Abstract
Background
The COVID-19 pandemic has variably affected the stress levels among students. Nursing students, as the reserve force of medical resources and the successors of frontline nursing staff, warrant particular attention regarding their stress levels. This study investigates the relationship between emotional empathy, emotional intelligence, and COVID-19-related stress in nursing students and examines the masking role of emotional intelligence in this relationship.
Methods
A cross-sectional study was conducted from March to June 2023 using multi-stage sampling method to recruit 1126 nursing students from a medical university. Participants completed a demographic information questionnaire, the COVID-19 Student Stress Questionnaire, the Multidimensional Emotional Empathy Scale, and the Trait Meta-Mood Scale. Data were analyzed using t-tests/ one-way ANOVA, Pearson correlations, multiple linear regression, and the PROCESS macro program to examine the relationships between emotional empathy, emotional intelligence, and COVID-19-related stress, as well as the masking role of emotional intelligence.
Results
Statistically significant differences were observed in COVID-19-related stress scores among nursing students from different residential areas (P < 0.05); Emotional empathy was significantly positively correlated with emotional intelligence and its dimensions. Emotional empathy also showed a significant positive correlation with COVID-19-related stress. Emotional intelligence and its dimensions were significantly negatively correlated with COVID-19-related stress; Emotional empathy and emotional intelligence were significant predictors of COVID-19-related stress; Emotional intelligence and its dimensions demonstrated a masking effect on the relationship between emotional empathy and COVID-19-related stress, with total effect sizes of -0.023 for emotional intelligence, -0.021 for emotional attention, -0.017 for emotional clarity, and − 0.018 for emotional repair.
Conclusion
Emotional empathy and emotional intelligence were significant predictors of COVID-19-related stress among nursing students. Emotional intelligence masked the impact of emotional empathy on COVID-19-related stress. Schools should implement stress management programs for nursing students that focus on enhancing emotional intelligence and moderating excessive emotional empathy. These programs are particularly crucial during public health emergencies to reduce stress levels and promote mental well-being.
Clinical trial number
Not applicable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06474-z.
Keywords: COVID-19, Stress, Emotional empathy, Emotional intelligence, Nursing students
Introduction
Since December 2019, the COVID-19 pandemic has had a significant and widespread impact, and is considered the most severe global emerging public health crisis since the 21st century [1]. The emergence and prevention of COVID-19 have posed challenges for students in various aspects, including learning, returning to school, and going out. The long-term home isolation, school closures, changes in learning modes and lifestyles, combined with the fear of the pandemic, have exacerbated the burden on students’ mental health, generating negative emotions such as anxiety and stress [2]. It has been shown that a significant number of students have experienced stress, fear, and unease following the COVID-19 outbreak [3]. Compared with general university students, nursing students face greater psychological stress due to the dual roles they assume as learners and semi-professional caregivers, stemming from the unique characteristics of their profession. On the one hand, nursing students must manage demanding academic workloads, including mastering professional knowledge and developing clinical skills. On the other hand, during the COVID-19 pandemic, they were directly exposed to high-risk work environments, witnessing patients’ suffering and healthcare workers succumbing to infections or even losing their lives. These experiences heightened their awareness of occupational risks and intensified their fear of such dangers [4]. As their perception of high-risk environments deepened, their sense of stress became increasingly pronounced [5]. Studies have shown that during the COVID-19 pandemic, nursing students experienced significantly higher levels of stress and anxiety compared to non-medical students, due to increased exposure to risk and emotional burdens [6]. As a significant determinant of mental health [7], stress plays an indispensable role in the healthy development of nursing students. Therefore, investigating the COVID-19-related stress and its influencing factors among nursing students is of paramount importance.
In nursing practice, understanding the role of emotional empathy becomes crucial due to the critical nature of emotional connections. Emotional empathy refers to the ability to resonate with the emotional state of others and generate similar emotional responses [8], and is intrinsic to communication between nurses and patients [9]. High levels of emotional empathy among nursing staff are often recognized as contributing to improved nurse-patient relationships, enhanced social support, and active participation in healthcare decision-making, as well as improved patient experience and satisfaction [10, 11]. However, emotional empathy, as a complex and multifaceted trait, may also pose potential psychological risks [12]. Emotion regulation theory states that individuals need to adapt to environmental stress by regulating emotional experience and expression [13]. In high-stress work environments (e.g., during the COVID-19 pandemic), emotional empathic responses can significantly deplete emotional regulation capacity. When faced with patient suffering or even death, nursing staff with high levels of emotional empathy may struggle to adapt, leaving them more vulnerable to emotional exhaustion and heightened psychological burden and stress [14]. Tobias Altmann and Marcus Roth [15] suggest that high levels of emotional empathy in healthcare professionals, especially those working in emotionally demanding environments over the long term, could significantly amplify their emotional workload and consequently contribute to increased stress. Liu et al. [16] have suggested that an overabundance of empathy in journalists could heighten their susceptibility to the emotional strains intrinsic to their profession. In a cross-sectional study of medical students, there was a significant positive correlation between emotional empathy and perceived stress [17]. Therefore, emotional empathy may exacerbate the stress experienced by nursing students in the face of the novel coronavirus pneumonia outbreak.
