Abstract
Background
Compassion fatigue is a significant issue in nursing, affecting both registered nurses and nursing students, potentially leading to burnout and reduced quality of care. During internships, compassion fatigue can shape nursing students’ career trajectories and intent to stay in the profession. Identifying those at high risk is crucial for timely interventions, yet existing tools often fail to account for within-group variability, limiting their ability to accurately predict compassion fatigue risk.
Objectives
This study aimed to develop and validate a predictive model for detecting the risk of compassion fatigue among nursing students during their placement.
Design
A cross-sectional study was used to capture the prevalence and associations of compassion fatigue among nursing interns, as it allows for timely assessment of key influencing factors without requiring long-term follow-up.
Methods
A convenience sampling strategy was used to recruit 2256 nursing students from all ten public junior colleges in Hunan province in China between December 2021 and June 2022. Participants completed questionnaires assessing compassion fatigue, professional identity, self-efficacy, social support, psychological resilience, coping styles, and demographic characteristics. Predictors were selected based on prior literature and theoretical frameworks related to compassion fatigue in nursing. Latent profile analysis was used to classify compassion fatigue levels, and potential predictors were identified through univariate analysis and least absolute shrinkage and selection operator (LASSO) regression. Eight machine learning algorithms were applied to predict compassion fatigue, with performance assessed through cross-validation, calibration, and discrimination metrics. The best-performing model was further validated to ensure robustness.
Results
A three-profile model best fits the data, identifying low (55.73%), moderate (32.17%), and severe (12.10%) profiles for compassion fatigue. Generally, an area under the curve (AUC) above 0.700 is acceptable, and above 0.800 indicates good predictive performance. The AUC values for the eight machine learning models ranged from 0.644 to 0.826 for the training set and 0.651 to 0.757 for the test set, indicating moderate to good discriminatory ability. The eXtreme Gradient Boosting (XGBoost) performed best, with AUC values of 0.840, 0.768, and 0.731 in the training, validation, and test sets, respectively. Shapley Additive Explanation (SHAP) analysis interpreted the model by quantifying the contribution of each variable to the prediction, revealing that psychological resilience, professional identity, and social support were the key contributors to the risk of compassion fatigue. A user-friendly, web-based prediction tool for calculating the risk of compassion fatigue was developed.
Conclusions
The XGBoosting classifier demonstrates excellent performance, and implementing the online tool can help nursing administrators manage compassion fatigue effectively. It holds practical value for nursing education and practice by supporting early detection and intervention. Future research should validate its use across settings, and longitudinal studies could assess its long-term impact.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06505-9.
Keywords: Nursing student, Internship nonmedical, Compassion fatigue, Prediction model, Latent profile analysis, Machine learning
Background
Nursing is a profession defined by its commitment to compassion but also accompanied by significant stress. Nurses frequently witness patients’ suffering and distress while providing care and support. Prolonged exposure to such traumatic experiences can result in psychological distress, impairing their capacity to deliver optimal care [1–3]. This phenomenon, known as compassion fatigue, was first defined by Joinson in 1992, and it encompasses physical, psychological, and social dysfunction arising from continuous exposure to patient suffering or traumatic events [4]. Compassion fatigue, encompassing both burnout and secondary traumatic stress [5, 6], represents a complex phenomenon in nursing. Burnout stems from prolonged exposure to job-related stress, leading to emotional exhaustion and detachment, while secondary traumatic stress arises from indirect exposure to patients’ suffering. Together, these elements intensify the emotional and psychological exhaustion of nurses, contributing to a range of adverse outcomes such as musculoskeletal disorders, sleep disturbances, depression, diminished professional identity, and decreased work engagement [7–10].
Compassion fatigue is not exclusive to registered nurses; it also affects nursing students [11–14]. In China, pre-licensure nursing education includes both associate (three or five-year programs) and baccalaureate (four-year programs) tracks. These programs emphasize a combination of theoretical knowledge and practical skills. After completing on-campus theoretical studies, students are required to undertake at least eight months of clinical placement in secondary or higher-level hospitals. These students are referred to as nursing interns during this clinical placement period. A survey of 972 Chinese nursing interns revealed that 97.8% experienced moderate burnout, and 55.3% suffered from secondary traumatic stress [15]. High levels of compassion fatigue or burnout are associated with a higher intention to drop out, increasing attrition rates [16–20]. Additionally, burnout developed during educational programs may persist after graduation, impacting the health and retention of new nurses [20, 21]. Thus, compassion fatigue or burnout adversely affects the career development of nursing students. Early identification and intervention for those at risk of compassion fatigue are crucial to prevent worsening symptoms.
Current assessments of compassion fatigue primarily rely on survey-based tools [22], such as those developed by Figley and Stamm, including the Compassion Fatigue Self-Test [23], the Compassion Satisfaction and Fatigue Scale [24], the Compassion Fatigue Scale [25], the Compassion Fatigue Short Scale [26] and the Professional Quality of Life Scale [27]. While these tools have been widely used, they present notable limitations. For instance, tools that treat compassion fatigue as a combination of burnout and secondary traumatic stress can oversimplify their assessment by failing to address distinct dimensions, as highlighted in studies where these tools were unable to account for within-group variability or predict compassion fatigue effectively in nursing interns [22–25, 27]. Furthermore, despite its brevity, the Compassion Fatigue Short Scale needs to have defined cutoff values, making it difficult to distinguish between different risk levels, which has been problematic in research and clinical settings [26, 28]. Importantly, these tools primarily rely on total scores, which may mask individual differences and are focused on assessment rather than prediction [15, 16, 29, 30]. As a result, there is a pressing need for the development of predictive tools that assess and predict the risk of compassion fatigue among nursing interns, considering individual variability and providing actional insights for early intervention.
Several psychosocial factors, such as social support, coping strategies, self-efficacy, psychological resilience, and professional identity, have been identified as relevant to compassion fatigue among nursing students [15, 16, 31, 32]. These particular factors were chosen for this study based on their consistent associations with compassion fatigue and burnout risk in prior research. Specifically, these factors have been shown to either buffer or exacerbate stress responses in healthcare settings, making them strong candidates for predicting compassion fatigue. They are commonly examined in similar studies, providing a robust basis for compassion fatigue across different populations and settings. Moreover, psychosocial variables like educational background, academic major, program length, previous student leadership, and career intentions have also been linked to compassion fatigue or burnout [15, 31, 33, 34]. Demographic factors such as gender, residence, only-child status, monthly expenses, and internship-related characteristics such as the level of the internship hospital and the frequency of night shifts are also associated with compassion fatigue or burnout [32, 33, 35–37]. These variables were selected not only for their predictive value, as demonstrated in prior studies but also to capture a comprehensive understanding of the multifaceted influences on compassion fatigue among nursing students.
Compassion fatigue is a complex and dynamic phenomenon, making traditional “one-size-fits-all” approaches insufficient to capture its variability among nursing interns. Most existing studies rely on variable-centered approaches, typically measuring compassion fatigue through total scale scores, which overlook nuances within groups [15, 16, 31, 32, 38]. Latent profile analysis (LPA) is particularly suitable for this study because it identifies unobserved heterogeneity within a population, classifying individuals into distinct subgroups based on their responses to continuous variables. This method enables researchers to move beyond arbitrary cutoffs, allowing the identification of nuanced patterns in compassion fatigue across nursing interns [39, 40]. These subgroups provide the foundation for more tailored interventions, addressing the specific needs of each profile, which is especially beneficial in preventing and mitigating compassion fatigue in a targeted manner [41, 42]. While LPA is highly effective at identifying latent profiles, it lacks predictive capabilities. Its practical implementation is also complex, requiring significant expertise in both statistical methods and clinical practice to translate findings into actionable interventions. Moreover, LPA depends on high-quality data, poor data quality or missing information can lead to inaccurate results. These limitations can be mitigated when LPA is combined with machine learning. Machine learning algorithms are effective at handling complex data structures and learning patterns from large datasets, complementing LPA by providing predictive capabilities [43]. In this study, machine learning was employed to predict the likelihood of compassion fatigue by utilizing the classification results from LPA along with other relevant variables. Commonly used algorithms, such as random forest and multi-layer perceptron, were chosen for their robustness in handling multi-dimensional data and their interpretability, making them particularly suitable for predicting compassion fatigue risk among nursing interns. This dual approach of LPA and machine learning provides both a granular understanding of compassion fatigue and the ability to predict individual risk levels. Despite the complexity of these methods, the comprehensive framework they offer enhances our ability to assess and address this critical issue in nursing education.
The main objectives of this study are (1) to identify potential classifications of compassion fatigue among nursing interns using LPA, (2) to develop and validate machine learning models for predicting individual risk levels, and (3) to develop an online prediction tool for practical application. Generally speaking, this study will provide nursing educators and clinical supervisors with a practical resource to better support nursing interns. Meanwhile, this tool could facilitate early identification of high-risk individuals, enabling timely interventions and personalized support during internships, thus enhancing their well-being and overall performance.
Methods
Study design
This cross-sectional study, conducted from December 2021 to June 2022 with nursing interns at all ten public junior colleges in Hunan Province, China, aimed to capture a snapshot of compassion fatigue. While longitudinal studies could track changes over time, our objective was to develop and validate a predictive model based on current data. Although cross-sectional studies cannot establish causality, they efficiently identify risk profiles and contributing factors, providing valuable insights without the complexity of time-based analysis. The study adheres to guidelines outlined in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE, Supplementary file 1) and Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD, Supplementary file 2).
Participants
Participants were recruited using convenience sampling from all public junior colleges in Hunan province, China. While this method is efficient, it may introduce selection bias and limits generalizability. To address this, we included students from multiple colleges and recruited both 3-year and 5-year associate nursing program students to ensure a more diverse and representative sample. The inclusion criteria were: (1) enrollment in a three- or five-year associate nursing program, (2) active participation in a clinical internship lasting at least eight months in a secondary-level or above hospital, and (3) willingness to participate with informed consent. Nursing interns whose clinical practice was in clerical management or administration, without direct patient contact, were excluded.
Sample size
While there is no standardized method for calculating sample size in survey studies using machine learning techniques [44], a sample size of over 500 is typically recommended for LAP [45]. A review by Spurk et al. indicated that 53.4% of studies using LPA follow this rule [46]. To ensure adequacy in our study, we conducted a post-hoc power analysis, which revealed that a sample size of 322 participants provided sufficient power (> 0.800) to detect significant effects in the machine learning model. Although our sample size is below the recommended 500 for LPA, the combination of LPA and post-hoc power analysis supports that our sample size is appropriate for the study’s objectives.
Data collection
Data were collected using an online survey created on the WenJuanXing platform (https://www.wjx.cn), a widely used survey tool in China. The survey link was distributed through WeChat groups specifically created for this study, which included nursing interns in 10 public junior colleges across Hunan province. Full-time student counselors, responsible for managing nursing interns during their placements, facilitated recruitment by inviting interns to join the WeChat groups. Participants were provided with standardized information about the study, including its purpose, potential risks, and benefits. Participation was entirely voluntary, with anonymity fully guaranteed. Reminders were sent to non-responders one week after the initial invitation via WeChat groups, as no direct follow-up was conducted due to the anonymous nature of the data collection process. To ensure a diverse and representative sample, recruitment efforts targeted interns from various academic and clinical backgrounds. All survey questions were mandatory to reduce missing data, and each IP address was restricted to one submission. Identical, patterned, or invalid responses were excluded to maintain data quality. After excluding 149 invalid responses, the final sample consisted of 2256 valid responses, resulting in a 93.8% effective response rate.
