Abstract
This study aims to evaluate the feasibility, safety, and effectiveness of an optimized treatment approach for complex renal calculi, utilizing visual needle nephroscopy in conjunction with standard PCNL and holmium YAG laser. We collected data from 62 patients diagnosed with complex kidney stones who underwent this combined procedure using the visual needle nephroscope (Needle-perc®, Youcare Tech, Wuhan, China). The percutaneous nephroscopic working channel was established by visual needle nephroscope, and the primary channel was expanded to 20 F to treat most of the main body of the calculi with a 550 μm holmium laser fiber. Visual needle nephroscope was used to locate the renal calyx where the residual calculi were located for precise puncture as a secondary channel, and the residual stones were treated by a 200 μm holmium laser fiber. Clinical data were collected, and intraoperative variables, postoperative complications and outcomes were assessed. All 62 patients successfully completed the operation without severe complications. The S.T.O.N.E. score of 62 patients before operation was 10.5 ± 0.9 points and above, of which the N score was more than 2 points. The average operation time was (65.5 ± 12.7) minutes, and the average hospital stay was (7.3 ± 2.1) days. After operation, 2 patients developed a fever, which improved after symptomatic treatment by intravenous antibiotics. 4 patients had clinically significant residual fragments, and the stone-free rate of primary operation was 93.5% (58/62). The optimized operation for the treatment of complex renal calculi based on standard PCNL combined with visual needle nephroscope by holmium YAG laser has good feasibility, safety and effectiveness.
Keywords: Percutaneous nephrolithotomy, Visual needle nephroscope, Complex renal calculi, Stone free rate, Complication, Holmium YAG laser
Introduction
Urolithiasis represents a prevalent condition within the field of urology. Common surgical interventions employed in the management of urolithiasis include percutaneous nephrolithotripsy (PCNL), flexible ureteroscopic lithotripsy (FURSL), and extracorporeal shock wave lithotripsy (ESWL), among other modalities. Treatment of complex stones which scored 9–13 points according to the S.T.O.N.E. scoring system [1] is difficult in the clinic, and percutaneous nephrolithotripsy is still the main choice. However, single modality treatment is often not effective, which manifests as a low stone-free rate for the single channel or one-stage surgical lithotripsy, and multi-channels, multiple stages of treatment are often needed, while complications are correspondingly increased [2].
The visualization puncture technique has gained wider adoption in percutaneous nephrolithotripsy (PCNL) in recent years. This technique allows for visual guidance during the puncture process, enabling more precise positioning and potentially reducing the risk of puncture-related complications in PCNL procedures. The visualization puncture technique has gained wider adoption in percutaneous nephrolithotripsy (PCNL) in recent years. This technique allows for visual guidance during the puncture process, enabling more precise positioning and potentially reducing the risk of puncture-related complications in PCNL procedures. Building on the visualization puncture concept, a novel endoscopic technique called “Needle-perc” has also been gradually applied in the treatment of kidney stones [3]. The Needle-perc system, derived from the visualization puncture approach, was described by Xiao et al. in a 2020 publication in the Chinese Medical Journal [3]. This new instrument and its initial clinical application represent an advancement in minimally invasive endoscopic approaches for managing urolithiasis.
Additionally, the microperc technique using a polydiagnost system is another example of a visualization-guided percutaneous nephrolithotripsy approach that has emerged in recent years [3].
Because of the performance and characteristics of visual needle nephroscope, it is currently mainly used for the treatment of single calyceal stones smaller than 2 cm. However, its lithotripsy efficiency and therapeutic effect for larger complex kidney stones still cannot be the same level as that of conventional percutaneous nephroscopy [4]. We summarize the past years of experience in the treatment of complex kidney stones and try to utilize visual needle nephroscope in combination with traditional percutaneous nephroscopy for the optimization of complex kidney stone treatment options, with the hope of improving the treatment outcomes of complex kidney stone in one-stage surgery, while reducing surgical trauma and the risk of surgery.
Materials and methods
Patients’ inclusion
We retrospectively evaluated patients with unilateral complex kidney stones who underwent PCNL between January and December 2022. This study was approved by the ethics committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, and the observational study were followed by the STROBE guidelines. Patients with complex kidney stones (based on specificities defining a complex kidney stone: stone size, stone density, stone location or anatomical abnormalities) were selected, and the inclusion and exclusion criteria were as follows.
Inclusion criteria
(1) Age between 20 and 70 years.
