Abstract
Background
In April 2023, quality of life (QOL) and quality of care experience (QCE) indicators were introduced as mandatory indicators in Australian residential aged care (RAC) to measure and monitor wellbeing and consumer experience respectively. In this study, we used data for the initial four months after their introduction to describe QOL and QCE scores, explore related factors and assess variations by completion mode and facility.
Methods
A retrospective cohort study using electronic data (Mar–Jun 2023) from 1,772 residents in 22 RAC facilities in metropolitan Sydney, Australia. QOL was measured by the Quality of Life-Aged Care Consumer (QOL-ACC) scale, and QCE by the Quality of Care Experience-Aged Care Consumer (QCE-ACC) scale, both through three completion modes: self, interviewer-facilitated and proxy completion. Propensity score matching was used to compare QOL/QCE differences by completion mode; multilevel ordinal logistic regression to investigate QOL-/QCE-related factors; and funnel plots to explore facility-level score variations.
Results
Of 1,772 residents, 1,706 completed the QOL-ACC survey and 1,686 the QCE-ACC. The median score was 21 (interquartile range 18–24) for QOL and 23 (interquartile range 20–24) for QCE, both indicating ‘excellent’ outcomes. The leisure activities component of QOL, and social relationships and complaint lodging of QCE, were rated relatively lower than other dimensions. The scores of both indicators were significantly higher for self-completion versus other completion modes. Significant variation in QOL and QCE scores by facility were also observed, with seven and four facilities with lower-than-expected proportions of residents with ‘excellent’ or ‘good’ ratings of QOL and QCE, respectively. A longer length of stay (odd ratio [OR] = 0.70, 95% CI: 0.53–0.92 for ≥ 3 years of stay versus < 1 year of stay) and fall history (OR = 0.74, 95% CI: 0.60–0.91) were associated with lower QOL, while having a visual impairment (OR = 0.74, 95% CI: 0.55–0.99) and fall history (OR = 0.80, 95% CI: 0.64–0.99) were associated with lower QCE.
Conclusion
We found high QOL and QCE across the 22 Australian RAC facilities. Enhancing residents’ leisure activities, social relationships, and addressing specific needs (e.g., visual impairment and fall history) may enhance QOL and QCE.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05472-6.
Keywords: Quality of life, Quality of care experience, Residential aged care, Propensity score matching, Multilevel ordinal logistic regression
Introduction
The Australian population is ageing, with proportions of older adults (i.e., aged ≥ 65) and the oldest old (i.e., aged ≥ 80) projected to reach 23.8% and 8.7%, respectively, by 2050 [1]. With an ageing population, particularly those at very old age, demand for aged care services will increase considerably in Australia, with an estimated 3.5 million older Australians expected to access aged care services by the middle of this century [2]. Consequently, attention is growing over how to provide sufficient, safe and high-quality care services to older adults to ensure they age with dignity [3]. Concerns are particularly strong within residential aged care (RAC), where care recipients are generally very old and frailer than those community-dwelling [4, 5]. Such concerns are further intensified in the context of recent investigations from the Australian Royal Commission into Aged Care Quality and Safety, which highlighted many failings in the Australian RAC sector (e.g., substandard care, neglect and elder abuse) [6–8].
To better measure and monitor quality of care and services delivered in the aged care sector, the Australian Government initiated the National Aged Care Mandatory Quality Indicator Program (QI program) in 2019, requiring RAC service providers to report on a range of indicators of quality of care (e.g., falls, weight loss and pressure injuries) on a quarterly basis [9]. These QIs were developed in consultation with the aged care sector and experts, measuring critical areas of care that can affect the health and wellbeing of RAC users. In 2023, as a response to the Royal Commission’s recommendations, the QI program has more than doubled its number of indicators from five to eleven, adding six additional indicators into its quality assessments [10].
Among the newly introduced indicators of the QI program, were quality of life (QOL) and quality of care experience (QCE), two key indicators that reflect RAC users’ ratings of their overall wellbeing status and quality of care received [9]. The inclusion of these two indicators extends the quality assessment from purely clinical domains to encompass both clinical and non-clinical aspects that transcend health [11]. Adding these indicators also fills an important gap in the Australian aged care’s quality monitoring system, which had been lacking routine data collection of QOL, a crucial component of aged care quality monitoring that has been achieved in many other developed countries, such as the United States, the United Kingdom, Canada and New Zealand [12].
The mandatory data collection on QOL and QCE for Australia’s RAC providers commenced from 1st April 2023, providing an opportunity to gain insights into the less-investigated care recipients’ ratings of QOL and quality of care in the Australian RAC sector. Using the initial four-month QI data sourced from a large RAC provider in Australia, this study aimed to: (1) examine QOL and QCE of RAC facility residents to establish a baseline understanding of the QOL and QCE among Australian aged care sector (Subsections 3.2 and 3.3), (2) examine any differences in the two indicators by completion mode and facility to identify how the method of data collection and variations between facilities may influence residents’ QOL and QCE scores (Subsections 3.2, 3.3, and 3.4), and (3) explore factors associated with variations in scores of QOL and QCE to identify key demographic, clinical, and contextual factors that contribute to differences in QOL and QCE scores (Subsection 3.5). These insights are crucial for enhancing resident well-being, informing policy and practice improvements, and guiding future QI data collection and QOL/QCE monitoring in aged care settings.
Data and methods
Study design and setting
This was a retrospective cohort study using routinely collected aged care data from 22 RAC facilities in New South Wales, Australia. The study period was from 1st March 2023 to 30th June 2023. The starting date of the study period was earlier than the inaugural reporting date of the new QI program (i.e., 1st April 2023) because the RAC service provider adopted the scales early to allow staff to adapt to the new data collection/reporting requirements. This study was approved by Macquarie University Human Research Ethics Committee (No.52019614412614).
Participants and data sources
We used routinely collected data containing resident profile data and information on the two indicators. The profile dataset provided information of residents regarding demographic characteristics (e.g., age and sex), admission records (e.g., resident/RAC facility ID) and information on 20 health conditions at the time of admission (see Table 1). The QOL and QCE datasets comprised information of resident ID, date of collection, residents’ responses to each dimension of QOL and QCE, total score and completion mode.
Table 1.
