Abstract
Background
Health systems that are responsive to maternal mental health recognise the importance of integrating mental health services into maternal care. Studies from Vietnam have reported particularly high rates of common perinatal mental health disorders (CPMDs) in both rural and urban areas of the country. Despite the increasing burden of maternal mental health conditions, there is currently no guidance on the screening for CPMDs within maternal care, both antenatal and postnatal. In this paper, we report the findings from a survey that examined health systems responsiveness to the needs of pregnant women at the primary care-level in Vietnam, utilising the WHO’s validated responsiveness questionnaire.
Methods
Cluster sampling was used in two districts, in Bac Giang Province. Data were collected using the WHO responsiveness tool, including questions on the domains of responsiveness relating to pregnant women’s last antenatal visit. SPSS (version 24) software was used for data entry and analysis, respectively. Bivariate and multivariable logistic regression were computed to identify the associated factors of health system responsiveness in maternity care at 95% CI.
Results
We found that the overall mean health systems responsiveness score was 2.86 (out of maximum 4), with 30.4% pregnant women rating responsiveness as “poor” for maternal health care (based on the cutoff point of 60 for overall score). The three highest scoring domains were “social support”, “trust”, and “dignity” and lowest scoring domains were “choice of providers”, “prompt attention”, and “communication”. There is a strong preference for seeking maternal health care at private facilities which meet women’s needs of “confidentiality” and “basic amenities”. Household income was found to have a significant impact on the six responsiveness domains. Finally, only a small proportion of pregnant women self-reported having CPMDs and accessed mental health facilities.
Conclusions
These findings highlight the need to improve the responsiveness of the Vietnamese health system to meet pregnant women’s expectations, mainly in relation to prompt attention and communication. This study also highlights the importance of specifically targeting efforts towards improving the responsiveness of the public health sector. Integrating maternal and mental health at the primary care-level can be one approach to tackle the mental health treatment gap experienced by pregnant women in Vietnam. This can promote early detection and intervention of CPMDs, but may also contribute towards reducing mental health-related stigma.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-12040-6.
Keywords: Mental health, Maternal health, Health systems responsiveness, Common perinatal mental disorders
Background
Health systems responsiveness (HSR) is one of the three intrinsic goals of health system performance, alongside health and fairness of financial contribution [1, 2]. Responsiveness relates to a health system’s ability to respond to the legitimate expectations of users about the non-medical aspects of care [3]. The concept of “health system responsiveness” is central to understanding people’s experiences of their health systems and how these experiences are shaped by the expectations of both service users and health system actors. In this way, peoples’ interactions with and evaluations of their health system is shaped by their initial expectations, as well as past experiences of care [1, 4]. HSR has a direct relationship with service utilisation, coverage and health outcomes (such as maternal mortality), service coverage, while also being influenced by financial protection coverage [1, 5]. HSR can also contribute to ensuring equity in access to quality care [6]. Routine HSR measurement is recommended for monitoring health system’s performance and the results can provide an opportunity for patient voices to be heard within the health care system [5]. This, in turn, can allow policymakers, practitioners, and researchers to anticipate and respond to patients’ existing and future health needs and expectations for better health outcomes.
The World Health Organization’s (WHO) original framework and conceptualisation of responsiveness has been well received by scholars and practitioners alike [7]. Within this conceptualisation, responsiveness is operationalised through the measurement of eight specific elements or domains: autonomy, choice of provider, confidentiality, communication, dignity, prompt attention, quality of basic amenities, and access to social support. The responsiveness of a health system is shaped by the expectations of individuals, families, and the broader community, as well as the health system’s capacity to respond to these expectations [6]. However, the characteristics of health services, peoples’ expectations, and the wider context has not yet received sufficient attention [4].
Mirzoev and Kane [4] proposed a conceptual framework that locates people’s experiences of interacting with their health system at the center of health system responsiveness. This framework includes the seven WHO domains and the additional domain of trust. These domains are important in determining people’s expectations and their decisions about whether to use health services. Two important determinants of people’s experiences of their interaction with health systems are people’s initial expectations (shaped by their characteristics and relationships within their families and communities) and the systems response to these expectations (e.g. through interactions with health providers who, in turn, also engage with policymakers and managers, as well as institutional and organisational arrangements, structures, and resources). In addition, the context (historical, political, cultural, and socioeconomic) is influential in shaping the interactions between the health system and people. Studies revealed that mental illness and medical treatment can undermine the dignity and autonomy of the patients [1] in which responsiveness is increasingly essential for such patients [8]. Health system responsiveness can involve both internal interactions amongst key health system actors, such as policymakers, managers, and providers, as well as external interactions between service users and health facility staff [4, 9]. Mirzoev and Kane’s [4] framework incorporates trust – interpersonal and institutional trust – as the eighth element of responsiveness. However, Valentine et al.’s [6] conceptualisation of responsiveness also acknowledges “clarity of communication” as an important feature of responsive health systems. Clarity of communication implies that providers clearly explain the nature of the illness to patients and their family, required treatment and treatment options, while also allowing sufficient time for patients to understand their symptoms and ask questions. As we explain further below, we incorporated Valentine et al.’s [6] notion of communication within the conceptual framework of responsiveness which guided our inquiry.
Health systems responsiveness has primarily been measured and examined using the corresponding WHO Multi Country Survey Study, structured around the eight domains of responsiveness. The tool asks respondents to rate their most recent encounter with the health system with respect to the eight elements of health systems responsiveness with Likert scale from 1–4 (1 being “very poor’ to 4 corresponding to ‘very good’). The health systems responsiveness questionnaire has been validated and applied in various country contexts, measuring the responsiveness of a range of health services. For instance, Liabsuetrakul et al. [10] examined the responsiveness of delivery care in Southern Thailand finding that women rated prompt attention, dignity, clear communication, and autonomy as particularly important aspects of care which ultimately influenced their choice of delivery facility. More broadly, Kapologwe et al. [11] assessed the responsiveness of primary care facilities in Tanzania finding that all domains of health system responsiveness were rated poorly except for confidentiality and dignity. Additional work by Awoke et al. [12] has highlighted the importance of examining the responsiveness of both public and private health services. In this study, respondents perceived that responsiveness was better in private, for-profit healthcare facilities, with higher wealth and multimorbidity being significant predictors of private healthcare utilisation. However, few studies have assessed health systems responsiveness at the primary care-level. However, some studies have compared health systems responsiveness between public and private providers. While studies have examined the responsiveness of mental health care in a high-income country context [8, 13], few have systematically examined the responsiveness of primary care towards the maternal and mental health needs of pregnant women in a low- and middle-income country context [10, 14].
Vietnam was among six countries that achieved the Millennium Development Goal-5 (MDG5) on reducing maternal mortality in 2015. The maternal mortality ratio (MMR) of the country has also declined considerably over time from 88 in 2000 to 46 in 2020 and is expected to reach the target of the National Action Plan to implement the 2030 Agenda. However, disparities in health outcomes and inequalities in maternal healthcare access and utilisation remain, especially for women from disadvantaged groups, such as those who are ethnic minorities [15]. Several factors can impact maternal mortality, including socioeconomic conditions, cultural and biological concerns, awareness of maternal health and psychological needs, insufficient health workforce numbers and skills, and limited access to maternal health services within the community. Poor maternal health outcomes are reported among women who have limited awareness of maternal health and psychological needs and those who lack access to skilled maternal health services [16]. The interaction of the mother with the healthcare system affects access, utilisation, coverage, as well as the well-being (health outcome) of the individual [10, 14, 17].
Studies from Vietnam have reported particularly high rates of common perinatal mental health disorders (CPMDs) in both rural and urban areas of the country. The prevalence rates of CPMDs, which refer to common mental disorders that occur during pregnancy or in the first year postpartum, range from 16.9%, to as high as 39.9% [18–20]. Multiple studies have highlighted the importance of paying attention to mental health in pregnancy due to the association between increased CPMD symptoms and intimate partner violence [21–23], as well as the normalisation of CPMDs during pregnancy [24] Despite the increasing burden of maternal mental health conditions, Vietnam’s mental health policy was last updated in 1989, with no community- or primary care-level policies addressing mental health [25]. Commune health centers (CHCs) are the first level of primary health care in Vietnam. However, while primary care workers at CHCs are intended to be the main gatekeepers to all mental health services, severe mental health conditions are treated at National and Provincial Psychiatric hospitals [23]. Moreover, there is currently no guidance, within the National Guideline on Reproductive Health Services (2009, 2016), on the screening for CPMDs within antenatal care. As a result, incidents of CPMDs, particularly in rural regions of Vietnam, can be largely overlooked [19]. Integration of maternal and mental health at the primary care-level could be one strategy for improving maternal mental health access and utilisation in Vietnam [26].
