Abstract
Background
Middle-aged adults, defined as individuals between the ages of 45 and 64, represent a significant yet under researched group of healthcare service users. This scoping review aimed to provide a comprehensive overview of the patterns of healthcare utilisation and the factors contributing to them within this demographic.
Methods
Following PRISMA-ScR guidelines and the framework proposed by Arksey and O’Malley, a systematic literature search was conducted across PubMed, EMBASE, and the Cochrane Library databases from their inception until July 2023. Key search terms such as “healthcare utilisation” and “middle-aged” were used to identify relevant studies. Articles were included if they were original cohort, case-control, or cross-sectional studies published in English. The findings were then synthesised narratively, by identifying recurring concepts and grouping them into broader themes. The themes were categorised according to the Andersen healthcare utilisation model’s three factors: predisposing factors, enabling factors, and need-related factors.
Results
After screening 4,810 records, a total of 25 articles were selected for final analysis, comprising 15 from developed countries and 10 from developing countries. Consistent factors influencing healthcare utilisation included multimorbidity, socioeconomic status, and poor health behaviours. Differences emerged across contexts: in developed countries, healthcare utilisation was influenced by lifestyle behaviours and access to private care, while in developing countries, socioeconomic inequalities and limited insurance coverage played more dominant roles. Healthcare system structures likely shaped utilisation patterns.
Conclusion
Healthcare utilisation among middle-aged adults is driven by an interplay of medical, social, and economic factors that vary across contexts. Common contributors, such as multimorbidity and poor health behaviours, highlight the need for targeted interventions and policies focusing on primary and preventive care to address the long-term burden of healthcare utilisation. This demographic faces unique challenges in managing healthcare decisions amidst varying systemic and individual-level challenges, which should be further studied.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41043-024-00715-z.
Keywords: Middle-aged, Healthcare utilisation, Contributory factors, Scoping review
Introduction
Middle-aged patients contribute to a substantial proportion of high utilisers of healthcare services. In the United States, middle-aged Americans aged 45 to 64 comprise 37.0% of the top 10% of healthcare utilisers in terms of expenditures [1]. In Australia, 28.54% of men and 26.54% of women aged 45–54 have presented to the Emergency Department between 2020 and 2021 [2]. While it is established that senescence is the main contributing factor to healthcare utilisation among patients aged 45 and above, there is a need to explore the contributions of other factors to the catastrophic health expenditure and persistently high healthcare utilisation, especially among middle-aged persons.
The Andersen healthcare utilisation model [3] provides a simple framework to investigate contributing factors to healthcare utilisation. This model outlines three key concepts that explain the use of healthcare services: predisposing factors, enabling factors, and need-related factors [4]. Predisposing factors include demographic characteristics such as age, gender, and social structure. Enabling factors encompass resources available to individuals for using health services, including income, health insurance, and access to care. Need-related factors refer to the individual’s perceived and evaluated need for health services, including the presence of chronic conditions and comorbidities. In this scoping review, we aim to further explore how all three types of factors may act to contribute to high healthcare utilisation among certain middle-aged patients.
To achieve this, we chose to conduct a scoping review rather than a systematic review and meta-analysis. Scoping reviews are particularly useful when the topic has not been comprehensively reviewed before, or when the literature is heterogeneous and complex, with varied methodologies and outcome measures, making it difficult to apply more precise systematic review methodologies [5]. This approach allows us to explore a broad range of factors contributing to healthcare utilisation among middle-aged patients, rather than focusing narrowly on specific variables as would be necessary in a systematic review or meta-analysis. A scoping review would also allow us to map the existing literature, identify key concepts, and highlight gaps in the research that require further investigation, as per Arksey and O’Malley’s framework for scoping reviews [6].
For the purposes of this study, we defined “middle-aged” as individuals between 45 and 64 years of age, a range widely used in existing literature [7]. This age group was selected to capture a broad spectrum of healthcare utilisation patterns and contributing factors. For “healthcare utilisation,” our focus was limited to hospital-based services, including both inpatient and outpatient care, as these typically account for the largest healthcare expenditures. Dental services and non-hospital psychiatric care were excluded to maintain a clear scope. While much of the existing research focuses on healthcare utilisation among the elderly or specific disease populations, middle-aged adults face distinct challenges, such as balancing preventive care with the early management of chronic conditions. This scoping review thus seeks to address this research gap by offering a comprehensive analysis of the factors influencing healthcare utilisation in this demographic. By identifying these factors, we aim to provide actionable insights to guide healthcare policies and interventions that optimise utilisation patterns and improve health outcomes for middle-aged adults.
Methods
Type of study
In accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines [8] and the framework proposed by Arksey and O’Malley [6], along with recommendations from Levac et al. [9], we conducted a comprehensive search of PubMed, EMBASE, and the Cochrane Library databases from their inception until July 2023. In consultation with a medical information specialist, the following key terms were used in combination: “healthcare utilisation,” “healthcare utilisation,” “middle-aged,” and relevant synonyms. The full search strategy for Medline is provided below:
Middle-aged adults: exp Middle Aged/ OR (“middle-age*” OR “middle age*”).ti, ab.
Healthcare utilisation: exp “Facilities and Services Utilization”/ OR (“health utilization*” OR “health utilisation*” OR “health utilizer*” OR “health utiliser*” OR “healthcare utilization*” OR “healthcare utilisation*”).ti, ab.
Limits: limit to English language; limit to (case reports OR classical article OR clinical study OR clinical trial, all OR clinical trial OR comparative study OR controlled clinical trial OR “corrected and republished article” OR observational study OR randomised controlled trial).
The complete search strategies for Medline, EMBASE and the Cochrane Library are provided in the Supplementary Material (Table S1).
Backward searching was also performed to look for articles of interest. This involved examining the reference lists of all included articles to identify additional studies that may not have been captured in the initial database search.