(2) The patients were diagnosed with unilateral complex kidney stones by kidney, ureter, and bladder (KUB) X-ray, and non-contrast computed tomography (NCCT), which showed clinical features of multiple calyces and multiple stones with a total stone burden of more than 25 mm.
(3) S.T.O.N.E. scores were all 9 and above (where N score was 2 or more, i.e. multiple calyceal involvement or staghorn calculi).
(4) The patients can tolerate percutaneous nephrolithotripsy and completed surgery.
(5) Follow up with postoperative review can be completed.
Exclusion criteria
(1) Patients with bilateral kidney stones.
(2) Isolated kidney or renal insufficiency (serum creatinine > 177 µmol/L);
(3) Renal malrotation, horseshoe kidney, or abnormal intrarenal anatomy.
(4) Excessive adiposity, body mass index (BMI) ≥ 35.
(5) Severe scoliosis or left kidney stone with splenomegaly.
(6) Uncorrected coagulation disorder.
(7) Uncorrected severe cardiopulmonary dysfunction.
(8) Urinary tract infections that are not effectively treated.
Preoperative preparation
All patients were examined with KUB X-ray and NCCT of the urinary system before treatment to understand the stone size, location, degree of hydronephrosis, and exclude renal malformations. Urine routine and urine culture were performed to assess urinary infection. Biochemical routine examination was performed to evaluate renal function. Complete blood routine, coagulation function, electrocardiogram and other examinations to exclude surgical contraindications. Antibiotics were administered prophylactically 30–60 min before surgery.
Surgical technique
Following the successful administration of general anesthesia, the patient was positioned in the prone position after the ureteral catheter was inserted. In combined with the preoperative imaging data, the renal cortex and medulla, upper and lower pole of the kidney, stones, hydronephrotic calyces and perinephric viscera were examined by ultrasound. To establish the percutaneous nephroscopy working channel using a visual needle nephroscope (“Needle-perc”, Youcare@, Wuhan, China, Fig. 1), we tried to select the middle and upper calyces of the postrenal group, and we performed a vertical puncture of the highest point of the dome of the target calyces through 11 intercostal or 12 subcostal under ultrasound real-time guidance. Nephrostomy tract dilatation was completed by peel-away sheath of 20 F and the nephroscope was entered into the percutaneous renal channel. The stone was fragmented with the power set at 30–60 W (2.0–3.0 J / 15–20 Hz) by a 550 μm holmium laser fiber, Throughout the procedure, we employed continuous irrigation and real-time monitoring of both laser power and tissue temperature to ensure patient safety and minimize the risk of thermal injury during the lithotripsy. After treating most of the main body of the stone by percutaneous nephroscopy, the residue of the calyceal stone was examined by B-ultrasound, and precision puncture was performed by using the “Needle-perc” to locate the calyces where the residual stone was located, as a secondary channel, without dilation of the channel. A 200 μm holmium laser fiber, with the power set at 12–20 W (0.8–1.0 J / 15–20 Hz) was used to deal with residual stones, in which larger stone fragments can be moved to the vicinity of main 20 Fr channel with the help of endoscopy and fluid and removed from it. A 6 F ureteral stent tube, main access nephrostomy tube, and balloon urinary catheter were routinely retained after surgery.
Fig. 1.

Structural diagram of the visualization needle nephroscope (“Needle-perc”). The length of the nephroscope body is 152 mm and the outer diameter is only 4.2 F, which is almost equivalent to that of a common puncture needle, and it has a perfusion channel, an endoscope channel and a working channel
Postoperative review
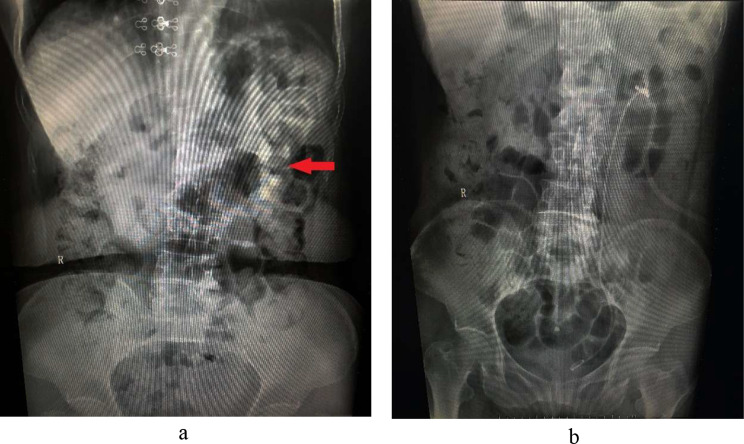
All patients had the urinary catheter and nephrostomy tube removed 3–4 days after surgery and the ureteral stent tube removed 2–3 weeks after surgery. The postoperative antibiotic was given for 24–48 h. All patients underwent postoperative KUB X-ray and NCCT to assess whether there were any residual stones 2–3 days after surgery. While KUB X-ray serves as a standard initial assessment tool due to its accessibility and speed presented in Fig. 2, we recognize that NCCT is the gold standard for accurately detecting residual stones, given its superior sensitivity and specificity.
