Abstract
Background
The cost accounting of medical service projects forms the basis for disease cost accounting and DRG (Diagnosis-Related Groups) cost accounting. Among the various costs involved, human resources represent a significant portion and are highly complex, making their accurate accounting a critical and challenging aspect of cost accounting for medical service projects.
Methods
This paper introduces the itemized point cost (IPC) method, a novel cost accounting approach based on the RBRVS (Resource-Based Relative Value Scale) theory. It outlines the core concepts of “points” and “process steps” within the IPC framework and details its application in human cost accounting. An example of impacted tooth extraction in the stomatology department of Hospital A is used to illustrate the IPC method's implementation process.
Findings
A comparative analysis with activity-based costing and time-estimation costing methods shows that the IPC method is concise, practical, and operable. It is also aligned with the principles of cost-effectiveness.
Conclusions
The paper proposes strategies to promote the IPC method, including leveraging information technology, enhancing top-level design, and standardizing processes, to improve its adoption and effectiveness in medical cost accounting.
Keywords: Human cost, Itemized point cost method, Delicacy management, RBRVS
Introduction
Cost accounting for medical procedures involves the collection and allocation of various costs associated with medical services provided by different departments within a hospital. This data is then used to calculate the unit cost of each service. Human resources are the most important resources in a hospital [2, 4, 9]. These resources include doctors, medical technicians, nurses, administrative staff, and others, and together they ensure a hospital’s competitiveness. The cost of these human resources in medical service projects reflects various medical personnel’s value of service, including cost elements such as wages, bonuses, benefits, and social security [14]. These cost elements are interrelated and influence each other. In project cost accounting, labor costs typically account for over 50% of the total costs, and in labor-intensive medical service projects, this proportion is even higher. For example, in surgical projects labor costs often exceed 70%, and in nursing projects they can reach 80% or higher. Thus, when multiple medical service projects share the same human resource pool, how to allocate human resources reasonably to each medical service project and accurately calculate the unit cost of these projects is a problem that needs to be solved.
The implementation of cost accounting methods, such as Activity-Based Costing (ABC) and Time-Driven Activity-Based Costing (TDABC), has been studied by many scholars. ABC enables healthcare organizations to trace indirect costs to the activities driving them, which is particularly beneficial given the complexity of healthcare services [1, 10, 17]. It enhances decision-making by providing insights into the cost variations across service lines and departments, thus helping in optimizing resource use and reducing unnecessary expenses [6]. Several studies have highlighted the effectiveness of ABC in aligning costs with clinical decisions and improving the financial transparency of healthcare services [11, 16, 19]. TDABC offers further simplicity and accuracy by assigning costs based on the time required for healthcare activities [3, 5, 8]. By calculating a capacity cost rate (CCR) for each resource and linking it to time-driven processes, TDABC provides a clearer picture of resource utilization across patient care pathways. Studies by Keel et al. [12] and Silva et al. [3] support the use of TDABC for its ability to streamline costing in both high-resource and low-resource healthcare environments. For example, Kaplan and Porter [10] reported the success of TDABC in reducing costs for joint replacement surgeries, demonstrating the method’s capacity to identify inefficiencies and optimize resource allocation.
This paper proposes a new cost accounting method known as the Itemized Point Cost (IPC) method by deploying the Resource-Based Relative Value Scale (RBRVS) and by introducing factors such as Job-level ranks and technical risk values. Based on an analysis of a practical case in the stomatology department of Hospital A, the paper explains in detail how the IPC method is applied and further discusses this method’s comparative advantages over ABC and TDABC methods. Finally, the paper suggests implementation pathways for the IPC method with the perspective of refined management in service hospitals.
The case study hospital, Hospital A, is one of the highest ranked public hospitals in the country, achieving an A + evaluation grade in the national performance assessment of tertiary public hospitals in 2022. Furthermore, the hospital is highly representative of the nation’s hospitals in terms of cost management practices. In 2023, the hospital’’s outpatient visits exceeded 5 million, discharges approached 180,000, and surgical procedures exceeded 120,000. The focus of this study, the stomatology department in Hospital A, has a typical human resource structure, including positions such as oral health doctors, nurses, technicians, and others, with significant differences in salaries and benefits among different positions. At the same time, the stomatology department requires high-level technical skills from its staff based on the medical services provided. In this respect, studying the cost accounting of human resources in stomatology medical service projects effectively illustrates features and advantages of the IPC method for cost accounting in medical service projects.
The contributions of this paper are threefold: First, this paper introduces the IPC method, a more refined and convenient cost accounting method than activity-based costing and time-estimation costing methods. By considering the job levels and technical difficulties of medical personnel, the IPC method offers medical institutions more precise and comprehensive cost information, which more accurately reflects the true costs of medical service projects. Second, the paper compares the IPC method with traditional costing methods, clearly demonstrating the advantages of the IPC method in terms of lower operational costs, higher accuracy, and broader applicability. Such a comparison also provides application scenarios for various methods, providing decision-makers with more evidence-based options. Lastly, this study uses practical cases to provide specific and feasible pathways to implement the IPC method and make related recommendations. Medical institutions will then be able to gather refined, accurate cost data. This then provides support for government health investment and financial compensation, for medical service price-setting and regulation, for improvement of medical insurance payment policies, and for hospital performance evaluation.
Methodology
Institutional background
As noted above, the “Guidelines for Public Hospital Cost Accounting” proposed that by the end of 2025 all tertiary hospitals should carry out cost accounting for medical service projects, disease cost accounting, and DRG (Diagnosis-Related Groups) cost accounting. Secondary and lower-level hospitals are mandated to conduct departmental cost accounting, outpatient visit cost accounting, and bed-day cost accounting, while gradually extending to medical service project cost accounting, disease cost accounting, and DRG cost accounting. By the end of 2030, all hospitals are expected to engage in the latter group of more advanced accounting activities. The policy aims to enhance cost management and improve internal operational efficiency; meet the information needs related to internal cost control and performance evaluation; optimize resource allocation; and promote the high-quality development of public hospitals.
Traditional cost accounting methods often fall short in the face of complex medical service projects where healthcare institutions struggle to meet the policy requirements for comprehensive cost accounting. The “Public Hospital Cost Accounting Standards” jointly issued by the National Health Commission of the People’s Republic of China and the National Administration of Traditional Chinese Medicine in 2021 encourage medical institutions to innovate and apply cost accounting methods suitable for their specific circumstances. They are also required to deploy activity-based costing and cost-equivalent methods.
By considering factors such as labor intensity, technical difficulty, and risk in medical service projects, the IPC method can more accurately reflect the labor value of medical personnel. Moreover, the flexibility and convenience of the method ensure improved operability and scalability in labor-intensive medical institutions.
Basic principles of human resource cost accounting
In standardized product cost accounting in the industrial sector, relatively mature algorithms account for direct labor costs and indirect labor costs (included those in manufacturing overhead). However, due to the personalized and complex nature of medical services, the actual consumption relationship for human resource costs among various medical service projects is difficult to define. Algorithms are not easily applied to medical service products with low standardization and with participation of diverse medical personnel. Only by adopting an algorithm that matches the labor input and output of medical personnel from various positions can the direct human resource costs be calculated and included in the medical service projects.