Characteristics of residents and by completion mode
| All (n = 1,772) |
Residents with completed QOL-ACC data (n = 1,706) | Residents with completed QCE-ACC data (n = 1,686) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Interviewer-facilitated (n = 1,082) |
Proxy-completion (n = 333) |
Self-completion (n = 291) |
p
value |
Interviewer-facilitated (n = 1,012) |
Proxy-completion (n = 336) |
Self-completion (n = 338) |
p
value |
|||
| Female, n (%) | 1,180(66.6) | 704(65.1) | 225(67.6) | 211(72.5) | 0.054 | 653(64.5) | 226(67.3) | 239(70.7) | 0.105 | |
| Age, median (IQR) | 88(82–93) | 87(82–93) | 88(82–93) | 88(83–93) | 0.238 | 87(82–93) | 88(82–93) | 89(83–93) | 0.025 | |
| Age category, n (%) | ||||||||||
| 65–79 | 315(17.8) | 191(17.7) | 57(17.1) | 50(17.1) | 0.534 | 187(18.4) | 60(17.8) | 58(17.2) | 0.095 | |
| 80–84 | 288(16.3) | 187(17.3) | 52(15.6) | 40(13.8) | 181(17.9) | 55(16.4) | 40(11.8) | |||
| 85–89 | 449(25.3) | 286(26.4) | 82(24.6) | 71(24.4) | 262(25.9) | 78(23.2) | 87(25.7) | |||
| ≥ 90 | 720(40.6) | 418(38.6) | 142(42.7) | 130(44.7) | 382(37.8) | 143(42.6) | 153(45.3) | |||
| Length of stay (days), median (IQR) | 591(284-1,388) | 576(290-1,348) | 730(288-1,606) | 563(273-1,387) | 0.208 | 570(290-1,327) | 757(296-1,578) | 563(260-1,451) | 0.204 | |
| Entry type, n(%) | ||||||||||
| Permanent | 1,749(97.6) | 1054(97.4) | 329(98.8) | 282(96.9) | 0.247 | 987(97.5) | 333(99.1) | 324(96.0) | 0.052 | |
| Respite | 43(2.4) | 28(2.6) | 4(1.2) | 9(3.1) | 25(2.5) | 3(0.9) | 14(4.0) | |||
| Health status, n (%) | ||||||||||
| Circulatory disease, any | 1550(87.5) | 947(87.5) | 288(86.5) | 258(88.7) | 0.715 | 887(87.6) | 290(86.3) | 300(88.8) | 0.627 | |
| Diabetes | 460(26.0) | 288(26.6) | 74(22.2) | 79(27.1) | 0.238 | 280(27.7) | 74(22.0) | 87(25.7) | 0.123 | |
| Chronic respiratory disease | 314(17.7) | 214(19.8) | 36(10.8) | 56(19.2) | 0.001 | 202(20.0) | 37(11.0) | 62(18.3) | 0.001 | |
| Neoplasms/cancer | 480(27.1) | 279(25.8) | 83(24.9) | 99(34.0) | 0.012 | 263(26.0) | 84(25.0) | 107(31.7) | 0.085 | |
| Dementia | 770(43.5) | 418(38.6) | 235(70.6) | 86(29.6) | < 0.001 | 403(39.8) | 238(70.8) | 96(28.4) | < 0.001 | |
| Parkinson’s disease | 146(8.2) | 80(7.4) | 36(10.8) | 24(8.2) | 0.139 | 73(7.2) | 40(11.9) | 26(7.7) | 0.023 | |
| Depression, mood & affective disorders | 726(41.0) | 443(40.9) | 143(42.9) | 109(37.5) | 0.370 | 410(40.5) | 143(42.6) | 132(39.1) | 0.646 | |
| Anxiety & stress-related disorders | 498(28.1) | 293(27.1) | 102(30.6) | 78(26.8) | 0.417 | 278(27.5) | 102(30.4) | 95(28.1) | 0.595 | |
| Renal disease | 305(17.2) | 180(16.6) | 65(19.5) | 44(15.1) | 0.312 | 170(16.8) | 64(19.0) | 55(16.3) | 0.570 | |
| Arthritis | 943(53.2) | 578(53.4) | 183(55.0) | 150(51.5) | 0.696 | 540(53.4) | 184(54.8) | 184(54.4) | 0.879 | |
| Osteoporosis | 521(29.4) | 310(28.7) | 107(32.1) | 84(28.9) | 0.465 | 289(28.6) | 103(30.7) | 101(29.9) | 0.733 | |
| Fracture | 563(31.8) | 334(30.9) | 111(33.3) | 98(33.7) | 0.531 | 318(31.4) | 103(30.7) | 113(33.4) | 0.714 | |
| Hearing impairment | 347(19.6) | 202(18.7) | 67(20.1) | 63(21.6) | 0.493 | 187(18.5) | 73(21.7) | 67(19.8) | 0.417 | |
| Visual impairment | 252(14.2) | 153(14.1) | 52(15.6) | 38(13.1) | 0.651 | 145(14.3) | 55(16.4) | 42(12.4) | 0.344 | |
| Fall history | 784(44.2) | 465(43.0) | 170(51.1) | 119(40.9) | 0.016 | 449(44.4) | 164(48.8) | 136(40.2) | 0.081 | |
| Faecal incontinence | 252(14.2) | 126(11.6) | 89(26.7) | 21(7.2) | < 0.001 | 132(13.0) | 84(25.0) | 25(7.4) | < 0.001 | |
| Urinary Incontinence | 307(17.3) | 185(17.1) | 56(16.8) | 54(18.6) | 0.816 | 168(16.6) | 61(18.2) | 66(19.5) | 0.443 | |
| Double incontinence | 191(10.8) | 90(8.3) | 77(23.1) | 12(4.1) | < 0.001 | 97(9.6) | 70(20.8) | 17(5.0) | < 0.001 | |
| Constipation | 217(12.2) | 124(11.5) | 59(17.7) | 26(8.9) | 0.002 | 118(11.7) | 58(17.3) | 36(10.7) | 0.013 | |
| Urinary tract infection | 306(17.3) | 179(16.5) | 74(22.2) | 38(13.1) | 0.008 | 169(16.7) | 73(21.7) | 47(13.9) | 0.022 | |
Note: 1, IQR denotes interquartile range; 2, QCE-ACC: Quality of Care Experience-Aged Care Consumer; QOL-ACC: Quality of Life-Aged Care Consumer; 3 p-value is based on analysis of variance for numeric variables and Chi-square test for categorial variables
A total of 2,489 residents lived in the 22 RAC facilities over the study period. The average survey completion rate was approximately 68% among the 22 RAC facilities, with a range from 27 to 91% (see Supplementary Table 1 for facility variations of completion rate). The reasons for low completion rates in some facilities may include residents being absent from the service for the entire quarter or choosing not to complete the QOL/QCE assessment. Additionally, as this was the first four months of QOL and QCE data collection, some facilities may have been slow to respond and implement the changes.
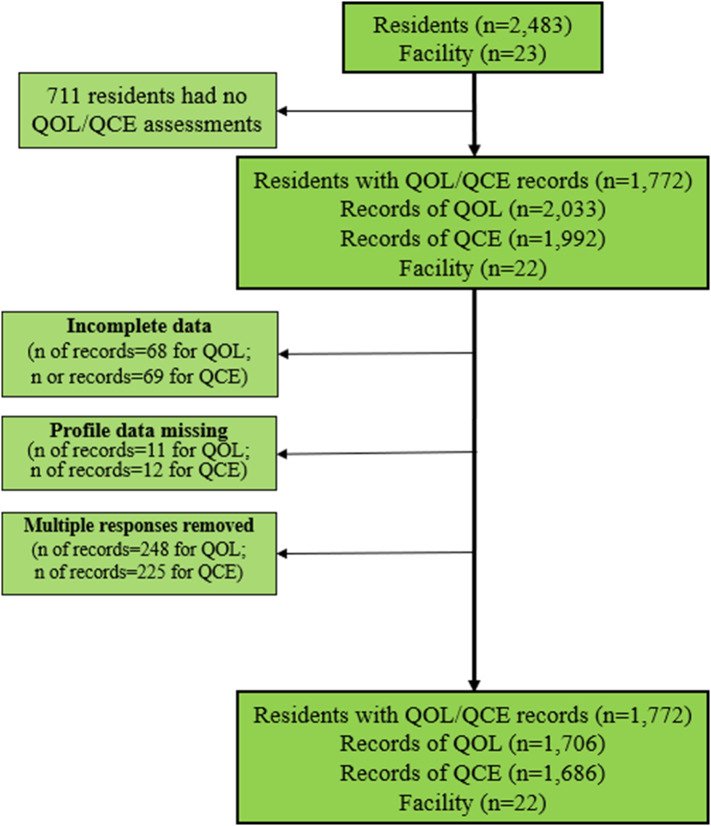
All residents with ≥ 1 QOL/QCE questionnaire completed were eligible for inclusion, producing 2,033 records of QOL and 1,992 records of QCE from 1,772 participants. We excluded records with incomplete data (n = 68 for QOL and n = 69 for QCE) and with missing profile data (e.g., demographic characteristics) (n = 11 for QOL and n = 12 for QCE).1 We used the latest record for those residents with multiple records, excluding 248 non-latest records of QOL and 225 of QCE. The final sample included 1,706 records of QOL and 1,686 records of QCE for subsequent analysis (see Fig. 1 for sample selection process).
