Abstract
Background
Despite high coverage of antenatal care (ANC) and family welfare assistant (FWA) visits, emergency contraceptive pill (ECP) awareness is critically low in Bangladesh. We aim to investigate the missed opportunities in generating ECP awareness through ANC and FWA visit programs; and assess the missed opportunities and sociodemographic discrimination in receiving family planning (FP) counseling during ANC.
Methods
We used data from the nationwide Bangladesh Demographic and Health Survey 2017–18. Sample includes 5012 reproductive-aged women who gave live birth in the last 3 years preceding the survey. We used mixed-effect multiple logistic regression considering women nested within clusters to conclude.
Results
Nationally, 79% of women who gave live birth in the last 3 years preceding the survey were unaware of ECP. The estimated missed opportunities in generating ECP awareness was 59.5% in ANC, 0.9% in FWA visits, and 12.3% in both ANC and FWA visits. While FWA visit was not associated with ECP awareness, receiving FP counseling during ANC was significantly associated. About 88.4% of women remained unexposed to FP counseling through ANC during their last pregnancy. Missed opportunities in FP counseling during ANC was 80.4% of which 72% points were from qualified providers. The odds of missed opportunities was not associated with provider type, rather significantly increased among women with low education, lower parity, and poor socioeconomic status.
Conclusions
This study highlights the fragile status of FP counseling during ANC and FWA visits in generating ECP awareness. A prominent provider bias is excluding women of the disadvantageous sociodemographic group from receiving FP counseling.
Keywords: Emergency contraceptive pills, Family planning, Awareness, Antenatal care, Family welfare assistance, Provider bias, Bangladesh
Plain language summary
Emergency contraceptive pill (ECP) awareness is low in Bangladesh, particularly among women with low education, and poor socioeconomic status. However, the extent to which the antenatal care (ANC) and family welfare assistant (FWA) programs fail to generate ECP awareness is never measured.
To address this knowledge gap, we estimated the missed opportunity to generate ECP awareness through ANC and FWA programs. Further, we investigated the missed opportunity and sociodemographic discrimination in receiving family planning counseling during ANC. We scrutinized the Bangladesh Demographic and Health Survey 2017–18 data of 5012 women who gave their last live birth 3 years preceding the survey.
About 73% of women remain unaware of ECP despite receiving ANC or getting FWA visits at home. Family planning counseling during ANC increased ECP awareness but the FWA program did not. Women from rural areas, with low education, limited media exposure, and from lower wealth quintiles are still left unaware of ECP. The missed opportunity of providing family planning counseling during ANC is high (80.4%), particularly among women with low education, lower parity, and poor socioeconomic status.
The study provides valuable insights to the policy planners for rectifying the family planning program of ANC and FWA visits in Bangladesh. Findings reveal the disadvantaged women who know less about ECP and are informed less about family planning during ANC which may help programs to reach the unreached women.
Background
Unintended conception has detrimental consequences on mothers and newborns. Women with unintended conception are less likely to seek essential maternity care, and more likely to have pre-term birth, and adverse psychological outcomes [1–6]. Newborns of unintended conception have a greater risk of being born with low birth weight and dying during infancy [1–6]. Beyond maternal and neonatal outcomes, unintended conception’s consequences affect the entire society’s well-being through adverse social, health, and economic outcomes [6–8].
Bangladesh, the third largest populous country in South Asia and eighth in the world is suffering from 0.27 million (estimated) unwanted births and 0.43 million (estimated) mistimed births every year [9, 10]. Many mistimed and unwanted conceptions often end with abortion which accumulates to a total of 1.2 million abortions every year in Bangladesh [11]. As a result, Bangladesh is now struggling to reduce its TFR which has stagnant at the level of 2.3 since 2011 [12, 13]. In Bangladesh, mistimed births primarily occur among women of young age (< 24 years) and first or second parity, and unwanted births mostly occur at late reproductive age (> 30 years) with high parity [10]. Fifty percent of women in Bangladesh completed their child desire by the age of 26 years and fifty percent underwent menopause by the age of 46 years [10]. This suggests on average, a Bangladeshi woman remains at risk of unwanted birth for 20 years. Uninterrupted FP use throughout these years becomes troublesome because ensuring continuous availability and compliance are challenging.
To avert an unintended conception a woman needs to choose an appropriate FP method based on her child-desire. However, Bangladeshi women are not adopting methods based on their child-desire. For example: women who do not want more children mainly use short-acting modern methods (48%) and traditional methods (13%), or no method (15%). As short-acting methods are widely used, emergency contraceptive pill (ECP) can be a supportive measure alongside the short-acting family planning (FP) methods aimed at averting unwanted births [14]. ECP can be used if there is unprotected intercourse or concerns about possible contraceptive failure from non-compliance such as condom breakage, slippage, 3 or more consecutively missed combined oral contraceptive pills, or 3 days late during the first week of the cycle, more than 7 days late for the combined injectable contraceptive, miscalculation of the abstinence period, failed withdrawal. In such cases, if ECP is administered within 72 h, it exhibits an 89% efficacy rate in averting unintended conception [15].
The World Health Organization (WHO) recommended that all women and girls have a right to access emergency contraception and these methods should be routinely included within all national family planning programs [16]. In line with the WHO recommendation, Bangladesh’s national family planning programs have the provision of counseling on ECP. However, ECP awareness remains critically low (18%) [10], which demands scrutinizing the FP programs. FP counseling has already been introduced as one of the key components of antenatal care (ANC). Hence, the high coverage of ANC (92% received at least one ANC [10]) provides an excellent opportunity to counsel women about ECP. In addition, Bangladesh’s FP program provides door-to-door FP counseling by family welfare assistants (FWAs) [17]. FWA program was first introduced in 1976 [18]. FWAs are permanent female staff under the Directorate General of Family Planning (DGFP) who must have at least 10 years of formal schooling. They are supposed to visit each household in their catchment area once every 2 months. During their visits, they are obliged to register new couples and update the couple registers containing information about all currently married women ages 15–49 and their husbands in their catchment area. The primary responsibilities of FWAs include counseling couples on FP, distributing oral contraceptive pills, condoms and misoprostol, and referring couples to appropriate health facilities if they express interest in long-acting reversible contraceptives or permanent methods.
