Abstract
Background
informal caregivers of people with dementia are at greater risk of developing physical and mental health problems when compared to the general population: they often experience high levels of stress which can lead to a lowered sense of well-being, feelings of being burdened, depression and compromised physical health. The significant beneficial effects of Psychoeducational Interventions on the critical outcomes of caregiver burden and strain were considered sufficient to warrant a recommendation in favour of the intervention. The emergence of the COVID-19 pandemic has significantly increased the use internet-based interventions: this study describes the effectiveness of support program for informal caregivers of people with dementia internet-based and on-site conditions.
Methods
A Psychoeducational Interventions program, consisting of 5 meetings every 2 weeks, has been structured. It aims to provide information and strategies for managing cognitive and psycho-behavioral symptoms in neurodegenerative diseases, as well as to develop effective communication skills and understanding of the caregiver's experience. Intervention formats include slides, video, group discussions and are always led by a psychologist. We assessed in 73 caregivers (33 internet-based and 40 on-site conditions) level of Behavioural and Psychological Symptoms of Dementia management, dementia awareness, social support, find leisure time, harmony with relative, stress, with Visual-Analogue Scale at the beginning of PI and at the end. During the pandemic period the protocol was adapted to be available online and subsequently proposed to caregivers belonging to the Cognitive Disorders and Dementia Centre.
Results
in both modalities, internet-based and on-site condition, a statistically significant improvement was highlighted in all aspects (p < 0.05, for all p-value). Questionnaire on basic dementia knowledge was successfully completed at 100%. Also, participants reported a medium to high level of satisfaction with very limited dropouts (< 3%).
Conclusions
The evidence from this pilot study indicated that caregiver support interventions in both conditions significantly improved several and important outcomes: they showed a significant effect in reducing caregiver strain and improving ability and knowledge. Indeed, Psychoeducational Interventions contribute to effective coping strategies to mitigate caregiver burden so they can continue to provide care for loved ones.
Keywords: Psychoeducational Interventions, Telemedicine, Caregiver
Background
Currently, more than 55 million people worldwide are affected by dementia, with nearly 10 million new cases reported each year. It is projected that this number will rise to 131 million by 2050 [1]. Dementia, impacting memory, cognition, behavior, and daily functioning, stands as a leading cause of dependency among elderly adults [2].
The impact of dementia is significantly burdensome not only for individuals living with dementia but also for those who care for them, affecting society and countries both financially and in human terms [3]. Those affected often require constant care, usually provided by family members or informal caregivers [4]. Informal caregivers of individuals with dementia are those who provide unpaid care, often family members, to those diagnosed with dementia. The assistance provided, for which individuals are often not formally trained, varies from emotional support to supervision, assistance in daily activities, and management of healthcare needs.
Caregiving is a complex role that encompasses both rewarding experiences and significant challenges. The caregiving experience can be influenced by individual, social, and contextual factors, such as gender, living conditions, or the presence of Behavioral and Psychological Symptoms of Dementia (BPSD), which may lead to differential outcomes [5, 6]. Research indicates that caregivers report both positive emotions, such as fulfillment and strengthened relationships, as well as negative experiences, including stress and burnout [7].
The burden of caregiving is a well-documented aspect, recognized both socially and scientifically. Specifically, caregivers of individuals with dementia are at greater risk of experiencing mental and physical health effects compared to caregivers of individuals with other chronic conditions [8, 9]. They may suffer from symptoms of depression and anxiety, social isolation, reduced quality of life, and financial strain [10–14]. Anxiety and depression persist throughout the caregiving journey, and it is well established that the caregiver burden is greater and heavier for women than for men [15].
To ensure good mental and physical health for caregivers and the best care they can provide, training and support actions are crucial. These aim to alleviate the stress arising from insufficient knowledge in handling the daily challenges of the condition [16].
Psychoeducational Interventions (PI) offer an effective tool to support caregivers in maintaining their mental health and well-being. There are many interventions designed to improve the psychological health of caregivers. Specifically, combined interventions (educational, support, psychotherapy, and relief) have been shown to be the most effective approach in the short term to improve caregiver burden, depression, subjective well-being, skills, and knowledge compared to single approaches of psychotherapy, support, or training [17].
The global action plan on dementia, endorsed in 2017 by the 194 Member States of the WHO, has highlighted the need to use technologies like the Internet to increase education and social support [18].
Considering the various types of support available, healthcare specialists should choose the most appropriate mode based on the needs and resources available to the patient [19]. For example, face-to-face interventions that offer information, training, and support can improve the quality of care and reduce psychological distress among caregivers [20]. However, these interventions often require substantial resources or may be inaccessible due to transportation limitations, long distances from care centers, or the inability to leave the person with dementia unattended [21]. To expand caregiver training and support programs, the use of Internet-based interventions seems to have significant potential [22].
There are numerous reviews highlighting the plausibility of online training and support programs for family caregivers of people with dementia to alleviate psychological distress, improve mental health, and offer cost-effectiveness [23, 24]. However, global dissemination has remained elusive due to variability in protocols, assessment, and follow-up, requiring a solid evidence base before a recommendation can be made. The emergence of the COVID-19 pandemic has significantly increased the use of Internet-based interventions, initiating specific studies on how to best provide these interventions, such as determining optimal content, underlying theoretical models, and course intensity.
