Abstract
Aim
This study aimed to determine adherence with follow‐up from the New Zealand pre‐school vision screening programme. The study also examined associations between pre‐school vision screening outcomes and cognitive measures assessed at the 54‐month follow‐up in the Growing Up in New Zealand study cohort.
Methods
A cross‐sectional retrospective record review of pre‐school vision screening outcomes and hospital ophthalmology records with linkage to Growing Up in New Zealand cohort study data.
Results
Of 176 children referred from vision screening, 21.6% did not attend a referral appointment. Of 138 children who attended a referral appointment, 21.0% did not attend one or more follow‐up appointments. Ethnic differences were observed in attendance at referral appointments (attended Māori 13%, Pacific 22.5%, European/Other 64.5%; not attended Māori 26.3%, Pacific 28.9%, European/Other 44.7%; P = 0.04) and follow‐up appointments (attended Māori 11.9%, Pacific 15.6%, European/Other 72.5%; not attended Māori 17.2%, Pacific 48.3%, European/Other 34.5%; P = 0.001). Vision screening outcome was significantly associated with letter naming fluency scores (P = 0.01) but not name and numbers scores (P = 0.05).
Conclusions
Non‐attendance at referral and follow‐up appointments limits the efficacy of vision screening, particularly for children of Māori and Pacific ethnicity. Children referred from vision screening achieve lower scores on letter naming fluency, a key predictor of reading ability in later childhood. Equity‐based improvements are required to ensure that all children referred from vision screening receive appropriate follow‐up eye care.
Keywords: child, education, ethnic groups, pre‐school, socio‐economic factors, vision screening
What is already known on this topic
Vision screening is important for the early detection of childhood vision conditions.
Pre‐school vision screening coverage in New Zealand is high.
Uncorrected vision conditions are associated with reduced academic outcomes.
What this paper adds
Following vision screening, 21.6% of children did not attend a referral appointment and among children who did attend a referral appointment, a further 21.0% failed to attend one or more follow‐up appointments.
Non‐attendance at both referral and follow‐up appointments occurred more frequently for Māori and Pacific children compared with children of other ethnic groups.
Children who were referred from vision screening achieved lower scores on letter naming fluency compared with those who passed vision screening.
Failure to detect and treat vision problems during childhood may result in permanent vision loss. 1 In addition, uncorrected vision conditions are associated with poorer academic outcomes. 2 Therefore, vision screening during childhood is important for detecting vision problems, particularly as children frequently do not report symptoms caused by impaired vision. 3
Children living in areas with greater socio‐economic disadvantage are less likely to see an eye care professional than those from more advantaged areas. 4 In Aotearoa New Zealand (NZ), children of Māori and Pacific ethnicity more frequently live in areas of socio‐economic disadvantage than children from other ethnic groups. 5
As part of the B4 School Check (B4SC) nationwide well‐child check, children in NZ receive a publicly funded vision screening at 4–5 years of age. 6 The B4SC and subsequent referral processes are administered independently in each of the country's 20 District Health Boards (DHBs).
Counties Manukau DHB has a higher proportion of children compared to the overall NZ population, and is the DHB with the largest Pacific population and second largest Māori population. 7 In addition, a large proportion of children in Counties Manukau DHB live in areas of socio‐economic deprivation. 7 In the Counties Manukau DHB area, all children who fail the B4SC vision screening are referred to the hospital eye department for publicly‐funded eye care services. In other DHBs, some children who are referred for vision screening receive a recommendation to see their local optometrist.
Previous research has shown inequities in attendance at vision screening by socio‐economic status and ethnic group. 8 However, there are currently no published data on socio‐economic and ethnic disparities in adherence with follow‐up from vision screening in NZ.
Growing Up in New Zealand is a large multidisciplinary prospective study investigating health, education and social outcomes in a cohort of 6853 NZ children who were born in 2009 and 2010. 9 Determining vision screening outcomes for the children enrolled in this cohort study provides a unique opportunity to examine these screening results in the context of the NZ health‐care system and the social and cognitive measures that were assessed as a component of the cohort study.
Therefore, the aims of this study were to:
Examine adherence with recommended follow‐up after B4SC vision screening by children enrolled in the Growing Up in New Zealand cohort study and residing in the Counties Manukau DHB area.