The basic principles for applying the IPC method for human resource cost accounting are as follows. (1) To simplify calculations, the workload and efficiency of doctors, nurses, and other medical staff are assumed to be stable over a certain period. (2) Direct human resource costs of departments cannot be directly included in the project human resource costs due to the complex nature of hospital business management. They can, however, be calculated and then included through a well-reasoned algorithm and cost drivers (allocation parameters); indirect human resource costs are the same as direct human resource costs. (3) The cost drivers for each element of human resource costs (basic wages, bonuses, etc.) are assumed to be consistent and independent of each other. (4) Medical service projects are considered to be standardized, workflow tasks proceduralized, and patient conditions homogeneous. (The uniqueness of individual cases is not considered.) Thus, we assume the human resource consumption of medical staff for a similar medical service project will be the same (which can be at the hospital level or level of a smaller accounting unit). The quantification standards for cost drivers (allocation parameters) are consistent within the same accounting unit. Of course, the human resource costs calculated in this way are not what could be called standard costs. Similarly, they are not target costs that can be achieved with existing medical technology or under current levels of management at the hospital. Instead, we can understand it as a requirement of a thoroughly standardized management of the hospital’s medical work flows. Not only is the operation of technology in medical and nursing procedures standardized, through standardized management, medical work processes, order of medical procedures, and diagnostic and treatment protocols can be performed for an actual average cost. Therefore, the cost driver parameters here can also be called standard cost driver parameters. (5) More difficult techniques and high-risk operations often require medical staff to have higher professional qualifications and levels of skill, which are accumulated through long-term learning and practice. Therefore, taking into account the technical difficulty of the work and levels of risk in human resource cost accounting helps us accurately evaluate the labor value of medical and nursing staff.
Theoretical foundation
RBRVS, or Resource-Based Relative Value Scale, is a method for paying physician labor costs based on resource consumption and relative value [7]. In 1992, RBRVS was approved by the US Congress to calculate physician remuneration in the Medicare system. It has also been used as a point of reference when Medicaid and other non-profit health insurance companies pay physician remuneration. The initial model of RBRVS considered the time and labor costs of physicians, and later gradually introduced other factors such as technical difficulty, risk, and complexity [13, 15, 18]. The RBRVS performance allocation theory is also applicable to cost accounting, mainly because both perspectives are based on similar theoretical approaches and methodologies: They both assess resource consumption and relative value of medical services, aim to achieve fairness and efficiency in resource allocation, and promote quality and efficiency of medical services. The cost accounting model based on RBRVS takes medical service projects as objects of accounting, comprehensively considering factors such as labor intensity, technical difficulty, and risk of medical service projects. It can also more reasonably reflect the labor value of medical personnel. This model is relatively evidence-based, objective, and fair, meeting the needs of hospitals for refined management during periods of rapid development.
Key concepts of IPC“Points” and “Process Steps”
“Points” and “process steps” are the core concepts of the IPC method. Based on the theory of RBRVS, the IPC method selects key elements of various medical service costs for evaluation and assigns a certain score to the corresponding elements, which is the “point” [20, 21]. Specifically, medical service projects that consume more resources are assigned higher “points” in the IPC method. The core objective of the itemized point costing method is to link the costs of medical service projects with the degree of resource consumption of key elements. Here, the consumption of human resources not only includes direct material and time costs but also considers factors such as labor intensity, technical difficulty, and risk of the project.
Another important concept in the IPC method is “process steps.” Unlike the activity-based costing method, the IPC method divides the medical service project process into “process steps” of different medical and nursing personnel. “Process steps” refer to a series of continuous, orderly operational steps and activities performed by medical staff for patients during the medical service process. These steps and activities develop based on medical knowledge and practical experience to ensure that patients receive correct, timely, and effective medical services. For example, a simple medical service process step may involve medical staff receiving patients, inquiring about their conditions, conducting necessary physical examinations, issuing corresponding examination orders or prescriptions based on symptoms and behavior, and finally providing treatment recommendations or medication. In this process, each step is orderly and intricately connected, together constituting a complete medical service “process step”.
The corresponding “activities” in the activity-based costing method refer to various processes or links in the medical service provision process, such as “intramuscular injection,” which is divided into “verification, material collection, positioning, disinfection, injection, observation” and other activities. Therefore, the sum of physician activities equals physician process steps, the sum of nurse activities equals nurse process steps, and the sum of medical technician activities equals medical technician process steps. We can take the electronic gastroscopy stent implantation in the “Guidelines for Public Hospital Cost Accounting” as an example. The relationship between the activities under the activity-based costing method and the process steps under the IPC method is shown in Table 1. The underlying logic of dividing “Activities” in the activity-based costing method and process steps in the IPC method is consistent; the “Process Steps” in the IPC method are the collection of activities in the activity-based costing method, and the process of cost accounting is much clearer and simpler. Therefore, under this method, the human resource costs of medical service projects are divided into process steps of different medical and nursing personnel. This dynamic can be understood as “services consume process steps, and process steps consume resources.”
Table 1.
The relationship between "Activities” and “Process Steps”: the electronic gastroscopy stent implantation example
| Activity based costing | Point costing method | |||||
|---|---|---|---|---|---|---|
| Activity | Type of operator | Quorum | Operating time (minutes) | Working procedure | Quorum | Operating time (minutes) |
| Preoperative preparation | Physiotherapists | 1 | 4 | Surgeon | 1 | 30 |
| Lubricity | Surgeon | 1 | 2 | Physiotherapists | 1 | 30 |
| Physiotherapists | 1 | 2 | ||||
| Defoamer | Surgeon | 1 | 2 | |||
| Physiotherapists | 1 | 2 | ||||
| Insertion | Surgeon | 1 | 8 | |||
| Physiotherapists | 1 | 8 | ||||
| Implantation | Surgeon | 1 | 10 | |||
| Physiotherapists | 1 | 10 | ||||
| Withdrawal | Surgeon | 1 | 3 | |||
| Report | Surgeon | 1 | 5 | |||
| Post-operative testing | Physiotherapists | 1 | 4 | |||
| Subtotal | Surgeon | 1 | 30 | |||
| Physiotherapists | 1 | 30 | ||||
The essence of the IPC method lies in establishing the appropriate “points,” which involves setting cost drivers for different types of costs to quantify the costs of medical service projects. Then once the process steps are determined, the direct human resource costs of physicians, nurses, or medical technicians are allocated to the respective projects according to their individual points. Therefore, the precision in accounting for human resource costs within medical service projects does not hinge on the granularity of job division. Instead, it relies on the accurate estimation/measurement of the standard human resource consumption drivers for various medical personnel in the medical projects.
