Abstract
Background
The adoption of integrated curricula in medical schools has grown globally, emphasizing the need to understand academic medical staff satisfaction as a crucial factor influencing successful implementation.
Aim
This study aimed to assess satisfaction levels among academic medical staff with integrated medical curricula, identifying socio-demographic and work-related predictors of dissatisfaction.
Methods
A cross-sectional, online multinational survey was conducted from December 2023 to April 2024 among 525 academic medical staff. A structured, self-reported questionnaire was used to assess satisfaction levels, demographic characteristics, and work-related factors. The data were analyzed using descriptive and inferential statistics, including logistic regression analysis, to identify predictors of dissatisfaction.
Results
The study revealed a low satisfaction rate (44.2%) among medical staff, with significant dissatisfaction influenced by nationality (Jordanian: OR = 7.74, and Egyptian: OR = 4.68), male gender (OR = 3.27), over ten years of teaching experience in integrated curricula (OR = 4.25), and employment in governmental universities (OR = 4.23). Dissatisfaction was particularly high with aspects such as the integration of basic and clinical sciences, assessment methods, and implementation schedules. Faculty from private universities demonstrated significantly higher satisfaction (65.1%) compared to those in governmental institutions (41.3%). Younger staff < 45 years reported higher satisfaction rates (50.9%) compared to their older counterparts ≥ 45 years (39.1%), reflecting greater adaptability to curriculum changes.
Conclusions
The findings highlight substantial dissatisfaction among academic medical staff with the design and implementation of integrated curricula, particularly in governmental institutions and among senior faculty. Institutions must address challenges in curriculum design, resource allocation, and faculty support to enhance satisfaction. Revisiting conventional curriculum components or adopting a hybrid approach may help balance innovation with faculty preferences, fostering a more conducive educational environment.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06468-x.
Keywords: Medical staff, Satisfaction, Integrated medical curriculum, Conventional medical curriculum, Exploratory multinational survey
Introduction
Medical schools around the world have faced significant changes in their curricula where the integrated curriculum becoming increasingly popular worldwide to bridge the gap between basic and clinical sciences with promoting early clinical exposure and ongoing integration of biomedical and clinical sciences. Integration was defined as the organization of teaching material to interrelate or unify subjects frequently taught in separate academic courses or departments. This organization can take place across a spectrum of time periods or depths both within and among subjects along an integration ladder. The relevant curriculum models included are horizontal (integration across disciplines), vertical (integration across time), and spiral which is the ideal form with integration across time and disciplines [1].
Concerning the issue of integration, some researchers described integration in curriculum reform as a cyclizing issue. It refers to the recurring nature of discussions and debates surrounding curriculum integration without significant progress in implementation. This pattern has been observed by researchers like Hopkins et al. (2015), who highlight that despite repeated recommendations and discussions in medical education, no substantial changes have emerged. The focus tends to be on altering the curricular structure rather than addressing the specific learning needs of the medical education community. This misalignment between structural changes and the practical educational needs of educators and students contributes to the ongoing struggle with successful integration. Hopkins and colleagues argue that medical educators from different disciplines might aim for diverse learning outcomes, which complicates the implementation of an integrated curriculum. The persistent challenge lies in the fact that structural reforms fail to engage with the individual learning goals of medical educators, leading to a sense of “change without difference” in medical curriculum reforms [2]. Also, Muller et al., 2008 discuss this cyclizing issue and how the process of integrating medical school curricula often involves repetitive cycles of discussion and recommendation without meaningful, lasting change. The authors explain that while the idea of integration continues to be revisited, the focus frequently remains on structural adjustments rather than on the deeper, more nuanced challenges faced by educators and students in achieving genuine integration across disciplines. It was emphasized that this repeated revisiting of curriculum reform often results in what is termed “integration without transformation,” where the changes implemented fail to address the root educational needs of medical faculty and students [3]. Thus, despite its extensive global adoption in many medical schools, the benefits of the integrated curriculum over the traditional one have not been conclusively confirmed [4].
Pedagogical strategies, methods and practices of teaching are crucial for translating structural innovations into meaningful learning experiences. These approaches determine how content is delivered, how students interact with the material, and how feedback is provided. One meta-analysis shows that formative feedback, active learning, and student engagement strategies are powerful tools in enhancing student performance, often surpassing the direct benefits of infrastructural changes alone [5]. Structural reforms and pedagogical approaches must ultimately align to support the achievement of clear learning outcomes as noted by Biggs, 2003 who found that teaching methods and assessment tasks are aligned with the desired learning outcomes, and this is a powerful framework for achieving educational effectiveness. Without a focus on learning outcomes, structural changes run the risk of being superficial improvements that do not address the deeper goals of education [6].
The transition to such curriculum forms represents a significant shift from traditional, and discipline-based approaches, which necessitates a thorough evaluation of faculty perceptions and satisfaction to ensure successful implementation and ongoing improvement. The satisfaction of academic medical staff with integrated medical curricula is a crucial aspect of medical education that has garnered increasing attention in recent years [3]. Academic medical staff play a pivotal role in the delivery and success of integrated curricula. Their satisfaction is linked to various factors including curriculum design, teaching workload, administrative support, and professional development opportunities. Studies have indicated that when faculty members are satisfied with the curriculum, they are more likely to be committed to teaching, mentoring, and continuous curriculum development [7].