Assess the associations of B4SC vision screening check outcomes with measures of school readiness and early literacy at approximately 4 years of age.
Methods
Data source and study sample
A retrospective record review of the B4SC vision screening results was undertaken for children from the Growing Up in New Zealand study whose parents had provided consent for this data linkage. The review was restricted to participants who were living in the Counties Manukau DHB catchment area at the time of screening (n = 1879).
Measures
Data obtained from the Growing Up in New Zealand B4SC dataset included ethnicity (classified as per NZ Statistics level 1), 10 and B4SC vision screening outcome.
The B4SC vision screening comprises measurement of uniocular unaided visual acuity (VA) using the Parr vision test, 11 a single, crowded, letter matching task, at a distance of 4 m. Children with reduced VA or who are unable to complete vision screening are referred for further eye care. Possible B4SC vision screening outcomes were: ‘Pass’, ‘Rescreen’, ‘Refer’ ‘Under care [of an eye care professional]’ or ‘Decline [to participate in B4SC vision screening]’. Children who had been categorised as ‘Decline’ (n = 40), ‘Under care’ (n = 41) or ‘Rescreen’ (n = 41), or whose date of birth was not valid for a Growing Up in New Zealand participant (n < 10) were excluded from data analysis.
For children who were referred from the vision screening, hospital eye department records were used to collate information on cycloplegic refraction, visual diagnoses and the number of attended and non‐attended appointments.
Data obtained from the Growing Up in New Zealand 54‐month follow‐up included the NZDep2013 Index of Deprivation (an area‐based measure of socio‐economic deprivation), 12 and scores from two cognitive tasks; ‘Name and Numbers’ and ‘Letter Naming Fluency’. NZDep2013 deciles were categorised as low (deciles 1–3), moderate (deciles 4–7) or high (deciles 8–10) deprivation.
The Name and Numbers task comprised four parts. Two tasks, name and number writing, were adopted from the ‘Who Am I?’ developmental assessment and scored according to the standard scoring manual. 13 Additionally, children were asked to count aloud from 1 to 10 and then backwards from 10 to 1. The counting tasks were scored as the number of correct digits in the longest sequence given by the child. A total score (ranging from 0 to 28) was calculated by summing the individual scores for each task.
The Letter Naming Fluency task from the Dynamic Indicators of Basic Early Literacy tools was administered and scored according to the instructions in the manual. Children were presented with a page of randomly ordered uppercase and lowercase letters and using standardised directions, asked to name the letters. The total score (ranging from 0 to 110) was the number of letters correctly named in 1 min. 14
Definitions for visual outcomes
Refractive error was classified using cycloplegic refraction and defined according to the Refractive Error Studies in Children group. 15 Amblyopia risk factors were defined according to the American Academy of Ophthalmology (Table 1). 1
Table 1.
Definitions for significant refractive error and amblyopia risk factors
| Vision condition | Definition |
|---|---|
| Refractive error | |
| Myopia† | ≤−0.50 D |
| Hyperopia† | ≥+2.00 D |
| Astigmatism | ≥0.75 D |
| Amblyopia risk factors | |
| Visual pathway obstruction | Visual pathway obstruction present |
| Strabismus | Any manifest deviation |
| Anisometropia | |
| Myopia† | ≥2.50 D |
| Hyperopia† | ≥1.50 D |
| Astigmatism | ≥1.50 D in any meridian |
| Bilateral refractive error | |
| Myopia† | ≤−2.50 D |
| Hyperopia† | ≥3.50 D |
| Astigmatism | ≥1.50 D |
Spherical equivalent.
D, Dioptres.
Data analysis
Data analysis was conducted using IBM SPSS Statistics (Version 26, IBM Corporation, USA). A two‐tailed P < 0.05 was considered statistically significant. Descriptive statistics were used to summarise the data using counts and percentages (for categorical variables) or medians and interquartile ranges (IQRs; for non‐parametric variables). Owing to study ethical requirements, ‘<10’ denotes categories with fewer than 10 participants.
Among children who were referred (n = 176) from vision screening, the chi‐squared test was used to assess ethnic and socio‐economic differences in the proportion of children who attended a referral appointment versus those who did not and, of those who attended a referral appointment (n = 138), children who failed to attend follow‐up appointments versus those who had no unattended appointments.
