Abstract
Background:
Digital knowledge translation (KT) interventions play a crucial role in advancing adolescent sexual and reproductive health (ASRH). Despite the extensive literature on their effectiveness, there’s a lack of synthesized evidence on the efficacy of digital KT tools for adolescent ASRH globally.
Objectives:
This review aimed to systematically identify and map existing empirical evidence on digital KT tools targeting ASRH outcomes and identify research gaps.
Design:
The review employed an evidence gap-map (EGM) approach following 2020 PRISMA reporting guidelines.
Data sources and methods:
A comprehensive literature search was conducted across databases including Medline, EMBASE, Global Health, CINAHL, Scopus, and Cochrane. Covidence software was used for data management. EPPI-Mapper software was used to synthesize findings and develop a graphical EGM.
Results:
The EGM comprises 68 studies: 59 experimental and 9 systematic reviews, predominantly from African (19 studies) and American regions (22 studies), with limited research from the Eastern Mediterranean and South East Asian regions. It examines digital KT tools’ influence on sexual and reproductive health (SRH) outcomes, identifying research gaps. Websites are extensively studied for their impact on adolescent behavior, knowledge, attitude, and self-efficacy, yet research on their effects on ASRH and health services access is limited. Similarly, mobile apps and short message service (SMS)/text messages impact various aspects of SRH outcomes, but research on their effects on health services utilization is insufficient. Interventions like digital pamphlets and gaming lack exploration in health service access. OTT media and social media need further investigation. Mass media, including radio, television, and podcasts, are largely unexplored in adolescent SRH outcomes. Topics such as menstrual hygiene, abortion, and sexual and intimate partner violence also lack research.
Conclusion:
The review underscores the dominance of certain KT tool interventions like SMS and websites. Despite advancements, research gaps persist in exploring diverse digital platforms on underrepresented outcomes globally. Future research should expand exploration across digital platforms and broaden the scope of outcome measures.
Trial registration:
The protocol is registered with PROSPERO (CRD42022373970).
Keywords: adolescents, sexual and reproductive health, digital tools, knowledge translation, evidence gap-map
Introduction
According to the World Health Organization (WHO) 2023, adolescence is a crucial phase typically ranging from aged 10 to 19 years, marked by significant physical, emotional, cognitive, and social changes. 1 Adolescents experience rapid changes in their physical and psychosocial development including pubertal changes and increased demand for independence, self-discovery, and the formation of one’s identity.1,2 Adolescents are more prone to acquiring sexually transmitted infections (STIs) and facing unexpected pregnancies, as a result of various factors, such as behavioral and social aspects.1,3 According to the Centre for Disease Control and Prevention (2021), 26 million new cases of STIs were reported in the year 2018 and almost half of the new STIs cases were among youth (15–24 years). 4 The most common contributing factor to these infections is limited knowledge about sexual health, including how STIs are transmitted and prevented. 5 In addition, adolescents may face barriers in accessing sexual health services, and contraceptive use, including concerns about confidentiality, stigma, lack of awareness about available services, and judgmental attitudes of healthcare professionals.5,6 As a result, they engage in risky sexual behaviors, such as unprotected sex or having multiple sexual partners, which increases their vulnerability to STIs.6,7
Adolescents’ sexual and reproductive health (ASRH) needs and issues are a critical aspect of their overall health and well-being. Evidence reports that adolescents are not equipped with specific sexual and reproductive health (SRH) education.7,8 Therefore, it is imperative to utilize evidence-based innovative and novel approaches to address educational needs among this population. Among the others, comprehensive sexuality education and access to reproductive health services remain a priority for healthy sexual development.1,9 Open and non-judgmental communication, along with the provision of accurate information and accessible services, plays a vital role in supporting adolescents in making informed decisions about their sexual health. Bridging the gap between research and practice ensures that valuable insights and evidence contribute to informed decision-making, policy development, and improvements in professional practices—a process called knowledge translation (KT). 10
KT is particularly crucial in fields where evidence-based decision-making is essential. This process involves developing and employing strategies and tools to integrate research findings into practice. 10 There are several digital KT tools such as mobile phones, websites, mobile apps, short message service (SMS)/text messages, YouTube, Facebook, Twitter, Instagram, WeChat, and other social media platforms that have been identified as useful public health tools, particularly to promote SRH among adolescents.8,9,11,12 Several studies reported the positive use of digital tools in addressing SRH for adolescents; these include: maintaining privacy, anonymity,12–14 and convenience, 15 making it a valuable way to provide accurate information about sexual health to adolescents.6,8,9,16 Other studies reported text messaging through mobile phone technology to increase awareness of adolescents to prevent STIs/HIV and improve safe sexual practices,17–19 and chatbots—a user-friendly digital tool for adolescents to maintain confidentiality of their queries related to topics around sex and sexual activities. 20
Although there is sufficient evidence available on the effectiveness of digital tools in addressing adolescent SRH, there is a lack of synthesis of literature on the available digital or mHealth KT tools. Also, there is a lack of evidence on which digital KT tools prove to be more reliable and effective sources of SRH information for adolescents. Therefore, this review aimed to synthesize current and available evidence on the usefulness of digital KT tools to improve ASRH.
Study aims and objectives: This review aimed to identify, map, and describe existing empirical evidence on the digital KT tools designed to enhance awareness of SRH among adolescents globally. The specific objectives of this evidence gap-map (EGM) are to:
identify, assess, and report on empirical studies that describe the development, implementation, and/or evaluation of adolescent SRH digital KT tools;
identify current uses, purposes, and methods in the development of digital KT tools;
describe the characteristics of digital KT tools studies: such as target population, sample size, age of the participants, sex/gender, and regions
identify research gaps in the literature
Methods
The study is conducted in alignment with standard methodologies for the development of EGM as detailed in our previously published protocol. 21 An EGM is an emerging process that presents visual representations that highlight the existing evidence on a specific subject, illustrating where research has been conducted and where there are gaps in knowledge. 21 This review followed a priori-developed 22 and is registered with PROSPERO (CRD42022373970). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines have been followed to ensure comprehensive and transparent reporting of the research process. 23 We followed the below-mentioned specific eligibility criteria to include studies in the EGM.
Topics of interest: We included studies reported digital KT tools on SRH topics such as knowledge, attitude, and efficacy of SRH, pregnancy and birth, abortion, HIV, AIDS, and other STIs testing and their incidence, sexual and intimate partner violence, sexual behavior, menstrual hygiene, family planning and contraception use, communication and support related to SRH, and access to SRH services.
Population: We included studies conducted on adolescents aged between 10 and 19 years. We also included studies if they included mixed population inclusive of adolescents age group.
Exposure/Intervention: We included studies assessing digital KT tools for disseminating SRH information to adolescents. These KT tools included websites, mobile apps, SMS/text messages, digital pamphlets, brochures, digital storytelling and gaming, podcasts, mass media such as radio messages or videos on television, social media such as Instagram TikTok, Facebook, Twitter, YouTube, and OTT platforms such as Netflix, Prime, YouTube, online films, and videos.
Comparison: We included studies comparing the above-mentioned KT tools with no interventions, the standard of care, or other interventions such as self-directed learning, traditional teaching (lecture), reminders, educational website, and controlled messages.
Setting: We included studies conducted globally regardless of the settings (healthcare organizations, community, educational setting, etc.) or context of its conduct.
Timeframe and language: Studies and reports published from 2010 onward were included in the review to capture current advancements and practices in the field. Due to language limitations of researchers, literature published only in the English language was considered to be included in the review.
Types of studies: We included experimental studies (randomized/cluster randomized and non-randomized controlled trials, including quasi-randomized, controlled before-after, and interrupted time series), and observational studies, that is, including prospective cohort and case-control studies. The experimental and observational studies are only included in the presence of control/comparison arms. Studies with a historical control arm were excluded to focus on contemporary practices. Studies such as cross-sectional studies, case reports, series, editorials, and commentaries were excluded from this review. We included systematic reviews; however, following consistent criteria with the primary studies, systematic reviews with no comparison arm were excluded from this review. None of the scoping reviews was found relevant to be included in this review. Other types of reviews such as narrative reviews were excluded based on inconsistent and incomprehensive search strategies used in those reviews and lack of methodological robustness.
The search strategy for this review is reported in adherence to the PRISMA for Searching (PRISMA-S) extension 24 (Appendix A). The search strategy was developed by an experienced health sciences librarian at the University of Alberta (MK) in consultation with the research team. The following databases were searched individually from inception to present: Medline (1946–present), EMBASE (1974–present), and Global Health (1910–present) via OVID; Cumulative Index to Nursing and Allied Health Literature (CINAHL, 1936–present) via EBSCOhost; Scopus (1976–present); and Cochrane Library (1993–present) via Wiley. The search strategy was derived from four main concepts: (1) adolescents, teenagers, or young adults; (2) SRH or health services including vocabulary related to contraception, family planning, pregnancy, STIs, and gender-based violence; (3) digital communication tools such as websites, online messaging, smartphones, mobile applications, social media, podcasts, television, or digital information; (4) KT including vocabularies such as information dissemination, research innovation, knowledge transfer, implementation science, research into practice, knowledge into practice, and evidence-based practice. Bibliographic databases were searched using a combination of natural language (keywords) and subject headings, such as Medical Subject Headings (MeSH), wherever they are available. Items such as books, book chapters, editorials, conference materials, and opinion pieces were removed from the results and a publication date limit of 2010–present was applied. A preliminary search for OVID Medline was developed and executed in October 2022 to determine the feasibility of this project and test the scope. An updated search was completed in October 2023 for this review. Covidence web-based software was used for the deduplication of database search results and for facilitating the title/abstract screening and full-text screening phases.
All the studies identified from the databases were imported to Covidence (an online screening software), and two independent reviewers completed the first level (title/abstract) (SI, KR) and second-level of screening (full-text) (AH, KR). Disagreements were resolved by consensus among the two reviewers. The reference list of all the included studies was scanned and searched to include any relevant study that may have been missed during searching of databases. For data extraction, we used a standardized data extraction form to extract descriptive data from all studies meeting our inclusion criteria. Data extracted from each study include bibliographic details, KT tool types and descriptions, outcome types and descriptions, study design, context/geographical information, and details on the outcome and quality of the included studies. Two review authors independently extracted the data (SI, AH), and discrepancies were resolved through discussion until consensus was achieved or by consulting a third reviewer (SM) if required. The PRISMA chart was used to document inclusion and exclusion decisions and ensure transparency and rigor in the reporting of the studies (Appendix A).
Data from the review is visually synthesized in an EGM using EPPI-Mapper, a tool developed by the EPPI-Centre at University College London (UCL). The 2D graphical EGM is presented with an accompanying narrative. Rows of the EGM list digital KT strategies and columns components of outcomes and other relevant data coding. Each cell shows the number and quality of evidence for digital KT strategies. We conducted the quality assessment of the included studies using tool ROB2 developed by the Cochrane Collaboration, for randomized control trials (RCTs), ROB1 for quasi-experimental studies, and AMSTAR2 for systematic reviews.25,26 The EGM identified areas with high-quality, evidence-based digital KT tools and areas where few or no KT tools exist (for targeted KT tool development and research/policy prioritization).