This study aimed to explore satisfaction with the integrated medical curriculum and its associated socio-demographic and work characteristics among academic medical staff. Unfortunately, despite the widespread global adoption of integrated medical curricula, there remains a significant gap in understanding the satisfaction levels of academic medical staff, particularly in diverse multinational contexts. Addressing faculty satisfaction is crucial because educators play a pivotal role in the successful implementation of any curriculum reform. Their perceptions directly impact curriculum delivery, student outcomes, and the overall success of educational programs. Furthermore, there is limited published data on this subject, especially in regions where the integrated curriculum is relatively new or where faculty have had substantial experience with traditional curricula. By exploring the satisfaction levels of academic medical staff and identifying predictors of dissatisfaction, this study can inform necessary adjustments to curriculum design and implementation, ultimately contributing to the advancement of medical education. Conducting this research not only addresses a critical knowledge gap but also provides actionable insights for improving curriculum strategies that align with the needs of both faculty and students in diverse settings.
Methods
Study design and setting
An online multinational survey was conducted during the academic year 2023–2024. Data were collected through filling a Google form built from a structured questionnaire. The survey continued over a period of 5 months starting from December 2023 to April 2024.
Study population
The study population was a sample of academic medical staff (525) who were invited to fill the study form. The participation was voluntary through using an online google form. The overall response rate among the invited medical teachers was 67% (525/783). Non-participation was due to lack of interest and incomplete forms. Participation also, may be overlooked if the respondents were not highly invested in curriculum reforms. The main problem always summarized in time constraints as medical educators often face academic demands including teaching, administrative, and research commitments. These time constraints may lead to hesitance in committing to even brief surveys, especially if they require reflective responses or cover multiple curriculum dimensions.
Inclusion and exclusion criteria
Eligible invited persons to this study were academic medical staff of different specialties who were working in different countries, affiliated to both governmental and private medical schools that adopted and applied the integrated curriculum in their universities. The persons who were lacking any of the previous inclusion criteria were excluded from the study.
Sample size calculation
Based on the maximum expected prevalence of medical teachers’ satisfaction with the integrated medical curriculum, it was assumed to be 50%. Using Daniel formula [8]: N = Z2P (1-P)/d2whereas, Z = 1.96 (at 95% confidence level), P = 0.50 (the expected prevalence) and d = 0.05 (the margin of error) thus, the estimated sample size has to be at least 384. In order to overcome the non-responders, we added 15% to the estimated sample size to be finally at least 442.
Study instrument
A structured self-reported online questionnaire was constructed to collect the data. The survey instrument was developed utilizing the literature and informal discussions with many academic medical staff. The content validity was determined by consulting a panel of experts. To ensure reliability, the questionnaire was pre-tested on a pilot sample and modified accordingly. The Cronbach alpha of internal consistency was calculated to be 0.85 for curriculum design subscale, 0.87 for curriculum implementation and 0.92 for the overall satisfaction scale. The questionnaire was finally edited in English version and consisted of 2 main sections: The First Section inquires 8-items on some socio-demographic and work characteristics of the respondents. The Second Section explores satisfaction of medical teachers about some issues related to the integrated curriculum. Satisfaction scale was subdivided into 2 subscales: first is 6 items on satisfaction with curriculum design, second is another 6 items on satisfaction with curriculum implementation (questions’ answers for both subscales were reported on 3-point response: satisfied, unsatisfied, and unknown) [9].
Data management
The collected data were coded, processed and analyzed using Statistical Package of Social Science (SPSS) program version 26. Descriptive statistics were presented as numbers (n), and percentages (%).
Each question in satisfaction scale was scored between 0 (= unsatisfied/unknown) and 1 (satisfied). The overall satisfaction rate was calculated considering the cut of point = 7 which was the median score for the all 12 questions of the satisfaction scale whereas, ˃7 was considered satisfied, and ≤ 7 was unsatisfied.
The association between categorical variables and satisfaction score was tested using Pearson’s chi-square test for Table (2 × 2), while, Monte-Carlo test was used for table (> 2 × 2). Significant variables on univariate analysis entered into Logistic regression model (enter-method) to specify the most significant predictors of staff unsatisfaction with the integrated curriculum. Adjusted odds ratios (AOR) and their 95% confidence interval (CI) were calculated. P-value ≤ 0.05 was considered to be statistically significant.