Fig. 1.
Sample selection. Note: One facility (ID: 1001) was closed in 2023 so the QOL/QCE data collection in this facility discontinued after obtaining very few data
Measure of QOL and QCE
QOL was measured by the Quality of Life-Aged Care Consumer (QOL-ACC) scale, a tool specifically designed for aged care settings and developed from inception with the input of older Australians accessing aged care [11, 13, 14]. The QOL-ACC scale gauges six dimensions of QOL: (1) mobility, (2) pain management, (3) emotional wellbeing, (4) independence, (5) social relationships and (6) leisure activities/hobbies (Supplementary Material 1). For each dimension there is one question, e.g., ‘I am generally happy’. Residents select response, from five options: ‘none of the time’, ‘a little of the time’, ‘some of the time’, ‘most of the time’ and ‘all of the time’. Each dimension is scored from 0 to 4 and thus the total score of QOL-ACC ranges 0–24. A higher score indicates better QOL.
QCE was measured by the Quality of Care Experience-Aged Care Consumer (QCE-ACC) scale, a new tool designed specifically to collect information about care experience of older adults receiving aged care services and supports [15]. The QCE-ACC scale assesses six dimensions of QCE: (1) respect and dignity, (2) supported decision-making, (3) skills of aged care staff, (4) impact on health and wellbeing, (5) social relationships and community connection and (6) confidence in lodging complaints (Supplementary Material 1). For each dimension there is one question, e.g., ‘I am treated with respect and dignity’. Residents select from five options: ‘never’, ‘rarely’, ‘sometimes’, ‘mostly’ and ‘always’. These options are scored from 0 to 4 correspondingly, so the total score of QCE-ACC ranges 0–24. A higher score indicates better QCE.
Both scales of QOL-ACC and QCE-ACC were developed following comprehensive literature review, and in-depth qualitative interviews and workshops with older people across different care settings, including RAC facilities, using quantitative methods to test validity and with preference-based scoring algorithm developed to facilitate application [14–18]. The process of extensive engagement with aged care consumers and care provider representatives was designed to ensure language and questions included are meaningful, acceptable and suitable for older adults in aged care settings [15, 16, 19]. The two scales share the same scoring method for determining the total score, which is grouped into five categories, ‘very poor’ (0–7), ‘poor’ (8–13), ‘moderate’ (14–18), ‘good’ (19–21) and ‘excellent’ (22–24).
The QOL-ACC and QCE-ACC surveys use three completion modes: self-completion (i.e., completed by residents themselves), interviewer-facilitated completion (i.e., completed with assistance from staff) and proxy completion (i.e., completed by proxy assessors frequently visiting the resident, e.g., spouse/siblings/son/daughter). Interviewer-facilitated and proxy completion are used when a care recipient is unable to self-complete the assessment e.g., due to the presence of moderate to severe cognitive impairment. The surveys were facilitated by facility staff rather than third-party surveyors or contractors. Facility staff administered the surveys, including both self-completion and proxy-completion methods. Proxies were defined as individuals who could represent residents unable to complete the survey themselves, such as family members or facility staff. Proxy surveys were completed mostly in person, but also by phone or via mail if the proxy was not local.
Statistical analyses
We first descriptively analysed QOL and QCE data to determine the overall aggregated scores and categorise individual responses to each of the six dimensions of the two indicators, including the median score and proportions in each category for the QOL and QCE. Descriptive statistics are presented for the entire sample and by completion mode.
To examine whether QOL and QCE scores varied by different completion modes, we used propensity score matching. Propensity score matching is an established method used to account for demographic and case-mix differences between groups, ensuring that comparisons of QOL and QCE scores across different survey completion modes are not biased by these factors [20]. This method allows us to estimate the impact of survey completion modes more accurately by comparing groups with similar characteristics, addressing the issue of selection bias inherent in non-randomised designs. When using propensity score matching, we controlled for a number of covariates, including resident age, sex, entry type, length of stay and 20 health conditions at time of admission. We applied the nearest-neighbour matching, with each observation in certain completion mode being matched with ≥ 4 observations from another completion mode to increase robustness of the results. We then compared the proportion of participants rating QOL and QCE as ‘excellent’/‘good’ among the 22 RAC facilities to examine any variation by facility, adjusting for covariates used in the propensity score matching.
We conducted multilevel ordinal logistic regression with random intercept for facilities to investigate the factors associated with QOL and QCE scores, controlling for the same covariates used in the propensity score matching along with completion mode. Multilevel ordered logistic regression was applied given that the dependent variables in our analysis (i.e., QOL and QCE) are ordinal variables and that participants were organised in two levels (i.e., individual level and RAC-home level). We merged the ‘very poor’ category with ‘poor’ in the multilevel ordinal logistic regression, since the proportions of ‘very poor’ were small for both outcomes (0.9% for QOL and 0.2% for QCE). We used odds ratios (OR) to compare differences in QOL and QCE outcomes (i.e., ‘excellent’, ‘good’, ‘moderate’ and ‘poor/very poor’) by different covariates. Analysis was performed using Stata 18 (StataCorp LP, College Station, TX).
Results
Participant characteristics
Of the 1,772 residents, approximately two-thirds (66.6%) were female and the vast majority were permanent residents (97.6%). The median age was 88 (interquartile range [IQR] 82–93) years, and the median length of stay was 591 (IQR 284–1,388) days. The most prevalent comorbidity was circulatory disease (87.5%). Most residents used interviewer-facilitated completion (63.4% for QOL-ACC; 60.0% for QCE-ACC), while the percentage of residents using self-completion (17.1% for QOL-ACC; 20.1% for QCE-ACC) and proxy completion (19.5% for QOL-ACC; 19.9% for QCE-ACC) were similar (Table 1).
Quality of life scores
Overall, the median QOL score was 21 (IQR 18–24), with self-completion exhibiting the highest median score at 22 (IQR 20–24), followed by interviewer-facilitated completion (21, IQR 19–24) and proxy completion (20, IQR 15–24) (Table 2). The majority of the residents’ scores indicated their QOL as ‘excellent’ (49.2%)/‘good’ (26.1%). For the six dimensions of QOL, approximately 80% of the participants selected ‘all of the time’ or ‘most of the time’ for all dimensions of QOL. However, leisure activities of QOL were rated lower than the other five dimensions, with more than 21% of residents selecting ‘some of the time’ or a lower frequency. The results of the propensity score matching showed that overall and for each the six dimensions (except pain management), residents using self-completion exhibited the best QOL outcomes, while participants using proxy completion mode the worst (Table 2).
Table 2.