The Mann–Whitney U test was used to examine whether the distribution of Name and Numbers total test scores and Letter Naming Fluency scores differed between children who were referred and those who passed vision screening. Using median‐splits for Name and Numbers total test scores and Letter Naming Fluency scores as dependent variables (dichotomous variable indicating scores above vs. below or equal to the median), separate logistic regression models examined whether children who were referred from vision screening were less likely to achieve scores above the median value. These models adjusted for the following potential confounding variables: child's birthweight, sex, ethnicity and area‐level socio‐economic deprivation. The results were summarised using adjusted odds ratios (aORs) and their 95% confidence intervals (CIs).
Results
Study sample
The characteristics of the study population are shown in Table 2. The 1847 participants (51% male, 43% European ethnicity) had a median (IQR) age of 4.24 (4.13–4.44) years. Of these, 1763 participants completed vision screening with a ‘Pass’ or ‘Refer’ outcome.
Table 2.
Characteristics of participants from the Growing Up in New Zealand study living in the Counties Manukau region at 4 years of age
| Characteristic | n (%) (n = 1847) |
|---|---|
| Age (median (IQR)), years | 4.24 (4.13–4.44) |
| Sex | |
| Female | 900 (48.7) |
| Male | 947 (51.3) |
| Child ethnicity | |
| Māori | 301 (16.3) |
| Pacific | 460 (24.9) |
| European | 795 (43.0) |
| Other | 291 (15.8) |
| Socioeconomic deprivation† | |
| Deciles 1–3 (low) | 502 (27.2) |
| Deciles 4–7 (moderate) | 510 (27.6) |
| Deciles 8–10 (high) | 830 (44.9) |
| Unknown | <10 (0.3) |
Deciles based on NZDep2013 scores. Decile 1 households are located in the least deprived 10% of meshblocks and decile 10 households are located in the most deprived 10% of meshblocks.
IQR, interquartile range.
Attendance at referral appointments and follow‐up appointments
Of the 1847 participants, 176 (9.5%) were referred for vision screening (Māori 15.9%, Pacific 23.9%, European/Other 60.2%). Thirty‐eight of these children (21.6%) did not attend a referral appointment at the hospital eye department (Fig. 1). Among children who attended a referral appointment, 21.0% (29/138) failed to attend one or more follow‐up appointments.
Fig. 1.
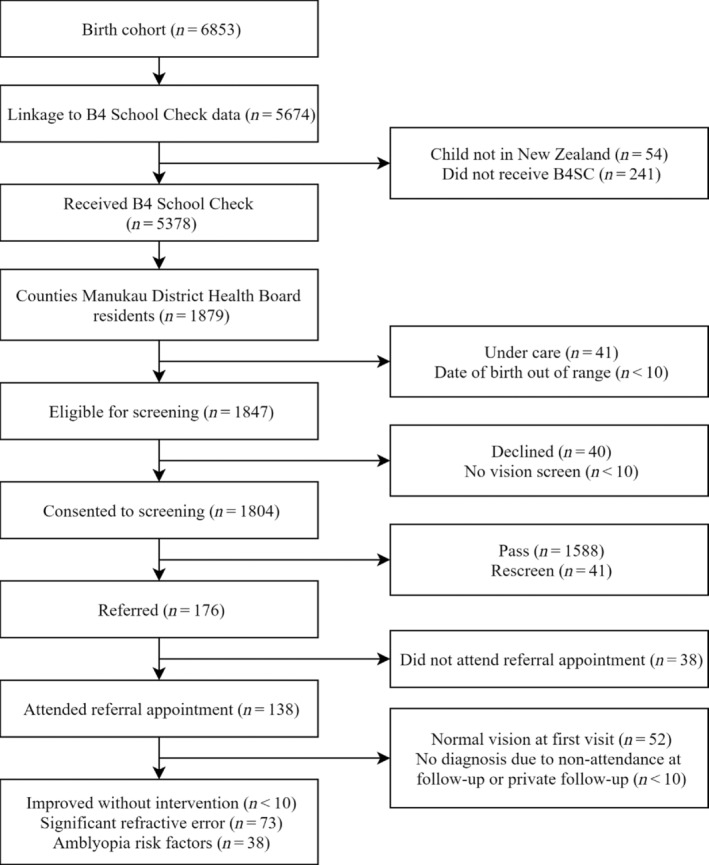
Flow diagram of vision screening eligibility, consent, referral and outcome for children enrolled in the Growing Up in New Zealand study and residing in the Counties Manukau District Health Board region.