In Italy, the emergence of the COVID-19 pandemic has led to the need for new approaches and tools for caregiving. The Italian National Institute of Health in Report ISS COVID-19 n. 61/2020 has drafted "Interim indications for appropriate support for people with dementia in the current scenario of the COVID-19 pandemic," providing useful practical guidance for appropriate support for people with dementia, suggesting the use of remote interventions by Centers for Cognitive Disorders and Dementias (CDCD) to ensure continuity of care and address the main care needs of users.
A recent exploratory review extensively describes the effectiveness of peer support interventions for informal caregivers of individuals with dementia through both modes [25]. It has been highlighted that caregivers have positive opinions regarding receiving online support to cope with the challenges they face while caring for someone with dementia [26]. Online accessible programs could represent a convenient and efficient support tool and educational resource, potentially reducing negative outcomes associated with caregiving, especially for those who lack access to face-to-face support groups.
Unfortunately, establishing a definitive best practice model has been challenging due to the variability in protocols, populations, and outcome measurements [25].
The Global Action Plan on the Public Health Response to Dementia 2017–2025, as part of the overall goal of achieving physical, mental, and social well-being for people with dementia, their caregivers, and families, has developed iSupport, an online training and support program for caregivers of people with dementia [27]. The psychoeducational program to ensure effectiveness consists of training on patient management techniques, disease knowledge, caregiving, and caregiver burden. Information and support for patients and caregivers represent a central component of high-quality dementia care [27].
iSupport has been adapted and implemented successfully in various countries worldwide [28–31]. The first extensive randomized controlled trial using iSupport was conducted in Australia, involving 185 family caregivers, to evaluate its effectiveness, cost–benefit ratio, and the caregivers' experience with this innovative program [32].
In general, recent findings concur in affirming that the online intervention mode is acceptable, feasible, and promotes health and well-being benefits for caregivers, especially in self-efficacy, anxiety, and depression measures [33, 34]. They also highlight heterogeneity in experimental designs, populations, and outcome measurement, making it challenging to identify parameters that guarantee the effectiveness of such interventions [35, 36].
However, evidence that interventions can be successfully offered both online and face-to-face presents a unique opportunity to develop and provide personalized peer support interventions for informal caregivers of people with dementia to meet their specific needs [25].
The aim of our protocol is to provide effective emotional and social support, along with accessible evidence-based information tailored to the caregivers' needs, to enhance their knowledge and caregiving skills while emphasizing the importance of self-care.
The current pilot project, developed through the Ministerial Fund for Alzheimer's and Dementia 2021–2023, stems from the necessity to create a remote support protocol via video conferencing for caregivers of individuals with dementia, who by preference or due specific needs such as health emergencies, reduced mobility, long distances, or family arrangements, wish to participate in the psychoeducational sessions, already available in person at the CDCD.
Methods
Study design
PI involve a structured program of 5 meetings, each lasting an average of 1 h and a half, every 2 weeks, in line with the literature [27, 37] and in accordance with the healthcare service provided by the clinic. PI geared toward providing information about cognitive disorders in neurodegenerative diseases, BPSD management (e.g. depression, apathy), daily home activities to train cognitive functions (e.g. memory, attention), effective communication (e.g. improving communication, involving others), caregiving experience (e.g. how to manage stress and emotion to reduce daily stress, thinking differently) (Table 1).
Table 1.
Themes and the related topics covered 5 sessions of Psychoeducational Interventions every 2 weeks
| Meeting | Topic |
|---|---|
| 1 |
Overview of dementia and cognitive disorders ● What is dementia and how does it affect someone ● Memory and attention loss, changes in judgement, repetitive questions and behaviors, language changes, visuo-spatial difficult ● Strategies to cope with cognitive difficulties |
| 2 |
Overview of Behavioural and Psychological Symptoms of Dementia (BPSD) and management ● Aggression, depression, anxiety, apathy, difficulty sleeping, wondering, delusions and hallucinations ● Reasons for behaviour: developing an understanding of the purpose and cause of behaviours and the trigger-behaviour reaction chain ● Understanding the origins of behaviors and the trigger-response pattern through the Antecedent-Behavior-Consequence (ABC) behavior model ● Formulating behavioral approaches based on recognized triggers and the family member's influence on altering behaviors |
| 3 |
Daily home activities ● Training cognitive functions (e.g. memory, attention, language) ● Planning a daily routine ● Finding new activities and tailoring them to the person's residual abilities ● The importance of the environment in reducing symptoms of the condition |
| 4 |
Effectivecommunication ● Improving communication with a person living with dementia ● Supported decision-making ● Establishing a new family balance post-diagnosis and adjusting to new roles ● Involvingothers |
| 5 |
Caring for yourself ● Focus on the caregiver's emotional experience ● Reducing stress in everyday life ● Developing new strategies to thinking differently ● Identifying and understanding helpful and unhelpful thoughts ● Making time for pleasant activities ● Overview of care and support options to plan well for the future |
The study includes an evaluation at the beginning (T0) and at the end (T1) of the program of the crucial facets of the caregiver experience related to the pathology, and at the program's conclusion, a verification of the acquired information and an assessment of satisfaction with the program. The present observational study falls within the current care procedures and clinical practice of the CDCD. The data has been collected and examined in an anonymous form without any experimental procedure. The study adhered to the ethical guidelines of the 1975 Declaration of Helsinki.
