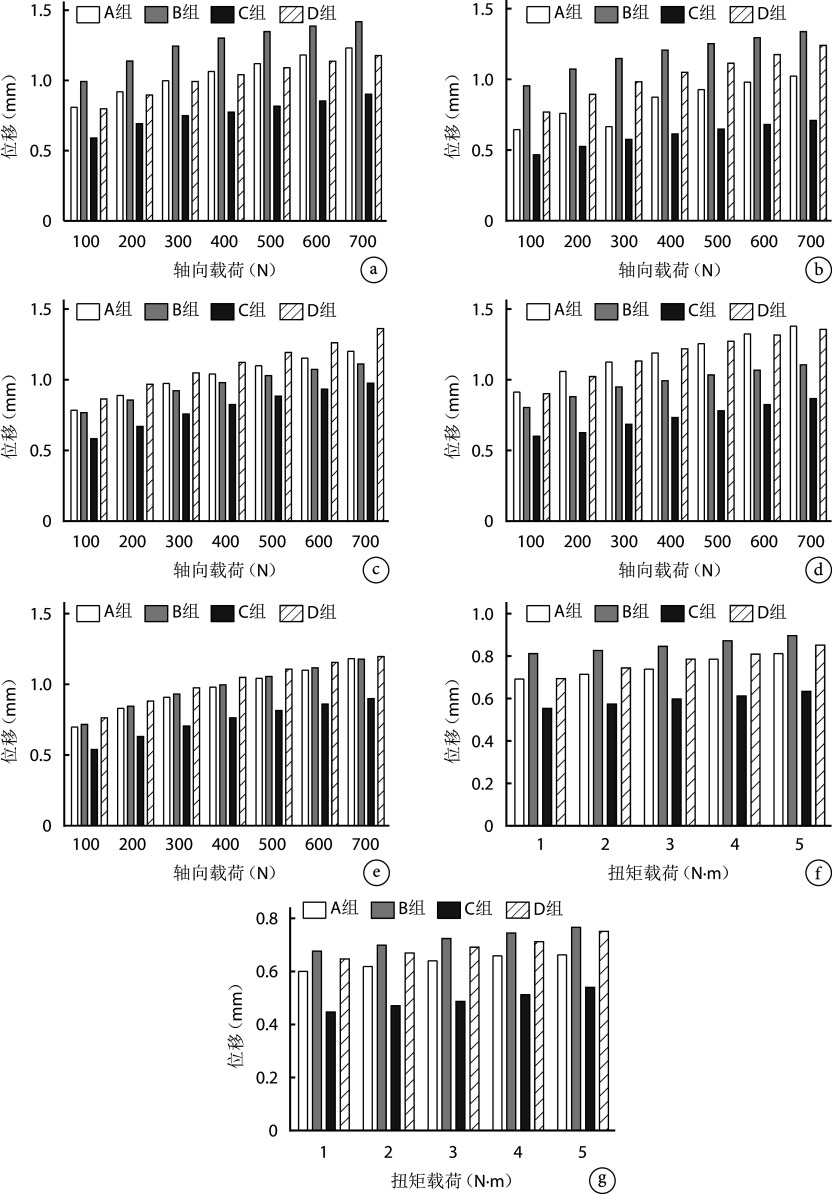
不同体位及载荷条件下,C组位移均最小。中立位时,A组300~700 N载荷条件下、B组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05)。背伸位时,A组500~700 N载荷下、B组及D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05);A组与B组各载荷条件下差异亦有统计学意义(P<0.05)。跖屈位时,D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05)。外翻位时,A组400~700 N载荷条件下、B组及D组各载荷条件下位移与C组比较,差异有统计学意义(P<0.05)。其余条件下各组间位移差异均无统计学意义(P>0.05)。见图3a~e。
图 3.