Among those referred for comprehensive eye examinations, there were significant differences between ethnic groups in attendance at referral appointments and follow‐up appointments (Fig. 2). Compared with children who attended referral appointments, a larger proportion of those who did not attend referral appointments were of Māori or Pacific ethnicities (attended Māori 13.0%, Pacific 22.5%, European/Other 64.5%; not attended Māori 26.3%, Pacific 28.9%, European/Other 44.7%; P = 0.04). Furthermore, compared to children who attended all follow‐up appointments, a larger proportion of those who did not attend at least one follow‐up appointment were of Māori or Pacific ethnicities (attended Māori 11.9%, Pacific 15.6%, European/Other 72.5%; not attended Māori 17.2%, Pacific 48.3%, European/Other 34.5%; P = 0.001). In contrast, there were no significant differences in attendance at referral or follow‐up appointments by area‐level socio‐economic deprivation (Fig. 3).
Fig. 2.
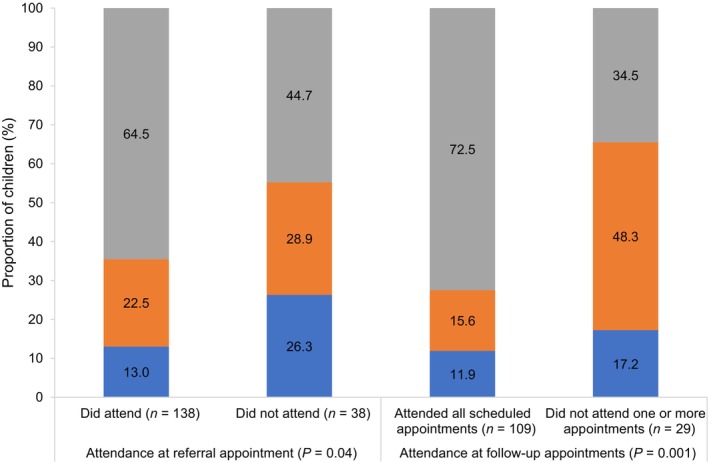
Attendance at referral appointments and follow‐up appointments by child ethnicity. ( ) Māori; (
) Māori; ( ) Pacific; (
) Pacific; ( ) European/Other.
) European/Other.
Fig. 3.
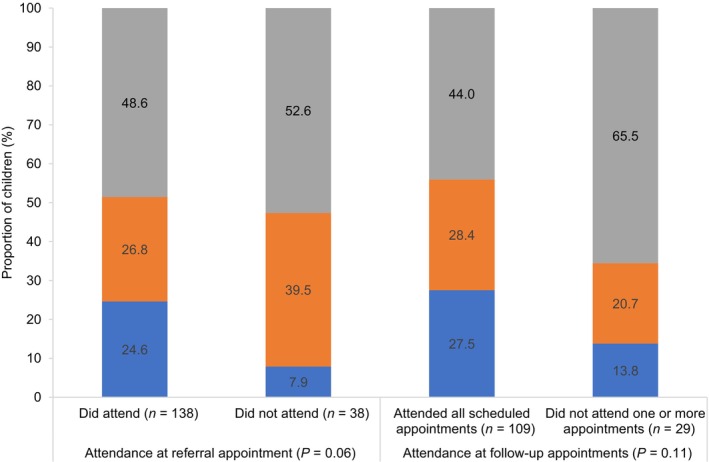
Attendance at referral appointments and follow‐up appointments by area‐level socio‐economic deprivation of household where child lives. ( ) Deciles 1–3 (low); (
) Deciles 1–3 (low); ( ) Deciles 4–7 (moderate); (
) Deciles 4–7 (moderate); ( ) Deciles 8–10 (high).
) Deciles 8–10 (high).
Visual outcomes
Among the 138 children who attended the hospital for a referral appointment, 76 children had a diagnosed vision condition (Table 3). Significant refractive error and amblyopia risk factors were detected in 73 out of 138 (52.9%) and 38 out of 138 (27.5%) children, respectively.