Participants
Carers were recruited from Neurology Unit, CDCD, Pisa University Hospital. To participate in the psychoeducational program, caregivers needed to be at least 18 years old, providing care for a person with dementia according to National Institute on Aging- Alzheimer’s Association criteria [2] with Clinical Dementia Rating Scale’ score 1 or 2 [38] at their own residence for a minimum of 6 months, and not using residential care services, such as day care centers or nursing homes. The Psychoeducational Interventions are aimed at caregivers who have not previously participated in support or training programs organized by the clinic, in order to ensure a similar level of basic knowledge; a variety of personal skills remains unchangeable and acceptable. Participants may include spouses, adult children, more distant relatives, or friends who care for the person with dementia. For those engaging in the videoconferencing mode, participants were required to have a desktop computer, a tablet, or a smartphone and be capable of conducting a video call using the selected platform for the sessions.
The groups are formed as homogeneously as possible based on the needs and challenges faced at the start of the program: this allows for a deeper exploration of specific issues, such as managing difficult behaviors or supporting daily activities.
In this study, participants with an attendance rate exceeding 80% were included. It is worth noting that only two individuals, one from the Internet-based condition and one from the On-site condition, had a lower attendance rate and were considered dropouts.
Procedure
The contents of the Psychoeducational Interventions were drafted taking into account the WHO guidelines [27] and the requests of the caregivers attending the clinic. Specifically, the themes that frequently emerged were identified during preliminary interviews with the caregivers and defined through thematic content analysis (Table 2). The expectations observed regarding the meetings are broad and range from information to dementia management, from supporting the caregiver's well-being. The entire program transversely focuses on accepting the condition beyond understanding it and learning strategies that aid in coexistence. Some of the key concepts conveyed include: "It's the illness talking!"; "Who knows how hard it is to live with this disease.
Table 2.
Topics and related examples frequently recurring among caregivers
| Topics and related examples frequently recurring among caregivers |
|---|
|
● Help in caregiving (what to do in specific situations, strategies and advice) “I am doing enough?” “What changes will I have to face?” “Can I still go out and travel with my loved one who has the condition?” “Sometimes it feels like they don't understand me… how can I communicate?" |
|
● Feeling supported and sharing (talking to someone) “I need moments to vent out.” “I often feel guilty, but no one understands me.” “I spend my days with a stranger now." |
|
● Finding new family adaptation and balance “I don't have time for myself.” “Everyone distanced themselves after the diagnosis.” “I don't know how to act with our children; they have their own lives.” |
|
● Information about the condition and treatments “Can we hope for a cure in the coming years?” “How can I help my loved one remember?” “Is the condition hereditary?” “How will the illness progress in the coming years?” |
The "Internet-based" sessions utilized the televisita.sanita.toscana.it, a platform provided by the national healthcare system, while the "On-site condition" meetings were held at the Neurology Unit, Cognitive Disorders and Dementia Centre, Pisa University Hospital. All participants attended at least one introductory meeting; for those engaging in videoconference sessions, an additional "computer literacy" meeting was conducted, either in person or via telephone, to ensure proper use of the online platform.
The sessions are synchronous and not recorded. If a participant misses a meeting, the information covered is sent via email and summarized at the beginning of the next session. During the meetings, in both modalities, professionals and participants interact through direct questions and participate in group discussions in an interactive manner, making important contributions with reflections and personal experiences. The topics addressed (Table 1) also reflect the most frequently asked questions recurring among caregivers (Table 2). While maintaining rigor in conducting the protocol and addressing the topics, professionals encourage personal questions that require further exploration, in order to provide a personalized and more fulfilling experience for participants.
During the videoconference sessions, in case of any difficulties with platform usage or connectivity, instant chat support, telephone contact, and an email address were provided as points of reference.
Instruments
PIs are the most commonly used type of intervention to support caregivers of people with dementia, with a strong emphasis on knowledge acquisition, such as the disease process and available services, the development of effective skills to address disease-related problems, and providing social support [39].
Our intervention is designed as a multi-component approach, not focusing exclusively on one strategy but containing multiple activities such as education, social support, problem-solving techniques, coping, and skill-building activities [17].
The intervention formats included slides, videos, and group discussions, all led by psychologists with clinical qualifications and expertise in neurodegenerative diseases. Specifically, the educational materials in textual and video format illustrate various aspects of the pathology, the less and more effective ways to handle stressful caregiving situations, coping strategies, and decision-making techniques to use in daily life.
The language used was simple to ensure comprehension among all participants and to facilitate interactive discussions and sharing of personal experiences.
At the conclusion of the PI, all participants received illustrated materials containing the most relevant information covered during the program.
Assessment
In a cohort of 73 caregivers (n = 33 internet-based group; n = 40 on-site conditions group), we evaluated crucial facets of the caregiver experience linked to the pathology (the level of management of BPSD, dementia awareness, social support, find leisure time, harmony with relative, stress) using a Visual-Analogue Scale (VAS) at the beginning (T0) and end (T1) of the program. This scale is widely employed in subjectively assessing various variables [40]: specifically, a vertically oriented VAS ranging from 0 to 100 was utilized. Participants were asked to rate aspects proposed on this continuum, for example: “How do you assess your level of disease knowledge from 0 (none) to 100 (very extensive)?” (Table 3).