Results
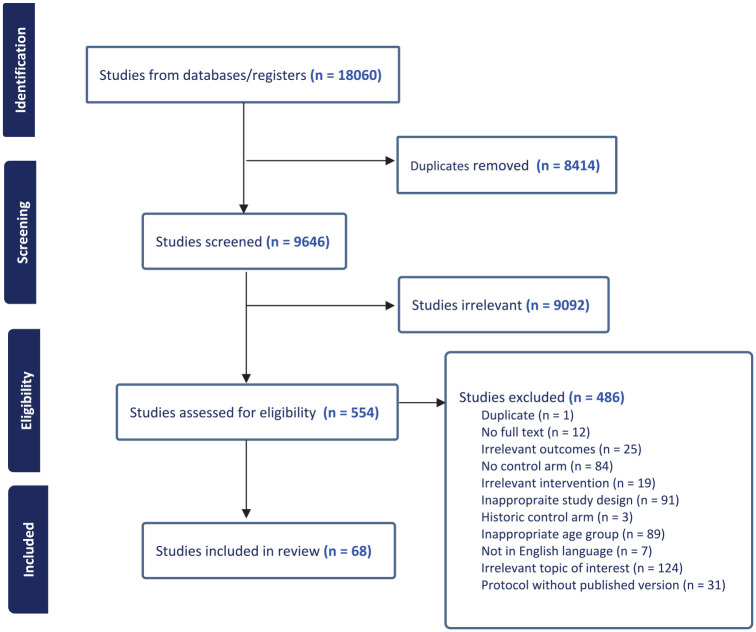
We identified 18,060 studies from electronic databases and finally included 68 studies in the EGM. The PRISMA study flow chart for the study is shown in Appendix A. Out of the 68 included studies, 59 were primary effectiveness studies and 9 were systematic reviews. The majority of primary studies conducted were RCTs (48 studies).27–74 Four studies were clustered RCTs,75–78 seven were quasi-experimental studies,79–85 and nine were review articles.7–9,12,14,16,17,20,86
The majority of the evidence comes from African (19 studies),31,35,36,42–44,48,56,57,61,62,69,70,72,75,80–82,84 and American regions (22 studies).27,29,30,32–34,38,40,45–47,49,50,53,58–60,63–65,74,77 Eight studies were based in European28,37,39,41,51,55,66,76 and eight in Western pacific region,54,67,68,71,73,78,79,83 while only one from Eastern Mediterriean 52 and one from South East Asian region. 85
The evidence base from 59 studies (excluding review articles) was concentrated in 23 countries. The highest evidence comes from African and American regions, with the United States having the highest evidence among other countries (18 studies),27,29,32,33,38,40,45,47,49,50,53,59,60,63–65,74,77, followed by Kenya with 7 studies.42,43,48,56,62,69,84 European region displays a varied range of evidence among countries, with the United Kingdom having the highest (four studies),28,37,66,76 while Western pacific region showcases a mix of low-to-moderate counts across its listed countries, with China having the most evidence (four studies; Figure 1).68,71,73,78 Among nine review studies, six studies focused on a global perspective,9,12,14,16,20,86 while two targeted low and middle-income countries,7,17 and one specifically centered on Sub-Saharan Africa 8 .
Figure 1.
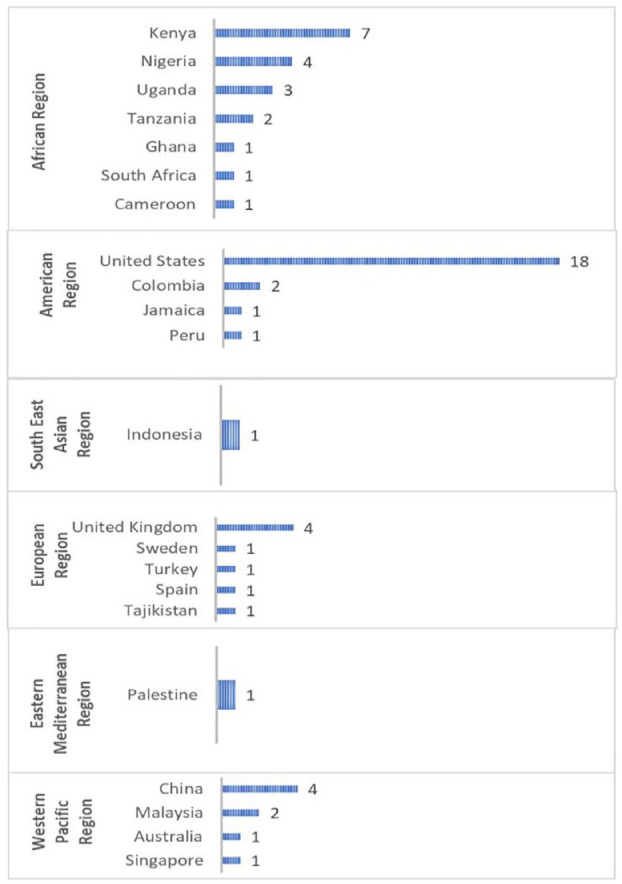
Evidence by region and country.
This EGM is comprised of data from 43,382 participants in 59 primary studies. Sample sizes ranged from 50 to 8999 participants.29,33 Of the 59 primary studies, 22 studies had only female participants,29,31,39–41,43,46,47,49,52,59–61,65,66,70,71,74,75,77,78,84 2 studies only had male participants,38,56 5 studies had males who had sex with male participants (MSM),34,45,53,63,67 and the remaining 30 studies had both male and female participants27,28,30,32,33,35–37,42,44,48,50,51,54,55,57,58,62,64,68,69,72,73,76,79–83,85 (refer to Appendices B and C).
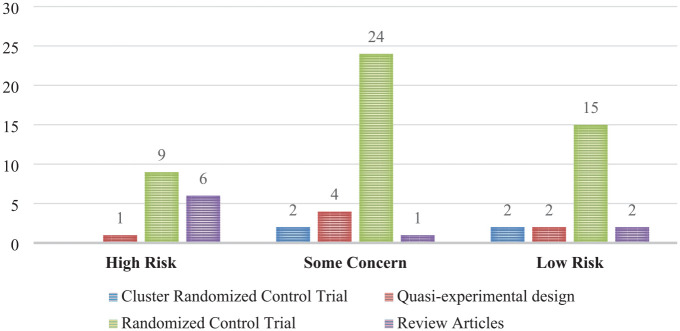
In terms of quality appraisal, the majority of studies included were rated moderate quality with some concerns (31 studies)20,28,30,34,38,39,41–45,47,49,50,53,58,62–64,67,69–73,75,77,79,80,82,85 largely due to inadequate reporting of methodological details. Sixteen studies had low quality with high risks,7,9,12,14,17,27,32,33,35,48,59,65,68,74,81,86 and 21 were of good quality that had a low risk8,16,29,31,36,37,40,46,51,52,54–57,60,61,66,76,78,83,84 (Figure 2).
Figure 2.
Quality appraisal of studies.
A 2D graphical EGM was developed on EPPI-Mapper with a bubble map view consisting of rows and columns. Rows were types of KT tools divided into broad categories like website, mobile app, SMS/text messages, digital technology (pamphlet/brochure/storytelling/gaming), OTT media (Netflix, Prime, YouTube, online film, video), social media (Facebook, Instagram, WhatsApp, TikTok, Snapchat, LinkedIn), mass media (radio and television), and podcast. The columns encompass outcome categories grouped into broader categories, each with subcategories such as adolescent behaviors (sexual behavior, menstrual hygiene, contraception and prevention, communication, and support-seeking), adolescent knowledge, attitude and empowerment (knowledge and awareness, attitudes, self-efficacy), adolescent SRH outcomes (pregnancy and birth, abortion, HIV testing and incidence, sexual and intimate partner violence), and health services (accessing and utilizing services). The quality appraisals are highlighted by color codes: green for low risk of bias/high-quality, yellow for some concerns of bias/moderate quality, and red for high risk of bias/low-quality assessments. More detailed and dynamic versions that enable filtering by each specific subgroup with linked study references and additional study characteristics are available at the link here OR

The EGM examined how different digital mediums affect adolescent SRH outcomes based on available studies. While most of the studies examined individual digital KT tools separately within a specific study, few studies explored the combined effects of multiple tools in a single study. Similarly, in some instances, certain studies reported more than one piece of SRH information. Websites wield significant influence over adolescent behavior, as evidenced by 12 studies,8,16,17,30,39,45,50,65,66,71,74,81 while impacting knowledge, attitude, and self-efficacy in 16 studies.8,16,17,30,33,39,50,53,54,65,66,71,74,78,81,83 However, only four studies have delved into their effects on adolescent SRH outcomes16,50,54,67 and merely two have investigated their impact on health services access and utilization.53,54 Mobile apps have exhibited impacts on adolescent behavior (14 studies),7,17,32,40,49,51,55,62,63,68,69,75,77,82 knowledge, attitude and self-efficacy (13 studies),7,17,32,40,48,49,51,62,68,69,77,82,85 adolescent SRH outcomes (4 studies),32,55,63,82 and healthcare access and utilization (only 1 study). 7 SMS/text messages have emerged as highly influential, affecting adolescent behavior (22 studies),7–9,12,17,20,27–29,37,38,42,43,49,51,52,56,60,70,72,84,86 knowledge, attitude and self-efficacy (16 studies),7,8,12,17,38,42,49,51,52,58,60,61,70,73,79,86 SRH outcomes (13 studies),9,12,28,31,37,38,42,52,60,61,72,84,86 and to some extent, health services access and utilization (4 studies).7,29,38,52 Interventions involving digital technology like digital pamphlets, brochures, storytelling, and gaming have limited research but exhibit an impact on behavior (3 studies),64,80,81 and knowledge and attitude (6 studies),35,44,57,64,80,81 necessitating further exploration in terms of adolescent SRH outcomes and health services utilization.
Areas with less exploration in digital technology include OTT media and social media. There is a moderate amount of research on the influences of OTT media on adolescent behavior (five studies)9,29,46,47,76 and knowledge and attitude (four studies),34,47,57,76 with limited studies on effects on adolescent SRH outcomes (three studies)9,34,76 and healthcare access (two studies).29,59 There are also few studies on the impacts of social media on adolescent behavior (four studies),9,14,27,86 knowledge and attitude (four studies),14,36,41,86 and SRH outcomes (three studies),9,14,86 yet none explore its impact on healthcare access and utilization. Moreover, research on the effects of mass media, such as radio and television, on adolescent SRH behavior (one study), 81 knowledge, attitude and self-efficacy, remains lacking (one study), 81 with no studies focusing on adolescent SRH outcomes and health service access, indicating an unexplored area. Notably, within the outcome category, the EGM revealed that subcategories like menstrual hygiene (one study), 82 abortion (three studies),12,31,52 and sexual and intimate partner violence (two studies)9,42 were less explored (Figure 3 or click here).
Figure 3.
Evidence gap-map.