Table 3.
Vision conditions of children who attended a referral appointment
| Vision conditions | n (%) (n = 138) |
|---|---|
| Refractive error† | |
| Myopia | 16 (11.6) |
| Hyperopia | 36 (26.1) |
| Astigmatism | 49 (35.5) |
| Any refractive error | 73 (52.9) |
| Amblyopia risk factors‡ | 38 (27.5) |
| No ocular condition | 58 (42.0) |
| No diagnosis made§ | <10 (2.9) |
Fourteen children had both myopia and astigmatism and 14 had both hyperopia and astigmatism.
Thirty‐five children had both refractive error and amblyopia risk factors.
No diagnosis made due to follow‐up with private provider or non‐attendance at follow‐up appointment.
Cognitive outcomes
Among the 1763 children with a ‘Pass’ or ‘Refer’ vision screening outcome, 1708 (96.9%) and 1633 (92.6%) completed the Name and Numbers and Letter Naming Fluency tasks, respectively. For both tasks, the median values of the participants' total scores were significantly lower for children who were referred from the B4SC vision screening compared with those who passed the B4SC vision screening (Table 4). In the logistic regression analysis, the B4SC vision screening outcome was significantly associated with Letter Naming Fluency scores (P = 0.01) but not Name and Numbers total test scores (P = 0.05) (Table 5). The adjusted analysis showed that compared to children who passed vision screening, those who were referred from screening were less likely to achieve scores above the median value on the Letter Naming Fluency task (aOR = 0.61; 95% CI = 0.43–0.88).
Table 4.
Name and Numbers and Letter Naming Fluency scores by B4SC outcome
| Name and Numbers scores | Letter Naming Fluency scores | |||||
|---|---|---|---|---|---|---|
| n (%) | Median | P value | n (%) | Median | P value | |
| (n = 1708) | (IQR) | (n = 1633) | (IQR) | |||
| B4SC vision screening outcome | ||||||
| Passed | 1535 (89.9) | 17 (13–23) | 0.001 | 1473 (90.2) | 4 (1.0–12.0) | 0.02 |
| Referred | 173 (10.1) | 15 (9–20) | 160 (9.8) | 2 (0.0–7.8) | ||
B4SC, B4 School Check; IQR, interquartile range.
Table 5.
Logistic regression analysis of measures of school readiness and early literacy at 4 years of age in relation to the B4 School Check (B4SC) vision screening outcome
| Name and Numbers total scores | Letter Naming Fluency total scores | |||||||
|---|---|---|---|---|---|---|---|---|
| ≤Median (≤17) | >Median (>17) | Adjusted† OR‡ (95% CI) | P value | ≤Median (≤3) | >Median (>3) | Adjusted† OR‡ (95% CI) | P value | |
| n (%) | n (%) | n (%) | n (%) | |||||
| B4SC vision screening outcome | ||||||||
| Passed | 845 (88.4) | 690 (91.8) | Reference | 732 (88.4) | 741 (92.0) | Reference | ||
| Referred | 111 (11.6) | 62 (8.2) | 0.71 (0.51–1.00) | 0.05 | 96 (11.6) | 64 (8.0) | 0.61 (0.43–0.88) | 0.01 |
Adjusted for child's birthweight, sex, ethnicity and area‐level socio‐economic deprivation.
Logistic regression analysis modelling the probability that total scores (separate models) are above the median value.
CI, confidence interval; OR, odds ratio.
Discussion
While this study shows that the B4SC vision screening programme in NZ identifies children at risk of eye conditions; one in five children in this study who were referred for further eye care did not attend a referral appointment. A further one in five children who attended a referral appointment then failed to attend one or more follow‐up appointments. Non‐attendance occurred more frequently for Māori and Pacific children compared with children from other ethnic groups. Furthermore, children who were referred from pre‐school vision screening achieved lower scores on Letter Naming Fluency, than those children who passed vision screening, underlining the importance of vision screening follow‐up.
Similar to the results of the present study, a previous study of children seen at Counties Manukau DHB found that 80% of children referred from B4SC vision screening were seen at the hospital eye department. 16 In contrast, a study in Tairāwhiti and Southland DHBs was only able to obtain follow‐up results for half of the children referred following vision screening. 17 The contrast in findings by Muller et al. 17 could be because it relied on voluntary participation by community optometrists and may have underestimated the follow‐up care received, and/or may reflect differences in referral pathways between DHBs.
