Abstract
Objective
Femoral neck fractures (FNFs) are a common orthopedic type, and there are many treatment methods for it, and cannulated screw internal fixation is currently one of the main treatment methods. The choice of fully threaded cannulated screw (FCS) or partially threaded cannulated screw (PCS) remains controversial. Therefore, we performed this meta-analysis to evaluate the outcomes of FCS and PCS in the treatment of FNF.
Methods
Articles published before 29 April, 2024 were selected from PubMed, Embase, the Cochrane Library, and CNKI, using the PRISMA guidelines. Two independent reviewers searched and assessed the literature. The PICOS criteria were used to ensure that the included studies met the inclusion criteria. We used RevMan 5.3. Software to perform analysis.
Results
Compared with the PCS group, the FCS group had a lower femoral head necrosis rate (OR 0.60, 95% CI 0.37–0.98, P = 0.04), lower internal fixation failure rate (OR 0.37, 95% CI 0.22–0.62, P = 0.0002) and lower femoral neck shortening rate (OR 0.27, 95% CI 0.19–0.40, P < 0.00001). There was no statistically significant difference between the two groups in terms of the Harris hip score or nonunion rate.
Conclusions
The results of this meta-analysis revealed that compared with PCS, FCS had a lower incidence of postoperative complications and better postoperative outcomes in the treatment of FNF. Therefore, we believe that FCS may be a more effective treatment for FNF.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-024-05327-1.
Keywords: Femoral neck fracture, Internal fixation, Cannulated screws, Meta-analysis
Introduction
FNFs are a common form of clinical trauma, accounting for approximately 50% of hip fractures [1]. According to epidemiological surveys, the number of hip fractures worldwide is expected to increase from 1.26 million in 1990 to 4.5 million in 2050 [2]. FNFs are mostly in elderly individuals and are caused by low-energy falls [3], often the result of the osteoporosis [4], and younger patients are associated mainly with high-energy trauma [5]. The preferred treatment for most hip fractures is surgery, which allows patients to resume early mobility, reduces the risk of complications, and improves patient outcomes. Nonsurgical treatment should be considered only for patients with severe conditions and high surgical risk [5]. Surgical treatment options for femoral neck fractures include artificial hip joint replacement and internal fixation. Joint replacement is the main treatment strategy for displaced FNFs in elderly individuals. However, internal fixation is still the most commonly used surgical treatment for most young patients and patients who cannot tolerate hip arthroplasty [6]. Current internal fixation methods include dynamic hip screws, femoral neck systems, cannulated screws, and locking plates. Among these methods, three parallel PCSs in an inverted triangle is the common traditional internal fixation methods for FNFs [5]. Although many surgical strategies are available, hip fractures are still associated with a high rate of postoperative complications [7]. Numerous clinical studies have shown that three PCSs can provide good fixation effects [8–10]. However, there is also a risk of complications such as avascular necrosis of the femoral head (ANFH), femoral neck shortening, and internal fixation failure [11]. In recent years, FCS has been gradually applied in the internal fixation treatment of FNFs. Compared with PCSs, FCSs have biomechanically superior compressive strength and provide more stable support against shear forces and less muscle irritation [12]. However, in practical clinical applications, the conclusions of different clinical studies vary greatly in terms of their clinical effects and advantages over PCS. Therefore, it is necessary to integrate existing clinical study data via meta-analysis to investigate the safety and effectiveness of FCS and PCS in the treatment of FNF. In this study, we aimed to determine whether there are any differences between FCS and PCS in terms of femoral head necrosis, internal fixation failure, femoral neck shortening, postoperative nonunion, and the Harris hip score. We hypothesized that compared with PCS, FCS would improve the postoperative outcomes in the treatment of FNF.
Materials and methods
Search strategy
Electronic searches were performed by using PubMed, the Cochrane Library, Embase, and the China National Knowledge Infrastructure (CNKI) without restrictions for publication date and languages on April 29th, 2024. The search strategy employed for PubMed is presented in Table S1.
Inclusion criteria and exclusion criteria
The inclusion criteria were as follows: (1) patients with cannulated screw fixation for femoral neck fracture; (2) intervention: parallel FCS fixed experimental group; (3) control: parallel PCS fixed control group; (4) results: ANFH, nonunion rate, internal fixation failure rate, Harris hip score and femoral neck shortening rate; and (5) study design: prospective cohort studies, retrospective comparative controlled trials and randomized controlled trials.
