Abstract
Background & Aims
Burnout is a global concern, and critical healthcare professionals have been identified as a high-risk population of burnout. Early identification is crucial, but the prevalence of burnout and its risk factors demonstrate significant geographical variations. This study aims to investigate the prevalence of burnout among critical healthcare professionals and explore potential risk factors during the post-pandemic era in Taiwan.
Methods
A web-based questionnaire survey was conducted from December 1, 2023, to January 31, 2024, targeting critical healthcare professionals employed in selected medical institutions affiliated with the Chang Gung Memorial Hospital Foundation, one of Taiwan’s largest healthcare organizations. Demographic information, the Subjective Happiness Scale (SHS), current work stressors and self-reported general health data were collected. The study utilized the Maslach Burnout Inventory Human Services Survey for Medical Personnel (MBI-MP). Univariate and multivariate logistic regression were employed to investigate the association between risk factors and each burnout subscales. A systematic review of Asian literature concerning burnout among critical care practitioners was also conducted.
Results
In our study, 254 participants were enrolled, with an overall burnout rate of 35.4%. The prevalence of high emotional exhaustion (EE) was 70.9%, high depersonalization (DP) was 56.3%, and low personal accomplishment (PA) was 60.6%. Young, unmarried populations, individuals with limited work experience, longer working hours, and night shifts are potential vulnerable groups susceptible to burnout. The top three stressors identified were excessive workload, the burden of administrative tasks, and a shortage of vacation time. Our systematic review included 20 Asian studies on the same issue, with variable burnout prevalence ranging from 16.3 to 82.1%.
Conclusion
The prevalence of burnout was high among critical healthcare professionals in post-pandemic Taiwan, particularly affecting younger, unmarried populations and individuals with limited work experience, longer hours, and more night shifts. The influence of pandemic-related factors has decreased. Regional variations in burnout have been observed across Asia, highlighting the need for further research to identify local risk factors and protect the well-being of professionals and healthcare quality.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-21084-6.
Keywords: Burnout, Occupational burnout, Mental wellbeing, Critical healthcare professionals, Post-COVID-19 era
Introduction
Burnout is a global issue resulted from chronic workplace stress that has not been successfully managed. It’s characterized by dimensions of EE, DP, and low PA [1–4]. Burnout led to not only the physical and psychological adverse effects of the suffering individuals but undesirable organizational consequences [5–9].
According to the previous studies, the overall prevalence of burnout rate ranged from 0 to 80.5% [10–12]. The estimated prevalence of burnout was 28.3% in the United States, 15.8% in Europe, 22.7% in Asia and 52.9% in Africa [10]. In the United States, key factors contributing to long working hours, inadequate staffing, lack of good management or leadership and work-life imbalance [10, 13]. In Asia, burnout was primarily driven by work pressure, job dissatisfaction and emotional strain [14–16]. Despite geographical variation in the risk factors for burnout, there are common issue, such as staffs working in emergency department (ED) and intensive care unit (ICU) being at higher risk for burnout and poor wellbeing [16–22]. High-quality critical care is not without cost to the clinicians [23]. Early identification and prevention of burnout are thus crucial to reduce negative consequences on critical healthcare professionals, patients, organizations, and the healthcare system [24–26].
As the COVID-19 pandemic raged on, the rising physical and psychological burden of the frontline critical healthcare professionals was discovered [20, 27–34]. Multiple studies demonstrated that the ED and ICU staffs were vulnerable groups of suffering from burnout [20, 28, 35–38]. Possible risk factors of burnout syndrome were reported by S Ramírez-Elvira et al. and M.R. Gualano et al. through conducting systematic reviews of literatures, the risk factors included the socio-demographic factors (being younger, unmarried, and lower professional experience) and working conditions (workload and working longer hours) [16, 36, 39–41].
Though threats related to the COVID pandemic, including lockdown policy, fear of uncertainty or shortages of Personal Protective Equipment (PPE), have lessened [42, 43], the post-pandemic era has seen a persistently high level of burnout [44, 45]. Unlike pre-pandemic period, issues such as understaffing, post-traumatic stress disorder (PTSD), overcrowding and the healthcare transformation have emerged as significant threats to healthcare professionals [44–48]. We hypothesize that the prevalence of burnout among the critical healthcare professionals remains high, with the landscape of the risk factors shifting in the post-pandemic era.
However, the prevalence and potential risks factors contributing to burnout vary across nations owing to the geographical heterogeneity, making local data crucial for developing effective strategies to mitigate burnout at both individual and organizational level [10, 16, 36]. To the best of our knowledge, there is limited literature on burnout among critical healthcare professionals in Asia during the post-pandemic era. Our study in Taiwan seeks to address this knowledge gap by exploring the prevalence and risk factors of burnout, with the aim of promoting the well-beings of the healthcare professionals.
Methods
Study design and setting
We performed a web-based, structural questionnaire survey from December 1, 2023, to January 31, 2024, to gather self-reported and cross-sectional information. The survey was anonymous, and we guaranteed the survey confidentiality to the participants. The link of the online questionnaire was shared with the emergency department and intensive care unit staff members who were willing to participate in the study after explaining the aim of our research. All the participants were employed at one of the following medical institutions of Chang Gung Memorial Hospital Foundation: Keelung Chang Gung Memorial Hospital (regional hospital), Linkou Chang Gung Memorial Hospital (medical center), Chiayi Chang Gung Memorial Hospital (regional hospital) and Jen-Ai Hospital, Dali Branch (regional hospital). As one of the largest healthcare providers in Taiwan, Chang Gung Memorial Hospital annually handles an average of 8.6 million outpatient visits and around 370,000 admissions. The study was conducted in accordance with relevant guidelines and regulations, and in compliance with the Declaration of Helsinki. Approved was obtained from the Jen-Ai Hospital Institutional Review Board (IRB), which waived the need for informed consent (IRB Number: 202300085B0).
Selection of study participants and sample size
The critical healthcare professionals including physicians and nurses were invited to participant the study if they worked in the emergency department or intensive care unit of the selected hospital and department since the outbreak of the pandemic. The selected hospital included Keelung Chang Gung Memorial Hospital, Linkou Chang Gung Memorial Hospital, Chiayi Chang Gung Memorial Hospital and Jen-Ai Hospital, Dali Branch. Staff who did not work in the emergency department or intensive care unit or did not care for COVID patients during the pandemic were excluded. Other medical staffs, such as social workers, secretaries, pharmacists, Hospital porters or radiographers were not included in the study. Using a 95% confidence interval and a 5% margin of error, our estimate suggests a minimum sample size of approximately 218 participants.
Description of the Survey and Measures
All participants comprehensively grasped the objective of this questionnaire upon reviewing the informed consent form prior to proceeding. The questionnaire comprises five sections with a total of forty-nine questions (Appendix Table 1). The sections, in sequence, encompass demographic data, personal health information, COVID-related inquiries, MBI-MP and SHS.
The MBI-MP stands as one of the most widely used measurement tools for assessing burnout comprising three subscales and a total of 22 items (EE: 9 items, DP: 5 items, PA: 8 items) [49]. Responses to scale items range from “1 = never” to “7 = always.” The scores for each of the three subscales are calculated separately and categorized as low, moderate, or high levels of burnout (EE, high: ≥27, moderate: 19 to 26, low: ≤18; DP, high: ≥10, moderate: 6 to 9, low: ≤5; PA, high: ≥40, moderate: 34 to 39, low: ≤33). In this study, the more conservative and widely accepted definition of overall burnout rate was employed. Burnout is defined as having ‘high EE,’ ‘high DP,’ and ‘low PA [10, 50].
The SHS is a 4-item scale of global subjective happiness [51]. Two items prompt respondents to characterize themselves using both absolute and relative ratings, while the other two items provide brief descriptions of happy and unhappy individuals, asking respondents to gauge how well each description fits them. The answers range from 1 to 7. To score the scale, sum the scores for the four questions and divide the total by four. This result is the “subjective happiness score”, typically ranging from about 4.5 to 5.5, with a higher score indicating greater happiness.
Data collection
Upon completion of the questionnaire, non-identifiable data were gathered. Two independent researchers (PTC and MYC) were responsible for assessing the questionnaire’s adequacy and performing additional data extraction. Any discrepancies were resolved through discussion with the senior researcher (CHW).