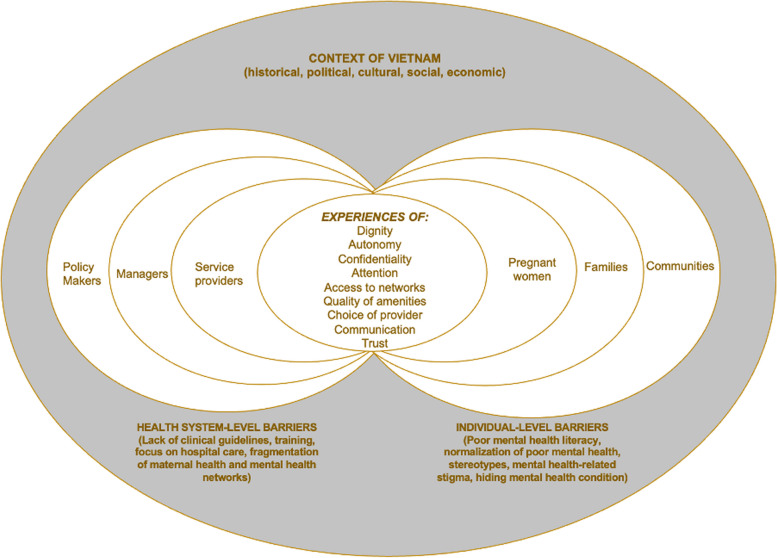
This study uses an adapted version of the Mirzoev and Kane [4] and Valentine et al. framework [6] on HSR to assess the responsiveness of the Vietnamese health system to pregnant women’s maternal and mental health needs (Fig. 1). Pregnant women with mental health needs should have to: (a) recognise their health needs, (b) decide to seek care, and then (c) initiate contact with the system/utilisation, and finally, (d) receive service coverage [6]. Care-seekers’ decisions related to utilisation of healthcare are influenced by three broad factors: (i) the personal context (family and friends, personal beliefs); (ii) providers (therapeutic guidelines/decisions, organisation of delivery, provider attitudes and reputation); and (iii) the perceived health system’s capacity to be responsive to peoples’ needs and expectations.
Fig. 1.
Conceptual framework on Health System Responsiveness in Vietnam. (Adapted from Mirzoev and Kane [4] and Valentine et al. framework [6])
The domains of health systems responsiveness comprise of nine domains covering the non-medical aspects of the interaction between people and their health systems. These domains progress from accessibility (users able to reach and use health services) and acceptability of care (users willing to use accessible services), and are influenced by individual- and system-level barriers.
At an individual-level, several barriers that have been identified in the literature include, poor mental health literacy, the normalisation of mental health or seeking alternative care for mental health, stereotypes of mental illness, a strong fear of mental health-related stigma, concealing one’s mental health condition, as well as self-treatment [24, 27]. Ultimately, these factors can lead to delays in seeking care.
At the health system-level, barriers can include, a lack of clinical guidelines on integrating mental health into routine ANC services and a lack of knowledge and training on mental health among maternal care providers [24, 27]. Other system-wide barriers may include applying a biomedical approach with a focus on hospital treatment of severe mental illness, and fragmented and siloed management and delivery of perinatal mental health [24, 27]. These barriers can lead to pervasive negative healthcare experiences and provider-patient relationships which can, in turn, prevent pregnant women from accessing mental health services. Pregnant women may avoid seeking mental health care altogether due to perceptions of poor treatment during the care encounter, low quality of existing services, or a lack of services in the first place [4, 6, 28]. Enhancing communication within the health system provides a potential entry point for improving responsiveness. Clear communication is associated with dignity, better involvement in decision-making, and, in addition, supports better coverage or access [6].
Previous studies on HSR have been published since 2000, but most of these focus on general health services, delivery care, and individual programmes such as mental health care. Very few have focused on intersecting health domains, such as pregnant women who have sought antenatal care services with mental health needs. Therefore, there is a knowledge gap about pregnant women’s perspectives on the responsiveness of ANC services. The main objective of this study is to assess pregnant women’s perceptions of the responsiveness of the Vietnamese health system to their mental health-related needs. We do so by utilising the WHO’s validated questionnaire on health systems responsiveness. We hope that our results will contribute towards strengthening the responsiveness of primary care in Vietnam to meet pregnant women’s mental health-related needs. We seek to define the measures needed to improve responsiveness which, in turn, can improve overall health system performance.
Methods
Study design and study setting
A cross-sectional survey was conducted in two districts in Bac Giang province, Vietnam, during July–October 2022. Bac Giang is located in northern Vietnam and is comprised of 10 districts and 209 communes. The province has about two million inhabitants and 25% of them are women aged between 15 – 49 [29]. Despite 90% of the population living in rural areas [29], the industrial zones of Bac Giang province are in a stage of rapid development and, as a result, the province has one of the highest gross regional domestic product (GRDP) in Vietnam [30, 31]. The regional minimum wage for Bac Giang varies from 153 and 137 USD/month and monthly average income per capita in 2023 is about 195 USD [32]. The immigration rate is 1.24% with more females moving into the province than males (1.62% vs. 1.15%) [29]. In 2019, the total fertility rate was 2.31, with a national rate of 2.09 [33]. Bac Giang’s healthcare system consists of provincial and district health centers, commune health centers, and other private medical facilities.
Sampling and sample size
A cluster sampling method was applied to estimate and select study participants. In brief, we selected two from eight districts of Bac Giang province to represent urban and rural settings. The population of each district is about 240,000 inhabitants, the urban districts are around 300 km square, while the rural districts are typically 600 km square. Within each district, three communes were randomly selected. Based on the list provided by local commune health centers, all the women who satisfied the inclusion and exclusion criteria in the selected communes were invited to participate to our study. The eligibility criteria for inclusion in this study were: (1) households with pregnant women, (2) aged 18 or older, (3) experienced at least one contact with health clinics (private/public) for their present pregnancy, (4) were living within the study area, (5) consented to participate in the study, (6) were literate, and (7) were able to answer all questions. Those who were excluded were women who were not able to answer the questionnaire (due to physical and/or mental incapacities).
The sample size for the study was determined using a cluster sampling formula of:
wherein n is estimated sample size, Zα/2 is the critical value of the normal distribution at α/2 (Zα/2 = 1.96). p is the estimated value from previous data on the subject for HSR. As there is no local data available, the p was assumed at 50% to get the maximum sample size; the absolute precision (d) = 0.06 and design effects (Deff) of 2, after adding a 10% non-response rate the minimal sample size was estimated to be 587.
Lists of 655 pregnant women in all communes that met the requirements for inclusion in this study were provided by local commune health centers, with 639 participating in this study (97.5% response rate).
Study tool
All data were collected using a questionnaire survey, which was developed based on the instruments used in the WHO’s Multi-Country Survey Study on health systems responsiveness [1]. Questions for the domain on trust were added in line with the conceptualisation of responsiveness by Mirzoev and Kane [4]. The study questionnaire had three parts. The first part included basic socio-demographic questions on characteristics such as age, education, occupation, income, and place of last antenatal care (ANC) visit. In this section, the study participants noted the number of ANC visits that they had during this pregnancy, place of ANC checkup, as well as whether they have experienced any common mental health symptoms such as excessive fears or worries, mood changes, depression, significant tiredness, or low energy in this pregnancy. If they had any symptoms, participants were asked whether they sought medical care or psychoeducation by medical doctors and, in particular, the places where they sought this care (i.e. hospitals at the district- or provincial-level).