Despite the high coverage of ANC and FWA visits, ECP awareness is low with large sociodemographic heterogeneity [10] demanding investigation of missed opportunities for generating ECP awareness in ANC and FWA visits. To authors best knowledge, only two national-level studies had identified the correlates of ECP awareness in Bangladesh [19, 20]. None of these studies focused on the missed opportunities in ECP knowledge generation during ANC and FWA visits which are essential in bridging the sociodemographic inequity in ECP awareness. Therefore, this study aims to investigate the missed opportunities in generating ECP awareness through ANC and FWA visit programs. Furthermore, we aim to assess the missed opportunity and sociodemographic discrimination in receiving FP counseling during ANC.
Materials and methods
Data, setting, and participants
We used secondary data from the nationally representative cross-sectional Bangladesh Demographic and Health Survey (BDHS) 2017–2018. The BDHS 2017-18 data was collected using two-stage stratified cluster sampling making the data representative at the administrative division level, as well. As we aimed to examine the missed opportunities in ECP awareness and family planning counseling by FWA and ANC visits, we conducted the analyses on all women (5012) aged 15–49 who gave their most recent live birth 3 years preceding the survey. Figure 1 presents the data flow of the analytical sample.
Fig. 1.
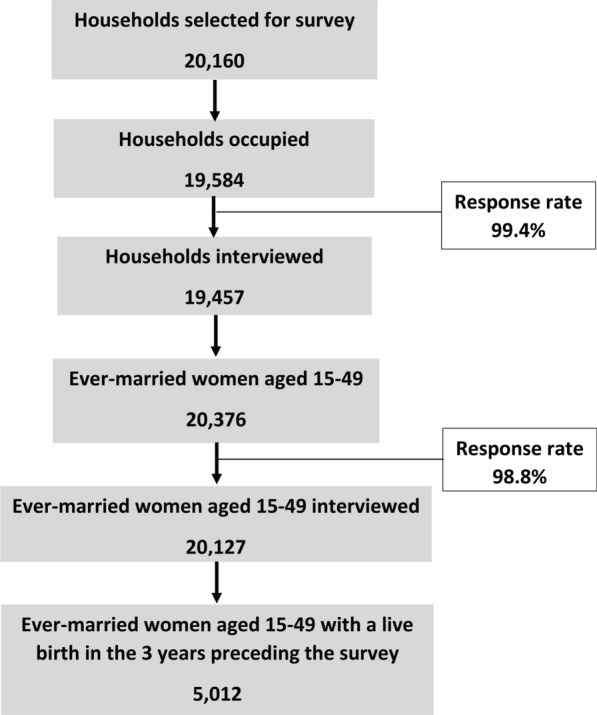
Data flow of the analytical sample
Outcome measures
Outcome variable 1: ECP awareness was the first outcome variable with two categories: aware of ECP (if a woman ever heard about ECP from any source) and unaware of ECP (if a woman never heard about ECP from any source).
Outcome variable 2: We constructed the second binary outcome variable- “missed opportunity in providing FP counseling during ANC” as follows:
missed opportunity (if women had ANC visits but did not receive FP counseling during ANC),
utilized opportunity (if women had ANC visits and received FP counseling during ANC).
Conceptual framework and covariates
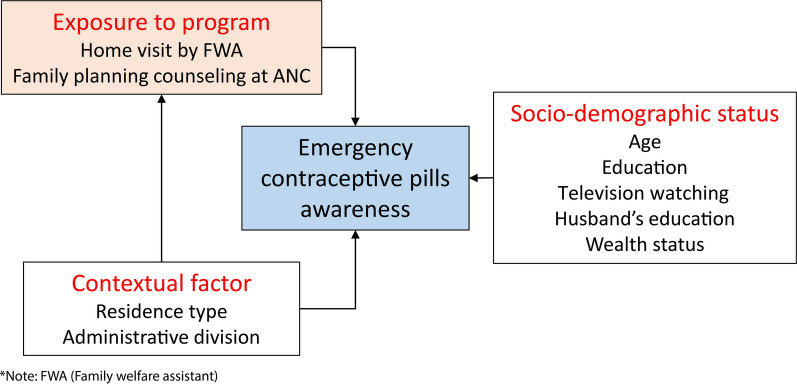
Conceptual framework for outcome 1: We conceptualize that ECP awareness can be influenced by three broad domains: exposure to the FP program, contextual factors, and socio-demographic characteristics (Fig. 2). If a woman is exposed to FP programs like FWA or ANC visits, she may have a higher chance of knowing about ECP than a woman who is unexposed to such programs. Contextual factors shape customs and beliefs of the community which may further influence women’s knowledge about FP methods. For example: A community with conservative customs and beliefs will have less discussion about FP than a community where people are concerned about FP rights and choices. Thus, conservative customs of the community may shape women’s perception and urge of FP which may lessen the chance of knowing about ECP. Contextual factors may further influence ECP awareness through varying intensities of FP programs because FP programs of a region are designed based on the needs of that region. Women from advantageous socio-demographic groups (i.e. better education and wealth, frequent media exposure) may have higher ECP knowledge because of their better exposure to health services and their desire to limit family size.
Fig. 2.
Conceptual framework of emergency contraceptive pills awareness
Covariates for modeling outcome 1: Under each domain, we selected covariates based on earlier studies from Bangladesh [19, 20], Nepal [21], India [22, 23] and Sub-Saharan Africa [24]. The details of the covariates are presented in Table 1. The wealth status was constructed using a principal component analysis based on household goods, which ranged from having a television to having a bicycle or a car, and households’ sources of drinking water, sanitation facilities, and flooring materials. Detailed about household wealth can be found in BDHS 2017–18 final report.
Table 1.