Instruments
General demographic information collection table
A self-designed table collected sociodemographic data, including gender, academic major, program length, place of residence, only-child status, monthly expenditure, previous experience as a student leader, hospital level during an internship, number of night shifts per month, and career intentions. This set of variables was chosen to comprehensively capture factors potentially influencing compassion fatigue, as identified in previous studies.
The compassion fatigue short scale
The Compassion Fatigue Short Scale, developed by Adams et al., was chosen due to its widespread use and strong psychometric properties in healthcare settings, particularly in nursing populations. It effectively captures secondary traumatic stress and job burnout [26], which are critical components of compassion fatigue. We selected the Chinese version validated by Sun (2015) [28], as it demonstrated strong reliability and validity in Chinese nursing populations, making it well-suited for our study’s demographic. In addition to the good internal consistency reflected by Cronbach’s alpha coefficients ranging from 0.87 to 0.95, the scale’s construct validity was confirmed using exploratory and confirmatory factor analyses, supporting its two-dimensional structure. Its brevity, with only 13 items, also made it practical for use with a large sample within limited time constraints. In this study, the overall Cronbach’s alpha coefficient for the Chinese version was 0.92.
The professional identity scale
We selected the Professional Identity Scale, which was developed by Brown et al. to assess professional identity in healthcare professionals [47]. The scale only includes ten items, therefore its concise provides a practical yet comprehensive assessment, making it ideal for large-scale surveys. Higher scores indicate a more robust professional identity. The Chinese version, translated and validated by Lu et al., demonstrated adequate internal consistency, with a Cronbach’s alpha coefficient of 0.82 [48], confirming its suitability for measuring professional identity among Chinese nursing interns. The content validity of this scale was ensured through expert consultations during its initial development, confirming its relevance in capturing professional identity dimensions in healthcare settings. In this study, the overall Cronbach’s alpha coefficient of the Chinese version was 0.80.
The general self-efficacy scale
The General Self-Efficacy Scale, developed by Schwarzer and Jerusalem (1995) [49], was chosen for its robustness in measuring self-efficacy across various populations. The Chinese version, validated by Zeng et al. [50], exhibited strong internal consistency and criterion validity in multiple studies, with a Cronbach’s alpha coefficient of 0.89 in this study, reinforcing its reliability. In addition to Cronbach’s alpha, previous studies have confirmed the scale’s construct validity via factor analysis, and its cross-cultural adaptability has made it a reliable tool for self-efficacy assessment across diverse populations, including healthcare workers.
The perceived social support scale
The Perceived Social Support Scale, developed by Zimet et al. [51], was selected for its strong psychometric properties and widespread use in healthcare research. The Chinese version, translated by Jiang [52] and modified by Yan et al. [53], has been validated extensively, demonstrating excellent internal consistency (Cronbach’s α = 0.85) and test-retest reliability (Cronbach’s α = 0.87) [53]. This scale includes 12 items across three dimensions: family support (items 3, 4, 8, 11), friend support (items 6, 7, 9, 12), and other support (items 1, 2, 5, 10). Responses range from 1 (strongly disagree) to 7 (strongly agree), resulting in a total score of 12 to 84. Higher scores indicate higher levels of perceived social support. Its ease of administration, with just 12 items, was an added benefit, facilitating its use in large-scale surveys without overburdening participants. In the present study, the Chinese scale version achieved an overall Cronbach’s alpha coefficient of 0.92.
The 10-item connor-davidson resilience scale
We selected the 10-item Connor-Davidson Resilience Scale, a refinement by Campbell-Sills of the original scale developed by Connor and Davidson [54, 55], due to its strong track record in measuring resilience in healthcare professionals. This unidimensional scale comprises ten items, each rated on a 5-point scale (0–4), with higher scores indicating greater resilience. The Chinese version of the scale, validated by Ye in 2016 [56], has been used in nursing populations, exhibiting good reliability, with a Cronbach’s α coefficient of 0.851 [34]. The scale’s validation studies included exploratory and confirmatory factor analyses supporting its construct validity in Chinese nursing samples. In the present study, the overall Cronbach’s α coefficient for the scale was 0.93.
Simple coping style questionnaire
The simple coping style questionnaire, adapted by Xie et al. from Folkman and Lazarus’ Ways of Coping Questionnaire [57, 58], was chosen for its ability to capture both positive and negative coping strategies, which are key factors developing and managing compassion fatigue. In this 20-item scale, each item is rated on a Likert four-point scale, with 1 indicating “do not take” and with 4 indicating “often take”. Higher scores in the positive coping style dimension indicate a greater likelihood of adopting positive coping strategies, while higher scores in the negative coping style dimension indicate a greater likelihood of adopting negative coping strategies. The scale’s translation and adaptation have been validated in Chinese populations, demonstrating psychometric solid properties with a Cronbach’s α coefficient of 0.90 [57]. Factor analyses conducted in previous studies further confirmed the two-dimensional structure of the scale, validating its use for assessing coping styles in Chinse nursing populations. The scale achieved an overall Cronbach’s α coefficient of 0.87 in the present study.
Statistical analyses
Descriptive and univariate analysis
Descriptive statistics summarized the general characteristics of the participants. Continuous variables, which did not follow a normal distribution, were represented as median and inter-quartile range, while categorical variables were shown as numbers and percentages. Univariate analysis identified predictive factors for compassion fatigue or burnout using the Mann-Whitney U test, chi-squared test, or Fisher’s exact test. The candidate factors included demographic characteristics, professional identity, self-efficacy, social support, psychological resilience, and coping styles. Analyses were performed using SPSS 26.0 (IBM Corp., Armonk, NY, USA), with a significance threshold of p < 0.05 for the two-sided test.
Handling of missing data
Although the survey required responses to all questions to minimize missing data, any instances of incomplete data were addressed systematically. If missing data occurred, cases were excluded from the final analysis to avoid introducing bias. Given the large sample size, excluding these cases did not significantly affect the study’s statistical power. No imputation methods were employed, as missing data were minimal, and excluding incomplete cases ensured that only complete data were included in both the statistical and machine learning analyses.
Latent profile analysis
LPA was conducted using the 13 items from the Compassion Fatigue Short Scale as indicators, employing robust maximum likelihood estimation to identify subgroups of compassion fatigue symptoms. To determine the optimal number of latent profiles, several statistical criteria were employed: entropy, the Lo-Mendell-Rubin likelihood ratio test (LMR), the bootstrap likelihood ratio test (BLRT), Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and adjusted Bayesian Information Criterion (aBIC) [59–61]. Each criterion contributed to assessing model fit and determining the appropriate number of profiles. Entropy measures classification accuracy, with values range from 0 to 1, where higher values indicate better separation between latent classes. An entropy value > 0.80 was chosen based on prior methodological recommendations [59]. as it ensures accurate profiles assignment and minimizes overlap between groups, which is critical for reliable model interpretation. LMR and BLRT statistics compared the k-class model to the (k-1) class model, with significant p-values indicating a better fit for more complex k-class model [59]. Lower AIC, BIC, and aBIC values indicated better model fit by balancing model complexity with goodness of fit [60, 62]. A scree plot was used to visually examine aBIC values, identifying the “elbow” point where the slope begins to flatten, signaling the optimal number of classes. This visual tool, along with other statistical criteria, guided the final selection of latent profiles [63]. Analyses were conducted using Mplus version 8.3 [63]. Ultimately, the combinations of these fit criteria, supported by theoretical considerations, determined the final number of latent profiles. To facilitate the construction of the subsequent predictive model, following recommendations from previous studies [63, 64], we assigned individuals who belonged to the latent profile representing the lowest level of symptoms or risks as “non-cases,” while other individuals were considered “cases.”
Features selection
After determining the optimal model and defining classifications, we assessed differences in some sociodemographic characteristics, professional identity, self-efficacy, social support, psychological resilience, and coping styles between the “non-cases” and “cases” groups. Significant variables from the univariate analysis (p ≤ 0.05) were further analyzed using the Least Absolute Shrinkage and Selection Operator (LASSO) regression, a technique that penalizes regression coefficients to optimize the model by retaining only significant predictors [65]. This approach handles complex covariance structures and improves predictive accuracy. LASSO regression was performed using Lasso CV with 10-fold cross-validation.
Development and evaluation of machine learning models learning
Eight machine learning algorithms were employed to develop and compare models for predicting the risk of compassion fatigue, including logistic regression, support vector machine, random forest, multi-layer perceptron, extreme gradient boosting (XGBoost), gradient boosting decision trees, Gaussian naive Bayes, and adaptive boosting. All models were implemented using Python 3.7, with the “xgboost 2.0.1” package for XGBoost and the “scikit-learn 1.1.3” package for the remaining algorithms. Hyperparameter tuning was performed for each algorithm using grid search with cross-validation to optimize the model performance. For each model, hyperparameters were selected based on cross-validated accuracy and the area under the receiver operating characteristic curve (AUC) on the training set. The optimal configuration was chosen by maximizing these metrics. Additionally, For more computationally intensive models, randomized search was used to identify the best configurations efficiently. Models were trained and validated using bootstrap resampling, with a 7:3 training-to-testing ratio. Performance was evaluated using metrics such as area under the receiver operating characteristic curve (ROC), accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and F1 score. Calibration was assessed by comparing predicted and observed incidence of “cases.”
Model optimization and evaluation
To ensure robustness and mitigate overfitting, 10-fold cross-validation assessed predictive performance. The dataset was randomly divided into ten equal parts, with training and validation repeated five times. Model discrimination was evaluated using ROC analysis and quantified by AUC. Calibration plots assessed the agreement between predicted probabilities and actual outcomes. Decision curve analysis (DCA) estimated the clinical utility and net benefit. Feature importance was assessed using Shapley additive explanation (SHAP) analysis, with higher absolute SHAP values indicating a greater impact on predictions [66]. Additionally, we explored the distribution of feature values and their relationship with model predictions to gain further insights into model behavior. SHAP analysis was conducted using the “shap 0.43.0” package.
Ethical considerations
Institutional Review Board approval was granted for this study by the institution review board of Hunan Traditional Chinese Medical College, with an approval number of YX202212001.
Results
Descriptive statistics
Data were collected from 2256 nursing interns, with notable trends in participants’ demographics and internship conditions. A significant majority of participants were female (2077, 92.07%) and from rural areas (1784, 79.08%), reflecting the widespread recruitment of nursing students from these regions. Most participants were non-only children (1962, 86.97%), suggesting stronger family support systems that may buffer stress. Economically, the majority reported a monthly expenditure between 1000 and 2000 RMB (1574, 69.77%). A substantial portion (1660, 73.58%) were enrolled in nursing programs, with most in three-year programs (1736, 76.95%), indicating potential socioeconomic challenges that influence stress and coping. Internship conditions revealed that most students worked in tertiary hospitals (1708, 75.71%) and typically worked 3 to 4 night shifts per month (1037, 45.96%), factors likely contributing to compassion fatigue due to the high-intensity environment. Despite these challenges, 86.13% of participants expressed a strong desire to pursue a nursing career, which may help mitigate emotional exhaustion linked to compassion fatigue. Psychological assessments revealed median scores of 39.00 for professional identity, 2.800 for self-efficacy, 58.00 for social support, 23.00 for psychological resilience, and 34.00 for coping style. Further details of participants’ characteristics are presented in Table 1.