The second part of the questionnaire, as per the WHO tool, included 21 sub-domain questions across nine responsiveness domains (the eight WHO domains plus the trust domain) in relation to the pregnant woman’s last ANC visit. Within each domain, the sub-domain questions asked about the specific experiences of pregnant women at their last ANC visit in relation to factors relevant to each domain. For example, in relation to dignity, respondents were asked whether they felt they were treated with respect. The WHO’s eight domains were: dignity (having respectful treatment and communication, four questions), autonomy (having autonomy in making decisions; two questions), confidentiality (having personal information kept confidential, two questions), prompt attention (being attended to promptly, two questions), social support (having access to social support during care, two questions) and basic amenities (having amenities in the healthcare environment, two questions), choice of provider (having a choice of healthcare provider, three questions), clear communication (having the healthcare provider communicate in a way which can be understood, two questions). The ninth domain added for this study asked about trust (confidence in knowledge and skills of healthcare providers in service delivery, two questions). All sub-domain questions required responses on a 4-point scale, either “never” (1), “sometimes” (2), “usually” (3), “always” (4) and converted to “very bad” (1), “bad” (2), “good” (3), “very good” (4), depending on the question and appropriate phrasing required.
Before the main study, a pilot study was conducted with 10 participants, where experts in the field were invited to review the questionnaire. Based on the results of this pilot study, the questionnaire was further refined and this process ensured the content validity of the questionnaire. To ensure equivalence of the original version, a bilingual English-to-Vietnamese translator with medicine, epidemiology, and public health background was asked to perform a back-translation after the English WHO questionnaire had been translated to Vietnamese by a professional. Where differences were noted, the issues were discussed among the two translators, and researchers in the study area.
Data collection
Pregnant women were guided to complete the paper questionnaire themselves by local health workers at their households. The local health workers were trained in data collection skills. Each questionnaire took about 30 min to complete. Data collection was conducted under the supervision of researchers from Hanoi University of Public Health. The collected information was securely kept in a locked cupboard to ensure confidentiality and only researchers could access the data for the research purposes. Before starting the actual data collection, the data collectors performed field practice and pretested the questionnaires on 10 individuals. The data collection tool was modified based on insights and experiences gained from the pretest. In the event of any problems, the researchers discussed them daily and made corrections.
Statistical analysis
The data were checked for completeness and entered into the Epi-data version 4.6 Software Package. Then it was exported to SPSS 24 statistical software packages for cleaning, coding, and analysis. In accordance with the WHO approach in the Multi-Country Survey Study on Health and Responsiveness [34], we scored responsiveness in each domain based on the “rating” question, which was asked only after participants had answered a series of detailed “report” questions related to the relevant domain. A further summary score for “overall responsiveness” was obtained by aggregating all 21 4-scale questions from 9 domains. The responsiveness outcomes were then dichotomised into good responsiveness (combining the very good and good responses) and poor responsiveness (combining the bad, and very bad responses) [35]. For defining the cutoff point for overall HSR, the formula of [(totalhighestscore-totallowestscore)/2 + totallowestscore] was used [36, 37]. Therefore, women with the overall score of 60 or higher was labeled as “good” HSR, and below was considered as “poor” HSR.
Descriptive analysis was used to describe the frequency distribution of each variable. The Chi-square test was employed to compare the differences in overall health systems responsiveness and by domain according to type of health facility and mental health symptoms experienced during current pregnancy. For assessing the difference in the mean of health systems responsiveness score the T-test and ANOVA test were used. The outcome variables were coded as “1” for poor responsiveness in ANC visits whereas “0” for good responsiveness in maternity care. The association between the outcome variables (i.e., poor responsiveness in maternity care and independent variables) was analysed using a logistic regression model. Initially, bivariate logistic regression analysis was performed on all independent variables. Multivariable logistic regression was then performed on variables that had a p-value ≤ 0.25 in the bivariate logistic regression analysis to assess the strength of the relationship between an outcome and several independent variables and to control for potential confounders. The degree of association between independent and dependent variables was assessed using an adjusted odds ratio with a 95% confidence interval. The P–value < 0.05 was considered statistically significant in the multivariable model. Hosmer and Lemeshow’s goodness-of-fit test was used to assess whether the necessary assumptions were fulfilled.
Ethics approval
The study was approved by the Institutional Review Boards of the Hanoi University of Public Health (Decision Number 33/2022-YTCC-HD3), London School of Hygiene and Tropical Medicine (ref 22,981), and the University of Leeds (ref MREC 19–051).
The participants were informed about the purposes, procedures, potential risks, and benefits of the study. Thereafter, written informed consent was obtained from each study participant, before any primary data collection. Confidentiality was maintained throughout the study by excluding personal identifiers, such as names and addresses, from the analysis.
Results
A total of 639 pregnant women participated in the survey. The characteristics of the study participants by health facilities are shown in Table 1. Of the participants, 28.3% were aged between 25–29, about 25% were 20–24 years of age, while only a small number were aged 16–19. Nearly all pregnant women were married (95.8%).
Table 1.
Participants’ characteristics by socio-demographic and type of health facilities (N = 639)
| Characteristics | N (%) |
Commune Health Centers n (%) |
Public district hospital n (%) |
Public provincial and higher n (%) |
Private clinics/ hospital n (%) |
|---|---|---|---|---|---|
| Total | 639 (100%) | 46 (7.2%) | 112 (17.5%) | 17 (2.7%) | 464 (72.6%) |
| Age group | |||||
| 16–19 | 30 (4.7%) | 2 (4.3%) | 3 (2.7%) | 2 (11.8%) | 23 (5.0%) |
| 20–24 | 161 (25.2%) | 6 (13.0%) | 23 (20.5%) | 5 (29.4%) | 127 (27.4%) |
| 25–29 | 181 (28.3%) | 14 (30.4%) | 29 (25.9%) | 2 (11.8%) | 136 (29.3%) |
| 30–34 | 160 (25.0%) | 13 (28.3%) | 42 (37.5%) | 5 (29.4%) | 100 (21.6%) |
| 35- 43 | 107 (16.7%) | 11 (23.9%) | 15 (13.4%) | 3 (17.6%) | 78 (16.8%) |
| Marital status | |||||
| Unmarried/others | 27 (4.2%) | 1 (2.2%) | 1 (0.9%) | 0 (0.0%) | 25 (5.4%) |
| Married | 612 (95.8%) | 45 (97.8%) | 111 (99.1%) | 17 (100.0%) | 439 (94.6%) |
| Education | |||||
| Illiteracy /Primary | 19 (2.3%) | 0 (0.0%) | 4 (3.6%) | 1 (5.9%) | 14 (3.0%) |
| Secondary | 158 (24.7%) | 9 (19.6%) | 28 (25.0%) | 4 (23.5%) | 117 (25.2%) |
| High School | 336 (52.6%) | 22 (47.8%) | 68 (60.7%) | 5 (29.4%) | 241 (51.9%) |
| College + | 126 (19.8%) | 15 (32.6%) | 12 (10.7%) | 7 (41.2%) | 92 (19.8%) |
| Ethnicity | |||||
| Kinh | 573 (89.7%) | 44 (95.7%) | 102 (91.1%) | 14 (82.4%) | 413 (89.0%) |
| Others | 66 (10.3%) | 2 (4.3%) | 10 (8.9%) | 3 (17.6%) | 51 (11.0%) |
| Religion | |||||
| No | 581 (90.9%) | 42 (91.3%) | 104 (92.9%) | 16 (94.1%) | 419 (90.3%) |
| Yes | 58 (9.1%) | 4 (8.7%) | 8 (7.1%) | 1 (6.9%) | 45 (9.7%) |
| Occupation | |||||
| Farmer | 48 (7.5%) | 4 (8.7%) | 7 (6.3%) | 1 (5.9%) | 36 (7.8%) |
| Factory worker | 413 (64.6%) | 27 (58.7%) | 87 (77.7%) | 8 (47.1%) | 291 (62.7%) |
| Public officer | 42 (6.6%) | 3 (6.5%) | 4 (3.6%) | 4 (23.5%) | 31 (6.7%) |
| Freelancer | 111 (17.4%) | 9 (19.6%) | 14 (12.5%) | 4 (23.5%) | 84 (18.1%) |
| Others | 25 (3.9%) | 3 (6.5%) | 0 (0.0%) | 0 (0.0%) | 22 (4.7%) |
| Houshold income (VND/USD) | |||||
| < 2mil/month (80 USD)) | 87 (13.6%) | 10 (21.7%) | 13 (11.6%) | 5 (29.4%) | 59 (12.7%) |
| 2–4 mil/month (80–160) | 374 (58.5%) | 28 (60.9%) | 76 (67.9%) | 10 (58.8%) | 260 (56.0%) |
| 4–6 mil/month (160–240 USD) | 131 (20.5%) | 5 (10.9%) | 21 (18.8%) | 2 (11.8%) | 103 (22.2%) |
| > 6 mil/month (240 USD) | 47 (7.4%) | 3 (6.5%) | 2 (1.8%) | 0 (0.0%) | 42 (9.1%) |
| Gestational age | |||||
| 1st trimester | 86 (13.5%) | 12 (26.1%) | 11 (9.8%) | 2 (11.8%) | 61 (13.1%) |
| 2nd trimester | 334 (52.3%) | 23 (50.0%) | 59 (52.7%) | 8 (47.1%) | 244 (52.6%) |
| 3rd trimester | 219 (34.2%) | 11 (23.9%) | 42 (37.5%) | 7 (41.2%) | 159 (34.3%) |
| Number of children | |||||
| 0 | 184 (28.8%) | 12 (26.1%) | 27 (24.1%) | 6 (35.3%) | 139 (30.0%) |
| 1 child | 226 (35.4%) | 8 (17.4%) | 51 (45.5%) | 3 (17.6%) | 164 (35.3%) |
| 2 children | 176 (27.5%) | 17 (37.0%) | 25 (22.3%) | 7 (41.2%) | 127 (27.4%) |
| 3 + children | 53 (8.3%) | 9 (19.6%) | 9 (8.0%) | 1 (5.9%) | 34 (7.3%) |
Most of the participants were Kinh ethnicity (89.7%) and had no religion (90.9%). About two-thirds were factory workers (64.6%) and freelancers (17.4%), while a small proportion were farmers (7.5%) or public officers (6.6%). Participants’ monthly household income roughly corresponded to the national level with more than a half varying from 2 to 4 million VND (90–180 USD) per month, one-fifth was 4 to 6 million VND per month (180–270 USD), 13.6% was under 2 million VND per month (180 USD) and only 7.4% was more than 6 million VND (270 USD) per month. More than half were in the second trimester (52.3%), about one-third were in the last trimester (34.2%), and a small proportion were in the first trimester of pregnancy (13.5%). More than one-third of the study participants already had one child (35.4%), more than one-fourth stated that this was their first pregnancy (28.8%), and a few participants had more than three children.