Covariate construction: Definition of all the categories under each covariate
| Covariates | Categories | Definition |
|---|---|---|
| Exposure to the FP program | ||
| Got FWA Visit | No | Woman did not get FWA visit at home in 6 months preceding the survey |
| Yes | Woman got FWA visit at home in 6 months preceding the survey | |
| FP counseling during ANC | Had no ANC visits during last birth | Woman did not receive ANC during last birth |
| Didn’t receive FP counseling during ANC | Woman did not receive FP counseling during ANC for last birth | |
| Received FP counseling during ANC | Woman received FP counseling during ANC for last birth | |
| Contextual factors | ||
| Type of residence | Urban | Reside in urban areas |
| Rural | Reside in rural areas | |
| Administrative division | Dhaka | Reside in Dhaka division |
| Chattogram | Reside in Chattogram division | |
| Barishal | Reside in Barishal division | |
| Khulna | Reside in Khulna division | |
| Mymensingh | Reside in Mymensingh division | |
| Rajshahi | Reside in Rajshahi division | |
| Rangpur | Reside in Rangpur division | |
| Sylhet | Reside in Sylhet division | |
| Socio-demographic characteristics | ||
| Women’s current age | 15–19 | Woman aged 15–19 years |
| 20–24 | Woman aged 15–19 years | |
| 25–29 | Woman aged 25–29 years | |
| 30–34 | Woman aged 30–34 years | |
| 35–49 | Woman aged 35–49 years | |
| Women’s education | No education or primary | No formal education or completed primary-level education only |
| Secondary incomplete | Ever attended class 6–10 but did not complete class 10 | |
| Secondary complete or higher | Completed at least class 10 | |
| Watching Television | Not at all | Does not watch television |
| Less than once a week | Watches television less than once a week | |
| At least once a week | Watches television at least once a week | |
| Husband’s education | No education or primary | No formal education or completed primary-level education only |
| Secondary incomplete | Ever attended class 6–10 but did not complete class 10 | |
| Secondary complete or higher | Completed at least class 10 | |
| Unknown | Husband's educational information is unknown | |
| Household wealth quintile | First | Household belonged to the first wealth quintile group |
| Second | Household belonged to the second wealth quintile group | |
| Third | Household belonged to the third wealth quintile group | |
| Fourth | Household belonged to the fourth wealth quintile group | |
| Fifth | Household belonged to the fifth wealth quintile group | |
| Additional covariates for modeling outcome 2 | ||
| Type of ANC provider | Medically trained provider | Qualified doctor, nurse/midwife/paramedic, family welfare visitor, community skilled birth assistant, and sub-assistant community medical officer |
| Non-medically trained provider | Otherwise | |
| Parity | First | Ever born one child |
| Second | Ever born two children | |
| Third or higher | Ever born three or more children | |
Conceptual framework for outcome 2: We conceptualized that missed opportunities for FP counseling during ANC can be shaped by two broad domains: providers’ characteristics and women’s characteristics. Providers’ perceptions about FP counseling during ANC can be one of the key drivers of counseling. In regards, medically trained providers (MTP) are likely to hold a more positive attitude towards post-partum FP counseling during ANC than non-MTP, maybe because of receiving more training on ANC services. As we aimed to explore whether the providers are being selective in providing FP counseling during ANC, we included broad sociodemographic groups as covariates. As TFR is comparatively high among women from disadvantageous socioeconomic groups like low education, rural residents, and lower wealth quintiles, they may have a higher chance of not receiving FP counseling during ANC. We also hypothesized that women with first or second parity may be less likely to be counseled because providers may emphasize higher parity cases for FP counseling [25, 26].
Covariates for modeling outcome 2: Under the domain provider’s characteristics, BDHS 2017–18 data only allows to include provider type (MTP or non-MTP). BDHS 2017–18 considered qualified doctors, nurses/midwives/paramedics, family welfare visitors, community skilled birth assistants, and sub-assistant community medical officers as medically trained providers. Under sociodemographic characteristics, we included women’s education, number of children ever born, type of residence, administrative division, and wealth quintile.
Statistical analysis
Analysis under objective 1
Firstly, we estimate the missed opportunities in ANC and FWA visits for generating ECP awareness at the national level and then at the divisional level to explore regional variation. Estimation procedures were as follows:
Missed opportunity in ANC visits in generating ECP awareness: This was measured as the percentage of women who had ANC visits in their most recent live birth but never heard about ECP among women who gave their last live birth in 3 years preceding the survey.
Missed opportunity in FWA visits in generating ECP awareness: This was measured as the percentage of women who had FWA visits in the last 6 months preceding the survey but never heard about ECP among women who gave their last live birth in 3 years preceding the survey.
For measuring missed opportunity we used “all women who gave live birth in 3 years preceding the survey” as the denominator because this will reflect where FP awareness could reach if all contact points could reach their highest mark.
Secondly, we estimated the prevalence of ECP awareness across the factors considered under each domain. As BDHS 2017–18 used a cluster sampling design, we used a mixed-effect multiple logistic regression model considering random intercept at the cluster level to examine the factors associated with ECP awareness. The random intercept model can deal with the hierarchical nature of the clustered data by incorporating both fixed effects and random effects at the cluster level. These random effects capture the variation across clusters by explicitly modeling the clustering structure and fixed effects represent the average relationship between the predictors and the response variable across all clusters.
Analysis under objective 2
Firstly, we estimated the missed opportunities for FP counseling during ANC by providers’ type (medically trained and untrained) at the national level and then at the divisional level to explore regional variation. Missed opportunity in FP counseling during ANC was estimated as the percentage of women who had ANC visits in their most recent live birth but did not receive FP counseling among women who gave their last live birth 3 years preceding the survey. For measuring missed opportunity we used “all women who gave live birth in 3 years preceding the survey” as the denominator because this will reflect where FP awareness could reach if all contact points could reach their highest mark.
Secondly, we measured missed opportunities among “women who had ANC visits for their most recent birth” to understand whether the providers are being selective in providing FP counseling during ANC. We also used a mixed-effect multiple logistic regression considering women nested within clusters to examine the factors associated with missed opportunities in FP counseling during ANC.