Discussion
To the best of our knowledge, this is the first comprehensive evidence map focused on digital KT tools for adolescent SRH. The findings substantiate the diverse and impactful role of digital KT tools in shaping adolescent SRH knowledge, attitudes, and behaviors, underscoring their significance in promoting informed decision-making and positive SRH outcomes among adolescents. Websites emerge as essential platforms offering accessible and influential avenues for adolescents seeking SRH information and behavior. These websites serve as easily accessible, user-friendly, and potentially influential mediums, catering to adolescents seeking information regarding their sexual and reproductive well-being. 9 Consistent with prior reviews, these online platforms serve as conduits for disseminating crucial knowledge, shaping attitudes, and potentially modifying behaviors related to SRH.9,16,17 Within the evolving digital landscape, mobile apps have emerged as exemplars of innovation and adaptability in addressing adolescent SRH outcomes. These applications present interactive, captivating, and tailored content, serving as an effective means to engage adolescents. These findings align with the literature highlighting the potential of well-designed, evidence-based mobile apps to deliver customized content and interactive features.6,12
Moreover, the review underscores the profound influence of SMS/text messages as powerful tools in the domain of adolescent SRH. Supported by extensive literature, these text-based interventions play a significant role in shaping adolescents’ understanding and attitudes toward SRH-related knowledge and behaviors.9,17,20 Additionally digital interventions, such as pamphlets, brochures, storytelling, and gaming, exhibit promise in engaging and educating adolescents on SRH matters. Consistent with prior literature, these digital interventions showcase effectiveness in influencing SRH-related knowledge and behaviors among adolescents.33,34,37
Our synthesis of the existing EGM highlights the significant gap in understanding the landscape of available digital KT options and their impact on adolescent SRH information. Despite the increasing prevalence of digital platforms, such as social media, OTT media, and technology-driven interventions like radio/TV and podcasts, 87 their effects on adolescent SRH outcomes remain relatively underexplored. Investigating the influence of these platforms is crucial, as they serve as pervasive sources of information and influence adolescents, shaping their attitudes and behaviors related to SRH. 88 Furthermore, parental consent may affect the accessibility and effectiveness of these digital KT interventions, particularly on sensitive topics. Some families may have reservations about certain SRH subjects, potentially limiting adolescents’ opportunities to seek and obtain critical information, thereby impacting their informed decision-making.
EGM revealed that the outcomes related to abortion, and sexual and intimate partner violence, were least explored. The lack of work in these areas is a concern for several reasons. First, neglecting outcomes related to abortion, and sexual and intimate partner violence overlooks critical components of comprehensive SRH.8,14,89 Second, abortion and intimate partner violence are often stigmatized and surrounded by societal taboo.8,32,52 Digital KT tool options have the potential to provide a more discreet and accessible platform for individuals seeking support in these areas. Neglecting these topics may perpetuate stigma and discourage individuals from seeking help.74,75 By incorporating these dimensions into the discourse, we can enrich our understanding of how digital interventions can comprehensively address the multifaceted aspects of adolescent SRH, fostering more effective strategies for promoting the ASRH.
The EGM further underscores a concerning scarcity of work on menstrual hygiene within the context of digital interventions for adolescent SRH. This lack of focus on menstrual hygiene is problematic due to the reason that menstrual hygiene is an integral component of SRH and rights,8,89 and the omission of KT tools in this area poses a significant gap in our understanding of how digital KT tools can address the unique challenges faced by adolescents in managing menstrual health.
The variation in different numbers of studies in different states in different regions and countries might be due to a high prevalence of SRH issues, the presence of digital technology, and/or the capacity to undertake research in these countries and regions. 90 There is a need to conduct research and introduce digital technology, potentially in all regions and countries, to understand its impact on ASRH. Key considerations for policy, practice, and research are summarized in Table 1 and discussed subsequently.
Table 1.
Key policies, practice, and research considerations.
| 1. Policies should be enacted to encourage and support research initiatives in underrepresented regions (South East and Eastern Mediterranean region) to rectify the current geographical imbalance in understanding the impacts of digital interventions on adolescent health. This would promote a more comprehensive global understanding. |
| 2. Future funding should prioritize the development and implementation of neglected mediums like radio and podcasts, ensuring tailored, culturally sensitive approaches for effective engagement with diverse adolescent populations. |
| 3. We recommend the integration of highly impactful digital mediums such as SMS/text messages, mobile applications, and websites within healthcare systems is necessary to expedite the improvement of adolescent SRH outcomes. |
| 4. The significance of essential areas like menstrual hygiene, abortion, and sexual and intimate partner violence, prioritizing research focused on recognizing and comprehending the influence of digital KT interventions on these crucial aspects should be encouraged. |
| 5. Active promotion and incentivization of international collaborations among researchers and institutions across regions should be undertaken to facilitate knowledge exchange and the sharing of best practices. |
| 6. The sustainability and scaling up of these KT tools in different contexts will not only enhance the impact of digital interventions on adolescent SRH health but also economize research funds. Therefore, there is a critical need to evaluate the scalability of these tools in varied settings to ensure their effective implementation. |
The strength of this study is the methodological rigor with which it was performed, which included an extensive search strategy, a comprehensive summary of the results, and an independent assessment of each stage of the study selection process. Moreover, this review provided a holistic, prescriptive model that can be used to scale up the available KT tools in international contexts, and simultaneously leverage significant economies of scale.
Limitations
Certain limitations of this review warrant acknowledgment. Some articles were excluded for not being written in the English language and no full-text article availability, which may have resulted in studies exploring the impact on a broader range of outcomes being missed. The focus on effectiveness limited our selection to experimental and quasi-experimental studies, omitting cross-sectional, qualitative studies, and gray literature. Further 48% of studies are of moderate-quality evidence. This suggests that findings should be interpreted with caution in light of moderate-quality review evidence.
Conclusion
The EGM has illuminated the multifaceted landscape of research and knowledge gaps surrounding available digital tools for disseminating knowledge in ASRH. This overview has underscored the geographical disparities in digital tool accessibility, their varying impacts on different facets of SRH, research capacities, and essential study characteristics. Furthermore, the analysis has emphasized the dominance of specific interventions while highlighting persistent research voids in exploring diverse digital platforms and less-represented outcome areas globally. It is imperative that future research endeavors focus on broadening the investigation into various digital platforms and expanding the range of measured outcomes to ensure a more comprehensive understanding and advancement in other critical domains of ASRH. By offering policymakers, healthcare providers, and researchers the ability to gauge evidence accessibility and reliability, EGMs serve as invaluable tools in shaping decisions regarding future research funding.
Acknowledgments
We acknowledge the University of Alberta for their institutional support.
Appendix
Appendix A.
PRISMA flow diagram.
Appendix B.
Extraction table for primary studies.
| Sr. no | Author and year | Country | Study design | Target population (age and sex) | Total participants | Purpose | Intervention (Digital KT tool) | Control group | Outcome | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Babalola (2019) 75 | Nigeria | Cluster Randomized control trial |
Sex: Female, Age: 18–35 years | Intervention group (n = 211), control group (n = 344) Total: 565 |
Assess the effects of exposure to the digital tool on contraceptive ideation and use among women of reproductive age | The Smart Client digital health tool delivered via mobile phone | No intervention | • Considerations for desired family size • Perceive self-efficacy for communicating with a family planning provider • Spousal communication about family size • Spousal communication about contraceptive methods • Misinformation rejection that contraceptives can harm the womb • Current modern contraceptive use |
Some concerns |
| 2 | Bourdeau (2021) 27 | United States | Randomized control trial | Sex: Male and female with their families Age: 16–17 years |
Intervention group (n = 206), control group (n = 205) Total: 411 |
Promote healthy decision-making among adolescents and leverage the ongoing impact of parental relationships through older adolescence and young adulthood | Smart Choices 4 Teens, a web-based intervention | No intervention | • Parent-adolescent communication • Birth control • Sex permissive • Health risk • Delaying sex |
High risk |
| 3 | Brown (2018) 28 | United Kingdom | Factorial design Randomized control trial |
Sex: Female and male Age: ⩾16 years |
Intervention group 1 (n = 2421), group 2 (2357), group 3 (n = 2411), control group (n = 2396) Total: 8999 |
Determine whether behaviorally informed SMS primer and reminder messages could increase the return rate of HIV self-sampling kits ordered online | Text message 1. Primer sent 1 day after dispatch plus standard reminders 2. BI reminders (no primer 3. Primer plus BI reminders |
Standard reminders sent days 3 and 7 after dispatch (control) | • The primary outcome: The percentage of kits returned according to intervention combination • Secondary outcomes: HIV self-sampling kit return rates by age, sexual behavior and gender identity, ethnicity, and deprivation |
Some concerns |
| 4 | Chernick (2022) 29 | United States | Pilot Randomized control trial |
Sex: Females Age: 14–19 years |
Intervention group (n = 72), control group (n = 74) Total: 146 |
Assess implementation outcomes and potential efficacy digital health intervention to improve SRH for adolescent females | Multimedia and text messages on patient-centered contraception education | Standard care | • Contraception initiation • Sex in the last 3 months • Consistent condom use • Emergency contraception use • Access the healthcare facility • Intentions toward using birth controls |
Low risk |
| 5 | Chong (2020) 30 | Colombia | Randomized control trial | Sex: Male and female Age: 14–15 years ninth grade students |
Intervention group (n = 46 groups), spillover condition (n = 46 groups), control group (n = 46) Total: 138 groups (4599 participants with an average of 33 students per group) |
To see if using information technology in a classroom will assist teenagers navigate the informational challenges associated with sexual education | An internet-based sexual health course covered | No intervention | • Sex knowledge • Attitude: condom use • Sexual activity and condom demand |
Some concerns |
| 6 | Constant (2014) 31 | South Africa | Randomized control trial | Sex: Female undergoing early medical abortion Age: >18 years (mean age = 25.6 years) |
Intervention group (n = 234), control group (n = 235) Total: 469 |