Fig. 2.
Comparison of preoperative and postoperative KUB imaging results of a typical case treated by standard PCNL combined with visual needle nephroscope. (a) The red arrow shows the kidney stones before surgery. (b) Postoperative KUB 2 days after surgery
A review at 30 days to assess stone clearance as a follow-up was received by the patients. To ensure a comprehensive evaluation of the stone-free rate (SFR), we interpreted the results from both imaging modalities. KUB X-ray results were used for preliminary assessment, while NCCT findings were prioritized for confirmation of any residual stone burden. Clinically significant residual stones were identified with a diameter of ≥ 4 mm. The operation time, the proportion of complications, the stone-free rate of one-stage operation were recorded (presented in Fig. 3). Complications were classified according to the Clavien grading system [5]. Data were reported as numbers, percentages, and mean ± standard deviation (SD).
Fig. 3.
Establishment the main working channel by “Needle-perc” under ultrasound real-time guidance
Results
73 patients were included initially, and 11 patients were excluded by the exclusion criteria. All 62 patients successfully completed the operation without severe complications such as hemorrhagic shock, urogenic sepsis and death. The demographics of the patients included for final analysis such as age, gender, BMI were showed in the Table 1. The S.T.O.N.E. score of 62 patients before operation was 9 points and above (the average was 10.5 points, of which the N score was more than 2 points, that is, multiple renal calyces were involved or staghorn stones), and the mean stone size was 4.7 cm.
Table 1.
Demographics and stone characteristics of the patients that underwent standard PCNL combined with “Needle-perc”
| Parameters | No.(%) | Mean ± SD (range) |
|---|---|---|
| Patients | 62(100) | |
| Laterality (left/right) | 40(64.5)/22(35.5) | |
| Gender (male/female) | 36(58.1)/26(41.9) | |
| Age (year) | 43.1 ± 8.9(33–60) | |
| BMI (kg/m2) | 26.3 ± 2.7(22–32) | |
| S.T.O.N.E. scores | 10.5 ± 0.9(9–12) | |
| Stone size (mm2) | 1205.7 ± 51.1(800–2000) | |
| Tract length (mm) | 101.1 ± 8.2(80–120) | |
| Obstruction | ||
| No | 36(58.1%) | |
| Yes | 26(41.9%) | |
| Number of involved calices | 3.2 ± 1.2(2–5) | |
| Essence stone density (HU) | 862.2 ± 101.5(700–1400) | |
| Staghorn stone | 32(51.6%) | |
| Complete | 14(22.6%) | |
| Partial | 18(29.0%) |
The perioperative and postoperative data such as average operation time, average hospital stay was shown in the Table 2. After operation, 2 patients (3.2%) developed a fever (> 38.5℃, Clavien grade II), which improved after symptomatic treatment by intravenous antibiotics. 4 patients had clinically significant residual fragments (≥ 4 mm), and the stone-free rate of primary operation was 93.5%.
Table 2.