The outbreak of novel coronavirus pneumonia has imposed higher demands on nursing work and presented significant challenges to the nursing profession [18]. In a complex and ever-changing healthcare environment, nursing students not only need to have good professional qualities, solid professional knowledge, and proficient nursing skills, but also require a high level of emotional intelligence [19]. Emotional intelligence refers to the ability to perceive one’s own and others’ emotions and is the capacity to recognize emotions and use emotional information to guide behavior and thinking. It includes three aspects: emotional attention (the ability to attend to own feelings), clarity (the ability to discriminate among feelings), and repair (the ability to recover from a negative mood) [20]. Stress buffering theory suggests that certain personal traits can alleviate the negative impact of stressors on individuals. Emotional intelligence, as an internal resource of an individual, is able to effectively identify his or her own emotions and sources of stress, and to adopt positive emotion regulation strategies to cope with stressful situations, thereby mitigating the adverse effects of stress [21]. Previous study has indicated that emotional intelligence has a significant negative impact on perceiving stress [22]. Nursing personnel who possess elevated levels of emotional intelligence can diminish the intensity and presence of negative emotions, thereby positively influencing the management of stressful situations. El Bermejo-Martins et al. [23] also reported a negative relationship between emotional intelligence and its components (clarity and repair) with stress perception in individuals during the COVID-19 pandemic. In addition, emotional intelligence and its components can act as mediators in alleviating stress, as explored in studies examining the relationship between stress and related factors. Bao et al. [24] reported that emotional repair was identified as an intermediate factor in the connection between inherent mindfulness and the perception of stress. Previous study has also found that emotional intelligence among Sicilian teachers played an intermediate role between certain remote work risk factors and stress during the COVID-19 pandemic [25]. Therefore, emotional intelligence and its components may play a mediating role in reducing COVID-19-related stress among nursing students.
In addition, some studies have demonstrated that emotional empathy has a significant positive predictive effect on emotional intelligence [26, 27], such that individuals with high levels of emotional empathy are associated with better emotional intelligence. Furthermore, emotional empathy plays an active role in the processes of emotion attention and emotion recognition [28, 29]. Individuals with high levels of emotional empathy are more effective in attending to and understanding the emotions of others, which positively affects emotional intelligence. Therefore, it can be inferred that emotional intelligence and its components may mediate the relationship between emotional empathy and COVID-19-related stress. However, in a mediation model where emotional intelligence acts as the mediating variable, the indirect pathway may reduce individuals’ COVID-19-related stress through emotional intelligence, resulting in a situation where the direct and indirect effects have opposite signs, and the total effect is masked. This suggests that the indirect pathway of emotional empathy affecting stress through emotional intelligence may overshadow the direct effect of emotional empathy on stress.
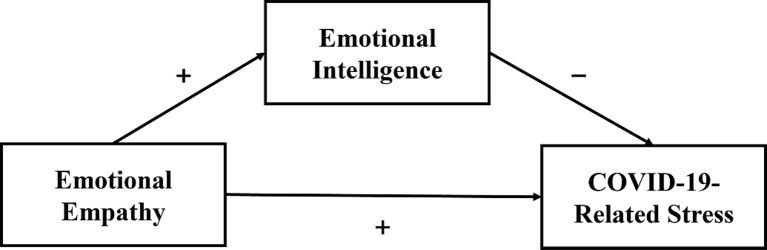
This study examines the role of emotional intelligence in the relationship between emotional empathy and COVID-19-related stress based on conservation of resources theory (COR). According to conservation of resources theory, individuals cope with environmental stress by acquiring, conserving, and effectively utilizing emotional resources. When faced with a lack of resources or investing in existing resources without acquiring new ones, individuals will perceive psychological threats and stress [30]. In high-pressure environments, emotional empathy tends to consume large amounts of emotional resources, which may lead to emotional depletion and increased stress. However, emotional intelligence, as an important resource, can help individuals cope with and regulate these emotional responses, protecting them from resource loss and mitigating the negative impact of emotional empathy on stress. Based on the above analysis, this study proposes the following hypothesis: Emotional intelligence and its dimensions have a masking effect between emotional empathy and COVID-19-related stress. The hypothesized model is illustrated in Fig. 1.
Fig. 1.
Hypothetical model
Materials and methods
Study design and participants
This study collected data using a multi-stage sampling design from March to June 2023. The inclusion criteria for participants were as follows: (1) full-time nursing students currently enrolled in nursing professional courses; (2) clear consciousness, without hearing, vision, or verbal communication impairments, and able to cooperate in completing the questionnaire; and (3) informed of the purpose of the study and volunteering to participate in the study. Exclusion Criteria: (1) those who refused to participate in the study; (2) individuals whose education was disrupted or who were unable to complete their studies during the investigation period; (3) non-nursing students [31]. According to the sample size estimation method proposed by Kendall [32], the sample size should be 10–20 times the number of items. This study’s questionnaire comprises a total of 61 items, which include the COVID-19 Student Stress Questionnaire (7 items), the Multidimensional Emotional Empathy Scale (30 items), and the Trait Meta-Mood Scale (24 items). Consequently, the inferred sample size ranges from 610 to 1220.
Firstly, we used a random number Table [33] to select one school from 6 nursing schools in Liaoning Province, and finally identified Jinzhou Medical University as the investigation site for this study. Secondly, in the selected school, 80% of the classes in each year of the university were selected using the same random number table method, covering 16–18 classes, for a total of 40 classes. Subsequently, 25–30 students from each class continued to be selected using the random number table method for a total of 1186 nursing students. Before data collection, ten graduate students received consistent training on conducting interviews using standardized language and instructions. Finally, a total of 1176 nursing students participated in the survey. After excluding 50 students who submitted incomplete questionnaires, the final analysis included 1126 nursing students, resulting in an effective response rate of 94.94%.
The researchers obtained informed consent from the nursing students and then administered and completed individual questionnaires to the nursing students. The study was approved by the Medical Ethics Committee (approval number: JZMULL2023028). All methods are in line with the declaration of Helsinki.
Measurements
General information questionnaires
The questionnaire was designed by the researchers and included information on age, gender, residence status, grade, willingness to choose nursing upon admission, and whether to engage in nursing after graduation (An additional file shows this in more detail [see Additional file 1]). Ages were categorized into three groups: 17 ~ 21, 22 ~ 26, and ≥ 27. Gender was divided into two categories: male and female. Residence status was classified into urban, rural, and suburban areas. Grade was divided into three groups: Freshman, Sophomore, and Junior. Willingness to choose nursing upon admission was categorized into three types: voluntary choice, influenced by others, and others (favorable job prospects, transfer). Whether to engage in nursing after graduation was divided into three responses: yes, no, and uncertain.