Evaluate the effect of automated text messages on anxiety emotional discomfort, and to prepare for symptoms among women undergoing medical abortion | Automated text messages | Standard care | • Experience and acceptability of abortion | Low risk |
| 7 | Cordova (2020) 32 | United States | Randomized control trial | Sex: Male and female Age: 13–21 years |
Intervention group (n = 25), control group (n = 25) Total: 50 |
Effects of storytelling on substance use, sexual risk behaviors, and testing for STIs and HIV | Multi-level mobile health app (through storytelling) | Enhanced usual practice | • Clinician-youth risk communication • Substance use prevention knowledge • Sexual risk prevention knowledge • Sexual risk refusal self-efficacy • STIs and HIV testing |
High risk |
| 8 | Cortese (2012) 33 | United States | Randomized control trial | Sex: Male and female Age: Not reported (grade 7–10 students) |
Total: 151 (sample size for control and intervention group not reported separately) | Evaluate the effectiveness of a web-based tailored intervention in increasing knowledge and encouraging deeper elaborations of health messages related to teen sexual health and decision-making | Web-based tailored educational site on teen sexual health | Nontailored educational Web site on the same topic. | • Sexual health knowledge • Decision making (attitude) |
High risk |
| 9 | Del Río-González (2021) 34 | Colombia | Randomized control trial | Sex: Male who have sex with men Age: 18–40 years |
Intervention group (n = 150), control group (n = 150) Total: 300 |
Evaluate the online education-entertainment intervention on HIV knowledge and uptake of HIV testing | Online educational entertainment video | No intervention | • HIV knowledge • HIV testing behavior and intention |
Some concerns |
| 10 | Dike (2021) 35 | Nigeria | Randomized control trial | Sex: Male and female school children Age: 9 years and above |
Intervention group (n = 41), control group (n = 43) Total: 84 |
Effect of educational digital storytelling on knowledge and perception of HIV/AIDS among English language speaking children in rural areas of Nigeria | Educational digital storytelling | No intervention | • Knowledge and perception of HIV/AIDS | High risk |
| 11 | Ezegbe (2018) 36 | Nigeria | Randomized control trial | Sex: Male and female Age: Junior secondary school children (mean age = 14.63 ± 1.23 years) |
Intervention group (n = 40), control group (n = 40) Total: 80 |
Determine the efficacy of a rational emotive digital storytelling therapy on knowledge and perception of risk of HIV/AIDS among schoolchildren in Nigeria | Audiovisual intervention at social media digital storytelling (REDStory) | No intervention | • HIV knowledge and perception | Low risk |
| 12 | Ujang (2018) 79 | Malaysia | Quasi-experimental | Sex: Male and female Age: 18–19 years |
Intervention group (n = 96), control group (n = 121) Total: 217 |
Evaluate the effects of mobile phone messaging in improving SRH among late adolescents | Mobile phone text messages (short SMS) covered sexual reproductive health domain | Health talk | • SRH knowledge • HIV/AIDS knowledge and attitude |
Some concerns |
| 13 | Free (2016) 37 | United Kingdom | Randomized control trial | Sex: Male and female Age: 16–24 years diagnosed with chlamydia or reporting unprotected sex with more than one partner |
Intervention group (n = 99), control group (n = 101) Total: 200 |
To assess safer sex behaviors in young people by text messages | Automated mobile phone messaging (A theory- and evidence-based safer sex intervention) | The control messages contained checking contact detail but no information regarding sexual health | • Behavioral outcome such as treatment compliance, safe sexual practices, and STI testing | Low risk |
| 14 | Gerend (2021) 38 | United States | Randomized control trial | Sex: Male Age: 18–25 years old sexual minority men |
Intervention group (n = 72), control group (n = 76) Total: 148 |
Efficacy of a text messaging-based HPV vaccination intervention for young sexual minority men | Text messages on sexual health program called txt2protect focused on vaccination, with only a brief mention of other sexual health practices (e.g., condom use and HIV testing) | Control condition messages focused on a variety of sexual health practices with only a brief mention of HPV vaccination | • Primary outcomes: Intervention feasibility, acceptability, and preliminary efficacy (i.e., HPV vaccine initiation) • Secondary outcomes: Attitudes and self-efficacy) • Condom use and HIV testing |
Some concerns |
| 15 | Gil-Llario (2014) 39 | Spain | Randomized control trail | Sex: Female Age: Age not reported (mean age = 21.3 years old) |
Total five intervention groups: Intervention 1: Talk (n = 28), Intervention 2: Discussion (n = 31), Intervention 3: Role-play (n = 31), Intervention 4: Fear (n = 33), Intervention 5: Web (n = 23), control = 21) Total: 167 |
Examine the differential effectiveness of six intervention elements on HIV prevention | Informative website: Intervention 1: Informative talk on HIV knowledge Intervention 2: Attitudinal discussion and debate about HIV/AIDS topic Intervention 3: Role-play on risky sexual situations Intervention 4: Fear induction, that is, showing fear-inducing images and videos Intervention 5: Informative website |
No intervention | • Knowledge, attitude and self-efficacy • Confidence in condom use • Sexual acts • Perceived fear • Sexual behavior |
Some concerns |
| 16 | Gilliam (2014) 40 | United States | Randomized control trial | Sex: Female Age: 15–29 years | Intervention group (n = 28), control group (n = 24) Total: 52 |
Evaluate the app’s impact on contraceptive knowledge, LARC interest, and selection of a LARC method | Tablet computer programmed with the app on IUD or implants | Standard care | • knowledge of contraceptive • Interest and interest, and selection of a LARC method |
Low concern |
| 17 | Gonenc (2021) 41 | Turkey | Randomized controlled trial | Sex: Female (midwifery students) Age: Age not reported (mean age = 19.24 ± 1.140 years) |
Intervention 1: WhatsApp education group (n = 32), Intervention 2: Convention education group (n = 35), control group (n = 31) Total: 98 |
Evaluate the effects of sexual education via WhatsApp and the conventional method on the level of sexual knowledge and sexual myths in midwifery students | Intervention 1: Online education via WhatsApp group Intervention 2: Conventional education (face to face) |
No intervention | • Sexual health knowledge test, and sexual myths | Some concerns |
| 18 | Gonsalves (2019) 42 | Kenya | Randomized controlled trial | Sex: Male and female Age: 18–24 years |
Intervention 1: (n = 203), Intervention 2: (n = 221), control (n = 236) Total: 660 |
Evaluate the effect of the ARMADILLO intervention on SRH-related outcomes | ARMADILLO text messages Intervention 1: One SMS text message Intervention 2: Two pushed messages per week |
Usual care | • Primary outcome: Change in myths and misconceptions related to contraception • Secondary outcomes: Change in knowledge, attitudes, and behavior for key SRH outcomes (e.g., knowledge of HIV/AIDS and its transmission, attitudes around violence against women, engagement in sexual activity) |
Some concerns |
| 19 | Green (2018) 43 | Kenya | Randomized control trial | Sex: Female Age: 15–49 years |
Intervention (n = 56), control (n = 56) Total: 112 | Examine the effect of the digital health intervention on contraception uptake | Automated investigational digital health tool (SMS text message) to try the service and complete a free family planning screening (plus bonus) | Message for thanking them for participating in the study only | • Self-reported use of modern contraception | Some concerns |
| 20 | Haruna (2018) 44 | Tanzania | Randomized control trial | Sex: Male and female Age: 11–15 years |
Intervention 1: Gamified instruction, (n = 40), Intervention 2: Gamification (n = 40), control (n = 40) Total: 120 |
Investigates the extent to which GBL and gamification could improve the sexual health education of adolescent students | Intervention 1: GBL Intervention 2: Gamification |
Traditional teaching (lecture) | • MAKE • Sexual health behavior |
Some concerns |
| 21 | Haruna (2021) 80 | Tanzania | Quasi-experimental | Sex: Male and female Age: 11–15 years in secondary school |
Intervention 1: Gamified instruction (n = 40), Intervention 2: Gamification (n = 40), control (n = 40) Total: 120 |
Improve sexual health knowledge and understanding of the problems associated with unhealthy sexual practices and address SRH challenges experienced in a low-tech setting. | Intervention 1: Gamified instruction (actual serious games in teaching); Intervention 2: Gamification (making nongame’s, such as game-like learning) | Traditional teaching class | • Motivation, attitude, know-how, and participation in learning | Some concerns |
| 22 | Horvath (2017) 45 | United States | Randomized control trial | Sex: Gay and bisexual male Age: 15–24 years |
Intervention (n = 84), control (n = 43) Total: 130 | Assessed whether young men who have sex with men’s accept online Get Connected! intervention and impact on subsequent sexual health decision-making | Website-based intervention (online Go connected!) | No intervention | • Intervention system quality scores, sexual health decision-making | Some concerns |
| 23. | Hylton-Kong (2021) 46 | Jamaica | Randomized control trial | Sex: Female Age: 18–25 years |
Intervention (n = 110), control (n = 110) Total: 220 |
To evaluate video effectiveness on perceived contraceptive safety | LARC-based videos | Intervention to control mosquitoes | • Perceived contraceptive safety | Low risk |
| 24 | Lohan (2018) 76 | United Kingdom | Clustered Randomized control trial |
Sex: Male and female Age: 14–16 years |
Intervention (n = 420), control (411) Total: 831 |
Evaluate an interactive film-based intervention to reduce teenage pregnancy and promote positive sexual health | Interactive film “If I Were Jack” | No intervention | Primary outcome: • Unintended teenage pregnancy rates • Avoidance of unprotected sex via consistent use of contraception Secondary outcomes: • Knowledge, attitudes, skills and intentions relating to avoiding teenage pregnancy |
Low risk |
| 25 | Jones (2013) 47 | United States | Randomized control trial | Sex: Female Age: 18–29 years |
Intervention (n = 117), control (n = 121) Total: 238 |
To reduce risk of sexually transmitted HIV in young urban African American women | Video series (soap opera) on love, sex, and choices | HIV prevention text messages | • Changes in unprotected sex (sexual behavior and contraception use) • Knowledge, attitude, and self-efficacy |
Some concerns |
| 26 | Macharia (2022) 48 | Kenya | Randomized control trial | Sex: Male and female Age: 15–19 years |
Intervention (n = 146), control (n = 154) Total: 300 |
Investigate the impact of an USSD-based app in increasing adolescents’ knowledge about contraceptives, gender-based stereotypes, STIs, abstinence, and perceived vulnerability, and helping adolescents make informed decisions about their SRH | Mobile phone-based health intervention: USSD-based app | No intervention | Primary outcome: • SRH knowledge and attitude Secondary outcome: • Decision-making on SRH. |
High risk |
| 27 | Manlove (2021) 49 | United States | Randomized control trial | Sex: Female Age: 18–20 years |
Intervention (n = 146), control (n = 154) Total: 1588 |
Evaluate pulse, an app-based pregnancy prevention program implemented with women aged 18–20, a population with high rates of unplanned pregnancy | App-based sexual health program (pulse) | General health control app | • Sexual intercourse without using modern contraception • Contraceptive knowledge |
Some concerns |
| 28 | Marsch (2015) 50 | United States | Randomized control trial | Sex: Male and female Age: 12–18 years |
Intervention (n = 69), control (n = 72) Total: 141 |
Evaluate changes in knowledge about HIV, hepatitis, and STIs, intentions to engage in safer sex, sex-related risk behavior, self-efficacy to use condoms, and condom use skills | Web-based TES intervention | Traditional education | • Knowledge about HIV, hepatitis, and STIs, intentions to engage in safer sex, sex-related risk behavior, self-efficacy to use condoms, and condom use skills | Some concerns |
| 29 | McCarthy (2018) 51 | Tajikistan | Randomised control trial | Sex: Male and female Age: 16–24 years |
Intervention (n = 275), control (n = 298) Total: 537 |