Eligibility and inclusion criteria
All references were imported into Covidence (Melbourne, Victoria, Australia, https://app.covidence.org/) for compilation and duplicate removal. All titles and abstracts were independently screened by three authors (Y.N., A.J.A.L. and C.C.) for inclusion. Full-text reviews were subsequently conducted to confirm eligibility. The inclusion criteria required studies to: (1) focus on healthcare utilisation among middle-aged individuals (defined as ages 45–64); (2) be original cohort, case-control, or cross-sectional studies; (3) be published in English; and (4) report data relevant to the three factors of the Andersen Healthcare Utilisation Model: predisposing, enabling, or need-related factors.
Exclusion criteria
Studies were excluded if they: (1) were not peer-reviewed original research, (2) were opinion pieces, reviews, or editorials, (3) focused on populations outside the age range of 45–64 or did not provide age-stratified data relevant to middle-aged individuals, (4) were not available in English, and (5) lacked data relevant to healthcare utilisation or its contributing factors, such as studies on unrelated medical outcomes, interventions, or populations.
Reviewer agreement process
To ensure consistency and accuracy, all titles and abstracts were independently screened by three reviewers (Y.N., A.J.A.L., and C.C.). Each reviewer made inclusion decisions independently, blinded to the others’ decisions. Disagreements at this stage were resolved through consensus discussions. For full-text reviews, all disagreements were reviewed and resolved by the senior author (Q.X.N.) after consulting the study protocol and inclusion criteria. Agreement rates among reviewers were monitored, and any substantial discrepancies were addressed to enhance inter-reviewer reliability.
Data extraction and outcomes
Healthcare costs and healthcare utilisation, though related, were treated as distinct concepts in this analysis. Healthcare costs refer to the financial expenditure incurred for medical services, while healthcare utilisation pertains to the frequency and types of medical services accessed. This distinction was maintained throughout the study to ensure conceptual clarity and accurate interpretation of the findings. The primary outcome of interest in this review is the identification of factors and patterns underlying healthcare utilisation among the middle-aged population. Extracted data included study characteristics (e.g., author, year of publication, country, study design, and study population). Patient demographics included sample size, age, gender, presence of comorbidities, and income level. Each article was double coded by three independent authors (Y.N., A.J.A.L. and C.C.), and all disagreements were resolved through consensus with the senior author (Q.X.N.). Findings were cross-checked and verified by the senior author. The studies were classified into two groups: (1) developed countries and (2) developing countries, based on World Bank economic stratification.
Synthesis of findings
In the synthesis of findings, we employed both quantitative and qualitative methods to aggregate and interpret the data collected from the included studies. We started by conducting a descriptive analysis of the studies included. This involved summarizing the study characteristics, such as author name, year of publication, country, study design, and study population. Patient demographics, including sample size, age, gender, presence of comorbidities, and income level, were summarised. We categorised studies into two groups based on the country of origin: (1) developed countries and (2) developing countries. We then performed a narrative synthesis of the qualitative findings, as guided by Popay et al. [10] to identify common themes and patterns in the factors contributing to healthcare utilisation among middle-aged individuals. This qualitative approach involved coding the data to identify recurring concepts and grouping them into broader themes. The themes were categorised according to the Andersen healthcare utilisation model’s three factors: predisposing factors, enabling factors, and need-related factors [3].
To provide a comprehensive understanding of the factors influencing healthcare utilisation, we integrated quantitative and qualitative findings where applicable. This integration was guided by a mixed-methods synthesis approach that combined numerical data (e.g., prevalence rates, statistical associations) with narrative themes derived from the included studies. The rationale for integrating these data types was to bridge numerical patterns with contextual insights, thereby enhancing the interpretability and applicability of findings. While quantitative data allowed us to measure the prevalence and magnitude of healthcare utilisation factors, qualitative findings provided deeper insights into the underlying reasons, motivations, and barriers reported by study participants. The process involved identifying common themes across qualitative studies, such as psychological distress, socioeconomic barriers, or the impact of multimorbidity; mapping quantitative data (e.g., prevalence rates, statistical correlations) onto these themes to quantify the magnitude or significance of the reported factors; and using these mapped themes to identify patterns, contradictions, or gaps between quantitative and qualitative findings.
The following research questions guided this integration:
What are the quantitative patterns (e.g., prevalence, associations) of healthcare utilisation factors among middle-aged adults?
How do qualitative studies contextualise and explain these quantitative patterns?
How do these findings align or diverge across different economic settings (developed vs. developing countries)?
Study quality assessment
The quality of included cohort, case-control or cross-sectional studies was assessed based on reporting quality and methodological rigor using the Newcastle-Ottawa Scale (NOS) [11]. The NOS is based on three domains: selection, comparability, and outcome (or exposure for case-control studies). For the selection domain, studies were evaluated for representativeness, selection of controls or cohorts, and ascertainment of exposure or outcomes, scoring up to four points. The comparability domain, which assessed the control of confounding factors such as demographics and socioeconomic variables, allowed for a maximum of two points. The outcome or exposure domain evaluated factors like the adequacy of follow-up, completeness of data, and consistency in methodology, with a maximum of three points. Each study was independently scored by two reviewers (Y.N. and A.J.A.L.), with discrepancies resolved through discussion with a third reviewer (Q.X.N.), and assigned a total score out of nine, labelling studies as high quality (7–9 points), moderate quality (4–6 points), or low quality (≤ 3 points). This approach ensured a rigorous and transparent assessment of study quality. Details of the assessment criteria and results are provided in the Supplementary Material (Table S2).