COVID-19 student stress questionnaire (CSSQ)
The COVID-19 Student Stress Questionnaire (CSSQ) was developed by Zurlo et al. in 2020 to measure students’ perceived stress during the COVID-19 pandemic [34]. The scale has been shown to be valid in Chinese populations [35–38]. The scale consists of 7 items on a 5-point Likert scale, where 0 indicates “not at all stressful” and 4 indicates “extremely stressful.” The total score ranges from 0 to 28, with higher scores indicating greater levels of perceived stress associated with COVID-19. The study by Zurlo et al. demonstrated good reliability of the CSSQ, with a Cronbach’s α coefficient of 0.710. We translated the CSSQ into Chinese and validated it through a back-translation procedure. Next, two pilot studies were conducted in the Southeast and Northwest to ensure that the translated version did not have any geographical and cultural differences. Finally, the reliability and validity of the Chinese version were assessed, which confirmed that the Chinese version has good properties for measuring COVID-19-related stress in college students, with a Cronbach’s α coefficient of 0.876, test-retest reliability of 0.884, I-CVI of 0.857 ~ 1.000, S-CVI/UA of 0.857, and KMO value of 0.883. The Cronbach ‘s α coefficient of this study was 0.895.
Multidimensional emotional empathy scale (MDEES)
The MDEES scale, originally developed by Caruso and Mayer in 1998, is a scale designed to measure the ability to recognize and understand the emotions experienced by others [39]. The scale consisted of 30 items, divided into six subscales: Suffering, Positive Sharing, Responsive Crying, Emotional Attention, Feel for Others, and Emotional Contagion. The scale was scored from 1 to 5 (completely disagree to completely agree), with a total score ranging from 30 to 150. Higher scores indicated higher levels of emotional empathy. The MDEES is a reliable tool, with Cronbach’s α coefficients for different samples ranging from 0.880 to 0.910. The MDEES was translated into Chinese and validated through a back-translation procedure. Subsequently, two pilot studies were conducted in the southeast and northwest of China to ensure the translated version was free from geographical and cultural biases across different regions. Finally, the reliability and validity of the Chinese version were assessed, confirming its suitability for measuring emotional empathy among college students, with a Cronbach’s α coefficient of 0.877, test-retest reliability of 0.844, I-CVI of 0.857 ~ 1.000, S-CVI/UA of 0.933, and KMO value of 0.926. The scale has demonstrated validity in Chinese populations [40]. In this study, the scale demonstrated acceptable internal consistency, with a Cronbach’s α of 0.810.
Trait meta-mood scale (TMMS-24)
The Trait Meta-Mood Scale was developed by Salovey et al. in 1995 to measure emotional intelligence [41]. To improve the efficiency of the measurement, the researchers simplified the original TMMS, resulting in the TMMS-24 [42]. The scale consists of 24 items, each of which is scored on a scale of 1 to 5, with 1 indicating strong disagreement and 5 indicating strong agreement. The scale is divided into three subscales: attention, clarity, and repair, with scores ranging from 8 to 40 for each subscale. Higher scores in Clarity and Repair indicate a more appropriate level, while a higher score in Attention suggests excessive emotional focus that needs to be improved. The Cronbach ' s α coefficients of all subscales in the original scale [42] were above 0.850. Li et al. [43] translated it into Chinese by the translating-callback method in 2002 and confirmed that the Chinese version had good reliability and validity among Chinese college students, with a Cronbach ‘s α coefficient of 0.750. The scale demonstrated acceptable internal consistency in this study (Cronbach’s α = 0.891).
Statistical analysis
Statistical analysis of the questionnaire data was performed using SPSS 25.0 software and the Process macro program developed by Hayes. Descriptive statistics were used to describe the general demographic characteristics of the study population, the independent sample t-tests or ANOVA were used to compare the differences between the groups. Pearson’s correlation analysis was used to examine the correlation between emotional empathy, emotional intelligence, and COVID-19-related stress. Multiple linear regression was used to examine potential predictive relationships and masking effects among emotional empathy, emotional intelligence, and COVID-19-related stress. Further validation of the masking effect of emotional intelligence was conducted using the PROCESS macro program, and the study conclusions were obtained.
Results
Descriptive statistics
A total of 1126 valid questionnaires were finally analyzed. Among them, 145 (12.88%) were male and 981 (87.12%) were female; more than half of them lived in the urban; 45.38% of them were in the first year of their grade; more than half of them voluntarily chose to specialize in nursing (640, 56.84%); and 135 (11.99%) of them did not want to work as a nurse after graduation. According to the COVID-19-related stress scores of nursing students with different characteristics, the results showed statistically significant differences between different residence status (P < 0.05), as shown in Table 1.
Table 1.
Demographic variables of nursing students (N = 1126)
| Variables | Group | N (%) | COVID-19-related stress | F/t | P | |
|---|---|---|---|---|---|---|
| Mean | SD | |||||
| Age | 17 ~ 21 | 396(35.17%) | 9.31 | 6.53 | 0.143 | 0.867 |
| 22 ~ 26 | 727(64.56%) | 9.29 | 6.63 | |||
| ≥ 27 | 3(0.27%) | 11.33 | 9.50 | |||
| Gender | Male | 145(12.88%) | 9.12 | 7.02 | -0.349 | 0.727 |
| Female | 981(87.12%) | 9.33 | 6.53 | |||
| Residence status | Urban | 597(53.02%) | 8.30 | 6.57 | 15.768 | 0.000 |
| Rural | 436(38.72%) | 10.58 | 6.49 | |||
| Suburb | 93(8.26%) | 9.77 | 6.21 | |||
| Grade | Freshman | 511(45.38%) | 9.38 | 6.73 | 0.069 | 0.934 |
| Sophomore | 460(40.85%) | 9.26 | 6.41 | |||
| Junior | 155(13.77%) | 9.18 | 6.73 | |||
| Willingness | Voluntary choice | 640(56.84%) | 9.08 | 6.65 | 1.219 | 0.296 |
| Influenced by others | 272(24.16%) | 9.82 | 6.51 | |||
| Others | 214(19.01%) | 9.33 | 6.53 | |||
| Whether to engage in nursing after graduation | Yes | 534(47.43%) | 8.95 | 6.59 | 2.388 | 0.092 |
| No | 135(11.99%) | 10.30 | 6.86 | |||
| Uncertain | 457(40.59%) | 9.42 | 6.50 | |||
Scores and correlation analysis of emotional empathy, emotional intelligence, and COVID-19-related stress among nursing students
Pearson’s correlation analysis showed that nursing students’ emotional empathy was significantly positively correlated with COVID-19-related stress, as well as significantly positively correlated with emotional intelligence and its dimensions (emotional attention, clarity, and repair) (P < 0.01). Emotional intelligence and its dimensions were significantly negatively correlated with the COVID-19-related stress scores (P < 0.01), as shown in Table 2.
