Abstract
Introduction
The heart team approach is now the standard of care for patients with complex coronary artery disease; however, the definition of a heart team is variable. We embarked on a project to create an extended, multidisciplinary heart team to evaluate patients we deemed high risk for coronary revascularization. In doing so, we created a new service, workflow, and paradigm.
Methods
Herein, we describe the process through which we created our high-risk percutaneous coronary intervention team, our criteria for determining risk, our process for evaluating these patients, and quality assurance. Additionally, we describe the design of our prospective study assessing 200 patients with complex coronary artery disease. The primary outcomes include the final heart team revascularization decision, all-cause mortality, major adverse cardiac events, acute kidney injury, postintervention bleeding, and length of stay.
Conclusion
Establishing a multidisciplinary heart team may help with complex and high-risk patient and family scenarios and potentially improve patient outcomes. A study has been initiated to test this hypothesis formally.
Keywords: Coronary artery bypass graft, coronary artery disease, heart team, high risk, National Cardiovascular Data Registry
The heart team (HT) approach for patients with complex coronary artery disease consists of a multidisciplinary model that provides individualized risk assessment to optimize patient care. The HT approach has been well described in the literature and is considered the standard of care in North American and European guidelines.1–4 There is no uniform consensus on what constitutes a HT, but the basic tenet consists of communication and collaboration between an interventional cardiologist and a cardiothoracic surgeon. However, with the increasing complexity of pathology, sentiment has emerged that the “traditional” HT is inadequate.5 Therefore, we embarked on a hospital-wide approach to form a multidisciplinary HT consisting of noninvasive cardiology, interventional cardiology, cardiothoracic surgery, pulmonary/critical care, palliative care, and hospital medicine. Multiple risk prediction models exist, based on anatomic and physiologic data, for determination of which patients are “high risk” for percutaneous revascularization.6,7 We developed our own definition/criteria for “high-risk” patients who would be evaluated by the multidisciplinary HT.
In an effort to work toward continuous quality improvement within our institution, we thoroughly reviewed our data from the National Cardiovascular Data Registry (NCDR) database, and a potential area for improvement was noted with regard to high-risk, complex patients requiring percutaneous coronary intervention (PCI). Therefore, we established a formal team for high-risk coronary revascularization known as the high-risk PCI (HRPCI) team. Specifically, we involved multiple specialties to ensure that PCI was in the best interest of the patient and that additional comorbidities were optimally managed before and after revascularization. We also established specific definitions of high-risk patients, created a procedural workflow, and organized a monthly review of mortality and quality outcomes. Herein we describe the process for assembling an HRPCI team, collecting data, and evaluating prospective outcomes to determine the clinical impact of the HRPCI team.
METHODS
High-risk PCI service
The HRPCI service consists of an interventional cardiology attending, a general cardiology fellow, and an advanced practice provider who also manages the service administratively. Occasionally, residents and medical students also join the service. The HRPCI attendings must be approved for the role by senior cardiology and surgery leadership, who evaluate multiple aspects of the physician’s qualifications, including time in practice, number and complexity of cases, and overall outcomes. There is a clear definition of patients to be followed by the HRPCI service, which is described in more detail below. The HRPCI service follows patients in addition to their primary cardiologist and serves as a “safety net” for patients. Patients are followed from the time of initial consultation until discharge from the hospital, including on weekends.
The HRPCI physician is available 24/7 for consultation or procedural backup. If a patient meets any of the criteria listed below, the HRPCI service is consulted. In the setting of an ST-segment elevation myocardial infarction (STEMI), the HRPCI is available for second opinions prior to the procedure if needed. However, our institution has a STEMI-specific interventional cardiologist on call. Therefore, interventions may proceed in a timely manner even if the HRPCI physician is not consulted beforehand. However, all STEMI patients are followed by the HRPCI team for the duration of their inpatient stay. The HRPCI attendings are able to schedule outpatient cases as their schedule allows, with the understanding they will be available for HRPCI consults as needed. In our experience, the HRPCI attending usually completes two to three outpatient cases per day during their on-call week. If an urgent HRPCI consult is required, the outpatient cases may be delayed.