Assess the effect of the intervention (instant messages) on the acceptability of effective contraceptive methods among young people in Tajikistan | Instant messages about contraception through the app. (access to an app plus intervention messages) | Access to the app plus control messages | • Use of effective contraception, service uptake, knowledge, attitude, perceived norms, personal agency, and intention to use effective contraception | Low risk |
| 30 | McCarthy (2019) 52 | Palestine | Randomised control trial | Sex: Female Age: 18–24 years |
Intervention (n = 229), control (n = 235) Total: 464 |
Assess the impact of mobile text message on attitudes toward the non-permanent effective contraceptive methods available in Palestine | Mobile text message (three messages per day) | Mobile text message (60 messages over 120 days) | Primary outcome: • Acceptability of at least one method of effective contraception Secondary outcome: • Effective contraception use acceptability of individual methods, service uptake, unintended pregnancy, and abortion Other outcomes: Knowledge, attitude, perceived norms, personal agency, and intention |
Low risk |
| 31 | McRee (2018) 53 | United States | Randomised control trial | Sex: Gay and bisexual men Age: 18–25 years not received HPV vaccine |
Intervention (n = 68), control (n = 73) Total: 150 |
Pilot test a web-based, Outsmart HPV intervention, to promote HPV vaccination among YGBM | Web-based intervention (individually tailored content called Outsmart HPV intervention) | Standard HPV vaccination information | • HPV vaccination attitudes, beliefs, and intentions | Some concerns |
| 32 | Mortimer (2015) 54 | Australia | Randomised control trial | Sex: Male and female Age: 18–29 years |
Intervention (n = 369), control (n = 378) Total: 747 |
Determine if a web-based PCHMS could increase the uptake of STI screening among a young university population | Web-based Healthy.me (PCHMS) | Redirected to a static webpage informing them of their allocation | • Self-reported being tested for STIs, accessing healthcare facility, attitudes, and intentions toward accessing healthcare services for STI screening | Low risk |
| 33 | Musiimenta (2012) 81 | Uganda | Quasi-experimental Pre post intervention |
Sex: Male and female Age: 11–16 years |
Intervention (n = 180), control (n = 218) Total: 398 |
Determine the effect of WSWM intervention on students’ sexual behaviors, HIV/AIDS knowledge, attitudes, and self-efficacy | Computer-based HIV/AIDS Education that includes websites, television, and printouts | No intervention | • HIV/AIDS knowledge, attitudes self-efficacy, sexual behavior, and condom use. | High risk |
| 34 | Nalwanga (2021) 82 | Uganda | Quasi-experimental | Sex: Male and female Age: 18–30 years |
Intervention (n = 556), control (n = 556) Total: 1112 |
Assess the utilization of a MPA to increase access to SRH information, goods, and services among university students in Uganda | MPA | No intervention | • Awareness and utilization of MPA regarding use of contraception, sanitary pads, HIV testing | Some concerns |
| 35 | Nielsen (2021) 55 | Sweden | Randomized control trial | Sex: Male and female Age: 18–23 years |
Intervention (n = 214), control (n = 219) Total: 433 |
Evaluate the effectiveness of a MPA to improve sexual health among youth of Stockholm County in addition to routine care | Smartphone app to promote safe sex among youth called “Skyddslaget” (“protection team”) | A “dumdum” application and routine care | Primary outcome: • Self-reported condom use Secondary outcome: • Self-reported number of partners, occurrence of STIs, pregnancy, and STI tests |
Low risk |
| 36 | Nik (2018) 83 | Malaysia | Quasi-experimental Pre and post-test design |
Sex: Male and female Age: 12 years |
Intervention (n = 101), control (n = 108) Total: 209 |
Identify the potential of an internet-based program to improve SRH knowledge among Malaysian young people | Online internet-based SRH education | Face to face information | • Adolescents’ knowledge of SRH | Low risk |
| 37 | Njuguna (2016) 84 | Kenya | Quasi-experimental | Sex: Female Age: 18–24 years | Intervention (n = 300), control (n = 300) Total: 600 |
Determine the effect of an SMS intervention on uptake of HIV testing among female Kenyan college students | SMS text on HIV sensitization messages weekly | Weekly control surveys | • Sexual behavior and HIV testing | Low risk |
| 38 | Odeny (2014) 56 | Kenya | Randomized control trial | Sex: Male Age: older than 18 years (74.6% between 18 and 30 years) |
Intervention (n = 600), control (n = 600) Total: 1200 |
Determine the effect of text messaging to deter resumption of sex before 42 days post circumcision | A series of text messages | Standard care | • Frequency of self-reported resumption of sexual activity | Low risk |
| 39 | Ofoegbu (2020) 57 | Nigeria | Randomized control trial | Sex: Male and female Age: Adolescent (mean age = 20.43 ± 0.89 years) |
Intervention (n = 49), control (n = 49) Total: 98 |
Investigate the impact of an EDSI on HIV risk perception and knowledge among Nigerian adolescents | EDSI | No intervention | • HIV risk perception and knowledge | Low risk |
| 40 | Perez-Lu (2022) 58 | Peru | Randomized control trial | Sex: Male and female Age: 13–17 years |
Intervention 1 (n = 236), Intervention 2 (n = 237), control (n = 239) Total: 712 |
To determine whether adolescents able to access SRH information on-demand and via SMS are better able to reject contraception-related myths and misconceptions as compared with adolescents receiving pushed SMS or usual care | Intervention 1: Access to ARMADILLO SMS information on-demand Intervention 2: Access to ARMADILLO SMS information pushed to their phone |
No Intervention | • SRH knowledge and contraception-related myths | Some concerns |
| 41 | Riese (2019) 59 | United States | Pilot Randomized control trial |
Sex: Female Age: 14–16 years |
Intervention (n = 35), control (n = 31) Total: 66 |
Evaluate the acceptability and feasibility of an electronic sexual health module for inpatient adolescent girls their uptake of sexual health services | Electronic sexual health module included a sexual health assessment, tailored feedback, and a questionnaire to request sexual health services | Electronic sexual health module included a sexual health assessment but no tailored feedback | • Acceptability and feasibility of intervention • Uptake of sexual health services |
High concern |
| 42 | Rinehart (2020) 60 | United States | Randomized control trial | Sex: Females Age: 13–18 years |
Intervention (n = 122), control (n = 122) Total: 244 |
Evaluate the feasibility, acceptability, and initial efficacy of a pilot texting intervention (“t4she”) to increase sexual health knowledge and promote protection strategies to reduce unintended pregnancies and STIs | Text messages for Sexual Health Education and Empowerment (t4she) | Standard care | • Knowledge, condom use, and sexual behaviors | Low risk |
| 43 | Rokicki (2017) 61 | Ghana | Randomized control trial | Sex: Female Age: 14–24 years |
Intervention (n = 205), control (n = 293) Total: 498 |
Assess the degree to which mHealth programs reach target adolescents who may be at higher risk of poor SRH outcomes | Text messages about SRH (mHealth intervention) | Placebo message | • Engagement with the mHealth program, SRH knowledge, and self-reported pregnancy | Low risk |
| 44 | Sabben (2019) 62 | Kenya | Randomized control trial | Sex: Male and female Age: 15–24 years |
Intervention (n = 30), control (n = 30) Total: 60 |
To help prevent HIV among young Africans by delaying first sex and increasing condom use at first sex | Narrative-based smartphone game app (Tumaini) | No intervention | • Acceptability of the game • Sexual behavior and knowledge • Communication with parents |
Some concerns |
| 45 | Schnall (2020) 63 | United States | Randomized control trial | Sex: Male who report same sex attractions (YMSM) Age: 13–18 years |
Total: 350 | Evaluate the efficacy of MyPEEPS, an evidence-based intervention for reducing reduce sexual risk behaviors and strengthen protective factors among racially and ethnically diverse YMSM | MyPEEPS mobile | Delayed intervention | • HIV prevention self-efficacy, HIV testing, condomless sexual acts, and HIV prevention measures | Some concerns |
| 46 | Shegog (2014) 64 | United States | Randomized, two-arm nested design | Sex: Male and female Age: 8th grade students, 12–14 years |
Intervention (n = 768), control (n = 606) Total: 1374 |
Assess impact of IYG-Tech on psychosocial factors related to sexual behavior-perceptions of friends’ beliefs, reasons for not having sex, condom use self-efficacy, abstinence intentions, negotiating with others to protect personal rules, and improved knowledge about what constitutes healthy relationships | Computer-based sexual health program: t’s Your Game-Tech (IYG-Tech) | State-approved health education usually from a textbook, without any exposure to a structured health education program | • Sexual behavior including and condom use efficacy (1) delayed initiation of specific types of sexual activity; (2) number of lifetime sexual partners; (3) current sexual activity; (4) number of occasions students had sex without a condom; (5) number of partners in the past 3 months; (6) number of partners without a condom in the past 3 months; and (7) use of a condom during last sex | Some concerns |
| 47 | Starosta (2016) 65 | United States | Randomized control trial | Sex: Female Age: 17–41 years |
Intervention (n = 215), control (n = 207) Total: 422 |
To increase condom, use among college women through web-based intervention | Web-based motivational enhancement intervention | Binge drinking | • Intentions to use and attitudes toward condoms | High risk |
| 48 | Stephenson (2020) 66 | United Kingdom | Randomized control trial | Sex: Female Age: 15–20 years |
Intervention (n = 464), control (n = 463) Total: 927 |
To increase the uptake of LARC methods in young women | An interactive website | Standard care | • Knowledge and use of LARC and satisfaction with contraceptive method | Low risk |
| 49 | Tan (2022) 67 | Singapore | Pragmatic, randomized controlled trial | Sex: Gay, bisexual, and other men who have sex with men HIV negative (GBMSM) Age: 18–29 years |
Intervention (n = 150), control (n = 150) Total: 300 |
Evaluate the effectiveness of a popular web drama video series developed by a community-based organization in Singapore for GBMSM on HIV and other STI testing behaviors | Web-based drama video series | Standard care | • Self-reported regular testing and participants’ intentions to test for HIV and chlamydia or gonorrhea | Some concerns |
| 50 | Tang (2022) 68 | China | Randomized controlled trial | Sex: Male and female Age: 15–24 years |
Intervention (n = 50), control (n = 46) Total: 96 |
Evaluate the effect of AIDS fighter health defense on young students in improving AIDS-related knowledge, stigma, and attitude related to high-risk behaviors in Southwest China | AIDS educational mobile game AIDS Fighter · Health Defense | AIDS-related knowledge through independent learning on the QQ chat group | • Knowledge awareness rate, stigma score, attitudes of high-risk AIDS behaviors | High risk |
| 51. | Tebb (2021) 77 | United States | Cluster Randomized controlled trial |
Sex: Female Age: 14–18 years |
Intervention (n = 693), control (n = 667) Total: 1360 |
Evaluate the effectiveness of Health-E You/Salud iTu, a mobile health application (app), on knowledge, self-efficacy, and contraception use among Latina adolescents, its impact on visit, quality, and satisfaction | Health-E You/Salud iTu: an mHealth application of patient-centered contraceptive decision-making support | Provided questions to answer about sexual health on iPads | • Knowledge, self-efficacy, and contraceptive use • App satisfaction |
Some concerns |
| 52 | Turah (2019) 85 | Indonesia | Quasi-experimental pre and post test | Sex: Male and female Age: 15–19 years |
Intervention (n = 53), control (n = 53) Total: 106 |
Determine the effect of health education using an android application namely Gapin on adolescent knowledge and attitudes about premarital sex | Gapin intervention an android application | No intervention | • Knowledge and attitudes toward premarital sex | Some concerns |
| 53 | Widman (2018) 74 | United States | Randomized controlled trial | Sex: Females Age: 14–17 years |
Intervention (n = 107), control (n = 115) Total: 222 |