Perioperative and postoperative data about standard PCNL combined with “Needle-perc”
| Parameters | No.(%) | Mean ± SD (range) |
|---|---|---|
| Operative time (min) | 65.5 ± 12.7(40–100) | |
| Postoperative hospital time (d) | 7.3 ± 2.1(5–10) | |
| SFR 30 days after surgery | 58(93.5%) | |
| Complications (Clavien grade I + II) | 2(3.2) | |
| Fever(> 38.5℃) | 2(3.2) |
Discussion
Complex nephrolithiasis refers to stones greater than 2.5 cm in diameter, staghorn calculi, or multiple calculi, including those in kidneys with anatomical or functional abnormalities that complicate treatment [6]. Okhunov et al. first proposed the S.T.O.N.E. scoring system to estimate the postoperative stone-free rate for patients undergoing PCNL, with scores of 9–13 indicating high complexity [1]. The complexity of stone size and distribution significantly influences the choice of surgical options [7]. Managing complex kidney stones is challenging, and percutaneous nephrolithotripsy (PCNL) remains the preferred treatment. However, the surgical efficacy of PCNL is impacted by stone size and distribution, with single-tract PCNL achieving stone-free rates of 40-70% for simpler cases [8]. For patients with S.T.O.N.E. scores of 9–13, the stone-free rate after one-stage PCNL is approximately 50% [9]. Multiple calyces and stones can complicate clearance, particularly in single-tract PCNL, due to the endoscopic field’s limitations and the angles of the calyceal neck [10]. While some studies suggest that establishing multiple tracts may enhance stone-free rates, this approach often leads to increased surgical complications and trauma [11]. Recent advancements in visualization puncture techniques have improved the safety and efficacy of PCNL. This includes the use of the visual needle nephroscope (“Needle-perc”), which facilitates real-time monitoring of the puncture process, enhancing precision and potentially reducing associated risks [12]. The “Needle-perc” combines the functions of a nephroscope and puncture needle, allowing for direct visualization during percutaneous renal punctures, which can minimize trauma and improve outcomes [3]. Through the built-in fiberoptic endoscope, the percutaneous renal puncture process can be visualized throughout, while using B-ultrasound-guided, the puncture process can be monitored by a monitor, and if a bleeding tendency is recognized, the puncture can be stopped immediately and further aggravation of bleeding can be avoided [13]. Whereas when the puncture enters the intrarenal collecting system, it can increase the precision of puncture by visually monitoring before dilating the puncture channel, and determine whether the puncture position is ideal, avoids blind dilation [14]. When used as a nephroscope, after visual puncture into the target calyces, through its built-in working channel, 200 μm holmium laser can be directly utilized for lithotripsy, which eliminates the need to dilate the puncture channel, thereby greatly reducing surgical trauma and reducing surgical risk [15].
“Needle-perc” is mainly used for the treatment of single calyceal stones smaller than 2 cm. But for larger complex renal stones, its lithotripsy efficiency and therapeutic effect are still inferior to standard PCNL [4]. This study utilizes “Needle-perc” in combination with traditional PCNL to optimize treatment options for complex kidney stones. The visualization needle nephroscope was used to select suitable targets for visualizing percutaneous renal puncture, and was expanded to 18–20 F as the main working channel, which was responsible for dealing with most of the stones or stone main bodies, followed by intraoperative ultrasound examination of the residual stone conditions, using the “Needle-perc” to locate the calyces where the residual stone was located for precision puncture as the auxiliary channel, and direct stone fragmentation without expansion of the channel [16]. This optimized protocol may deal with the complex kidney stones while avoiding multichannel expansion and reducing surgical trauma and risks with the help of “Needle-perc” for an optical puncture [17]. While dealing with residual stones, due to the presence of the main working channel, it can ensure the effective reflux of perfusion fluid during surgery, thereby the intrarenal pressure can be sufficiently reduced during surgery. This has an important positive effect on reducing the surgical risks caused by abnormally high intrarenal pressure, such as infection, subcapsular hematoma and so on [18].
Intraoperative percutaneous renal puncture approach was performed using B-ultrasound guidance, following the these principles: The point of puncture closest to the skin was chosen in order to achieve a minimum of damage, usually between the posterior axillary line and the scapular line, between the 11th or the 12th subcostal space; The calyces with the highest relative position were selected for puncture, generally with a preference for the middle and upper calyces, in order to achieve maximization of the single channel percutaneous renal field of view [19]; Notably, while the prone position has traditionally been used in PCNL, it is associated with anesthesiological risks and is no longer the sole standard approach. The Valdivia position presents a viable alternative, offering benefits in terms of safety and flexibility during ECIRS procedures, while also mitigating some of the risks linked with traditional positioning [20].
Some researchers have used PCNL in the same period combined with flexible ureteroscopy to treat complex renal stones, which make full use of the advantages and characteristics of both equipment [21]. PCNL combined with flexible ureteroscopy, which also be called endoscopic combined intrarenal surgery (ECIRS), can effectively expand of the field of view for a wider range of intrarenal collecting system, and mutual supplementation of each own field blind area, to improve the stone-free rate of one-stage surgery. However, this surgery needs to utilize such a special body position as oblique 45 ° supine, and there is difficulty in body position placement. Due to the mutual influence between endoscopes and the alternating use of holmium laser in both PCN and flexible ureteroscopy, there may be a high risk of damage to endoscopic equipment. Fortunately, these problems do not exist in surgical methods utilizing standard PCNL combined with “Needle-perc”, whose surgical position can be performed with the standard prone position, and the attrition of endoscopic equipment is also not different from standard percutaneous nephroscopy while effectively improving the effect of surgery [22].