Additional team members
In addition to the HRPCI service described above, the multidisciplinary HRPCI team includes colleagues from hospital medicine, supportive and palliative care, pulmonary and critical care medicine, and cardiothoracic surgery. These teams are consulted for patients on the HRPCI service, as needed. Additional subspecialties such as advanced heart failure, advanced cardiac imaging, nephrology, hematology/oncology, etc. are also consulted on an as-needed basis depending on the patient’s comorbidities and clinical status. Before the patient undergoes PCI, all specialties consulted as part of the HRPCI team are asked for their input, and the case is discussed on an ad hoc conference call. All recommendations from each respective team are documented in the patient record in a consult or progress note, as appropriate. The HRPCI interventional cardiologist is responsible for verbally communicating the HRPCI team’s final recommendations directly to the primary team. It is important to note that the HRPCI team serves to provide recommendations to the primary team and does not supersede the primary cardiologist.
The supportive and palliative care service is an essential component in our HRPCI discussions. The patient’s personal wishes and goals are explored, family support is assessed, and limits of care are established. The risks and benefits of the procedure can then be explained in a way that is consistent with the patient’s wishes (and compatible with his or her social situation). In the event that the procedure turns out poorly for the patient, early involvement of supportive and palliative care ensures that the patient’s wishes are respected. In extremely high risk cases, this approach allows for a smooth transition to hospice care if the procedural goal cannot be met.
In a similar manner, pulmonary and critical care medicine is consulted early for periprocedural critical care management. For patients who are at risk for respiratory failure, early involvement of pulmonary and critical care specialists allows for prospective airway management and ventilator liberation strategies (including early tracheostomy).
“High risk” inclusion criteria
There are formal criteria for a patient to be placed on the HRPCI service, although any patient can be followed by the service after consultation with the HRPCI attending physician. The following types of patients are automatically added to the service:
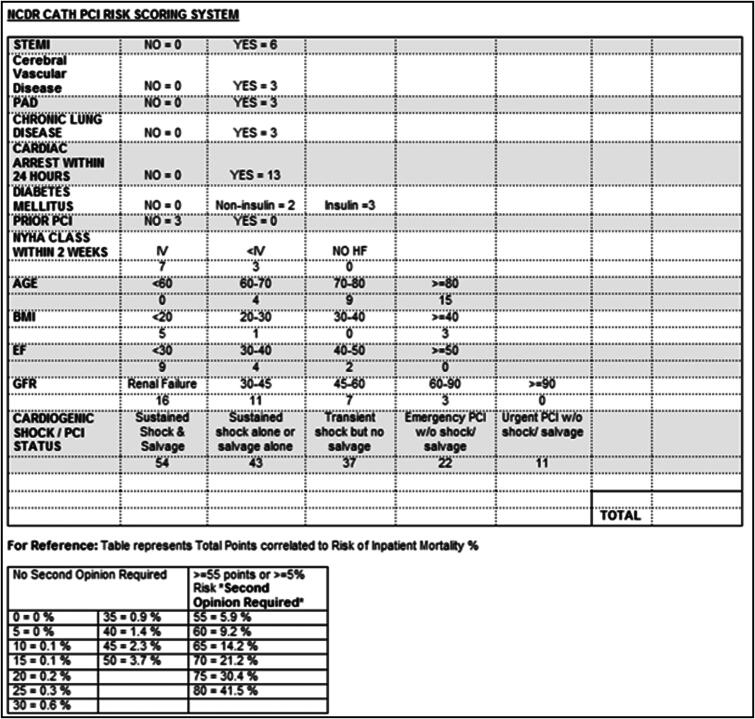
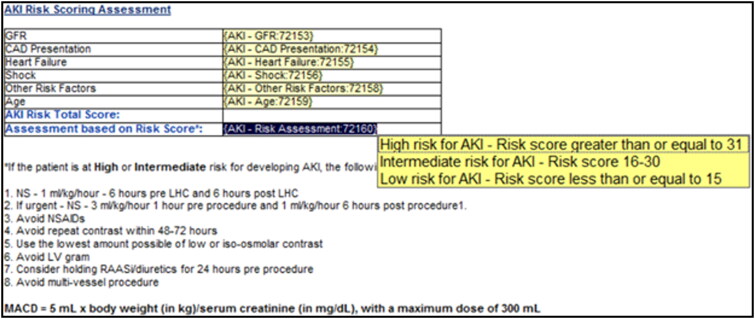
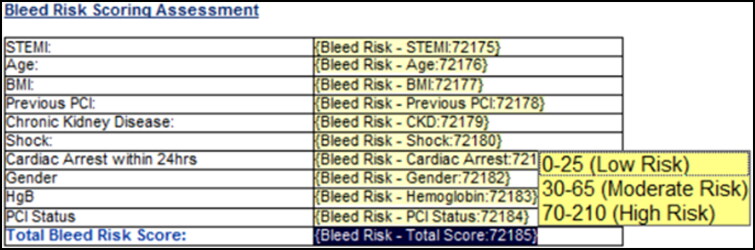