Table 2 shows participant’s utilisation of medical services. Private clinics and hospitals were the most common health facilities women visited for pregnancy checkups, accounting for 79% of participants. The district hospital was the next most commonly used facility, accounting for 14.6%, while commune health centers (4.2%) and the national/ provincial hospital (2.2%) accounted for a very small proportion of visits.
Table 2.
Use of medical services
| Frequency | Percentage (95%CI) | ||
|---|---|---|---|
| The most common health facility for ANC | CHC | 27 | 4.2 (2.8–6.1) |
| District hospital | 93 | 14.6 (11.9–17.5) | |
| National/provincial hospital | 14 | 2.2 (1.2–3.7) | |
| Private clinic and hospital | 505 | 79.0 (76.1–82.2) | |
| Health facility for last ANC | CHC | 46 | 7.2 (5.3–9.5) |
| District hospital | 112 | 17.5 (14.7–20.7) | |
| National/provincial hospital | 17 | 2.7 (1.6–4.2) | |
| Private clinic and hospital | 464 | 72.6 (69.0–76.0) | |
| Number of ANC visits during this pregnancy | 1—3 times | 182 | 28.5 (25.0–32.2) |
| 4–6 times | 291 | 45.5 (21.6–49.5) | |
| ≥ 7 times | 166 | 26.0 (22.6–29.6) | |
| Having mental health symptoms | Yes | 66 | 10.3 (8.1–13.0) |
| No | 573 | 89.7 (87.1–91.9) | |
| Use of mental health services | Yes | 7 | 10.6 (4.3–20.6) |
| No | 59 | 89.4 (79.4–95.6) |
The same pattern was reported for the last ANC visit, where most women reported seeking care at private clinics and hospitals and district hospitals, with few women visiting CHCs and the national/provincial hospital (Table 2). About half of the women had 4–6 ANC visits during this pregnancy (45.5%), and around one-fourth had 1–3 or ≥ 7 times (28.5 and 26.0%, respectively). The proportion of women who self-reported having mental health conditions was low (10.3%) and, of these, only 10.6% reported using mental health services. This suggests that a very low number of pregnant women with self-reported mental health issues sought care from mental health services (about 1% overall and 10.6% of respondents were experiencing mental health symptoms).
Table 3 presents health systems responsiveness by type of health facility and self-reported mental health symptoms. The overall average score of health system responsiveness was 2.86 (SD = 0.14). 30.4% of participants rated overall responsiveness as poor, when the cutoff point of 60 for the total core of all items was used. The domain of social support had the highest score as an indicator of health systems responsiveness (3.12 out of a maximum 4) and was ranked as “poor” by only 2.2% of participants. This was followed by trust and basic amenities, with only 4.9% and 8.9% of participants ranking the domains as “poor”, respectively. Choice of provider had the lowest score (2.63) and was considered as “poor” by 49.8% of participants. Prompt attention and communication was ranked as “poor” by 49.8% and 54% of participants, respectively.
Table 3.
Comparison of poor HSR by health facility (N = 639)
| HSR Domain | Poor HSR | Type and level of Health Facility | Having mental health problems during this pregnancy | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Commune health centers | Public district hospital | Public provincial and higher | Private clinics/ hospitals | P-value | Yes | No | P-value | ||
|
N = 639 Mean (SD) |
N= 46 Mean (SD) |
N = 112 Mean (SD) |
N = 17 Mean (SD) |
N = 464 Mean (SD) |
N= 66 Mean (SD) |
N = 573 Mean (SD) |
|||
| Overall | 194 (30.4%) | 15 (32.6%) | 39 (34.8%) | 14 (82.4%) | 126 (27.2%) | < 0.001 | 31 (47%) | 163 (28.4%) | 0.002 |
| 2.86 (0.14) | 2.85 (0.10) | 2.83 (0.14) | 2.67 (1.7) | 2.88 (0.14) | < 0.001 | 2.82 (0.16) | 2.87 (0.14) | 0.150 | |
| Dignity | 179 (28.0%) | 11 (23.9%) | 29 (25.9%) | 7 (41.2%) | 132 (28.4%) | 0.544 | 17 (25.8%) | 162 (28.3%) | 0.667 |
| 2.92 (0.22) | 2.98 (0.22) | 2.90 (0.24) | 2.88 (0.34) | 2.93 (0.21) | 0.160 | 2.91 (0.22) | 2.92 (0.22) | 0.500 | |
| Autonomy | 160 (25.0%) | 11 (23.9%) | 28 (25.0%) | 7 (41.2%) | 114 (24.6%) | 0.485 | 19 (28.8%) | 141 (24.6%) | 0.458 |
| 2.87 (0.26) | 2.86 (0.27) | 2.88 (0.27) | 2.74 (0.36) | 2.87 (0.25) | 0.214 | 2.83 (0.31) | 2.87 (0.26) | 0.282 | |
| Confidentiality | 172 (26.9%) | 20 (43.5%) | 24 (21.4%) | 4 (23.5%) | 124 (26.7%) | 0.041 | 21 (31.8%) | 151 (26.4%) | 0.343 |
| 2.84 (0.33) | 2.73 (0.34) | 2.85 (0.31) | 2.76 (0.44) | 2.85 (0.32) | 0.075 | 2.80 (0.34) | 2.84 (0.33) | 0.338 | |
| Prompt attention | 355 (55.6%) | 15 (32.6%) | 104 (92.9%) | 17 (100%) | 219 (47.2%) | < 0.001 | 36 (54.5%) | 319 (55.7%) | 0.862 |
| 2.64 (0.45) | 2.80 (0.40) | 2.4 (0.31) | 1.35 (0.29) | 2.73 (0.4) | < 0.001 | 2.58 (0.52) | 2.65 (0.44) | 0.230 | |
| Basic amenities | 57 (8.9%) | 7 (15.2%) | 14 (12.5%) | 4 (23.5%) | 32 (6.9%) | 0.013 | 10 (15.2%) | 47 (8.2%) | 0.061 |
| 3.02 (0.33) | 2.97 (0.32) | 2.94 (0.26) | 2.88 (0.42) | 3.05 (0.34) | < 0.001 | 3.02 (0.4) | 3.02 (0.32) | 0.967 | |
| Social support | 14 (2.2%) | 0 (0%) | 0 (0%) | 2 (11.8%) | 12 (2.6%) | 0.011 | 1 (1.5%) | 13 (2.3%) | 0.692 |
| 3.12 (0.33) | 3.12 (0.26) | 3.11 (0.29) | 3.18 (0.5) | 3.12 (0.35) | 0.885 | 3.13 (0.34) | 3.12 (0.33) | 0.817 | |
| Choice | 319 (49.9%) | 32 (69.6%) | 52 (46.6%) | 11 (64.7%) | 224 (48.1%) | 0.022 | 48 (72.7%) | 270 (47.1%) | < 0.001 |
| 2.62 (0.45) | 2.48 (0.47) | 2.68 (0.42) | 2.59 (0.38) | 2.63 (0.46) | 0.076 | 2.46 (0.41) | 2.64 (0.45) | 0.002 | |
| Communication | 345 (54.0%) | 31 (67.4%) | 54 (48.2%) | 12 (70.6%) | 248 (53.4%) | 0.080 | 38 (57.6%) | 307 (53.6%) | 0.537 |