Biomechanical test results
生物力学测试结果
a~e. 中立、背伸、跖屈、内翻和外翻位压力分离试验;f、g. 内、外旋扭矩分离试验
a-e. Pressure separation test at neutral, dorsiflexion, plantar flexion, varus, and valgus positions; f, g. Internal and external rotation torque separation test
2.2. 扭矩分离试验
不同载荷条件下,C组位移最小、B组最大。内旋时,B组各载荷条件下、D组3~5 N·m载荷条件下位移与C组比较,差异均有统计学意义(P<0.05)。外旋时,B组和D组各载荷条件下位移与C组比较,差异均有统计学意义(P<0.05)。其余条件下各组间位移差异均无统计学意义(P>0.05)。见图3 f、g。
3. 讨论
螺钉固定是治疗下胫腓联合损伤的金标准,但其螺钉植入角度仍存在争议。为确保固定强度,需在腓骨和胫骨冠状面后外侧位置倾斜植入螺钉,并穿过至少四层皮质,以增强抵抗胫、腓骨位移的能力。Hu等[3]使用6个新鲜尸体下肢标本,通过摄像机观察不同踝关节位置下施加600 N轴向载荷时远端腓骨位移和旋转情况。他们发现当踝关节从中立位到跖屈位时,腓骨远端倾向于向内侧和前方移动并内旋;从中立位到背伸位时,腓骨远端倾向于向外侧和后方移动并外旋。由此可见,下胫腓联合在限制胫、腓骨相对位移中起到关键作用。
目前,临床上常规螺钉固定植入角度为与水平面成20°~30°[13-15]。然而,Park等[14]研究表明,从后外侧到前内侧的螺钉放置平均理想角度为18.8°。我们研究发现,C组在不同踝关节位置腓骨位移均最小,但是C组并非与其他各组均存在统计学差异。相关生物力学研究显示,将螺钉固定于胫距关节上方20~25 mm处可产生最高的等效应力和最佳固定效果,在关节上方30~40 mm处则会降低等效应力[16-19]。结合上述研究,我们认为将螺钉以20°~25° 植入后,下胫腓联合与螺钉固定端处于合适位置,可能具有更高的等效应力和更佳的固定效果。此外,若在此位置出现螺钉损坏,手术拆除较容易[19]。在背伸位,A组与B组差异存在统计学意义,且A组位移较小。这可能是由于螺钉在水平固定时,中立和背伸位运动轴与螺钉固定方向一致所致[9,17,20]。在承重过程中,人体腓骨轴向负荷占体质量的6.4%~17%,对保持踝关节的机械稳定性至关重要[19,21]。相较于外翻,腓骨在内翻时表现出更大的位移,这可能是因为腓骨远端在外翻位能承受更大负荷,从而有利于踝关节稳定[11,22]。
下胫腓联合损伤通常涉及踝关节轴向背伸力和外旋扭矩联合作用[23]。我们研究发现,在扭转分离试验中,C组位移最小,与B、D组相比差异有统计学意义,表明螺钉以与水平面成20°~25° 植入固定效果更佳,能提供更好的稳定性。这与既往有限元分析结果一致,即螺钉在前倾25° 植入时能更有效地分散应力,降低螺钉断裂风险,并增强踝关节稳定性[24]。此外,在内旋和外旋载荷作用下,螺钉最大应力点均位于胫、腓骨之间靠近胫骨处。而在前倾25° 植入时,无论内旋还是外旋载荷下,螺钉最大位移均较小,能提供更强稳定性[24]。
综上述,在下胫腓联合损伤螺钉固定治疗中,选择与水平面成20°~25° 植入螺钉固定后腓骨位移更小。但本研究样本量少,且模型制备时切除了周围软组织,与临床踝关节正常生理应变状态存在一定差距,研究结论需进一步临床研究明确。
利益冲突 在课题研究和文章撰写过程中不存在利益冲突;经费支持没有影响文章观点和对研究数据客观结果的统计分析及其报道
伦理声明 研究方案经西南医科大学附属中医医院伦理委员会批准(YJ-KY2021012)
作者贡献声明 张磊:研究设计及实施、文章撰写、经费支持;周鑫:研究实施;张梦瑶、熊吉祥:数据收集整理及统计分析;李明慧、王俊秋:文章撰写;石厚银、汪国友:文章撰写、行政支持
Funding Statement
2022年西南医科大学附属中医医院科研团队培育项目(2022-CXTD-08);2023年度四川省中医药管理局中医药科研专项课题面上项目(中医药基础)(2023MS248);2023年度泸州市科技计划项目(科技创新领军人才)(2023RCX172)
Scientific Research Cultivation Project of the Affiliated Traditional Chinese Medicine Hospital, Southwest Medical University (2022-CXTD-08); General Project of Sichuan Traditional Chinese Medicine Administration Traditional Chinese Medicine Research Special Project (Fundamentals of Traditional Chinese Medicine) (2023MS248); Luzhou Science and Technology Program (Leading Talents in Scientific and Technological Innovation) (2023RCX172)
References
- 1.Tourné Y, Molinier F, Andrieu M, et al Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res. 2019;105(8S):S275–S286. doi: 10.1016/j.otsr.2019.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Delahunt E, Farrell G, Boylan A, et al Mechanisms of acute ankle syndesmosis ligament injuries in professional male rugby union players: a systematic visual video analysis. Br J Sports Med. 2021;55(12):691–696. doi: 10.1136/bjsports-2020-102281. [DOI] [PubMed] [Google Scholar]
- 3.Hu WK, Chen DW, Li B, et al. Motion of the distal tibiofibular syndesmosis under different loading patterns: A biomechanical study. J Orthop Surg (Hong Kong), 2019, 27(2): 2309499019842879.