Table 1.
Univariate analysis of influencing factors of compassion fatigue of nursing interns
| Variable | N (%) | Non-case a | Case b | Statistics | p |
|---|---|---|---|---|---|
| Academic major, n (%) | 15.358 | < 0.001 | |||
| Nursing | 1660 (73.58) | 973 (76.80) | 687 (69.46) | ||
| Midwifery | 596 (26.42) | 294 (23.20) | 302 (30.54) | ||
| Length of schooling, n (%) | 1.452 | 0.228 | |||
| 3-year | 1736 (76.95) | 963 (76.01) | 773 (78.16) | ||
| 5-year | 520 (23.05) | 304 (23.99) | 216 (21.84) | ||
| Gender, n (%) | 14.759 | < 0.001 | |||
| Male | 179 (7.93) | 125 (9.87) | 54 (5.46) | ||
| Female | 2077 (92.07) | 1142 (90.13) | 935 (94.54) | ||
| Residence, n (%) | 0.167 | 0.683 | |||
| Urban | 472 (20.92) | 269 (21.23) | 203 (20.53) | ||
| Rural | 1784 (79.08) | 998 (78.77) | 786 (79.47) | ||
| Only child or not, n (%) | 0.988 | 0.320 | |||
| Yes | 294 (13.03) | 173 (13.65) | 121 (12.24) | ||
| No | 1962 (86.97) | 1094 (86.35) | 868 (87.76) | ||
| Monthly expenses, n (%) | 0.447 | 0.800 | |||
| <1000 RMB | 420 (18.62) | 242 (19.10) | 178 (18.00) | ||
| 1000–2000 RMB | 1574 (69.77) | 879 (69.38) | 695 (70.27) | ||
| 2001–3000 RMB | 262 (11.61) | 146 (11.52) | 116 (11.73) | ||
| Whether as a student cadre, n (%) | 0.035 | 0.851 | |||
| Yes | 1172 (51.95) | 656 (51.78) | 516 (52.17) | ||
| No | 1084 (48.05) | 611 (48.22) | 473 (47.83) | ||
| Hospital level during internship, n (%) | 6.498 | 0.011 | |||
| Tertiary | 1708 (75.71) | 985 (77.74) | 723 (73.10) | ||
| Secondary | 548 (24.29) | 282 (22.26) | 266 (26.90) | ||
| Frequency of night-shift per month, n (%) | 8.868 | 0.031 | |||
| 0–2 | 803 (35.60) | 468 (36.94) | 335 (33.87) | ||
| 3–4 | 1037 (45.96) | 590 (46.57) | 447 (45.20) | ||
| 5–6 | 278 (12.32) | 145 (11.44) | 133 (13.45) | ||
| >6 | 138 (6.12) | 64 (5.05) | 74 (7.48) | ||
| Career intention, n (%) | 79.820 | < 0.001 | |||
| Yes | 1943 (86.13) | 1164 (91.87) | 779 (78.77) | ||
| No | 313 (13.87) | 103 (8.13) | 210 (21.23) | ||
| Professional identity, median (IQR) | 39.00 (34.00, 43.00) | 41.00 (37.00, 44.00) | 36.00 (31.00, 40.00) | 17.774 | < 0.001 |
| Self-efficacy, median (IQR) | 2.800 (2.50, 3.000) | 2.80 (2.60, 3.00) | 2.70 (2.40, 3.00) | 10.160 | < 0.001 |
| Social support, median IQR) | 58.00 (50.00, 66.00) | 61.00 (53.00, 69.00) | 54.00 (48.00, 61.00) | 13.058 | < 0.001 |
| Psychological resilience, median (IQR) | 23.00 (20.00, 29.00) | 26.00 (21.00, 30.00) | 20.00 (18.00, 25.00) | 16.793 | < 0.001 |
| Coping style, median (IQR) | 34.00 (27.00,4 0.00) | 34.00 (27.00, 40.00) | 33.00 (27.00, 39.00) | 2.691 | 0.007 |
Note: IQR, Interquartile spacing; CF, compassion fatigue. a:“non-cases” refers to nursing interns with low levels of compassion fatigue; b: “cases” refers to nursing interns with moderate to severe levels of compassion fatigue. The bold p values indicate statistical significance
Latent profiles of nursing students’ compassion fatigue
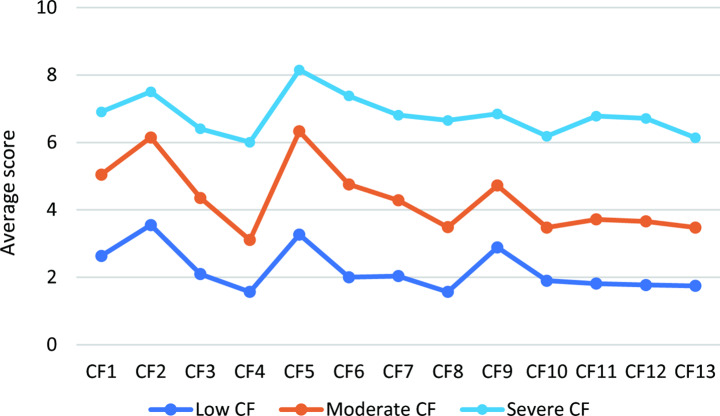
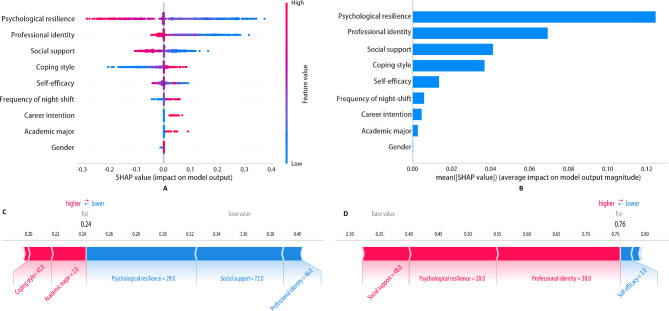
Our LPA, ranging from one to four latent classes, produced models with fit indices detailed in Table 2. All classifications demonstrated excellent separation of classes, with entropy values consistently exceeding 0.9, indicating excellent separation of classes. The BLRT was statistically significant across all models, while the LMR was significant only for the one to three-class models. As the number of classes increased, the AIC, BIC, and aBIC values progressively decreased, and the scree plot of aBIC flattened after the three-class model (Fig. 1), suggesting a point of diminishing returns. Based on statistical criteria, interpretability, and parsimony, the three-class model was selected as the optimal, with significant implications for future research and intervention strategies.
Table 2.
Goodness of fit statistics for 1 to 4 class models
| Class | AIC | BIC | aBIC | Entropy | LMR(p) | BLRT(p) | Sample proportion (%) per class |
|---|---|---|---|---|---|---|---|
| 1 | 135405.166 | 135553.921 | 135471.315 | n.a. | n.a. | n.a. | n.a. |
| 2 | 125201.556 | 125430.410 | 125303.324 | 0.935 | < 0.001 | < 0.001 | 71.37/28.63 |
| 3 | 122468.063 | 122777.016 | 122605.449 | 0.908 | < 0.001 | < 0.001 | 55.73/32.17/12.10 |
| 4 | 121328.755 | 121717.807 | 121501.759 | 0.916 | 0.3132 | < 0.001 | 25.67/55.70/8.23/10.40 |
Note: AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; aBIC, adjusted Bayesian Information Criterion; LMR, Lo–Mendell–Rubin; BLRT, bootstrap likelihood ratio test; n.a., not applicable. An entropy value of more than 0.80 indicates good discrimination. Significant results from LMR and BLRT tests indicate that the more complex model (k-class) fit the data better. Lower AIC, BIC, and aBIC values indicate better model fit
Fig. 1.
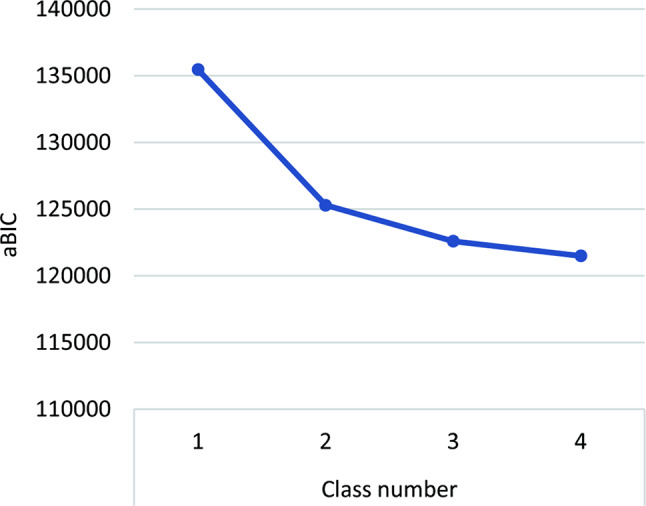
Scree plot of aBIC from LPA analysis. The “elbow” point in the plot, where the slope begins to flatten, indicates the turning point. aBIC, adjusted Bayesian information criterion; LPA, latent profile analysis
Table 3 presents the average latent class probabilities for the most likely latent class membership in the three-class model (0.968, 0.940, and 0.960), indicating reasonable classification and good distinction. The distribution and conditional means of the Compassion Fatigue Short Scale items for each class in the three-class model are illustrated in Fig. 2. Based on the conditional means of the items for each class, Class 1 (n = 1257, 55.73%) was defined as the “low compassion fatigue” group, Class 2 (n = 726, 32.17%) as the “moderate compassion fatigue” group, and Class 3 (n = 273, 12.10%) as the “severe compassion fatigue” group. Class 1 consists of interns with lower levels of compassion fatigue, likely benefiting from solid coping strategies. Interventions for this group should focus on maintaining resilience to prevent future escalation. Class 2 shows noticeable emotional strain, and to avoid progression, these interns may benefit from targeted support, such as stress management and self-care practices. Class 3 exhibits significant emotional exhaustion and detachment, indicating a need for intensive mental health support and monitoring to prevent burnout. These profiles offer valuable insights for tailoring interventions to different risk levels, enabling early identification and targeted support for nursing interns.
Table 3.
Average latent class probabilities for most likely latent class membership by latent class
| Latent class | Latent class membership | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| 1 | 0.968 | 0.032 | 0.000 |
| 2 | 0.043 | 0.940 | 0.018 |
| 3 | 0.000 | 0.040 | 0.960 |
The average latent class probabilities for most likely latent class membership by latent class reflects the classification accuracy, with higher diagonal values indicating greater accuracy in classifying individuals into the correct latent class
Fig. 2.