Although eye care within the public health system is at no direct cost to the family/whānau, barriers to accessing care remain. Inability to book an appointment at a suitable time, lack of transport, and parents not having time to take their child to the doctor were identified as barriers to accessing primary care within the Growing Up in New Zealand cohort, 9 and are likely to also affect the ability of parents to access eye care services for their children. Cultural factors including institutional and personal racism, and language barriers may also influence access to health‐care services. 5 Further research is required to determine the barriers to attendance at hospital appointments, and to develop strategies for improving access to eye care services for these families. Such research should be developed with a Kaupapa Māori approach to ensure improvement in Māori health and a reduction in health inequities. 18
In the present study, children who were referred from vision screening achieved poorer results on the Letter Naming Fluency task, compared with those who passed the B4SC vision screen. These findings suggest that children who are referred from pre‐school vision screening in NZ are at risk of poor literacy development. Previous studies have found that pre‐school‐aged children with reduced VA, uncorrected hyperopia, or astigmatism have lower scores on tests of early literacy compared with children with normal VA and no refractive error. 2 Children in NZ living in areas of higher socio‐economic deprivation, and those of Māori and Pacific ethnicities, are more likely to have poorer academic outcomes than their peers. 19 Thus, detection and correction of vision problems that may affect academic performance is particularly important for these children to prevent further disadvantage.
While children who were referred from vision screening had lower median scores on the Name and Numbers task, compared with those who passed the screening, this was not significant in the adjusted model. The Letter Naming Fluency task involved recognition of written letters, whereas the Name and Numbers task required written and verbal responses to verbal instructions. Additionally, while the Name and Numbers test included tasks derived from the ‘Who Am I?’ standardised test, the complete test was not administered in the Growing Up in New Zealand study. It is unclear how these modifications affect the ability of the test to discriminate between children with age‐appropriate and delayed school readiness skills.
Limitations of the present study include its retrospective nature, and only including the referral results of those children who were referred from the screening and received follow‐up care in Counties Manukau DHB. Due to differences in referral pathways and demographics between DHBs, the generalisability of the results to the remainder of NZ may be limited. The study design also did not allow for assessment of access for eye care from community and private providers; however, recorded reasons for non‐attendance suggest that less than 10% of children received eye care elsewhere. The retrospective nature of the study means that the cause of lower cognitive scores in children who were referred from vision screening cannot be determined. The lower cognitive scores may be the result of uncorrected vision problems or cognitive issues that may have resulted in the vision screening failure.
While the Growing Up in New Zealand cohort was powered based on overall developmental outcomes, the present study included only a subset of the data collected. Therefore, it is possible that the sample size was insufficient to detect significant differences. Therefore, studies with larger samples are required to confirm these results.
Conclusion
Pre‐school vision screening in NZ identifies children with reduced VA from uncorrected refractive error and with amblyopia risk factors, resulting in diagnosis and treatment for these children. However, non‐attendance at hospital appointments limits the efficacy of the screening programme, particularly for children of Māori and Pacific ethnicity. Children who are referred from vision screening have lower scores on letter naming fluency, which may have implications in terms of school readiness and acquisition of early literacy skills. Further research is required to determine additional support required to improve access to eye care. Equity‐based improvements are required to ensure that all children receive vision screening and appropriate follow‐up eye care.
Ethics Statement
Ethical approval for the Growing Up in New Zealand cohort study was obtained from the Northern Y Health and Disability Ethics Committee of the New Zealand Ministry of Health (Reference number: NTY/08/06/055). The research followed the tenets of the Declaration of Helsinki. Approval for this research was also obtained from the Counties Manukau DHB Research Office and the Growing Up in New Zealand study's Data Access Committee.
Acknowledgements
This project was supported with funding from the SJ Taylor Grant, School of Medicine Foundation, University of Auckland, the New Zealand Association of Optometrists and a Senior Health Research Scholarship from the University of Auckland. Recruitment and data collection in the Growing Up in New Zealand cohort study has been funded (grants‐in‐aid) by the New Zealand Government, Health Research Council, University of Auckland and Auckland UniServices Limited. Open access publishing facilitated by The University of Auckland, as part of the Wiley ‐ The University of Auckland agreement via the Council of Australian University Librarians.