The exclusion criteria were as follows: (1) review articles, conference summaries, case reports or biomechanical studies and (2) multiple injury patients.
Data extraction
Two researchers independently extracted the data from the identified articles following a standardized form. The following data were extracted: first author, country, year of publication, study type, age, sex ratio, affected side, Garden type, Pauwels type, follow-up time, outcome measures, etc. If data extraction inconsistencies among investigators occurred, a consensus was reached through discussion.
Data analysis and statistical methods
Statistical analyses were conducted with Review Manager Version 5.3 (Cochrane Collaboration, Software Update, Oxford, UK). Statistical heterogeneity was assessed using the I2 value. When I2 > 50%, P < 0.1 was considered to indicate significant heterogeneity, and the random-effect model was applied for the meta-analysis. Otherwise, the fixed-effect model was used. If possible, sensitivity analysis was conducted to search for the origins of heterogeneity. Dichotomous outcomes are expressed as odds ratios (ORs) with 95% confidence intervals (CIs). For continuous outcomes, mean differences (MDs) and 95% confidence intervals (CIs) were calculated. If P < 0.05, the results were considered statistically significant.
Results
Search results
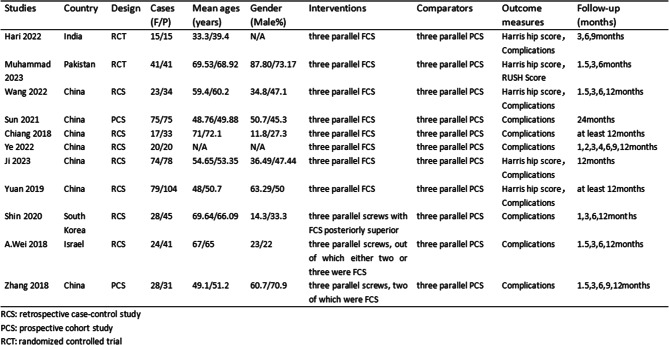
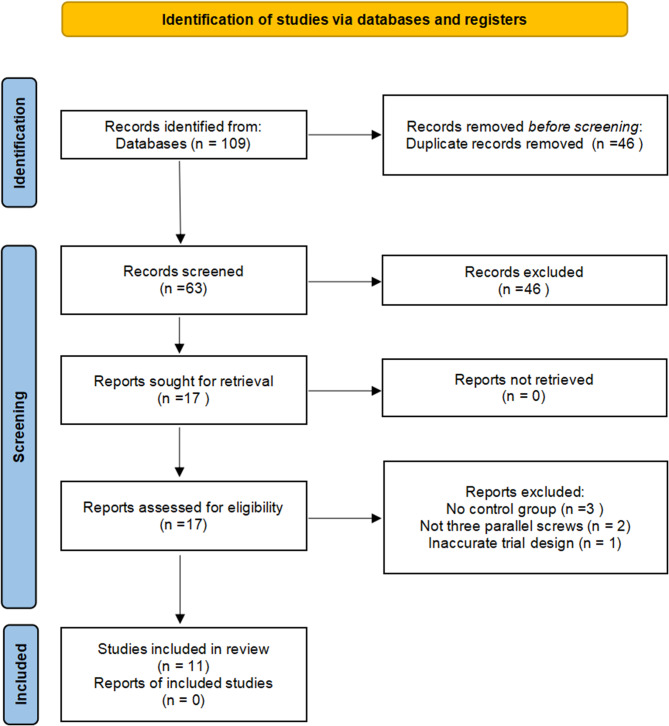
A total of 109 studies were identified with an initial decision, 46 duplicates were removed, and 63 studies were eligible for title and abstract screening. Following initial screening and application of the inclusion/exclusion criteria, there were two RCTs, two prospective cohort studies and seven retrospective case‒control studies, a total of 11 articles with 941 patients were ultimately included in this meta-analysis [12, 13, 15–23]. The characteristics are described in Table 1. The search process is shown in Fig. 1.
Table 1.
Characteristics of the included studies
Fig. 1.