Statistical analysis
Baseline demographic categorical variables are depicted as percentages (%), while continuous variables are presented as mean ± SD. One-way ANOVA (Analysis of variance ) is used to examine differences between groups. However, if Levene’s test for homogeneity of variances fails (indicating significant variance differences between groups with p < 0.05), Welch’s ANOVA is used instead to check for differences. If differences are found, Tukey post hoc analysis is used to analyze the differences between groups. Univariate logistic regression was employed to investigate the association between potential risk factors and each burnout subscales (EE, DP, and PA; Table 1). Variables demonstrating significant univariate associations in logistic regression (P-values < 0.05) were further analyzed in multivariate logistic regression (Table 2 and Appendix Table 4). All analyses were conducted using SPSS Statistics, version 24.
Table 1.
The demographics of the included participants and the univariable analysis of the associated factors of burnout
| Variable | N | Emotional Exhaustion (EE) | Depersonalization (DP) | Personal Accomplishment (PA) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | meidan | High | M ± SD | P-value | Low | meidan | High | M ± SD | P-value | Low | meidan | High | M ± SD | P-value | ||
| All | 254 | 29(11.4%) | 45(17.7%) | 180(70.9%) | 35.4 ± 11.6 | NA | 41(16.1%) | 70(27.6%) | 143(56.3%) | 11.8 ± 6.5 | NA | 154(60.6%) | 71(28.0%) | 29(11.4%) | 30.6 ± 7.9 | NA |
| Age | ||||||||||||||||
| 20–29 | 119 | 10(8.4%) | 16(13.4%) | 93(78.2%) | 35.4 ± 11.6 | < 0.001 | 16(13.4%) | 33(27.7%) | 70(58.8%) | 12.7 ± 6.7 | < 0.008 | 81(68.0%) | 27(22.7%) | 11(9.2%) | 29.7 ± 8.1 | 0.121 |
| 30–39 | 92 | 9(9.8%) | 15(16.3%) | 68(73.9%) | 32.9 ± 11.4 | 12(13.0%) | 23(25.0%) | 57(62.0%) | 12.1 ± 6.4 | 53(57.6%) | 29(31.5%) | 10(10.9%) | 30.8 ± 7.4 | |||
| 40–49 | 39 | 7(17.9%) | 13(33.3%) | 19(48.7%) | 28.3 ± 10.2 | 10(25.6%) | 14(35.9%) | 15(41.0%) | 9.2 ± 5.5 | 17(43.6%) | 14(35.9%) | 8(20.5%) | 33.2 ± 8.3 | |||
| > 50 | 4 | 3(75.0%) | 1(25.0%) | 0(0.0%) | 16.8 ± 5.6 | 3(75.0%) | 0(0.0%) | 1(25.0%) | 6.0 ± 4.0 | 3(75.0%) | 1(25.0%) | 0(0.0%) | 30.0 ± 5.0 | |||
| Occupation | ||||||||||||||||
| Physician | 46 | 9(19.6%) | 9(19.6%) | 28(60.9%) | 30.6 ± 12.7 | 0.106 | 8(17.4%) | 11(23.9.%) | 27(62.8%) | 12.7 ± 6.9 | 0.331 | 24(52.2%) | 19(41.3%) | 3(6.6%) | 31.4 ± 8.3 | 0.483 |
| Nurse | 208 | 20(9.6%) | 36(17.3%) | 152(73.1%) | 33.7 ± 11.3 | 33(15.9%) | 59(28.4%) | 116(55.8%) | 11.6 ± 6.5 | 130(62.5.%) | 52(25.0%) | 26(12.5%) | 30.5 ± 7.8 | |||
| Workplace | ||||||||||||||||
| ER | 133 | 16(12.0%) | 22(16.6%) | 95(71.4%) | 33.9 ± 12.7 | 0.718 | 15(11.3%) | 32(24.1%) | 86(64.7%) | 13.7 ± 7.0 | < 0.001 | 81(60.9%) | 36(27.1%) | 16(12.0%) | 30.3 ± 8.3 | 0.134 |
| ICU | 121 | 13(10.7%) | 23(19.0%) | 85(70.2%) | 32.3 ± 10.3 | 26(21.5%) | 38(31.4%) | 57(47.1%) | 9.7 ± 5.3 | 73(60.3%) | 35(28.9%) | 13(10.7%) | 30.9 ± 7.4 | |||
| Marital status | ||||||||||||||||
| Single | 154 | 12(7.8%) | 21(13.6%) | 121(78.6%) | 35.4 ± 11.9 | < 0.001 | 21(13.6%) | 38(24.7%) | 95(61.7%) | 12.8 ± 6.8 | < 0.001 | 102(66.2%) | 39(25.3%) | 13(8.4%) | 29.7 ± 7.7 | 0.016 |
| Married | 100 | 17(17.0%) | 24(24.0%) | 59(59.0%) | 29.6 ± 10.3 | 20(20.0%) | 32(32.0%) | 48(48.0%) | 10.2 ± 5.8 | 52(52.0%) | 32(32.0%) | 16(16.0%) | 32.1 ± 8.0 | |||
| Number of children | ||||||||||||||||
| 0 | 170 | 14(8.2%) | 24(14.1%) | 132(77.6%) | 34.6 ± 11.6 | 0.007 | 24(14.1%) | 42(24.7%) | 104(61.2%) | 12.7 ± 6.7 | 0.007 | 113(66.5%) | 44(25.9%) | 13(7.7%) | 29.8 ± 7.6 | 0.091 |
| 1 | 22 | 3(13.6%) | 4(18.2%) | 15(68.2%) | 33.7 ± 11.6 | 1(4.6%) | 7(31.8%) | 14(63.6%) | 11.9 ± 6.2 | 13(59.1%) | 5(22.7%) | 4(18.2%) | 31.4 ± 7.9 | |||
| 2 | 50 | 9(18.0%) | 14(28.0%) | 27(54.0%) | 29.2 ± 10.8 | 13(26.0%) | 17(34.0%) | 20(40.0%) | 9.7 ± 6.0 | 22(44.0%) | 18(36.0%) | 10(20.0%) | 32.7 ± 8.7 | |||
| ≥ 3 | 12 | 3(25.0%) | 3(25.0%) | 6(50.0%) | 26.9 ± 10.3 | 3(25.0%) | 4(33.3%) | 5(41.7%) | 8.1 ± 4.7 | 6(50.0%) | 4(33.3%) | 2(16.7%) | 32.6 ± 7.7 | |||
| Do you have pets | ||||||||||||||||
| No | 189 | 22(11.6%) | 36(19.0%) | 131(69.3%) | 33.2 ± 11.9 | 0.789 | 28(14.8%) | 51(27.0%) | 110(58.2%) | 11.7 ± 6.2 | 0.633 | 117(61.9%) | 50(26.5%) | 22(11.6%) | 30.7 ± 7.9 | 0.928 |
| Yes | 65 | 7(10.8%) | 9(13.8%) | 49(75.4%) | 32.8 ± 10.9 | 13(20.0%) | 19(29.2%) | 33(50.8%) | 12.1 ± 7.4 | 37(56.9%) | 21(32.3%) | 7(10.8%) | 30.6 ± 7.8 | |||
| Previous work experience in ED/ICU | ||||||||||||||||
| No | 190 | 19(10.0%) | 30(15.8%) | 141(74.2%) | 35.4 ± 12.1 | 0.108 | 28(14.7%) | 54(28.4%) | 108(56.8%) | 12.0 ± 6.7 | 0.338 | 118(62.1%) | 54(28.4%) | 18(9.5%) | 30.7 ± 7.3 | 0.919 |
| Yes | 64 | 10(15.6%) | 15(23.4%) | 39(60.9%) | 33.2 ± 10.2 | 13(20.3%) | 16(25.0%) | 35(54.7%) | 11.1 ± 6.0 | 36(56.3%) | 17(26.6%) | 11(17.2%) | 30.5 ± 9.5 | |||
| The length of time of being critical healthcare professionals (years) | ||||||||||||||||