Applications of the method
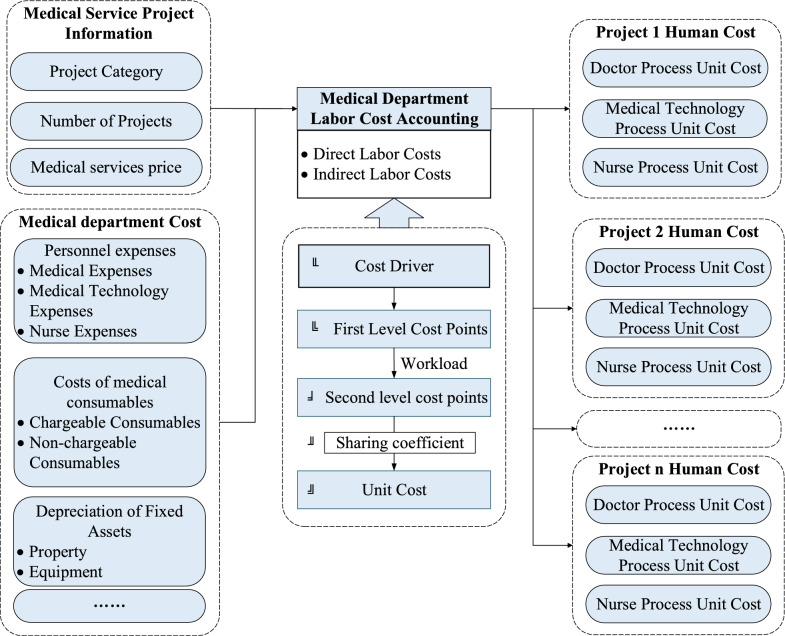
Figure 1 illustrates the process of applying the IPC method in human resource cost accounting of medical service projects. This includes the determination of cost items, the collection of cost driver data, the setting of points, and the calculation of unit costs, among other processes.
Fig. 1.
Human resource cost accounting for medical project with IPC method
Determining cost items, setting points, and cost drivers
In accordance with “Public Hospital Cost Accounting Standards,” cost accounting data collection includes seven major categories of first-level cost items: personnel expenses, medical material costs, pharmaceutical costs, fixed asset depreciation costs, intangible asset amortization costs, medical risk fund extraction, and other operating expenses.1 Based on this foundation, secondary cost items2 are categorized, and corresponding points and cost drivers are set according to the principle of importance and resource consumption patterns. The rational setting of cost drivers is a crucial step, as the more reasonable the cost drivers, the closer the correlation between actual costs and cost drivers, leading to better allocation results. Human resource costs, for example, can be divided into direct and indirect costs:
Direct human resource costs = Physicians + Nurses + Medical technicians’ labor costs.
Indirect human resource costs = Non-physician, non-nurse, non-medical technician costs within the department (including research, teaching, and auxiliary personnel) + Administrative and logistical overhead labor costs + Medical auxiliary labor costs.
For direct human resource costs, the drivers (first-level cost points) include service volume, Job-level rank, service duration, and comprehensive technical level. For instance, if nursing costs are directly proportional to the direct labor hours of nurses, this relationship should be reflected in the allocation, making it appropriate to choose nursing service time as the cost driver. Compared to the activity-based costing method, the human resource costs under the IPC method include two additional cost drivers: Job-level rank and comprehensive technical level. The advantage of this approach lies in the standardization of cost drivers under the itemized point cost method, which facilitates the comparison and integration of departmental cost data. Various cost drivers, such as Job-level rank, working hours, and the number of operators, independently influence labor cost accounting, without interdependence or variability. Moreover, taking into account multi-dimensional cost drivers is more comprehensive than in the activity-based costing method. This is especially true when accounting for the technical difficulty and risk-related labor characteristics of medical projects, which can more fully reflect the differences in the labor value of medical personnel.
Indirect human resource costs are allocated based on the proportion of direct human resource costs of physicians, nurses, and medical technicians within the department. The specific calculation method then converges with that of direct human resource costs. The logic inherent in accounting for direct and indirect human resource costs under the IPC method is consistent; such an approach is simpler and adheres to the principle of importance, avoiding the complex and cumbersome work of accounting for indirect costs under the activity-based costing method.
Determining first- and second-level cost points
The determination of points is central to the calculation process in the IPC method. The magnitude of points reflects the weight of resource consumption of each process step and directly affects the accuracy and usability of the IPC method’s accounting results. First-level cost points are the most basic element point values used for project cost accounting, reflecting the basic weight of each medical project’s secondary cost items. Second-level cost points are the final weights allocated to medical projects. Points are obtained through observation, information systems, field research records, and other methods. The cost items, points, and corresponding cost drivers are shown in Table 2.
Table 2.
Cost item categories and point settings
| Serial number | Cost item | Cost points | Cost driver (first-level points) |
|---|---|---|---|
| 1 | Personnel expenses | Human resource cost points | Job-level rank, service volume, working hours and comprehensive technical level |
| 2 | Medical material costs | Special non-chargeable consumable points | Unit usage |
| General non-chargeable consumable points | Unit usage or low-value consumable coefficient in the 2023 edition of the “Standards” | ||
| 3 | Fixed asset depreciation costsa | Special building Depreciation points | Project duration |
| Bed fee type projects | Bed count or the area of buildings involved | ||
| General building depreciation points | Project duration | ||
| Special equipment depreciation points | Project duration | ||
| General equipment depreciation points | Project duration | ||
| 4 | Intangible asset amortization costs | Intangible asset amortization points | Project duration |
| 5 | Extraction of Medical Risk Fund | Medical risk fund points | Risk degree coefficient of medical service projects |
| 6 | Other operating expenses | E.g., special electricity points | Power consumption of large special equipment, project duration |
| … | … |
aFor the fixed assets of a hospital, the most important are buildings and medical equipment. These buildings and medical equipment can be divided into two categories: special and general. Among them, the special house refers to the development of some medical service projects in the special site, then in the project cost accounting, the depreciation of these special houses should only be included in some specific projects, in order to more accurately conform to the principle of value transfer. For example, the operating room is a place to provide surgery and rescue for patients, and its depreciation should be shared in the various medical projects carried out in the operating room. Special equipment is treated similarly. The cost driver parameter of the cost sharing between them is mainly the service time. Limited by the length of this paper, we will not go into details here
As shown in Step 2 of Fig. 1, this paper takes the most representative and typical human resource costs as an example to demonstrate the process of determining first-level cost points. The IPC method incorporates technical elements into the human resource cost accounting, in addition to the “time” variable, reflecting the labor value of medical personnel. Thus, human resource cost points are not only related to the Job-level rank, service volume, and service duration of medical and nursing staff but also to the technical difficulty and risk degree elements of medical services. This is one of the key innovations of the IPC method.
First-level human resource cost points = Job-level rank × Operation volume × Operation time × Comprehensive technical level.
The Job-level rank is determined based on the average income of all medical and nursing staff's job levels. If the annual average income of doctors with an entry-level position is taken as the benchmark, the corresponding Job-level ranks for doctors of other position levels can be obtained by comparing their annual average incomes. Operation volume and operation time refer to the standard number and standard service time of medical and nursing staff for medical projects, which can be determined through on-site observation, system data statistics, expert interviews, and industry standard database. The comprehensive technical level coefficient is derived from the “National Medical Service Project Technical Standards (2023 edition).” This calculation is based on the comprehensive technical level assignment value obtained by weighting the technical difficulty coefficient and risk degree coefficient corresponding to the medical service project, while dividing every 10 points from 1 to 100 into a grade coefficient; assigning a corresponding comprehensive technical level to each grade; and then obtaining the corresponding comprehensive technical level coefficient based on the comprehensive technical assignment value.