Flowchart of the study selection process
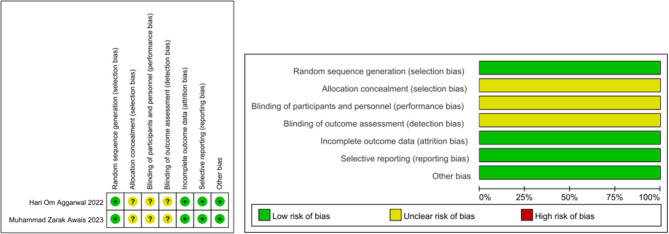
Risk assessment
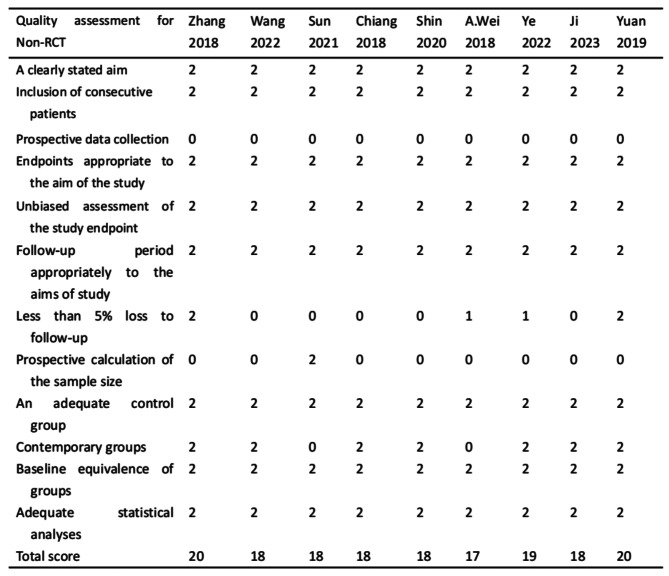
Two reviewers independently assessed all included studies via the risk-of-bias tool. The details of the included studies are summarized in Table 1. The Cochrane risk-of-bias criteria were used to assess the quality of the RCTs. Allocation concealment, blinding of participants and personnel and blinding of outcome assessment were unclear in all the included RCTs, and the remaining items (Fig. 2) were assessed to be at low risk of bias. The risk of bias was assessed for two prospective cohort studies and seven retrospective comparative controlled trials via the MINORs scale, the results of which are shown in Table 2. The MINORS score of the included articles ranged between 17 and 20 points, with an average of 18.4 points.
Fig. 2.
Risk of bias graph and risk of bias summary
Table 2.
Quality assessment for nonrandomized trials (MINORs)
Results of the meta-analysis
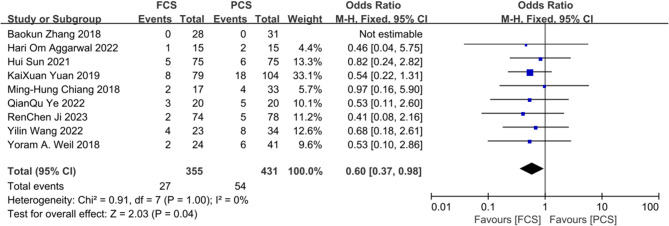
Femoral head necrosis rate
Nine studies reported data on the femoral head necrosis rate. Compared with PCS, FCS was more effective at reducing the rate of postoperative femoral head necrosis in patients with internal fixation of FNFs (OR 0.60, 95% CI 0.37–0.98, P = 0.04, I2 = 0%; Fig. 3).
Fig. 3.
Forest plot analysis of the femoral head necrosis rate
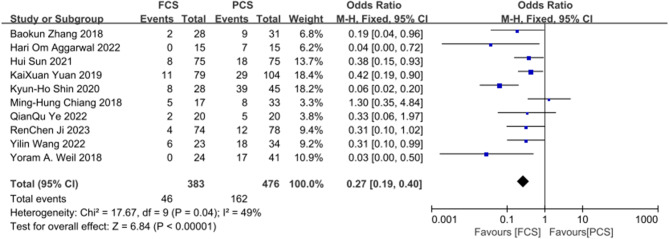
Femoral neck shortening rate
A total of 10 studies provided data on the femoral neck shortening rate. The probability of femoral neck shortening in the FCS group was lower than that in the PCS group (OR 0.27, 95% CI 0.19–0.40, P < 0.00001, I2 = 49%; Fig. 4).