| 1–5 | 105 | 8(7.6%) | 13(12.4%) | 84(80.0%) | 35.5 ± 11.1 | 0.007 | 13(12.4%) | 26(24.8%) | 66(62.9%) | 13.0 ± 6.7 | < 0.001 | 67(63.8%) | 28(26.7%) | 10(9.5%) | 30.5 ± 7.6 | < 0.001 |
| 6–10 | 56 | 5(8.9%) | 12(21.4%) | 39(69.6%) | 33.9 ± 12.6 | 7(12.5%) | 15(26.8%) | 34(60.7%) | 12.6 ± 6.7 | 37(66.1%) | 13(23.2%) | 6(10.7%) | 29.1 ± 8.4 | |||
| 11–15 | 46 | 6(13.0%) | 8(17.3%) | 32(69.6%) | 31.2 ± 10.5 | 8(17.3%) | 12(26.1%) | 26(56.5%) | 11.2 ± 6.3 | 28(60.9%) | 11(23.9%) | 7(15.2%) | 30.6 ± 8.2 | |||
| > 15 | 47 | 10(21.3%) | 12(25.5%) | 25(53.2%) | 28.7 ± 11.3 | 13(27.7%) | 17(37.0%) | 17(36.1%) | 8.8 ± 5.3 | 22(47.8%) | 19(40.4%) | 6(12.8%) | 32.8 ± 7.2 | |||
| Average working hours a week | ||||||||||||||||
| ≤ 30 | 5 | 0(0.0%) | 2(40.0%) | 3(60.0%) | 32.2 ± 10.0 | 0.001 | 1(20.0%) | 2(40.0%) | 2(40.0%) | 11.0 ± 6.3 | 0.474 | 3(60.0%) | 1(20.0%) | 1(20.0%) | 33.2 ± 7.0 | 0.743 |
| 31–40 | 114 | 15(13.2%) | 25(21.9%) | 74(64.9%) | 30.9 ± 11.3 | 16(14.0%) | 34(29.8%) | 64(56.1%) | 11.5 ± 6.0 | 68(59.6%) | 35(30.7%) | 11(9.6%) | 30.2 ± 8.4 | |||
| 41–50 | 114 | 14(12.3%) | 16(14.0%) | 84(73.7%) | 33.8 ± 11.5 | 21(18.4%) | 30(26.3%) | 63(55.3%) | 11.8 ± 6.7 | 71(62.3%) | 29(25.4%) | 14(12.3%) | 31.3 ± 7.4 | |||
| > 50 | 21 | 0(0.0%) | 2(9.5%) | 19(90.5%) | 41.7 ± 10.4 | 3(14.3%) | 4(19.0%) | 14(66.7%) | 13.9 ± 8.4 | 12(57.1%) | 6(28.6%) | 3(14.3%) | 30.3 ± 8.1 | |||
| Average night shifts in one month | ||||||||||||||||
| ≤ 25% | 64 | 12(18.8%) | 16(25.0%) | 36(56.3%) | 29.2 ± 11.4 | 0.014 | 14(21.9%) | 24(37.5%) | 26(40.6%) | 9.9 ± 6.4 | 0.038 | 33(51.6%) | 22(34.4%) | 9(14.1%) | 31.5 ± 8.4 | 0.445 |
| 25–50% | 74 | 5(6.8%) | 15(20.3%) | 54(73.0%) | 33.9 ± 10.8 | 8(10.8%) | 16(21.6%) | 50(65.8%) | 13.0 ± 6.4 | 47(63.5%) | 18(24.3%) | 9(12.2%) | 29.5 ± 8.7 | |||
| 50–75% | 60 | 6(10.0%) | 6(10.0%) | 48(80.0%) | 35.6 ± 11.9 | 10(16.7%) | 16(26.7%) | 34(56.7%) | 12.2 ± 6.4 | 39(65.0%) | 16(26.7%) | 5(8.3%) | 30.5 ± 7.5 | |||
| ≥ 75% | 56 | 6(10.7%) | 8(14.3%) | 42(75.0%) | 34.0 ± 11.7 | 9(16.1%) | 14(25.0%) | 33(58.9%) | 12.0 ± 6.7 | 35(62.5%) | 15(26.8%) | 6(10.7%) | 31.3 ± 6.6 | |||
Table 2.
The multivariable analysis of overall burnout and the associated factors of the included participants
| Category | Covariate | Hazzard ratio (95% CI) | P-value |
|---|---|---|---|
| Age | 20–29 | 1 | |
| 30–39 | 1.19(0.48–2.96) | 0.706 | |
| 40–49 | 0.29(0.04–2.15) | 0.223 | |
| > 50 | 0 | 0.999 | |
| Marital status | Single | 1 | |
| Married | 0.67(0.24–1.85) | 0.443 | |
| Number of children | 0 | 1 | |
| 1 | 3.39(0.89–12.88) | 0.073 | |
| 2 | 1.82(0.50–6.50) | 0.363 | |
| ≥ 3 | 1.95(0.22–16.96) | 0.545 | |
| The length of time working | 1–5 | 1 | |
| 6–10 | 0.80(0.35–1.86) | 0.609 | |
| 11–15 | 0.97(0.30–3.11) | 0.956 | |
| > 15 | 0.15(0.02–0.98) | 0.048 | |
| Working hours per week | ≤ 30 | 1 | |
| 31–40 | 1.26(0.12–13.8) | 0.848 | |
| 41–50 | 1.32(0.12–14.49) | 0.823 | |
| > 50 | 1.76(0.14–22.14) | 0.663 | |
| Average night shifts per month | ≤ 25% | 1 | |
| 25–50% | 2.55(0.98–6.63) | 0.055 | |
| 50–75% | 2.93(1.09–7.83) | 0.033 | |
| ≥ 75% | 1.76(0.68–4.56) | 0.247 |
Ethical considerations
Ethics approval
was secured from the IRB of Jen-Ai Hospital (IRB Number: 202300085B0). All submitted questionnaires were treated with strict confidentiality, accessible only to the researchers involved in this study. License granting the right to utilize and administer the Maslach Burnout Inventory has been secured. There was no external funding source was involved in this research initiative.
Results
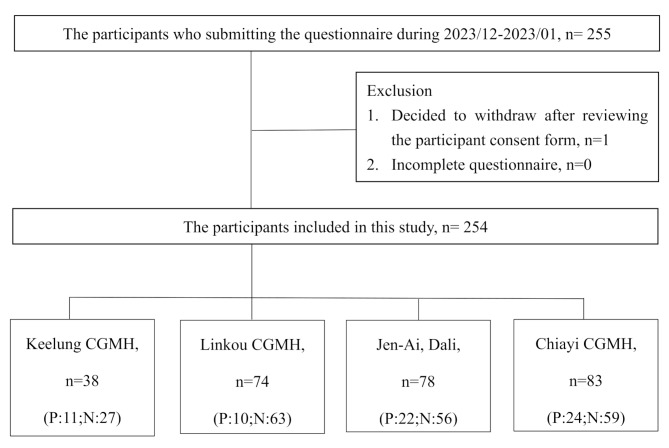
We conducted a self-reported questionnaire survey spanning from December 2023 to January 2024. The study involved 254 critical healthcare professionals across four hospitals in Taiwan: Keelung Chang Gung Memorial Hospital (38 participants), Linkou Chang Gung Memorial Hospital (74 participants), Chiayi Chang Gung Memorial Hospital (83 participants), and Jen-Ai Hospital, Dali Branch (78 participants, Fig. 1). The response rate achieved was around 51.0%. Through manual examination, no duplicated or incomplete questionnaires were identified but one participant decided to withdraw after reviewing the participant consent form.
Fig. 1.
The study flowchart. * n: number; P: physician; N: nurse
Demographic characteristics, general health conditions and the Subjective Happiness Scale (SHS) of the included participants
Among 254 participants, 46.9% were under 30 years old, with the majority being nurses (81.9%) and unmarried (60.6%). A total of 133 participants worked in the emergency room (ER, 52.4%). A significant portion (41.3%) had less than five years of experience in their current emergency department or intensive care unit. Furthermore, 53.2% of participants worked over 40 h per week, and 45.7% had night shifts for over 50% of the month. Table 1 provides detailed demographic characteristics.