Summary of the quality of life (QOL) responses overall and by the six survey dimensions and completion mode
| All (n = 1,706) |
By completion mode | Differences of means by completion mode using propensity-score matching | ||||||
|---|---|---|---|---|---|---|---|---|
| Interviewer-facilitated (n = 1,082) |
Proxy-completion (n = 333) |
Self-completion (n = 291) |
Proxy vs. Interviewer-facilitated | Self vs. Interviewer-facilitated | Self vs. Proxy | |||
| Overall QOL (0–24) | ||||||||
| Median (IQR) | 21(18–24) | 21(19–24) | 20(15–24) | 22(20–24) | -1.988** | 0.740** | 2.536*** | |
| Mobility: I am able to get around as much as I want to: (with the use of mobility aids e.g., wheelchair, walker, stick if you use them). | ||||||||
| All of the time | 1035(60.7) | 665(61.5) | 156(46.9) | 214(73.5) | -0.542*** | 0.220*** | 0.727*** | |
| Most of the time | 396(23.2) | 269(24.9) | 75(22.5) | 52(17.9) | ||||
| Some of the time | 140(8.2) | 82(7.6) | 43(12.9) | 15(5.2) | ||||
| A little of the time | 71(4.2) | 45(4.2) | 17(5.1) | 9(3.1) | ||||
| None of the time | 64(3.8) | 21(1.9) | 42(12.6) | 1(0.3) | ||||
| Pain management: When I experience pain, it is well managed: | ||||||||
| All of the time | 1064(62.4) | 674(62.3) | 193(58.0) | 197(67.7) | -0.035 | 0.015 | -0.021 | |
| Most of the time | 523(30.7) | 330(30.5) | 121(36.3) | 72(24.7) | ||||
| Some of the time | 99(5.8) | 67(6.2) | 17(5.1) | 15(5.2) | ||||
| A little of the time | 14(0.8) | 9(0.8) | 1(0.3) | 4(1.4) | ||||
| None of the time | 6(0.4) | 2(0.2) | 1(0.3) | 3(1.0) | ||||
| Emotional wellbeing: I am generally happy: | ||||||||
| All of the time | 896(52.5) | 581(53.7) | 142(42.6) | 173(59.5) | -0.241** | 0.084 | 0.308*** | |
| Most of the time | 606(35.5) | 393(36.3) | 115(34.5) | 98(33.7) | ||||
| Some of the time | 163(9.6) | 90(8.3) | 58(17.4) | 15(5.2) | ||||
| A little of the time | 32(1.9) | 13(1.2) | 14(4.2) | 5(1.7) | ||||
| None of the time | 9(0.5) | 5(0.5) | 4(1.2) | 0(0.0) | ||||
| Independence: I have as much independence as I want: | ||||||||
| All of the time | 982(57.6) | 638(59.0) | 147(44.1) | 197(67.7) | -0.616*** | 0.154** | 0.677*** | |
| Most of the time | 462(27.1) | 303(28.0) | 84(25.2) | 75(25.8) | ||||
| Some of the time | 138(8.1) | 97(9.0) | 30(9.0) | 11(3.8) | ||||
| A little of the time | 59(3.5) | 29(2.7) | 25(7.5) | 5(1.7) | ||||
| None of the time | 65(3.8) | 15(1.4) | 47(14.1) | 3(1.0) | ||||
| Social Relationships: I have good social relationships with family and friends: | ||||||||
| All of the time | 1253(73.5) | 793(73.3) | 226(67.9) | 234(80.4) | -0.137* | 0.055 | 0.202*** | |
| Most of the time | 322(18.9) | 216(20.0) | 62(18.6) | 44(15.1) | ||||
| Some of the time | 93(5.5) | 54(5.0) | 33(9.9) | 6(2.1) | ||||
| A little of the time | 30(1.8) | 14(1.3) | 9(2.7) | 7(2.4) | ||||
| None of the time | 8(0.5) | 5(0.5) | 3(0.9) | 0(0.0) | ||||
| Leisure activities/hobbies: I have leisure activities / hobbies I enjoy: | ||||||||
| All of the time | 860(50.4) | 534(49.4) | 146(43.8) | 180(61.9) | -0.486*** | 0.212** | 0.642*** | |
| Most of the time | 485(28.4) | 342(31.6) | 64(19.2) | 79(27.2) | ||||
| Some of the time | 217(12.7) | 142(13.1) | 52(15.6) | 23(7.9) | ||||
| A little of the time | 92(5.4) | 44(4.1) | 42(12.6) | 6(2.1) | ||||
| None of the time | 52(3.1) | 20(1.9) | 29(8.7) | 3(1.0) | ||||
Note: * indicates a significant difference at < 0.05, ** indicates a significant difference at < 0.01, while *** indicates a significant difference at < 0.001
Quality of consumer experience scores
Participants scores also indicated an overall high level of QCE, with a median score of 23 (IQR 20–24) (Table 3). Residents using self-completion exhibited the highest median QCE score at 23 (IQR 21–24), and the median scores for participants using other two completion modes were similar (both at 22). Almost two thirds (62.4%) of the participants had scores which indicated their QCE was ‘excellent’, and 22.4% as ‘good’. For all six dimensions of QCE, ratings were generally high with more than 90% of participants selecting ‘all of the time’ or ‘most of the time’ for almost all dimensions of QCE. Notably, the social relationship and complaint lodging dimensions were rated relatively lower than the other four dimensions, being the only two dimensions with more than 10% of the participants selecting ‘sometimes’ or a lower frequency. The results of propensity score matching demonstrated that participants using self-completion mode exhibited the best QCE outcomes, while participants using other completion modes had similar QCE outcomes (Table 3).
Table 3.
Level of overall quality of care experience (QCE) and its six dimensions, by completion mode
| All (n = 1,686) |
By completion mode | Differences of mean by completion mode using propensity-score matching | ||||||
|---|---|---|---|---|---|---|---|---|
| Interviewer-facilitated (n = 1,012) |
Proxy-completion (n = 336) |
Self-completion (n = 338) |
Proxy vs. Interviewer-facilitated | Self vs. Interviewer-facilitated | Self vs. Proxy | |||
| Overall QCE | ||||||||
| Median (IQR) | 23(20–24) | 22(20–24) | 22(19–24) | 23(21–24) | 0.181 | 0.734*** | 0.669** | |
| Respect & dignity: I am treated with respect and dignity: | ||||||||
| Always | 1360(80.7) | 784(77.5) | 278(82.7) | 298(88.2) | 0.086** | 0.103** | 0.054 | |
| Mostly | 286(17.0) | 198(19.6) | 53(15.8) | 35(10.4) | ||||
| Sometimes | 34(2.0) | 24(2.4) | 5(1.5) | 5(1.5) | ||||
| Rarely | 4(0.2) | 4(0.4) | 0(0.0) | 0(0.0) | ||||
| Never | 2(0.1) | 2(0.2) | 0(0.0) | 0(0.0) | ||||
| Supported in decision-making: I am supported to make my own decisions about the care and services I receive: | ||||||||
| Always | 1112(66.0) | 661(65.3) | 202(60.1) | 249(73.7) | -0.100 | 0.089* | 0.144 | |
| Mostly | 429(25.4) | 270(26.7) | 84(25.0) | 75(22.2) | ||||
| Sometimes | 108(6.4) | 66(6.5) | 35(10.4) | 7(2.1) | ||||
| Rarely | 19(1.1) | 6(0.6) | 9(2.7) | 4(1.2) | ||||
| Never | 18(1.1) | 9(0.9) | 6(1.8) | 3(0.9) | ||||
| Supported by skilled aged care staff: I receive care and support from aged care staff who have the appropriate skills and training: | ||||||||
| Always | 1089(64.6) | 648(64.0) | 214(63.7) | 227(67.2) | 0.033 | 0.056 | 0.012 | |
| Mostly | 508(30.1) | 300(29.6) | 108(32.1) | 100(29.6) | ||||
| Sometimes | 78(4.6) | 55(5.4) | 13(3.9) | 10(3.0) | ||||
| Rarely | 10(0.6) | 8(0.8) | 1(0.3) | 1(0.3) | ||||
| Never | 1(0.1) | 1(0.1) | 0(0.0) | 0(0.0) | ||||
| Supported in health and wellbeing: I receive services and supports for daily living that are important for my health and wellbeing: | ||||||||
| Always | 1176(69.8) | 682(67.4) | 237(70.5) | 257(76.0) | 0.114* | 0.125*** | 0.058 | |
| Mostly | 432(25.6) | 266(26.3) | 90(26.8) | 76(22.5) | ||||
| Sometimes | 68(4.0) | 55(5.4) | 8(2.4) | 5(1.5) | ||||
| Rarely | 9(0.5) | 8(0.8) | 1(0.3) | 0(0.0) | ||||
| Never | 1(0.1) | 1(0.1) | 0(0.0) | 0(0.0) | ||||