| 2.69 (0.31) | 2.63 (0.29) | 2.71 (0.33) | 2.59 (0.32) | 2.70 (0.30) | 0.213 | 2.66 (0.33) | 2.70 (0.31) | 0.322 | |
| Trust | 31 (4.9%) | 1 (2.2%) | 4 (3.6%) | 2 (11.8%) | 24 (5.2%) | 0.395 | 3 (4.5%) | 28 (4.9%) | 0.93 |
| 3.06 (0.33) | 3.14 (0.38) | 3.02 (0.24) | 3.09 (0.51) | 3.06 (0.34) | 0.222 | 3.03 (0.31) | 3.06 (0.33) | 0.448 | |
Poor HSR in each domain was defined as the average values of all items (4 scale measures) in the domain below 3
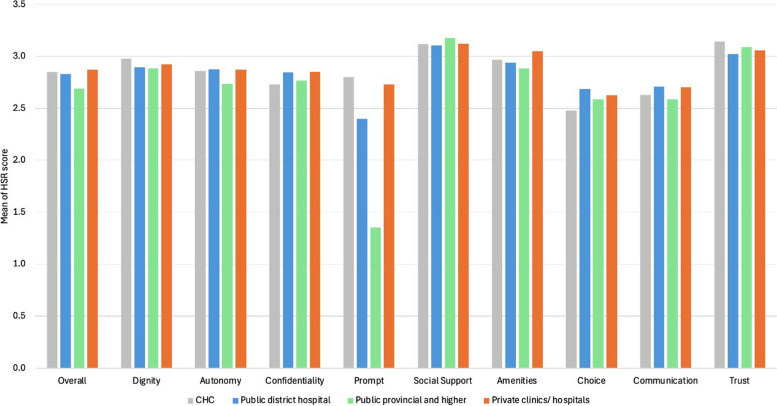
When analysing domain by type of facility, the significant difference of health systems responsiveness was found in confidentiality (p < 0.05), prompt attention (p < 0.001), basic amenities (p < 0.05), social support (p < 0.05), and choice of provider (p < 0.05). The mean HSR score by type of health facility is also presented in Fig. 2. Regarding self-reported mental health symptoms, the significant difference of health systems responsiveness was only observed in the choice of provider domain.
Fig. 2.
Health systems responsiveness score by health facility
The relationship between participants’ characteristics and overall responsiveness performance is highlighted in Table 4 through logistic regression. In the univariate analysis, the age groups, education level, household economic income, level of health facility (commune health center, public district hospitals, public provincial and higher and private clinics/hospitals), and number of ANC visits were factors associated with poor responsiveness, while occupation was not found to relate to poor responsiveness performance. In our multivariate analysis, while people aged 20–43 years-old were less likely to report the poor responsiveness, a significant association was only found in women aged 30–34 (aOR = 0.39; 95%CI = 0.17–0.93). Similarly, women with a higher educational level (those who completed secondary school) had an odds ratio of approximately 0.3 (aOR = 0.33, 95% CI = 0.12–0.90), compared to women who had completed high school (aOR = 0.31, 95% CI = 0.12–0.82). As shown in Table 4, it was found that women were more likely to report the responsiveness of provincial and higher-level facilities as “poor” (aOR = 8.76, 95% CI = 2.13–35.96). “Poor” responsiveness was also more likely to be reported by women who had seven or more ANC visits (aOR = 1.75; CI = 1.07–2.84).
Table 4.
Participants' characteristics and their relations with experience of HSR
| Characteristics | Responsiveness | OR (95% CI) | ||
|---|---|---|---|---|
| Good | Poor | Crude OR | Adjusted ORa | |
| Age group | ||||
| 16–19 | 17 (56.7%) | 13 (43.3%) | Ref | Ref |
| 20–24 | 108 (67.1%) | 53 (32.9%) | 0.64 (0.29–1.42) | 0.66 (0.29–1.51) |
| 25–29 | 121 (66.9%) | 60 (33.1%) | 0.65 (0.29–1.42) | 0.67 (0.29–1.53) |
| 30–34 | 119 (74.4%) | 41 (25.6%) | 0.45 (0.20–1.00) | 0.39 (0.17–0.93) |
| 35- 43 | 80 (74.8%) | 27 (25.2%) | 0.44 (0.19–0.99) | 0.42 (0.17–1.02) |
| Education | ||||
| Illiterate /Primary | 9 (47.3%) | 10 (52.7%) | Ref | Ref |
| Secondary | 112 (70.9%) | 46 (29.1%) | 0.37 (0.14–0.97) | 0.33 (0.12–0.90) |
| High School | 239 (71.1%) | 97 (28.9%) | 0.37 (0.14–0.93) | 0.31 (0.12–0.82) |
| College + | 85 (67.5%) | 41 (32.5%) | 0.43 (0.16–1.15) | 0.40 (0.14–1.12) |
| Occupation | ||||
| Farmer | 29 (60.4%) | 19 (39.6%) | Ref | |
| Worker | 299 (72.4%) | 114 (27.6%) | 0.58 (0.31–1.08) | |
| Public officer | 25 (59.5%) | 17 (40.5%) | 1.04 (0.45–2.41) | |
| Freelancer | 79 (71.2%) | 32 (28.8%) | 0.62 (0.30–1.26) | |
| Others | 13 (52.0%) | 12 (48.0%) | 1.41 (0.53–3.74) | |
| Household income (VND/USD) | ||||
| < 2mil/month (80 USD)) | 52 (59.8%) | 35 (40.2%) | Ref | Ref |
| 2–4 mil/month (80–160) | 267 (71.4%) | 107 (28.6%) | 0.60 (0.37–0.97) | 0.66 (0.40–1.10) |
| 4–6 mil/month (160–240 USD) | 91 (65.9%) | 40(30.5%) | 0.65 (0.37–1.52) | 0.71 (0.39–1.30) |
| > 6 mil/month (240 USD) | 35 (74.5%) | 12 (25.5%) | 0.51 (0.23–1.12) | 0.49 (0.21–1.13) |
| Level of health facility | ||||
| Commune health centers | 31 (67.4%) | 15 (32.6%) | Ref | Ref |
| Public district hospital | 73 (65.2%) | 39 (34.8%) | 1.10 (0.53–2.29) | 1.02 (0.48–2.18) |
| Public provincial and higher | 3 (17.6%) | 14 (82.4%) | 9.64 (2.40–38.76) | 8.76 (2.13–35.96) |
| Private clinics/ hospitals | 338 (72.8%) | 126 (27.2%) | 0.77 (0.40–1.48) | 0.72 (0.37–1.40) |
| Number of ANC | ||||
| 1—3 times | 135 (74.2%) | 47 (25.8%) | Ref | Ref |
| 4–6 times | 207 (71.1%) | 84 (28.9%) | 1.17 (0.77–1.77) | 1.13 (0.73–1.74) |
| > = 7 times | 103 (62.0%) | 63 (38.0%) | 1.76 (1.11–2.77) | 1.75 (1.07–2.84) |
Poor responsiveness was used as reference for all models. The overall HSR was defined as the total score of 21 items (4 scale measures) below 60
OR odd ratio; 95%CI 95% confidence interval; ANC
aAdjusted for age groups, education level, household income, level of health facility, and number of ANC
Table 5 shows the association between socio-demographic characteristics and healthcare setting. The three domains of basic amenities, social support, and trust were not included in this subdomain analysis due to the small number of women reporting these subdomains as “poor”. Therefore, the six domains of responsiveness, namely, dignity, autonomy, confidentiality, prompt attention, choice of provider and communication, were analysed. Income and level of facility were found to have a significant relationship with these domains.