Table 3.
Crucial facets of the caregiver experience linked to the pathology assessed using a Visual-Analogue Scale (VAS) at the beginning (T0) and end (T0) of the program
| Questions in Visual-Analogue Scale (VAS) |
|---|
| ● What is your ability to manage problematic situations related to the illness (e.g., symptoms)? |
| ● What is your knowledge of the illness? |
| ● How supported do you feel by friends, family, and local services? |
| ● At what level do you perceive your harmony with the family member (the person with the illness)? |
| ● What is your ability to find leisure time? |
| ● How much stress related to the condition do you experience? |
At the program's conclusion, a true/false questionnaire regarding specific basic information, learned during the course, was administered to all caregivers (Table 4). Participants' satisfaction was evaluated using a Likert scale and by tracking dropout rates. Additionally, upon completion of the program, acceptability, feasibility, and effectiveness were explored solely among participants engaged in internet-based sessions (n = 33) using a Likert scale (Table 5). The Likert scale used consists of five smiling-face elements, prompting participants to indicate their overall satisfaction level with the course or their degree of agreement or disagreement with specific statements about the feasibility of the online course, ranging from 'strongly disagree' on one end to 'strongly agree' on the other, with 'neither agree nor disagree' in the middle.
Table 4.
Questionnaire “True or False” on basic dementia knowledge
| Questionnaire “True or False” on basic dementia knowledge |
|---|
| ● When the patient's language becomes less understandable, communication becomes challenging |
| ● If the patient becomes agitated, trying to distract them with a pleasant activity might help |
| ● The disease doesn't manifest itself in the same way in every individual |
| ● Not all cognitive functions are affected by the disease |
| ● If the patient doesn't remember information, providing hints can be helpful |
| ● The illness doesn't affect genders equally |
| ● Physical exercise has no impact on mood |
| ● Taking care of oneself ensures better care for the person with dementia |
Table 5.
Research questions on the acceptability, feasibility, and effectiveness posed to caregivers with smiling face scale at the end of the Psychoeducational Interventions
| Acceptability, feasibility and effectiveness questions |
|---|
| ● Overall, did you enjoy the program? |
| ● Was the videoconference mode suitable for your needs? |
| ● Were you satisfied with the content covered in the sessions? |
| ● Did you feel the program had any beneficial aspects for you? |
| ● Have you implemented any of the strategies learned during the program? |
| ● Have the tools (chat and email contact) and materials (slides and pamphlets) provided during the course been helpful and effective? |
| ● Would you consider recommending this program to other caregivers? |
Statistical analysis
To describe the demographic and clinical characteristics of the study population and aspects of caregiver experience related to dementia, investigated using a Visual-Analogue Scale, descriptive parameters were calculated, including the mean and standard deviation (mean ± SD).
Differences between internet-based and on-site conditions groups for age, gender and degree of kinship have been evaluated using for quantitative variables, unpaired t tests or the nonparametric Mann–Whitney Rank Sum Test; for categorical variables, Chi-squared tests or Fisher’s exact method was applied. Shapiro–Wilk test was considered to test the normal distribution of quantitative variables.
For Visual Likert scale scores, a two-way analysis of variance (ANOVA) for repeated measures (RM) was performed, considering both factor “condition” (internet-based or on-site) and factor “time” (at beginning (T0) or at the end (T1)), with post hoc analysis Bonferroni method. A variance analysis was conducted to examine the effect of the categorical variables "gender” and “kinship" on the delta change between T0 and T1 in the VAS scale.
Statistical analyses were performed using statistical software package Sigma Stat 4.0; statistical significance was assumed for a p-value < 0.05.
Results
Of the 73 caregivers, n = 33 followed the program in "internet-based" condition, while n = 40 were in "on-site conditions" group. The two groups exhibited similarity in age, gender distribution, and kinship (p > 0.05 for all p-value; Table 6); specifically, the mean age was around 60 years, with a higher presence of females and spouses noted overall.
Table 6.
Demographic characteristics of participants in "internet-based" and “on-site condition” Psychoeducational Interventions (data are expressed as n, n (%), mean ± SD)
|
Total (n = 73) |
Internet-based (n = 33) |
On-site condition (n = 40) |
p-value | |
|---|---|---|---|---|
|
Age, years (means ± SD) |
60.4 ± 14.8 | 61.6 ± 14.2 | 59.4 ± 15.4 | 0.713 |
| Sex, women (n,%) | 51 (69.9) | 25 (75.8) | 26 (65.0) | 0.678 |
| Kinship | 0.134 | |||
| spouse (n,%) | 44 (60.3) | 20 (60.6) | 24 (60.0) | |
| son (n,%) | 26 (35.6) | 13 (39.4) | 13 (32.5) | |
| other (n,%) | 3 (4.1) | 0 (0.0) | 3 (7.5) | |
Dropout rates were extremely low, as only one individual in Internet-based condition (2.9%) and one individual in on-site conditions (2.5%) had an attendance rate below 80% at the sessions.