Table 2.
Correlations among continuous variables
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| Emotional Empathy | 87.67 | 15.28 | 1.000 | |||||
| Emotional Intelligence | 91.70 | 15.26 | 0.319** | 1.000 | ||||
| Emotional Attention | 31.23 | 5.62 | 0.318** | 0.896** | 1.000 | |||
| Emotional Clarity | 30.15 | 5.63 | 0.257** | 0.922** | 0.745** | 1.000 | ||
| Emotional Repair | 30.32 | 5.59 | 0.293** | 0.901** | 0.690** | 0.761** | 1.000 | |
| COVID-19-related stress | 9.30 | 6.60 | 0.111** | -0.123** | -0.110** | -0.122** | -0.103** | 1.000 |
Multiple linear regression analysis
Three multiple linear regression analyses were conducted, with COVID-19-related stress as the dependent variable, residence status as the control variable, and emotional empathy and emotional intelligence as the main independent variables. In the first step, emotional empathy was the independent variable and emotional intelligence was the dependent variable. The results showed that emotional empathy positively predicted emotional intelligence and its dimensions (emotional attention, clarity, and repair) (β = 0.319, P < 0.001; β = 0.318, P < 0.001; β = 0.256, P < 0.001; β = 0.293, P < 0.001). In the second step, emotional empathy was the independent variable and COVID-19-related stress was the dependent variable. The results showed that emotional empathy was a significant positive predictor of COVID-19-related stress (β = 0.112, P < 0.001). In the third step, emotional empathy and emotional intelligence were the independent variables and COVID-19-related stress was the dependent variable. The results showed that emotional intelligence and its dimensions (emotional attention, clarity, and repair) had a significant negative predictive effect on COVID-19-related stress (β=-0.166, P < 0.001; β=-0.152, P < 0.001; β=-0.150, P < 0.001; β=-0.140, P < 0.001), and emotional empathy remained a significant positive predictor of COVID-19-related stress (β = 0.165, P < 0.001; β = 0.160, P < 0.001; β = 0.150, P < 0.001; β = 0.153, P < 0.001). The specific results are shown in Table 3.
Table 3.
Multiple linear regression analysis results
| Dependent variable | Emotional Intelligence | Emotional Attention | Emotional Clarity | Emotional Repair | COVID-19-related stress | ||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 | |
| Control variable | |||||||||
| Residence status | -0.076** | -0.072* | -0.078** | -0.055 | 0.136*** | 0.123*** | 0.125*** | 0.124*** | 0.128*** |
| Independent variable | |||||||||
| Emotional Empathy | 0.319*** | 0.318*** | 0.256*** | 0.293*** | 0.112*** | 0.165*** | 0.160*** | 0.150*** | 0.153*** |
| Emotional Intelligence | -0.166*** | ||||||||
| Emotional Attention | -0.152*** | ||||||||
| Emotional Clarity | -0.150*** | ||||||||
| Emotional Repair | -0.140*** | ||||||||
| R² | 0.108 | 0.107 | 0.072 | 0.089 | 0.031 | 0.055 | 0.051 | 0.052 | 0.049 |
| △R² | 0.102 | 0.101 | 0.066 | 0.086 | 0.012 | 0.025 | 0.021 | 0.021 | 0.018 |
| F | 67.692*** | 66.971*** | 43.552*** | 54.767*** | 17.812*** | 21.924*** | 20.240*** | 20.395*** | 19.154*** |
*:P<,05; **:P<0.01; ***:P<0.001
Bootstrapping mediating effect analysis
To test the masking effect of emotional intelligence and its dimensions, 5000 Bootstrap replicates were sampled using Model 4 from the PROCESS macro. The results are shown in Table 4. For path 1, the results showed that the total effect of emotional empathy on COVID-19-related stress was 0.048, with a confidence interval of [0.020, 0.075]. The direct effect was 0.071, with a confidence interval of [0.043, 0.098]. The indirect effect was − 0.023, with a confidence interval of [-0.034, -0.013]. According to Wen and Ye [44], due to the opposite signs of the indirect and direct effects, we categorize this as a masking effect, with the magnitude of the masking effect |ab/c’| being 32.39%. Consequently, the masking effect of emotional intelligence on the relationship between emotional empathy and COVID-19 related stress is validated. For path 2, the results revealed that emotional attention played a significant mediating role between emotional empathy and COVID-19-related stress, with a masking effect of 30.43%. For path 3, the results showed that emotional clarity had a significant mediating effect between emotional empathy and COVID-19-related stress, with a masking effect of 26.15%. Lastly, for path 4, the results indicated that emotional repair played a significant mediating role between emotional empathy and COVID-19-related stress, with a masking effect of 27.27%.
Table 4.