Assess the feasibility and acceptability of HEART | HEART, a web-based intervention focused on developing sexual assertiveness skills and enhancing sexual decision-making | Controlled web program focused on cultivating academic growth mindsets | • Self-reported assertiveness, intentions to communicate about sexual health, knowledge regarding HIV and other STDs, safer sex norms and attitudes, and condom self-efficacy | High risk |
| 54 | Winskell (2018) 69 | Kenya | Randomised control trail | Sex: Male and female Age: 11–14 years |
Intervention (n = 30), control (n = 30) Total: 60 |
Pilot test a theory-based, empirically grounded smartphone game for young Kenyans to increase condom use at first sex | Android smartphone game (Tumaini) | No intervention | • Sexual health-related knowledge, self-efficacy, behavioral intention for risk-avoidance strategies, sexual risk communication | Some concerns |
| 55 | Wirsiy (2022) 70 | Cameroon | Randomized controlled trail | Sex: Female Age: 10–19 years |
Intervention (n = 230), control (n = 230) Total: 460 |
Improve perception of adolescent girls on sexo-reproductive health in Cameroon | MASHS | Usual care | • Knowledge, attitude, and practice about sexo-reproductive health | Some concerns |
| 56 | Wong (2021) 71 | China | Randomized controlled trail | Sex: Female university students Age: ⩾18 years |
Intervention (n=384), control (n=397) Total:781 |
Development and systematic evaluation of a web-based sexual health literacy intervention called “Smart Girlfriend” for female Chinese university students | Web-based sexual health literacy intervention: The Smart Girlfriend was based on the Dating CAFE initiative | No intervention | • Self-reported consistency of condom use, appraisal of the knowledge, attitudes, norms, and self-efficacy of condom use | Some concerns |
| 57 | Ybarra (2021) 72 | Uganda | Randomized controlled trial | Sex: Male and female Age: 18–22 years |
Intervention (n = 101), control (n = 101) Total: 202 |
Examine the impact of an internet-based HIV prevention program on Information-Motivation-Behavior Skills | A text messaging-based HIV prevention program: InThistoGether (ITG) | Text message focused on general health | Behavior change: Frequency of unprotected sex acts; sustained sexual abstinence, and HIV testing rates | Some concerns |
| 58 | Zha (2021) 73 | China | Randomized controlled trail | Sex: Male and female Age: College students >18 years (age not reported) |
Intervention (n = 56), control (n = 55) Total:111 |
Evaluate a WeChat-based HIV and AIDS educational intervention to enhance knowledge, improve attitudes, and reduce stigma among college students in China | WeChat-based HIV and AIDS educational intervention | No intervention | • HIV- and AIDS-related knowledge, attitudes, and stigma | Some concerns |
| 59 | Zhang (2022) 78 | China | Cluster randomized controlled trial | Sex: Female Age: Not reported (mean age = 18.99 years) |
Intervention (n = 532), control (n = 414) Total:946 |
Investigate the effect of a web-based educational intervention on changing female college students’ willingness and uptake of HPV vaccines and its factors | Web-based health education regarding HPV and HPV vaccines | Health tips unrelated to HPV vaccination or prevention | • Awareness, knowledge, and willingness to be vaccinated against HPV | Low risk |
BI, behavioural insights; EDSI, educational digital storytelling intervention; GBL, game-based learning; HEART, Health Education and Relationship Training; HIV, human immunodeficiency virus; HPV, human papillomavirus; LARC, long-acting reversible contraception; MAKE, Motivation, Attitude, Knowledge, and Engagement; MASHS, Mobile-based adolescent sexo-reproductive health scheme; MPA, Mobile phone application; PCHMS, personally controlled health management system; SMS, short message service; SRH, sexual and reproductive health; STD, sexually transmitted disease; STI, sexually transmitted infection; TES, therapeutic education system; USSD, Unstructured Supplementary Service Data; WSWM, World Starts With Me; YGBM, Young Gay and Bisexual Men.
Appendix C.
Extraction table for review studies.
| Sr. no | Author and year | Objective/aim/purpose | Country/setting | Target population | Total number of studies | Study design | KT tool | Intervention | Outcomes | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Martin (2020) 9 | To describe existing published studies on online participatory intervention methods used to promote the sexual health of adolescents and young adults | Global | Adolescents and young adults aged between 10 and 24 years | n = 60 | Systematic review | Facebook, YouTube, MySpace, Twitter, Flickr, Tumblr, Instagram, WeChat | • Information dissemination with participatory components (games, quizzes, discussions) • Online community/discussion • Participation in activities only (including games) • Participatory educational sessions • Personalized assistance |
• Sexual health promotion • HIV/sexually transmitted infection prevention specifically • Sexual violence prevention • Hepatitis B virus and hepatitis C virus testing promotion • Improve HIV care linkage • Observe peer influence in sexual situations only |
High risk |
| 2 | Feroz (2021) 7 | To identify a range of different mHealth solutions that can be used for improving young people SRH in LMICs and highlight facilitators and barriers for adopting mHealth interventions designed to target SRH of young people | LMICs | Young people (adolescents and youth) aged 10–24 years | n = 15) | Systematic review | Mobile phones | The most reported use of mHealth was for client education and behavior change communication followed by financial transactions and incentives | • Access to SRH services • Behavior change communication • SRH outcomes • Factors facilitating and impeding uptake of mHealth interventions for young people SRH |
High risk |
| 3 | Onukwugha (2022) 8 | To describe mHealth intervention components, assesses their effectiveness, acceptability, and cost in improving adolescent’s uptake of SRH services in SSA | SSA | Adolescents aged 10–19 years and young people aged 10–24 years | n = 10 | Systematic review | • SMS An interactive web-based peer support platform |
The interventions focused on shaping knowledge and increasing the use of reproductive health interventions or services. Two studies evaluated SRH knowledge,29,35 four assessed contraceptive use/birth control,29,33,34,39 three examined pregnancy and fertility intentions.29,33,34 One focused on facility childbirth delivery, 33 two on EBF,33,34 four on HIV ART adherence,31,32,37,38 and two on sexual behavior29,34 | • SRH knowledge • Sexual health behavior. • Contraceptive/birth control access and use • ART adherence |
Low risk |
| 4 | Guse (2012) 14 | To summarize the currently published evidence-based on the effectiveness of new digital media-based sexual health interventions for adolescents aged 13–24 years | Global | Adolescents aged 13–24 years | n = 10 | Systematic review | Internet | The shortest program was a single e-mail and the longest consisted of 24 45-min sessions administered over 2 years. Two of the interventions were delivered to adolescents in rural settings. Two of the interventions enrolled HIV-positive youth, and one enrolled youth with substance use disorders | • Youth behaviors, including initiation of vaginal sex recent sexual intercourse, frequency of sex, number of sexual partners, condom use, and sex while under the influence of drugs or alcohol • Adherence to medication. among young HIV-positive participants and alterations to public profiles on an SNS • Attitudes, self-efficacy, and intentions regarding sexual abstinence • Knowledge-based outcomes pertaining to HIV/ STIs, condoms, pregnancy, and emergency contraception |
High risk |
| 5 | Saragih (2021) 16 | To explore the meta-effects of telehealth interventions on self-efficacy of using condoms, condom use practices, and sexually transmitted infection testing behaviors among adolescents | Global | Adolescent population aged 13–24 years old | n = 15 | Systematic review and meta-analysis of randomized controlled studies | Web-based and game-based interventions | The telehealth interventions were designed to influence knowledge, attitudes, norms, self-efficacy, and behaviors; a range of sexual health and general health topics were addressed, including substance use, safer sex strategies, sexual risk behaviors, and risk-reducing behaviors including condom use, STI testing practices, and contraceptive options. A variety of professionals delivered the telehealth interventions, including clinicians (n = 3), a school nurse (n = 1), researchers in tropical medicine (n = 2 studies), a public health researcher (n = 1 study), a social worker (n = 1 study), and psychologists (n = 4 studies). The frequency of intervention delivery was most often weekly, with each session lasting 20–45 min, and the sessions occurring over a 3-week to 6-month period of time | • Knowledge, attitude, self-efficacy for condom use, and sexual behavior • Being screened/tested for sexual transmitted infections |
Low risk |
| 6 | Nwaozuru (2021) 17 | To summarize what is known, and what we need to know about implementing mhealth interventions for HIV/STI prevention targeting young people in LMICs | LMICs | Young people aged 10–24 years | n = 11 | Systematic review and meta-analyses | Mobile phones, SMS | The mHealth components across the six interventions were delivered using three modalities: (1) as mobile applications, (2) as phone-based SMSs, and (3) as web-based application. Specifically, two interventions used mobile phone applications to provide HIV/STI prevention services and information. One of the interventions was delivered as a narrative-based game for android smartphones 33 and one used WeChat—a messaging mobile application | • Acceptability, appropriateness, and feasibility • Condom use and sexual and reproductive health knowledge. • Sexual intercourse after male circumcision |
High risk |
| 7 | Handschuh (2019) 20 | To synthesize research examining the association between adolescent sexing and sexual activity | Global | Adolescents 10–19 years of age | n = 6 | Systematic review and meta-analysis | Mobile phones, SMS | Sexting as sending either a written message or an image, one differentiated between sending a message and sending an image | • Sexual behavior | Some concerns |
| 8 | Jones (2014) 86 | To examine the effectiveness of social media and text messaging interventions designed to increase STD knowledge, increase screening/testing, decrease risky sexual behaviors, and reduce the incidence of STDs among young adults aged 15 through 24 years | Global | Young adults 15–24 years | n = 11 | Systematic review | SMS messaging and e-mail communications | Intervention modes included SMS messaging via text, e-mail communications, and internet-based health education programming | • STD knowledge: Significant increases in STD knowledge, including increased understanding of sexual protection methods and transmission • STD screening/testing • Increases in STD testing among participants after the intervention • Sexual risk behavior: Sexual risk behaviors were examined in 10 studies • Self-efficacy/intention • Significant increases in condom use self-efficacy and intention |
High risk |
| 9 | L’Engle (2016) 12 | To assess strategies, findings, and quality of evidence on using mobile phones to improve ASRH by using the mERA checklist recently published by the World Health Organization mHealth Technical Evidence Review | Global | Adolescents aged 10–24 years | n = 35 | Systematic review | Mobile phones | mHealth intervention programs where mobile phones were used to address ASRH | • Knowledge and STI testing • Increased sexual health knowledge and awareness, lower rates of unprotected sex and higher rates of condom use, and greater STI testing • Adolescents commonly asked about sexual acts and practices, physical and sexual development, abortion, and contraception and unplanned pregnancy. Confidentiality: Adolescents y liked the confidentiality of mobile phone communication and found the SRH content simple to understand, informative, and easily shared • HPV vaccine: Increased HPV vaccination through vaccination reminders sent via SMS to parents or teens |
High-risk |
ART, antiretroviral therapy; ASRH, adolescent sexual and reproductive health; EBF, exclusive breastfeeding; HPV, human papillomavirus; LMIC, low- and middle-income country; mERA, mHealth Evidence Reporting and Assessment; SMS, short message service; SNS, Social Networking Site; SRH, sexual and reproductive health; SSA, Sub-Saharan Africa; STD, sexually transmitted disease; STI, sexually transmitted infection.
