Abstract
Background
Müllerian cysts of the posterior mediastinum are rare, benign lesions typically discovered incidentally via routine medical exams.
Case presentation
We present a distinctive case of a 49-year-old asymptomatic woman, illustrating a rare Müllerian cyst located in the posterior mediastinum with serous papillary cystadenoma-like features, a novel finding in the medical literature. Identified during a routine health screening in December 2020, a 20 mm cystic lesion adjacent to the T4-5 vertebral body was detected through chest CT and MRI, initially suggesting a neurogenic tumor. Histopathological analysis revealed a Müllerian cyst characterized by an epithelium resembling serous papillary cystadenoma, with positive immunohistochemical markers for Paired Box 8 (PAX8), Estrogen Receptor (ER), and Progesterone Receptor (PR), indicative of Müllerian differentiation. The papillary growth pattern initially raised concerns about malignancy, yet the benign nature was confirmed by minimal cellular atypia, well-defined borders, absence of invasion, and a low proliferation index.
Conclusion
This case underscores the significance of detailed pathological analysis and immunohistochemical profiling in managing atypical Müllerian cysts, adding to the limited knowledge on Müllerian cysts. Future research should explore the mechanisms leading to Müllerian cysts with serous papillary cystadenoma-like features in the posterior mediastinum.
Keywords: Müllerian cysts, Posterior mediastinum, Serous papillary adenomas, Video-assisted thoracic surgery, PAX8
Introduction
Müllerian cysts of the posterior mediastinum are uncommon, benign lesions, frequently discovered incidentally during imaging studies or routine medical examinations. These cysts, with embryological origins akin to the fallopian tubes, predominantly occur in women aged 40 to 60 years, typically presenting without symptoms and measuring approximately 30 mm in diameter. The prevalence of Müllerian cysts among mediastinal cysts is estimated to range between 5.5% and 15.8%, according to various studies [1]. Despite their relative rarity, accurate identification is crucial for proper management. Precise diagnosis necessitates detailed histopathological and immunohistochemical analysis. This report presents a distinctive case of a posterior mediastinal Müllerian cyst with serous papillary cystadenoma-like features, which is a novel observation in the literature.
Case presentation
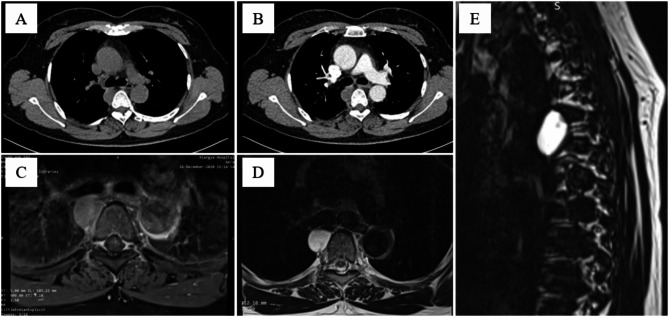
A 49-year-old asymptomatic woman underwent a routine health screening in December 2020, which included a chest computed tomography (CT) scan. The CT revealed a well-defined, 20 mm diameter cystic lesion located in the right posterior mediastinum, adjacent to the T4-5 vertebral body. Magnetic resonance imaging (MRI) T2 sequence showed a hyperintense lesion in the right posterior mediastinum with clear boundaries, suggesting a neurogenic tumor [Fig. 1]. The patient had no history of respiratory symptoms, chest pain, or other related complaints. After a thorough evaluation, including a review of her medical history and the absence of significant findings on physical examination, surgical resection was decided due to the rarity of the lesion and the potential for malignancy or symptomatic progression.
Fig. 1.
Imaging of the Müllerian cysts of the posterior mediastinum. (A) Chest CT plain scan shows a clearly defined cyst in the posterior mediastinum through the mediastinal window. (B) Enhanced CT shows mild enhancement at the edge of the cyst. (C) Axial T1 weighted MRI. (D) Axial T2 weighted MRI. (E) Sagittal MRI of Mullerian cyst at level T4-5
The patient underwent video-assisted thoracoscopic surgery (VATS) for cyst removal. The procedure utilized a two-port thoracoscopy technique, which minimized invasiveness and optimized cosmetic outcomes. Intraoperatively, the cyst was encapsulated and well-separated from adjacent structures, enabling complete removal without complications. Postoperatively, the patient experienced an uneventful recovery and was discharged on the fourth day following surgery. After a 3-year follow-up, she showed no signs of recurrence or metastasis.