Fig. 4.
Forest plot analysis of the femoral neck shortening rate
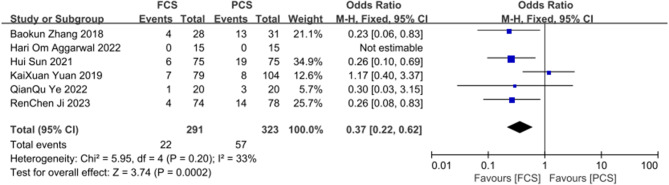
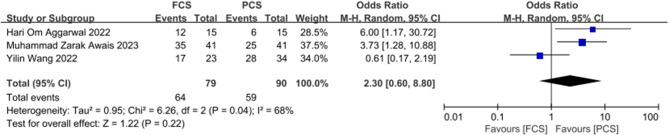
Internal fixation failure rate
Six studies provided data on the internal fixation failure rate. The results showed that FCS could significantly reduce the probability of postoperative internal fixation failure in patients (OR 0.37, 95% CI 0.22–0.62, P = 0.0002, I2 = 33%; Fig. 5).
Fig. 5.
Forest plot analysis of the internal fixation failure rate
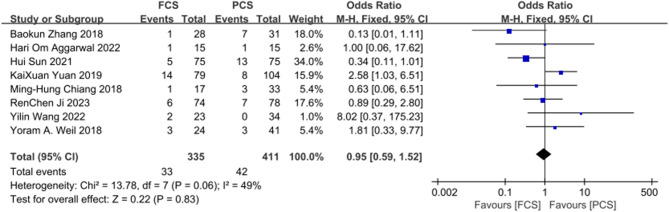
Nonunion rate
Eight studies reported data on the nonunion rate. The results revealed no significant differences between FCS and PCS in terms of the rate of nonunion after surgery (OR 0.95, 95% CI 0.59–1.52, P = 0.83, I2 = 49%; Fig. 6).
Fig. 6.
Forest plot analysis of the nonunion rate
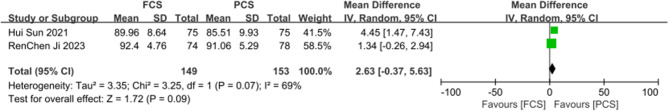
Harris hip score
Only 2 studies provided specific data on the Harris hip score and 3 studies provided excellent and good rate of Harris hip score. There were no differences between the two groups in Harris hip score (MD 2.63, 95% CI -0.37-5.63, P = 0.09, I2 = 69%; Fig. 7) and the excellent and good rates of Harris hip score (OR 2.30, 95% CI 0.60–8.80, P = 0.22, I2 = 68%; Fig. 8).
Fig. 7.
Forest plot analysis of the Harris hip score
Fig. 8.
Forest plot analysis of the rates of excellent and good Harris hip scores
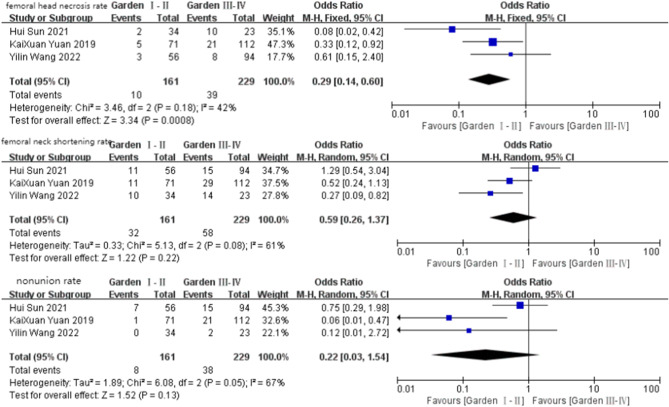
Further analysis of fracture types
We noticed that three articles provided detailed data on postoperative complications according to different fracture types. Therefore, we further analyzed these three articles according to the Garden classification, as shown in Fig. 9. Notably, the incidence of femoral head necrosis in displaced fractures is higher than that in non-displaced fractures, which indicates that fracture displacement may have a significant effect on patient prognosis.