Three profiles of the best-fitting three-class pattern based on the Compassion Fatigue Short Scale
Influencing factors of nursing students’ compassion fatigue
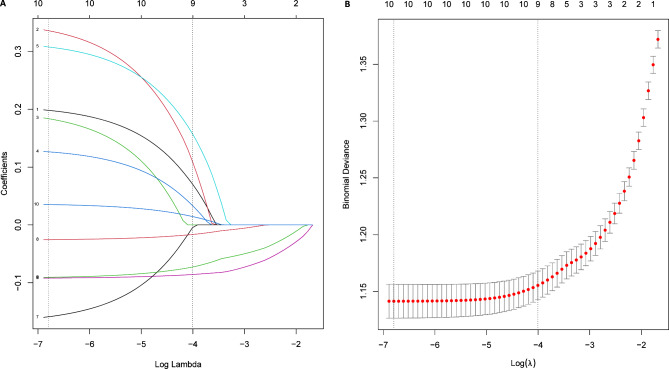
LAP identified participants in the “low compassion fatigue” group as “non-cases” (i.e., without compassion fatigue), and those in the “moderate compassion fatigue” and “severe compassion fatigue” groups as “cases” (i.e., potentially experiencing compassion fatigue). Univariate analysis revealed significant differences between these groups in major (χ2 = 15.358, p < 0.001), gender (χ2 = 14.759, p < 0.001), level of internship hospital (χ2 = 6.498, p = 0.011), night shifts frequency (χ2 = 8.868, p = 0.031), career intention (χ2 = 79.820, p < 0.001), professional identity (z = 17.774, p < 0.001), self-efficacy (z = 10.160, p < 0.001), social support (z = 13.058, p < 0.001), psychological resilience (z = 16.793, p < 0.001), and coping style (z = 2.691, p = 0.007) (see Table 1). These ten variables were included in the LASSO model, and nine key features were retained for developing the prediction model: major, gender, frequency of night shifts per month, career intention, professional identity, self-efficacy, social support, psychological resilience, and coping style (see Fig. 3). Gender differences may reflect cultural expectations. Female nursing students often experience greater emotional labor and are more likely to use emotion-focused coping strategies, which could increase their vulnerability to compassion fatigue. In contrast, male students may rely on problem-solving coping strategies, which could serve as a buffer. Career intention was a strong predictor. Uncertainty or dissatisfaction with nursing profession may increase emotional burden. Those weaker career commitment may internalize challenges, potentially exacerbating fatigue. Although Coping style showed a weaker effect than professional identity and social support, this suggests that coping strategies alone may not fully mitigate fatigue without additional psychological or social support. Similarly, night shift frequency had less impact, indicating the greater importance of psychological and social factors in compassion fatigue.
Fig. 3.
Feature selection based on the LASSO regression. Coefficient profile (A) and penalty plot (B). The minimum criteria and the one standard error of the minimum criteria were chosen as the optimal values for the drawn dotted vertical lines
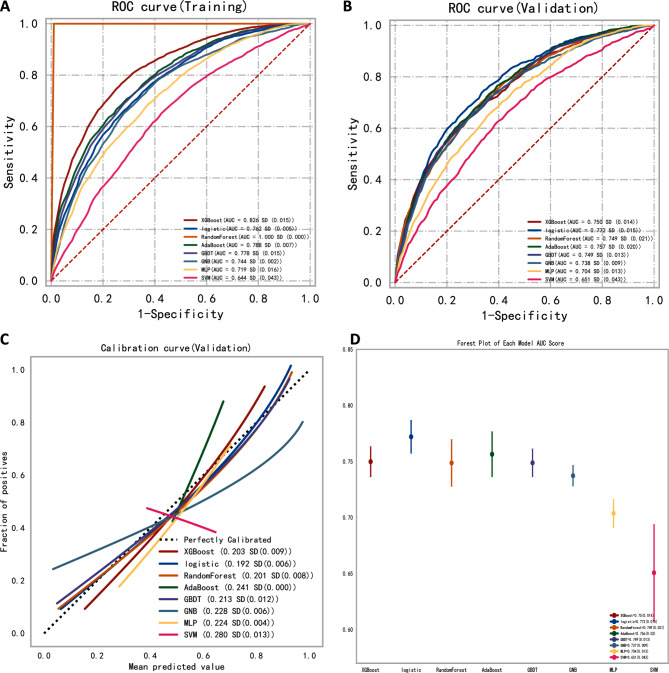
Comparison of multiple classification models
We compared eight machine learning models for predicting the risk of compassion fatigue in nursing interns. The XGBoost model outperformed others, showing high accuracy and stability across both training and validation sets. This is due to its regularization techniques and iterative boosting, which help prevent overfitting and improve generalization. In contrast, the Random Forest models overfitted the training data, leading to a drop in validation accuracy, likely because it lacks the same level of regularization as XGBoost and is prone to capturing noise in the training data. Other models, such as Logistic Regression, Support Vector Machine, and Multi-Layer Perceptron, showed weaker performance. Logistic regression struggled with non-linear feature interactions, Support Vector Machine was sensitive to hyperparameters, and Multi-Layer Perceptron required more tuning to handle complex relationships. The results, presented in Table 4; Fig. 4, provide a detailed comparison of the models’ ROC curves in the training and validation sets (Fig. 4A and B), the calibration plots (Fig. 4C), and the forest plot with the AUC score results (Fig. 4D). These results highlighted XGBoost’s balance between complexity and generalization, which led to its selection as the final model See Table 5.
Table 4.
Predictive performance of the eight machine learning techniques in the training and validation sets for compassion fatigue of nursing interns
| Models | AUC (95% CI) | Accuracy | Sensitivity | Specificity | PPV | NPV | F1score |
|---|---|---|---|---|---|---|---|
| Training set | |||||||
| XGBoost | 0.826 (0.810, 0.842) | 0.748 | 0.771 | 0.731 | 0.697 | 0.797 | 0.732 |
| LR | 0.762 (0.744, 0.780) | 0.700 | 0.663 | 0.730 | 0.663 | 0.737 | 0.659 |
| RF | 1.000 (1.000, 1.000) | 0.999 | 1.000 | 1.000 | 1.000 | 0.999 | 1.000 |
| AdaBoost | 0.788 (0.771, 0.805) | 0.709 | 0.731 | 0.694 | 0.657 | 0.768 | 0.688 |
| GBDT | 0.778 (0.761, 0.795) | 0.707 | 0.711 | 0.699 | 0.665 | 0.742 | 0.687 |
| GNB | 0.744 (0.726, 0.762) | 0.686 | 0.712 | 0.667 | 0.631 | 0.746 | 0.667 |
| MLP | 0.719 (0.700, 0.738) | 0.654 | 0.703 | 0.617 | 0.587 | 0.729 | 0.639 |
| SVM | 0.644 (0.624, 0.664) | 0.611 | 0.677 | 0.562 | 0.548 | 0.688 | 0.605 |
| Validation set | |||||||
| XGBoost | 0.750 (0.732, 0.768) | 0.679 | 0.643 | 0.730 | 0.613 | 0.738 | 0.627 |
| LR | 0.772 (0.755, 0.789) | 0.707 | 0.710 | 0.709 | 0.665 | 0.747 | 0.684 |
| RF | 0.749 (0.731, 0.767) | 0.682 | 0.696 | 0.684 | 0.708 | 0.673 | 0.701 |
| AdaBoost | 0.757 (0.739, 0.775) | 0.677 | 0.668 | 0.722 | 0.608 | 0.751 | 0.635 |
| GBDT | 0.749 (0.731, 0.767) | 0.679 | 0.624 | 0.753 | 0.638 | 0.712 | 0.630 |
| GNB | 0.738 (0.720, 0.756) | 0.671 | 0.661 | 0.711 | 0.603 | 0.738 | 0.630 |
| MLP | 0.704 (0.685, 0.723) | 0.637 | 0.696 | 0.610 | 0.577 | 0.707 | 0.630 |
| SVM | 0.651 (0.631, 0.671) | 0.612 | 0.694 | 0.552 | 0.548 | 0.685 | 0.611 |
Note: AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; LR, logistic regression; SVM, support vector machine; RF, random forest; GBDT, gradient boosting decision tree; MLP, multi-layer perceptron; XGBoost, extreme gradient boosting; GNB, Gaussian naive Bayes; AdaBoost, adaptive boosting; CI, confidence interval
Fig. 4.
Construction and comparison of eight ML models. ROC curves of eight ML algorithms for predicting psychological distress in the train (A) and validation (B) sets as well as calibration curves (C) and forest plot of various models (D). ROC, receiver operating characteristic; ML, machine learning
Table 5.
Performance of the XGBoost classification model for predicting the risk of compassion fatigue of nursing interns
| Models | AUC (95% CI) | Accuracy | Sensitivity | Specificity | PPV | NPV | F1 score |
|---|---|---|---|---|---|---|---|
| Training set | 0.840 (0.825, 0.855) | 0.761 | 0.720 | 0.793 | 0.730 | 0.788 | 0.723 |
| Validation set | 0.768 (0.738, 0.798) | 0.704 | 0.653 | 0.789 | 0.660 | 0.741 | 0.653 |
| Test set | 0.731 (0.698, 0.764) | 0.656 | 0.770 | 0.581 | 0.607 | 0.704 | 0.679 |
Note: AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value. XGBoost, extreme gradient boosting; CI, confidence interval
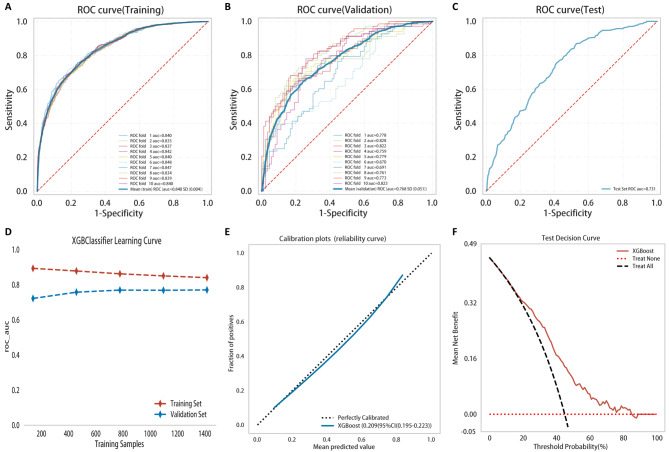
Model optimization
The XGBoost model, identified as the best performer in predicting compassion fatigue risk, was optimized using hyperparameter tuning to enhance predictive accuracy. The process involved adjusting parameters such as the learning rate and the number of estimators, improving the model’s overall performance by balancing bias and variance more effectively. This tuning process helped control overfitting and enhanced generalization to unseen data. Consequently, the XGBoost model selected nine pre-identified variables as input features, and a 10-fold cross-validation strategy was employed to ensure that 90% of the data was used for training and 10% for validation. The ROC curves and AUC values (shown in Fig. 5A-C) demonstrate the model’s strong discriminative ability, with AUC values of 0.840, 0.768, and 0.731 across the training, validation, and test sets. The slight decline in AUC suggests some overfitting from the training to validation. However, the learning curve (Fig. 5D) shows that the error between the training and validation sets gradually converged, indicating effective learning. Calibration plot (Fig. 5E) confirmed that predicted probabilities aligned well with actual outcomes.