Results
Table (1) shows the sociodemographic and work characteristics of the studied group which revealed that more than half of them were males (55%) and aged ≥ 45 years (57%). The majority of the studied staff had MD/PhD qualification (83.2%), of Jordanian nationality (43.4%) followed by Egyptian nationality (37.3%). They were largely affiliated to governmental universities (88%). Furthermore, most respondents (54.8% in conventional and 79.4% in integrated curricula) stated that they had more than 10 years of teaching experience. The table also, shows that the overall satisfaction rate among the studied medical teachers was only 44.2% however, 55.8% were unsatisfied. Age illustrated a statistically significant association with satisfaction levels regarding integrated curriculum where, younger staff members (< 45 years) reported higher satisfaction rates (50.9%) compared to their older counterparts (≥ 45 years) who had a satisfaction rate of 39.1% (p = 0.007). The table shows that the unsatisfied group had significantly higher percentage of male teachers (61.9%) compared to higher percentage of female teachers (51.7%) in the satisfied group (p = 0.002). Medical teachers with higher qualification (MD/PhD) expressed more unsatisfaction (56.3%) although, it was statistically non-significant (p = 0.6). Furthermore, among studied staff, Egyptian and Jordanian nationality showed significantly unsatisfaction dominance with integrated system (64.3% and 61.8% respectively) compared to only 25.7% with other nationality (p < 0.001). The result also revealed that staff dissatisfactions with integrated curriculum were more significantly associated with working in governmental institutions (58.7%), and having experience ˃10 years in teaching both old and new curriculum (61.8%, and 60.4% respectively with p < 0.001).
Table 1.
Association between satisfaction score with socio-demographic and some work characteristics of the studied academic medical staff
| Staff characteristics | Total N = 525 | Overall Satisfaction Scorea | p-value | |
|---|---|---|---|---|
| Satisfied n = 232 (44.2%) | Unsatisfied n = 293 (55.8%) | |||
| Age: | ||||
|
< 45 years ≥ 45 years |
226 (43.0) 299 (57.0) |
115 (50.9) 117 (39.1) |
111 (49.1) 182 (60.9) |
0.007* |
| Gender: | ||||
|
Male Female |
289 (55.0) 236 (45.0) |
110 (38.1) 122 (51.7) |
179 (61.9) 114 (48.3) |
0.002* |
| Qualification: | ||||
|
MBBCh M.Sc. MD/PhD |
15 (2.9) 73 (13.9) 437 (83.2) |
7 (46.7) 34 (46.6) 191 (43.7) |
8 (53.3) 39 (53.4) 246 (56.3) |
0.6 |
| Nationality: | ||||
|
Egyptians Jordanians Othersb |
196 (37.3) 228 (43.4) 101 (19.2) |
70 (35.7) 87 (38.2) 75 (74.3) |
126 (64.3) 141 (61.8) 26 (25.7) |
< 0.001* |
| Affiliated university: | ||||
|
Governmental Private |
462 (88.0) 63 (12.0) |
191(41.3) 41 (65.1) |
271 (58.7) 22 (34.9) |
< 0.001* |
| Teaching experience in conventional medical curriculum: | ||||
|
˃10 years ≤10 years |
283 (54.8) 233 (45.2) |
108 (38.2) 124 (53.2) |
175 (61.8) 109 (46.8) |
< 0.001* |
| Teaching experience in integrated medical curriculum: | ||||
|
˃10 years ≤10 years |
417 (79.4) 108 (20.6) |
165 (39.6) 67 (62.0) |
252 (60.4) 41 (38.0) |
< 0.001* |
a: Cut of point = Median = 7 (˃7 = satisfied and ≤ 7 = unsatisfied). *: Statistically significant at p ≤ 0.05
b: Others include Saudis, Americans, Palestinians, Sudanese, and Iraqis
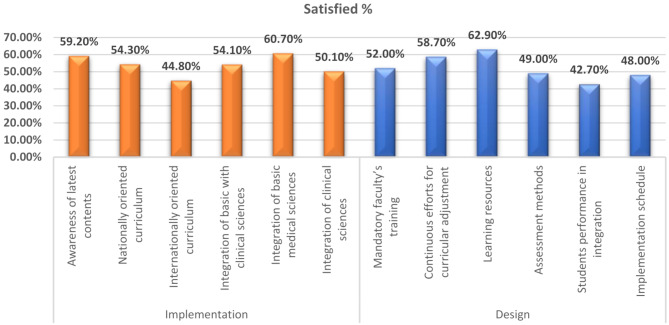
Figure (1) depicts the percentage distribution of self-reported satisfaction levels among academic medical staff regarding the design and implementation of an integrated curriculum. The data reveals a notable split, with a significant portion of the staff expressing varying levels of satisfaction and dissatisfaction. It shows that the lowest satisfaction percentage with curriculum design questions was for the internationally oriented curriculum (44.8%), followed by integration of clinical sciences (50.1%) and integration of basic with clinical sciences (54.1%). However, the lowest satisfaction rate with curriculum implementation questions was for the students’ performance (42.7%) followed by implementation schedule (48%) and assessment methods (49%).
Fig. 1.