Table 5.
Association of selected characteristics with the HSR by domain
|
Dignity aORa (CI 95%) |
Autonomy aORa (CI 95%) |
Confidentiality aORa (CI 95%) |
Prompt aORa (CI 95%) |
Choice aORa (CI 95%) |
Communication aORa (CI 95%) |
|
|---|---|---|---|---|---|---|
| Age group | ||||||
| 16–19 | Ref | Ref | Ref | Ref | Ref | Ref |
| 20–24 | 0.93 (0.38–2.32) | 0.59 (0.24–1.43) | 1.14 (0.47–2.77) | 100 (0.42–2.38) | 0.66 (0.29–1.53) | 1.03 (0.46–2.28) |
| 25–29 | 1.26 (0.51–3.08) | 0.72 (0.30–1.74) | 1.01 (0.42–2.47) | 0.86 (0.36–2.02) | 0.61 (0.26–1.40) | 1.23 (0.55–2.73) |
| 30–34 | 0.82 (0.33–2.06) | 0.89 (0.37–2.16) | 0.58 (0.23–1.47) | 1.07 (0.44–2.58) | 0.28 (0.12–0.66) | 0.96 (0.43–2.15) |
| 35–43 | 0.97 (0.38–2.49) | 0.95 (0.38–2.36) | 0.76 (0.3–1.96) | 1.01 (0.41–2.48) | 0.37 (0.15–0.89) | 0.97 (0.42–2.25) |
| Education | ||||||
| Illiterate /Primary | Ref | Ref | Ref | Ref | Ref | Ref |
| Secondary | 0.75 (0.28–2.01) | 0.75 (0.26–2.15) | 0.55 (0.19–1.62) | 1.02 (0.35–3) | 0.72 (0.26–1.96) | 0.82 (0.30–2.19) |
| High School | 0.52 (0.20–1.37) | 0.81 (0.29–2.27) | 0.69 (0.25–1.95) | 1.18 (0.41–3.39) | 0.85 (0.32–2.27) | 0.76 (0.29–1.99) |
| College + | 0.61 (0.22–1.70) | 0.94 (0.32–2.76) | 1.17 (0.4–3.43) | 1.22 (0.40–3.68) | 1.21 (0.43–3.38) | 0.86 (0.31–2.37) |
| Household income (VND/USD) | ||||||
| < 2mil/month (80 USD)) | Ref | Ref | Ref | Ref | Ref | Ref |
| 2–4 mil/month (80–160) | 0.80 (0.48–1.33) | 0.74 (0.44–1.26) | 0.59 (0.35–0.98) | 1.26 (0.75–2.13) | 0.45 (0.27–0.74) | 0.53 (0.32–0.88) |
| 4–6 mil/month (160–240 USD) | 0.74 (0.41–1.35) | 0.82 (0.44–1.51) | 0.57 (0.31–1.05) | 1.16 (0.64–2.12) | 0.57 (0.32–1.02) | 0.53 (0.30–0.95) |
| > 6 mil/month (240 USD) | 0.19 (0.06–0.60) | 0.30 (0.11–0.82) | 0.44 (0.19–1.02) | 0.53 (0.23–1.2) | 0.77 (0.35–1.71) | 0.60 (0.28–1.29) |
| Level of health facility for last ANC | ||||||
| CHC | Ref | Ref | Ref | Ref | Ref | Ref |
| District hospital | 1.20 (0.52–2.76) | 0.91 (0.39–2.10) | 0.42 (0.19–0.9) | 26.73 (10.17–70.27) | 0.35 (0.16–0.77) | 0.44 (0.21–0.93) |
| National/provincial hospital | 2.19 (0.65–7.31) | 1.83 (0.54–6.16) | 0.35 (0.10–1.27) | - | 0.59 (0.17–2.03) | 1.07 (0.31–3.71) |
| Private clinics/ hospitals | 1.36 (0.66–2.82) | 1.05 (0.50–2.18) | 0.49 (0.26–0.94) | 1.94 (1.00–3.74) | 0.34 (0.17–0.68) | 0.56 (0.29–1.08) |
| Number of ANC | ||||||
| 1—3 times | Ref | Ref | Ref | Ref | Ref | Ref |
| 4–6 times | 0.71 (0.47–1.08) | 2.22 (1.38–3.57) | 1.04 (0.68–1.60) | 0.94 (0.63–1.41) | 1.57 (1.06–2.33) | 0.87 (0.60–1.28) |
| > = 7 times | 0.76 (0.47–1.24) | 2.24 (1.30–3.86) | 0.87 (0.52–1.45) | 0.93 (0.58–1.51) | 2.00 (1.26–3.16) | 1.52 (0.97–2.39) |
Poor responsiveness was used as reference for all; aOR adjusted Odd Ratios; 95%CI 95% Confidence Interval
aAdjusted for age groups, education level, household income, level of health facility, and number of ANC
Women in the highest household income group (> 6mil/m), which was above the average national income, were more likely to report 81% and 70% lower odds of experiencing poor responsiveness in the domains of dignity and autonomy, respectively, compared to women in the lowest income group. Women with household income similar to national average (2–4 mil/m) were more likely to report 55% and 47% lower odds of experiencing poor responsiveness in the domains of choice of provider (aOR = 0.45, 95%CI = 0.27–0.74) and communication (aOR = 0.53, 95% CI = 0.32–0.88), compared to women in the lowest income group (which is below the national average). Women in the income level (4–6 mil/m) were more likely to report 47% lower odds of experiencing poor responsiveness in the domains of choice of provider (aOR = 0.53, 95%CI = 0.30–0.95), compared to the lowest income group (Table 5).
Further, using ANC service at the district hospital showed reduced odds of poor responsiveness in regard to confidentiality (aOR = 0.42, 95% CI = 0.19–0.9), choice of provider (aOR = 0.35, 95% CI = 0.16–0.77), and communication (aOR = 0.44, 95% CI = 0.21–0.93) compared to commune health centers. Interestingly, we found that, when compared with CHCs, women who used ANC service at the district-level had over 26 times higher odds of experiencing poor responsiveness in the analysis of the prompt attention domain (aOR = 26.73, 95% CI = 10.17–70.27) (Table 5).
Discussion
This study was conducted to determine the level of health system responsiveness, within maternal health care in Vietnam, with regards to pregnant women’s most recent ANC visit. An adapted conceptual framework on HSR, drawing on the work of Mirzoev and Kane [4] and Valentine et al. [6], framed this study. We found that nearly one-third of pregnant women (30.4%) rated “poor” HSR in relation to maternal care, which indicates that a large proportion (30.4%) of pregnant women viewed the maternal health system as unresponsive to their needs.
The lowest-scoring domains in our study were choice of providers, prompt attention, and communication. In contrast to our study’s findings, communication and prompt attention were identified as the highest performing domains in a study conducted in Thailand [10]. This contrast could be attributed to the difference in health service delivery in the two countries, where Thailand’s health system has operated with a focus on patient-oriented care longer than Vietnam. The finding of poor communication within maternal health care in Vietnam could be due to a shortage of staff and a lack of time for communication [24]. This highlights the need to improve health system performance in terms of both the quality and quantity of human resources.
Compared with the first assessment of HSR in Vietnam from a Multi-Country Survey Study in 2000, where dignity (i.e. having respectful treatment and communication) was the highest scoring domain, with pregnant women scoring choice of provider lower at the fourth place [34]. This is also in contrast to other studies conducted in Thailand and Ethiopia, where the domain of dignity was scored highest by women receiving care at maternal health services [10, 17]. This variation may be due to differences in the study setting, design, population, year of the study, as well as training on respectful maternity care received by health staff in these study areas. In the last 20 years, the growth of the private health sector in Vietnam and the emergence of “on-demand” services in public hospitals have potentially meant that pregnant women now expect more patient-oriented and respectful services from the health system [34, 38]. Nevertheless, these results indicate that there is opportunity to strengthen the provision of respectful, dignified maternity care in Vietnam, a key element of responsive health systems.