Results
Summary of included articles
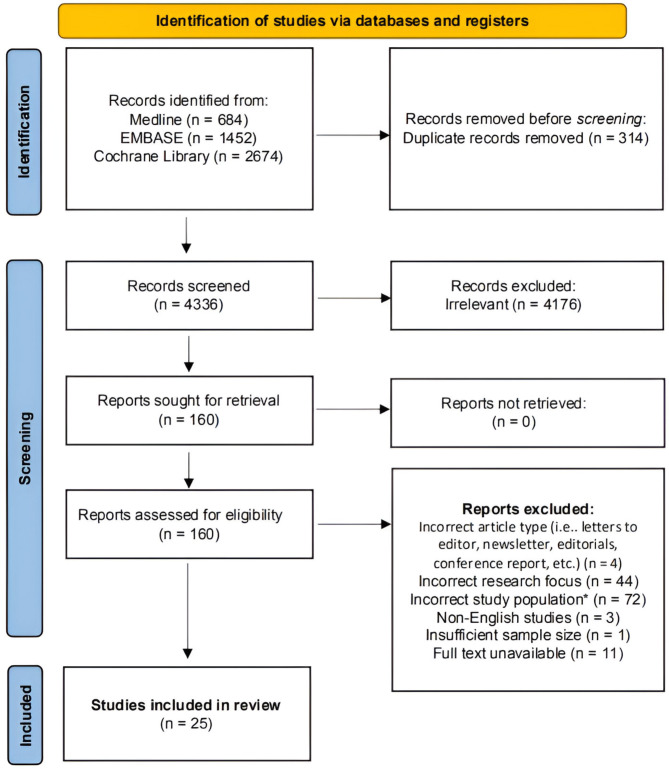
The initial database search, along with screening of review articles, yielded 4,810 articles. After removing 314 duplicates, we manually screened the titles and abstracts of 4,336 articles, leaving 160 articles for full-text screening. During the title and abstract screening phase, articles were excluded based on the following criteria: (1) incorrect research focus (meaning articles that did not examine healthcare utilisation or its contributing factors, e.g., studies on unrelated medical outcomes, interventions, or populations outside the defined age range); (2) incorrect article type (letters, newsletters, editorials, conference reports, and other non-peer-reviewed publications); and (3) incorrect study population (studies that focused on populations outside the 45–64 age range or that lacked age-stratified data relevant to middle-aged individuals).
After full-text review, a total of 25 articles were included in the final analysis [12–36]. Most of the included studies were conducted in the United States [14, 15, 19, 20, 22, 26], Australia [16, 21, 24, 25], and China [28, 29, 33–36], while a minority were carried out in Canada [12], Cyprus [27], India [31], Iran [32], Japan [25], Norway [13], Taiwan [18], and the United Kingdom [23]. The selection process and reasons for excluding articles are illustrated in the PRISMA flow diagram (Fig. 1). Studies were categorised according to the World Bank data [37] into high-income countries (HIC or developed) and low or middle-income countries (LMIC or developing). Fifteen studies were conducted in developed countries [12–26], while the remaining ten were conducted in developing countries [27–36]. A summary of the included articles and their findings can be found in Tables 1 and 2 for developed countries and developing countries, respectively.
Fig. 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flowchart showing the article screening and selection process
Table 1.
Summary of findings from developed countries
| Author, Year | Country | Study Design | Sample Size | Factors Analysed | Study Conclusions |
|---|---|---|---|---|---|
| Alberga et al., 2018 [12] | Canada | Cohort Study | 87,338 | Household income, health status (BMI), life stress, and health behaviours (smoking, alcohol, physical activity, diet) | There is an association between high healthcare utilisation and behavioural factors, particularly for smoking and physical activity (or lack thereof) |
| Edwards et al., 2019 [13] | Norway | Cross-sectional | 33,882 | Body Mass Index | Both overweight and obesity are associated with increased healthcare utilisation, despite adjustments for BMI-specific survival |
| Ezeamama et al., 2016 [14] | United States | Cross-sectional | 4,562 | Resilience Indicators (Mastery, Social Support, Cumulative Lifetime Adversity) | Higher resilience reduces healthcare utilisation, but cumulative lifetime adversity increases hospitalizations |
| Fazeli Dehkordy et al., 2016 [15] | United States | Cross-sectional | 1,078 | Everyday discrimination | Perceived discrimination correlates with increased healthcare use, but race/ethnicity is not a significant factor |
| Ishida et al., 2023 [16] | Australia | Cross-sectional | 11,211 | Obesity | Being overweight or obese is significantly associated with greater healthcare utilisation (for instance, the number of GP visits and number of prescribed medications), loss of work productivity and greater number of sick days taken |
| Lee et al., 2010 [17] | Taiwan | Cross-sectional | 1,492 | Health literacy | Low health literacy is common but does not significantly affect healthcare utilisation |
| Lee et al., 2017 [18] | Taiwan | Cross-Sectional | 2,911 | Individual lifestyle and habits (i.e., exercise habits, breakfast, regular meals, 5 servings of fruits and vegetables, dieting habits, awareness of food packaging labels, awareness of self-health, regular blood pressure, smoking habits, drinking habits, and betel-nut chewing), participant demographics (i.e., gender, age, education level and presence of disease) | Healthy lifestyles increase preventive care utilisation but have little impact on outpatient visits |
| Musich et al., 2016 [19] | United States | Cohort Study | 10,816 | Enrolment in personalised preventive medicine program | Personalised preventive care models like MDVIP improve healthcare management and quality for similar expenditure |
| Peterson et al., 2015 [20] | United States | Cohort Study | 215,107 | Obesity, physical disability, insurance, education level, exercise | Obesity increases healthcare utilisation, with an additional burden on those with physical disabilities |
| Rana et al., 2020 [21] | Australia | Cross-sectional | 30,669 | Private health insurance (PHI) effect on care seeking behaviour | PHI holders had greater utilisation of preventive care, specialist care, and hospital stays but shows minimal impact after dropping coverage |
| Rasu et al., 2015 [22] | United States | Cohort Study | 22,599 | Health Literacy | Lower health literacy leads to higher healthcare costs and utilisation, especially for prescriptions |
| Rudisill et al., 2016 [23] | United Kingdom | Cohort Study | 250,046 | Obesity, comorbidity, depression | Comorbidity is the greatest predictor of healthcare costs, followed by depression and increased BMI |
| Schlichthorst et al., 2016 [24] | Australia | Cross-sectional | 13,763 |
Socio-demographic factors: Education; location; marital status; country of birth; employment status; financial problems, etc. Individual health, lifestyle factors: Self-rated health; smoking; drinking; weight; pain medication usage |
In general, obesity and daily pain medication use drive healthcare utilisation, but most men underutilise healthcare services |
| Sum et al., 2020 [25] | Australia & Japan | Cross-sectional | 6832 Australians, 3503 Japanese | Multimorbidity (i.e., non-communicable diseases); socioeconomic group/status | In both countries, greater multimorbidity increases healthcare utilisation, especially among lower education and socioeconomic groups |
| Weissman et al. 2016 [26] | United States | Cohort Study | 9,271 | Serious Psychological Distress (unable to make efforts, nervousness, hopelessness, sadness, worthlessness, and restlessness) | Serious psychological distress increases healthcare utilisation, particularly due to hopelessness, even after adjusting for comorbidities |
Legend: BMI, Body mass index; NCD, non-communicable diseases; PHI, Private health insurance; GP, General Practitioner; MDVIP, MD-Value in Prevention; SPD, Serious Psychological Distress
Table 2.