Percentage distribution of self-reported satisfaction scale (design & implementation) among the studied academic medical staff
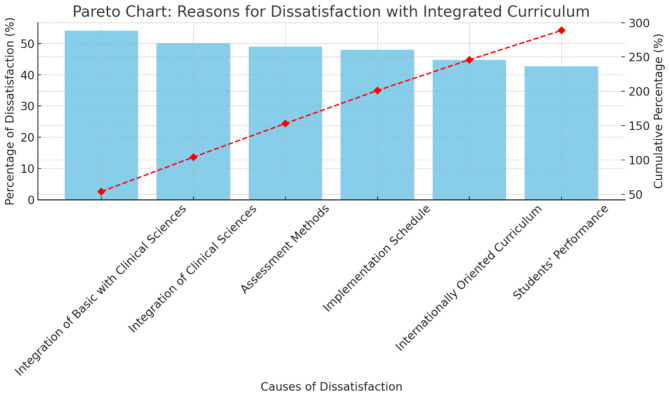
Figure (2) is a Pareto chart that shows the distribution of various causes of dissatisfaction with integrated curriculum among medical staff and highlights their cumulative impact. The chart reveals that integration of basic with clinical sciences and integration of clinical sciences both have the highest percentages of dissatisfaction as each contributing slightly above 50% followed by dissatisfaction with assessment methods and implementation schedule which were around 45–50%. The chart indicates that internationally oriented curriculum and students’ performance contributed the least to overall dissatisfaction each with percentages just under 45%, but they were still significant. The cumulative line, shown in red, helps to inform that by the time if we include the first three causes: integration of basic and clinical sciences and assessment methods, we reach over 150% cumulative dissatisfaction. This means that addressing these top concerns could alleviate the majority of dissatisfaction among faculty.
Fig. 2.
Causes of dissatisfaction with integrated curriculum among the studied academic medical staff
Table (2) shows the percentages of dissatisfaction causes among academic medical staff, stratified by rank and nationality. This stratification reveals that the dissatisfaction rates among senior staff of Jordanian and Egyptian nationalities are generally higher than those among junior and “other” nationalities whereas, senior Egyptian report 34.5% dissatisfaction with curriculum support, 28.7% with resources and 20.7% with workload, higher than their counterparts from juniors and other nationalities. However, the table shows that junior Jordanian staff report higher dissatisfaction rate of 20.7% with institutional support and 17.2% with assessment methods than their counterparts of senior and other nationalities.
Table 2.
Percentages distribution of dissatisfaction causes by rankings and nationality of studied medical staff
| Cause of Dissatisfaction* | Senior Jordanian | Senior Egyptian | Senior Other | Junior Jordanian | Junior Egyptian | Junior Other |
|---|---|---|---|---|---|---|
| Curriculum Support | 35/115 (30.4%) | 30/87 (34.5%) | 20/75 (26.7%) | 25/87 (28.7%) | 20/70 (28.6%) | 15/91 (16.5%) |
| Adequate Resources | 28/115 (24.3%) | 25/87 (28.7%) | 15/75 (20.0%) | 22/87 (25.3%) | 18/70 (25.7%) | 12/91 (13.2%) |
| Manageable Workload | 22/115 (19.1%) | 18/87 (20.7%) | 12/75 (16.0%) | 20/87 (23.0%) | 15/70 (21.4%) | 10/91 (11.0%) |
| Institutional Support | 18/115 (15.7%) | 15/87 (17.2%) | 10/75 (13.3%) | 18/87 (20.7%) | 12/70 (17.1%) | 8/91 (8.8%) |
| Effective Assessment Methods | 15/115 (13.0%) | 12/87 (13.8%) | 8/75 (10.7%) | 15/87 (17.2%) | 10/70 (14.3%) | 7/91 (7.7%) |
*: Categories are not mutually exclusive
Table (3) shows logistic regression analysis of the studied sociodemographic and work characteristics. It illustrates that the significant predictors of unsatisfaction with integrated system among medical staff were having Jordanian nationality (OR = 7.74) followed by Egyptian nationality (OR = 4.68), having experience more than 10 years in teaching integrated curriculum (OR = 4.25), working in governmental universities (OR = 4.23), and lastly having male gender (OR = 3.27).
Table 3.
Logistic regression analysis of sociodemographic and work predictors of unsatisfaction among the studied academic medical staff
| Predictors | β | p-value | AOR (95% CI) |
|---|---|---|---|
| Age: | |||
|
< 45 years ≥ 45 years |
0.360 | 0.120 |
1 # 1.43 (0.91–2.26) |
| Gender: | |||
|
Female Male |
1.186 | < 0.001* |
1 # 3.27 (1.98–5.40) |
| Nationality: | |||
|
Others Jordanians Egyptians |
2.046 1.543 |
< 0.001* < 0.001* |
1 # 7.74 (3.88–15.41) 4.68 (2.58–8.49) |
| Affiliated university: | |||
|
Private Governmental |
1.442 | < 0.001* |
1 # 4.23 (2.01–8.88) |
| Teaching experiences in conventional curriculum: | |||
|
≤ 10yrs > 10yrs |
0.075 | 0.754 |
1 # 1.08 (0.67–1.72) |
| Teaching experiences in integrated curriculum: | |||
|
≤ 10yrs > 10yrs |
1.447 | < 0.001* |
1 # 4.25 (2.49–7.27) |
|
Modelχ2 % correctly predicted P-value |
13.68 52.89% ≤ 0.001* |
||
β: regression coefficient, #: reference group; CI: confidence interval, AOR: adjusted odds ratio
*: statistically significant at p ≤ 0.05
Discussion
Integrated curriculum has been a popular concept in medical education for decades, however, the satisfaction of academic medical staff with integrated medical curricula has garnered increasing attention in recent years [10].