Footnotes
ORCID iDs: Amber Hussain  https://orcid.org/0000-0003-0353-1117
https://orcid.org/0000-0003-0353-1117
Komal Abdul Rahim  https://orcid.org/0000-0002-0790-6644
https://orcid.org/0000-0002-0790-6644
Contributor Information
Salima Meherali, University of Alberta, Edmonton, AB, Canada.
Amber Hussain, Edmonton Clinic Health, Faculty of Nursing, University of Alberta,11405 87 Ave NW, Edmonton, Alberta, Canada T6G 1C9.
Komal Abdul Rahim, Aga Khan University, Karachi, Sindh, Pakistan.
Sobia Idrees, University of Alberta, Edmonton, AB, Canada.
Soumyadeep Bhaumik, The George Institute for Global Health, Newtown, NSW, Australia.
Megan Kennedy, University of Alberta, Edmonton, AB, Canada.
Zohra S. Lassi, University of Adelaide, Adelaide, SA, Australia
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Salima Meherali: Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Resources; Software; Supervision; Validation; Writing – original draft; Writing – review & editing.
Amber Hussain: Data curation; Formal analysis; Methodology; Project administration; Resources; Software; Visualization; Writing – original draft; Writing – review & editing.
Komal Abdul Rahim: Data curation; Formal analysis; Investigation; Methodology; Project administration; Software; Writing – review & editing.
Sobia Idrees: Data curation; Methodology; Project administration; Software; Writing – original draft; Writing – review & editing.
Soumyadeep Bhaumik: Investigation; Methodology; Validation; Writing – review & editing.
Megan Kennedy: Data curation; Methodology; Resources; Software; Writing – review & editing.
Zohra S. Lassi: Conceptualization; Formal analysis; Methodology; Project administration; Resources; Supervision; Validation; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Competing interests: The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. World Health Organization. Adolescents health, https://www.who.int/health-topics/adolescent-health/#tab=tab_1 (n.d., accessed 18 December 2023).
- 2. Kuzma EK, Peters RM. Adolescent vulnerability, sexual health, and the NP’s role in health advocacy. J Am Assoc Nurse Pract 2016; 28(7): 353–361. [DOI] [PubMed] [Google Scholar]
- 3. Hensel DJ, Nance J, Fortenberry JD. The association between sexual health and physical, mental, and social health in adolescent women. J Adolesc Health 2016; 59(4): 416–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Adolescents and school health, https://www.cdc.gov/healthyyouth/sexualbehaviors/index.htm (2019, accessed 18 December 2023).
- 5. Leichliter JS, Copen C, Dittus PJ. Confidentiality issues and use of sexually transmitted disease services among sexually experienced persons aged 15–25 years—United States, 2013–2015. MMWR Morb Mortal Wkly Rep 2017; 66(9): 237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Meherali S, Salami B, Okeke-Ihejirika P, et al. Barriers to and facilitators of South Asian immigrant adolescents’ access to sexual and reproductive health services in Canada: a qualitative study. Can J Hum Sex 2021; 30(3): 329–338. [Google Scholar]
- 7. Feroz AS, Ali NA, Khoja A, et al. Using mobile phones to improve young people sexual and reproductive health in low and middle-income countries: a systematic review to identify barriers, facilitators, and range of mHealth solutions. Reprod Health 2021; 18(1): 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Onukwugha FI, Smith L, Kaseje D, et al. The effectiveness and characteristics of mHealth interventions to increase adolescent’s use of Sexual and Reproductive Health services in Sub-Saharan Africa: a systematic review. PLoS One 2022; 17(1): e0261973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Martin P, Cousin L, Gottot S, et al. Participatory interventions for sexual health promotion for adolescents and young adults on the internet: systematic review. J Med Internet Res 2020; 22(7): e15378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Meijers K, van der Kwaak A, Aqel I, et al. Using a Rapid knowledge translation approach for better sexual and reproductive health and rights in Bangladesh, Burundi, Indonesia, and Jordan. Glob Health Sci Pract 2022; 10(2): e2100461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Crutzen R, Peters GJY, Portugal SD, et al. An artificially intelligent chat agent that answers adolescents’ questions related to sex, drugs, and alcohol: an exploratory study. J Adolesc Health 2011; 48(5): 514–519. [DOI] [PubMed] [Google Scholar]
- 12. L’Engle KL, Mangone ER, Parcesepe AM, et al. Mobile phone interventions for adolescent sexual and reproductive health: a systematic review. Pediatrics 2016; 138(3): e20160884. [DOI] [PubMed] [Google Scholar]
- 13. Cornelius JB, St. Lawrence JS, Howard JC, et al. Adolescents’ perceptions of a mobile cell phone text messaging-enhanced intervention and development of a mobile cell phone-based HIV prevention intervention. J Spec Pediatr Nurs 2012; 17(1): 61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guse K, Levine D, Martins S, et al. Interventions using new digital media to improve adolescent sexual health: a systematic review. J Adolesc Health 2012; 51(6): 535–543. [DOI] [PubMed] [Google Scholar]
- 15. Chen E, Mangone ER. A systematic review of apps using mobile criteria for adolescent pregnancy prevention (mCAPP). JMIR Mhealth Uhealth 2016; 4(4): e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Saragih ID, Imanuel Tonapa S, Porta CM, et al. Effects of telehealth interventions for adolescent sexual health: a systematic review and meta-analysis of randomized controlled studies. J Telemed Telecare 2024; 30(2): 201–214. [DOI] [PubMed] [Google Scholar]
- 17. Nwaozuru U, Obiezu-Umeh C, Shato T, et al. Mobile health interventions for HIV/STI prevention among youth in low- and middle-income countries (LMICs): a systematic review of studies reporting implementation outcomes. Implement Sci Commun 2021; 2(1): 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buchanan CRM, Tomaszewski K, Chung S-E, et al. Why didn’t you text me? Poststudy trends from the DepoText Trial. Clin Pediatr (Phila) 2018; 57(1): 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Reback CJ, Fletcher JB, Kisler KA. Text messaging improves HIV care continuum outcomes among young adult trans women living with HIV: Text Me, Girl! AIDS Behav 2021; 25(9): 3011–3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Handschuh C, La Cross A, Smaldone A. Is sexting associated with sexual behaviors during adolescence? A systematic literature review and meta-analysis. J Midwifery Womens Health 2019; 64(1): 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Snilstveit B, Vojtkova M, Bhavsar A, et al. Evidence & Gap Maps: a tool for promoting evidence informed policy and strategic research agendas. J Clin Epidemiol 2016; 79:120–129. [DOI] [PubMed] [Google Scholar]
- 22. Meherali S, Bhaumik S, Idrees S, et al. Digital knowledge translation tools for disseminating sexual and reproductive health information to adolescents: protocol for an evidence gap map review. JMIR Res Protoc 2024; 13: e55081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169(7): 467–473. [DOI] [PubMed] [Google Scholar]
- 25. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 26. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017; 358: j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bourdeau B, Miller BA, Byrnes HF, et al. Efficacy of a web-based intervention (Smart Choices 4 Teens) for facilitating parent-adolescent communication about relationships and sexuality: randomized controlled trial. JMIR Pediatr Parent 2021; 4(2): e19114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brown L, Tan K, Guerra L, et al. Using behavioural insights to increase HIV self-sampling kit returns: a randomized controlled text message trial to improve England’s HIV self-sampling service. HIV Med 2018; 19(9): 585–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chernick LS, Santelli J, Stockwell MS, et al. A multi-media digital intervention to improve the sexual and reproductive health of female adolescent emergency department patients. Acad Emerg Med 2022; 29(3): 308–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chong A, Gonzalez-Navarro M, Karlan D, et al. Do information technologies improve teenagers’ sexual education? Evidence from a randomized evaluation in Colombia. World Bank Econ Rev 2020; 34(2): 371–392. [Google Scholar]
- 31. Constant D, de Tolly K, Harries J, et al. Mobile phone messages to provide support to women during the home phase of medical abortion in South Africa: a randomised controlled trial. Contraception 2014; 90(3): 226–233. [DOI] [PubMed] [Google Scholar]
- 32. Cordova D, Munoz-Velazquez J, Mendoza Lua F, et al. Pilot study of a multilevel mobile health app for substance use, sexual risk behaviors, and testing for sexually transmitted infections and HIV among youth: randomized controlled trial. JMIR Mhealth Uhealth 2020; 8(3): e16251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cortese J, Lustria MLA. Can tailoring increase elaboration of health messages delivered via an adaptive educational site on adolescent sexual health and decision making? J Am Soc Inf Sci Technol 2012; 63(8): 1567–1580. [Google Scholar]
- 34. Del Río-González AM, Zea MC, Calabrese SK, et al. Development and evaluation of an online education-entertainment intervention to increase knowledge of HIV and uptake of HIV testing among Colombian men who have sex with men (MSM). Int J Environ Res Public Health 2021; 18(4): 1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Dike IC, Ebizie EN, Njoku OC, et al. Improving knowledge and perception of HIV/AIDS among English language speaking children in rural areas through educational digital storytelling. Medicine (Baltimore) 2021; 100(50): e28058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ezegbe B, Eseadi C, Ede MO, et al. Efficacy of rational emotive digital storytelling intervention on knowledge and risk perception of HIV/AIDS among schoolchildren in Nigeria. Medicine (Baltimore) 2018; 97(47): e12910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Free C, McCarthy O, French RS, et al. Can text messages increase safer sex behaviours in young people? Intervention development and pilot randomised controlled trial. Health Technol Assess 2016; 20(57): 1–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gerend MA, Madkins K, Crosby S, et al. Evaluation of a text messaging-based human papillomavirus vaccination intervention for young sexual minority men: results from a pilot randomized controlled trial. Ann Behav Med 2021; 55(4): 321–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gil-Llario MD, Ballester-Arnal R, Giménez-García C, et al. Effectiveness of HIV prevention for women: what is working? AIDS Behav 2014; 18(10): 1924–1933. [DOI] [PubMed] [Google Scholar]
- 40. Gilliam ML, Martins SL, Bartlett E, et al. Development and testing of an iOS waiting room “app” for contraceptive counseling in a Title X family planning clinic. Am J Obstet Gynecol 2014; 211(5): 481.e1–481.e8. [DOI] [PubMed] [Google Scholar]