To reduce bias, we incorporated appropriate sampling weights that adjusted for the complex survey design characteristics of BDHS. For all the statistical analyses, we used Stata V.14.0 (Stata SE V.14, Stata Corp., College Station, Texas, USA).
Results
Sample characteristics
About 53% of women were aged 15–24, only 6% were uneducated, and more than one-third did not watch television, 13.6% women’s husbands were uneducated, and 73% were from rural areas (Table 2). Only 16.4% got FWA visits, 82% received ANC from MTP, and 11.5% received FP counseling during ANC.
Table 2.
Percentage distribution of women across different sociodemographic groups and program exposure
| Factors | Number of women | Percentage distribution of women |
|---|---|---|
| Overall | 5012 | 100.0 |
| Women’s current age | ||
| 15–19 | 869 | 17.9 |
| 20–24 | 1773 | 35.2 |
| 25–29 | 1310 | 25.9 |
| 30–34 | 749 | 15.1 |
| 35–49 | 311 | 5.9 |
| Women’s education | ||
| No education | 312 | 6.3 |
| Up to primary complete | 1392 | 27.6 |
| Secondary incomplete | 2136 | 43.7 |
| Secondary complete or higher | 1172 | 22.4 |
| Watching television | ||
| Not at all | 1907 | 36.4 |
| Less than once a week | 442 | 9.3 |
| At least once a week | 2663 | 54.3 |
| Husband’s education | ||
| No education | 679 | 13.6 |
| Up to primary complete | 1657 | 33.6 |
| Secondary incomplete | 1366 | 28.0 |
| Secondary complete or higher | 1231 | 23.8 |
| Unknown | 79 | 1.5 |
| Parity | ||
| First | 1915 | 38.2 |
| Second | 1638 | 32.8 |
| Third or higher | 1459 | 29.0 |
| Household wealth quintile | ||
| First | 1079 | 20.6 |
| Second | 1017 | 20.5 |
| Third | 905 | 19.2 |
| Fourth | 988 | 20.2 |
| Fifth | 1023 | 19.5 |
| Type of residence | ||
| Urban | 1725 | 26.8 |
| Rural | 3287 | 73.2 |
| Administrative division | ||
| Dhaka | 741 | 25.6 |
| Barishal | 533 | 5.7 |
| Chattogram | 835 | 21.2 |
| Khulna | 524 | 9.2 |
| Mymensingh | 603 | 8.5 |
| Rajshahi | 527 | 11.6 |
| Rangpur | 559 | 10.6 |
| Sylhet | 690 | 7.6 |
| Got FWA visit | ||
| No | 4233 | 83.6 |
| Yes | 779 | 16.4 |
| Type of ANC provider | ||
| Medically trained provider | 4100 | 81.9 |
| Non-medically trained provider | 504 | 10.1 |
| Had no ANC during last birth | 408 | 8.0 |
| FP counseling during ANC | ||
| Didn’t receive FP counseling during ANC | 4011 | 80.5 |
| Received FP counseling during ANC | 593 | 11.5 |
| Had no ANC during last birth | 408 | 8.0 |
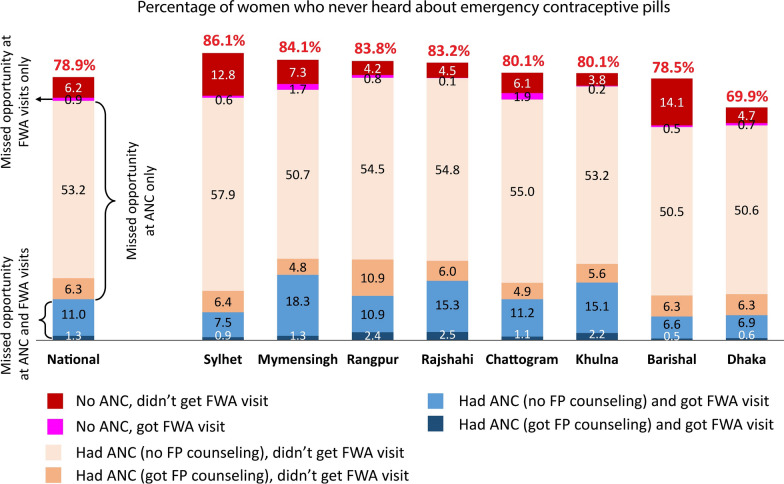
Missed opportunities to generate ECP awareness during ANC and FWA visits
Nationally, 78.9% of women who gave live birth in the last 3 years preceding the survey were unaware of ECP (Fig. 3). However, only 6.2% of women were unexposed to ANC or FWA visits and remained unaware of ECP. The estimated missed opportunities in generating ECP awareness were 59.5% in ANC, 0.9% in FWA visits, and 12.3% in both ANC and FWA visits. The level of missed opportunity collectively in ANC and FWA visits was around 75% in all the divisions except for Dhaka (65.2%) and Barishal (64.4%).
Fig. 3.
Percentage of women who never heard about emergency contraceptive pills among women aged 15–49 who gave live birth 3 years preceding the BDHS 2017–18
Prevalence and factors associated with ECP awareness
Only one-fifth (21.1%) of the women who had a live birth 3 years preceding the survey ever heard about ECP (Table 3). The prevalence of ECP awareness did not differ by FWA visit. Importantly, only one-third of the women who received FP counseling during ANC were aware of ECP. However, this was higher compared to women who did not receive FP counseling during ANC (34.2% vs. 20.2%). Urban women were more aware of ECP than rural women (31.9% vs. 17.1%). ECP awareness was monotonically increased by women’s and their husbands’ education and household wealth.
Table 3.