Analyzing the responses from the studied 525 academic medical staff members showed that 44.2% were satisfied versus 55.8% were unsatisfied with the integrated curriculum. Also, the current percentage distribution of self-reported satisfaction levels among medical staff indicated that most of the staff members were not in favor with the integrated curriculum’s current design and implementation, highlighting several potential areas for improvement. Previous literature stated that Faculty members felt that the integrated program might not be helpful in better performance in the professional examinations [11]. In a study by Khanna, et al., faculty satisfaction varied significantly based on resource availability and institutional support. Institutions with better support structures reported higher satisfaction [7]. However, lower satisfaction in some cases was reported by a previous study due to the complexity of implementing integrated curricula and the resistance from experienced faculty [12]. Additionally, studies have found that integrated curricula can significantly increase faculty workload due to the need for additional preparation, new teaching strategies, and administrative demands. Faculty often express dissatisfaction when their workload increases without adequate compensation or support [13]. Furthermore, larger student groups make small group activities and personalized instruction more difficult to manage, especially when physical spaces such as classrooms or laboratories are insufficient. Limited resources, such as available rooms for small group learning or technological support, can hinder the success of an integrated curriculum [14]. Also, the reliance on certain instructional methods, particularly lectures, can undermine the goals of integration if they fail to promote active learning, critical thinking, and application of knowledge across disciplines [15].
One of the significant findings in the present work is the association between age and satisfaction levels. Younger staff members (< 45 years) exhibited higher satisfaction rates (50.9%) compared to their older counterparts (≥ 45 years), who had a satisfaction rate of 39.1%. This disparity could be explained by the idea that young staff might have higher satisfaction rates due to fear of speaking up, being less involved in coordination, and not comparing old and integrated teaching methods or might be more adaptable to innovative teaching methodologies and changes inherent in the integrated curriculum. They might also have had less exposure to the conventional curriculum, making them less resistant to the new system. Conversely, older staff may have more ingrained teaching practices and preferences for conventional system, leading to dissatisfaction with the newer integrated approach. Similar studies have found that younger faculty members were generally more open to and satisfied with innovative teaching methods, including integrated curriculums [16].
This study found that gender differences also emerged as a notable factor, with male staff reporting significant lower satisfaction (38.1%) compared to higher satisfaction among female staff (51.7%). This might suggest that females are more resilient to changes and less resistant than males. Additionally, reflects varying expectations and perceptions of support and effectiveness within the integrated curriculum. Female educators might find the integrated curriculum more inclusive or better aligned with their teaching style and professional expectations. Alternatively, male educators might experience more difficulty adjusting to or perceiving value in the new curriculum structure. A previous study revealed that female educators often prefer and perform better in collaborative and integrated teaching environments [17].
Our study interestingly, found that qualification level (MBBCh, M.Sc., MD/PhD) did not significantly impact satisfaction (p = 0.6), indicating that the level of education or academic achievement is not necessarily associated with integrated curriculum satisfaction. However, this study showed that nationality had a significant effect, with Egyptian and Jordanian staff members reporting lower satisfaction rates (35.7%, and 38.2% respectively) compared to those from other nationalities (p < 0.001). This suggests that cultural and educational backgrounds might influence acceptance and perception of the integrated curriculum. Staff from different educational systems may have different expectations and experiences that shape their views on curriculum integration.
Institutional affiliation played a critical role in staff satisfaction levels. Staff from governmental universities reported significant lower satisfaction (41.3%) compared to those from private universities (65.1%), with a highly significant difference (p < 0.001). This could be explained by differences in resources, support, and flexibility between governmental and private institutions. Private universities might offer more robust support systems and resources, facilitating smoother transitions to the new integrated curricula, and accordingly showing higher satisfaction among their staff. Our current result is supported by findings in other study, which suggest that private institutions typically provide better resources and support for implementing integrated curriculula [18].