- 41. Gonenc IM, Alan Dikmen H, Golbasi Z. The effect of WhatsApp-based and conventional education methods on sexual myths and sexual health knowledge: a comparative intervention study in midwifery students. Int J Sex Health 2021; 33(3): 326–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gonsalves L, Njeri WW, Schroeder M, et al. Research and implementation lessons learned from a youth-targeted digital health randomized controlled trial (the ARMADILLO study). JMIR Mhealth Uhealth 2019; 7(8): e13005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Green EP, Augustine A, Naanyu V, et al. Developing a digital marketplace for family planning: pilot randomized encouragement trial. J Med Internet Res 2018; 20(7): e10756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Haruna H, Hu X, Chu S, et al. Improving sexual health education programs for adolescent students through game-based learning and gamification. Int J Environ Res Public Health 2018; 15(9): 2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Horvath KJ, Bauermeister JA. eHealth literacy and intervention tailoring impacts the acceptability of a HIV/STI testing intervention and sexual decision making among young gay and bisexual men. AIDS Educ Prev 2017; 29(1): 14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hylton-Kong T, Steiner MJ, Bailey A, et al. Debunking myths about contraceptive safety among women in Kingston, Jamaica: pilot randomized controlled trial. Contraception 2021; 103(5): 356–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jones R, Hoover DR, Lacroix LJ. A randomized controlled trial of soap opera videos streamed to smartphones to reduce risk of sexually transmitted human immunodeficiency virus (HIV) in young urban African American women. Nurs Outlook 2013; 61(4): 205–215.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Macharia P, Pérez-Navarro A, Sambai B, et al. An Unstructured Supplementary Service Data-based mHealth app providing on-demand sexual reproductive health information for adolescents in Kibra, Kenya: randomized controlled trial. JMIR Mhealth Uhealth 2022; 10(4): e31233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Manlove J, Whitfield B, Finocharo J, et al. Lessons learned from replicating a randomized control trial evaluation of an app-based sexual health program. Int J Environ Res Public Health 2021; 18: 3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Marsch LA, Guarino H, Grabinski MJ, et al. Comparative effectiveness of web-based vs. educator-delivered HIV prevention for adolescent substance users: a randomized, controlled trial. J Subst Abuse Treat 2015; 59: 30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McCarthy O, Ahamed I, Kulaeva F, et al. A randomized controlled trial of an intervention delivered by mobile phone app instant messaging to increase the acceptability of effective contraception among young people in Tajikistan. Reprod Health 2018; 15(1): 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McCarthy OL, Zghayyer H, Stavridis A, et al. A randomized controlled trial of an intervention delivered by mobile phone text message to increase the acceptability of effective contraception among young women in Palestine. Trials 2019; 20(1): 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McRee AL, Shoben A, Bauermeister JA, et al. Outsmart HPV: acceptability and short-term effects of a web-based HPV vaccination intervention for young adult gay and bisexual men. Vaccine 2018; 36(52): 8158–8164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mortimer NJ, Rhee J, Guy R, et al. A web-based personally controlled health management system increases sexually transmitted infection screening rates in young people: a randomized controlled trial. J Am Med Inform Assoc 2015; 22(4): 805–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Nielsen AM, De Costa A, Gemzell-Danielsson K, et al. The MOSEXY trial: mobile phone intervention for sexual health in youth—a pragmatic randomised controlled trial to evaluate the effect of a smartphone application on sexual health in youth in Stockholm, Sweden. Sex Transm Infect 2021; 97(2): 141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Odeny TA, Bailey RC, Bukusi EA, et al. Effect of text messaging to deter early resumption of sexual activity after male circumcision for HIV prevention: a randomized controlled trial. J Acquir Immune Defic Syndr 2014; 65(2): e50–e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ofoegbu TO, Otu MS, Christopher I, et al. Impact of an educational digital storytelling intervention on HIV risk perception among Nigerian adolescents. J Int Med Res 2020; 48(1): 030006051985463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Perez-Lu JE, Guerrero F, Cárcamo CP, et al. The ARMADILLO text message intervention to improve the sexual and reproductive health knowledge of adolescents in Peru: results of a randomized controlled trial. PLoS One 2022; 17(2): e0262986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Riese A, Houck C, Abdullahi N, et al. An electronic sexual health module for hospitalized adolescent girls. Hosp Pediatr 2019; 9(11): 880–887. [DOI] [PubMed] [Google Scholar]
- 60. Rinehart DJ, Leslie S, Durfee MJ, et al. Acceptability and efficacy of a sexual health texting intervention designed to support adolescent females. Acad Pediatr 2020; 20(4): 475–484. [DOI] [PubMed] [Google Scholar]
- 61. Rokicki S, Fink G. Assessing the reach and effectiveness of mHealth: evidence from a reproductive health program for adolescent girls in Ghana. BMC Public Health 2017; 17(1): 969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sabben G, Mudhune V, Ondeng’e K, et al. A smartphone game to prevent HIV among young Africans (Tumaini): assessing intervention and study acceptability among adolescents and their parents in a randomized controlled trial. JMIR Mhealth Uhealth 2019; 7(5): e13049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Schnall R, Kuhns L, Pearson C, et al. Preliminary results from a pragmatic clinical trial of MyPEEPS mobile to improve HIV prevention behaviors in young men. Stud Health Technol Inform 2020; 270: 1365–1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Shegog R, Peskin MF, Markham C, et al. It’s your game-tech: toward sexual health in the digital age. Creat Educ 2014; 5(15): 1428–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Starosta AJ, Cranston E, Earleywine M. Safer sex in a digital world: a Web-based motivational enhancement intervention to increase condom use among college women. J Am Coll Health 2016; 64(3): 184–193. [DOI] [PubMed] [Google Scholar]
- 66. Stephenson J, Bailey JV, Blandford A, et al. An interactive website to aid young women’s choice of contraception: feasibility and efficacy RCT. Health Technol Assess 2020; 24(56): 1–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Tan RKJ, Koh WL, Le D, et al. Effect of a popular web drama video series on HIV and other sexually transmitted infection testing among gay, bisexual, and other men who have sex with men in Singapore: community-based, pragmatic, randomized controlled trial. J Med Internet Res 2022; 24(5): e31401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Tang J, Zheng Y, Zhang D, et al. Evaluation of an AIDS educational mobile game (AIDS Fighter · Health Defense) for young students to improve AIDS-related knowledge, stigma, and attitude linked to high-risk behaviors in China: randomized controlled trial. JMIR Serious Games 2022; 10(1): e32400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Winskell K, Sabben G, Akelo V, et al. A Smartphone game-based intervention (Tumaini) to prevent HIV among young Africans: pilot randomized controlled trial. JMIR Mhealth Uhealth 2018; 6(8): e10482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Wirsiy FS, Atuhaire C, Ngonzi J, et al. A randomized controlled trial on mobile phone text messaging to improve sexo-reproductive health among adolescent girls in Cameroon. Contracept Reprod Med 2022; 7(1): 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wong JYH, Zhang W, Wu Y, et al. An interactive web-based sexual health literacy program for safe sex practice for female Chinese university students: multicenter randomized controlled trial. J Med Internet Res 2021; 23(3): e22564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ybarra ML, Agaba E, Nyemara N. A pilot RCT evaluating InThistoGether, an mHealth HIV prevention program for Ugandan youth. AIDS Behav 2021; 25(10): 3437–3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Zha P, Mahat G, Qureshi R, et al. Utilising a WeChat intervention to improve HIV and AIDS education among college students in China. Health Educ J. 2021;80(8):1002–1013. [Google Scholar]
- 74. Widman L, Golin CE, Kamke K, et al. Sexual assertiveness skills and sexual decision-making in adolescent girls: randomized controlled trial of an online program. Am J Public Health 2018; 108(1): 96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Babalola S, Loehr C, Oyenubi O, et al. Efficacy of a digital health tool on contraceptive ideation and use in Nigeria: results of a cluster-randomized control trial. Glob Health Sci Pract 2019; 7(2): 273–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lohan M, Aventin Á, Clarke M, et al. Can teenage men be targeted to prevent teenage pregnancy? A feasibility cluster randomised controlled intervention trial in schools. Prev Sci 2018; 19(8): 1079–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Tebb KP, Rodriguez F, Pollack LM, et al. Improving contraceptive use among Latina adolescents: a cluster-randomized controlled trial evaluating an mHealth application, Health-E You/Salud iTu. Contraception 2021; 104(3): 246–253. [DOI] [PubMed] [Google Scholar]
- 78. Zhang X, Chen H, Zhou J, et al. Impact of web-based health education on HPV vaccination uptake among college girl students in Western and Northern China: a follow-up study. BMC Womens Health 2022; 22(1): 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ujang F, Sutan R. The effects of short health messages intervention in improving knowledge and attitude on sexual and reproductive health among late adolescents at colleges in Malaysia. Open J Prev Med 2018; 8(8): 207–228. [Google Scholar]
- 80. Haruna H, Okoye K, Zainuddin Z, et al. Gamifying sexual education for adolescents in a low-tech setting: quasi-experimental design study. JMIR Serious Games 2021; 9(4): e19614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Musiimenta A. A controlled pre-post evaluation of a computer-based HIV/AIDS education on students’ sexual behaviors, knowledge and attitudes. Online J Public Health Inform 2012; 4(1): ojphi.v4i1.4017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Nalwanga R, Nuwamanya E, Nuwasiima A, et al. Utilization of a mobile phone application to increase access to sexual and reproductive health information, goods, and services among university students in Uganda. Reprod Health 2021; 18(1): 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Nik Farid ND, Mohd Arshad MFB, Yakub NA, et al. Improving Malaysian adolescent sexual and reproductive health: an internet-based health promotion programme as a potential intervention. Health Educ J 2018; 77(7): 837–848. [Google Scholar]
- 84. Njuguna N, Ngure K, Mugo N, et al. The effect of human immunodeficiency virus prevention and reproductive health text messages on human immunodeficiency virus testing among young women in rural Kenya: a pilot study. Sex Transm Dis 2016; 43(6): 353–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Turah S, Anggraen MD, Setiawati N. The effect of an android application on adolescent’s knowledge and attitudes toward premarital sex. Ann Trop Med Public Health 2019; 22(11): 150–157. [Google Scholar]
- 86. Jones K, Eathington P, Baldwin K, et al. The impact of health education transmitted via social media or text messaging on adolescent and young adult risky sexual behavior: a systematic review of the literature. Sex Transm Dis 2014; 41(7): 413–419. [DOI] [PubMed] [Google Scholar]
- 87. United Nations Educational, Scientific and Cultural Organization (UNESCO). Comprehensive sexuality education: for healthy, informed and empowered learners, https://www.unesco.org/en/health-education/cse (2023, accessed 10 December 2023).
- 88. Huang KY, Kumar M, Cheng S, et al. Applying technology to promote sexual and reproductive health and prevent gender based violence for adolescents in low and middle-income countries: digital health strategies synthesis from an umbrella review. BMC Health Serv Res 2022; 22(1): 1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Liberty A, Samuelson Bannow B, Matteson K, et al. Menstrual technology innovations and the implications for heavy menstrual bleeding. Obstet Gynecol 2023; 141(4): 666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Adler A, Biggs MA, Kaller S, et al. Changes in the frequency and type of barriers to reproductive health care between 2017 and 2021. JAMA Netw Open 2023; 6(4): e237461. [DOI] [PMC free article] [PubMed] [Google Scholar]