Prevalence and factors associated with ECP awareness among women aged 15–49 who gave live birth three years preceding the BDHS 2017–18 (n = 5012)
| Factors | Prevalence1 | AOR | 95% CI |
|---|---|---|---|
| Overall | 21.1 | ||
| Got FWA visit | |||
| No | 21.5 | Reference | |
| Yes | 19.0 | 1.14 | (0.89, 1.44) |
| FP Counseling during last birth | |||
| Didn’t receive FP Counseling during ANC | 20.2 | Reference | |
| Received FP Counseling during ANC | 34.2 | 1.53** | (1.19, 1.97) |
| Had no ANC during last birth | 11.0 | 1.20 | (0.77, 1.87) |
| Type of residence | |||
| Urban | 31.9 | Reference | |
| Rural | 17.1 | 0.77* | (0.61, 0.95) |
| Administrative division | |||
| Dhaka | 30.1 | Reference | |
| Barishal | 21.5 | 1.07 | (0.75, 1.52) |
| Chattogram | 19.9 | 0.59** | (0.42, 0.82) |
| Khulna | 19.9 | 0.68* | (0.47, 0.99) |
| Mymensingh | 15.9 | 0.68* | (0.48, 0.96) |
| Rajshahi | 16.8 | 0.61* | (0.41, 0.90) |
| Rangpur | 16.2 | 0.64* | (0.43, 0.94) |
| Sylhet | 13.9 | 0.66* | (0.47, 0.91) |
| Women’s current age | |||
| 15–19 | 15.1 | Reference | |
| 20–24 | 22.4 | 1.31* | (1.01, 1.69) |
| 25–29 | 23.0 | 1.45* | (1.08, 1.93) |
| 30–34 | 22.6 | 1.50** | (1.11, 2.03) |
| 35–49 | 18.8 | 1.49 | (0.97, 2.28) |
| Women’s education | |||
| No education or primary | 9.7 | Reference | |
| Secondary incomplete | 18.2 | 1.48** | (1.17, 1.88) |
| Secondary complete or higher | 43.9 | 3.18** | (2.35, 4.30) |
| Watching television | |||
| Not at all | 10.9 | Reference | |
| Less than once a week | 19.2 | 1.68** | (1.23, 2.29) |
| At least once a week | 28.2 | 1.62** | (1.26, 2.09) |
| Husband’s education | |||
| No education or primary | 10.4 | Reference | |
| Secondary incomplete | 21.5 | 1.62** | (1.28, 2.05) |
| Secondary complete or higher | 42.2 | 2.44** | (1.83, 3.24) |
| Unknown | 10.6 | 0.88 | (0.37, 2.05) |
| Household wealth quintile | |||
| First | 7.3 | Reference | |
| Second | 12.6 | 1.38 | (0.94, 2.00) |
| Third | 17.9 | 1.51* | (1.04, 2.18) |
| Fourth | 24.3 | 1.56* | (1.05, 2.33) |
| Fifth | 44.2 | 2.52** | (1.63, 3.89) |
1Percentage of women heard about ECP among women aged 15–49 who gave live birth 3 years preceding the BDHS 2017–18; *p < 0.05, **p < 0.01; AOR: Adjusted odds ratio; CI: Confidence interval
The results of the multivariable regression suggest no significant association between FWA visit and ECP awareness (Table 3). However, a strong positive association between FP counseling during ANC and ECP awareness was noticed. The odds of ECP awareness was 53% higher (AOR: 1.53, 95% CI 1.19–1.97) among women who received FP counseling during ANC than those who did not receive FP counseling during ANC. The odds of ECP awareness was 3 times (AOR: 3.18, 95% CI 2.35–4.30) among women with secondary or higher levels of education in reference to women with no or primary level education. In addition, residing in urban areas, frequently watching television, higher educational level of husbands, belonging to middle or upper quintiles were associated with higher odds of ECP awareness.
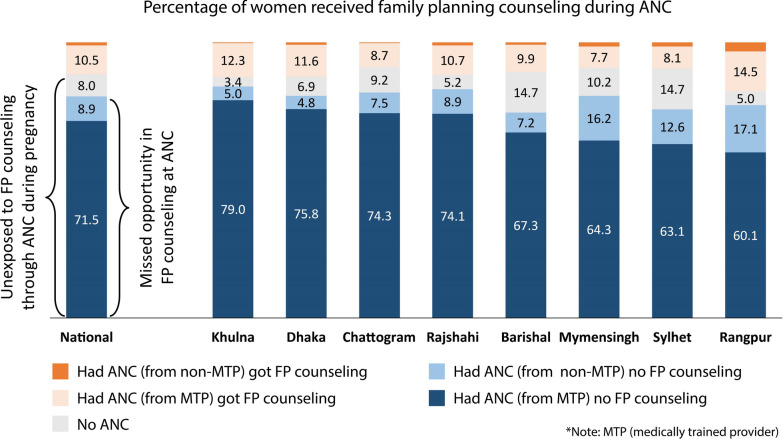
Missed opportunities for family planning counseling during ANC
Figure 4 displays the status of FP counseling during ANC. The majority of women (88.4%) who gave their last live birth in 3 years preceding the survey remained unexposed to FP counseling through ANC during their last pregnancy. The missed opportunity in FP counseling during ANC was 80.4%. Devastatingly, missed opportunity from medically trained providers was 72%. Missed opportunity remains around 80% across divisions.
Fig. 4.
Percentage of women received family planning counseling during ANC for their most recent live birth among women aged 15–49 who gave live birth 3 years preceding the BDHS 2017–18 (n = 5012)
For readers’ convenience, we have addressed ANC-taker women as “women” while interpreting Table 4. The overall prevalence of missed opportunities in FP counseling during ANC (among ANC-takers) was 87.4% and it was above 80% across all the socio-demographic groups. The prevalence of missed opportunities was similar among women who received ANC from MTO and non-MTO providers. A higher prevalence of missed opportunities was observed among women with low education, first parity, residing in rural, and from bottom wealth quintile.
Table 4.