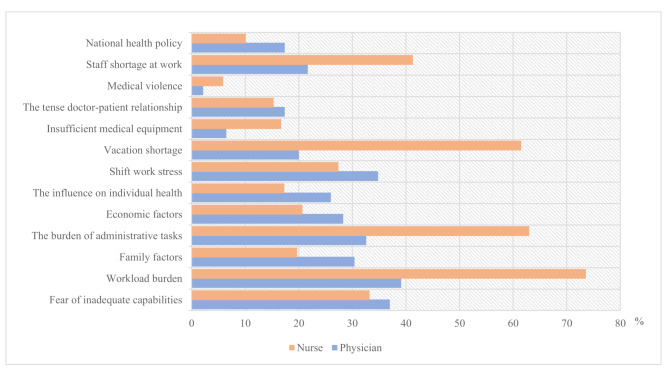
Regarding self-assessed general health conditions, detailed results can be found in Appendix Table 5. Half of the participants rated their health condition as comparable to others. A low percentage relied on medication for sleep (7.8%), used tobacco (2.4%), or consumed alcohol (2.8%). Additionally, the majority (41.7%) did not have regular exercise habits. More than half (58.3%) sometimes experienced stress, while only 15.7% never considered quitting in the past month. About the current workplace stressors, there is differences between physicians and nurses. Nurses reported workload burden (73.6%), additional administrative tasks (63.0%), and a shortage of vacation time (61.5%) as their primary sources of workplace stress, while physicians mentioned workload burden (39.1%), fear of inadequate capabilities (37.0%), and shift work stress (34.8%) as their top stressors. Among the participants, the average subjective happiness score was 4.6, with detailed scores of each subgroup listed in Appendix Table 6.
Prevalence of burn-out among critical healthcare professionals and the results of each subscale of the MBI-Human Services Survey for Medical Personnel (MBI-MP)
In our study, we found that the overall burnout rate was 35.4% (nurses: 37.5%, physicians: 26%). Specifically, the prevalence of high EE was 70.9%, high DP was 56.3%, and low PA was 60.6%.
Regarding the results of each subscale, the average EE score was 35.4 ± 11.6. Nurses experienced higher EE compared to physicians. Additionally, younger individuals, those who were single, worked in the ER, had longer average working hours per week, and had more night shifts tended to have higher levels of EE. The mean score for DP was 11.8 ± 6.5. Younger individuals, physicians, those working in the ER, singles, those with no previous critical care experience, and those who had been critical healthcare professionals for a shorter period tended to have higher levels of DP. The average score for PA was 30.6 ± 7.9. Lower levels of PA were observed among younger and single individuals. For a concise overview of burnout components, please refer to the details outlined in Table 1.
Associated factors of burn-out syndrome
Table 1 summarizes the results of the univariable analysis regarding the potential factors associated with each burnout subscale. Variables that revealed significant univariate associations were subsequently included in the multivariate analyses (Table 2 and Appendix Table 4). The results demonstrated that individuals with less experience (6–10 years: 0.80, 95% CI 0.35 to 1.86; 11–15 years: 0.97, 95% CI 0.30 to 3.11; >15 years: 0.15, 95% CI 0.02 to 0.98) and those with more night shifts (25–50%: 2.55, 95% CI 0.98 to 6.63; 50–75%: 2.93, 95% CI 1.09 to 7.83; ≥75%: 1.76, 95% CI 0.68 to 4.56) had an increased risk of overall burnout.
Further analysis showed that none of the factors remained significant in increasing the risk of higher EE. However, younger individuals (30–39 years: 2.72, 95% CI 1.05 to 7.07; 40–49 years: 1.20, 95% CI 0.23 to 6.21; >50 years: 0.19, 95% CI 0.01 to 4.62), less experienced individuals (6–10 years: 0.70, 95% CI 0.29 to 1.71; 11–15 years: 1.06, 95% CI 0.31 to 3.59; >15 years: 1.92, 95% CI 0.41 to 9.11), and those with more night shifts (25–50%: 2.85, 95% CI 1.16 to 7.00; 50–75%: 2.54, 95% CI 1.02 to 6.32; ≥75%: 1.80, 95% CI 0.74 to 4.39) had a higher risk of suffering from DP. The risk of experiencing low PA was greater for less experienced individuals (6–10 years: 0.52, 95% CI 0.22 to 1.21; 11–15 years: 0.31, 95% CI 0.09 to 1.00; >15 years: 0.79, 95% CI 0.19 to 3.29).
Discussion
This study explored the prevalence of burnout among critical healthcare professionals in Taiwan during the post-pandemic era. Data were collected from 254 participants employed at medical institutions affiliated with the Chang Gung Memorial Hospital Foundation. The findings revealed a burnout rate of 35.4%, characterized by high levels of EE, DP, and low PA. Younger, unmarried professionals with less experience, longer working hours, and night shifts were identified as particularly vulnerable. Our study also highlighted excessive workload, administrative burdens, and insufficient vacation time as key stressors. Additionally, a review of Asian studies revealed regional variations in burnout prevalence, underscoring the need for further research to address local risk factors and safeguard the well-being of healthcare professionals.
COVID pandemics and its impact on staff wellbeing
The COVID-19 pandemic has adversely impacted the wellbeing of the critical healthcare professionals. According to the recent systematic review, the prevalence of overall burnout of critical care staff ranged from 34.6–61.5% [12, 36] Exhausting workload, anxiety and fear of the pandemic, the burden of responsibility and moral distress were previously known possible issues of burnout during the pandemics [36, 52]. Despite the decrease in stress associated with caring for COVID patients during the post-pandemic era (Appendix Table 5), the overall prevalence of burnout didn’t decrease [44]. The pandemic itself was not necessarily the only reason associated with increased burnout [36, 53]. However, certain issues such as job overload, staff shortages, additional administrative tasks, shift work stress, and economic concerns continue to pose significant stress for critical healthcare practitioners [10, 12, 18, 54–57].
Prevalence of burnout before and after the COVID pandemics
We summarized the published studies on burnout among critical healthcare professionals in Asian (see Table 3). Before the pandemic, the burnout prevalence of burnout ranged from 16.0 to 80.0%, and it slightly increased to 24.3–82.1% after the pandemic [12, 54, 58–65]. MBI was the most used assessment instrument of burnout. Compared to the previous studies, the burnout prevalence in our study was 35.4% during the post-pandemic era. The substantial variability in the prevalence of burnout across studies was attributed not only to the difference in medical systems but to the marked variation in assessment instruments and definitions of burnout [10]. These variations preclude the cross-national comparisons regarding the trends in the prevalence of burnout before and after the COVID-19 pandemics. The importance of developing a consensus definition of burnout, standardizing assessment instruments and obtaining local data were emphasized.
Table 3.