This study also found that the length of teaching experience in both conventional and integrated curricula was also a determining factor. Staff with over ten years of experience in the conventional curriculum were less satisfied (38.2%) compared to those who had less than ten years (53.2%), with a significant difference (p < 0.001). Similarly, those with extensive experience in the integrated curriculum reported higher dissatisfaction compared to their less experienced counterparts (60.4%, and 38.0% respectively with p < 0.001). These findings suggest that longer exposure to conventional curriculum may create a resistance to change, or being convinced that conventional system is the best. However, those who were new to the integrated curriculum might be more open and adaptable to its methodologies even if they were never being exposed to the conventional approach at all. Our result aligns with findings from previous study which highlights that experienced faculty may find it challenging to shift from traditional methods to integrated approaches. A study reported that experienced educators often face difficulties in adapting to new, interdisciplinary teaching methods due to entrenched practices and a preference for traditional, discipline-specific instruction [14]. The effectiveness of integrated curricula often depends on the duration of implementation and how well institutions support the transition process. For example, it has been observed that early implementation phases are challenging due to unfamiliarity and resistance to change, but over time, institutions and faculty tend to adapt better when continuous support is offered [3]. Moreover, it was reported that faculty development programs are essential to help educators adapt to integrated curricula, particularly for those accustomed to traditional teaching methods. Institutions that provide regular professional development opportunities report higher levels of faculty satisfaction and smoother transitions to new curricula [16].
The Pareto analysis highlights primary areas of dissatisfaction among academic staff with the integrated curriculum. The highest dissatisfaction levels in this Pareto focus on the integration of basic and clinical sciences. This might suggest that faculty may find it challenging to balance these areas due to differences in teaching methods and assessment requirements. The present finding aligns with previous study which reported that integrating basic sciences with clinical training posed significant challenges, especially in institutions with established traditional curriculums. Faculty members in their study expressed frustration over inadequate time to cover essential foundational knowledge while also integrating clinical applications [3]. The pareto also shows that dissatisfaction with assessment methods, likely reflects concerns over how well these assessments evaluate students’ competencies in an integrated learning environment. A study conducted on faculty perceptions for assessment methods within integrated curriculums and noted that traditional exams might not effectively measure interdisciplinary competencies [16]. This misalignment contributes to dissatisfaction as faculty believe assessments do not reflect the true breadth of the integrated curriculum’s objectives. Furthermore, our pareto result reveals faculty dissatisfaction with the curriculum’s implementation schedule points to difficulties in managing the integrated curriculum’s demands within limited time frames. This is consistent with findings from previous study which emphasized that integrated schedules can increase workload and reduce flexibility for educators, leading to burnout and frustration [15].
The present work revealed a comprehensive view of dissatisfaction causes among academic medical staff, stratified by rank and nationality. This stratification reveals insightful trends and potential areas for targeted improvements in medical curriculum integration. The results mentioned that dissatisfaction rates among senior staff of Jordanian and Egyptian nationalities are generally higher than those among junior and “other” nationalities while, junior Jordanian staff were more dissatisfied with institutional support and with assessment methods than their counterparts of senior and other nationalities. Parallels to this current results, similar dissatisfaction trends with higher dissatisfaction rates among senior staff were noted in one study in which senior faculty reported challenges with curriculum integration due to inadequate administrative and structural support [3]. Another study highlights that well-supported institutions reported lower dissatisfaction, emphasizing the importance of robust curriculum design frameworks [18]. Furthermore, it was reported that dissatisfaction with resource availability was common in institutions transitioning to integrated curricula [15], and this was aligned with the findings from the current study, particularly for Egyptian faculty. Institutions with comprehensive resource planning showed improved faculty satisfaction [7]. Also, faculty dissatisfaction with workload was similarly observed in Peicu et al. study (2019), where junior staff often expressed concerns about balancing teaching and curriculum-related tasks [13]. It was found that workload dissatisfaction decreased with experience, supporting the lower workload dissatisfaction rates among senior staff in our study [3]. Dissatisfaction with institutional support has been a recurring theme in integrated curriculum studies as both emphasized the need for tailored support systems to address faculty concerns during curriculum transitions [15, 18]. A previous study explained that dissatisfaction with assessment methods was linked to misalignment between integrated learning goals and traditional assessment structures [18]. This matches the trends seen in the current study.
The Logistic regression analysis identified that the rank of predictors of integrated system dissatisfaction were nationality, years of experience, affiliation, and gender. The result of the present study was unique whereas male staff with Jordanian and Egyptian nationality, affiliated to governmental institutions with extensive experience were significantly more prone to unsatisfaction. Clinical faculty in previous studies reported that increased workload, deficiency of resources, and development of competitive environment have been very challenging. They also mentioned that inadequate knowledge and attitude regarding clerkship planning, and implementation may be due to lack of team work, and effective teaching techniques. Furthermore, it was reported that curriculum redesigning is a strenuous, tiresome, persistent, and time consuming [13]. Other study mentioned that according to the qualitative data obtained from the faculty members, integration requires facilities and a well-equipped skill lab. The integrated approach posed several constrains including unsuitability for large groups of students, many subject areas are missing, limited cooperation among disciplines, and some subject areas are not fully covered in the allocated 50 min lecture. Furthermore, the integrated approach is more stressful than the conventional system and students can pass the course without achieving the minimum requirements in each discipline. With the integrated curriculum, students can leave out some disciplines according to their weight in the course, and they can, therefore, pass the programme without identifying their shortcomings in each discipline separately [9].