Fig. 9.
Forest plot analysis of postoperative complications by fracture type
Discussion
To our knowledge, this is the first meta-analysis comparing the efficacy of FCS versus PCS in the treatment of FNF. FNFs, especially in young adults, are still a topic of concern because of the special anatomy of the femoral neck. Currently, complications may occur regardless of which internal fixation method is used to treat FNFs, and the incidence of internal fixation-related complications has been reported to be as high as 48% in the literature [11], especially in elderly patients with comorbidities [24]. Therefore, how to reduce the incidence of postoperative complications of FNF has become a hot issue for orthopedic surgeons worldwide. With the in-depth study of cannulated screw fixation by domestic and foreign scholars, PCS fixation has become the mainstream method for the treatment of FNFs in clinical practice [25]. However, problems such as screw pull-out and femoral neck shortening, femoral head necrosis, nonunion, and internal fixation failure can also occur [11]. Therefore, some scholars have proposed the use of FCS to replace PCS in the treatment of FNF and have achieved good results [15]. However, the results of individual clinical studies have not been consistent as to whether they compare favourably with the PCS. A prospective cohort study by Okcu G et al. [14] revealed that the use of FCS was not beneficial in reducing postoperative complications. Weil et al. [20] reported that FCS can significantly reduce femoral neck shortening after internal fixation without increasing the incidence of nonunion and osteonecrosis, which helps to improve the treatment outcome of FNF. Chiang et al. [18] found no significant differences in the rates of femoral neck shortening, osteonecrosis, nonunion or other complications between the two groups. Therefore, a meta-analysis is necessary to pool previous studies.
Our study suggests that treatment of FNF with FCS leads to a better prognosis. The reduction in postoperative complication rates may be related to the biomechanical advantages of this technique. Zhang et al. [26] showed that, compared with the PCS, FCS exhibited superior compressive strength and maximum load to failure. Li et al. [27] used finite element analysis to conclude that the fully threaded design of the FCS resulted in more stable support to counteract the shear force of vertical fracture.
In terms of clinical studies, several articles [13, 17, 18, 20, 22, 23] reported that there was no statistically significant difference in the rate of femoral head necrosis between the FCS and PCS groups, but our meta-analysis revealed that FCS was effective in reducing the rate of postoperative femoral head necrosis in patients with internal fixation of femoral neck fractures, and the results were significantly different (P < 0.05). This may be due to the small sample size of each clinical study.
In addition, femoral neck shortening is also a major problem. It can lead to abductor weakness due to shortening of the abductor muscle arm, resulting in impaired gait and reduced functional outcomes, ultimately reducing the patient’s quality of life. Related studies have evidenced marked loss of skeletal muscle mass 1 year after hip surgery [28]. Our study revealed that FCS significantly reduced the rate of femoral neck shortening. This is consistent with the findings of Weil et al. [20]. On the one hand, the PCS, as a sliding implant, provides dynamic compression during surgery and sliding during healing, and the proximal fragments and PCS may move laterally distally, resulting in neck shortening and lateral screw protrusion [13]. On the other hand, the tapered shape of the FCS allows it to have certain length stability to prevent neck shortening [26]. Chiang et al. [18] reported that FCS did not prevent femoral neck shortening, which is inconsistent with most findings [12, 13, 15, 17, 20] and we believe that this may be because this study was mainly based on elderly patients (mean age 71.7 years) and low-energy fracture patterns (Pauwels I-II 90%).
Internal fixation failure and nonunion are also major postoperative complications of femoral neck fracture, and our study suggests that FCS is effective in reducing the incidence of both. This finding is also consistent with the conclusions of most relevant studies [12, 13, 15]. Okcu G et al. [14] concluded that PCS resulted in a shorter healing time and a lower complication rate than did FCS, which may be related to the small sample size and the fact that fully threaded cannulated screws are not typically placed in three parallel inverted triangles.