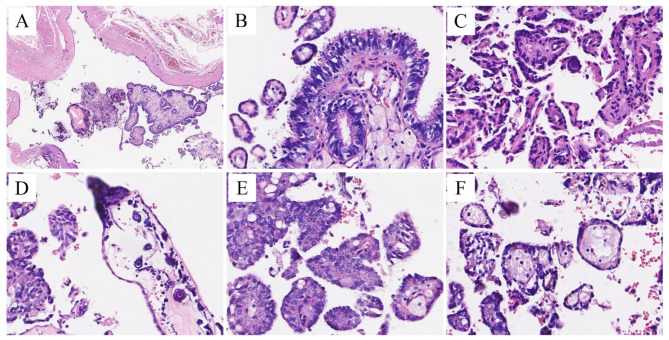
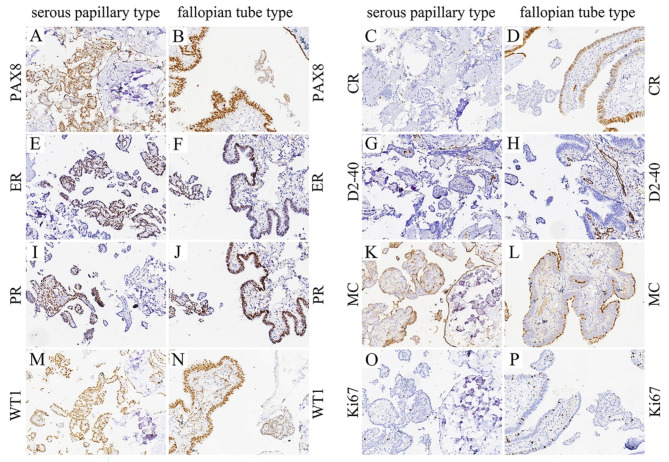
Histopathological examination confirmed the diagnosis of a Müllerian cyst in the posterior mediastinum, characterized by the presence of endometrioid or ciliated columnar epithelium lining the cyst wall. Notably, the cyst displayed a unique feature: the epithelium exhibited delicate fibrovascular cores containing psammoma bodies and foamy macrophages, corresponding to serous papillary adenomas [Fig. 2]. All epithelial tissues showed mild atypia without invasive behavior. The immunohistochemical analysis revealed isolated Ki-67 positivity in scattered cells, weak p53 positivity in a few tumor epithelial cells consistent with wild-type expression, and patchy weak p16 positivity. Positive expression of Paired Box 8 (PAX8), Estrogen Receptor (ER), Progesterone Receptor (PR), and Wilm’s tumor gene 1 (WT1) supported the evidence of Müllerian histogenesis. Mesothelin was positive but did not assist in differentiating between fallopian tube-type epithelium and mesothelioma. Calretinin (CR) was negative in most epithelial tissues, and D2-40 was entirely negative except in lymph vessels, thereby excluding the diagnosis of mesothelioma [Fig. 3].
Fig. 2.
Representative H&E stains. (A) A low power field (×4) showed cystic mass whose wall consisted of a smooth muscle layer and lined with cuboidal epithelia. (B) High power (×40) H&E image demonstrated two different structure: small papilla surrounded by flat epithelia and bigger papilla composed of ciliated columnar epithelium, resembling fallopian tube epithelium and serous papillary adenoma. High power (×40) fields showed that epithelia was hypoplastic (C) or hyperplastic (E), cores of papilla contained psammoma bodies (D) or foamy macrophages (F)
Fig. 3.
Representative IHC stains (×20). Most of epithelial cells were positive for PAX8 (A, B), ER (E, F), PR (I, J), WT1 (M, N). Focal positive expression of CR was found in fallopian tube epithelium (D), however, the serous papillary epithelium was negative for CR (C). Both types of epithelium did not express D2-40 (G, H). Cavity margin expression pattern of mesothelin was observed (K, L). Ki-67 index was less than 5% (O, P)
Discussion
The initial report of a mediastinal Müllerian cyst was made by Hattori in 2005 [2]. Since then, over 20 case reports have been documented. Sullivan et al. reviewed data from 39 patients with posterior mediastinal Müllerian cysts, revealing that all patients were female, with an average age of 47.2 years and an average cyst diameter of 30.4 mm [3]. The demographic characteristics of our reported cases align with these previous findings.
The etiology of mediastinal Müllerian cysts remains elusive. It is hypothesized that these cysts result from residual Müllerian tissue during embryogenesis [4]. Hattori suggests that the cyst may originate from the transformation of mesothelial cells into Müllerian epithelium. This transformation may involve mesothelial cells converting into cells with Müllerian characteristics under certain conditions, leading to the formation of the cyst [2]. Predominantly, mediastinal Müllerian cysts manifest during the peri-menopausal phase and are frequently associated with a history of obesity and various gynecological interventions, including hormone therapy, hysterectomy, induced abortion, and oophorectomy. These associations suggest that hormonal imbalances may contribute to the development of mediastinal Müllerian cysts [5].