- 4.Yuen CP, Lui TH Distal tibiofibular syndesmosis: anatomy, biomechanics, injury, and management. Open Orthop J. 2017;11:670–677. doi: 10.2174/1874325001711010670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu K, Zhang J, Zhang P, et al Comparison of suture-button versus syndesmotic screw in the treatment of distal tibiofibular syndesmosis injury: a meta-analysis. J Foot Ankle Surg. 2021;60(3):555–566. doi: 10.1053/j.jfas.2020.08.005. [DOI] [PubMed] [Google Scholar]
- 6.薛阳, 赵永杰, 邓明明, 等 TightRope弹性固定联合下胫腓韧带功能性全修复治疗下胫腓联合损伤. 中国修复重建外科杂志. 2023;37(8):964–969. doi: 10.7507/1002-1892.202305020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walley KC, Hofmann KJ, Velasco BT, et al Removal of hardware after syndesmotic screw fixation: a systematic literature review. Foot Ankle Spec. 2017;10(3):252–257. doi: 10.1177/1938640016685153. [DOI] [PubMed] [Google Scholar]
- 8.Cornu O, Manon J, Tribak K, et al Traumatic injuries of the distal tibiofibular syndesmosis. Orthop Traumatol Surg Res. 2021;107(1S):102778. doi: 10.1016/j.otsr.2020.102778. [DOI] [PubMed] [Google Scholar]
- 9.Swords MP, Shank JR Indications and surgical treatment of acute and chronic tibiofibular syndesmotic injuries with and without associated fractures. Foot Ankle Clin. 2021;26(1):103–119. doi: 10.1016/j.fcl.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Wang L, Wang B, Xu G, et al Biomechanical comparison of bionic, screw and Endobutton fixation in the treatment of tibiofibular syndesmosis injuries. Int Orthop. 2016;40(2):307–314. doi: 10.1007/s00264-015-2920-6. [DOI] [PubMed] [Google Scholar]
- 11.Laflamme M, Belzile EL, Bédard L, et al A prospective randomized multicenter trial comparing clinical outcomes of patients treated surgically with a static or dynamic implant for acute ankle syndesmosis rupture. J Orthop Trauma. 2015;29(5):216–223. doi: 10.1097/BOT.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 12.Baek JH, Kim TY, Kwon YB, et al Radiographic change of the distal tibiofibular joint following removal of transfixing screw fixation. Foot Ankle Int. 2018;39(3):318–325. doi: 10.1177/1071100717745526. [DOI] [PubMed] [Google Scholar]
- 13.McKeon PO, Donovan L A perceptual framework for conservative treatment and rehabilitation of ankle sprains: an evidence-based paradigm shift. J Athl Train. 2019;54(6):628–638. doi: 10.4085/1062-6050-474-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park YH, Choi WS, Choi GW, et al Ideal angle of syndesmotic screw fixation: A CT-based cross-sectional image analysis study. Injury. 2017;48(11):2602–2605. doi: 10.1016/j.injury.2017.08.067. [DOI] [PubMed] [Google Scholar]
- 15.Penera K, Manji K, Wedel M, et al Ankle syndesmotic fixation using two screws: risk of injury to the perforating branch of the peroneal artery. J Foot Ankle Surg. 2014;53(5):534–538. doi: 10.1053/j.jfas.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Sierra-Martínez O, Saucedo-Valencia J, Saldívar-Moreno A. Functionality and stability of the treatment of Weber B ankle fractures with syndesmotic injury depending on the placement level of the screw (2.0 versus 3.5 cm). Acta Ortop Mex, 2017, 31(6): 264-268.
- 17.Sipahioglu S, Zehir S, Isikan UE Syndesmotic screw fixation in tibiofibular diastasis. Niger J Clin Pract. 2018;21(6):692–697. doi: 10.4103/njcp.njcp_5_17. [DOI] [PubMed] [Google Scholar]
- 18.Solan MC, Davies MS, Sakellariou A Syndesmosis stabilisation: Screws versus flexible fixation. Foot Ankle Clin. 2017;22(1):35–63. doi: 10.1016/j.fcl.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Weng Q, Lin C, Liu Y, et al Biomechanical analysis of a novel syndesmotic plate compared with traditional screw and suture button fixation. J Foot Ankle Surg. 2020;59(3):522–528. doi: 10.1053/j.jfas.2019.07.025. [DOI] [PubMed] [Google Scholar]
- 20.Lubberts B, Vopat BG, Wolf JC, et al Arthroscopically measured syndesmotic stability after screw vs. suture button fixation in a cadaveric model. Injury. 2017;48(11):2433–2437. doi: 10.1016/j.injury.2017.08.066. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy MT, Carmody O, Leong S, et al A computed tomography evaluation of two hundred normal ankles, to ascertain what anatomical landmarks to use when compressing or placing an ankle syndesmosis screw. Foot (Edinb) 2014;24(4):157–160. doi: 10.1016/j.foot.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Akoh CC, Phisitkul P Anatomic ligament repairs of syndesmotic injuries. Orthop Clin North Am. 2019;50(3):401–414. doi: 10.1016/j.ocl.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Patel NK, Chan C, Murphy CI, et al. Hybrid fixation restores tibiofibular kinematics for early weightbearing after syndesmotic injury. Orthop J Sports Med, 2020, 8(9): 2325967120946744.
- 24.米涛, 丁军稳, 李泽清, 等 单枚下胫腓联合螺钉不同角度固定下胫腓损伤的生物力学特性. 中国组织工程研究. 2022;26(36):5770–5774. doi: 10.12307/2022.788. [DOI] [Google Scholar]