Retrospective nature and the small number of cases are the limitations of the present study, but it will contribute to the literature. Prospective randomized and larger cohorts of comparative studies should be conducted to support our findings, and further follow-up of the treated patients are needed to reach a consensus.
Conclusion
The optimized technique for treating complex renal calculi, utilizing standard percutaneous nephrolithotomy (PCNL) with holmium YAG laser and a visual needle nephroscope, demonstrates excellent feasibility, safety, and effectiveness. This approach enhances precise puncture accuracy, improves lithotripsy efficiency, and minimizes patient trauma. By reducing the likelihood of multi-stage or multi-tract procedures, it also decreases surgical risks. However, further randomized controlled studies are necessary to validate these findings.
Acknowledgements
Not applicable.
Author contributions
ENGO OVONE Yanne: Conceptualization, Methodology, Formal Analysis, Investigation, Writing - Original Draft, Visualization. Bai Lin WU: Conceptualization, Methodology, Resources, Writing - Review & Editing, Supervision, Project Administration. Cong Li: Data Curation, Software, Formal Analysis, Visualization, Writing - Review & Editing. Jiaqiao Zhang: Resources, Investigation, Writing - Review & Editing, Validation. Xiao Yu and Xiaolin Guo guided operative procedures. The specific contributions of each author are as follows: ENGO OVONE Yanne: Conceived the study design, developed the methodology, performed the data analysis, investigated the research questions, wrote the original draft of the manuscript, and created the visualizations. Huan Yang: Contributed to the conceptualization and methodology, provided resources for the study, reviewed and edited the manuscript, supervised the project, and handled project administration. Lei Cui: Curated the data, developed the software tools, conducted the formal data analysis, created the visualizations, and reviewed and edited the manuscript. Huan Yang: Provided resources for the study, participated in the investigation, reviewed and edited the manuscript, and validated the findings.All authors have read and approved the final version of the manuscript.
Funding
Project supported by the General Program of the Hubei Health Commission (Grant No. WJ2021M115).
Data availability
All data generated or analyzed during this study are included in this published article.
Declarations
Ethical approval and consent to participate
The experimental protocol was established according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. Written informed consent was obtained from individual or guardian participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Engo Ovone Yanne and Bai Lin Wu are co-first authors.
Contributor Information
Lei Cui, Email: cui1986lei@163.com.
Huan Yang, Email: yhpz123@163.com.
References
- 1.Okhunov Z, Friedlander JI, George AK, Duty BD, Moreira DM, Srinivasan AK, Hillelsohn J, Smith AD, Okeke Z. S.T.O.N.E. nephrolithometry: novel surgical classification system for kidney calculi. Urology. 2013;81:1154–9. [DOI] [PubMed] [Google Scholar]
- 2.Tyson MD 2nd, and, Humphreys MR. Postoperative complications after percutaneous nephrolithotomy: a contemporary analysis by insurance status in the United States. J Endourol. 2014;28:291–7. [DOI] [PubMed]
- 3.Xiao B, Ji CY, Su BX, Hu WG, Fu M, Li JX. (2020). Needle-perc: a new instrument and its initial clinical application. Chin Med J (Engl), 732–4. [DOI] [PMC free article] [PubMed]
- 4.Xiao B, Diao X, Jin S, Ji C, Zhang G, Su B, Tang Y, Li J. A Novel Surgical technique for treatment of Renal stones in Preschool-aged patients: initial experience with needle-perc. Urology. 2020;146:211–5. [DOI] [PubMed] [Google Scholar]
- 5.de la Rosette JJ, Opondo D, Daels FP, Giusti G, Serrano A, Kandasami SV, Wolf JS Jr., Grabe M, Gravas S. Categorisation of complications and validation of the Clavien score for percutaneous nephrolithotomy. Eur Urol. 2012;62:246–55. [DOI] [PubMed] [Google Scholar]