Summary of published studies about burnout of critical healthcare professionals in Asian
| First author (Publication year) |
Country | Settings | Occupation | Sample size, n |
Burnout evaluation tool | Burnout Prevalence | Potential risk factors |
|---|---|---|---|---|---|---|---|
|
Our study (2024) |
Taiwan | ICU/ED | physicians, nurses | 254 | MBI a |
•Overall burnout: 35.4% EEb: low: 11.4%, average: 17.7%, high: 70.9% DPc: low: 16.1%, average: 27.6%, high: 56.3% PAd: low: 60.6%, average: 28.0%, high: 11.4% |
|
| Before the outbreak of COVID pandemics | |||||||
|
Yilmaz F et al. (2011) [14] |
Turkey | ICU | nurses | 85 | MBI | •Mean score: EE: 14.90 ± 5.53, DP: 3.87 ± 2.77, PA: 11.43 ± 4.63 | NA |
|
Yunbei Xiao et al. (2014) [101] |
China | ED | physicians | 205 | MBI | •Mean score: EE: 6.98 ± 5.79, Cynicism: 3.37 ± 4.35, PA: 24.79 ± 10.81 | NA |
| Xiao-Chun Zhang et al. (2015) [59] | China | ICU | nurses | 431 | MBI |
•High degree burnout rate: 16.0% •Mean score: EE: 24.55 ± 12.36, DP: 7.05 ± 6.50, PA: 35.08 ± 9.36 |
NA |
|
Yildiz Denat et al. (2016) [102] |
Turkey | ICU | nurses | 51 | MBI | •Mean score: EE: 14.68 ± 6.10, DP: 5.31 ± 3.84, PA: 19.19 ± 7.08 | NA |
| Motasem Hamdan et al. (2017) [24] | Palestine | ED | Nurses, physicians, and administrative personnel | 444 | MBI |
EE: low: 14.6%, average: 20.5%, high: 64.8% DP: low: 36.1%, average: 25.8%, high: 38.1% PA: low: 34.6%, average: 21.1%, high: 44.4% |
•workplace violence, young age ( ≤ 30 years) |
|
Wacharasint P et al. (2018) [54] |
Thailand | ICU | physicians, nurses | 171 | MBI | •Burnout rate: physicians: 65.2%; nurses: 62.6% |
•Physician: Income, thinking idea to quit their ICU job, need vacation > 2 days/week •Nurse: age > 40 years old, ICU experience > 5 years, patient’s ICU length of stay > 5 days, workload and thinking idea to quit their ICU job |
|
Kay Choong See et al. (2018) [12] |
Asia | ICU | physicians, nurses | 4092 | MBI |
•High degree burnout rate: 51.6% •Mean score: EE: 25.3 ± 11.2, DP: 8.9 ± 6.2, PA: 32.3 ± 9.0 |
•Lower risks: religiosity, years of working in the current department, shift work, better work-life balance and number of stay-home night calls •Higher risks: work days per month and having a bachelor’s degree |
|
Atefeh Soltanifar et al. (2018) [103] |
Iran | ED | female physicians | 77 | MBI |
EE Moderate to high: 84.5% DP Moderate to high:48.1% PA low: 80.5% |
NA |
| Abdulghani M Alqahtani et al. (2019) [60] | Saudi Arabia | ED | physicians, nurses | 282 | MBI | •Burnout rate: 16.3% | •Higher risks: male, Smokers and sleep disorders |
|
Saravanabavan L et al. (2019) [58] |
India | ICU | physicians, nurses | 204 | MBI | •High degree burnout rate: 80.0% | NA |
| After the outbreak of COVID pandemics | |||||||
|
Sedigheh Salimi et al. (2020) [104] |
Iran | ICU | nurses | 400 | ProQOL Scalee |
•Average burnout score:36.27 ± 7.45 •low: 8.0%, average: 49.8%, high: 42.3% |
NA |
|
Zakaria MI et al. (2021)61 |
Malaysia | ED | physicians, nurses, assistant medical officer | 216 | Burnout Questionnaire f | •Nurses:61.2%, doctors:35.1%, assistant medical officer: 29.6% | Frequent exposure to angry public, job overload, lack of clear guidelines, and perception of underpaid |
| Wei Ping Daniel Chor et al. (2021) [20] | Singapore | ED | physicians, nurses | 337 | CBI | •Average burnout score: 49.2 ± 18.6 | Previously working in the ED or UCC before the COVID-19 pandemic; nurse (compared to physicians) |
|
Zihan Hu MS et al. (2021) [62] |
China | ICU | physicians, nurses | 2411 | MBI |
•Burnout rate: 69.7% EE: low: 6.1%, average: 35.1%, high: 58.8% DP: low: 29.8%, average: 36.7%, high: 33.5% PA: low: 64.9%, average: 14.9%, high: 20.2% |
•Lower risks: exercise every day, more paid vacation •Higher risks: Having Comorbidities, more years of work experience and more night shifts |
|
Huan Ma et al. (2022) [63] |
China | ED | physicians, nurses | 342 | ProQOL Scale |
•Average burnout score:27.74 ± 6.19 •low: 19.3%, average: 78.4%, high: 2.3% |
NA |
|
Jing Wang et al. (2022) [64] |
China | ICU | physicians | 1813 | MBI |
•Burnout rate: 82.1% •Mean score: EE: 24.14 ± 10.90, DP: 9.69 ± 5.70, PA: 28.55 ± 9.82 |
Number of children, income, and difficulties in treatment decisions |
|
Artem Kashtanov et al. (2022) [67] |
Russia | ICU | physicians, nurses | 1259 | MBI |
•Non-COVID-19 ICU EE: low: 14.6%, average: 30.8%, high: 54.6% DP: low: 11.6%, average: 16.5%, high: 71.9% PA: low: 23.5%, average: 40.3%, high: 36.2% •COVID-19 ICU EE: low: 16.5%, average: 31.5%, high: 52.0% DP: low: 7.4%, average: 9.4%, high: 83.1% PA: low: 25.4%, average: 45.4%, high: 29.1% |
NA |
|
Kim C et al. (2022) [105] |
South Korea | ED | physicians | 247 | ProQOL Scale | •Average burnout score:33.81 ± 6.56 | NA |
|
Akira Kuriyama et al. (2022) [65] |
Japan | ICU | All critical care professionals | 936 | Mini Z 2.0 Survey | •Burnout rate: 24.3% |
•Lower risks: higher resilience scores and perceived support from the hospital or colleagues •Higher risks: having depression or anxiety, experiencing stigma from caring for patients with COVID-19, or having experienced self-quarantine |
|
Aylin Arıkan et al. (2023) [27] |
Turkey | PED | nurses | 164 | MBI |
EE: low: 9.1%, average: 40.5%, high: 51.4% DP: low: 14.4%, average: 26.7%, high: 58.9% PA: low: 89.6%, average: 10.4%, high: 0% |
NA |
a MBI: Maslach Burnout Inventory; b EE: Emotional Exhaustion; c DP: Depersonalization; d PA: Personal Accomplishment; e ProQOL Scale: The Professional Quality of Life Scale; f Burnout Questionnaire was adapted from Michelle Post, Public Welfare, Vol. 39, No. 1, 1981, American Public Welfare Association
Associated factors of burnout during the post-pandemic era
Although the causal relationship between burnout and risk factors may be limited by the cross-sectional design of studies, we can still take a glance at the vulnerable populations. The risk factors of burnout reported in previous study were summarized in Table 3. Consistent with earlier findings, we identified young age, unmarried status, longer working hours, less working experience and night shifts as potential risk factors for burnout [12, 14, 16, 20, 54, 61, 62, 65–67]. However, unlike other studies, we didn’t find a significant relationship between previous working experience, occupation and the degree of burnout [20, 54, 62].
Undoubtedly, being a critical care professional entails a high risk of burnout compared to other specialties due to the nature of the job [12, 68–70]. However, there remains conflicts concerning level of burnout between different occupation. Previous meta-analysis by MM Macaron et al. and multinational survey by See KC et al. revealed no significant difference in pooled estimate of burnout prevalence between physicians and nurses [11, 12]. On the contrary, critical care nurses were recognized as high-risk group by Gualano MR et al. and the multi-center study by Chor WP et al. also discovered slightly higher burnout rate among nurses compared with physicians working in ED (53.3% versus 42.5%) [20, 36]. These variation between studies may reflect the difference in organization-level healthcare systems. In Taiwan, the physician-to-population and nurse-to-population ratios are lower than in most Organization for Economic Cooperation and Development (OECD) countries, with 2.2 physicians and 7.9 nurses per 1,000 people, compared to the OECD averages of 3.6 and 9.6 per 1,000, respectively [71–73]. Moreover, the number of adult critical care beds leads among Asian countries, with 28.5 beds per 100,000 population, compared to the average of 3.6 beds per 100,000 population [74]. In our study, we found one-third of critical care professionals reported stress related to shift work, and over 70% of nurses experienced a workload burden (Fig. 2). Despite no significant difference in each subscale of burnout between physicians and nurses, nurses had higher prevalence of overall burnout compared to physicians (37.5% versus 26%), which may be associated with the critical care nurses were often working understaffed, having additional administrative tasks, and working overtime [36, 75].
Fig. 2.
The distribution of current work stressors
High EE and DP were observed in younger, less experienced individuals in our survey, consistent with previous studies [75–79]. Despite burnout often being a concern primarily for those in their later careers, this phenomenon may be related to the shortage of critical professionals. It is common for young nurses to be forced to handle excessive, unfamiliar clinical tasks before they are fully prepared and resilient [80–84]. Our data reflected that workload burden and staff shortages were reported as the top work stressors (Fig. 2). According to a survey by the Taiwan Ministry of Health and Welfare, one nurse in Taiwan cares for an average of 9 to 15 patients. Notably, younger individuals comprise most critical healthcare professionals in Taiwan. Therefore, it’s not surprising that the turnover rate for nurses is as high as 14.5% annually, with most nurses leaving within an average of 6.5 years, according to the Taiwan Ministry of Health and Welfare’s 2023 survey [85, 86].