Second-level cost points are the final weights allocated to medical projects, determined based on first-level cost points and the number of medical projects, as shown in Step 3 of Fig. 1. The calculation formula is as follows:
Calculating project unit costs
After completing the collection of various medical service project business volume data, human resource costs, and project standard cost driver data, first- and second-level cost points are calculated. Based on this, the collected direct and indirect human resource costs can then be allocated to the various medical service projects carried out.
As shown in Step 4 of Fig. 1, the cost allocation coefficient for each process step is calculated first.
For example, for cost allocation coefficient of the “physician” process step, the costs of the “physician” process step in the department must first be summed up. Then, the sum of the second-level cost points for the “physician” process step is calculated to determine the cost allocation coefficient for the “physician” process step. Next, as shown in Step 5 of Fig. 1, based on the cost allocation coefficient of the process step and the first-level cost points of the corresponding medical service project, the unit cost of the process step is calculated as . Finally, the unit cost of a specific medical project is the sum of the unit costs of the various process steps corresponding to that project: .
Analysis and feedback
In the analysis and feedback stage, the calculation results of the itemized point cost method need to be analyzed and compared to assess their accuracy, to identify their strengths and weaknesses, and to optimize the calculation process and point settings according to actual conditions.
First, it is necessary to analyze the unit costs of medical service projects calculated through the IPC method. This process includes (1) re-examining the cost structure, influencing factors, and relative value of each project to determine its rationality and accuracy; and (2) comparing the calculation results of the itemized point cost method with other cost accounting methods (such as ratio coefficient method, activity-based costing method, time-driven activity-based costing method, etc.). In other words, we are comparing the unit costs derived from different methods, analyzing the differences and reasons for these differences, and thus evaluating the advantages and limitations of the IPC method in cost accounting.
Second, based on the results of the comparative analysis and actual conditions, we can optimize and adjust the calculation process and point settings of the IPC method. For example, we can re-evaluate the weight and point settings of various indicators, adjust the process division and cost allocation methods, etc., while continuously improving the calculation model and operational process of the IPC method. This enhances the accuracy and applicability of cost accounting, making it more aligned with the actual needs and management objectives of medical institutions.
A human resource cost accounting case study in the stomatology department using IPC method
Case selection
This paper has chosen the human resource costs of medical service projects in the stomatology department of Hospital A in 2021 as the object of our analysis, focusing on the specific project of an impacted tooth extraction (completely buried CP) for cost accounting purposes. As a vital clinical department within the hospital, accurate cost accounting of the stomatology department's service projects is essential for the hospital's efficient operational management. The department comprises 12 doctors, including 3 resident physicians, 6 attending physicians, 3 deputy chief physicians, and 1 chief physician, as well as 9 nurses. As indicated in Table 3, the combined direct and indirect costs for doctors and nurses in this department total approximately 15.38 million yuan.
Table 3.
Categorized costs of dental personnel in Hospital A (units: CNY)
| Direct cost | Indirect cost | Total (Direct cost & Indirect cost) | |
|---|---|---|---|
| Surgeon | 7,716,396.92 | 3,056,936.64 | 10,773,333.57 |
| Physiotherapists | 3,302,912.70 | 1,308,485.68 | 4,611,398.38 |
| Total | 11,019,309.62 | 4,365,422.32 | 15,384,731.95 |
Impacted tooth extraction (completely buried CP), a typical operation in the stomatology department, involves a complex treatment process and significant human resource investment. Selecting this project for cost accounting analysis allows for a comprehensive discussion of the cost structure and management situation within the stomatology department. The project’s workload in 2021 was 11,017 cases, with a fee schedule of 460 yuan per case. In addition to the general risks associated with routine tooth extraction, such as post-extraction bleeding, infection, and anesthesia, the extraction of completely buried impacted tooth carries a higher risk of nerve damage, root displacement into the lingual cortical bone of the mandible, communication with the maxillary sinus, soft tissue injury, and fractures of the alveolar bone or jawbone. Improper handling can also lead to damage of adjacent tooth or the temporomandibular joint, postoperative swelling, and difficulty in opening the mouth, among other postoperative reactions. Therefore, the operation requires doctors to possess advanced knowledge and skills; thoroughly consider anatomical structures, variations in tooth morphology, and relationships with adjacent tooth; and integrate the patient’s overall health status. Thus, doctors will be able to devise meticulous surgical plans and select appropriate operational angles based on the tooth’s position.
In the case of a tooth extraction (completely buried CP), it is necessary to ascertain the first-level cost points for each process step involved in the impacted tooth extraction. In the stomatology department, the procedures related to medical service projects are categorized into “doctors” and “nurses.” The Job-level ranks for doctors (including medical technicians) and nurses are calculated based on the average annual income per professional level of the medical staff for the current year, as illustrated in Table 4. The comprehensive technical level is derived from the weighted comprehensive technical level corresponding to the medical service project in the 2023 edition of the “National Medical Service Project Technical Standards.” Scores ranging from 1 to 100 are divided into levels based on every 10 points, with each level assigned a corresponding coefficient. The appropriate comprehensive technical level is then obtained based on the comprehensive technical level. For instance, scores between 0 and 10 are classified as Level 1, and so on, with scores between 90 and 100 categorized as Level 10.
Table 4.
Grade factor for dental section, Hospital A
| Quorum | Grading factor | |
|---|---|---|
| Resident | 3 | 1.0 |
| Attending physician | 6 | 1.4 |
| Deputy chief physician | 3 | 1.7 |
| Chief physician | 1 | 3.2 |
The calculation process for the comprehensive technical level of impacted tooth extraction (completely buried CP) is as follows: Referring to the 2023 edition of the “National Medical Service Project Technical Standards,” the technical difficulty coefficient and risk degree coefficient for this procedure are 72 and 66 respectively. After weighting, the comprehensive technical risk assignment value is 69, which corresponds to a comprehensive technical level of Level 7. Based on the confirmed process steps, number of operators, procedure time, comprehensive technical level, and Job-level rank, the first-level human resource cost points for the impacted tooth extraction procedure are calculated using the following formula, as shown in Table 5:
Table 5.
Processes and first-level cost points for extraction of impacted tooth
| Project name | Type of process | Number of operators | Operating time | Consolidated technical value-at-risk | Grade factor | First-level human resource cost points |
|---|---|---|---|---|---|---|
| Extraction of impacted tooth | Surgeon | 1 | 20 | 7 | 1.4 | 196 |
| Physiotherapists | 1 | 7 | 1 | 1 | 7 |
Based on the first-level human resource cost points, the second-level human resource cost points for a medical project are determined by multiplying them with the current period’s workload. As illustrated in Table 6, for the “attending physician” process step in the impacted tooth extraction procedure, the second-level human resource cost points are calculated by multiplying the first-level human resource cost points of 196 by the current period's workload of 11,017.
Table 6.