The domains of health systems responsiveness were rated differently for the various health facilities. Private clinics and hospitals were the most commonly used, with 79% of women visiting private providers for pregnancy check-ups. Women visiting private health facilities rated the domains of confidentiality and basic amenities particularly highly compared to public facilities. A similar finding has been reported in a study conducted in Ethiopia [36]. Although we did not find a significant relationship between private clinics/hospitals and responsiveness domains, these findings are consistent with existing literature which highlights the proliferation of the private sector in Vietnam, a trend that can be traced back to the Doi Moi reforms of the 1980s and 1990s [38, 39]. Private facilities, in particular, aim to maximise their profits and, in order to attract more patients/clients, can thus be more responsive to their needs.
In our study, we found that household income had a significant relationship with all six domains of health systems responsiveness—those with income higher than 2 million VND (80 USD) were more likely to report good health systems responsiveness across all six domains. This was similarly reported in Negash et al.’s [3] study in Ethiopia [36]. HSR can depend on health care expenditure, particularly within the public sector and it is possible that, as financial fairness improves, ratings of HSR could also improve [5, 6, 40, 41]. This suggests the need to improve public health care expenditure for health service users.
In our study, 10.3% of pregnant women reported having a CPMD and, of these, 10.6% accessed mental health services, a finding that is lower compared to other reported data [18–20]. In our study, pregnant women were required to self-report a mental health condition. This could result in an underestimate as women may normalise poor mental health during pregnancy, while also potentially fearing mental health-related stigma [24, 27]. Nevertheless, our study reveals that a low proportion of pregnant women with mental health needs are accessing care, which indicates that there is room for improving the accessibility and utilisation of mental health services at the primary care-level. One of the reasons for this could relate to pregnant women’s decision to seek care in the first place. At an individual-level, self-stigma can contribute towards fear of acknowledging mental health conditions, possibly leading to shame, avoidance of sharing information, and delays in seeking healthcare, with only the severely ill seeking care at psychiatric hospitals [27]. In Vietnam, mental health conditions are typically only treated at higher-level psychiatric hospitals. The lack of mental health care at the primary care-level has therefore been identified as a barrier to accessing mental health care by pregnant women [23, 24]. This can be exacerbated by the siloed provision of maternal and mental health care, highlighting the need for integrating the maternal and mental health networks at primary care-level in Vietnam. Such a strategy may not only promote early detection and intervention of CPMDs, but can also contribute towards reducing mental health-related stigma [28, 42].
Mirzoev and Kane [4] incorporated the domain of trust in their conceptualisation of responsiveness. Our results show that trust is an essential element of responsiveness, further supporting the theoretical work of Mirzoev and Kane [4]. Our analysis also suggests that the responsiveness concept can be applied to specific domains of the health system, such as maternal and mental health care [43]. Further research is needed to examine the responsiveness of maternal mental health services which takes into account the influence of historical, political, social, cultural, and economic contexts, in addition to health system and individual-level factors. Future inquiries should also focus on the needs, expectations, and demands that are particularly important to pregnant women accessing mental health services with consideration of mental health literacy and stigma.
Implications for policy and practice
Our analysis revealed that private clinics and hospitals were the most commonly used facility by women for ANC check-ups. This is consistent with existing literature which suggests that private health facilities in Vietnam are better able to respond to peoples’ increasing expectations, particularly those relating to prompt attention and communication [39]. There is therefore a need to consider investing efforts to improve the responsiveness of the public health system in Vietnam, alongside private sector growth, to meet peoples’ needs and expectations in LMICs [44]. Only a small proportion of pregnant women in our study reported experiencing a mental health condition and fewer still accessed mental health services. This emphasises the need for better integration of maternal mental health at the primary care-level [45]. Such an approach should also involve referring women, diagnosed CPMDs, to specialised mental health services, while also addressing societal and intrapersonal stigma towards mental health conditions [19, 46]. More broadly, previous studies on responsiveness have focused mainly on the evaluation of the responsiveness of entire health systems but, as our analysis suggests, there is also a need to measure the responsiveness of specific services, such as those relating to mental health [43].
This study has some limitations. First, the data was collected only from the patient’s perspective which required some recall information and did not include providers’ perspectives on what constitutes responsive maternal health care. Another limitation of this study is its cross-sectional design, so causation cannot be inferred. There might also be a possibility of recall bias and reporting bias, which could not be avoided for the present design. As Mirzoev and Kane [4] argue, health service users’ expectations of care shape their experiences of their health system interactions and, in this way, evaluations of responsiveness. In particular, expectations that services users deem as ‘legitimate’ [2, 42]. Therefore, in this study, evaluations of responsiveness are likely influenced by what women considered as ‘legitimate’, reasonable expectations of their health systems [42].
Conclusion
This study contributes towards important global research on health system responsiveness and sheds light on pregnant women’s evaluations of their encounters at primary-level maternal health care in Vietnam. While nearly two-thirds of pregnant women viewed their care as responsive, there is still a need to improve the responsiveness of the Vietnamese health system to meet the expectations of pregnant women, mainly in relation to prompt attention and communication. Moreover, the finding that private clinics and hospitals are the most commonly used facilities for antenatal care suggests the importance of specifically targeting efforts towards strengthening the responsiveness of the public health sector. Finally, integrating maternal and mental health at the primary care level can be one approach to tackle the mental health treatment gap experienced by pregnant women in Vietnam. Such an approach may not only promote early detection and intervention of CPMDs, but can also contribute towards reducing mental health-related stigma.
Supplementary Information
Authors’ contributions
Conceptualization, T.M., S.K., B.T.T.H; J.H; A.C, A.M. methodology, T.M., S.K., B.T.T.H; investigation, T.M; S.K; B.T.T.H; data collection, D.T.H.T, L.T.V, N.T.Q.C, L.M.T, L.X.Q data analysis, N.T.H, B.T.TH; L.T.V writing—original draft preparation, N.T.H; B.T.T.H; K.L; writing—review and editing, B.T.TH, K.L, T.M., S.K; project administration, D.T.H.T. All authors have read, reviewed, and agreed to the published version of the manuscript.
Funding
The research reported in this paper received funding from the Joint Health Systems Research Initiative comprising Medical Research Council (MRC), Foreign, Commonwealth & Development Office (FCDO) and Wellcome Trust (grant ref: MR/T023481/2). The views are of the authors only and do not necessarily represent those of the funders.
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Boards of the Hanoi University of Public Health (Decision Number 33/2022-YTCC-HD3), London School of Hygiene and Tropical Medicine (ref 22981), and the University of Leeds (ref MREC 19–051).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Valentine N, Silva A. Health System Responsiveness: Concepts, Domains and Operationalization. 2003.
- 2.World Health Organization. World Health Report 2000. World Health Organization: Geneva; 2000.
- 3.Murray CJ, Frenk J. A framework for assessing the performance of health systems. Bull World Health Organ. 2000;78(6):717–31. [PMC free article] [PubMed] [Google Scholar]
- 4.Mirzoev T, Kane S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ Glob Health. 2017;2(4):e000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valentine NB, Bonsel GJ. Exploring models for the roles of health systems’ responsiveness and social determinants in explaining universal health coverage and health outcomes. Glob Health Action. 2016;9:29329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valentine N, Prasad A, Rice N, Robone S, Chatterji S. Health systems responsiveness: a measure of the acceptability of health-care processes and systems from the user's perspective. In: Mossialos E, Papanicolas I, Smith PC, Leatherman S, editors. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Health Economics, Policy and Management. Cambridge: Cambridge University Press; 2010. p. 138–86.