Results of mediating effect test
| Path | Effect types | Effect value | Boot SE | Boot LLCI | Boot ULCI |
|---|---|---|---|---|---|
| Path 1: Emotional Empathy→ Emotional Intelligence→ COVID-19-related stress | Indirect effect | -0.023 | 0.006 | -0.034 | -0.013 |
| Direct effect | 0.071 | 0.014 | 0.043 | 0.098 | |
| Total effect | 0.048 | 0.014 | 0.020 | 0.075 | |
| Path 2: Emotional Empathy→ Emotional Attention→ COVID-19-related stress | Indirect effect | -0.021 | 0.005 | -0.032 | -0.012 |
| Direct effect | 0.069 | 0.014 | 0.041 | 0.096 | |
| Total effect | 0.048 | 0.014 | 0.020 | 0.075 | |
| Path 3: Emotional Empathy→ Emotional Clarity→ COVID-19-related stress | Indirect effect | -0.017 | 0.005 | -0.026 | -0.009 |
| Direct effect | 0.065 | 0.014 | 0.037 | 0.092 | |
| Total effect | 0.048 | 0.014 | 0.020 | 0.075 | |
| Path 4: Emotional Empathy→ Emotional Repair→ COVID-19-related stress | Indirect effect | -0.018 | 0.005 | -0.028 | -0.009 |
| Direct effect | 0.066 | 0.014 | 0.038 | 0.093 | |
| Total effect | 0.048 | 0.014 | 0.020 | 0.075 |
Discussion
This study analyzed the effects of emotional empathy and emotional intelligence on COVID-19-related stress among nursing students and explored the masking effect of emotional intelligence and its dimensions between emotional empathy and COVID-19-related stress.
In this study, COVID-19-related stress in nursing students was found to be influenced by their residential areas. Nursing students residing in urban areas perceived lower COVID-19-related stress compared to those in rural and suburban areas, which is consistent with the findings of Sun et al. [45]. This difference may be due to the imbalance in economic, cultural and material resources between urban and rural areas. First, compared to urban areas, rural and suburban areas may have slower access to and dissemination of epidemic control information. Due to information asymmetry, rural and suburban college students may feel more anxious and worried [46]. Second, the COVID-19 pandemic has led to restrictions on the primary sources of income for many rural households [47]. Rural and suburban college students may bear greater responsibilities and stress due to financial difficulties and instability within their families, such as taking care of family members and shouldering family expenses. These pressures, along with the uncertainties brought by the COVID-19 pandemic, contribute to a greater perception of stress among rural and suburban college students [48]. Third, relative to urban areas, rural and suburban regions tend to have limited medical resources. During the pandemic, rural and suburban college students who contract or exhibit suspected symptoms of COVID-19 may have limited access to medical care and treatment, which exacerbates their concerns about inadequate healthcare provisions and, consequently, increases psychological stress [49].
After adjusting for demographic characteristics, emotional empathy was significantly associated with COVID-19-related stress, aligning with the outcomes of similar research. A cross-sectional study conducted among college students during the COVID-19 pandemic explored the association between different dimensions of empathy and the stress experienced, and showed that specific dimensions of empathy were significantly associated with increased stress [50]. The results of the study by Vučinić et al. showed that there was a significant correlation of moderate strength between the stressor scale scores and the overall empathy scale scores of general secondary school teachers. This relationship was not generated by empathic concern (related to positive feelings), but by personal distress (related to negative feelings when observing others in discomfort) [51]. Argentinean scholars surveyed 651 students and found a significant positive correlation between emotional empathy and stress perception [52]. When empathizing with others, individuals experience their emotions and feelings as if they were their own, which may include negative emotions and stress [53]. This is particularly true for individuals with high levels of emotional empathy, who may be more sensitive to these pressures and difficulties, leading to a greater perception of stress. Nursing students, as future healthcare professionals, are more likely to develop emotional resonance when witnessing healthcare workers experiencing trauma related to the pandemic. Nursing students with higher levels of empathic competence have a greater tendency to be deeply involved in the negative emotional circumstances caused by an epidemic [54]. While empathic competence is often beneficial to nursing practice [55, 56], in the context of an epidemic it can lead to exacerbated vicarious distress and psychological stress, making it more difficult for students to manage and recover from empathic stress [50]. Additionally, individuals with stronger empathic abilities may exhibit more altruistic behaviors, often preferring to expend greater effort to help others, even at the expense of their interests and needs [57]. They may feel a sense of responsibility and pressure to help others solve their problems and alleviate their dilemmas, but this may be associated with increased stress for themselves. However, it is important to note that emotional empathy itself is not the primary factor leading to increased stress, but rather individual perceptions and response styles [58, 59]. Individuals may feel an increase in stress because they are overly invested and burdened with the emotions of others, or because they are unable to deal effectively with their own and others’ emotions. Therefore, the use of appropriate emotional boundaries and coping strategies is important along with the development of emotional empathy to help individuals cope with their own and others’ emotional challenges to avoid unnecessary increases in stress levels.
This study also examined the masking effects of emotional intelligence and its dimensions (emotional attention, clarity, repair) on the relationship between emotional empathy and COVID-19-related stress. Based on the distinction between mediating and masking effects made by MacKinnon et al. [60], the indirect effect of emotional intelligence and its dimensions on emotional empathy and COVID-19-related stress is essentially a masking effect. Baron and Kenny [61] suggest that the question of the masking effect needs to shift from “How does X affect Y” to “How does X not affect Y”. Therefore, the present study examines “Why does emotional empathy not partially affect perceived stress when individuals are high in emotional intelligence?” Possible reasons are as follows: Individuals with high emotional intelligence have greater abilities in emotional attention and differentiation, which enable them to employ more balanced empathetic strategies. While empathizing with others’ emotions, they maintain the independence of their own emotions and avoid becoming overwhelmed by the stress associated with emotional empathy [62]. In addition, individuals with high emotional intelligence tend to adopt effective coping strategies, such as confronting stress and solving problems through action-oriented or goal-oriented approaches, rather than being troubled by the negative impacts of emotional empathy [63]. Moreover, according to the broaden and build theory, negative emotions typically narrow and diminish an individual’s cognitive and behavioral repertoire, while positive emotions activate action, broaden cognition, and alleviate stress [64]. Nursing students with higher emotional intelligence were able to regulate their emotions effectively, and this ability helped them to be more inclined to generate positive emotions in the face of challenges, which mitigated to some extent the negative emotions experienced by highly emotionally empathic individuals during the COVID-19 pandemic. Nursing students demonstrated a high level of emotional intelligence in this study, which is consistent with the findings of Gregor Stiglich et al. [65]. It is worth noting that emotional intelligence is a competency or trait that can be developed [66], which indicates the necessity for educational institutions to evaluate students’ emotional intelligence as early as possible. Institutions should promptly identify individuals with low levels of emotional intelligence and those whose perceived stress is affected by excessive emotional empathy. In addition, the emotional intelligence level of nursing students can be enhanced through the introduction of social-emotional learning courses, problem-solving skills training, and mindfulness exercises in nursing higher education programs [67–69]. By systematically designing curricula that promote the application of emotional intelligence in practical nursing work and personal life, nursing students can not only better understand and respond to patients’ emotional needs but also manage their own emotional responses more effectively during public health crises, reducing the burden and stress brought about by emotional empathy and maintaining mental health.