Prevalence and factors associated with not receiving family planning counseling during ANC among women aged 15–49 who had ANC visits for the most recent live birth 3 years preceding the BDHS 2017–18 (n = 4604)
| Factors | Prevalence1 | AOR | 95% CI |
|---|---|---|---|
| Type of ANC provider | |||
| Medically trained provider | 87.3 | Reference | |
| Non-medically trained provider | 88.8 | 0.93 | (0.64, 1.37) |
| Women’s education | |||
| Secondary complete or higher | 81.0 | Reference | |
| Secondary incomplete | 88.9 | 1.91** | (1.46, 2.51) |
| No education or primary | 90.3 | 2.23** | (1.61, 3.09) |
| Parity | |||
| Third or higher | 87.2 | Reference | |
| Second | 86.9 | 1.23 | (0.93, 1.62) |
| First | 88.1 | 1.53** | (1.15, 2.03) |
| Type of residence | |||
| Urban | 84.8 | Reference | |
| Rural | 88.5 | 1.20 | (0.94, 1.52) |
| Administrative division | |||
| Dhaka | 86.6 | Reference | |
| Chattogram | 90.3 | 1.45 | (1.00, 2.11) |
| Barishal | 87.3 | 0.90 | (0.58, 1.39) |
| Khulna | 87.2 | 0.87 | (0.59, 1.30) |
| Mymensingh | 89.8 | 1.10 | (0.72, 1.69) |
| Rajshahi | 87.7 | 0.88 | (0.55, 1.41) |
| Rangpur | 81.2 | 0.50** | (0.34, 0.75) |
| Sylhet | 89.0 | 1.02 | (0.63, 1.64) |
| Household wealth quintile | |||
| Fifth | 82.4 | Reference | |
| Fourth | 87.3 | 1.29 | (0.93, 1.78) |
| Third | 88.4 | 1.38 | (0.98, 1.93) |
| Second | 89.7 | 1.49* | (1.01, 2.20) |
| First | 89.8 | 1.56* | (1.03, 2.36) |
1Percentage of women did not receive family planning counseling during ANC among women aged 15–49 who had ANC visits for most recent live birth 3 years preceding the BDHS 2017–18; *p < 0.05, **p < 0.01; AOR: Adjusted odds ratio; CI: Confidence interval
Results from the multivariable regression in Table 4 reveal the group of women whom we are significantly deprived of FP counseling during ANC. Unpleasantly, the odds of missed opportunities was not significantly lower among women who took ANC from MTO than non-MTO. The odds of missed opportunities was 2 times (AOR: 2.23, CI 1.61–3.09) among the women with no or primary education compared to women with secondary completed or higher education. Women of first parity had 53% greater odds of not receiving FP counseling than women with third or higher-order parities. The odds of missed opportunities were respectively 49% (AOR: 1.49, CI 1.01–2.20) and 56% (AOR: 1.56, CI 1.03–2.36) higher among women from the first and second wealth quintiles compared to women from the highest quintile.
Discussion
Main findings
Effective use of ECP could lessen the heavy burden of unintended conception in Bangladesh. Despite the high coverage of ANC and FWA visits, ECP awareness remains critically low here. The first objective of this study was to investigate the missed opportunities in generating ECP awareness through ANC and FWA visit programs. Using the national level data, we found huge missed opportunities in generating ECP awareness through ANC and FWA programs. In addition, regression analysis revealed that family planning counseling during ANC helped increase ECP awareness but the FWA program did not. The second objective was to assess the missed opportunities and sociodemographic discrimination in receiving FP counseling during ANC. We found a tremendously high level of missed opportunities in FP counseling during ANC; particularly among women with low education, lower parity, and poor socioeconomic status. These findings may aid in the development of a targeted service delivery model that could potentially improve the quality of FP counseling resulting in adequate knowledge and effective use of ECP among reproductive-aged women.
Social inequity in ECP awareness
The deep-rooted sociocultural beliefs and norms often influence people’s perceptions of contraception, particularly in rural areas of LMICs where education is not optimal. Additionally, socio-religious values can limit discussions on contraception, further limiting awareness. We found substantial social inequity in ECP awareness. Women from rural areas, with low education, limited media exposure, and from lower wealth quintiles were less aware of ECP which is consistent with the earlier studies from BDHS 2014 [19, 20].
Despite being a patriarchal Muslim-majority LMIC, Bangladesh remarkably reduces its TFR by uplifting modern contraceptive use. The knowledge of modern contraceptive methods is now almost universal among Bangladeshi married women. Women who are not using a method, none are left unaware of contraceptive methods [27]. There is no differential in modern method use between rural and urban areas (54% vs. 55%) [27]. Thus, the urban–rural inequity in ECP awareness may be attributable more to the differentials in programmatic factors rather than the differentials in socio-cultural beliefs and norms between rural and urban. For example: less internet access and scarcity of social marketing campaigns could be the possible drivers of low ECP awareness among rural women [28]. Girls from rural areas and poor households are still vulnerable to child marriage, which limits their educational attainment. This disadvantageous group has high child wantedness. Thus, may have limited search for contraceptive methods which possibly left them unaware of ECP [29]. In addition, ECP is a costly FP method compared to other methods, making it less familiar to poor people.
Missed opportunity to generate ECP awareness
The limited ECP awareness despite receiving ANC and FWA visits signals the fragile status of ECP counseling during these programs. FWA programs started in 1976 with 23,500 FWAs when the population was 78.8 million [18]. By 2017, the number of FWAs reduced to approximately 19,600 with the population increasing more than 2 times [17]. Thus, FWAs are now in serious human resource scarcity which may have severely affected the quality of counseling [30]. In a recent study providers mentioned human resource scarcity as one of the main reasons for limited FP counseling during ANC [31]. This human resource scarcity could be attributed to limited counseling on ECP despite high coverage of services uptake.
When the scope of counseling is limited, providers may choose a limited number of methods he/she is more convinced to discuss with women. Literature shows that provider bias often stems from their perception of contraception methods on future fertility [32, 33]. A systematic review from low and middle-income countries revealed widespread misconceptions among providers, including the abortifacient perception of ECP or that access to it would increase sexual activity among adolescents [32]. However, we cannot certainly conclude whether such perceptions from Bangladeshi providers restrict them from providing counseling on ECP in ANC and FWA visits.