Conflict of interest: None declared.
References
- 1. Holmes JM, Clarke MP. Amblyopia. Lancet 2006; 367: 1343–1351. [DOI] [PubMed] [Google Scholar]
- 2. Hopkins S, Narayanasamy S, Vincent SJ, Sampson GP, Wood JM. Do reduced visual acuity and refractive error affect classroom performance? Clin. Exp. Optom. 2019; 103: 278–289. [DOI] [PubMed] [Google Scholar]
- 3. Irving EL, Harris JD, Machan CM et al. Value of routine eye examinations in asymptomatic patients. Optom. Vis. Sci. 2016; 93: 660–666. [DOI] [PubMed] [Google Scholar]
- 4. Majeed M, Williams C, Northstone K, Ben‐Shlomo Y. Are there inequities in the utilisation of childhood eye‐care services in relation to socio‐economic status? Evidence from the ALSPAC cohort. Br. J. Ophthalmol. 2008; 92: 965–969. [DOI] [PubMed] [Google Scholar]
- 5. Paine SJ, Harris R, Stanley J, Cormack D. Caregiver experiences of racism and child healthcare utilisation: Cross‐sectional analysis from New Zealand. Arch. Dis. Child. 2018; 103: 873–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ministry of Health . Well Child/Tamariki Ora Programme Practitioner Handbook: Supporting Families and whānau to Promote their child's Health and Development. Revised 2014 ed. Wellington: Ministry of Health; 2014.
- 7. Winnard D, Lee M, Macleod G. Demographic Profile: 2013 Census, Population of Counties Manukau. Auckland; 2015.
- 8. Findlay R, Hamm L, Anstice N et al. Vision screening in New Zealand preschool children: Is it equitable? J. Paediatr. Child Health 2021; 57: 1594–1599. [DOI] [PubMed] [Google Scholar]
- 9. Morton S, Grant C, Berry SD et al. Growing up in New Zealand: A Longitudinal Study of New Zealand Children and their Families. Now we Are Four: Describing the Preschool Years. Growing Up in New Zealand: Auckland; 2017. [Google Scholar]
- 10. Statistics New Zealand . Ethnicity Standard Classification 2005; 2005. Available from URL: http://infoshare.stats.govt.nz/methods/classifications-and-standards/classification-related-stats-standards/ethnicity.aspx#gsc.tab=0. Accessed Web Page 2019.
- 11. Parr JC. Clinical assessment of visual acuity. Trans. Ophthalmol. Soc. N. Z. 1981; 33: 157–167. [PubMed] [Google Scholar]
- 12. Atkinson J, Salmond C, Crampton P. NZDep2013 Index of Deprivation. Wellington: Department of Public Health, University of Otago; 2014. [Google Scholar]
- 13. Rothman S. Report on Adapted PPVT‐III and Who Am I. Growing Up in Australia: The Longitudinal Study of Australian Children; 2005.
- 14. Good RH III, Kaminski RA. Assessment Manual. Dynamic Measurement Group Inc; 2011.
- 15. Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive error study in children: Sampling and measurement methods for a multi‐country survey. Am. J. Ophthalmol. 2000; 129: 421–426. [DOI] [PubMed] [Google Scholar]
- 16. Langeslag‐Smith MA, Vandal AC, Briane V, Thompson B, Anstice NS. Preschool children's vision screening in New Zealand: A retrospective evaluation of referral accuracy. BMJ Open 2015; 5: e009207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Muller W, Mitchell L, Wilson G. Vision screening in New Zealand: An audit of the B4 school check. N. Z. Med. J. 2019; 132: 63–70. [PubMed] [Google Scholar]
- 18. Reid P, Paine SJ, Curtis E et al. Achieving health equity in Aotearoa: Strengthening responsiveness to Māori in health research. N. Z. Med. J. 2017; 130: 96–103. [PubMed] [Google Scholar]
- 19. Marriott L, Sim D. Indicators of inequality for Māori and Pacific people. J. N. Z. Stud. 2015; 20: 24–50. [Google Scholar]