Summary of findings from developing countries
| Author, Year | Country | Study Design | Sample Size | Factors Analysed | Study Conclusions |
|---|---|---|---|---|---|
| Abuduxike et al., 2020 [27] | Cyprus | Cross-sectional | 507 | Chronic disease, health perception, and socioeconomic inequalities | Healthcare utilisation is driven by income, education, age, insurance, chronic illness, self-perceived health, and family size |
| Gong et al., 2016 [28] | China | Cohort Study | 18,246 | Financial capacity, education, living standards, residency, perceived health, age and chronic illness | Higher education, urban residency, and better living standards increase healthcare utilisation. Socioeconomic status and chronic diseases are key factors |
| Lam et al., 2012 [29] | China | Cross-sectional | 1,543 | Migrant status, government insurance status, education level, occupation, income level | Migrant workers have lower healthcare utilisation due to limited insurance coverage; chronic conditions are strongly linked to increased utilisation |
| Nguyen et al., 2023 [30] | Vietnam | Cross-sectional | 362 | Chronic disease (namely: migraine, diabetes, cardiovascular disease), level of social support received, health information sources, health service utilisation (in- and out-patient) | Middle-aged Vietnamese women, in both urban and rural areas, present with relatively high rates of healthcare utilisation compared to the general Vietnamese population |
| Pati et al., 2020 [31] | India | Cross-sectional | 1,649 | Healthcare institution (private vs. public); multimorbidity (i.e. chronic diseases); sex; socioeconomic condition; ethnicity; education level; marital status | In general, patients in public facilities have more multimorbidity, with age being the strongest predictor across both public and private sectors |
| Vahedi et al., 2020 [32] | Iran | Cross-sectional | 25,664 | Socioeconomic inequalities | Subsidised inpatient healthcare services could increase utilisation among disadvantaged groups |
| Wang et al., 2018 [33] | China | Cohort Study | 18,433 | Health Insurance, Education Level, Income level | Individuals covered by UEMI had the highest healthcare costs and highest healthcare utilisation/expense |
| Wang et al., 2023 [34] | China | Cohort Study | 17,182 | Education level, insurance, BMI, multimorbidity | Multimorbidity increases the risk of catastrophic healthcare expenditures, especially in older populations with low socioeconomic status |
| Zhao et al., 2020 [35] | China | Cross-sectional | 17,867 | Multimorbidity (i.e. chronic diseases); income level | Multimorbidity increases healthcare utilisation, with younger multimorbid individuals utilizing more services; higher income is associated with lower utilisation |
| Zhou et al., 2020 [36] | China | Cohort Study | 17,250 in 2011, 18,195 in 2013, 19,842 in 2015 | Education level, insurance, multimorbidity, depression, self-reported health | Increased medical insurance coverage leads to higher healthcare utilisation |
Legend: BMI, Body Mass Index; UEMI, Urban Employee Medical Insurance
General patterns of healthcare utilisation among middle-aged individuals
Healthcare utilisation among middle-aged individuals vary depending on medical, social, and economic factors and across different regions. Common patterns such as the influence of multimorbidity and socioeconomic status are observed globally, the extent and nature of these influences differ between developed and developing countries. In developed regions, access to private healthcare and engagement in preventive care services are often linked to higher income levels and better health literacy [17, 22, 25]. Conversely, in developing countries, healthcare utilisation is more frequently driven by age, socioeconomic inequalities, and access to health insurance [27–36].
Risk factors contributing to increased healthcare utilisation
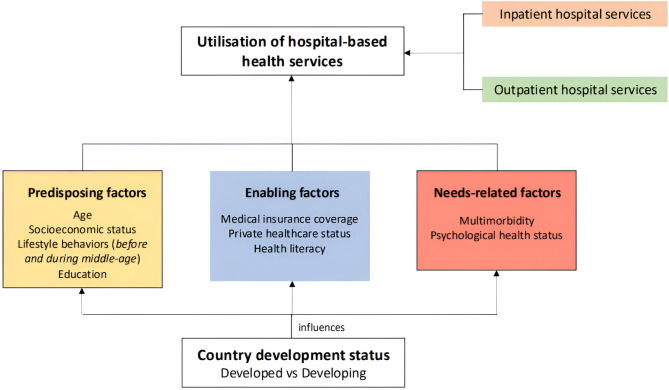
Our findings identified several prevalent medical and social risk factors predisposing individuals to increased healthcare utilisation, regardless of the country’s World Bank economic stratification. Investigated risk factors were classified according to the Andersen model predicting health service access and utilisation. Furthermore, additional analysis of the impact of Fig. 2 illustrates the key predisposing factors, enabling factors, and need-related factors identified across the included studies.
Fig. 2.
Conceptual figure illustrating the influence of predisposing, enabling and need-related factors on individuals’ healthcare utilisation, based on the Andersen model [3]
Predisposing factors
Poor health behaviours, such as smoking, lack of physical exercise, and poor self-care, were shown to be strong determinants of healthcare utilisation [12, 27].
Enabling factors
There was no consensus among the studies on how health literacy affects healthcare utilisation. Rasu et al. [22] found that lower health literacy is associated with higher healthcare utilisation and expenditures, with adults having basic or below basic health literacy incurring greater prescription costs (USD $3,362) compared to those with above basic health literacy (USD $910). Conversely, Lee et al. [18] and Gong et al. [28] found that individuals with higher health literacy are more likely to engage in healthcare services.