Common posterior mediastinal cysts include lymphatic malformations, spinal meningeal cysts, neurogenic lesions, and foregut cysts. Preoperative imaging often poses challenges in differentiation, with definitive diagnosis primarily relying on postoperative pathological examination. When encountering cystic findings in the posterior mediastinum, the possibility of a Müllerian duct cyst should be considered, especially in peri-menopausal and obese female patients.
PAX8 is a transcription factor belonging to the paired box gene family. It regulates the organogenesis of the thyroid gland, kidney, and Müllerian system. PAX8 immunohistochemistry is a recognized Müllerian marker, expressed in tumors originating from the Müllerian system. It is instrumental in differentiating between Müllerian and non-Müllerian tumors [6]. In this case, the cyst’s epithelium expressed PAX8, ER, and PR, indicative of Müllerian differentiation. The expression of PAX8 is a crucial immunohistochemical marker for Müllerian origin, and the presence of ER and PR suggests a hormonal influence on the cyst’s development. However, the serous papillary cystadenoma-like features observed in the cyst wall’s epithelium have not been previously documented in Müllerian cysts.
Our case presents an extraordinary and rare presentation that distinguishes it from typical Müllerian cysts encountered in clinical practice. Unlike conventional Müllerian cysts, which are benign fluid-filled sacs derived from Müllerian tissue, this case involves a complex transformation into a Müllerian epithelial papillary tumor, closely resembling ovarian serous papillary tumors. This unusual development underscores the complexity and diversity within the spectrum of Müllerian-derived lesions. A critical point to emphasize is that the presence of a papillary growth pattern might initially raise concerns about malignancy, particularly a low-grade carcinoma. However, key diagnostic features that differentiate a benign papillary tumor from a neoplastic one include minimal cellular atypia, well-defined borders, absence of invasive patterns on microscopic examination, and a low proliferation index. These characteristics are essential in distinguishing a benign entity from a potentially more aggressive tumor.
Our case exemplifies the importance of detailed pathological analysis and immunohistochemical profiling in cases with atypical features, such as a Müllerian cyst evolving into a papillary tumor. The rarity of this finding necessitates meticulous evaluation to ensure an accurate diagnosis, which is crucial for guiding patient management and prognosis.
Conclusion
This case represents a novel presentation of a Müllerian cyst in the posterior mediastinum, characterized by morphological features akin to serous papillary cystadenoma. This unique presentation adds to the limited literature on Müllerian cysts and underscores the necessity for comprehensive histopathological examination to identify such rare occurrences. Surgeons and pathologists should be cognizant of this variant to ensure accurate diagnosis and appropriate management. Future research should investigate the underlying mechanisms responsible for the development of Müllerian cysts with serous papillary cystadenoma-like features in the posterior mediastinum.
Funding Declaration: This research is supported by Hunan Provincial Department of Science and Technology (2021SK53520).
Author contributions
W.C., P.Z. and MY.P. wrote the main manuscript text, HJ.Y. prepared Fig. 1, and P.Z. prepared Figs. 2 and 3. All authors reviewed the manuscript.
Funding
Declaration: This research is supported by Hunan Provincial Department of Science and Technology (2021SK53520).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Peng Zhou, Email: zhouzipeng@csu.edu.cn.
Muyun Peng, Email: pengmuyun@csu.edu.cn.
Referances
- 1.Li XW, Xu PF, Wu QW, Wang MX. [Posterior mediastinal mullerian cyst: report of two cases]. Zhonghua Bing Li Xue Za Zhi. 2022;51(6):553–5. [DOI] [PubMed] [Google Scholar]
- 2.Hattori H. Ciliated cyst of probable mullerian origin arising in the posterior mediastinum. Virchows Arch. 2005;446(1):82–4. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan C, Swid MA, Klena JW, SA JK, Frank R. Mullerian cysts of the posterior mediastinum: a Case Report and Review of the literature. Cureus. 2022;14(11):e31298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skancke MD, Auzenne TD, Tabbara SO, Mortman KD. Thoracoscopic resection of multiple mullerian cysts. Ann Thorac Surg. 2015;100(5):1898–900. [DOI] [PubMed] [Google Scholar]
- 5.Thomas-de-Montpreville V, Dulmet E. Cysts of the posterior mediastinum showing mullerian differentiation (Hattori’s cysts). Ann Diagn Pathol. 2007;11(6):417–20. [DOI] [PubMed] [Google Scholar]
- 6.Chui MH, Ellenson LH. Mixed ovarian neoplasms with gastrointestinal-type mucinous and mullerian epithelial components: a Rare Group of tumors demonstrating the phenotypic plasticity of the mullerian epithelial cell. Am J Surg Pathol. 2023;47(7):756–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.