Limitations and strengths
This study encountered some limitations, first is the potential of recall bias as the data collected was self-reported information provided by medical staff. Another limitation was the online method of data collection which may influence sample representation. Unfortunately, it is noted that only a few junior staff members were included in this survey which could be a limitation however, this limited inclusion can be attributed to the focus on experienced academic medical staff, who generally have a deeper understanding of both the traditional and integrated medical curricula. Since this study aimed to assess satisfaction with curriculum design and implementation, it prioritized insights from more seasoned staff members, as their extended experience offers valuable perspectives on the integration process and potential challenges over time. Additionally, junior staff often have limited teaching experience, which may impact their ability to critically evaluate curriculum effectiveness across disciplines.
Despite these limitations, this is the first study that tackles this sensitive issue in different countries and different medical schools. So, it will overlay the way and provide baseline data for further studies to design a comprehensive intervention that calls for a potential return to the conventional medical curriculum.
Conclusions and recommendations
In conclusion, the study provided insightful data on the satisfaction of academic medical staff with the integrated medical curriculum. The findings reveal a general dissatisfaction whereas, more than half of studied medical staff were dissatisfied with the integrated curriculum’s design and implementation, spotting light on several predictors of staff dissatisfaction and potential areas for improvement. This means that addressing these top concerns could alleviate the majority of dissatisfaction among faculty. Dissatisfaction stems largely from challenges in integrating disciplines, misalignment in assessment methods, and demanding schedules. Addressing these areas could significantly enhance faculty satisfaction with the integrated curriculum.
The key factors influencing dissatisfaction included nationality, teaching experience, gender, and the type of institution. Specifically, academic staff from governmental universities, those with more than 10 years of experience, male educators, and staff from Jordan and Egypt were more likely to be dissatisfied. The dissatisfaction may stem from challenges such as increased workload, insufficient resources, resistance to new teaching methods, and a preference for the conventional curriculum, which many faculty members are more familiar with.
The study recommends that institutions should consider revisiting the structure and implementation of the integrated curriculum. They could offer more support, particularly in terms of resources, professional development, and workload management, to ease the transition from the traditional curriculum. However, our study revealed faculty satisfaction and familiarity with conventional curriculum over the integrated one that further support the effectiveness of old approach. The conventional medical curriculum has several advantages that make it a robust and reliable approach to medical education. Its structured discipline-specific format provides clear educational design and pathway, comprehensive coverage of specialties, and easier implementation. Thus, returning to the conventional approach can enhance the quality of medical education, increase faculty satisfaction and engagement, leading to a more positive educational environment, and future well-prepared healthcare professionals. So, institutions should consider these factors when evaluating their educational strategies and curriculum designs. However, offering targeted training programs for faculty, especially those with extensive experience in the conventional system, could help them adapt to the integrated curriculum. Faculty development initiatives should focus on fostering acceptance of integrated teaching methods and ensuring that staff are comfortable with the changes. Furthermore, private universities should be examined for best practices in implementing integrated curricula, as the study found higher satisfaction rates among staff from these institutions. Governmental universities might need more resources, administrative support, and flexibility in curriculum delivery. Additionally, tailored approaches based on age, nationality, and gender might be needed for staff. Younger staff appear more adaptable, so incorporating their feedback into curriculum reforms might drive more innovation. Finally, consideration of reintroducing conventional elements as the conventional curriculum seems to retain some advantages, it may be worth exploring a hybrid approach that blends elements of both systems. This could satisfy faculty who favor the traditional methods while also maintaining the benefits of an integrated curriculum.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all medical staff who participated in this study.
Author contributions
All authors reviewed the manuscript and shared in data collection process. DB, and AB conceptualized and created the research idea. GS, RE, TA, and AB shared to design the research. GS, RE, AE, and AK shared to review the literatures. RE and SA developed the questionnaire. GS, and AE shared to coordinate the research. SA performed data entry and analysis. GS, RE, and SA shared to prepare tables and figure. GS, AE, AK, and DB shared to comment on the results. GS, RE shared to develop the discussion part of research. RE, and TA shared in drafting and publication of the manuscript.
Funding
No funding was received from any institute, company, organization or individual.
Data availability
Data cannot be shared openly but are available on request from authors and after permission from the authority of Ibn Sina University of Medical Sciences, Amman, Jordan due to the following issues: 1. Participant confidentiality and privacy: the data collected might include sensitive information, and sharing it openly could risk compromising participant confidentiality, even if anonymized. Data privacy laws like General Data Protection Regulation impose strict requirements on handling and sharing personal data. 2. Ethical Restrictions: ethical approval obtained for the study not permit unrestricted sharing of data and IRB mandates data-sharing protocol to protect study participants. 3. Data ownership and institutional policies: the data are owned and managed by an Ibn Sina University of Medical Sciences, Amman, Jordan that restricts its open distribution. Authors must comply with such agreements or policies.