Project sub-itemized second-level points
| Medical projects | Attending physician process | Physiotherapists process |
|---|---|---|
| Extraction of impacted tooth | 2,159,332 | 77,119 |
| Alveoloplasty | 5740 | 615 |
| Extraction of complex tooth | 1,294,650 | 73,980 |
| … | … | … |
| Total | 12,550,552 | 800,414 |
Second-level human resource cost points for “Attending Physician” process step in impacted tooth extraction procedure = First-level human resource cost points × Current period workload = 196 × 11,017 = 2,159,332.
Similarly, for the “nurse” process step in the impacted tooth extraction procedure, the second-level human resource cost points are calculated by multiplying the first-level human resource cost points of 7 by the current period’s workload of 11,017.
Second-level human resource cost points for “Nurse” process step in impacted tooth extraction procedure = First-level human resource cost points × Current period workload = 7 × 11,017 = 77,119.
This calculation method allows for the distribution of human resource costs across the various process steps involved in the medical project and reflects the labor input and intensity associated with each step. It provides a detailed breakdown of costs, which is essential for accurate cost accounting and fiscal management.
As indicated in Table 6, after calculating the second-level human resource cost points for all “attending physician” process steps in the stomatology department, it is necessary to further compute the cost allocation coefficient.
For the “attending physician” process step in the stomatology department, the direct costs are divided by the sum of the second-level human resource cost points for the “attending physician” process step to obtain the direct cost allocation coefficient. Subsequently, this coefficient is multiplied by the corresponding first-level human resource cost points for the “attending physician” process step in the impacted tooth extraction procedure to arrive at the unit direct human resource cost for this process. For instance, the unit direct human resource cost for the “attending physician” process step in the impacted tooth extraction procedure is calculated using the following formula.
Unit direct cost for “Attending Physician” process = (Sum of direct costs of the process step/Sum of second-level human resource cost points of the process step) × First-level human resource cost points = (7,716,396.92 / 12,550,552) × 196 = 120.51.
Unit direct cost for “Physiotherapists” process = (Sum of direct costs of the process step / Sum of second-level human resource cost points of the process step) × First-level human resource cost points = 3,302,912.7/800,414 × 7 = 28.89.
The method of calculating indirect costs per unit for “Attending Physician” process and “Physiotherapists” process is similar to that for direct costs per unit.
Unit indirect cost for “Attending Physician” process = (Sum of indirect costs of the process step/Sum of second-level human resource cost points of the process step) × First-level human resource cost points = (3,056,936.64/12,550,552) × 196 = 47.74.
Unit indirect cost for “Physiotherapists” process = (Sum of indirect costs of the process step/Sum of second-level human resource cost points of the process step) × First-level human resource cost points = 1,308,485.68/800,414 × 7 = 11.44.
The sum of direct human resource costs per unit for each personnel type and indirect human resource costs per unit constitutes the human resource cost per unit for each process.
Unit human resource cost for “Attending Physician” process = Unit indirect human resource cost for “Attending Physician” process + Unit direct human resource cost for “Attending Physician” process = 120.51 + 47.74 = 168.25.
Unit human resource cost for “Physiotherapists” Process = Unit indirect human resource cost for “Physiotherapists” process + Unit direct human resource cost for “Physiotherapists” = 28.89 + 11.44 = 40.33.
The calculation of the unit cost for the nurse’s process step and the unit indirect cost is similar to that of the unit direct cost for the “attending physician” process step. Ultimately, the unit human resource cost for the impacted tooth extraction procedure is the sum of the unit costs corresponding to various process steps of the project, which amounts to 208.57 (168.25 + 40.33). The calculation process is detailed in Table 7. Based on this, the case also calculates the cost of an impacted tooth extraction project would be 186.13 yuan without considering the risk factor.
Table 7.
Calculations of unit human resource cost for medical projects
| Project name | Workload for the period | Type of process | First-level human resource | Second-level human resource | Direct cost per unit | Indirect cost per unit | Personnel cost per unit | Unit human resource costs for medical projects |
|---|---|---|---|---|---|---|---|---|
| Extraction of impacted tooth | 11,017 | Attending physician | 196 | 2,159,332 | 120.51 | 47.74 | 168.25 | 208.57 |
| Physiotherapists | 7 | 77,119 | 28.89 | 11.44 | 40.33 |
Comparative analysis of human resource cost accounting results
The cost accounting results presented in Table 8 provide a detailed comparison of the impacted tooth extraction procedure under different accounting methods. Building on this material, the paper further analyzes the comparative advantages of the IPC method.
Table 8.
Analysis and comparison of cost accounting results (in units: CNY)
| Project name | IPC method | IPC method without risk factors | ABC | TDABC | Fee scale | Differences between IPC method and ABC | Differences between IPC method and TDABC |
|---|---|---|---|---|---|---|---|
| Extraction of impacted tooth | 208.57 | 186.13 | 196.61 | 198.43 | 460 | 6.1% | 5.1% |
As shown in Table 8, under the IPC method, the cost of the impacted tooth extraction procedure is 208.57 yuan. Compared to the IPC method that does not consider the comprehensive technical level, the cost of the impacted tooth extraction project increased by 22.44 yuan. This indicates that by accounting for the risk coefficient, the IPC method more comprehensively captures the actual costs of the project and aligns more closely with the actual situation. The difference between the IPC method and Activity-Based Costing (ABC) is 11.96 yuan, with a difference percentage of 6.1%. This difference suggests that the IPC method is more efficient and applicable than ABC when considering the costs of medical service projects, which reflects the job levels and technical levels of medical personnel. Compared to the Time-Driven Activity-Based Costing (TDABC), the difference with the IPC method is 10.14 yuan, with a difference percentage of 5.1%. Since TDABC is primarily based on time, the IPC method is more comprehensive when considering factors such as the risk coefficient. This also indicates that the IPC method has certain advantages over TDABC in the impacted tooth extraction project, more comprehensively considering cost factors and making the cost accounting more accurate.
Through the analysis of these differences, the advantages of the IPC method in the impacted tooth extraction project become clear. Its consideration of the risk coefficient and its more comprehensive cost accounting approach enable it to better reflect the true costs of medical service projects in practical applications. For medical institutions, this method provides more scientifically sound and rational support for cost management and pricing decisions. The application of the IPC method in setting fee standards may also help elicit economic benefits and ensure quality of medical services. These cost accounting results similarly provide advantages for budget management, performance management, and cost compensation of medical institutions.
Table 9 presents a grouped analysis of cost results based on the comprehensive technical levels of 2023, as well as the differences in human resource cost accounting for stomatology medical projects under various costing methods. Negative differences indicate that the ICP method yields lower human resource cost accounting results compared to ABC and TDABC. As the technical risk level of the project increases, the cost accounting amounts under the IPC method are higher relative to ABC and TDABC. This suggests that for more complex and higher-level projects, the IPC method is more meticulous and accurate as it considers the costs of medical service projects, better reflecting the actual resource and technical inputs.
Table 9.