Fig. 5.
Development and evaluation of XGBoost classification model. ROC curves of XGBoost using the 5-fold cross-validation in the training (A), validation (B) and test (C) sets, respectively. D-F represent machine learning curve, calibration curve for XGBoost, and decision curve for XGBoost classification model, respectively. ROC, receiver operating characteristic
While ROC curves, AUC, and calibration plots are useful validation tools, they have certain limitations. ROC curves and AUC values primarily assess discriminative ability but may not fully reflect the clinical utility of the model in practice, especially in populations with different demographic or clinical characteristics. Calibration plots, while helpful for comparing predicted and actual probabilities, may not generalize well to populations with different compassion fatigue prevalence. Given the study’s focus on nursing interns in a specific region, caution is advised when applying these findings to other settings. DCA (Fig. 5F) demonstrated significant net benefits below a 70% risk threshold, supporting the model’s effectiveness in real-world applications.
Model interpretation
Figure 6 illustrates the impact of various features on the prediction outcomes of the model. As shown in Fig. 6A, the SHAP summary plot indicates that psychological resilience, professional identity, and social support are the features with the most significant influence on the model’s output. Figure 6B, the mean absolute SHAP values bar chart, further confirms this finding. Figure 6C and D decompose the feature contributions for two sample students, demonstrating the individual-level impact of these features on risk prediction. These figures identify which feature values significantly affect the final risk prediction scores and cause them to fluctuate.
Fig. 6.
Interpretation of the results of XGBoost classification model based on the SHAP method. SHAP summary chart (A) and bar chart (B). The left dot plot represents the direction of contribution of each value of each variable, with red indicating larger values and blue indicating lower values of each variable. The right bar plot represents the importance of the variables and their overall contribution to the model predictions. C-F indicates that the SHAP scores explain the predicted risk of compassion fatigue in two subjects
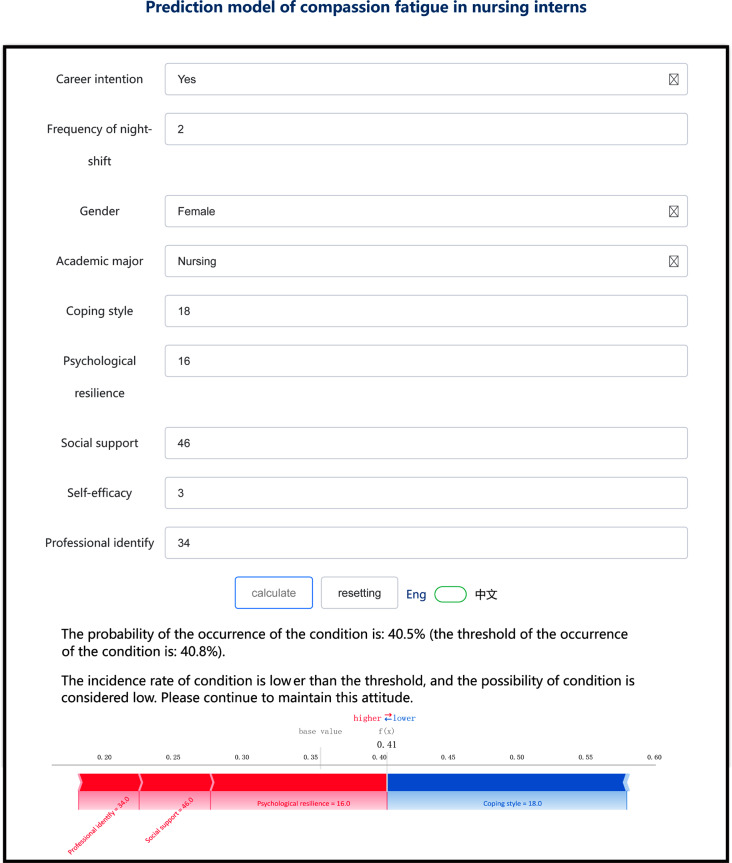
Development of a web-based application for predicting compassion fatigue
We developed a web-based application based on the final model’s predicted risks (available at http://www.xsmartanalysis.com/model/list/predict/model/html?mid= 15239&symbol = 21Dx71Ab62wF580Bl642), providing individualized risk assessments for compassion fatigue among nursing interns (Fig. 7). The application features a user-friendly interface for healthcare professionals. Key steps for developing this application include model integration (XGBoost was embedded to ensure accurate predictions), accuracy verification (outputs were tested using a holdout sample and compared with Python-generated results to verify consistency), and usability testing (nursing educators evaluated the usability of this application). The tool offers a practical method for early detection of compassion fatigue, helping educators and colleges intervene early.
Fig. 7.
The web-based calculator for predicting the risk of compassion fatigue among nursing interns
Discussion
Latent profile analysis of compassion fatigue among nursing students during the internship
This study identified three distinct profiles of compassion fatigue among nursing interns using LPA: low compassion fatigue, moderate compassion fatigue, and severe compassion fatigue. Each profile exhibits unique characteristics and levels of vulnerability, warranting tailored interventions to mitigate compassion fatigue and support emotional resilience during their internships.
The “low compassion fatigue” group, comprising 55.73% of the participants, had average scores of 18.74 for burnout and 10.14 for secondary traumatic stress, with an overall average score of 28.874 on the Compassion Fatigue Short Scale. Although these nursing interns showed low overall compassion fatigue, they scored higher on item 2 (“I feel I have not accomplished much in my life”) and item 7 (“I often feel weak, tired, or exhausted as a caregiver”). These scores reflect their emotional and psychological adaptation to new environments and work challenges, likely due to the high intensity of internship tasks, academic pressure, and the fear of incompetence during the transition to their new roles [68, 69]. Despite the overall low level of compassion fatigue, the higher scores on specific items warrant attention to prevent progression to moderate or severe fatigue levels. Preventive measures are vital for this group to ensure compassion fatigue does not escalate. Self-care workshops focused on stress management, peer support networks, and reflective practice sessions can help reinforce resilience. Early identification of emotional stress signals is crucial to prevent progression into higher fatigue levels.
The “moderate compassion fatigue” group included 32.17% of the participants, with average scores of 37.78 for burnout and 19.14 for secondary traumatic stress, totaling 56.92 on the Compassion Fatigue Short Scale. This group also scored highest on items 2 and 7. Besides, item 9 (“I feel frustrated with my job”) showed the most significant score difference, indicating professional confusion, fatigue, and emotional distress. This may stem from a heightened sensitivity to patient suffering and death, leading to increased burnout and frustration [70]. Additionally, the inability to establish stable relationships with supervisors and staff during a short internship exacerbates their emotional burden [71]. Mindfulness-based interventions, including mindfulness-based stress reduction (MBSR), can greatly enhance emotional regulation and self-awareness. Moreover, developing a structured mentorship program that ensures continuous emotional support from senior staff may help alleviate professional confusion and reduce burnout. This group would also benefit from training in empathy management techniques, enabling them to manage emotional boundaries more effectively when working with patients in distress [72, 73].
The “severe compassion fatigue” group, representing 12.10% of the participants, had average scores of 55.92 for burnout and 32.83 for secondary traumatic stress, with a total score of 88.75. This group scored highest on items 2 and 7. It showed the most significant score differences on item 8 (“I have intrusive thoughts about the traumatic situations I have encountered”) and item 10 (“I relive traumatic experiences when helping those in crisis”), indicating rapidly increasing psychological trauma and distress. These interns lack effective coping strategies and psychological resilience, leading to higher secondary traumatic stress and compassion fatigue [74, 75]. Long-term high-pressure environments and cumulative emotional burdens aggravate these issues [75]. For this group, immediate and intensive interventions are required. Psychological counseling, such as trauma-informed therapy and cognitive-behavioral therapy (CBT), should be provided to address underlying trauma and develop coping strategies. Stress management workshops focusing on crisis intervention and peer support groups can provide emotional outlets and coping mechanisms for dealing with trauma. Given the cumulative emotional burden, implementing resilience training and promoting a supportive workplace culture is essential for helping these interns recover from their experiences and prevent future burnout [76].
Influencing factors of compassion fatigue among nursing students during the internship
Demographic characteristics
Our study identified several demographic factors associated with higher compassion fatigue, including being female, specializing in midwifery, working frequent night shifts, and intending to leave the profession post-graduation. These findings align with earlier research but suggest underlying sociocultural and psychological mechanisms that merit further exploration.
Female students reported higher compassion fatigue than their male counterparts, which is consistent with Sacco et al.’s [77] findings in critical care nurses. This may be attributed to the fact that female students, generally possessing higher emotional intelligence and empathy [78], are more emotionally involved with patients, leading to emotional exhaustion over time [79, 80]. Additionally, cultural norms in China often discourage emotional expression in males, which may reduce their emotional engagement, thus lowering their risk of compassion fatigue [78]. This suggests that gender roles and societal expectations play a significant role in shaping how male and female nursing students experience and express compassion fatigue, enlightening our readers about the broader context of this issue.
Midwifery students reported higher compassion fatigue than general nursing students, echoing findings from obstetric nurses who frequently encounter emotionally intense situations such as complex births and neonatal deaths [81, 82]. The discrepancy between students’ expectations, often formed by a focus on normal physiological births, and the reliability of critical situations may exacerbate emotional strain, increasing their risk of secondary traumatic stress [76, 83]. These findings underscore the importance of targeted educational interventions addressing the emotional challenges of midwifery as necessary step to better prepare students for such experiences, reducing compassion fatigue [84].
Students who worked frequent night shifts reported higher compassion fatigue scores, consistent with findings among hospice nurses [85]. Night shifts not only disrupt students’ sleep patterns and circadian rhythms, but they also increase the likelihood of exposure to emotional exhaustion, exploitation, and workplace bullying. This aligns with research linking shift work to anxiety, depression, and psychological distress [85]. Institutions may need to revise internship structures to limit night shift hours or provide coping strategies for students, thereby mitigating compassion fatigue.
Students intending to leave the profession after graduation reported higher compassion fatigue, reflecting a misalignment between expectations and reality during internships. This lack of intrinsic motivation likely leads to emotional exhaustion and moral distress [86], reinforcing the importance of providing structured support systems for students who express dissatisfaction or uncertainty about their career path [87]. Encouraging reflection on nursing’s role and offering career guidance may help students align their expectations with reality, potentially reducing their compassion fatigue.
Psychological resilience
Our study confirmed that psychological resilience is a protective factor against compassion fatigue, consistent with previous research [15, 88]. Psychological resilience enhances nursing students’ psychosocial functioning and professional performance [88, 89], avoiding emotion-centered coping and building confidence in managing workplace stress. This mitigates compassion fatigue and aids in adapting to clinical environment [90]. These findings suggest that students with higher resilience are better equipped to handle emotional demands, supporting the integration of resilience training into nursing curricula [91]. Enhancing resilience can improve nursing students’ psychological functioning, professional performance, and overall well-being. Future interventions should explore how resilience-building programs can be tailored to individual needs, especially for those entering high-stress specialties.