- 6.Soucy F, Ko R, Duvdevani M, Nott L, Denstedt JD, Razvi H. Percutaneous nephrolithotomy for staghorn calculi: a single center’s experience over 15 years. J Endourol. 2009;23:1669–73. [DOI] [PubMed] [Google Scholar]
- 7.Chung BI, Aron M, Hegarty NJ, Desai MM. Ureteroscopic versus percutaneous treatment for medium-size (1-2-cm) renal calculi. J Endourol. 2008;22:343–6. [DOI] [PubMed] [Google Scholar]
- 8.Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. 2011;25:1131–5. [DOI] [PubMed] [Google Scholar]
- 9.Zhu W, Li J, Yuan J, Liu Y, Wan SP, Liu G, Chen W, Wu W, Luo J, Zhong D, et al. A prospective and randomised trial comparing fluoroscopic, total ultrasonographic, and combined guidance for renal access in mini-percutaneous nephrolithotomy. BJU Int. 2017;119:612–8. [DOI] [PubMed] [Google Scholar]
- 10.Ghani KR, Andonian S, Bultitude M, Desai M, Giusti G, Okhunov Z, Preminger GM, de la Rosette J. Percutaneous nephrolithotomy: Update, Trends, and future directions. Eur Urol. 2016;70:382–96. [DOI] [PubMed] [Google Scholar]
- 11.Li LY, Gao X, Yang M, Li JF, Zhang HB, Xu WF, Lin Z. Does a smaller tract in percutaneous nephrolithotomy contribute to less invasiveness? A prospective comparative study. Urology. 2010;75:56–61. [DOI] [PubMed] [Google Scholar]
- 12.Kaynar M, Sümer A, Şalvarcı A, Tekinarslan E, Cenker A, Istanbulluoğlu MO. Micropercutaneous nephrolithotomy (microperc) in a two-year-old with the ‘all-seeing needle’. Urol Int. 2013;91:239–41. [DOI] [PubMed] [Google Scholar]
- 13.Desai M, Mishra S. Microperc’ micro percutaneous nephrolithotomy: evidence to practice. Curr Opin Urol. 2012;22:134–8. [DOI] [PubMed] [Google Scholar]
- 14.Ganpule AP, Chabra J, Desai MR. Microperc micropercutaneous nephrolithotomy: a review of the literature. Urolithiasis. 2018;46:107–14. [DOI] [PubMed] [Google Scholar]
- 15.Ganpule AP, Chhabra JS, Sudharsan SB, Jairath A, Vijaykumar M, Sabnis R, Desai MR. Extending indications of micropercutaneous nephrolithotomy: it is not just about cracking stones. Arab J Urol. 2017;15:17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tepeler A, Armagan A, Sancaktutar AA, Silay MS, Penbegul N, Akman T, Hatipoglu NK, Ersoz C, Erdem MR, Akcay M. The role of microperc in the treatment of symptomatic lower Pole renal calculi. J Endourol. 2013;27:13–8. [DOI] [PubMed] [Google Scholar]
- 17.Bader MJ, Gratzke C, Seitz M, Sharma R, Stief CG, Desai M. The all-seeing needle: initial results of an optical puncture system confirming access in percutaneous nephrolithotomy. Eur Urol. 2011;59:1054–9. [DOI] [PubMed] [Google Scholar]
- 18.Tepeler A, Akman T, Silay MS, Akcay M, Ersoz C, Kalkan S, Armagan A, Sarica K. Comparison of intrarenal pelvic pressure during micro-percutaneous nephrolithotomy and conventional percutaneous nephrolithotomy. Urolithiasis. 2014;42:275–9. [DOI] [PubMed] [Google Scholar]
- 19.Akbulut F, Ucpinar B, Savun M, Kucuktopcu O, Ozgor F, Simsek A, Gurbuz G. (2015). A Major Complication in Micropercutaneous Nephrolithotomy: Upper Calyceal Perforation with Extrarenal Migration of Stone Fragments due to Increased Intrarenal Pelvic Pressure. Case reports in urology 2015, 792780. [DOI] [PMC free article] [PubMed]
- 20.Hong Y, Wang H, Xu Q, Chen L, Huang X, Xiong L. Mini-track, mini-nephroscopy, mini-ultrasonic probe percutaneous nephrolithotomy and its initial clinical application. BMC Urol. 2022;22:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeng J, Zhang L, Chen X, He H, Li X. (2022). The treatment option for calyceal diverticulum stones: flexible ureteroscopy lithotripsy (FURL) or all-seeing needle-assisted percutaneous nephrolithotomy (PCNL)? Urolithiasis. [DOI] [PubMed]
- 22.Jiang K, Chen H, Yu X, Chen Z, Ye Z, Yuan H. The all-seeing needle micro-PCNL versus flexible ureterorenoscopy for lower calyceal stones of ≤ 2 cm. Urolithiasis. 2019;47:201–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.