Needs-related factors
Individuals with high burdens of negative emotional states, diagnosed psychological conditions, or experiencing elevated levels of stress were observed to have increased risks of becoming high healthcare utilisers. Weissman et al. [26] suggested that poor emotional states associated with serious psychological distress (e.g., sadness, hopelessness, worthlessness, restlessness, anxiety) have a direct impact on increasing healthcare utilisation burden. Interestingly, this risk factor is significant regardless of the individual’s current health status. However, while negative emotional states lead to increased need for healthcare utilisation, Weissman et al. [26] also suggested that this does not necessarily result in individuals seeking the required medical care.
Additionally, many studies from both developed and developing countries emphasised the role of multimorbidity in increasing healthcare utilisation among the middle-aged population. The presence of long-term health conditions increases the likelihood of utilising health services, especially in older populations [35]. For example, the risk of long-term household catastrophic healthcare expenditure events was found to be 19% higher for each additional noncommunicable disease in middle-aged and older adults [34].
Different key drivers of Healthcare Utilisation in developed and developing countries
The distribution and influence of certain predisposing and enabling factors varied between developed and developing countries. In developed countries, several studies highlighted obesity and obesity-related morbidities, healthy lifestyle patterns, and private healthcare status as key drivers of healthcare utilisation. Studies pointed out that obesity increases outpatient visits [13, 20] and the number of prescribed medications [16, 24]. Rudisill et al. [23] reported that while obesity is a major predictor of healthcare costs, high healthcare service utilisation is primarily due to obesity-related morbidities rather than high body mass index (BMI) alone. Healthy lifestyle patterns were shown to increase outpatient service usage as individuals become more involved in monitoring their health conditions [18]. Additionally, private healthcare status significantly impacted health-seeking behaviours of middle-aged patients, especially in preventive care [21].
On the other hand, in developing countries, age, socioeconomic status, and medical insurance coverage were identified as significant factors associated with increased healthcare utilisation. Age was found to have a strong relationship with the presence of multimorbidity, as the number of morbidities increases linearly with age for both sexes [31]. Socioeconomic status (SES) plays a significant role in living standards, which consequently affects health status and the need for healthcare utilisation in the long run [28, 34]. A cross-sectional study involving 17,867 middle-aged adults from Shandong, China, found that individuals with more morbidities had higher healthcare utilisation compared to their healthier counterparts [35]. While higher income levels were associated with lower healthcare costs, it remains unclear whether the observed increase in healthcare utilisation among middle-aged individuals with morbidities is consistent across all SES groups or primarily driven by those in lower SES brackets. Further research is required to clarify the relationship between SES and healthcare utilisation in this demographic [35]. Studies by Wang et al. [33] and Zhou et al. [36] highlighted that higher medical insurance coverage increases healthcare utilisation, especially in public healthcare settings. Conversely, a lack of health insurance was associated with lesser healthcare utilisation [29].
Discussion
The 25 studies reviewed herein vary in their methodologies, databases used and findings, reflecting the multifaceted and complex nature of healthcare utilisation among the middle-aged population [12–36]. Numerous factors at play influence the pattern of healthcare utilisation and most notably, multimorbidity has been consistently highlighted in several studies across developed and developing countries [23, 25, 34–36]. The findings also evince that even among patients with multimorbidity, factors such as age, socioeconomic status, and lifestyle patterns significantly influence healthcare utilisation. With more comorbidities, patients are likely to incur more healthcare-related spending given the medical treatment and follow-ups often required. Consequently, it can decrease work productivity and employment odds, which in turn can affect one’s socioeconomic status [16, 25]. Individuals with lower socioeconomic status often face challenges in affording necessary healthcare and insurance coverage, which impedes effective health monitoring and preventive care. This creates a self-reinforcing cycle, wherein limited healthcare access and unmet medical needs exacerbate the demand for healthcare services over time [38].
The relationship between health literacy and healthcare utilisation is less consistent across the studies. Some studies, such as that by Rasu et al. [22], found that lower health literacy is associated with higher healthcare utilisation, while others, like Lee et al. [18] and Gong et al. [28], reported that individuals with higher health literacy are more likely to engage in healthcare services. Despite this increased engagement, those with higher health literacy often spend less on healthcare overall compared to individuals with multimorbidity. In developing countries, low health literacy has been linked to poor health perceptions and self-care, contributing to greater healthcare needs [17, 28].
The variability in the relationship between health literacy and healthcare utilisation may be influenced by socioeconomic factors [39]. For instance, higher socioeconomic status often correlates with better access to health insurance and lower healthcare costs [18, 28]. There may also be an inverse relationship between socioeconomic status and unhealthy behaviours [39]. However, such health literacy gaps are difficult to quantify, with physicians often unaware of individuals’ health literacy status [40]. Resultant care gaps may then become institutionalised, leading to increasing healthcare needs.
Behavioural and psychological risk factors, such as obesity, smoking, and physical inactivity, also significantly influence healthcare utilisation. These factors have been well-documented in the literature [41, 42], similar to the studies reviewed herein, which show the same trend for developed countries for these behaviours and increased healthcare utilisation [13, 16, 20, 23, 24]. In contrast, healthcare utilisation in developing countries appears to be more often affected by systemic factors like age, socioeconomic status, and medical insurance coverage [28, 29, 31, 33–35].
The findings of this review align with the broader consensus that multimorbidity increases the likelihood of becoming a high healthcare utiliser [43, 44]. Outside of the review, studies conducted in countries like the Netherlands [43] and Ireland [44] have found that patients with multimorbidity incur significantly higher healthcare costs across the healthcare system and are more frequent utilisers (with more primary care visits, hospital visits, and hospital admissions), regardless of their demographic or SES. The presence of multiple chronic conditions is an important predictor of future healthcare needs, emphasising the need for targeted interventions to reduce the burden of multimorbidity in the population.