Professional identity
Our study found a negative correlation between compassion fatigue and professional identity, consistent with findings from similar studies [92]. Professional identity is a psychological resource that helps nursing students maintain a positive attitude during high-pressure internships [93]. This finding suggests that building a strong professional identity can buffer against compassion fatigue by fostering commitment and resilience in challenging tasks. Conversely, students with lower professional identities may experience reduced job satisfaction and enthusiasm, making them more susceptible to compassion fatigue [94, 95]. These findings highlight the importance of strengthening professional identity in nursing education.
Social support
Greater social support was linked to a lower risk of compassion fatigue, a finding consistent with a study involving 307 intern nursing and midwifery students [14]. Social support is an external resource critical for stress management, reducing feelings of loneliness and anxiety [96, 97, 98]. According to the stress coping model, robust social networks enable students to employ positive coping strategies, effectively reducing compassion fatigue [99, 100]. Our findings underscore the importance of encouraging nursing students to cultivate social support systems, whether through peers, mentors, or family, especially during emotionally demanding internships. Nursing programs could benefit from integrating social support strategies, ensuring students are better equipped to handle stressors.
Coping style
Negative coping strategies significantly and positively predict higher compassion fatigue, while positive coping strategies negatively predict lower compassion fatigue. Rui’s study on clinical nurses [101] observed that negative coping strategies were linked to higher compassion fatigue, while positive coping strategies were protective. Nursing students who rely on negative coping mechanisms, such as avoidance, are more susceptible to compassion fatigue because these strategies tend to exacerbate stress and emotional exhaustion [102, 103, 104]. In contrast, students who adopt positive coping strategies can maintain a more constructive attitude toward stressful situations, reducing the impact of compassion fatigue [102, 104]. These findings suggest that teaching adaptive coping mechanisms should be a priority in nursing education to foster resilience and emotional stability.
Self-efficacy
Higher self-efficacy was associated with lower compassion fatigue in our study, consistent with previous studies focusing on nurse populations [105, 106]. Self-efficacy enables nursing students to perceive nursing as a meaningful and manageable profession, fostering a robust professional identity and more excellent career preparation [107, 108], enhancing job satisfaction and reducing burnout [105, 109]. Therefore, nursing educators should guide students in seeking meaningful experiences and learning opportunities to build self-efficacy, improve adaptability, and reduce the incidence of compassion fatigue. Abusubhiah et al. (2023) advocate for using multimodal interventions, including flipped classrooms, simulations, debriefing, and role-playing better to enhance nursing students’ self-efficacy [110]. These strategies should be incorporated into nursing education programs to improve adaptability and reduce the incidence of compassion fatigue.
Development and application of a machine learning-based predictive model for compassion fatigue among nursing students during internships
This study is the first to develop a user-friendly, personalized model to predict compassion fatigue among nursing interns using machine learning techniques. Traditional models, like the one developed for emergency department nurses [111], are often constrained by assumptions of linearity and struggle to account for complex interactions between variables as effectively as machine learning. In contrast, machine learning models such as XGBoost, used in our study, handle non-linear relationships and high-dimensional data more robustly. However, machine learning models carry the risk of overfitting, particularly with small datasets. We mitigated this through hyperparameter tuning and cross-validation, but external validation in other populations is necessary to confirm generalizability.
Our study identified nine significant predictors, such as gender and professional identity. Gender differences, particularly in nursing, align with existing literature, where female nurses often report higher levels of compassion fatigue due to societal expectations and caregiving roles. Professional identity is another crucial factor in how nursing students manage workplace stressors. A recent study across 21 tertiary hospitals in China developed a risk prediction model for compassion fatigue among emergency department nurses using a logistic regression model [111]. This model incorporated only seven factors: job position, job satisfaction, dietary habits, daily sleep duration, occupational stress, physical harassment, and workplace violence levels. By contrast, our model demonstrated higher predictive efficiency, covering a broader range of influencing factors and providing a more comprehensive assessment of the risk of compassion fatigue. However, since our model has not been validated in external populations, its generalizability still requires further investigation.
While the model demonstrated high accuracy, its application in real-world settings must address ethical and cultural considerations. Identifying high-risk students could lead to stigmatization, so strict confidentiality is crucial. Institutions should establish guidelines to protect students’ privacy, ensuring results are shared only with authorized personnel, such as trained student advisors or mental health professionals. Students should also have the option to opt-out of screenings and receive psychological support if identified as high-risk.
Cultural factors, especially in China, where emotional vulnerability is often minimized, may influence the expression and reporting of compassion fatigue. This could affect the accuracy of self-reported data due to social desirability bias. Integrating objective indicators like work hours or job roles can enhance the model’s predictive power beyond self-reported data.
Additionally, Chinese nursing interns face unique stressors such as academic pressure, family obligations, and the hierarchical healthcare structure, which may contribute to compassion fatigue differently compared to Western contexts. Gender roles in China often place extra caregiving expectations on female nurses, potentially amplifying their compassion fatigue risk. Future research should explore how these cultural dynamics influence the model’s performance across different settings.
Our model can identify nursing students at high risk of compassion fatigue before symptoms manifest. The online tool can be integrated into electronic health records or used in educational settings. To streamline routine psychological assessments in clinical environments, the model could be simplified by focusing on objective indicators like job roles or work hours without compromising predictive power. Adapting the model to other cultural or institutional contexts, by including locally relevant stressors like work conditions or healthcare policies, will enhance its applicability.
Strengths and limitation
This study has several strengths, most notably its innovative use of machine learning to predict compassion fatigue, an area where traditional models have shown limitations. Integrating LPA with machine learning allows for identifying risk groups and individualized risk prediction, providing more nuanced insights than conventional methods. Our machine learning algorithms offered enhanced predictive power by accounting for complex, non-linear relationships between variables, which may be overlooked in traditional statistical models. This makes our model a valuable tool for educational and clinical settings, where early identification and intervention are critical.
However, there are limitations to consider in our study. One of the primary challenges is that machine learning models, while powerful, require larger datasets for optimal performance and external validation to ensure generalizability. The reliance on a cross-sectional design limits our ability to infer causality, and future longitudinal studies could provide more robust evidence for the predictors of compassion fatigue. Additionally, the convenience sampling method, coupled with a high proportion of female participants, may introduce selection bias, reducing the model’s applicability to more diverse populations. Future studies should aim for more balanced samples to improve generalizability. Another limitation is the practical application of the model in clinical settings, as collecting psychological parameters in busy environments is challenging and may hinder implementation. Additionally, relying on self-reported data introduces potential biases, such as social desirability or recall bias, which could affect the accuracy of measuring compassion fatigue. Future research could explore using more readily available, objective data to enhance feasibility. Finally, cultural differences should be considered when applying this model internationally. The predictors of compassion fatigue may vary across different healthcare systems, and further validation in diverse settings is necessary to ensure the adaptability of the model.
Conclusion
This study developed a machine learning-based model for predicting compassion fatigue among nursing interns, integrating demographic and work-related characteristics and psychosocial variables. With strong predictive accuracy, the model led to an online tool that helps nursing educators and nursing administrators identify at-risk students early. enabling targeted interventions to improve well-being and learning outcomes. The this model’s adaptability suggests potential scalability for use across other nursing populations and settings, offering a broader approach for managing compassion fatigue in various clinical and educational contexts.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
Thank you to all nursing interns who volunteered to participate in this study and also to the full-time student counselors for their great support in data collection. At the same time, we are grateful for the hard work of the editors and the valuable suggestions of the reviewers.
Abbreviations
- LPA
Latent profile analysis
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology
- TRIPOD
Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis
- LMR
Lo-Mendell-Rubin likelihood ratio test
- BLRT
Bootstrap likelihood ratio test
- AIC
Akaike Information Criterion
- BIC
Bayesian Information Criterion
- aBIC
Adjusted Bayesian Information Criterion
- LASSO
Least Absolute Shrinkage and Selection Operator
- XGBoost
Extreme gradient boosting
- AUC
Area under the receiver
- ROC
Receiver operating characteristic curve
- DCA
Decision curve analysis
- SHAP
Shapley additive explanation
- RMB
Chinse yuan
- MBSR
Mindfulness-based stress reduction
- CBT
Cognitive-behavioral therapy
Author contributions
YLJ and TX conceived and designed the study. YLJ, ST, and TX contributed to the acquisition, analysis, and interpretation of data. YLJ, ZJJ, CL, and MFJH were involved in investigation, methodology, and data curation. YLJ drafted the manuscript. TX revised subsequent drafts. All authors reviewed and approved the final manuscript.
Funding
This work was supported bythe 2022 Institutional Science and Technology Innovation Team Project of Hunan Traditional Chinese Medical College, titled “Integrated Chinese and Western Medicine in Geriatric Nursing”, and the 2024 Hunan Provincial Vocational College Education and Teaching Reform Research Project (Grant Number: ZJGB2024003).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author[LJY] on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cheng J, Cui J, Yu W, Kang H, Tian Y, Jiang X. Factors influencing nurses’ behavioral intention toward caring for COVID-19 patients on mechanical ventilation: A cross-sectional study. PLoS ONE. 2021;16(11):e0259658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lombardo B, Eyre C. Compassion fatigue: a nurse’s primer. Online J Issues Nurs. 2011;16(1):3. [DOI] [PubMed] [Google Scholar]
- 3.Zhang YY, Zhang C, Han XR, Li W, Wang YL. Determinants of compassion satisfaction, compassion fatigue and burn out in nursing: A correlative meta-analysis. Med (Baltim). 2018;97(26):e11086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joinson C. Coping with compassion fatigue. Nursing. 1992;22(4):116. [PubMed] [Google Scholar]
- 5.Figley CR. Compassion Fatigue: Secondary traumatic stress disorders from treating the traumatized. In: New York: Brunner Mazel. vol. 7; 1995.