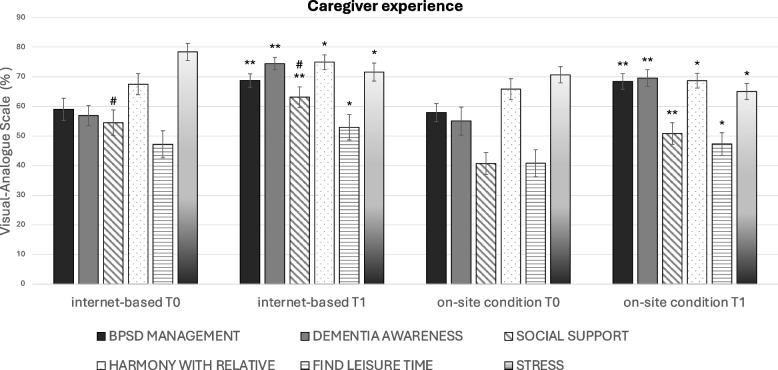
In the evaluation of aspects related to the caregiver experience concerning the pathology, both participation modalities showed a statistically significant improvement in all aspects examined on VAS scale. Specifically, the level of management of BPSD, dementia awareness and social support significantly improved at the end of the PI regardless of the mode of delivery (p < 0.001 for all p-values; Fig. 1); a similar improvement is also observed for harmony with relative, find leisure time and stress level (p = 0.007, p = 0.001, p = 0.001, respectively; Fig. 1). Overall, it is possible to observe that the group participating in online sessions perceives greater social support and lower stress levels (p = 0.013, p = 0.051, respectively; Fig. 1). Therefore, the aspects that have shown the greatest benefit from the intervention, both via videoconference and in-person, were the level of management of BPSD, dementia awareness, and social support which are specific objectives related to the course content. No significant effect of the variables "gender” and “kinship" was found on the change in VAS scores (delta T0-T1; p > 0.05).
Fig. 1.
Outcome measures pre- and post- Psychoeducational Interventions. Aspects of caregiver experience related to dementia, investigated using a Visual-Analogue Scale in internet-based and on- site conditions at the beginning (T0) and end (T1) of the PI. Two-way ANOVA post hoc analysis Bonferroni method, T0 versus T1 for “level of management of BPSD”, “dementia awareness” and “social support”, p < 0.001 for all p-values; for “harmony with relative”, “find leisure time” and “stress level”, p = 0.007, p = 0.001, p = 0.001, respectively. Statistical difference for factor “condition” were found for ““social support”, p = 0.013. *p < 0.01; ** p < 0.001 statistical significance for factor “time” (T0 vs T1); #p < 0.05 statistical significance for factor “condition” (internet-based vs on- site conditions); error bars = s.e.m
The questionnaire assessing basic dementia knowledge was completed successfully by 100% of the participants. Additionally, caregivers reported a medium to high level of satisfaction on all Smiling-face scales, indicating that the interaction with the therapist and group was appreciated, the content was beneficial, and the online mode was widely acceptable and usable.
Discussion
Caring for individuals with dementia is considered one of the most stressful and challenging caregiving tasks. Family caregivers consistently experience high levels of psychological burden, with symptoms of depression, anxiety, and physical strain [41, 42]. The physical and mental health of the caregiver is a prerequisite for supporting individuals with dementia and ensuring an improved quality of life. Long-term care systems must consider the significant emotional, financial, and social impact of caring for families and relatives while addressing the needs of people with dementia. This includes providing caregivers access to education, training, breaks, and social support through accessible and evidence-based resources [43]. In particular, PI are strongly recommended due to their beneficial effects on critical outcomes related to caregiver burden and stress [17, 25].
Many researchers have developed meta-analyses and systematic reviews to evaluate the effectiveness of various support protocols for caregivers. Leng and collaborators highlighted how the online support interventions examined significantly improved depressive symptoms, perceived stress, anxiety, and caregivers' self-efficacy, while no significant improvements were found in caregiver burden, ability to cope with behavioral symptoms or quality of life [44]. The results are in line with a recent study where participants in online interventions showed a significant improvement in caregiving ability and anxiety compared to control groups; modest results were also noted in measures of quality of life and caregiver burden [36].
This pilot study evaluates the applicability, feasibility and efficacy of a Psychoeducational Interventions program via videoconferencing compared to in-person sessions. The major uncertainties in remote usage focus on the replicability of effects, accessibility of content and materials used up to effective communication and interaction, both with the professional and the participant group, in addition to the availability of technology access and usability.
The two groups, online or face-to-face, show no statistically significant differences in demographic characteristics, level of participation, or aspects related to the caregiver experience concerning the pathology. It is noteworthy that the only discrepancy is the perception of greater social support and a tendency to have overall lower levels of stress in the group participating in videoconference meetings. This may indicate a reduced need for direct contact and better coping strategies, which would require further investigation using specific tools.
Our study highlights high participant engagement in both modes, recording extremely low drop-out rate. Additionally, the recorded satisfaction level has confirmed a high appreciation for the program in all its components, including topics, psychologists, group dynamics, and modality of interaction: caregivers, in general, felt valued in line with their expectations.
Significant participation is noted, with approximately 70% attendance by female caregivers and 60% by spouses in both modalities: this aligns with recent demographic estimates from the Italian National Institute of Health, which report that approximately 90% of family caregivers are female and about 50% are spouses [45]. These data are consistent with previous findings indicating a tendency for women to more frequently assume the role of caregiver compared to men [46]. Additionally, Poisson and collaborators observed that male caregivers tend to approach the role differently than female caregivers, showing less inclination to participate in research and a preference for practical assistance over emotional expression [47].