For middle-aged individuals, the metaphor of the “Goldilocks Zone” illuminates the challenges they encounter in navigating healthcare decisions amidst multiple conflicting pressures—be it the management of chronic conditions, preventive care, or the socioeconomic factors influencing access to services [45]. For instance, middle-aged adults must balance not overburdening the healthcare system with unnecessary visits (being mindful of scarce resources) while also not delaying care that could prevent worsening conditions or complications later in life. This is particularly relevant in the review’s findings on how enabling factors such as access to private healthcare and insurance coverage impact healthcare-seeking behaviour. In developed countries, access to private care allows individuals to engage more proactively in their health, navigating the “Goldilocks Zone” more effectively by not delaying preventive services. Conversely, in developing countries, individuals may struggle to access care at the right time due to barriers like insufficient insurance coverage, hence the need for improving access to care, enhancing health literacy, and reducing barriers. In doing so, health systems can help these individuals make more confident and informed decisions about when to seek medical care.
These findings also highlight the middle-aged phase of life as a crucial checkpoint and predictor of future health status. Middle-aged individuals play central roles in their families, workplaces, and society, making their health and well-being critical for the larger community [46]. Risk factors identified in this study, such as poor lifestyle habits, increase the likelihood of becoming high healthcare utilisers later in life. Moreover, middle-aged individuals with similar risk factors often experience poorer health outcomes and quality of life in older age [47]. Promoting healthy behaviours during this phase can increase the chances of successful aging, minimizing the onset of disability or chronic disease [48]. To mitigate the impact of multimorbidity, several strategies can be employed. Primary and preventive healthcare should be prioritised to better manage chronic conditions and prevent their onset. Secondary prevention programs, such as those targeting Diabetes mellitus, can help reduce future healthcare utilisation and costs [49, 50]. Additionally, lifestyle interventions aimed at reducing physical inactivity and unhealthy diets can help reduce the incidence of chronic conditions that lead to high healthcare utilisation.
This review offers novel contributions in three key areas. First, it highlights systemic inequities and contextual differences in healthcare utilisation, with private healthcare and preventive services playing a larger role in developed countries, while socioeconomic barriers and health insurance access are more critical in developing nations. These insights emphasise the need for context-specific policies and interventions. Second, it identifies underexplored areas, such as the complex interplay between health literacy and healthcare utilisation, providing a foundation for future research, including systematic reviews or meta-analyses on specific factors like health literacy or multimorbidity. Lastly, by mapping factors against the Andersen model, the review provides actionable insights for policymakers and healthcare providers. For example, addressing multimorbidity, enhancing health literacy, and expanding insurance coverage can reduce inequities and optimise healthcare access for middle-aged adults. As vital contributors to the workforce and caregivers within families, this demographic represents a critical population for improving health outcomes and achieving broader societal benefits.
Strengths and limitations of study
The strength of this review lies in its breadth and detailed comparison of healthcare utilisation across different contexts, revealing the multifactorial and context-specific drivers of healthcare use in middle-aged populations. By synthesizing findings from both developed and developing countries, this review provides a comprehensive overview of patterns and factors influencing healthcare utilisation, offering valuable insights for tailoring health policies and interventions. Nonetheless, several limitations have to be mentioned. Firstly, a significant limitation is the inability to directly compare the impacts of varied factors influencing healthcare utilisation. Without conducting a meta-analysis, it was not possible to assign relative weights to the data from each study or rank these factors in terms of their importance. Furthermore, inconsistent findings across studies could not be reconciled due to methodological heterogeneity. Addressing these discrepancies would require a more focused investigation, potentially incorporating meta-analytic techniques, to directly compare these outcomes and assess the relative contributions of factors such as multimorbidity, socioeconomic status, and health literacy. Secondly, this review focused on hospital-based services (both inpatient and outpatient) as they typically represent the largest healthcare expenditures. However, this approach introduces potential ‘confounding’, particularly when comparing health systems with different structures and roles for primary care. For instance, in countries such as the United States and China, where healthcare systems allow more direct access to hospital-based services, patients may bypass primary care entirely. Conversely, in countries such as Norway or the United Kingdom, hospital consultations often require a referral from primary care providers, reflecting their gatekeeping function. These differences in system design and referral pathways may influence healthcare utilisation patterns and should be carefully considered when interpreting findings. Thirdly, this review does not explicitly address whether middle-aged individuals seek appropriate medical attention when necessary. In resource-constrained settings, there is a possibility that individuals delay seeking care until their conditions become severe, potentially leading to poorer health outcomes and higher costs. This hypothesis warrants further investigation to explore whether delayed care-seeking behaviours contribute to increased healthcare utilisation or worse outcomes in middle-aged populations in such settings. Lastly, while this review categorised studies based on economic status (developed versus developing countries), future research could benefit from additional stratifications based on the role and structure of primary care within healthcare systems. Comparing countries with established gatekeeping models in primary care, such as Norway and the UK, to those with more open-access models, like the US and China, could provide deeper insights into how healthcare system structures influence utilisation patterns. Such an analysis could illuminate whether systems with strong referral frameworks and integrated primary care reduce reliance on hospital-based care, as well as how these systems impact health-seeking behaviours. Moreover, national funding and reimbursement policies can also shape healthcare utilisation patterns [51]. Future research could delve deeper into these limitations to further advance understanding and inform targeted health policies.
Conclusions
This scoping review explored the patterns of healthcare utilisation among middle-aged individuals, reiterating that both medical and social determinants influence healthcare behaviours and outcomes across different contexts. Key factors such as multimorbidity and health behaviours were identified. However, the complexity and variability of these factors underscore the need for targeted interventions and further research, with the goal of informing more effective population health policies and practices.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Author contributions
All authors have made substantial contributions to all the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. No writing assistance was obtained in the preparation of the manuscript. The manuscript, including related data, figures and tables has not been previously published, and the manuscript is not under consideration elsewhere. All authors approve the final version of the manuscript, including the authorship list and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Conceptualization, Design and Methodology: QXN, AJAL Data Curation: YN, AJAL, CC. Formal Analysis: YN, AJAL, CC, YLL, HKT, QXN. Investigation: YN, AJAL, CC, QXN. Supervision: CEL, HKT, QXN. Writing – original draft: YN, AJAL, CC, YLL, CEL, HKT, QXN. Writing – review & editing: YN, AJAL, CC, YLL, CEL, HKT, QXN.