Comparison analysis of activity based costing (ABC) and time driven activity based costing (TDABC) with respect to IPC method
| Risk value of comprehensive technical factors for the 2023 edition | Differences between IPC and ABC (%) | Differences between IPC and TDABC (%) | Differences between IPC and IPC without risk factors (%) | Differences between IPC and ABC without risk factors (%) | Differences between IPC and TDABC without risk factors (%) |
|---|---|---|---|---|---|
| 1 | − 41.62 | − 47.90 | − 46.39 | 5.59 | − 1.35 |
| 2 | − 39.68 | − 42.32 | − 41.43 | 3.09 | − 0.94 |
| 3 | − 32.46 | − 33.35 | − 32.67 | 0.45 | − 0.93 |
| 4 | − 17.02 | − 22.67 | − 21.41 | 5.28 | − 1.40 |
| 5 | − 15.03 | − 15.89 | − 15.41 | 0.60 | − 0.53 |
| 6 | − 7.15 | − 6.16 | − 5.81 | − 1.41 | − 0.35 |
| 7 | 21.21 | 23.29 | 22.80 | − 1.44 | 0.31 |
| 8 | 10.89 | 10.78 | 12.21 | − 1.12 | − 1.27 |
| 10 | 32.80 | 53.30 | 49.62 | − 11.24 | 2.47 |
| Overall average | − 41.62 | − 47.90 | − 46.39 | 5.59 | − 1.35 |
Comparative advantages of the IPC method
The IPC method more completely embodies the principle of cost-effectiveness in medical cost accounting than either activity-based costing (ABC) or time-driven activity-based costing (TDABC). It simplifies the division of “activities” and does not differentiate between value-added and non-value-added activities. Instead, it uses “process steps” to encompass all aspects of medical services, facilitating more convenient cost accounting while ensuring accuracy. Moreover, the method takes into account the number of personnel, time consumption, and technical levels of different process steps, enhancing the precision of cost accounting and ensuring that the labor value of medical staff is appropriately reflected. The flexibility and convenience of the IPC method also make it more favorable for practical application and promotion.
Alignment of “process steps” with medical cost characteristics
On the one hand, the IPC method better incorporates factors such as time consumption and risk levels of “process steps” compared to traditional ABC, making the accounting work simpler and more operable. The challenge with traditional ABC lies in the excessive division of activities, which makes it difficult to collect cost driver parameters and follow complex steps. On the other hand, there is no need under the IPC method to further distinguish between value-added and non-value-added activities; this approach is consistent with clinical medical practices. Unlike the ABC method, which is applied to standard industrial products and differentiates between value-added activities and non-value-added activities, the division of “process steps” is more suitable for medical institutions. Medical service processes are a series of orderly activities systematically planned and executed to ensure medical quality. These processes include patient consultation, preliminary diagnosis, treatment planning, treatment implementation, rehabilitation guidance, and follow-up. In this process, all stakeholders (including medical institutions, medical staff, health insurance institutions, and patients) must work together to prioritize quality, to ensure diagnostic and treatment behaviors are safe and effective, and to prevent medical errors and accidents. Therefore, even “non-value-added activities” may be considered essential medical processes worth retaining.
Enhancing precision through “Points” calculation
Unlike the TDABC, the IPC method constructs a point library based on the division of process steps, which establishes detailed records of time and resources for each process step. This makes cost accounting more specific and realistic. The IPC method more fully considers the complexity and variability of different process steps, improving the accuracy of cost accounting. It takes into account not only time consumption but also technical difficulty and risk levels. Based on this logic, the IPC method can more accurately reflect the actual costs of medical service projects because it comprehensively considers various aspects of resource input. As a result, the accounting results under the IPC method provide a more comprehensive reflection of the costs of medical projects. This approach creates a more scientific basis for setting medical service prices and ensures the labor value of medical staff is rationally reflected.
Iterative optimization in application of the IPC method
The long-term tracking and statistical treatment inherent in the IPC method allows for continuous correction and updating of basic data. Through feedback from actual operations, medical institutions can obtain real data on human resource cost parameters in a timely manner, thereby constantly optimizing the content of the point library. This dynamic data updating process helps ensure the authenticity and accuracy of cost accounting, making it more reliable and flexible compared to ABC.
The IPC method can also adjust the points for different elements according to actual conditions, thus adapting to the constant changes and innovations of medical service projects. This flexibility makes the IPC method more adaptable to the special needs of different medical institutions and service projects and enhances its feasibility in practical application. As medical institutions continuously optimize their cost accounting models, they can gradually improve and adjust the point library to better reflect the actual situation of medical service projects. This positive spillover effect makes the IPC method useful not only in cost accounting but also in the internal management of medical institutions.
Complex example
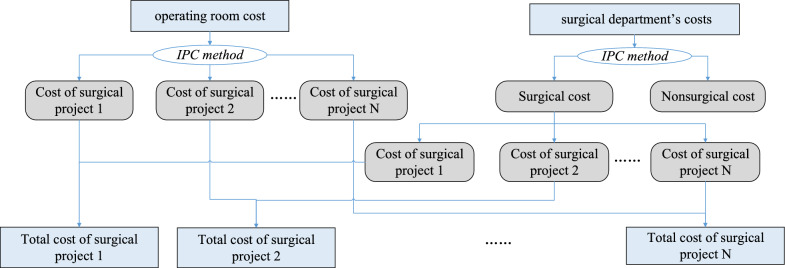
We use the cost accounting of surgical projects as an example to demonstrate that the IPC method is suitable for more complex medical projects. In hospital cost accounting, surgical project cost accounting is typically one of the most challenging and complex areas. This is because surgical projects involve various costs, and the process and resource consumption during surgery are highly complex and variable.
A typical surgery requires collaboration between the surgical department and the operating room. In Activity-Based Costing (ABC), surgical projects can be broken down into steps such as preoperative education, preoperative preparation, intraoperative operations, postoperative monitoring, and patient transfer. The difficulty with this approach lies in the excessive subdivision of tasks, making data collection more difficult and the process more cumbersome, thus increasing implementation complexity. In response, our approach is to calculate itemized costs separately along two lines: the operating room and the surgical department (as shown in Fig. 2).
Fig. 2.
Application of IPC method in surgical project
First Line: The Itemized Point Cost (IPC) method is used in the operating room to calculate the project costs of each surgery. The operating room costs are divided into labor costs (nursing procedures), non-billable surgical materials, surgical equipment depreciation, and operating room building depreciation. Each itemized cost is determined based on its respective cost driver, generating primary cost points. These primary points are multiplied by the number of surgeries performed during the period to obtain secondary cost points for each project (surgical project 1, surgical project 2, etc.). Finally, the total and unit costs of each surgical project are calculated by distributing the total costs based on the secondary points.
Second Line: Similarly, the surgical department’s costs are allocated to each surgical project using the IPC method, where labor refers to the doctor’s procedures.
Thus, the cost of a given surgical project is the sum of the costs from the operating room and the surgical department.