All inpatients undergoing heart catheterization with a calculated NCDR risk score of ≥55 (portending ≥5% mortality). This is calculated by the primary cardiologist. All inpatients are required to have a calculated NCDR risk score on the chart prior to being moved to the catheterization lab table. The first iteration, as shown in Figure 1, includes only the NCDR risk score. To curtail bleeding events and acute kidney injury following the procedures, bleeding and acute kidney injury risk scores have also been incorporated (Figures 2 and 3). These patients require a second opinion consultation with the HRPCI attending physician and are not moved to the catheterization lab until this has been completed.
All patients who present with STEMI.
All patients with unstable angina, non–ST-segment elevation myocardial infarction (NSTEMI), or elective PCI who stay more than 1 night after PCI.
All patients in cardiogenic shock who are being considered for revascularization. These patients are also followed by the advanced heart failure service.
All patients who are turned down for surgical revascularization, regardless of the reason.
All patients who undergo, or are being considered for, PCI with hemodynamic support devices.
Discretion of the primary cardiologist (difficult or high-risk coronary anatomy, need for assistance on a difficult case, challenging decision making prior to intervention, etc.).
Patients without a complex chronic total occlusion, as these cases are managed at our center by operators dedicated to chronic total occlusion PCI.
Figure 1.
National Cardiovascular Data Registry PCI risk scoring form. Scores ≥55 portend a mortality of >5%, prompting the need for a second opinion from the high-risk PCI attending physician.
Figure 2.
Acute kidney injury risk score and maximum allowable contrast dose calculation. Patients at intermediate or high risk for acute kidney injury are encouraged to be treated with the additional measures outlined. These patients are also encouraged to have early nephrology consultation if any acute kidney injury concerns arise.
Figure 3.
Bleeding risk score. Patients with a moderate or high risk of periprocedural bleeding are closely monitored after the procedure, especially if femoral access was used. In these patients, a “radial first” strategy is preferred.
HRPCI team meetings
When patients followed by the HRPCI service are scheduled for revascularization, their case is discussed early in the morning of their procedure. This discussion takes place either in person or via a teleconference. All available HRPCI attending physicians also participate. This meeting ensures that all members of the HRPCI team are aware of the planned procedure, all appropriate preprocedural planning has been completed, all input has been considered, and a bail-out strategy has been discussed. In the event of an urgent revascularization, an ad hoc meeting is held at any time of day or night.