- 6.Figley CR. Compassion fatigue: psychotherapists’ chronic lack of self care. J Clin Psychol. 2002;58(11):1433–41. [DOI] [PubMed] [Google Scholar]
- 7.Phillips CS, Becker H, Gonzalez E. Psychosocial well-being: An exploratory cross-sectional evaluation of loneliness, anxiety, depression, self-compassion, and professional quality of life in oncology nurses. Clin J Oncol Nurs. 2021;25(5):530–8. [DOI] [PubMed] [Google Scholar]
- 8.Lee LJ, Wehrlen L, Ding Y, Ross A. Professional quality of life, sleep disturbance and health among nurses: A mediation analysis. Nurs Open. 2022;9(6):2771–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y, Peng Q, Dong W, Hou C, Chen C. Professional identity and sense of coherence affect the between compassion fatigue and work engagement among Chinese hospital nurses. BMC Nurs. 2023;22(1):472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tuna R, Eskin Bacaksiz F, Kahraman B. The relationship between musculoskeletal discomfort and professional quality of life among nurses. Pain Manag Nurs. 2022;23(1):62–7. [DOI] [PubMed] [Google Scholar]
- 11.Xie W, Chen L, Feng F, Okoli CTC, Tang P, Zeng L, Jin M, Zhang Y, Wang J. The prevalence of compassion satisfaction and compassion fatigue among nurses: A systematic review and meta-analysis. Int J Nurs Stud. 2021;120:103973. [DOI] [PubMed] [Google Scholar]
- 12.Garnett A, Hui L, Oleynikov C, Boamah S. Compassion fatigue in healthcare providers: a scoping review. BMC Health Serv Res. 2023;23(1):1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han B, R,;, Chen H, Xie J. Current status of compassion fatigue level among nursing students at the late stage of internship and its influencing factors. Chin J Mod Nurs. 2017;23(21):5. [Google Scholar]
- 14.Li JN, Jiang XM, Zheng QX, Lin F, Chen XQ, Pan YQ, Zhu Y, Liu RL, Huang L. Mediating effect of resilience between social support and compassion fatigue among intern nursing and midwifery students during COVID-19: A cross-sectional study. BMC Nurs. 2023;22(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao XY, Wang L, Wei SY, Li J, Gong S. Prevalence and predictors for compassion fatigue and compassion satisfaction in nursing students during clinical placement. Nurse Educ Pract. 2021;51:102999. [DOI] [PubMed] [Google Scholar]
- 16.Chachula KM. Professional quality of life factors and relationships in nursing and psychiatric nursing students: An exploratory study. SAGE open Nurs. 2021;7:2377960821994394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chi DL, Randall CL, Hill CM. Dental trainees’ mental health and intention to leave their programs during the COVID-19 pandemic. Journal of the American Dental Association (1939). 2021;152(7):526–534. [DOI] [PMC free article] [PubMed]
- 18.Drummond JR, Duguid R. Student drop-out from UK dental schools. Br Dent J. 1997;182(9):347–9. [DOI] [PubMed] [Google Scholar]
- 19.Marôco J, Assunção H, Harju-Luukkainen H, Lin SW, Sit PS, Cheung KC, Maloa B, Ilic IS, Smith TJ, Campos J. Predictors of academic efficacy and dropout intention in university students: Can engagement suppress burnout? PLoS ONE. 2020;15(10):e0239816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rudman A, Gustavsson P, Hultell D. A prospective study of nurses’ intentions to leave the profession during their first five years of practice in Sweden. Int J Nurs Stud. 2014;51(4):612–24. [DOI] [PubMed] [Google Scholar]
- 21.Rudman A, Gustavsson JP. Burnout during nursing education predicts lower occupational preparedness and future clinical performance: A longitudinal study. Int J Nurs Stud. 2012;49(8):988–1001. [DOI] [PubMed] [Google Scholar]
- 22.Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. Int J Nurs Stud. 2017;69:9–24. [DOI] [PubMed] [Google Scholar]
- 23.Bride B, Radey M, Figley C. Measuring compassion fatigue. Clin Soc Work J. 2007;35:155–63. [Google Scholar]
- 24.Figley CR. Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. Philadelphia, PA,USA: Brunner/Mazel; 1995. [Google Scholar]
- 25.Gentry JE, Baranowsky AB, Dunning K. The accelerated recovery program (ARP) for compassion fatigue. In: Figley CR (Ed.), Treating compassion fatigue. New York, US: Brunner-Routledge; 2002;123–38. [Google Scholar]
- 26.Adams RE, Boscarino JA, Figley CR. Compassion fatigue and psychological distress among social workers: a validation study. Am J Orthopsychiatry. 2006;76(1):103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stamm BH. The concise ProQOL manual: The concise manual for the Professional Quality of Life Scale, 2 nd Edition. In.; 2010.
- 28.Sun B, Hu M, Yu S, Jiang Y, Lou B. Validation of the Compassion Fatigue Short Scale among Chinese medical workers and firefighters: a cross-sectional study. BMJ Open. 2016;6(6):e011279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bouchard L, Rainbow J. Compassion fatigue, presenteeism, Adverse Childhood Experiences (ACES), and resiliency levels of Doctor of Nursing Practice (DNP) students. Nurse Educ Today. 2021;100:104852. [DOI] [PubMed] [Google Scholar]
- 30.Liu H, Zhang Z, Chi C, Tao X, Zhang M. Exploring the Impact of the COVID-19 Pandemic on Academic Burnout Among Nursing College Students in China: A Web-Based Survey. Med Sci Monit Basic Res. 2023;29:e940997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jing T, Peng Y, Wu S. Study on the status and influencing factors of empathy fatigue among nursing interns under the background of public health emergencies. Health Vocat Educ. 2024;42(4):131–5. [Google Scholar]
- 32.Chen C, Li Y, Huang D, Liu X, Xu Z, Li J. Trends and influencing factors of empathy fatigue in nursing interns: A longitudinal study. J Adv Nurs. 2023.
- 33.Wang M, Guan H, Li Y, Xing C, Rui B. Academic burnout and professional self-concept of nursing students: A cross-sectional study. Nurse Educ Today. 2019;77:27–31. [DOI] [PubMed] [Google Scholar]
- 34.Yang H-J. Factors affecting student burnout and academic achievement in multiple enrollment programs in Taiwan’s technical–vocational colleges. Int J Educ Dev. 2004;24(3):283–301. [Google Scholar]
- 35.Ye L. Analysis of the current status and influencing factors of empathy fatigue among nursing interns. In: In Proceedings of the 2022 Shanghai International Nursing Conference. Shanghai; 2022: 35–36.
- 36.Liu Z, Xie Y, Sun Z, Liu D, Yin H, Shi L. Factors associated with academic burnout and its prevalence among university students: a cross-sectional study. BMC Med Educ. 2023;23(1):317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miranda-Ackerman RC, Barbosa-Camacho FJ, Sander-Möller MJ, Buenrostro-Jiménez AD, Mares-País R, Cortes-Flores AO, Morgan-Villela G, Zuloaga-Fernández del Valle CJ, Solano-Genesta M, Fuentes-Orozco C. Burnout syndrome prevalence during internship in public and private hospitals: a survey study in Mexico. Med Educ Online. 2019;24(1):1593785. [DOI] [PMC free article] [PubMed]
- 38.Wang X, Cai HJ, Ye HF, Wang Y, Li QQ. Analysis of the current situation and related factors of empathy fatigue in undergraduate nursing interns. Chin High Med Educ. 2023;3:19–21. [Google Scholar]
- 39.Williams GA, Kibowski F. Latent class analysis and latent profile analysis. Handbook of methodological approaches to community-based research: Qualitative, quantitative, and mixed methods. 2016;15:143–51.
- 40.Roeser RW, Eccles JS, Sameroff AJ. Academic and emotional functioning in early adolescence: Longitudinal relations, patterns, and prediction by experience in middle school. Dev Psychopathol. 1998;10(2):321–52. [DOI] [PubMed] [Google Scholar]
- 41.Mathew A, Doorenbos AZ. Latent profile analysis–an emerging advanced statistical approach to subgroup identification. Indian J Contin Nurs Educ. 2022;23(2):127–33. [Google Scholar]
- 42.Ferguson SL, Moore G, Hull EW. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int J Behav Dev. 2019;44(5):458–68. [Google Scholar]
- 43.Huettmann F, Craig EH, Herrick KA, Baltensperger AP, Humphries GRW, Lieske DJ, Miller K, Mullet TC, Oppel S, Resendiz C et al. Use of machine learning (ML) for predicting and analyzing ecological and ‘presence only’ data: An overview of applications and a good outlook. In: Machine Learning for Ecology and Sustainable Natural Resource Management. edn. Edited by Humphries G, Magness DR, Huettmann F. Cham: Springer International Publishing; 2018: 27–61.
- 44.Riley RD, Ensor J, Snell KIE, Harrell FE, Martin GP, Reitsma JB, Moons KGM, Collins G, van Smeden M. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;368:m441. [DOI] [PubMed] [Google Scholar]
- 45.Nylund-Gibson K, Garber AC, Carter DB, Chan M, Arch DAN, Simon O, Whaling K, Tartt E, Lawrie SI. Ten frequently asked questions about latent transition analysis. Psychol Methods. 2023;28(2):284–300. [DOI] [PubMed] [Google Scholar]
- 46.Spurk D, Hirschi A, Wang M, Valero D, Kauffeld S. Latent profile analysis: A review and how to guide of its application within vocational behavior research. J Vocat Behav. 2020;120:103445. [Google Scholar]
- 47.Brown J, Suls J. Psychological perspectives on the self. In.: Lawrence Erlbaum Associates Hillsdale, NJ; 1993.
- 48.Lu H, While AE, Barriball KL. Job satisfaction and its related factors: a questionnaire survey of hospital nurses in Mainland China. Int J Nurs Stud. 2007;44(4):574–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in health psychology: A user’s portfolio. Causal and control beliefs. Causal Control Beliefs. 1995;1(011):35–7. [Google Scholar]
- 50.Zeng G, Fung S-f, Li J, Hussain N, Yu P. Evaluating the psychometric properties and factor structure of the general self-efficacy scale in China. Curr Psychol. 2020; 40:3970–3980.
- 51.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55(3–4):610–7. [DOI] [PubMed] [Google Scholar]
- 52.Jiang Q. Perceived social support scale. Chin J Behav Med Sci. 2001;10(10):41–3. [Google Scholar]
- 53.Yan B, Zheng X, Zhang X. The influence mechanism of social support on subjective well-being of college students: the mediating role of self-control and depression. Psychol Sci. 2011;34(02):471–5. [Google Scholar]
- 54.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 55.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–28. [DOI] [PubMed] [Google Scholar]
- 56.Ye Z, Ruan X, Zeng Z, Xie Q, Cheng M, Peng C, Qiu H. Psychometric properties of 10-item Connor-Davidson resilience scale among nursing students. J Nurs. 2016;23:9–13. [Google Scholar]
- 57.Xie Y-N. A preliminary study on the reliability and validity of the simple coping style scale. Chin J Clin Psychol. 1998;6(2):114–5. [Google Scholar]
- 59.Folkman S, Lazarus RS. Ways of coping questionnaire. 1988.
- 59.Tein JY, Coxe S, Cham H. Statistical power to detect the correct number of classes in latent profile analysis. Struct Equ Model. 2013;20(4):640–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fonseca-Pedrero E, Ortuño-Sierra J, de Álbeniz AP, Muñiz J, Cohen AS. A latent profile analysis of schizotypal dimensions: Associations with psychopathology and personality. Psychiatry Res. 2017;253:110–5. [DOI] [PubMed] [Google Scholar]
- 61.Marsh HW, Hau K-T, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct Equ Model. 2004;11(3):320–41. [Google Scholar]
- 62.Li JB, Wu AMS, Feng LF, Deng Y, Li JH, Chen YX, Mai JC, Mo PKH, Lau JTF. Classification of probable online social networking addiction: A latent profile analysis from a large-scale survey among Chinese adolescents. J Behav Addict. 2020;9(3):698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fu H, Si L, Guo R. What Is the optimal cut-off point of the 10-item Center for Epidemiologic Studies Depression Scale for Screening Depression among Chinese individuals aged 45 and over? An exploration using latent profile analysis. Front Psychiatry. 2022;13. [DOI] [PMC free article] [PubMed]
- 64.Wu Y, Dai Z, Xiao W, Wang H, Huang Y, Si M, Fu J, Chen X, Jia M, Leng Z et al. Perceived stigma among discharged patients of COVID-19 in Wuhan, China: A latent profile analysis. Front Public Health. 2023;11. [DOI] [PMC free article] [PubMed]
- 65.Vasquez MM, Hu C, Roe DJ, Chen Z, Halonen M, Guerra S. Least absolute shrinkage and selection operator type methods for the identification of serum biomarkers of overweight and obesity: simulation and application. BMC Med Res Methodol. 2016;16(1):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Covert I, Lundberg SM, Lee S-I. Understanding global feature contributions with additive importance measures. In: Proceedings of the 34th International Conference on Neural Information Processing Systems. Vancouver, BC, Canada: Curran Associates Inc.; 2020: Article 1444.