| Supported in maintaining social relationships: I am supported to maintain my social relationships and connections with the community: | ||||||||
| Always | 1090(64.7) | 650(64.2) | 200(59.5) | 240(71.0) | -0.062 | 0.160*** | 0.274*** | |
| Mostly | 413(24.5) | 249(24.6) | 77(22.9) | 87(25.7) | ||||
| Sometimes | 149(8.8) | 97(9.6) | 42(12.5) | 10(3.0) | ||||
| Rarely | 22(1.3) | 7(0.7) | 14(4.2) | 1(0.3) | ||||
| Never | 12(0.7) | 9(0.9) | 3(0.9) | 0(0.0) | ||||
| Having confidence in lodging complaints: I am comfortable lodging complaints with confidence that the appropriate action will be taken: | ||||||||
| Always | 1113(66.0) | 639(63.1) | 224(66.7) | 250(74.0) | 0.113* | 0.198*** | 0.124* | |
| Mostly | 396(23.5) | 249(24.6) | 78(23.2) | 69(20.4) | ||||
| Sometimes | 124(7.4) | 88(8.7) | 23(6.9) | 13(3.9) | ||||
| Rarely | 34(2.0) | 24(2.4) | 6(1.8) | 4(1.2) | ||||
| Never | 19(1.1) | 12(1.2) | 5(1.5) | 2(0.6) | ||||
Note: * indicates a significance level < 0.05, ** indicates a significance level < 0.01, while *** indicates a significance level < 0.001
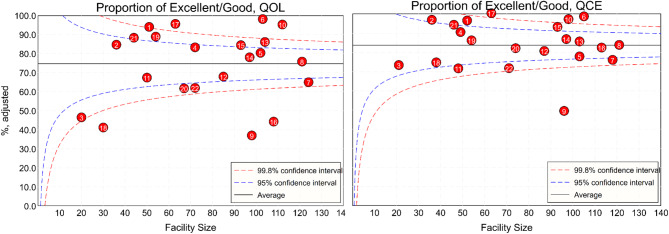
Variations in QOL and QCE by facility
Figure 2 presents the adjusted (by residents’ age, sex, entry type, length of stay and 20 health conditions at time of admission) proportions of participants’ ratings of their QOL and QCE as ‘excellent’/‘good’. Among the 22 RAC facilities, most facilities had overall QOL and QCE outcomes close to the average of the whole sample, though a few facilities had significantly lower scores. Seven facilities were under the 95% confident interval (CI) for the ‘excellent’/‘good’ rating in QOL, while four facilities were under the 95% CI in QCE. For lower-performing facilities there was no relationship between facility size and QOL or QCE ratings.
Fig. 2.
Variation in the percentage of residents with ‘Excellent’/‘Good’ quality of life (QOL) and quality of care experience (QCE) scores among the 22 residential aged care facilities. Note: Each dot represents a facility; Adjusted for age, sex, length of stay, entry type and health conditions including circulatory disease, diabetes, chronic respiratory disease, neoplasms/cancer, dementia, Parkinson’s disease, depression, mood & affective disorders, anxiety & stress-related disorders, renal disease, arthritis, osteoporosis, fracture, hearing impairment, visual impairment, fall history, faecal incontinence, urinary incontinence, double incontinence, constipation, urinary tract infection
Factors associated with QOL and QCE outcomes
Table 4 presents results of the multilevel ordinal logistic regression to examine factors associated with QOL and QCE scores. A longer length of stay, having a fall history, and using proxy mode were significantly associated with a lower probability of having high rating in QOL. Residents with a fall history or visual impairment were significantly associated with a lower probability of having a high QCE score, with all other factors being equal. Specifically, residents who had lived in a RAC facility for more than three years had a 30.3% lower probability of ‘excellent’ in QOL compared to residents who had stayed for a less than one year (OR = 0.70, 95% CI = 0.53, 0.93). Residents using proxy mode had a 48% lower probability of ‘excellent’ in QOL compared to those using interviewer-facilitated mode (OR = 0.52, 95% CI = 0.40, 0.69). Similarly, residents with a fall history showed a 26.0% lower probability of ‘excellent’ in QOL compared to residents with no history of falls (OR = 0.74, 95% CI = 0.60, 0.91), and also had a 20.3% lower probability of an ‘excellent’ QCE score (OR = 0.80, 95% CI = 0.64, 0.99).
Table 4.
Results of multilevel ordinal logistic regression models using quality of life (QOL) and quality of care experience (QCE) scores as outcome variables
| QOL | QCE | ||||
|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||
| Age | 0.99 | (0.99,1.01) | 1.01 | (1.00,1.03) | |
| Gender (ref.=female) | 1.09 | (0.88,1.36) | 1.08 | (0.85,1.37) | |
| Entry type (ref.=permanent residents) | 1.14 | (0.58,2.24) | 0.71 | (0.33,1.55) | |
| Length of stay | |||||
| <1 year (ref.) | |||||
| 1–2 years | 0.94 | (0.71,1.25) | 1.01 | (0.75,1.37) | |
| 2–3 years | 0.68 | (0.48,0.97) | 0.73 | (0.50,1.05) | |
| ≥3 years | 0.70 | (0.53,0.93) | 0.86 | (0.64,1.15) | |
| Completion mode | |||||
| Interviewer-facilitated (ref.) | |||||
| Proxy | 0.52 | (0.40,0.69) | 1.00 | (0.75,1.34) | |
| Self-completion | 1.63 | (1.21,2.20) | 1.15 | (0.84,1.57) | |
| Circulatory disease, any (ref.=no) | 1.01 | (0.73,1.40) | 0.79 | (0.56,1.11) | |
| Diabetes (ref.=no) | 0.98 | (0.78,1.23) | 1.03 | (0.81,1.32) | |
| Chronic respiratory disease (ref.=no) | 0.95 | (0.74,1.22) | 0.83 | (0.63,1.08) | |
| Neoplasms/cancer (ref.=no) | 0.92 | (0.74,1.15) | 0.91 | (0.72,1.15) | |
| Dementia (ref.=no) | 1.01 | (0.82,1.24) | 0.91 | (0.73,1.14) | |
| Parkinson’s disease (ref.=no) | 0.87 | (0.61,1.24) | 0.75 | (0.52,1.09) | |
| Depression, mood & affective disorders (ref.=no) | 0.94 | (0.76,1.16) | 0.94 | (0.75,1.18) | |
| Anxiety & stress-related disorders (ref.=no) | 0.97 | (0.77,1.22) | 1.12 | (0.87,1.43) | |
| Renal disease (ref.=no) | 0.88 | (0.68,1.14) | 1.06 | (0.80,1.41) | |
| Arthritis (ref.=no) | 0.89 | (0.73,1.09) | 0.96 | (0.77,1.19) | |
| Osteoporosis (ref.=no) | 1.10 | (0.88,1.38) | 1.03 | (0.81,1.31) | |
| Fracture (ref.=no) | 1.08 | (0.87,1.35) | 1.17 | (0.92,1.48) | |
| Hearing impairment (ref.=no) | 0.91 | (0.71,1.17) | 0.98 | (0.74,1.28) | |
| Visual impairment (ref.=no) | 0.92 | (0.69,1.22) | 0.74 | (0.55,0.99) | |
| Fall history (ref.=no) | 0.74 | (0.60,0.91) | 0.80 | (0.64,0.99) | |
| Faecal incontinence (ref.=no) | 1.01 | (0.57,1.81) | 1.26 | (0.69,2.28) | |
| Urinary Incontinence (ref.=no) | 1.04 | (0.78,1.37) | 1.14 | (0.84,1.54) | |
| Double incontinence (ref.=no) | 0.81 | (0.42,1.54) | 0.61 | (0.31,1.18) | |
| Constipation (ref.=no) | 0.89 | (0.67,1.20) | 0.84 | (0.61,1.14) | |
| Urinary tract infection (ref.=no) | 1.09 | (0.84,1.42) | 1.19 | (0.90,1.58) | |
| Intraclass Correlation Coefficient (ICC) | 0.337 | 0.228 | |||
| Akaike Information Criterion (AIC) | 3,748.5 | 3,091.7 | |||
| Log-likelihood | -1,837.2 | -1,509.9 | |||
Note: OR = odd ratio. ref.=reference
Discussion
Using the newly collected QI indicator data from a large not-for-profit RAC provider, this study provides new and timely evidence to better understand QOL and QCE in the Australian RAC sector. The results showed that the majority of residents reported good or excellent scores for both QOL and QCE in the 22 RAC facilities studied. There was however considerable variation by survey completion mode and by facility. We found QOL scores were lower for residents who had been in residential aged care for a longer time and for those with a history of falls. QCE scores were significantly lower for those who had visual impairment or a falls history.