Funding
No funding received.
Data availability
Data is provided within the manuscript or supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yong Ng and Abigail Jia Ai Low contributed equally to this work and should be considered co-first authors.
References
- 1.Zayas CE, He Z, Yuan J, Maldonado-Molina M, Hogan W, Modave F et al. Examining Healthcare Utilisation Patterns of Elderly Middle-Aged Adults in the United States. Proceedings of the International Florida AI Research Society Conference Florida AI Research Symposium. 2016;2016:361–6. [PMC free article] [PubMed]
- 2.Older, Australians. Health – service use. Australian Institute of Health and Welfare. 2023. https://www.aihw.gov.au/reports/older-people/older-australians/contents/health/health-care-gps-specialists#Hospitals (last accessed 20 Jul 2024).
- 3.Andersen RM. Revisiting the behavioral Model and Access to Medical Care: does it Matter? J Health Soc Behav. 1995;36(1):1. [PubMed] [Google Scholar]
- 4.Preethi Nagdev, Iyer MR, Naik S, Sanjeev Khanagar, Awawdeh M, Kheraif A, et al. Andersen health care utilisation model: a survey on factors affecting the utilisation of dental health services among school children. PLoS ONE. 2023;18(6):e0286945–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterson J, Pearce PF, Ferguson LA, Langford CA. Understanding scoping reviews. J Am Association Nurse Practitioners. 2017;29(1):12–6. [DOI] [PubMed] [Google Scholar]
- 6.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 7.Definition of MIDDLE AGE. Merriam-webster.com. 2019. https://www.merriam-webster.com/dictionary/middle age (last accessed 24 Jul 2024).
- 8.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 9.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews a Product from the ESRC Methods Programme. 2006. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf (last accessed 24 Jul 2024).
- 11.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (last accessed 24 Jul 2024).
- 12.Alberga A, Holder L, Kornas K, Bornbaum C, Rosella L. Effects of behavioural risk factors on high-cost users of healthcare: a population-based study. Can J Public Health. 2018;109(4):441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edwards CH, Aas E, Kinge JM. Body mass index and lifetime healthcare utilisation. BMC Health Serv Res. 2019;19(1). [DOI] [PMC free article] [PubMed]
- 14.Ezeamama AE, Elkins J, Simpson C, Smith SL, Allegra JC, Miles TP. Indicators of resilience and healthcare outcomes: findings from the 2010 health and retirement survey. Qual Life Res. 2016;25(4):1007–15. 10.1007/s11136-015-1144-y [DOI] [PubMed] [Google Scholar]
- 15.Fazeli Dehkordy S, Hall KS, Dalton VK, Carlos RC. The Link between Everyday discrimination, Healthcare Utilization, and Health Status among a National Sample of women. J Womens Health. 2016;25(10):1044–51. 10.1089/jwh.2015.5522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ishida M, D’Souza M, Zhao Y, Pan T, Carman W, Haregu T, Lee JT. The association between obesity, health service use, and work productivity in Australia: a cross-sectional quantile regression analysis. Sci Rep. 2023;13(1):6696. 10.1038/s41598-023-33389-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee SY, Tsai TI, Tsai YW, Kuo KN. Health literacy, health status, and healthcare utilization of Taiwanese adults: results from a national survey. BMC Public Health. 2010;10:614. 10.1186/1471-2458-10-614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee IC, Chang CS, Du PL. Do healthier lifestyles lead to less utilization of healthcare resources? BMC Health Serv Res. 2017;17(1):243. 10.1186/s12913-017-2185-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Musich S, Wang S, Hawkins K, Klemes A. The impact of Personalized Preventive Care on Health Care Quality, utilization, and expenditures. Popul Health Manag. 2016;19(6):389–97. 10.1089/pop.2015.0171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterson MD, Mahmoudi E. Healthcare utilization associated with obesity and physical disabilities. Am J Prev Med. 2015;48(4):426–35. 10.1016/j.amepre.2014.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rana RH, Alam K, Gow J. Selection of private or public hospital care: examining the care-seeking behaviour of patients with private health insurance. BMC Health Serv Res. 2020;20(1):380. 10.1186/s12913-020-05253-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rasu RS, Bawa WA, Suminski R, Snella K, Warady B. Health Literacy Impact on National Healthcare Utilization and expenditure. Int J Health Policy Manag. 2015;4(11):747–55. 10.15171/ijhpm.2015.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rudisill C, Charlton J, Booth HP, Gulliford MC. Are healthcare costs from obesity associated with body mass index, comorbidity or depression? Cohort study using electronic health records. Clin Obes. 2016;6(3):225–31. 10.1111/cob.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schlichthorst M, Sanci LA, Pirkis J, Spittal MJ, Hocking JS. Why do men go to the doctor? Socio-demographic and lifestyle factors associated with healthcare utilisation among a cohort of Australian men. BMC Public Health. 2016;16(Suppl 3):1028. 10.1186/s12889-016-3706-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sum G, Ishida M, Koh GC, Singh A, Oldenburg B, Lee JT. Implications of multimorbidity on healthcare utilisation and work productivity by socioeconomic groups: cross-sectional analyses of Australia and Japan. PLoS ONE. 2020;15(4):e0232281. 10.1371/journal.pone.0232281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weissman JD, Russell D, Beasley J, Jay M, Malaspina D. Relationships between adult emotional states and indicators of health care utilization: findings from the National Health interview Survey 2006–2014. J Psychosom Res. 2016;91:75–81. 10.1016/j.jpsychores.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 27.Abuduxike G, Aşut Ö, Vaizoğlu SA, Cali S. Health-seeking behaviors and its determinants: a facility-based cross-sectional study in the Turkish Republic of Northern Cyprus. Int J Health Policy Manag. 2020;9(6):240–9. 10.15171/ijhpm.2019.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gong CH, Kendig H, He X. Factors predicting health services use among older people in China: an analysis of the China Health and Retirement Longitudinal Study 2013. BMC Health Serv Res. 2016;16:63. 