Irregular night shifts and longer working hours were associated with higher scores in EE in our study. Night shift stress has been previously linked to burnout, mental health problems, and sleep disturbances [87, 88]. Furthermore, compared to those with fixed night shifts, participants with irregular night shifts had a higher risk of burnout [89]. Irregular shift schedules can compromise physical and psychological health as well as occupational functionality. Additionally, long working hours, especially working more than 55 h per week, were associated with greater sleep disturbances and occupational stress compared to working 40 h a week [90]. Implementing reasonable working hours and regular shift schedules may be effective interventions for preventing burnout and enhancing job performance.
Maintaining a work-life balance is crucial for well-being, and marriage appears to be one of the solutions [91, 92]. According to the theory of work-family enrichment, married individuals tend to experience better job satisfaction by actively engaging in their parental roles [93]. Recent studies conducted during the COVID-19 pandemic have highlighted the significant moderating role of family support in mitigating burnout across various dimensions and enhancing subjective well-being [94, 95]. Despite the potential stresses of parenthood, the protective effects of marriage can be attributed to lifestyle changes, involvement in parental responsibilities, and simply spending time with family [96]. Consistent with prior research, we found that married individuals exhibited lower EE and PA with higher DP compared to their unmarried counterparts [16]. Individuals with more children also exhibited lower EE and PA with higher DP, a phenomenon not observed in individuals with pets in our study.
The relationship between burnout interventions and locally identified workplace stressors and risk factors
Given the demographic variation in burnout, gathering local data, identifying vulnerable populations, and promoting interventions can help reduce the risk of burnout.
Based on our survey, several potential solutions to mitigate burnout have emerged. These include fostering a supportive work environment through mentorship programs, particularly for younger and less experienced staff, and ensuring open channels of communication for staff to voice their concerns. Reducing administrative burdens is essential, as is improving work schedules by limiting the number of consecutive and irregular night shifts, ensuring adequate rest periods between shifts, and offering flexible scheduling options and part-time positions [97–100]. Prioritizing the well-being of healthcare staff through these tailored interventions can establish a solid foundation for reducing burnout. Consequently, this approach may lead to improvements in the quality of care, reductions in medical expenditures, and lower turnover rates among healthcare professionals.
Conclusion
This multi-institutional study reveals a persistently high prevalence of burnout among critical healthcare professionals in Taiwan, even in the post-pandemic era. We identified several modifiable factors contributing to burnout, including age, marital status, work experience, working hours, and night shifts. Key stressors include heavy workloads, excessive administrative tasks, limited vacation time, and the demands of shift work. Our findings also highlight significant regional variations in burnout across Asia, emphasizing the need for locally tailored interventions. Continued research is crucial to monitor and support the well-being of critical care professionals, ultimately ensuring the maintenance and improvement of healthcare quality.
Strength and limitations
The study exhibits both strengths and potential limitations. Firstly, it authentically captures the psychological well-being of critical care healthcare professionals in Taiwan, despite variations in medical operation modes and disease severity among the included hospitals. However, the applicability of our findings to other countries should be approached with caution. Secondly, due to the lack of consensus definition of burnout, cautious should be taken if comparing our results to other studies, despite the widely accepted definition of burnout rate was used in our study. Thirdly, as a cross-sectional self-report questionnaire survey, drawing causal inferences from the research results requires careful consideration, and the presence of social desirability bias may introduce self-reporting bias. Fourth, when designing our questionnaire, we removed gender-related questions to avoid gender issues, potential gender bias, and to protect participant privacy. Consequently, we were unable to gather data on gender-specific differences in vulnerability to burnout. Lastly, participants in this study are voluntary, lacking compulsion, which may lead to a relatively low questionnaire response rate. However, their willingness to participate ensures more sincere responses, thereby enhancing the accuracy of the questionnaire. Moreover, by not mandating participation, the study avoids imposing additional psychological stress on critical healthcare professionals of selected hospitals.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Abbreviations
- SHS
The Subjective Happiness Scale
- MBI-MP
The Maslach Burnout Inventory Human Services Survey for Medical Personnel
- EE
Emotional exhaustion
- DP
Depersonalization
- PA
Personal accomplishment
Author contributions
YLL, CHW: study design; XWL and CHW: develop research strategy and perform systematic reviews; MYC and PTC: evaluating the questionnaire’s adequacy and data extraction; CHW: verified the extracted data; YLL and YCL: performed the statistical analysis; YLL, MYC, JWD and CHW: drift the manuscript; CHW: revised the manuscript; All authors read and approved the final manuscript.
Funding
None.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This research received approval from the Jen-Ai Hospital Institutional Review Board (IRB Number: 202300085B0). All participants fully understood the study’s goal and reviewed the informed consent form before proceeding.
Consent for publication
not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. [DOI] [PubMed] [Google Scholar]
- 2.Tanno LK, Chalmers RJ, Calderon MA, et al. Reaching multidisciplinary consensus on classification of anaphylaxis for the eleventh revision of the World Health Organization’s (WHO) International Classification of Diseases (ICD-11). Orphanet J Rare Dis. 2017;12:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maslach C, Jackson SE. The measurement of experienced burnout. J Organizational Behav. 1981;2:99–113. [Google Scholar]
- 4.Edú-Valsania S, Laguía A, Moriano JA, Burnout. A Review of Theory and Measurement. Int J Environ Res Public Health 2022;19. [DOI] [PMC free article] [PubMed]
- 5.Salvagioni DAJ, Melanda FN, Mesas AE, et al. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE. 2017;12:e0185781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15:103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han S, Shanafelt TD, Sinsky CA, et al. Estimating the Attributable Cost of Physician Burnout in the United States. Ann Intern Med. 2019;170:784–90. [DOI] [PubMed] [Google Scholar]
- 8.Grow HM, McPhillips HA, Batra M. Understanding physician burnout. Curr Probl Pediatr Adolesc Health Care. 2019;49:100656. [DOI] [PubMed] [Google Scholar]
- 9.Cecere L, de Novellis S, Gravante A, et al. Quality of life of critical care nurses and impact on anxiety, depression, stress, burnout and sleep quality: A cross-sectional study. Intensive Crit Care Nurs. 2023;79:103494. [DOI] [PubMed] [Google Scholar]
- 10.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018;320:1131–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macaron MM, Segun-Omosehin OA, Matar RH, et al. A systematic review and meta analysis on burnout in physicians during the COVID-19 pandemic: A hidden healthcare crisis. Front Psychiatry. 2022;13:1071397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.See KC, Zhao MY, Nakataki E, et al. Professional burnout among physicians and nurses in Asian intensive care units: a multinational survey. Intensive Care Med. 2018;44:2079–90. [DOI] [PubMed] [Google Scholar]