The Harris hip score is a commonly used scoring system for assessing hip function status and postoperative outcomes. The Harris hip score and excellent and good rates of FCS were greater than those of PCS, but there was no significant difference between the two groups (p > 0.05); moreover, there was high heterogeneity in the results. We considered that only two studies provided specific data on the Harris hip score and that three studies provided excellent and good rate of Harris hip score; therefore, the high degree of heterogeneity was caused by the small number of included studies. In terms of the rates of excellent and good Harris hip scores, sensitivity analysis revealed that heterogeneity was present in the study of Wang [17]. When this study was excluded, the heterogeneity disappeared (I2 = 68% to 0%), and P < 0.05.
Therefore, on the basis of our meta-analysis, FCS is more recommended for femoral neck fractures than PCS. Sun [13] stated that FCS fixation could significantly reduce the complication rate of young patients with FNFs, especially those with high-energy fracture patterns (Garden III-IV, Pauwels III, or vertical of the neck axis (VN) angle ≥ 15°). Shin [19] found that the prevention of further posterior neck collapse after the use of a posterior fully threaded screw. These studies all revealed the superiority of FCS.
The limitations of this study include the following: (1) Although we included a total of 11 relevant articles, the total number of patients studied was only 941, which may not be large enough for the sample size. Perhaps more clinical studies with larger samples are needed to further confirm our results. (2) Due to incomplete original data, we did not perform further analysis based on relevant factors such as age in addition to fracture classification.
Conclusions
Our meta-analysis of the available evidence revealed that, compared with PCS, FCS could improve clinical and radiological outcomes after cannulated screw fixation for femoral neck fractures to some extent. Among them, we believe that the most important are femoral head necrosis and femoral neck shortening. As one of the most popular surgical options for treating femoral neck fracture, FCS is recommended to replace PCS for better postoperative results.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1 Table S1 Search strategy for PubMed.
Author contributions
X.S. conceived and designed this meta analysis. M.J. was involved in study selection, analysis, report writing and manuscript review. C.D. was involved in study selection and analysis. X.Z. participated in information retrieval and manuscript review. X.H. and J.Z. contributed to the data analysis and manuscript review. All authors read and approved the final manuscript.
Data availability
Data is provided within the manuscript or supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Prospero
CRD42024537142.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thorngren KG, Hommel A, Norrman PO, et al. Epidemiology of femoral neck fractures[J]. Injury. 2002;33:1–7. [DOI] [PubMed] [Google Scholar]
- 2.Veronese N, Maggi S. Epidemiology and social costs of hip fracture[J]. Injury. 2018;49(8):1458–60. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N, Aicale R. Proximal femoral fractures in the elderly: a few things to know, and some to forget[J]. Medicina. 2022;58(10):1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quaranta M, Miranda L, Oliva F, et al. Haemoglobin and transfusions in elderly patients with hip fractures: the effect of a dedicated orthogeriatrician. J Orthop Surg Res. 2021;16:387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral neck fractures: current management[J]. J Orthop Trauma. 2015;29(3):121–9. [DOI] [PubMed] [Google Scholar]
- 6.Ye CY, Liu A, Xu MY, et al. Arthroplasty versus internal fixation for displaced intracapsular femoral neck fracture in the elderly: systematic review and meta-analysis of short-and long-term effectiveness[J]. Chin Med J. 2016;129(21):2630–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marsillo E, Pintore A, Asparago G et al. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA)[J]. Orthop Rev, 2022, 14(6). [DOI] [PMC free article] [PubMed]
- 8.Bouaicha W, Jlidi M, Elarbi M, et al. Surgical management of neck of femur fractures in patients younger than sixty-five years: a comparative study of three fixation methods[J]. Int Orthop. 2023;47(12):3099–106. [DOI] [PubMed] [Google Scholar]
- 9.Abdallatif AG, Sharma A, Mahmood T et al. Complications and outcomes of the internal fixation of non-displaced femoral Neck fracture in Old patients: a two-year Follow-Up[J]. Cureus, 2023, 15(7). [DOI] [PMC free article] [PubMed]