This study explored the relationship between emotional intelligence regarding emotional empathy and COVID-19-related stress and found that emotional intelligence was associated with mitigating the negative effects of excessive emotional empathy, which may help nursing students better cope with stress related to public health emergencies. Based on this, the following interventions are proposed: First, education departments should clarify the status of emotional intelligence courses in nursing education programs. Second, in developing emotional empathy, education departments should assist nursing students in establishing appropriate emotional boundaries and adopting effective coping strategies. Finally, interventions for excessive emotional empathy and measures to enhance emotional intelligence can be integrated into the stress management plans created for nursing students in response to public health emergencies. In the context of frequent public health emergencies, enhancing the stress management capabilities of nursing students—future healthcare providers—is crucial for their psychological well-being, preparedness for and response to public health challenges, and the development of the healthcare industry.
There are some limitations to this study. First, this study is a cross-sectional study, which cannot fully establish causal relationships between the examined variables. Additionally, the data collected were based on self-reports, which are susceptible to self-reporting bias. Future research should conduct in-depth interviews with individuals in the nursing students’ surrounding environments, such as teachers and parents, to obtain more comprehensive data. Combining longitudinal research methods with regular, time-specific follow-up surveys of participants would provide more convincing evidence for the relationships among variables. Second, the participants in this study were selected from only one university, and it remains to be tested whether the findings can be generalized to other samples. Future research should aim to include large-scale data from across the country to further test the generalizability of the findings. Third, the sample in this study was predominantly composed of female students. Future research should aim to include more heterogeneous samples to achieve a balanced representation of gender.
Conclusions
The results of this study emphasized that emotional empathy and emotional intelligence were significant predictors of COVID-19-related stress among nursing students, and that emotional intelligence masked the effects of emotional empathy on COVID-19-related stress. During the education of nursing students, educational institutions can help students cope and manage the stress of public health emergencies more effectively and mitigate the effects of excessive emotional empathy on COVID-19-related stress by providing training and guidance related to emotional intelligence.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We appreciate the contributions of each participant and the participation of the study members.
Abbreviations
- ANOVA
Analysis of Variance
- SD
Standard Deviation
- β
Standardized
- ΔR2
Amount of R2 change
- SE
Standard Error
- LLCI
Lower Limits of Confidence Interval
- ULCI
Upper Limits of Confidence Interval
Author contributions
Conceived and designed the research: Y-a C and L Z. Wrote the paper: Y-a C. Analyzed the data: Y-a C and L Z. Revised the paper: Y-a C, L Z, L-l G. All authors reviewed the manuscript.
Funding
Internal Medicine Nursing Teaching Team (2021jxtd02).
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Medical Ethics Committee of Jinzhou Medical University (approval number: JZMULL2023028) and written informed consent was obtained from the participants. All methods were performed following the Declarations of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yian Chen and Lin Zhang contributed equally to this work.
References
- 1.COVID 19 Public Health Emergency of International Concern (PHEIC). Global research and innovation forum: towards a research roadmap.
- 2.Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22(9):e22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chi X, Becker B, Yu Q, Willeit P, Jiao C, Huang L, Hossain MM, Grabovac I, Yeung A, Lin J. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID-19) pandemic. Front Psychiatry. 2020;11:803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun Q, Qian W, Yao Y, Zhu J, Xu J, Zhang L, Yao C, Wang L, Ni Y. Stress, coping and professional identity among nursing students during the COVID-19 pandemic: a latent profile analysis. Curr Psychol. 2024:1–10.
- 5.Ye W, Ye X, Liu Y, Liu Q, Vafaei S, Gao Y, Yu H, Zhong Y, Zhan C. Effect of the novel coronavirus pneumonia pandemic on medical students’ psychological stress and its influencing factors. Front Psychol. 2020;11:548506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Labrague LJ. Resilience as a mediator in the relationship between stress-associated with the Covid-19 pandemic, life satisfaction, and psychological well-being in student nurses: a cross-sectional study. Nurse Educ Pract. 2021;56:103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slimmen S, Timmermans O, Mikolajczak-Degrauwe K, Oenema A. How stress-related factors affect mental wellbeing of university students a cross-sectional study to explore the associations between stressors, perceived stress, and mental wellbeing. PLoS ONE. 2022;17(11):e0275925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gladstein GA. Understanding empathy: integrating counseling, developmental, and social psychology perspectives. J Couns Psychol. 1983;30(4):467. [Google Scholar]
- 9.Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the nature and specific effectiveness of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74(3):339–46. [DOI] [PubMed] [Google Scholar]
- 10.Wu Q, Jin Z, Wang P. The relationship between the physician-patient relationship, physician empathy, and patient trust. J Gen Intern Med. 2022;37(6):1388–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keshtkar L, Madigan CD, Ward A, Ahmed S, Tanna V, Rahman I, Bostock J, Nockels K, Wang W, Gillies CL. The effect of practitioner empathy on patient satisfaction: a systematic review of randomized trials. Ann Intern Med. 2024;177(2):196–209. [DOI] [PubMed] [Google Scholar]
- 12.Stosic MD, Blanch-Hartigan D, Aleksanyan T, Duenas J, Ruben MA. Empathy, friend or foe? Untangling the relationship between empathy and burnout in helping professions. J Soc Psychol. 2022;162(1):89–108. [DOI] [PubMed] [Google Scholar]
- 13.Gross JJ. Handbook of emotion regulation: Guilford publications. 2013.