Missed opportunities for FP counseling in ANC
In addition to ECP, overall FP counseling is low during ANC. We found that even MTPs are not providing FP counseling, which warrants scrutinizing the ANC programs. Literature shows that providers referred to human resource scarcity, patient load within a short time, and women’s unwillingness to hear FP during ANC as the main reasons for not counseling [31]. Studies also showed that ANC providers from the Government Upazila Health Complex (UHC) perceived treating pregnancy complications as their main responsibility, and FP counseling is the responsibility of the Family Planning Division [31]. In addition, both providers from UHC and mothers perceived that the pregnancy period is not suitable for discussing FP [31].
Moreover, inadequate training of the providers could also be attributed to limited FP counseling. Bangladesh Health Facility Survey 2022 revealed the fragile status FP training. In 40% of public facilities that offer modern FP methods, all the interviewed staff never received any training in some aspect of FP [34]. Above this, only 20% of these facilities had at least one interviewed staff who received FP training in past 2 years [34].
Sociodemographic discrimination in receiving FP counseling at ANC
In Bangladesh, most of the short-spaced, mistimed, and unwanted pregnancies are concentrated among less educated, rural, and poor women [35]. Our findings also reveal their limited FP counseling reception. FP conversation during ANC should be initiated by the provider, but in many cases, it is often initiated by clients (women) in Bangladesh. Thus, limited FP urge and inquiry from the disadvantageous (less educated, poor) mothers might subside FP conversation during ANC. In addition, educated women may better recall the FP counseling during ANC than less educated women because they have more urge to FP than less educated women. One possible reason for low FP counseling reception among low-parity mothers is that ANC providers find FP counseling easier for higher-parity women because they (women) have a fear of another child [31].
Strength and limitations
The main strengths of this study include the use of DHS data that ensures the quality of the questionnaire, representativeness of the sample at the national and divisional levels, high response rate (99%), and data completeness (100%). The use of survey weight and survey design characteristics of the BDHS 2017–18 reduces the bias from the estimates and yields robust standard error of the estimates. This study may also be affected by recall bias. Only a small proportion of mothers have to recall a maximum of 3 years back to report whether they received FP counseling during ANC. The magnitude of the recall period bias is possibly similar for all sociodemographic groups because the recall period depends on the time since the last birth which is unlikely to vary among sociodemographic groups.
Policy implication of findings
Findings highlight critical gaps and opportunities within Bangladesh’s reproductive health programs. The findings of this study involve two strong policy implications.
Enhanced integration of FP counseling in ANC services: Findings reveal the catastrophic missed opportunity to provide FP counseling and generate ECP awareness during ANC visits. This underscores the need to enhance training and resources for healthcare providers involved in ANC services. Operational plans of the Health Sector Program should prioritize comprehensive FP counseling as a core component of ANC disregarding the sociodemographic characteristics of pregnant women.
Reform and strengthening of the FWA Program: Findings reveal the ineffectiveness of the FWA program to improve ECP awareness which warrants re-evaluating and reinforcing the program’s training modules, outreach strategies, and accountability mechanisms.
Conclusions
This study highlights the substantial missed opportunity to generate ECP awareness through ANC and FWA programs. Increasing human resources and provider knowledge of ECP can significantly contribute to offsetting some of the provider bias and thus improving ECP awareness among women [33]. Further investigation is also recommended to better understand the reasons for missed opportunities. Moreover, findings reveal the disadvantaged women who know less about ECP and are informed less about FP during ANC which may help policies reach the unreached women.
Acknowledgements
We acknowledge the National Institute of Population Research and Training, ICF International, USA, and Mitra and Associates, who conducted this nationwide survey. Finally, icddr,b is grateful to the Government of the People’s Republic of Bangladesh and Canada for providing core/unrestricted support.
Abbreviations
- TFR
Total fertility rate
- ECP
Emergency contraceptive pill
- FP
Family planning
- ANC
Antenatal care
- FWA
Family welfare assistant
- BDHS
Bangladesh demographic and health survey
- MTP
Medically trained providers
- UHC
Upazila Health Complex
Author contributions
M.M.R. conceptualized the research problem. T.A. compiled data and performed the formal analysis under the guidance of M.M.R. S.N.E performed the literature review. T.A., S.S.S., S.I.S., and M.T.A. prepared the original draft. M.M.R. critically reviewed and provided constructive supervision. T.A. and M.T.A. revised and edited the final draft. All authors read and approved the final manuscript.
Funding
This study is non-funded.
Availability of data and materials
This study used secondary data from Bangladesh Demographic and Health Survey 2017–18. The dataset can be obtained from the DHS website (https://dhsprogram.com/data/available-datasets.cfm) and it is publicly available upon reasonable request.
Declarations
Ethics approval and consent to participate
This study used publicly available secondary data, so no Ethics Committee or Institutional Board approval is required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Marston C, Cleland J. Do unintended pregnancies carried to term lead to adverse outcomes for mother and child? An assessment in five developing countries. Popul Stud. 2003;57(1):77–93. [DOI] [PubMed] [Google Scholar]
- 2.Eggleston E, editor Unintended pregnancy and use of prenatal care in Ecuador. In: Annual meeting of the American Public Health Association, Washington, DC, Nov; 1998.
- 3.Chinebuah B, Pérez-Escamilla R. Unplanned pregnancies are associated with less likelihood of prolonged breast-feeding among primiparous women in Ghana. J Nutr. 2001;131(4):1247–9. [DOI] [PubMed] [Google Scholar]
- 4.Dye TD, Wojtowycz MA, Aubry RH, Quade J, Kilburn H. Unintended pregnancy and breast-feeding behavior. Am J Public Health. 1997;87(10):1709–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32(1):152–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown SS, Eisenberg L. Unintended pregnancy and the well-being of children and families. JAMA. 1995;274(17):1332. [DOI] [PubMed] [Google Scholar]
- 7.Singh S, Sedgh G, Hussain R. Unintended pregnancy: worldwide levels, trends, and outcomes. Stud Fam Plann. 2010;41(4):241–50. [DOI] [PubMed] [Google Scholar]
- 8.Klima CS. Unintended pregnancy: consequences and solutions for a worldwide problem. J Nurse Midwifery. 1998;43(6):483–91. [DOI] [PubMed] [Google Scholar]
- 9.Khan S, Haider MM, Jamil K, et al. The double burden of malnutrition among Bangladeshi women: Rethinking the country’s maternal and child health programs and policies. Data for impact. 2022.