The overall high ratings of QOL and QCE of RAC residents observed mirror the findings from the pilots of the QOL-ACC and the QCE-ACC scales in Australian home care and RAC settings [16, 21, 22], and also correspond to one prior study reporting overall high satisfaction on quality of care received in two RAC facilities in South Australia through qualitative interview (n = 10) [23]. Our findings also align with a small number of previous international studies reporting overall positive ratings on QOL and quality of care received among RAC residents in North America [24–26]. For example, one Canadian study showed high ratings in seven out of ten aspects of life (e.g., privacy, safety, respect and autonomy) in 48 RAC facilities (n = 928, completion rate = 51%) [26], while another study in the US reported that nearly 70% of surrogates rated QOL of RAC residents with advanced dementia as ‘excellent’/‘good’/‘fair’ [25]. In our study, more than three quarters of RAC respondents rated their QOL/QCE as ‘excellent’/‘good’ through the QOL-ACC and the QCE-ACC which are designed specifically for aged care settings with demonstrated satisfactory construct validity and meaningful dimensions to RAC recipients [15, 19]. This alignment suggests that the QOL-ACC and QCE-ACC, like many other Patient-Reported Outcome Measures (PROMs) and Patient-Reported Experience Measures (PREMs) for quality of life, tend to exhibit a positively skewed distribution. This positive skewness indicates that a majority of residents report favourable outcomes regarding their QOL and care. Such skewness may reflect a generally high satisfaction level within the study population. However, this distribution also suggests that there may be ceiling effects, where the measures do not adequately distinguish between high levels of satisfaction among different respondents.
The high ratings obtained for the QOL and QCE should also be treated with some caution as they may be partly driven by the so-called social desirability pressure. Social desirability pressure refers to the tendency that respondents strive to report what they think is required not what they actually thought or experienced, particularly in the presence of another individual, leading to an over-reporting of ‘good behaviour’ and an under-reporting of less desirable behaviour [27]. Noteworthily, many prior studies of patient satisfaction surveys have found higher average scores among participants who complete surveys on-site compared to those who complete an email-based survey [28]. Surveys orally administered by staff also receive more favourable ratings compared to those completed by patients [29]. In our study, most surveys were completed with the assistance of staff. RAC residents, many of whom are highly dependent upon and familiar with the staff administering the survey, might feel the need to provide positive ratings, leading to potentially artificially elevated outcomes in the two scales.
The QOL and QCE ratings varied significantly by completion mode, with self-completion tending to have the highest rating outcomes compared to the other two completion modes. This finding holds even after adjusting for a broad range of covariates using propensity score matching. This finding aligns with a recent study reporting a higher level of self-report compared to proxy rating in applying the QOL-ACC and the QCE-ACC scales in aged care based on a small sample (n = 63) [30]. However, unlike previous studies, which had tended to limit comparison between proxy and self-report assessments [31–35], we compared and analysed three completion modes (including the most common one, interviewer-facilitated completion, in RAC), demonstrating that completion by proxy and interviewer-facilitated were associated with lower scores than self-completion for both QOL and QCE. The lower scores linked to use of proxy assessors or interviewers might be explained by so-called ‘proxy bias’, which occurs when the responses from a proxy are systematically different from those from intended respondent, in terms of variables that cannot be measured directly (e.g., job satisfaction) [36]. Regarding QOL and QCE, a proxy tends to rate using the middle of a scale rather than at the extremes, while, in contrast, individuals themselves tend to be subject to positive cognitive bias, a psychological process that tends to give a positive view on self-perceived wellbeing [37]. The positive cognitive bias might result in right-skewed distribution of self-reported life outcomes, higher than proxy assessments which are subject to a central tendency [38]. We also acknowledge that the results of proxy mode are affected by a wide range of factors, including the relationship/interaction between proxy and interviewee, perspectives of proxy (proxy-patient perspective vs. proxy-proxy perspective), and communication barriers of interviewees [39, 40]. For example, family members might overestimate the resident’s QOL or QCE out of optimism or underreport issues to avoid criticism of the facility, while facility staff might be influenced by their professional experiences and observations, depending on their interactions with the resident and their perception of the care environment. This underscores the need to interpret proxy assessments with caution, recognising that they do not equate directly to self-reports and should be considered separately in analyses. Given that subjective self-appraisals are deemed as the gold standard to evaluate personal life outcomes or experience [41] while proxy and interviewer assistance are widely used in QOL and QCE assessment in RAC, future research is needed to further examine the underlying reasons behind the variations of QOL and QCE by completion mode and the ways to maximise the agreements over the three completion modes. Integrating insights from existing studies on non-RAC settings [42, 43] can help develop more reliable and valid assessment methods, ensuring a more accurate representation of residents’ QOL and care experiences in RAC settings.
Despite overall high ratings of QOL and QCE, we also observed variation in QOL and QCE ratings among dimensions of these two indicators. RAC residents rated leisure activities in QOL, and social relationships and complaint lodging in QCE, relatively lower than other dimensions. Two previous studies in US nursing homes found that meaningful activity and staff-resident relationships were of the lowest ratings among different domains of QOL measured (e.g., security and dignity) [24, 44]. Another study of long-term residents in Canada reported that staff-resident bonding and personal relationship received the worst ratings among eleven aspects of QOL studied (e.g., privacy and respect) [26]. Our findings suggest that complaint lodging is another dimension of quality of care requiring attention. RAC residents may not have sufficient confidence to provide feedback on issues that affect their care or that issues raised will be addressed.
Our results showed that the QOL and QCE of residents in some facilities is significantly poorer than others. Two prior studies indicated a negative association between residents’ QOL and facility size given the adverse effect as facility size increases, including greater probability of understaffing, management difficulty and more frequent consumer complaints [44, 45]. However, we found no association between ratings and facility size. Our study did not have data on specific facility characteristics which might explain some of the score variation and these factors would be important to consider in future analyses. Additionally, variations in completion rates across facilities were observed in our data, which may affect the QOL and QCE outcomes by facility as use of completion mode could potentially affect the survey results.