Ad hoc meetings
Frequently, we have patients for whom a HRPCI consult is requested urgently or emergently. In such situations, the HRPCI team is assembled on an ad hoc basis. The appropriate films are sent to the team via secure communication, and a real-time video conference call is initiated. All available HRPCI attending physicians and the appropriate consultants join the call, day or night. As such, even in emergent situations, the appropriate teams are intimately aware of high-risk revascularization plans and are available for immediate assistance. Films are shared on Health Insurance Portability and Accountability Act–secure file-sharing platforms, and the team converses via secure platform, such as Microsoft Teams (Microsoft, Redmond, WA, US).
High-risk interventions
At any time, interventional cardiologists may request HRPCI operator double scrub to ensure that adequate backup is in place or to assist with a difficult case. The intervention plan is discussed by the operators and catheterization lab staff prior to the procedure. The cardiothoracic surgeon and pulmonary/critical care physician are kept updated on the status of the PCI. Mechanical circulatory support insertion kits/device consoles, covered stents, an ultrasound machine (with vascular access and cardiac probes), and other appropriate bailout devices are kept in the room.
STEMI physicians
Our institution has a complement of approximately 20 highly skilled, complex interventionalists who take STEMI call. Every quarter, a mandatory meeting is held for all physicians with STEMI privileges. At this meeting, overall and individual operator statistics, including outliers, delays of care, outcomes, etc., are reviewed. Subsequent process improvements are then made. This meeting is not a peer-review session; those meetings are conducted separately and in private.
Phase of care mortality assessment
All mortalities are reviewed at a monthly phase of care mortality assessment meeting. The purpose of this session is to identify the phase of care where the causative factor for the death occurred. Subsequently, process improvements are explored to correct preventable measures for the future.
Study design and statistical considerations for assessing HRPCI team impact
We aim to conduct an institution-wide, prospective analysis regarding the HRPCI team to quantitatively describe its impact. We hypothesize that addition of the HRPCI team will improve all-cause mortality and risk of major adverse cardiac events following intervention. Approximately 200 patients will be prospectively studied. All patients who meet the above inclusion criteria will be included in the data analysis. An institutional review board–approved protocol will be used. The following data will be collected:
Demographic information: age, sex, weight, height
Clinical presentation: Unstable angina, NSTEMI, STEMI, elective outpatient, transfer, cardiogenic shock
NCDR risk score
SYNTAX I and II scores
Comorbidities, including diabetes mellitus, hypertension, hyperlipidemia, smoking, heart failure class, left ventricular ejection fraction, creatinine clearance, dialysis, aspartate transaminase, alanine transaminase, international normalized ratio, albumin, hemoglobin, platelets
Surgical turndown reason
Prior physical activity/current frailty index as documented on admission by nursing staff
Family support assessed by palliative care
Categorical variables will be reported as percentages and compared using ANOVA and/or the Student t test as warranted. Continuous variables will be reported as mean ± standard deviation and compared using chi-square analysis.
Primary endpoints will include the final HT revascularization decision (PCI vs surgery vs medical therapy vs palliation), all-cause mortality, major adverse cardiovascular events (a composite of cardiovascular death, myocardial infarction, stroke, and repeat revascularization), acute kidney injury, post-PCI bleeding, and length of stay. Kaplan-Meier analysis will be performed for 30-day, 6-month, and 1-year outcomes.
Variables will be analyzed using multivariate regression to identify predictive trends/risk factors. A standard significance value of 0.05 will be utilized.
Patients that do not receive intervention (surgical or PCI) will be added to a registry and their outcomes followed.
DISCUSSION
Our approach to the coronary revascularization HT is unique in its formal structure, the addition of an HRPCI team, flexible (and frequent) team meetings/discussions, and integration of additional specialties. Despite its numerous members, the team can be quickly assembled for ad hoc meetings. All appropriate specialists can give their input prior to procedures to avoid unforeseen, preventable complications. Bail-out strategies are discussed and planned. Early supportive and palliative care involvement allows for prospective definition of the patient’s social status, family support, and goals of care. If necessary, early transition to hospice can be accomplished. Moreover, this hospital-wide collaboration helps patients better understand the overall risks associated with their PCI and maximizes physician engagement to deliver on the promise of clinical transformation.