Suggestions on the application of IPC
In the process of promoting the point-based costing method, the scientific setting of point parameters, collaboration across departments, and the establishment of standards for the point-based costing method are all important pathways that must be carefully mapped out. First, the scientific setting of point parameters is the foundation for accurate cost accounting. Consideration of factors such as medical service duration, personnel numbers, etc. is essential. Second, inter-departmental collaboration is fundamental to the effective implementation of a point-based costing method; cross-departmental communication and collaboration mechanisms to achieve information sharing and task division are essential. Last, establishing and perfecting the implementation standards for the point-based costing method ensures the method is properly and efficiently promoted. This requires the standardization of calculation methods and steps, standardization of management applications, and standardization of result outputs.
Leveraging information technology for the evidence-based setting of point parameters
High-quality cost accounting requires data as the foundation, algorithms as the means, and computing power as the support. Among these three elements, “data” is crucial, because it allows implementation of various algorithms. The data required for cost accounting of medical service items can be divided into basic data related to revenue and expenditure details and standard cost driver parameter data. The standard cost driver parameter data refers to the standard (or average) resource consumption data for each medical project and includes items such as position rank, number of personnel, operation time, special non-chargeable consumable usage, and special equipment and usage time. These parameters are essential for allocating costs. The more detailed and accurate these parameters are determined, the closer the cost accounting results will be to the actual situation.
First, when determining point parameters, support for informatization is essential. For example, enhancing the interaction and sharing of data between different systems to ensure that the data for the point-based costing method can be matched and docked with other system data and achieving comprehensive data support and sharing are both equally important. Medical institutions can build a project cost survey platform to process granular-level income and cost data associated with the medical project provided by multiple information systems in the hospital (such as HIS, human resources system, materials/equipment systems, etc.). Institutions can also obtain the standard cost driver data for various medical service items carried out by clinical and medical technology departments through data sharing, online surveys, data uploading, and other data collection modes.
Second, once a data collection platform is established, data mining technology can be used to analyze the associations between data; in other words, it can correlate the “entire” data recorded in each information system, rather than relying solely on “sample” data. This can greatly improve the accuracy of the accounting results. For example, by reading the attendance scheduling data of every doctor, the operation information of each piece of equipment, and the usage status of each surgical consumable, robust project cost data can be summarized and calculated. Efficient and rapid data processing capabilities make such an accounting routine possible. At the same time, artificial intelligence systems can complete project cost survey work and even full-cost accounting work by utilizing their powerful deep-learning, computing, and analytical capabilities in conjunction with the existing information systems of the hospital. Ultimately, this strategy creates an intelligent cost accounting system for public hospitals and provides cost information crucial to the development of the hospital.
Last, continuous optimization and dynamic adjustment are still needed even after collecting and analyzing cost driver data and determining point parameters. After the establishment of the standard cost driver database, the hospital should regularly (in principle, every month) investigate the cost drivers of new medical projects and update the cost drivers of existing medical projects in a timely manner; these drivers may have changed due to technological innovation, new equipment purchases, changes in non-chargeable materials, and so on. Hospitals can also analyze abnormal data. In the case of an error in the selection of cost driver data, an analyst can further contact the clinical department to adjust the relevant driver data, forming a closed-loop optimization process within a given accounting period.
Business and financial collaborative governance through top-level design
Complex interconnections and interdependencies between various departments are common to all medical institutions, so cost accounting requires close cooperation and collaboration between departments, regardless of the method. Thus, inter-departmental collaboration to is essential to a point-based costing method.
First, it is necessary to optimize top-level design and establish cross-departmental collaboration mechanisms and communication channels. When promoting the point-based costing method, the hospital’s leadership must emphasize its importance; if a chief accountant is the professional person in charge of the roll-out, then the chief accountant must play an important role. In terms of arrangement of personnel, a survey work group should be formed by the hospital’s full-time cost accounting specialists, price specialists, and specialty business assistants. That work group will be responsible for the project survey work of the whole hospital or specialty, with third-party cost accounting service institutions providing auxiliary support. At the same time, each department should arrange medical staff familiar with the medical projects carried out by the department to participate in the survey work. Hospitals can also form a business expertise team to provide professional consultation on various related matters involving medical business resource consumption during the survey process.
Second, hospitals should maintain a dynamic tracking protocol for the usage of a point-based costing method. The promotion of the point-based costing method involves staff from various departments, and they need to be trained in the application of the point-based costing method and corresponding cost management measures. In addition, cross-departmental experience exchanges and case sharing activities should be organized. Such measures ensure that various departments learn from each other, discuss the experiences and lessons during the promotion process together, and continuously improve and enhance cost management work.
Last, hospitals must establish cross-departmental supervision and evaluation mechanisms. Promoting point-based costing methods is a long-term process, one that requires the establishment of cross-departmental supervision and evaluation mechanisms. These mechanisms can regularly evaluate and summarize the project cost accounting work, solve problems in a timely manner, adjust promotion strategies in a timely manner, and ensure the expected results of the promotion work are achieved.
Building a standard cost driver library and standardizing IPC method process
The standard cost drivers of medical projects must ensure the smooth implementation of the point-based costing method. Project cost accounting survey is a precise work. Thus, the required standard cost drivers involve the basic management of cost accounting, or quota management. This includes the labor quota, personnel quota, material consumption quota, equipment consumption quota, etc. required to complete a single project. However, if hospitals do not have a functioning department for quota management, then the formulation and modification of quota standards can’t efficiently occur. And when such fine-grained cost accounting is needed, a temporarily-formed team must be responsible for the work. The team’s familiarity with the work is going to determine whether the work can be carried out normally and what the quality of the work will ultimately be. These demands bring great difficulties to high-quality survey work. Therefore, local industry authorities and medical institutions can organize expert teams to meet the needs of different levels of hospitals and different specialty hospitals in the region. These teams can uniformly formulate “standard quotas” for the consumption of labor, materials, equipment, and housing required for project cost accounting. After the establishment of a standard point library, a unified standard can be used, which is easier to promote than ABC. In particular, small and medium-sized medical institutions can refer to low-cost applications. Then affiliated hospitals can refer to and apply these quotas in conjunction with the hospital’s own particular situation. Such measures can conserve investment and prevent unnecessary resource waste in the work of each hospital.
At the same time, standardizing the application of a point-based costing method is essential. Calculation methodologies and procedural steps must be clarified. This includes setting application rules and methods for medical process, time consumption, grade coefficient, technical difficulty coefficient, risk degree coefficient, and so on. Collection and sorting of points also must be clarified to ensure the calculation process of the IPC method is evidence-based, standardized, and transparent. Moreover, institutions must standardize the management of the point-based costing method at an institution level. This includes clarifying the scope and conditions of the IPC method’s application, which involves determining technical requirements of the point-based costing method in the cost accounting of medical service projects. Likewise, institutions must integrate supervision and evaluation mechanisms of the IPC method. Standardizing the application of the results of the point-based costing method is equally important. For example, institutions must clarify the presentation and interpretation methods of the IPC cost accounting results, stipulate the use range and purpose of the results, and guide medical institutions on how to formulate related management decisions and policies based on the results. Such measures will help institutions to both optimize resource allocation and improve the efficiency and quality of medical services. Finally, institutions deploying IPC methodology must dovetail their efforts with relevant policies, regulations, and international standards. This will ensure their efforts to integrate an IPC method complies with national policies and regulations. Such efforts will also promote interchange related to point-based costing methods on an international scale.