- 14.Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, Frankel A. Emotional exhaustion among US health care workers before and during the COVID-19 pandemic, 2019–2021. JAMA Netw Open. 2022;5(9):e2232748–2232748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altmann T, Roth M. The risk of empathy: longitudinal associations between empathy and burnout. Psychol Health. 2021;36(12):1441–60. [DOI] [PubMed] [Google Scholar]
- 16.Liu M, Wang N, Wang P, Wu H, Ding X, Zhao F. Negative emotions and job burnout in news media workers: a moderated mediation model of rumination and empathy. J Affect Disorders. 2021;279:75–82. [DOI] [PubMed] [Google Scholar]
- 17.Gupta K, Kiran N. Empathy and perceived stress among college students. Int J Indian Psychol. 2021.
- 18.Buerhaus P, Fraher E, Frogner B, Buntin M, O’Reilly-Jacob M, Clarke S. Toward a stronger post-pandemic nursing workforce. N Engl J Med. 2023;389(3):200–2. [DOI] [PubMed] [Google Scholar]
- 19.McQueen AC. Emotional intelligence in nursing work. J Adv Nurs. 2004;47(1):101–8. [DOI] [PubMed] [Google Scholar]
- 20.Mayer JD. What is emotional intelligence? Emotional Development and Emotional Intelligence. In: In Emotional Development and Emotional Intelligence: Educational Implications. edn. Edited by Peter Salovey, Sluyter DJ. New York: Basic Books. 1997: 3–31.
- 21.Fteiha M, Awwad N. Emotional intelligence and its relationship with stress coping style. Health Psychol Open. 2020;7(2):2055102920970416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Molero Jurado MM, Pérez-Fuentes MdC, Oropesa Ruiz NF. Simón Márquez MdM, Gázquez Linares JJ. Self-efficacy and emotional intelligence as predictors of perceived stress in nursing professionals. Medicina. 2019;55(6):237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bermejo-Martins E, Luis EO, Fernández-Berrocal P, Martínez M, Sarrionandia A. The role of emotional intelligence and self-care in the stress perception during COVID-19 outbreak: an intercultural moderated mediation analysis. Pers Indiv Differ. 2021;177:110679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bao X, Xue S, Kong F. Dispositional mindfulness and perceived stress: the role of emotional intelligence. Pers Indiv Differ. 2015;78:48–52. [Google Scholar]
- 25.Iacolino C, Cervellione B, Isgrò R, Lombardo EMC, Ferracane G, Barattucci M, Ramaci T. The role of Emotional Intelligence and Metacognition in teachers’ stress during Pandemic Remote Working: a Moderated Mediation Model. Eur J Invest Health Psychol Educ. 2023;13(1):81–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deng X, Chen S, Li X, Tan C, Li W, Zhong C, Mei R, Ye M. Gender differences in empathy, emotional intelligence and problem-solving ability among nursing students: a cross-sectional study. Nurse Educ Today. 2023;120:105649. [DOI] [PubMed] [Google Scholar]
- 27.Hajibabaee F, Farahani MA, Ameri Z, Salehi T, Hosseini F. The relationship between empathy and emotional intelligence among Iranian nursing students. Int J Med Educ. 2018;9:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu P, Sun J, Zhang W, Li D. Effect of empathy trait on attention to positive emotional stimuli: evidence from eye movements. Curr Psychol. 2020:1–11.
- 29.Naor N, Shamay-Tsoory SG, Sheppes G, Okon-Singer H. The impact of empathy and reappraisal on emotional intensity recognition. Cognition Emot Rev. 2018;32(5):972–87. [DOI] [PubMed] [Google Scholar]
- 30.Hobfoll SE. Conservation of resources theory: Its implication for stress, health, and resilience. The Oxford handbook of stress, health, and coping. 2011, 127:147.
- 31.Song M, Zhang L, Ji Q, Ji P, Xu J, Chen Y, Guo L. Nursing students’ emotions, educational concerns, and the impact of study careers and professional futures during the COVID-19 pandemic: a cross-sectional study. BMC Med Educ. 2024;24(1):278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kendall MG. The advanced theory of statistics. 1943.
- 33.Huang F, Shen H. Intel random number generator-based true random number generator. Di 1 Jun Yi da xue xue bao = academic. J First Med Coll PLA. 2004;24(9):1091–5. [PubMed] [Google Scholar]
- 34.Zurlo MC, Cattaneo Della Volta MF, Vallone F. COVID-19 student stress questionnaire: development and validation of a questionnaire to evaluate students’ stressors related to the coronavirus pandemic lockdown. Front Psychol. 2020;11:576758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ho MK, Bharwani AA, Chan VHY, Chan EHY, Poon KS. Cross-sectional case-control study on medical students’ psychosocial stress during COVID-19 pandemic in Hong Kong. Heliyon. 2021, 7(11). [DOI] [PMC free article] [PubMed]
- 36.Hu Z, Zhu Y, Li J, Liu J, Fu M. The COVID-19 related stress and social network addiction among Chinese college students: a moderated mediation model. PLoS ONE. 2023;18(8):e0290577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu Z, Li J, Pan L, Zhang X. COVID-19 lockdown stress and the mental health of college students: a cross-sectional survey in China. Sustainability. 2022;14(19):12923. [Google Scholar]
- 38.Ye Z, Yang X, Zeng C, Wang Y, Shen Z, Li X, Lin D. Resilience, social support, and coping as mediators between COVID-19‐related stressful experiences and acute stress disorder among college students in China. Appl Psychol Health Well Being. 2020;12(4):1074–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caruso DR, Mayer JD. A measure of emotional empathy for adolescents and adults. 1998.