The availability of an online platform has allowed access to the service to caregivers residing in areas not adjacent to the CDCD or those who have transport difficulties. Furthermore, online PI are indeed extremely useful in times of health emergencies or reduced mobility. The remote mode, besides guaranteeing continuous care, ensures cost containment, service optimization in terms of availability schedule and the possibility of tailored interventions in one's environment [31].
However, face-to-face support remains important due to the live contact that guarantees an optimal perception of non-verbal components and the absence of the need for technological support and skills. This last aspect can be mitigated through a simple preliminary computer training, that could enhance users' ability to access online support. Hybrid support groups could be experimented with to allow greater accessibility for all while still offering the option of face-to-face contact [48].
The evidence presented in this pilot study underscores the crucial importance of caregiver support interventions in both conditions, showing significant improvements in key aspects of the caregiving experience. The perceived improvement by participants in investigated aspects highlights the substantial benefits of this protocol. In particular, the greatest advantages are observed in the direct targets of the PI’s topics, such as disease-related skills and competencies, as well as increased social support. This is particularly significant as it emphasizes tangible positive effects on caregivers' well-being and their ability to manage the challenges associated with caregiving responsibilities. Indeed, PI contribute to the development of effective coping strategies to alleviate caregiver burden, enabling them to continue providing care for their loved ones.
Caregivers of individuals affected by dementia should have access to information and support to effectively respond to and address the physical, mental, and social needs associated with caring for those living with dementia: information and support for caregivers constitute a central component of high-quality dementia care [49].
The perceived improvement by the participants in the aspects investigated, along with the high acceptance and feasibility of the PI, indicates that the current approach deserves to be continued and optimized.
In the future, more specific evaluation scales will be added in order to measure the well-being and perceived burden of caregiving. Additionally, to highlight the advantages of the approach, a randomized controlled trial could be conducted in which the control group is provided only with informational material, without participating in group sessions with psychologists. We aim to increase the sample size to strengthen the data collected in the present study and to estimate the influence of variables on the perceived well-being effects of the caregivers participating in the study. A follow-up will be scheduled to monitor the caregivers' well-being through the inclusion of a long-term update meeting for the participants. The follow-up could provide valuable insights into the lasting impact of the results achieved. Moreover, this longitudinal approach could capture the evolving needs of caregivers beyond immediate concerns and offer guidance for adapting support strategies as their circumstances change, ensuring long-term resilience.
Conclusions
Overall, our study underscores the critical importance of supporting caregivers of individuals with dementia, who face significant challenges and stress in their caregiving role. The study demonstrated the feasibility and effectiveness of a Psychoeducational Interventions delivered via videoconferencing, highlighting high participant engagement and satisfaction rates. Importantly, both internet-based and in-person interventions showed significant improvements in caregiver stress levels and abilities; therefore, the benefits observed are tangible and comparable to those experienced in face-to-face settings although online interventions offer less direct personal interaction. The findings suggest that caregivers require access to comprehensive support, including education, training, and social support, to effectively manage the physical, mental, and social needs of individuals with dementia.
Moving forward, further research could explore additional assessment scales to evaluate caregiver well-being and perceived burden more comprehensively. Additionally, randomized controlled studies and long-term follow-ups could provide insights into the lasting impact of support interventions and guide the development of tailored strategies to promote caregivers' long-term resilience. Ultimately, addressing the needs of caregivers is essential for ensuring the well-being of both caregivers and individuals with dementia within our long-term care systems.
Acknowledgements
Not applicable
Abbreviations
- PI
Psychoeducational Interventions
- WHO
World Health Organization
- CDCD
Centers for Cognitive Disorders and Dementias
- ISS
Istituto Superiore di Sanità (The Italian National Institute of Health)
- Covid
CoronaVirus Disease
- BPSD
Behavioural and Psychological Symptoms of Dementia
- VAS
Visual-Analogue Scale
- ANOVA
Analysis of Variance
- RM
Repeated Measures
- Vs
Versus
- T0
At the beginning of the Psychoeducational Interventions
- T1
At the end of the Psychoeducational Interventions
- SD
Standard deviation
- s.e.m
Standard Error of the Mean
Authors’ contributions
All of the authors listed in the byline have consented to their names on the manuscript and they have read and approved the final manuscript. In particular, all of the authors have contributed to the study: S.C. has made substantial contributions to conception, design of methodology, statistical analysis, interpretation of data and preparation of original draft; L.T. has made contributions in data collection and revision of manuscript; E.D.P. has made contributions in data collection and she has given final approval of the version to be submitted with critical review; M.C. has made contributions in data collection and revision of manuscript; R.C. revised the paper critically for important intellectual content; G.T. has made a contributions to conceptualization of research goals and she has given critical review of the draft.