By utilizing this multidisciplinary team-based approach, we have retrospectively shown an improvement in our PCI mortalities.8 Based on this evidence, we have developed the presently described prospective analysis, which will offer the opportunity for a more complete description of the impact of a dedicated HRPCI team, including prospective data collection as well as comparison of endpoints such as major adverse cardiac events, acute kidney injury, postintervention bleeding, and length of stay.
This study is subject to limitations. Most notably, the HRPCI structure varies significantly by hospital and is dependent upon factors such as available providers, imaging and laboratory capabilities, and potential treatments offered at a given institution. For example, a critical component of this structure is the presence of high-volume interventionalists who are able to dedicate a significant portion of their practice to high-risk candidates. Therefore, it is conceivable that the HRPCI structure herein described may not be viable at all institutions, particularly those with lower volumes or without dedicated HRPCI interventionalists.
In conclusion, we describe the implementation of a high-risk HT for the purpose of improving outcomes among patients at high risk for coronary revascularization. We have retrospectively shown improved PCI mortalities and are in the process of collecting prospective data to further evaluate the impact of a HRPCI team in our institution. Until prospective data is available, we hope to provoke thoughts, discussions, and provide a template for establishing a truly multidisciplinary HT. We hope that the structure outlined in this report may serve as a framework for other institutions interested in developing a similar HRPCI consultation service.
Funding Statement
Funding was provided by the Cardiovascular Research Review Committee of the Baylor Scott & White Research Institute. Financial support of CD, KM, and GM is a generous philanthropic gift of the Baylor Scott & White Dallas Foundation, the Roberts Foundation, and the family of Satish and Yasmin Gupta. .
Disclosure statement/Funding
Funding was provided by the Cardiovascular Research Review Committee of the Baylor Scott & White Research Institute. Financial support of CD, KM, and GM is a generous philanthropic gift of the Baylor Scott & White Dallas Foundation, the Roberts Foundation, and the family of Satish and Yasmin Gupta. The authors report no conflicts of interest.
References
- 1.Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Thorac Cardiovasc Surg. 2015;149(3):e5–e23. doi: 10.1016/j.jtcvs.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31(20):2501–2555. doi: 10.1093/eurheartj/ehq277. [DOI] [PubMed] [Google Scholar]
- 3.Head SJ, Bogers AJ, Serruys PW, Takkenberg JJ, Kappetein AP.. A crucial factor in shared decision making: the team approach. Lancet. 2011;377(9780):1836. doi: 10.1016/S0140-6736(11)60775-7. [DOI] [PubMed] [Google Scholar]
- 4.Young MN, Kolte D, Cadigan ME, et al. Multidisciplinary heart team approach for complex coronary artery disease: single center clinical presentation. J Am Heart Assoc. 2020;9(8):e014738. doi: 10.1161/JAHA.119.014738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeoh J, MacCarthy P.. Is it time to refresh the heart team? New paradigms for shared decision making. Heart. 2021;107(8):674–681. doi: 10.1136/heartjnl-2020-316588. [DOI] [PubMed] [Google Scholar]
- 6.Brennan JM, Curtis JP, Dai D, et al. Enhanced mortality risk prediction with a focus on high-risk percutaneous coronary intervention: results from 1,208,137 procedures in the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv. 2013;6(8):790–799. doi: 10.1016/j.jcin.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 7.Peterson ED, Dai D, DeLong ER, et al. Contemporary mortality risk prediction for percutaneous coronary intervention: results from 588,398 procedures in the National Cardiovascular Data Registry. J Am Coll Cardiol. 2010;55(18):1923–1932. doi: 10.1016/j.jacc.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christensen J, Al-Azizi K, Caras L, et al. Mortality improvement after institution of a multidisciplinary high-risk cardiology service. J Am Coll Cardiol. 2021;77(18):169. doi: 10.1016/S0735-1097(21)01528-X. [DOI] [Google Scholar]