- 10.Dolatowski FC, Frihagen F, Bartels S, et al. Screw fixation versus hemiarthroplasty for nondisplaced femoral neck fractures in elderly patients: a multicenter randomized controlled trial[J]. JBJS. 2019;101(2):136–44. [DOI] [PubMed] [Google Scholar]
- 11.Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures[J]. Clin Orthop Relat Res (1976–2007). 2007;458:175–9. [DOI] [PubMed] [Google Scholar]
- 12.Zhang B, Liu J, Zhu Y, et al. A new configuration of cannulated screw fixation in the treatment of vertical femoral neck fractures[J]. Int Orthop. 2018;42:1949–55. [DOI] [PubMed] [Google Scholar]
- 13.Sun H, Shu LY, Sherrier MC, et al. Decreased complications but a distinctive fixation loosening mechanism of fully threaded headless cannulated screw fixation for femoral neck fractures in young adults[J]. J Orthop Surg Res. 2021;16:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okcu G, Özkayın N, Erkan S, et al. Should full threaded compression screws be used in adult femoral neck fractures?[J]. Injury. 2015;46:S24–8. [DOI] [PubMed] [Google Scholar]
- 15.Aggarwal HO, Sharma A, Bansal N, et al. A comparative study of 30 cases of fracture neck femur in young adult patients treated with partially threaded cannulated screw versus fully threaded cannulated screws[J]. Natl J Physiol Pharm Pharmacol. 2022;12(12):2144–2144. [Google Scholar]
- 16.Awais MZ, Salik E, Bokhari SHR, et al. A comparative study of early functional outcomes in undisplaced neck of femur fracture treated with partially threaded and fully threaded cannulated screw fixation in patients above 60 years age[J]. Pakistan J Med Sci. 2023;39(5):1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Han N, Zhang D, et al. Comparison between headless cannulated screws and partially threaded screws in femoral neck fracture treatment: a retrospective cohort study[J]. Sci Rep. 2022;12(1):1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiang MH, Wang CL, Fu SH, et al. Does fully-threaded Headless Compression Screw provide a length-stable fixation in undisplaced femoral neck fractures?[J]. Asian J Surg. 2019;42(1):320–5. [DOI] [PubMed] [Google Scholar]
- 19.Shin KH, Hong SH, Han SB. Posterior fully threaded positioning screw prevents femoral neck collapse in Garden I or II femoral neck fractures[J]. Injury. 2020;51(4):1031–7. [DOI] [PubMed] [Google Scholar]
- 20.Weil YA, Qawasmi F, Liebergall M, et al. Use of fully threaded cannulated screws decreases femoral neck shortening after fixation of femoral neck fractures[J]. Arch Orthop Trauma Surg. 2018;138:661–7. [DOI] [PubMed] [Google Scholar]
- 21.Ye Q, Zeng G, Yu X et al. Clinical study of partially threaded combined with fully threaded hollow screws in the treatment of unstable femoral neck fractures in young and middle-aged patients[J]. Renowned Doctor, 2022, (06): 86–8.
- 22.Ji R, Lu X, Cong R, et al. Comparison of full thread compression cannulated screw and partial thread cannulated screw in treatment of femoral neck fracture[J]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023;37(01):19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yuan K. Comparison of efficacy between fully-threaded cannulated screws and partially-threaded cannulated screws in treatment of femoral neck fractures[J]. Shanghai Jiao Tong University; 2020.
- 24.Gargano G, Poeta N, Oliva F, et al. Zimmer Natural Nail and ELOS nails in pertrochanteric fractures. J Orthop Surg Res. 2021;16:509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Slobogean GP, Sprague SA, Scott T, et al. Management of young femoral neck fractures: is there a consensus?[J]. Injury. 2015;46(3):435–40. [DOI] [PubMed] [Google Scholar]
- 26.Zhang B, Liu J, Zhang W. Ordinary cannulated compression screws or headless cannulated compression screws? A synthetic bone biomechanical research in the internal fixation of vertical femoral neck fracture[J]. Biomed Res Int. 2018;2018(1):4898301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li J, Wang M, Li L, et al. Finite element analysis of different configurations of fully threaded cannulated screw in the treatment of unstable femoral neck fractures[J]. J Orthop Surg Res. 2018;13:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen YP, Kuo YJ, Hung SW, et al. Loss of skeletal muscle mass can be predicted by Sarcopenia and reflects poor functional recovery at one year after surgery for geriatric hip fractures[J]. Injury. 2021;52(11):3446–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1 Table S1 Search strategy for PubMed.
Data Availability Statement
Data is provided within the manuscript or supplementary information files.