The detrimental nexus found between QOL/QCE and fall history and visual impairment is not unexpected, given the well-reported devastating consequences of falls and vision loss, including decreased independence, mobility and diminished social relationships [46–48], which might decrease residents’ QOL and care experience. By contrast, existing evidence regarding the linkage between length of stay and QOL/QCE is scarce. One previous study in the United States reported that length of stay is positively associated with RAC residents’ assessment of environment, food and enjoyment but is adversely associated with negative mood and overall level of QOL, possibly given an increasing proportion of functional and cognitive limitations among residents in old age [44]. It could also be due to the functional and/or cognitive decline over time, which is known to be closely related to QOL as measured using other established measures applied in RAC. This factor was not explicitly considered in our study, which is a limitation. More research is needed to explore the reasons behind the lower QOL/QCE among residents with a longer length of stay.
Policy implications and future research directions
Given the sample limitations of our study, it is essential to approach the policy implications with caution. While our findings provide valuable insights, they underscore the need for national-level studies to verify the observations related to low ratings on leisure participation and social bonding, as well as the associations with visual limitations, falls, and length of stay. Specifically, our study observed notably low ratings on leisure participation and social bonding among residents in RAC facilities. These findings suggest potential areas of concern that could significantly impact the residents’ overall well-being. Additionally, our study found associations between lower QOL scores and factors such as visual limitations, higher incidence of falls, and longer lengths of stay in the facilities. These associations highlight critical areas that may influence residents’ experiences and outcomes in RAC settings. However, these findings need to be validated through extensive research across diverse populations and settings to establish their generalisability and to understand the underlying mechanisms.
The primary policy implication of our study is the observed difference in ratings by completion modes, which has significant implications for public reporting. Ensuring accurate and consistent reporting across different completion modes is crucial for reliable assessments of QOL and QCE in RAC facilities. Extra caution should also be exercised when interpreting assessment results by considering the potential effect of completion mode on QOL/QCE outcomes. Further research is needed to explore the extent of these mode effects and to identify strategies for mitigating their impact.
Strengths and limitations
The strengths of this study lie in the uniqueness of its data, based on the newly collected information of QOL and QCE in the Australian RAC sector commencing in April 2023. To the best of our knowledge, this is the first study using QOL and QCE data from the QI program to examine overall QoL and consumer experience among Australian RAC residents.
This study has some limitations. First, the data used were sourced from one aged care service provider in New South Wales, Australia and hence may not be representative of other RAC providers. Second, RAC-home-level factors, e.g., staffing level, location of facility, and differences of residents’ characteristics, that might affect QOL/QCE outcomes were not adjusted for due to data unavailability. Nonetheless, a broad range of covariates were accounted for, and each facility was considered as a cluster in the current analyses. Third, 711 residents did not participate in the QOL-ACC/QCE-ACC surveys so we are unable to examine their QOL/QCE levels. However, by comparing residents with and without QOL/QCE data, no significant differences were observed regarding residents’ personal characteristics, indicating a random distribution of missing data. Fourth, while our study utilised raw scores for the QOL-ACC and the QCE-ACC, this approach has limitations. Preference-weighted scores could potentially offer a more nuanced understanding of QOL/QCE by accounting for the varying importance of different dimensions based on residents’ preferences. However, incorporating such weighted scores introduces additional complexity and requires a standardised weighting system, which was not applied in this study. The absence of preference-weighted scores means that our findings reflect the total score without considering the relative significance of individual dimensions, which could affect the interpretation of the QOL/QCE outcomes. Future research should explore the use of preference-weighted scores to enhance the sensitivity and relevance of QOL/QCE assessments. Fifth, while the QOL-ACC and QCE-ACC were designed specifically for aged care settings, we acknowledge the importance of considering potential limitations such as sensitivity, floor/ceiling effects, and variations in scores. Further evaluations are necessary to continually validate the measures and ensure their effectiveness across diverse resident populations.
Conclusions
The study observed overall high levels of QOL and QCE of residents in the 22 RAC facilities examined, though there is room for improvement especially in relation to availability of leisure activities (QOL) and social relationship and complaint lodging (QCE). Variations of QOL and QCE by completion mode and facility were prominent, with ratings by self-completion significantly higher than other two completion modes, and a few facilities clearly underperforming other facilities. Adverse associations between length of stay and fall history and QOL, and between visual impairment and fall history and QCE were also revealed. Future research is recommended to explore the causes of low QOL/QCE in certain facilities and the variations of these two indicators by completion mode.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the partners and collaborators of this project including Anglicare, Northern Sydney Local Health District, Sydney North Primary Health Network, the Deeble Institute for Health Policy Research, and the Australian Aged Care Quality and Safety Commission.
Author contributions
Author Contributions Conceptualisation: GH, NW, AN Data curation: GH, NW Formal analysis: GH, NW, SS Funding acquisition: NW, MR, JW Project administration: NW, JW Writing - original draft: GH Writing - review & editing: GH, NW, MR, AN, SM, YX, JR, JK, JW.
Funding
The study was part of a partnership project funded by the Australian National Health and Medical Research Council (NHMRC) Partnership Project Grant in partnership with Anglicare (1170898). The funding organisation did not have any influence on the study design, data collection, analysis and interpretation as well as the preparation, review, or approval of the manuscript for publication.
Data availability
The data used in this study are available from the aged care provider (Anglicare), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors (Guogui Huang, guogui.huang@mq.edu.au) upon reasonable request and with permission of Anglicare.
Declarations
Ethical approval and consent to participate
The study was reviewed and approved by Macquarie University Human Research Ethics Committee (No. 52019614412614). All methods and analysis in this study were carried out in accordance with the principles of the Declaration of Helsinki. Because de-identified data were used, requirement of obtaining participants’ consent was waived by Macquarie University Human Research Ethics Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Multiple imputation was considered as a method to handle missing data. However, since the proportion of missing data in the latest records was very low (approximately 4.4% for QOL-ACC and 4.6% for QCE-ACC), a complete case analysis was employed. This decision was based on the minimal impact of missing data on the overall results, ensuring that the analysis remained robust and reliable.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations. World Population Prospects 2022. website. https://population.un.org/wpp/Download/Standard/Population/. Published 2022.
- 2.Parliament of Australia. Reforming Australia’s aged care system: are we there yet? website. https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/BriefingBook44p/AgedCare. Published 2012. Accessed 17 July, 2023.
- 3.Moore CB. Consumer directed care aged care reforms in Australia since 2009: a retrospective policy analysis. Health Policy. 2021;125(5):577–81. [DOI] [PubMed] [Google Scholar]
- 4.Ronald LA, McGregor MJ, McGrail KM, Tate RB, Broemling A-M. Hospitalization rates of nursing home residents and community-dwelling seniors in British Columbia. Can J Aging/La Revue Canadienne Du Vieillissement. 2008;27(1):109–15. [DOI] [PubMed] [Google Scholar]
- 5.Graverholt B, Riise T, Jamtvedt G, Ranhoff AH, Krüger K, Nortvedt MW. Acute hospital admissions among nursing home residents: a population-based observational study. Bmc Health Serv Res. 2011;11(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Royal Commission into Aged Care Quality and Safety. Experimental Estimates Preval Elder Abuse Australian Aged Care Facilities 2020.
- 7.Royal Commission into Aged Care Quality. and Safety. Interim report: Neglect. Canberra2019.
- 8.Royal Commission into Aged Care Quality. and Safety. Final report-executive summary. Canberra2021.
- 9.Department of Health and Aged Care. National Aged Care Mandatory Quality Indicator Program (QI Program) Manual Part A – Version 3. 2023.
- 10.Department of Health and Aged Care. Learn about the QI Program expansion. website. https://www.health.gov.au/our-work/qi-program/learn-about-the-qi-program-expansion#:~:text=On%201%20April%202023%20we,activities%20of%20daily%20living. Published 2023.
- 11.Ratcliffe J, et al. Developing a new quality of life instrument with older people for economic evaluation in aged care: study protocol. Bmj Open. 2019;9(5):e028647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caughey GE et al. International and National Quality and Safety Indicators for Aged Care. Report for the Royal Commission into Aged Care Quality and Safety. South Australian Health and Medical Research Institute, Adelaide, South Australia. 2020.