- 13.Shah MK, Gandrakota N, Cimiotti JP, et al. Prevalence of and Factors Associated With Nurse Burnout in the US. JAMA Netw Open. 2021;4:e2036469–2036469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yilmaz F, Aytekin A, Kuguoglu S. The burnout levels of NICU nurses and its effect on their quality of life in north of Turkey. Intensive Care Med. 2011;37:S439. [Google Scholar]
- 15.Abdul Aziz AF, Ong T. Prevalence and associated factors of burnout among working adults in Southeast Asia: results from a public health assessment. Front Public Health. 2024;12:1326227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramírez-Elvira S, Romero-Béjar JL, Suleiman-Martos N et al. Prevalence, Risk Factors and Burnout Levels in Intensive Care Unit Nurses: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health 2021;18. [DOI] [PMC free article] [PubMed]
- 17.Hart D, Paetow G, Zarzar R. Does Implementation of a Corporate Wellness Initiative Improve Burnout? West J Emerg Med. 2019;20:138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85. [DOI] [PubMed] [Google Scholar]
- 19.Arora M, Asha S, Chinnappa J, et al. Review article: burnout in emergency medicine physicians. Emerg Med Australas. 2013;25:491–5. [DOI] [PubMed] [Google Scholar]
- 20.Chor WPD, Ng WM, Cheng L, et al. Burnout amongst emergency healthcare workers during the COVID-19 pandemic: A multi-center study. Am J Emerg Med. 2021;46:700–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Somville F, Van Bogaert P, Wellens B et al. Work stress and burnout among emergency physicians: a systematic review of last 10 years of research. Acta Clin Belg 2023:1–10. [DOI] [PubMed]
- 22.Naidoo R, Schoeman R. Burnout in emergency department staff: The prevalence and barriers to intervention. S Afr J Psychiatr. 2023;29:2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costa DK, Moss M. The Cost of Caring: Emotion, Burnout, and Psychological Distress in Critical Care Clinicians. Ann Am Thorac Soc. 2018;15:787–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamdan M, Hamra AA. Burnout among workers in emergency Departments in Palestinian hospitals: prevalence and associated factors. BMC Health Serv Res. 2017;17:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall LH, Johnson J, Watt I, et al. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE. 2016;11:e0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ge MW, Hu FH, Jia YJ, et al. Global prevalence of nursing burnout syndrome and temporal trends for the last 10 years: A meta-analysis of 94 studies covering over 30 countries. J Clin Nurs. 2023;32:5836–54. [DOI] [PubMed] [Google Scholar]
- 27.Arıkan A, Esenay FI. Compassion fatigue and burnout in Turkish pediatric emergency nurses during the COVID-19 pandemic. J Pediatr Nurs. 2023;71:120–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dixon E, Murphy M, Wynne R. A multidisciplinary, cross-sectional survey of burnout and wellbeing in emergency department staff during COVID-19. Australas Emerg Care. 2022;25:247–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lasalvia A, Amaddeo F, Porru S, et al. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11:e045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chu WM, Ho HE, Lin YL, et al. Risk Factors Surrounding an Increase in Burnout and Depression Among Health Care Professionals in Taiwan During the COVID-19 Pandemic. J Am Med Dir Assoc. 2023;24:164–e1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin YY, Pan YA, Hsieh YL et al. COVID-19 Pandemic Is Associated with an Adverse Impact on Burnout and Mood Disorder in Healthcare Professionals. Int J Environ Res Public Health 2021;18. [DOI] [PMC free article] [PubMed]
- 32.Shiu C, Chen WT, Hung CC, et al. COVID-19 stigma associates with burnout among healthcare providers: Evidence from Taiwanese physicians and nurses. J Formos Med Assoc. 2022;121:1384–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alanazy ARM, Alruwaili A. The Global Prevalence and Associated Factors of Burnout among Emergency Department Healthcare Workers and the Impact of the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Healthc (Basel) 2023;11. [DOI] [PMC free article] [PubMed]
- 34.Rizzo A, Yıldırım M, Öztekin GG, et al. Nurse burnout before and during the COVID-19 pandemic: a systematic comparative review. Front Public Health. 2023;11:1225431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bradley M, Chahar P. Burnout of healthcare providers during COVID-19. Cleve Clin J Med 2020. [DOI] [PubMed]
- 36.Gualano MR, Sinigaglia T, Lo Moro G et al. The Burden of Burnout among Healthcare Professionals of Intensive Care Units and Emergency Departments during the COVID-19 Pandemic: A Systematic Review. Int J Environ Res Public Health 2021;18. [DOI] [PMC free article] [PubMed]
- 37.Sharma R, Saxena A, Magoon R, et al. A cross-sectional analysis of prevalence and factors related to depression, anxiety, and stress in health care workers amidst the COVID-19 pandemic. Indian J Anaesth. 2020;64:S242–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fumis RRL, Costa ELV, Dal’Col SVC, et al. Burnout syndrome in intensive care physicians in time of the COVID-19: a cross-sectional study. BMJ Open. 2022;12:e057272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wahlster S, Sharma M, Lewis AK, et al. The Coronavirus Disease 2019 Pandemic’s Effect on Critical Care Resources and Health-Care Providers: A Global Survey. Chest. 2021;159:619–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Azoulay E, Cariou A, Bruneel F, et al. Symptoms of Anxiety, Depression, and Peritraumatic Dissociation in Critical Care Clinicians Managing Patients with COVID-19. A Cross-Sectional Study. Am J Respir Crit Care Med. 2020;202:1388–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gomez S, Anderson BJ, Yu H, et al. Benchmarking Critical Care Well-Being: Before and After the Coronavirus Disease 2019 Pandemic. Crit Care Explor. 2020;2:e0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burrowes SAB, Casey SM, Pierre-Joseph N, et al. COVID-19 pandemic impacts on mental health, burnout, and longevity in the workplace among healthcare workers: A mixed methods study. J Interprof Educ Pract. 2023;32:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Valdes-Elizondo GD, Álvarez-Maldonado P, Ocampo-Ocampo MA, et al. Burnout symptoms among physicians and nurses before, during and after COVID-19 care. Rev Lat Am Enfermagem. 2023;31:e4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Petrino R, Riesgo LG, Yilmaz B. Burnout in emergency medicine professionals after 2 years of the COVID-19 pandemic: a threat to the healthcare system? Eur J Emerg Med. 2022;29:279–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Muschitiello V, Milani M, Marseglia C, et al. Burnout symptoms, work motivation and their relationships among Italian ICU’s nurses after COVID-19 emergency. A multicenter study. Ann Ig. 2024;36:99–114. [DOI] [PubMed] [Google Scholar]
- 46.Gabra MA, Mohammed KAE, Hegazy MN, et al. Post-traumatic stress disorder symptoms among nursing staff who provided direct care to COVID-19 patients: a cross-sectional study. Middle East Curr Psychiatry. 2022;29:67. [Google Scholar]
- 47.Jazieh AR, Kozlakidis Z. Healthcare Transformation in the Post-Coronavirus Pandemic Era. Front Med 2020;7. [DOI] [PMC free article] [PubMed]
- 48.Giusti EM, Veronesi G, Callegari C, et al. Pre-pandemic burnout and its changes during the COVID-19 outbreak as predictors of mental health of healthcare workers: A lesson to be learned. Psychiatry Res. 2023;326:115305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maslach C, Jackson S, Leiter M. The Maslach Burnout Inventory Manual. Volume 3, 1997:191–218.
- 50.Doulougeri K, Georganta K, Montgomery A. Diagnosing burnout among healthcare professionals: Can we find consensus? Cogent Med. 2016;3:1. [Google Scholar]
- 51.Lyubomirsky S, Lepper HS. A Measure of Subjective Happiness: Preliminary Reliability and Construct Validation. Soc Indic Res. 1999;46:137–55. [Google Scholar]
- 52.Elliott R, Crowe L, Pollock W, et al. The impact of the COVID-19 pandemic on critical care healthcare professionals’ work practices and wellbeing: A qualitative study. Aust Crit Care. 2023;36:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Amanullah S, Ramesh Shankar R. The Impact of COVID-19 on Physician Burnout Globally: A Review. Healthc (Basel) 2020;8. [DOI] [PMC free article] [PubMed]
- 54.Wacharasint P, Laopakorn C, Kunakorn P. Prevalence and risk factors for ICU burnout syndrome among Thai intensivists and ICU nurses. Intensive Care Med Experimental 2018;6.