Funding
The study is supported by the "Alzheimer's and Dementia Fund" of the National Dementia Plan, funded by the Ministry of Health.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Consent was obtained from the participants; the aggregated data has been collected and examined retrospectively in an anonymous form without any experimental procedure. The study adhered to the ethical guidelines of the 1975 Declaration of Helsinki and have been approved by AOUP ethics committee. The study protocol received approval from the Regional Ethical Committee for Clinical Experimentation (Comitato Etico di Area Vasta Nord Ovest—CEAVNO) for the publication of aggregated and anonymously reviewed data collected from medical records without an experimental procedure. The study adhered to the ethical guidelines of the 1975 Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M. World Alzheimer report 2016: improving healthcare for people living with dementia: coverage, quality and costs now and in the future. London: Alzheimer’s Disease International; 2016. [Google Scholar]
- 2.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. AlzheimersDement. 2011;7(3):263–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alzheimer’s Disease International. 2019. World Alzheimer Report 2019: Attitudes to dementia. London: Alzheimer’s Disease International (ADI), 2019.
- 4.Sousa RM, Ferri CP, Acosta D, Albanese E, Guerra M, Huang Y, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: A 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–94. [DOI] [PubMed] [Google Scholar]
- 6.Cagnin A, Di Lorenzo R, Marra C, Bonanni L, Cupidi C, Laganà V, et al. SINdem COVID-19 Study Group Behavioral and Psychological Effects of Coronavirus Disease-19 Quarantine in Patients With Dementia. Front Psychiatry. 2020;11:578015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18(2):250–67. [DOI] [PubMed] [Google Scholar]
- 8.Gilhooly KJ, Gilhooly ML, Sullivan MP, McIntyre A, Wilson L, Harding E, et al. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatr. 2016;16:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chamberlain L, Anderson C, Knifton C, Madden G. Suicide risk in informal carers of people living with dementia. Nurs Older People. 2018;30(5):20–5. [DOI] [PubMed] [Google Scholar]
- 10.Karg N, Graessel E, Randzio O, Pendergrass A. Dementia as a predictor of care-related quality of life in informal caregivers: a cross-sectional study to investigate differences in health-related outcomes between dementia and non-dementia caregivers. BMC Geriatr. 2018;18(1):189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Victor C, Rippon I, Nelis SM, Martyr A, Litherland R, Pickett J, et al. Prevalence and determinants of loneliness in people living with dementia: Findings from the IDEAL programme. Int J GeriatrPsychiatry. 2020;35(8):851–8. [DOI] [PubMed] [Google Scholar]
- 12.Prince M, Wimo AG M, Guerchet M, Ali G-C, Wu YT, Prina M. World Alzheimer Report 2015. The global impact of dementia. an analysis of prevalence, incidence, cost and trends. London: Alzheimer’s Disease International, 2015.
- 13.Winblad B, Amouyel P, Andrieu S, Ballard C, Brayne C, Brodaty H, et al. Defeating Alzheimer’s disease and other dementias: a priority for European science and society. Lancet Neurol. 2016;15(5):455–532. [DOI] [PubMed] [Google Scholar]
- 14.Guterman EL, Allen IE, Josephson SA, Merrilees JJ, Dulaney S, Chiong W, et al. Association between caregiver depression and emergency department use among patients with dementia. JAMA Neurol. 2019;76(10):1166–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Association A. 2014 Alzheimer’s disease facts and figures. Alzheimers Dement. 2014;10(2):e47–92. [DOI] [PubMed] [Google Scholar]
- 16.Prince M, Ali GC, Guerchet M, Prina AM, Albanese E, Wu YT. Recent global trends in the prevalence and incidence of dementia, and survival with dementia. Alzheimer’sResearch Therapy. 2016;8(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sörensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis The Gerontologist. 2002;42(3):356–72. [DOI] [PubMed] [Google Scholar]
- 18.Rees G. Global action on dementia. Australian Journal of Dementia Care. 2017;16:4. [Google Scholar]
- 19.Van Mierlo LD, Meiland FJ, Van der Roest HG, Dröes RM. Personalised caregiver support: effectiveness of psychosocial interventions in subgroups of caregivers of people with dementia. Int J GeriatrPsychiatry. 2012;27(1):1–14. [DOI] [PubMed] [Google Scholar]
- 20.Brodaty H, Woodward M, Boundy K, Ames D, Balshaw R, PRIME Study Group. Prevalence and predictors of burden in caregivers of people with dementia. Am J GeriatrPsychiatr. 2014;22(8):756–65. [DOI] [PubMed] [Google Scholar]
- 21.Serafini JD, Damianakis T, Marziali E. Clinical practice standards and ethical issues applied to a virtual group intervention for spousal caregivers of people with Alzheimer’s. Soc Work Health Care. 2007;44(3):225–43. [DOI] [PubMed] [Google Scholar]
- 22.Egan KJ, Pot AM. Encouraging Innovation for Assistive Health Technologies in Dementia: Barriers, Enablers and Next Steps to Be Taken. Am Med Dir Assoc. 2016;17(4):357–63. [DOI] [PubMed] [Google Scholar]
- 23.Marziali E, Garcia LJ. Dementia caregivers’ responses to 2 Internet-based intervention programs. Am J AlzheimersDisOtherDemen. 2011;26(1):36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKechnie V, Barker C, Stott J. The effectiveness of an Internet support forum for carers of people with dementia: a pre-post cohort study. J Med Internet Res. 2014;16(2):e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carter G, Monaghan C, Santin O. What is known from the existing literature about peer support interventions for carers of individuals living with dementia: A scoping review. Health Social Care Community. 2020;28(4):1134–51. [DOI] [PubMed] [Google Scholar]
- 26.Davies N, Hopwood J, Walker N, Ross J, Iliffe S, Walters K, et al. Designing and developing a co-produced theoretical and evidence-based online support for family caregivers of people with dementia at the end of life. BMC Palliat Care. 2019;18(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization. iSupport for dementia. Training and support manual for carers of people with dementia. Geneva: World Health Organization; 2019; Licence CC BY-NC-SA 3.0 IGO.