- 13.Cleland J, et al. Developing dimensions for a new preference-based quality of life instrument for older people receiving aged care services in the community. Qual Life Res. 2021;30:555–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutchinson C et al. What quality of life domains are most important to older adults in residential care? J Aging Soc Policy 2022:1–22. [DOI] [PubMed]
- 15.Chen G, Ratcliffe J, Milte R, Khadka J, Kaambwa B. Quality of care experience in aged care: an Australia-wide discrete choice experiment to elicit preference weights. Soc Sci Med. 2021;289:114440. [DOI] [PubMed] [Google Scholar]
- 16.Hutchinson C, et al. The integration of mixed methods data to develop the quality of life–aged care consumers (QOL-ACC) instrument. Bmc Geriatr. 2021;21(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cleland J, Hutchinson C, Khadka J, Milte R, Ratcliffe J. What defines quality of care for older people in aged care? A comprehensive literature review. Geriatr Gerontol Int. 2021;21(9):765–78. [DOI] [PubMed] [Google Scholar]
- 18.Ratcliffe J, et al. Valuing the quality-of-life aged care consumers (QOL-ACC) instrument for Quality Assessment and economic evaluation. PharmacoEconomics. 2022;40(11):1069–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khadka J, et al. Assessing feasibility, construct validity, and reliability of a new aged care-specific preference-based quality of life instrument: evidence from older australians in residential aged care. Health Qual Life Out. 2022;20(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khadka J, et al. Assessing the construct validity of the quality-of-life-aged care consumers (QOL-ACC): an aged care-specific quality-of-life measure. Qual Life Res. 2022;31(9):2849–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ratcliffe J, et al. Australia’s Aged Care System: The quality of care experience and community expectations: Research Paper 20: A research Study for the Royal Commission into Aged Care Quality and Safety. Royal Commission into Aged Care Quality and Safety; 2021.
- 23.Hughes K, Moore S. Quality of life versus quality of care: elderly people and their experience of care in South Australian residential facilities. Practice. 2012;24(5):275–85. [Google Scholar]
- 24.Burack OR, Weiner AS, Reinhardt JP, Annunziato RA. What matters most to nursing home elders: quality of life in the nursing home. J Am Med Dir Assoc. 2012;13(1):48–53. [DOI] [PubMed] [Google Scholar]
- 25.Cordner Z, Blass DM, Rabins PV, Black BS. Quality of life in nursing home residents with advanced dementia. J Am Geriatr Soc. 2010;58(12):2394–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kehyayan V, Hirdes JP, Tyas SL, Stolee P. Residents’ self-reported quality of life in long-term care facilities in Canada. Can J Aging/La Revue Canadienne Du Vieillissement. 2015;34(2):149–64. [DOI] [PubMed] [Google Scholar]
- 27.Grimm P. Social desirability bias. Wiley international encyclopedia of marketing. 2010.
- 28.Burroughs TE, Waterman BM, Gilin D, Adams D, McCollegan J, Cira J. Do on-site patient satisfaction surveys bias results? Joint Comm J Qual Patient Saf. 2005;31(3):158–66. [DOI] [PubMed] [Google Scholar]
- 29.LeVois M, Nguyen TD, Attkisson CC. Artifact in client satisfaction assessment: experience in community mental health settings. Eval Program Plan. 1981;4(2):139–50. [DOI] [PubMed] [Google Scholar]
- 30.Hutchinson C, et al. Examining interrater agreement between self-report and proxy-report responses for the quality of life-aged care consumers (QOL-ACC) instrument. J Patient-Reported Outcomes. 2024;8(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zucchella C, Bartolo M, Bernini S, Picascia M, Sinforiani E. Quality of life in Alzheimer disease: a comparison of patients’ and caregivers’ points of view. Alz Dis Assoc Dis. 2015;29(1):50–4. [DOI] [PubMed] [Google Scholar]
- 32.Yeaman PA, Kim D-Y, Alexander JL, Ewing H, Kim KY. Relationship of physical and functional independence and perceived quality of life of veteran patients with Alzheimer disease. Am J Hospice Palliat Medicine®. 2013;30(5):462–6. [DOI] [PubMed] [Google Scholar]
- 33.Kim EJ, et al. Proxy and patients ratings on quality of life in patients with schizophrenia and bipolar disorder in Korea. Qual Life Res. 2010;19:521–9. [DOI] [PubMed] [Google Scholar]
- 34.Fleming A, Cook KF, Nelson ND, Lai EC. Proxy reports in Parkinson’s disease: caregiver and patient self-reports of quality of life and physical activity. Mov Disorders: Official J Mov Disorder Soc. 2005;20(11):1462–8. [DOI] [PubMed] [Google Scholar]
- 35.Jones JM, McPherson CJ, Zimmermann C, Rodin G, Le LW, Cohen SR. Assessing agreement between terminally ill cancer patients’ reports of their quality of life and family caregiver and palliative care physician proxy ratings. J Pain Symptom Manag. 2011;42(3):354–65. [DOI] [PubMed] [Google Scholar]
- 36.Ruggero L, Croot K, Nickels L. Quality of life ratings and Proxy Bias in Primary Progressive Aphasia: two sides to the story? Am J Alzheimer’s Disease Other Dementias®. 2023;38:15333175231177668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cummins RA, Nistico H. Maintaining life satisfaction: the role of positive cognitive bias. J Happiness Stud. 2002;3:37–69. [Google Scholar]
- 38.Rand S, Caiels J. Using proxies to assess quality of life: a review of the issues and challenges. 2015.
- 39.Neumann PJ, Araki SS, Gutterman EM. The use of proxy respondents in studies of older adults: lessons, challenges, and opportunities. J Am Geriatr Soc. 2000;48(12):1646–54. [DOI] [PubMed] [Google Scholar]
- 40.Pickard AS, Knight SJ. Proxy evaluation of health-related quality of life: a conceptual framework for understanding multiple proxy perspectives. Med Care. 2005;43(5):493–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL™ 4.0 generic core scales. Health Qual Life Out. 2007;5(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Claes C, Vandevelde S, Van Hove G, Van Loon J, Verschelden G, Schalock R. Relationship between self-report and proxy ratings on assessed personal quality of life‐related outcomes. J Policy Pract Intellect Disabil. 2012;9(3):159–65. [Google Scholar]
- 43.Hays R, et al. Agreement between self reports and proxy reports of quality of life in epilepsy patients. Qual Life Res. 1995;4:159–68. [DOI] [PubMed] [Google Scholar]
- 44.Shippee TP, Henning-Smith C, Kane RL, Lewis T. Resident-and facility-level predictors of quality of life in long-term care. Gerontologist. 2015;55(4):643–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baldwin R, Chenoweth L, dela Rama M, Wang AY. Does size matter in aged care facilities? A literature review of the relationship between the number of facility beds and quality. Health Care Manage Rev. 2017;42(4):315–27. [DOI] [PubMed] [Google Scholar]
- 46.World Health Organization. WHO global report on falls prevention in older age. 2007. 2007.
- 47.Suzuki M, Ohyama N, Yamada K, Kanamori M. The relationship between fear of falling, activities of daily living and quality of life among elderly individuals. Nurs Health Sci. 2002;4(4):155–61. [DOI] [PubMed] [Google Scholar]
- 48.Horowitz A. The prevalence and consequences of vision impairment in later life. Top Geriatric Rehabilitation. 2004;20(3):185–95. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this study are available from the aged care provider (Anglicare), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors (Guogui Huang, guogui.huang@mq.edu.au) upon reasonable request and with permission of Anglicare.