Conclusions
Based on RBRVS theory, this paper uses IPC method to calculate the cost of medical project, and takes the human cost accounting of stomatology department and complex surgical items as examples. The results of the case study show that the IPC method more completely embodies the principle of cost-effectiveness in medical cost accounting than either activity-based costing (ABC) or time-driven activity-based costing (TDABC). The IPC method takes the number of personnel, time consumption, and technical levels of different process steps into account, enhancing the precision of cost accounting and ensuring that the labor value of medical staff is appropriately reflected. The flexibility and convenience of the IPC method also make it more favorable for practical application and promotion.
Data and algorithms complement each other—high-quality data can enhance the effectiveness of algorithms, while effective algorithms can further improve data quality and utilization. In large comprehensive hospitals, the number of medical projects requiring cost accounting may exceed tens of thousands. Therefore, establishing a cost point database is a meticulous, complex, and essential system engineering task. As medical services evolve and technology advances, the cost driver parameters need to be updated and adjusted in a timely manner. However, manually reporting can be slow, making it difficult to quickly adapt to these changes, which in turn affects the timeliness and accuracy of cost accounting. Hence, acquiring standard cost driver parameter data is a broad and highly detailed task, requiring not only cost accounting theory and a culture of cost awareness across all staff, but also scientific research strategies, advanced information systems, and comprehensive data management.
Author contributions
Yingqi Li: conceptualization, methodology, project administration, supervision, writing—review and editing. Siyuan Liang: data curation, investigation, writing—original draft, writing—review and editing. Kui Qin: resources, data curation; Hongtong Su: validation, writing—original draft; Peiyong Xia (Corresponding author): conceptualization, funding acquisition, resources, supervision, writing—review and editing. All authors reviewed the manuscript.
Funding
This work was supported by the Project of Oriental Talents Program in 2022 (Shanghai People's Institute [2023] No.353-123) and Key research project of Shanghai Accounting Society in 2020 [SHKJ2020ZD01].
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Other operating expenses include: office expenses, utilities, gas fees, postage, property management fees, travel expenses, training fees.
Secondary cost items are classified as follows: personnel expenses (salary, bonus, welfare and social security), medical material costs(chargeable sanitary consumables and non-chargeable sanitary consumables), pharmaceutical costs(western medicine, Chinese medicine), fixed asset depreciation costs(medical equipment, houses and buildings), intangible asset amortization costs, medical risk fund extraction, and other operating expenses(office expenses, utilities, gas fees, postage, property management fees, travel expenses, training fees).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arnaboldi M, Lapsley I. Activity based costing in healthcare: a UK case study. Res Healthc Financ Manag. 2005;10(1):61–75. [Google Scholar]
- 2.Cogin JA, Ng JL, Lee I. Controlling healthcare professionals: how human resource management influences job attitudes and operational efficiency. Hum Resour Health. 2016;14:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.da Silva Etges APB, Ruschel KB, Polanczyk CA, Urman RD. Advances in value-based healthcare by the application of time-driven activity-based costing for inpatient management: a systematic review. Val Health. 2020;23(6):812–23. [DOI] [PubMed] [Google Scholar]
- 4.Emanuel EJ, Ubel PA, Kessler JB, Meyer G, Muller RW, Navathe AS, Volpp KG. Using behavioral economics to design physician incentives that deliver high-value care. Ann Intern Med. 2016;164(2):114–9. [DOI] [PubMed] [Google Scholar]
- 5.Fidanza A, Schettini I, Palozzi G, Mitrousias V, Logroscino G, Romanini E, Calvisi V. What is the inpatient cost of hip replacement? A time-driven activity based costing pilot study in an Italian public hospital. J Clin Med. 2022;11(23):6928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hofmann A, Ozawa S, Shander A. Activity-based cost of platelet transfusions in medical and surgical inpatients at a US hospital. Vox Sang. 2021;116(9):998–1004. [DOI] [PubMed] [Google Scholar]
- 7.Hsiao WC, Braun P, Dunn D, Becker ER. Resource-based relative values: an overview. JAMA. 1988;260(16):2347–53. [PubMed] [Google Scholar]
- 8.Ippolito A, Boni S, Cinque E, Greco A, Salis S. Using time-driven activity-based costing to establish a tariff system for home health care services. J Healthc Manag. 2016;61(6):436–47. [PubMed] [Google Scholar]
- 9.Johannesson M. The willingness to pay for health changes, the human-capital approach and the external costs. Health Policy. 1996;36(3):231–44. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan RS, Porter ME. How to solve the cost crisis in healthcare. Harv Bus Rev. 2017;89(9):46–52. [PubMed] [Google Scholar]
- 11.Kaplan RS, Witkowski M, Abbott M, Guzman AB, Higgins LD, Meara JG, Feeley TW. Using time-driven activity-based costing to identify value improvement opportunities in healthcare. J Healthc Manag. 2014;59(6):399–412. [PubMed] [Google Scholar]
- 12.Keel G, Savage C, Rafiq M, Mazzocato P. Time-driven activity-based costing in health care: a systematic review of the literature. Health Policy. 2017;121(7):755–63. [DOI] [PubMed] [Google Scholar]
- 13.Kim MS, Kim YH, Kim JS, Lee HJ. Nursing cost in operating room applying the resource-based relative value scale (RBRVS). J Korean Acad Nurs Adm. 2002;8(2):283–93. [Google Scholar]
- 14.Lüdemann C, Gerken M, Hülsbeck M. The role of human capital and stress for cost awareness in the healthcare system: a survey among German hospital physicians. BMC Health Serv Res. 2024;24(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCormack LA, Burge RT. Diffusion of Medicare’s RBRVS and related physician payment policies. Health Care Financ Rev. 1994;16(2):159. [PMC free article] [PubMed] [Google Scholar]
- 16.Pirankar SB, Ferreira AM, Vaz FS, Pereira-Antao I, Pinto NR, Perni SG. Application of ABC-VED analysis in the medical stores of a tertiary care hospital. Int J Pharmacol Toxicol. 2014;4(3):175–7. [Google Scholar]
- 17.Ramsey RH IV. Graduate: activity-based costing for hospitals. J Healthc Manag. 1994;39(3):385–96. [PubMed] [Google Scholar]
- 18.Riewpaiboon A, Malaroje S, Kongsawatt S. Effect of costing methods on unit cost of hospital medical services. Trop Med Int Health. 2007;12(4):554–63. [DOI] [PubMed] [Google Scholar]
- 19.Waters H, Abdallah H, Santillán D. Application of activity-based costing (ABC) for a Peruvian NGO healthcare provider. Int J Health Plann Manag. 2001;16(1):3–18. [DOI] [PubMed]
- 20.Peiyong X, Yang T. Application of itemized point cost method based on RBRVS in costing of surgical items. Health Econ Res. 2020;37(03):42–5. [Google Scholar]
- 21.Xia P, Xu G, Tong Y. Research and practice of point cost method in hospital project cost accounting. Chin J Hosp Adm. 2020;36(12):1002–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.