- 28.Mehta KM, Gallagher-Thompson D, Varghese M, Loganathan S, Baruah U, Seeher K, et al. iSupport, an online training and support program for caregivers of people with dementia: study protocol for a randomized controlled trial in India. Trials. 2018;19(1):271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teles S, Ferreira A, Paúl C. Feasibility of an online training and support program for dementia carers: results from a mixed-methods pilot randomized controlled trial. BMC Geriatr. 2022;22(1):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molinari-Ulate M, Guirado-Sánchez Y, Platón L, van der Roest HG, Bahillo A, Franco-Martín M. Cultural adaptation of the iSupport online training and support programme for caregivers of people with dementia in Castilla y León. Spain Dementia (London). 2023;22(5):1010–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Windle G, Flynn G, Hoare Z, Masterson-Algar P, Egan K, Edwards RT, et al. Effects of an e-health intervention “iSupport” for reducing distress of dementia carers: protocol for a randomised controlled trial and feasibility study. BMJ Open. 2022;12(9):e064314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xiao LD, Ye M, Zhou Y, Chang H, Brodaty H, Ratcliffe J, et al. Cultural adaptation of World Health Organization iSupport for Dementia program for Chinese-Australian caregivers. Dementia (London). 2022;21(6):2035–52. [DOI] [PubMed] [Google Scholar]
- 33.Parra-Vidales E, Soto-Pérez F, Perea-Bartolomé MV, Franco-Martín MA, Muñoz-Sánchez JL. Online interventions for caregivers of people with dementia: a systematic review. ActasEspanolas de Psiquiatria. 2017;45(3):116–26. [PubMed] [Google Scholar]
- 34.Ayoub MF, de Souza YLP, de Almeida T, Falcão DVDS. Synchronous psychological interventions by videoconferencing for caregivers of people with dementia: an integrative review. Dementia and Neuropsychologia. 2022;16(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miles L, McCausland BMS, Patel HP, Amin J, Osman-Hicks VC. A systematic review of the provision and efficacy of patient and carer information and support (PCIS) interventions for patients with dementia and their informal carers. Aging Clinical and ExperimentalResearch. 2020;32(12):2439–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boyt N, Ho AK, Morris-Bankole H, Sin J. Internet-facilitated interventions for informal caregivers of patients with neurodegenerative disorders: Systematic review and meta-analysis. Digital Health. 2022;8:20552076221129068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheng ST, Au A, Losada A, Thompson LW, Gallagher-Thompson D. Psychological Interventions for Dementia Caregivers: What We Have Achieved, What We Have Learned. Curr Psychiatry Rep. 2019;21(7):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72. [DOI] [PubMed] [Google Scholar]
- 39.Vandepitte S, Van Den Noortgate N, Putman K, Verhaeghe S, Faes K, Annemans L. Effectiveness of Supporting Informal Caregivers of People with Dementia: A Systematic Review of Randomized and Non-Randomized Controlled Trials. J Alzheimers Dis. 2016;52(3):929–65. [DOI] [PubMed] [Google Scholar]
- 40.Voutilainen A, Pitkäaho T, Kvist T, Vehviläinen-Julkunen K. Cite Share How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72(4):946–57. [DOI] [PubMed] [Google Scholar]
- 41.Shuter P, Beattie E, Edwards H. An exploratory study of grief and health-related quality of life for caregivers of people with dementia. Am J AlzheimersDisOtherDemen. 2014;29(4):379–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Z, Heffernan C, Tan J. Caregiver burden: A concept analysis. Int J Nurs Sci. 2020;7(4):438–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gauthier S, Rosa-Neto P, Morais JA, Webster C. World Alzheimer Report 2021: Journey through the diagnosis of dementia. London, England: Alzheimer’s Disease International. 2021.
- 44.Leng M, Zhao Y, Xiao H, Li C, Wang Z. Internet-Based Supportive Interventions for Family Caregivers of People with Dementia: Systematic Review and Meta-Analysis. JMIR J Med Internet Res. 2020;22(9): e19468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Istituto Superiore Di Sanità, 2024. Progetto fondo per l’Alzheimer e le demenze - le attività dell’osservatorio demenze dell’Istituto Superiore di Sanità (Anni 2021–2023) Report Nazionale. 2024
- 46.Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):P33-45. [DOI] [PubMed] [Google Scholar]
- 47.Poisson VO, Poulos RG, Withall AL, Reilly A, Emerson L, O’Connor CMC. A mixed method study exploring gender differences in dementia caregiving. Dementia (London). 2023;22(8):1862–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McLoughlin B, Atherton H, MacArtney JI, Dale J. Online support groups for carers of people living with dementia: An investigation of videoconferencing support groups in lockdown. Dementia. 2023;22(3):561–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Global status report on the public health response to dementia. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0 IGO.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.