- 67.Covert I, Lundberg SM, Lee S-I. Understanding global feature contributions with additive importance measures. Adv Neural Inf Process Syst. 2020;33:17212–23. [Google Scholar]
- 68.Lopes AR, Nihei OK. Burnout among nursing students: predictors and association with empathy and self-efficacy. Rev Bras Enferm. 2020;73(1):e20180280. [DOI] [PubMed] [Google Scholar]
- 69.Valero-Chillerón MJ, González-Chordá VM, López-Peña N, Cervera-Gasch Á, Suárez-Alcázar MP, Mena-Tudela D. Burnout syndrome in nursing students: An observational study. Nurse Educ Today. 2019;76:38–43. [DOI] [PubMed] [Google Scholar]
- 70.Zheng R, Guo Q, Dong F, Gao L. Death self-efficacy, attitudes toward death and burnout among oncology nurses: A multicenter cross-sectional study. Cancer Nurs. 2022;45(2):E388–96. [DOI] [PubMed] [Google Scholar]
- 71.Velando-Soriano A, Suleiman-Martos N, Pradas-Hernández L, Membrive-Jiménez MJ, Ramírez-Baena L, Gómez-Urquiza JL. Cañadas-De La Fuente GA. Factors related to the appearance and development of burnout in nursing students: a systematic review and meta-analysis. Front Public Health. 2023;11:1142576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Srour RA, Keyes D. Lifestyle Mindfulness In Clinical Practice. In: StatPearls. edn. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed]
- 73.Melissant HC, Hendriks RRA, Bakker EJM, Kox JHAM, Rietveld N, Miedema HS, Roelofs PDDM, Verhaegh KJ. Interventions that support novice nurses’ transition into practice: A realist review. Int J Nurs Stud. 2024;157:104785. [DOI] [PubMed] [Google Scholar]
- 74.Hegney DG, Rees CS, Eley R, Osseiran-Moisson R, Francis K. The contribution of individual psychological resilience in determining the professional quality of life of Australian nurses. Front Psychol. 2015;6:1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Barleycorn D. Awareness of secondary traumatic stress in emergency nursing. Emerg Nurse. 2019;27(5):19–22. [DOI] [PubMed] [Google Scholar]
- 76.Davies S, Coldridge L. No Man׳s Land’: An exploration of the traumatic experiences of student midwives in practice. Midwifery. 2015;31(9):858–64. [DOI] [PubMed] [Google Scholar]
- 77.Sacco TL, Ciurzynski SM, Harvey ME, Ingersoll GL. Compassion satisfaction and compassion fatigue among critical care nurses. Crit Care Nurse. 2015;35(4):32–43. quiz 31p following 43. [DOI] [PubMed] [Google Scholar]
- 78.Deng X, Chen S, Li X, Tan C, Li W, Zhong C, Mei R, Ye M. Gender differences in empathy, emotional intelligence and problem-solving ability among nursing students: A cross-sectional study. Nurse Educ Today. 2023;120:105649. [DOI] [PubMed] [Google Scholar]
- 79.Yu H, Qiao A, Gui L. Predictors of compassion fatigue, burnout, and compassion satisfaction among emergency nurses: A cross-sectional survey. Int Emerg Nurs. 2021;55:100961. [DOI] [PubMed] [Google Scholar]
- 80.Borges EMN, Fonseca CINS, Baptista PCP, Queirós CML, Baldonedo-Mosteiro M, Mosteiro-Diaz MP. Fadiga por compaixão em enfermeiros de urgência e emergência hospitalar de adultos. Rev Latinoam Enferm. 2019;27:e3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Weeks F, Pantoja L, Ortiz J, Foster J, Cavada G, Binfa L. Labor and birth care satisfaction associated with medical interventions and accompaniment during labor among Chilean women. J Midwifery Womens Health. 2017;62(2):196–203. [DOI] [PubMed] [Google Scholar]
- 82.Saxbe D, Horton KT, Tsai AB. The Birth Experiences Questionnaire: A brief measure assessing psychosocial dimensions of childbirth. J Fam Psychol. 2018;32(2):262–8. [DOI] [PubMed] [Google Scholar]
- 83.Curtis P, Ball L, Kirkham M. Why do midwives leave? (Not) being the kind of midwife you want to be. Br J Midwifery. 2006;14(1):27–31. [Google Scholar]
- 84.McKenna L, Rolls C. Undergraduate midwifery students’ first experiences with stillbirth and neonatal death. Contemp Nurse. 2011;38(1–2):76–83. [DOI] [PubMed] [Google Scholar]
- 85.Shi H, Shan B, Chen Q, Guo F, Zhou X, Shi M, Liu Y. Prevalence and predictors of compassion satisfaction, secondary traumatic stress, and burnout among Chinese hospice nurses: A cross-sectional study. Appl Nurs Res. 2023;69:151648. [DOI] [PubMed] [Google Scholar]
- 86.Kandil F, El Seesy N, Banakhar M. Factors affecting students’ preference for nursing education and their intent to leave: A cross-sectional study. Open Nurs J. 2021;15(1).
- 87.Kotera Y, Cockerill V, Chircop J, Kaluzeviciute G, Dyson S. Predicting self-compassion in UK nursing students: Relationships with resilience, engagement, motivation, and mental wellbeing. Nurse Educ Pract. 2021;51:102989. [DOI] [PubMed] [Google Scholar]
- 88.Karabey T. Compassion fatigue and psychological resilience levels of nursing final students: A descriptive, cross-sectional, and relational study. Palliat Support Care. 2023;13:1–7. [DOI] [PubMed]
- 89.Garcia-Dia MJ, DiNapoli JM, Garcia-Ona L, Jakubowski R, O’Flaherty D. Concept analysis: resilience. Arch Psychiatr Nurs. 2013;27(6):264–70. [DOI] [PubMed] [Google Scholar]
- 90.Yu F, Raphael D, Mackay L, Smith M, King A. Personal and work-related factors associated with nurse resilience: A systematic review. Int J Nurs Stud. 2019;93:129–40. [DOI] [PubMed] [Google Scholar]
- 93.well-being. and resilience [https://www.aacnnursing.org/our-initiatives/well-being-resilience]
- 92.Ruan TT. Analysis of nursing students’ professional identity and influencing factors under the epidemic of public health emergencies. Contemp Nurse. 2021;28(12):4. [Google Scholar]
- 93.Geoffrion S, Morselli C, Guay S. Rethinking compassion fatigue through the lens of professional identity: The case of child-protection workers. Trauma Violence Abuse. 2016;17(3):270–83. [DOI] [PubMed] [Google Scholar]
- 94.Zhou X, Yang H, Yang Y, Zhang Y, Yang H. Mediating effect of professional identity on professional benefit and work engagement among nurses. J Nurs Sci. 2019;34:51–4. [Google Scholar]
- 95.Xie Y, Zhao H, Huang Y, Liu C. The correlation between empathy fatigue and the sense of professional benefits in intern nurses. Contemp Nurse. 2020;27(10):153–6. [Google Scholar]
- 96.Jeong YJ, Koh CK. Female nursing graduate students’ stress and health: the mediating effects of sense of coherence and social support. BMC Nurs. 2021;20(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Labrague LJ. COVID-19 phobia, loneliness, and dropout intention among nursing students: the mediating role of social support and coping. Curr Psychol. 2023;13:1–9. [DOI] [PMC free article] [PubMed]
- 98.Onieva-Zafra MD, Fernández-Muñoz JJ, Fernández-Martínez E, García-Sánchez FJ, Abreu-Sánchez A, Parra-Fernández ML. Anxiety, perceived stress and coping strategies in nursing students: a cross-sectional, correlational, descriptive study. BMC Med Educ. 2020;20(1):370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer publishing company; 1984.
- 100.Zhang J, Wang X, Chen O, Li J, Li Y, Chen Y, Luo Y, Zhang J. Social support, empathy and compassion fatigue among clinical nurses: structural equation modeling. BMC Nurs. 2023;22(1):425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jiao R, Li J, Cheng N, Liu X, Tan Y. The mediating role of coping styles between nurses’ workplace bullying and professional quality of life. BMC Nurs. 2023;22(1):459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhou Y, Guo X, Yin H. A structural equation model of the relationship among occupational stress, coping styles, and mental health of pediatric nurses in China: a cross-sectional study. BMC Psychiatry. 2022;22(1):416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Visier-Alfonso ME, Sarabia-Cobo C, Cobo-Cuenca AI, Nieto-López M, López-Honrubia R, Bartolomé-Gutiérrez R, Alconero-Camarero AR, González-López JR. Stress, mental health, and protective factors in nursing students: An observational study. Nurse Educ Today. 2024;139:106258. [DOI] [PubMed] [Google Scholar]
- 104.Ding Y, Yang Y, Yang X, Zhang T, Qiu X, He X, Wang W, Wang L, Sui H. The mediating role of coping style in the relationship between psychological capital and burnout among Chinese nurses. PLoS ONE. 2015;10(4):e0122128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang J, Wang X, Xu T, Li J, Li H, Wu Y, Li Y, Chen Y, Zhang JP. The effect of resilience and self-efficacy on nurses’ compassion fatigue: A cross-sectional study. J Adv Nurs. 2022;78(7):2030–41. [DOI] [PubMed] [Google Scholar]
- 106.Hao X, Chen X, Sun C, Zhu Z, Qiao C, Ji M. The mediating effect of general self-efficacy of outpatient nurses on the relationship between perception of work environment and compassion fatigue. Chin Nurs Manag. 2023;23(3):461–6. [Google Scholar]
- 107.Fangonil-Gagalang E. Association of self-efficacy and faculty support on students’ readiness for practice. J Prof Nurs. 2024;52:30–9. [DOI] [PubMed] [Google Scholar]
- 108.Liu Y, Chong MC, Han Y, Wang H, Xiong L. The mediating effects of self-efficacy and study engagement on the relationship between specialty identity and career maturity of Chinese nursing students: a cross-sectional study. BMC Nurs. 2024;23(1):339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu R, Du W, Liu Z. Correlation analysis of general self-efficacy and nursing quality among neurology nurses in Lanzhou. Chin J Pract Nurs. 2016;32(19):1445–50. [Google Scholar]
- 110.Abusubhiah M, Walshe N, Creedon R, Noonan B, Hegarty J. Self-efficacy in the context of nursing education and transition to practice as a registered practitioner: A systematic review. Nurs Open. 2023;10(10):6650–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xie W, Liu M, Okoli CTC, Zeng L, Huang S, Ye X, Liu F, Wang J. Construction and evaluation of a predictive model for compassion fatigue among emergency department nurses: A cross-sectional study. Int J Nurs Stud. 2023;148:104613. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author[LJY] on reasonable request.