- 7.Khan G, Kagwanja N, Whyle E, Gilson L, Molyneux S, Schaay N, et al. Health system responsiveness: a systematic evidence mapping review of the global literature. International Journal for Equity in Health. 2021;20(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bramesfeld A, Klippel U, Seidel G, Schwartz FW, Dierks ML. How do patients expect the mental health service system to act? Testing the WHO responsiveness concept for its appropriateness in mental health care. Soc Sci Med. 2007;65(5):880–9. [DOI] [PubMed] [Google Scholar]
- 9.Mirzoev T, Manzano A, Ha BTT, Agyepong IA, Trang DTH, Danso-Appiah A, et al. Realist evaluation to improve health systems responsiveness to neglected health needs of vulnerable groups in Ghana and Vietnam: Study protocol. PLoS ONE. 2021;16(1):e0245755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liabsuetrakul T, Petmanee P, Sanguanchua S, Oumudee N. Health system responsiveness for delivery care in Southern Thailand. Int J Qual Health Care. 2012;24(2):169–75. [DOI] [PubMed] [Google Scholar]
- 11.Kapologwe NA, Kibusi SM, Borghi J, Gwajima DO, Kalolo A. Assessing health system responsiveness in primary health care facilities in Tanzania. BMC Health Serv Res. 2020;20(1):104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Awoke MA, Negin J, Moller J, Farell P, Yawson AE, Biritwum RB, et al. Predictors of public and private healthcare utilization and associated health system responsiveness among older adults in Ghana. Glob Health Action. 2017;10(1):1301723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bramesfeld A, Wedegärtner F, Elgeti H, Bisson S. How does mental health care perform in respect to service users’ expectations? Evaluating inpatient and outpatient care in Germany with the WHO responsiveness concept. BMC Health Serv Res. 2007;7:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayeh Y, Tsehay CT, Negash WD. Health system responsiveness and associated factors for delivery care in public health facilities, Dessie City Administration, South Wollo zone, Ethiopia: Cross-sectional study design. BMJ Open. 2023;13(7):e069655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dinh PL. Maternal Health Services Utilization Among Women of Ethnic Minorities in Vietnam. The Palgrave Handbook of Global Social Problems. Cham: Springer International Publishing; 2021. p. 1–11. [Google Scholar]
- 16.Win PP, Hlaing T, Win HH. Factors influencing maternal death in Cambodia, Laos, Myanmar, and Vietnam countries: A systematic review. PLoS ONE. 2024;19(5):e0293197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdo RA, Halil HM, Kebede BA, Anshebo AA, Ayalew MD, Nedamo SA, et al. Health system responsiveness in maternity care at Hadiya zone public hospitals in Southern Ethiopia: Users’ perspectives. PLoS ONE. 2021;16(10):e0258092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fisher JR, Morrow MM, Ngoc NT, Anh LT. Prevalence, nature, severity and correlates of postpartum depressive symptoms in Vietnam. BJOG. 2004;111(12):1353–60. [DOI] [PubMed] [Google Scholar]
- 19.Abrams D, Nguyen LT, Murphy J, Lee YA, Tran NK, Wiljer D. Perceptions and experiences of perinatal mental disorders in rural, predominantly ethnic minority communities in northern Vietnam. Int J Ment Health Syst. 2016;10:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen PH, Saha KK, Ali D, Menon P, Manohar S, Mai LT, et al. Maternal mental health is associated with child undernutrition and illness in Bangladesh. Vietnam and Ethiopia Public Health Nutr. 2014;17(6):1318–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher J, Tran T, Duc Tran T, Dwyer T, Nguyen T, Casey GJ, et al. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in Vietnamese women: a prospective population-based study. J Affect Disord. 2013;146(2):213–9. [DOI] [PubMed] [Google Scholar]
- 22.Hue MT, Van Nguyet NH, Nha PP, Vu NT, Duc PM, Van Trang NT, et al. Factors associated with antenatal depression among pregnant women in Vietnam: A multisite cross-sectional survey. Health Psychol Open. 2020;7(1):2055102920914076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niemi M, Thanh HT, Tuan T, Falkenberg T. Mental health priorities in Vietnam: a mixed-methods analysis. BMC Health Serv Res. 2010;10:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trang DTH, Ha BTT, Vui LT, Chi NTQ, Thi LM, Duong DTT, et al. Understanding the barriers to integrating maternal and mental health at primary health care in Vietnam. Health Policy Plan. 2024;00:1–11. [DOI] [PMC free article] [PubMed]
- 25.Vietnam Prime Minister. Draft of the National mental health strategy for the period of 2016–2025. 2015.
- 26.World Health Organization. World mental health report. Geneva: Transforming mental health for all; 2022. [Google Scholar]
- 27.Thi LM, Manzano A, Ha BTT, Vui LT, Quynh-Chi NT, Duong DTT, et al. Mental health stigma and health-seeking behaviors amongst pregnant women in Vietnam: a mixed-method realist study. Int J Equity Health. 2024;23(1):163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Viveiros CJ, Darling EK. Perceptions of barriers to accessing perinatal mental health care in midwifery: A scoping review. Midwifery. 2019;70:106–18. [DOI] [PubMed] [Google Scholar]
- 29.Vietnam General Statistic Office. Completed results of the 2019 population and housing census. 2020.
- 30.https://en.bacgiang.gov.vn/detailed-news/-/asset_publisher/MVQI5B2YMPsk/content/bac-giang-in-2023-grdp-growth-reaches-13-45-leading-the-country. Cited 6 Aug 2024.
- 31.https://www.gso.gov.vn/en/px-web/?pxid=E0312&theme=National%20Accounts%20and%20State%20budget. 2024.
- 32.https://www.vietnam-briefing.com/ng-business-guide/vietnam/human-resources-and-payroll/minimum-wage. 2024. Cited 6 August 2024.
- 33.General Statistics Office. Vietnam. The population and housing census 2019. The current status and determinants of fertility in Viet Nam Hanoi. Vietnam; 2021.
- 34.De Silva A, Valentine N, World Health Organization, Global Programme on Evidence for Health P. Measuring responsiveness: results of a key informants survey in 35 countries / Amala de Silva, Nicole Valentine. Geneva: World Health Organization; 2000. [Google Scholar]
- 35.Forouzan S, Padyab M, Rafiey H, Ghazinour M, Dejman M, San SM. Measuring the Mental Health-Care System Responsiveness: Results of an Outpatient Survey in Tehran. Front Public Health. 2015;3:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Negash WD, Tsehay CT, Yazachew L, Asmamaw DB, Desta DZ, Atnafu A. Health system responsiveness and associated factors among outpatients in primary health care facilities in Ethiopia. BMC Health Serv Res. 2022;22(1):249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asefa G, Atnafu A, Dellie E, Gebremedhin T, Aschalew AY, Tsehay CT. Health System Responsiveness for HIV/AIDS Treatment and Care Services in Shewarobit, North Shewa Zone. Ethiopia Patient Prefer Adherence. 2021;15:581–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Minh Thị Hải Võ, Karl Löfgren. An institutional analysis of the fiscal autonomy of public hospitals in Vietnam. Asia and the Pacific Policy Studies. 2018;6(1):90–107.
- 39.Ngo AD, Hill PS. The use of reproductive healthcare at commune health stations in a changing health system in Vietnam. BMC Health Serv Res. 2011;11:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yakob B, Ncama BP. Measuring health system responsiveness at facility level in Ethiopia: performance, correlates and implications. BMC Health Serv Res. 2017;17(1):263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stewart Williams J, Myléus A, Chatterji S, Valentine N. Health systems responsiveness among older adults: Findings from the World Health Organization Study on global AGEing and adult health. Glob Public Health. 2020;15(7):999–1015. [DOI] [PubMed] [Google Scholar]
- 42.Lakin K, Kane S. What can one legitimately expect from a health system? A conceptual analysis and a proposal for research and action. BMJ Glob Health. 2023;8(7): e012453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Njeru MK, Blystad A, Nyamongo IK, Fylkesnes K. A critical assessment of the WHO responsiveness tool: lessons from voluntary HIV testing and counselling services in Kenya. BMC Health Serv Res. 2009;9:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fanelli S, Salvatore FP, De Pascale G, Faccilongo N. Insights for the future of health system partnerships in low- and middle-income countries: a systematic literature review. BMC Health Serv Res. 2020;20(1):571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Do TTH, Bui QTT, Ha BTT, Le TM, Le VT, Nguyen QT, et al. Using the WHO Self-Reporting Questionnaire-20 (SRQ-20) to Detect Symptoms of Common Mental Disorders among Pregnant Women in Vietnam: a Validation Study. Int J Womens Health. 2023;15:599–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thornicroft G, Sunkel C, Alikhon Aliev A, Baker S, Brohan E, El Chammay R, et al. The Lancet Commission on ending stigma and discrimination in mental health. Lancet. 2022;400(10361):1438–80. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its supplementary information files).