10.1186/s12913-016-1307-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lam KK, Johnston JM. Health insurance and healthcare utilisation for Shenzhen residents: a tale of registrants and migrants? BMC Public Health. 2012;12:868. 10.1186/1471-2458-12-868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen CM, Nguyen MP, Luc LDP. How public health insurance expansion affects healthcare utilizations in middle and low-income households: an observational study from national cross-section surveys in Vietnam. BMC Public Health. 2023;23(1):624. 10.1186/s12889-023-15500-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pati S, Swain S, Knottnerus JA, Metsemakers JFM, van den Akker M. Magnitude and determinants of multimorbidity and health care utilization among patients attending public versus private primary care: a cross-sectional study from Odisha, India. Int J Equity Health. 2020;19(1):57. 10.1186/s12939-020-01170-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vahedi S, Yazdi-Feyzabadi V, Amini-Rarani M, Mohammadbeigi A, Khosravi A, Rezapour A. Tracking socio-economic inequalities in healthcare utilization in Iran: a repeated cross-sectional analysis. BMC Public Health. 2020;20(1):929. 10.1186/s12889-020-09001-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Z, Li X, Chen M, Si L. Social health insurance, healthcare utilization, and costs in middle-aged and elderly community-dwelling adults in China. Int J Equity Health. 2018;17(1):17. 10.1186/s12939-018-0733-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang Y, Du M, Qin C, Liu Q, Yan W, Liang W, Liu M, Liu J. Associations among socioeconomic status, multimorbidity of non-communicable diseases, and the risk of household catastrophic health expenditure in China: a population-based cohort study. BMC Health Serv Res. 2023;23(1):403. 10.1186/s12913-023-09391-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao Q, Wang J, Nicholas S, Maitland E, Sun J, Jiao C, Xu L, Leng A. Health-Related Quality of Life and Health Service Use among Multimorbid Middle-aged and older-aged adults in China: a cross-sectional study in Shandong Province. Int J Environ Res Public Health. 2020;17(24):9261. 10.3390/ijerph17249261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou Y, Wushouer H, Vuillermin D, Ni B, Guan X, Shi L. Medical insurance and healthcare utilization among the middle-aged and elderly in China: evidence from the China health and retirement longitudinal study 2011, 2013 and 2015. BMC Health Serv Res. 2020;20(1):654. 10.1186/s12913-020-05522-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The World Bank. World Bank Country and Lending Groups. 2024. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (last accessed 26 Jul 2024).
- 38.Zheng L, Peng L. Effect of Major Illness Insurance on vulnerability to poverty: evidence from China. Front Public Health. 2021;9:791817. 10.3389/fpubh.2021.791817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in Health behaviors. Annu Rev Sociol. 2010;36:349–70. 10.1146/annurev.soc.012809.102529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shahid R, Shoker M, Chu LM, Frehlick R, Ward H, Pahwa P. Impact of low health literacy on patients’ health outcomes: a multicenter cohort study. BMC Health Serv Res. 2022;22(1):1148. 10.1186/s12913-022-08527-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reidpath DD, Crawford D, Tilgner L, Gibbons C. Relationship between body mass index and the use of healthcare services in Australia. Obes Res. 2002;10(6):526–31. 10.1038/oby.2002.71 [DOI] [PubMed] [Google Scholar]
- 42.Wijga AH, Mohnen SM, Vonk JM, Uiters E. Healthcare utilisation and expenditure of overweight and non-overweight children. J Epidemiol Community Health. 2018;72(10):940–3. 10.1136/jech-2017-210222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hopman P, Heins MJ, Korevaar JC, Rijken M, Schellevis FG. Health care utilization of patients with multiple chronic diseases in the Netherlands: differences and underlying factors. Eur J Intern Med. 2016;35:44–50. 10.1016/j.ejim.2016.08.025 [DOI] [PubMed] [Google Scholar]
- 44.Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, Murphy AW. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–23. 10.1093/fampra/cmr013 [DOI] [PubMed] [Google Scholar]
- 45.Ziebland S, Rasmussen B, MacArtney J, Hajdarevic S, Sand Andersen R. How wide is the Goldilocks Zone in your health system? J Health Serv Res Policy. 2019;24(1):52–6. 10.1177/1355819618790985 [DOI] [PubMed] [Google Scholar]
- 46.Lachman ME, Teshale S, Agrigoroaei S. Midlife as a pivotal period in the life course: balancing growth and decline at the crossroads of Youth and Old Age. Int J Behav Dev. 2015;39(1):20–31. 10.1177/0165025414533223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.China Kadoorie Biobank Collaborative Group. Healthy lifestyle and life expectancy free of major chronic diseases at age 40 in China. Nat Hum Behav. 2023;7(9):1542–50. 10.1038/s41562-023-01624-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lafortune L, Martin S, Kelly S, Kuhn I, Remes O, Cowan A, Brayne C. Behavioural risk factors in Mid-life Associated with successful ageing, disability, dementia and Frailty in later life: a Rapid systematic review. PLoS ONE. 2016;11(2):e0144405. 10.1371/journal.pone.0144405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crandall JP, Knowler WC, Kahn SE, Marrero D, Florez JC, Bray GA, Haffner SM, Hoskin M, Nathan DM, Diabetes Prevention Program Research Group. The prevention of type 2 diabetes. Nat Clin Pract Endocrinol Metab. 2008;4(7):382–93. 10.1038/ncpendmet0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou X, Siegel KR, Ng BP, Jawanda S, Proia KK, Zhang X, Albright AL, Zhang P. Cost-effectiveness of diabetes Prevention interventions Targeting High-risk individuals and whole populations: a systematic review. Diabetes Care. 2020;43(7):1593–616. [DOI] [PubMed] [Google Scholar]
- 51.Ng QX, Ong C, Chan KE, Ong TSK, Lim IJX, Tang ASP, Chan HW, Koh GCH. Comparative policy analysis of national rare disease funding policies in Australia, Singapore, South Korea, the United Kingdom and the United States: a scoping review. Health Econ Rev. 2024;14(1):42. 10.1186/s13561-024-00519-1. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is provided within the manuscript or supplementary information files.