- 10.National Institute of Population Research and Training (NIPORT), and ICF. Bangladesh Demographic and Health Survey 2017–18. 2020. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF.
- 11.Singh S, Hossain A, Maddow-Zimet I, Vlassoff M, Bhuiyan HU, Ingerick M. The incidence of menstrual regulation procedures and abortion in Bangladesh, 2014. Int Perspect Sex Reprod Health. 2017;43(1):1–11. [DOI] [PubMed] [Google Scholar]
- 12.Worldometer. Bangladesh Population. Available: https://www.worldometers.info/world-population/bangladesh-population/#:~:text=Bangladesh%20ranks%20number%208%20in,(and%20dependencies)%20by%20population. [Accessed 10 Nov 2023].
- 13.National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. Bangladesh Demographic and Health Survey 2011. 2013. Dhaka, Bangladesh and Calverton, Maryland, USA: NIPORT, Mitra and Associates, and ICF International.
- 14.Trussell J, Rodríguez G, Ellertson C. Updated estimates of the effectiveness of the Yuzpe regimen of emergency contraception. Contraception. 1999;59(3):147–51. [DOI] [PubMed]
- 15.Shohel M, Rahman MM, Zaman A, Uddin MMN, Al-Amin MM, Reza HM. A systematic review of effectiveness and safety of different regimens of levonorgestrel oral tablets for emergency contraception. BMC Womens Health. 2014;14(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Fact sheets: Emergency contraception. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/emergency-contraception.
- 17.Perry H. Health for the people: National community health worker programs from Afghanistan to Zimbabwe. Washington, DC: USAID; 2020. [Google Scholar]
- 18.Stoeckel J, Piet-Pelon N. Bangladesh family planning programlme. 1997. [DOI] [PubMed]
- 19.Ahmed MS, Yunus FM. Factors associated with knowledge and use of the emergency contraceptive pill among ever-married women of reproductive age in Bangladesh: findings from a nationwide cross-sectional survey. Eur J Contracept Reprod Health Care. 2021;26(3):195–201. [DOI] [PubMed] [Google Scholar]
- 20.Mahfuzur MR, Alam MR, Billah MA. Determinants of emergency contraceptive pill use in Bangladesh: an analysis of national survey data. Asian Pac J Reprod. 2022;11(2):62–9. [Google Scholar]
- 21.Chaudhary S. Knowledge, attitude and practice towards emergency contraceptive pills and factors hindering its use among females of reproductive age group visiting urban health centre at Rajbiraj, Nepal. Int J Reprod Contracept Obstet Gynecol. 2022;11(3):676–82. [Google Scholar]
- 22.Narzary PK. Sexual exposure and awareness of emergency contraceptive pills among never married adolescent girls in India. J Soc Devel Sc. 2013;4(4):164–73. [Google Scholar]
- 23.Arora P, Scott K, Balabanova D. Do Indian women know about and use the emergency contraceptive pill? An analysis of nationally representative data from 2005–06 and 2019–21. Health Policy and Planning. 2023;38(Suppl 2):ii51. [DOI] [PMC free article] [PubMed]
- 24.Awopegba OE, Chukwudeh OS, Owolabi EO, Ajayi AI. Trends in emergency contraception awareness among women and girls in 28 sub-Saharan countries. BMC Public Health. 2021;21:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dieci M, Wagner Z, Friedman W, Burgess S, Vandermark J, McCoy SI, et al. Measuring family planning provider bias: a discrete choice experiment among Burkinabé, Pakistani, and Tanzanian providers. Stud Fam Plann. 2021;52(3):299–320. [DOI] [PubMed] [Google Scholar]
- 26.Solo J, Festin M. Provider bias in family planning services: a review of its meaning and manifestations. Global Health Sci Pract. 2019;7(3):371–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute of Population Research and Training (NIPORT) and ICF. 2024. Bangladesh Demographic and Health Survey 2022: Final Report. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF.
- 28.Hossain SM, Khan M, Vernon R, Keesbury J, Askew I, Townsend J, et al. ECP handbook: Introducing and mainstreaming the provision of emergency contraceptive pills in developing countries. 2009.
- 29.Hakizimana S, Odjidja EN. Beyond knowledge acquisition: factors influencing family planning utilization among women in conservative communities in Rural Burundi. Reprod Health. 2021;18(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hossain MB, Khuda B-E, Phillips JF. The effects of outreach on perceived quality of care in two rural areas of Bangladesh. J Biosoc Sci. 2004;36(5):507–22. [DOI] [PubMed] [Google Scholar]
- 31.Rahman MM, Haider MM, Barman P, Imam MA, Khan S, Alam A, Nahar Q, Shams Z, Begum NN, Rahman M. Assessment of a postpartum family planning intervention in selected areas of Bangladesh. Chapel Hill, NC, USA: Data for Impact. 2023.
- 32.Dawson A, Tran N-T, Westley E, Mangiaterra V, Festin M. Workforce interventions to improve access to emergency contraception pills: a systematic review of current evidence in low-and middle-income countries and recommendations for improving performance. BMC Health Serv Res. 2015;15:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Judge S, Peterman A, Keesbury J. Provider determinants of emergency contraceptive counseling and provision in Kenya and Ethiopia. Contraception. 2011;83(5):486–90. [DOI] [PubMed] [Google Scholar]
- 34.National Institute of Population Research and Training (NIPORT) and icddr,b (International Center for Diarrhoeal Disease Research, Bangladesh). 2024. Bangladesh Health facility Survey 2022. Dhaka, Bangladesh: NIPORT and icddr,b.
- 35.Roy TK, Singh BP. Correlates of unwanted births in Bangladesh: a study through path analysis. PLoS ONE. 2016;11(10): e0164007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study used secondary data from Bangladesh Demographic and Health Survey 2017–18. The dataset can be obtained from the DHS website (https://dhsprogram.com/data/available-datasets.cfm) and it is publicly available upon reasonable request.