- 40.Shen X, Zhang W. The effect of temperament on emotion regulation among Chinese adolescents: the Role of Teacher Emotional Empathy. Int Educ Stud. 2012;5(3):113–25. [Google Scholar]
- 41.Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional attention, clarity, and repair: Exploring emotional intelligence using the Trait Meta-Mood Scale. 1995.
- 42.Fernández-Berrocal P, Extremera N, Ramos N. Validity and reliability of the Spanish modified version of the Trait Meta-Mood Scale. Psychol Rep. 2004;94(3):751–5. [DOI] [PubMed] [Google Scholar]
- 43.Li C, Yan J, Yin X, Wu Z. A primary study of the application of the Trait Meta-Mood Scale in military medical students. Chin J Clin Psychol. 2002.
- 44.Wen Z, Ye B. Analyses of mediating effects: the development of methods and models. Adv Psychol Sci. 2014;22(5):731. [Google Scholar]
- 45.Sun Y, Li X, Liu H, Li X, Sun L, Zhang L, Wang C, Li J, Liu M, Zhang D. PTSD prevalence and factors in intern nursing students after COVID-19 full liberalization in China: a cross-sectional study. Front Public Health. 2024;12:1374977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang B, Bragazzi NL, Li Q, Tang S, Xiao Y, Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect Dis Model. 2020;5:248–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phillipson J, Gorton M, Turner R, Shucksmith M, Aitken-McDermott K, Areal F, Cowie P, Hubbard C, Maioli S, McAreavey R. The COVID-19 pandemic and its implications for rural economies. Sustainability. 2020;12(10):3973. [Google Scholar]
- 48.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Larrabee Sonderlund A, Wehberg S, Assing Hvidt E. Exploring the link between empathy, stress, altruism, and loneliness in university students during the COVID-19 pandemic: a cross‐sectional study. Brain Behav. 2024;14(9):e70049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vučinić V, Stanimirovic D, Gligorović M, Jablan B, Marinović M. Stress and empathy in teachers at general and special education schools. Int J Disabil Dev Ed. 2022;69(2):533–49. [Google Scholar]
- 52.Salerno N, Urquijo S. Emotional Empathy and Its Relationship with Perceived Stress. 2024.
- 53.Chikovani G, Babuadze L, Iashvili N, Gvalia T, Surguladze S. Empathy costs: negative emotional bias in high empathisers. Psychiatry Res. 2015;229(1–2):340–6. [DOI] [PubMed] [Google Scholar]
- 54.Fowler K, Wholeben M. COVID-19: outcomes for trauma-impacted nurses and nursing students. Nurse Educ Today. 2020;93:104525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Atta MHR, Hammad HA-H, Elzohairy NW. The role of Empathy in the relationship between emotional support and caring behavior towards patients among intern nursing students. BMC Nurs. 2024;23(1):443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oh E-j, Lee MH, Ko SH. Influence of emotional intelligence and empathy on the facilitative communication ability of psychiatric nurses. J Korean Acad Psychiatr Ment Health Nurs. 2016;25(4):283–93. [Google Scholar]
- 57.Nam J-H, Park H-S. The impacts of perceived stress and empathy ability on altruistic behavior of freshman nursing students. J Korea Academia-Industrial Cooperation Soc. 2018;19(11):653–61. [Google Scholar]
- 58.Montero ES, Morales-Rodríguez FM. Evaluation of anxiety, suicidal risk, daily stress, empathy, perceived emotional intelligence, and coping strategies in a sample of Spanish undergraduates. Int J Environ Res Public Health. 2021;18(4):1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sun R, Vuillier L, Hui BP, Kogan A. Caring helps: trait empathy is related to better coping strategies and differs in the poor versus the rich. PLoS ONE. 2019;14(3):e0213142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173. [DOI] [PubMed] [Google Scholar]
- 62.Thompson NM, Van Reekum CM, Chakrabarti B. Cognitive and affective empathy relate differentially to emotion regulation. Affect Sci. 2022;3(1):118–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Soni R, Agrawal JP, Meena M, Dave L, Sahu S. Emotional intelligence, coping strategies, and perceived stress among doctors during SARS-CoV-2 pandemic. J Ment Health Hum Be. 2023;28(1):37–41. [Google Scholar]
- 64.Fredrickson BL. Positive emotions broaden and build. In: Adv Exp Soc Psychol. 2013: 1–53.
- 65.Štiglic G, Cilar L, Novak Ž, Vrbnjak D, Stenhouse R, Snowden A, Pajnkihar M. Emotional intelligence among nursing students: findings from a cross-sectional study. Nurse Educ Today. 2018;66:33–8. [DOI] [PubMed] [Google Scholar]
- 66.Higgs M, Dulewicz V, Higgs M, Dulewicz V. Can Emotional Intelligence be developed? Int J Hum Resourc Manag. 2016:51–73.
- 67.Ahmed I, Hamzah AB, Abdullah MNLYB. Effect of Social and Emotional Learning Approach on Students’ Social-Emotional competence. Int J Instr. 2020;13(4):663–76. [Google Scholar]
- 68.Shahbazi S, Heidari M, Sureshjani EH, Rezaei P. Effects of problem-solving skill training on emotional intelligence of nursing students: an experimental study. J Educ Health Promot. 2018, 7. [DOI] [PMC free article] [PubMed]
- 69.Jiménez-Picón N, Romero-Martín M, Ponce-Blandón JA, Ramirez-Baena L, Palomo-Lara JC, Gómez-Salgado J. The relationship between mindfulness and emotional intelligence as a protective factor for healthcare professionals: systematic review. Int J Environ Res Public Health. 2021;18(10):5491. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.