Declarations
Ethics approval and consent to participate
Approval to conduct the survey was obtained by Ibn Sina University for Medical Sciences Institution’s Review Board (Approval Number: ISUMS-IRB# 1006/8-11-2023). Consent to participate was verbal and participation was based on voluntary base. The participants were guaranteed anonymity and confidentiality. We obtained an informed verbal consent from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.BMCM, Education. 2024. Designing health professional education curricula using systems thinking perspectives. 10.1186/s12909-020-02442-5 [DOI] [PMC free article] [PubMed]
- 2.Hopkins R, Pratt D, Bowen JL, Regehr G. Integrating basic science without integrating basic scientists: reconsidering the place of individual teachers in curriculum reform. Acad Med. 2015;90(2):149–53. 10.1097/ACM.0000000000000437 [DOI] [PubMed] [Google Scholar]
- 3.Muller J, Jain S, Loeser H, Irby DM. Lessons learned about integrating a medical school curriculum: Perceptions of students, faculty and curriculum leaders. Medical Education. 2008;42(8):778-85. 10.1111/j.1365-2923.2008.03110.x. [DOI] [PubMed]
- 4.Mohamed RHB, Jarrar M, Abumadini MS, Al Elq A, Abusalah MAH, Al Bsheish M, Alqahtani FM, Rayani A. Student Perspectives and Academic Achievement in a Traditional versus an Integrated Curriculum: Evidence from a Medical School. Health Professions Education. 2023;9(4):180-190. Accessed at https://hpe.researchcommons.org/journal/vol9/iss4/3/
- 5.Hattie J, Timperley H. The power of feedback. Rev Educ Res. 2007;77(1):81–112. 10.3102/003465430298487 [Google Scholar]
- 6.Biggs J. Aligning teaching for constructing learning. The Higher Education Academy, 2003. https://s3.eu-west-2.amazonaws.com/assets.creode
- 7.Atta I, El-Hag MA, Ihab S, Al-Ghamdi HS, Alghamdi T. Drawbacks in the implementation of an Integrated Medical Curriculum at Medical Schools and their potential solutions. Educ Med J. 2020;12(1):29–42. 10.21315/eimj2020.12.1.4 [Google Scholar]
- 8.Daniel W. Biostatistics: A foundation for Analysis in the Health Sciences, 7thed, 1998. New York: John Wiley and Sons. ISBN: 978-0471163862.
- 9.El-Masry R. Satisfaction of Academic Medical Staff with Integrated Medical Curriculum Questionnaire. Developed in November; 2023.
- 10.Wijnen-Meijer M, van den Broek S, Koens F, ten Cate O. Vertical Integration in Medical Education: the broader perspective. BMC Med Educ. 2020;20(509). 10.1186/s12909-020-02433-6 [DOI] [PMC free article] [PubMed]
- 11.Asad -M. Tanwir Khaliq. Faculty Perception Regarding Integrated Curriculum at Undergraduate Level: A Qualitative Study. Pak Armed Forces Med J 2020; 70 (1): 217 – 23. https://pafmj.org/index.php/PAFMJ/article/view/3966
- 12.Khanna -P. Andrew Stuart Lane. Designing health professional education curricula using systems thinking perspectives. BMC Med Educ. 2021;21(20). 10.1186/s12909-020-02442-5 [DOI] [PMC free article] [PubMed]
- 13.PV. Integrated Approach - Challenges in Pedagogical Design of Learning. In E. Soare, & C. Langa, editors. European Proceedings of Social and Behavioral Sciences. 2019, 67: 1029–1037. Future Academy. 10.15405/epsbs.2019.08.03.125
- 14.Harden RM. Ten questions to ask when planning a course or curriculum. Med Educ. 1986;20(4):356–65. 10.1111/j.1365-2923.1986.tb01379.x [DOI] [PubMed] [Google Scholar]
- 15.Brauer DG, Kristi J. Ferguson. The integrated curriculum in medical education. Med Teacher J. 2015;37:312–22. 10.3109/0142159X.2014.970998 [DOI] [PubMed] [Google Scholar]
- 16.Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE Guide 96. Med Teach. 2015;37(4):312–22. 10.3109/0142159X.2014.970998 [DOI] [PubMed] [Google Scholar]
- 17.Jennifer Dickfos. Academic professional development: Benefits of a pracademic experience. International Journal of Work-Integrated Learning. 2019, 20(3): 243–255. https://files.eric.ed.gov/fulltext/EJ1232894.pdf
- 18.Khanna P, Roberts C, Lane SA. Designing health professional education curricula using systems thinking perspectives. BMC Med Educ. 2021;21(20). 10.1186/s12909-020-02442-5 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared openly but are available on request from authors and after permission from the authority of Ibn Sina University of Medical Sciences, Amman, Jordan due to the following issues: 1. Participant confidentiality and privacy: the data collected might include sensitive information, and sharing it openly could risk compromising participant confidentiality, even if anonymized. Data privacy laws like General Data Protection Regulation impose strict requirements on handling and sharing personal data. 2. Ethical Restrictions: ethical approval obtained for the study not permit unrestricted sharing of data and IRB mandates data-sharing protocol to protect study participants. 3. Data ownership and institutional policies: the data are owned and managed by an Ibn Sina University of Medical Sciences, Amman, Jordan that restricts its open distribution. Authors must comply with such agreements or policies.