- 55.Dall’Ora C, Ejebu OZ, Ball J, et al. Shift work characteristics and burnout among nurses: cross-sectional survey. Occup Med (Lond). 2023;73:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Galanis P, Moisoglou I, Katsiroumpa A, et al. Increased Job Burnout and Reduced Job Satisfaction for Nurses Compared to Other Healthcare Workers after the COVID-19 Pandemic. Nurs Rep. 2023;13:1090–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alibudbud R. Addressing the Burnout and Shortage of Nurses in the Philippines. SAGE Open Nurs. 2023;9:23779608231195737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saravanabavan L, Sivakumar MN, Hisham M. Stress and burnout among intensive care unit healthcare professionals in an Indian tertiary care hospital. Indian J Crit Care Med. 2019;23:462–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang XC, Huang DS, Guan P. Job burnout among critical care nurses from 14 adult intensive care units in Northeastern China: a cross-sectional survey. BMJ Open. 2014;4:e004813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alqahtani AM, Awadalla NJ, Alsaleem SA, et al. Burnout Syndrome among Emergency Physicians and Nurses in Abha and Khamis Mushait Cities, Aseer Region. Southwest Saudi Arabia ScientificWorldJournal. 2019;2019:4515972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zakaria MI, Remeli R, Ahmad Shahamir MF, et al. Assessment of burnout among emergency medicine healthcare workers in a teaching hospital in Malaysia during COVID-19 pandemic. Hong Kong J Emerg Med. 2021;28:254–9. [Google Scholar]
- 62.Hu Z, Wang H, Xie J, et al. Burnout in ICU doctors and nurses in mainland China-A national cross-sectional study. J Crit Care. 2021;62:265–70. [DOI] [PubMed] [Google Scholar]
- 63.Ma H, Huang SQ, We B, et al. Compassion fatigue, burnout, compassion satisfaction and depression among emergency department physicians and nurses: a cross-sectional study. BMJ Open. 2022;12:e055941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang J, Hu B, Peng Z, et al. Prevalence of burnout among intensivists in mainland China: a nationwide cross-sectional survey. Crit Care. 2021;25:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kuriyama A, Sakuraya M, Kinjo M, et al. Burnout and Turnover Intention in Critical Care Professionals During the COVID-19 Pandemic in Japan: A Cross-sectional Survey. Ann Am Thorac Soc. 2023;20:262–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bes I, Shoman Y, Al-Gobari M, et al. Organizational interventions and occupational burnout: a meta-analysis with focus on exhaustion. Int Arch Occup Environ Health. 2023;96:1211–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kashtanov A, Molotok E, Yavorovskiy A et al. A Comparative Cross-Sectional Study Assessing the Psycho-Emotional State of Intensive Care Units’ Physicians and Nurses of COVID-19 Hospitals of a Russian Metropolis. Int J Environ Res Public Health 2022;19. [DOI] [PMC free article] [PubMed]
- 68.Somville F, Van Bogaert P, Wellens B, et al. Work stress and burnout among emergency physicians: a systematic review of last 10 years of research. Acta Clin Belg. 2024;79:52–61. [DOI] [PubMed] [Google Scholar]
- 69.Duarte I, Teixeira A, Castro L, et al. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health. 2020;20:1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jun J, Costa DK. Is It Me or You? A Team Approach to Mitigate Burnout in Critical Care. Crit Care Nurs Clin North Am. 2020;32:395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Phua J, Kulkarni AP, Mizota T, et al. Critical care bed capacity in Asian countries and regions before and during the COVID-19 pandemic: an observational study. Lancet Reg Health West Pac. 2024;44:100982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cho DD, Bretthauer KM, Schoenfelder J. Patient-to-nurse ratios: Balancing quality, nurse turnover, and cost. Health Care Manag Sci. 2023;26:807–26. [DOI] [PubMed] [Google Scholar]
- 73.OECD. Health at a Glance 2023, 2023.
- 74.Phua J, Faruq MO, Kulkarni AP, et al. Critical Care Bed Capacity in Asian Countries and Regions. Crit Care Med. 2020;48:654–62. [DOI] [PubMed] [Google Scholar]
- 75.Chuang CH, Tseng PC, Lin CY, et al. Burnout in the intensive care unit professionals: A systematic review. Med (Baltim). 2016;95:e5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bogue TL, Bogue RL. Extinguish Burnout in Critical Care Nursing. Crit Care Nurs Clin North Am. 2020;32:451–63. [DOI] [PubMed] [Google Scholar]
- 77.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513–9. [DOI] [PubMed] [Google Scholar]
- 78.Kim HS, Yeom HA. The association between spiritual well-being and burnout in intensive care unit nurses: A descriptive study. Intensive Crit Care Nurs. 2018;46:92–7. [DOI] [PubMed] [Google Scholar]
- 79.Moya-Salazar J, Buitrón LA, Goicochea EA, et al. The Age of Young Nurses Is a Predictor of Burnout Syndrome during the Care of Patients with COVID-19. Nurs Rep. 2023;13:721–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mealer M, Jones J, Newman J, et al. The presence of resilience is associated with a healthier psychological profile in intensive care unit (ICU) nurses: results of a national survey. Int J Nurs Stud. 2012;49:292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shapiro D, Duquette CE, Zangerle C, et al. The Seniority Swoop: Young Nurse Burnout, Violence, and Turnover Intention in an 11-Hospital Sample. Nurs Adm Q. 2022;46:60–71. [DOI] [PubMed] [Google Scholar]
- 82.Huang Z-p, Huang F, Liang Q, et al. Socioeconomic factors, perceived stress, and social support effect on neonatal nurse burnout in China: a cross-sectional study. BMC Nurs. 2023;22:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yu F, Raphael D, Mackay L, et al. Personal and work-related factors associated with nurse resilience: A systematic review. Int J Nurs Stud. 2019;93:129–40. [DOI] [PubMed] [Google Scholar]
- 84.Galanis P, Vraka I, Fragkou D, et al. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. 2021;77:3286–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ren H, Li P, Xue Y et al. Global Prevalence of Nurse Turnover Rates: A Meta-Analysis of 21 Studies from 14 Countries. Journal of Nursing Management. 2024;2024.
- 86.2023 Taiwan Health and Welfare Report.
- 87.Cheng H, Liu G, Yang J, et al. Shift work disorder, mental health and burnout among nurses: A cross-sectional study. Nurs Open. 2023;10:2611–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Al-hrinat J, Al-Ansi AM, Hendi A, et al. The impact of night shift stress and sleep disturbance on nurses quality of life: case in Palestine Red Crescent and Al-Ahli Hospital. BMC Nurs. 2024;23:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gu H, Lee J, Hwang Y et al. Job burnout among workers with different shift regularity: interactive factors between sleep, depression, and work environment. Front Public Health 2023;11. [DOI] [PMC free article] [PubMed]
- 90.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32:737–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yang D, Fang G, Fu D, et al. Impact of work-family support on job burnout among primary health workers and the mediating role of career identity: A cross-sectional study. Front Public Health. 2023;11:1115792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.la Cañadas-De GA, Ortega E, Ramirez-Baena L et al. Gender, Marital Status, and Children as Risk Factors for Burnout in Nurses: A Meta-Analytic Study. Int J Environ Res Public Health 2018;15. [DOI] [PMC free article] [PubMed]
- 93.Greenhaus J, Powell G. When Work And Family Are Allies: A Theory Of Work-Family Enrichment. Acad Manage Rev. 2006;31:72–92. [Google Scholar]
- 94.Karagöl A, Törenli Kaya Z. Healthcare workers’ burn-out, hopelessness, fear of COVID-19 and perceived social support levels. Eur J Psychiatry. 2022;36:200–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shin Y, Hur WM, Park K. The Power of Family Support: The Long-Term Effect of Pre-COVID-19 Family Support on Mid-COVID-19 Work Outcomes. Int J Environ Res Public Health 2021;18. [DOI] [PMC free article] [PubMed]
- 96.Chen Y-H, Lou S-Z, Yang C-w, et al. Effect of Marriage on Burnout among Healthcare Workers during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19:15811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Collett G, Korszun A, Gupta A. Potential strategies for supporting mental health and mitigating the risk of burnout among healthcare professionals: insights from the COVID-19 pandemic. EClinicalMedicine 2024;71. [DOI] [PMC free article] [PubMed]
- 98.Reshetnikov A, Abaeva O, Prisyazhnaya N et al. The Impact of the COVID-19 Pandemic on Burnout Levels among Healthcare Workers: A Comparative Analysis of the Pandemic Period and Post-Pandemic Period. Heliyon. 2024:e36769. [DOI] [PMC free article] [PubMed]
- 99.Rossi MF, Gualano MR, Magnavita N, et al. Coping with burnout and the impact of the COVID-19 pandemic on workers’ mental health: A systematic review. Front Psychiatry. 2023;14:1139260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.De Kock JH, Latham HA, Leslie SJ, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Xiao Y, Wang J, Chen S, et al. Psychological distress, burnout level and job satisfaction in emergency medicine: A cross-sectional study of physicians in China. Emerg Med Australas. 2014;26:538–42. [DOI] [PubMed] [Google Scholar]
- 102.Denat Y, Gokce S, Gungor H, et al. Relationship of anxiety and burnout with extrasystoles in critical care nurses in Turkey. Pak J Med Sci. 2016;32:196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Soltanifar A, Pishbin E, Attaran Mashhadi N, et al. Burnout among female emergency medicine physicians: A nationwide study. Emerg Med Australas. 2018;30:517–22. [DOI] [PubMed] [Google Scholar]
- 104.Salimi S, Pakpour V, Rahmani A, et al. Compassion Satisfaction, Burnout, and Secondary Traumatic Stress Among Critical Care Nurses in Iran. J Transcult Nurs. 2020;31:59–66. [DOI] [PubMed] [Google Scholar]
- 105.Kim C, Park KH, Eo EK, et al. Burnout and Resilience among Emergency Physicians at Korean University Hospitals during the COVID-19 Pandemic: A Cross-Sectional Analysis. Yonsei Med J. 2022;63:372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.