Abstract
Introduction
: Depression is a common and debilitating mental health issue among refugees in East Africa, who face numerous challenges. However, there is a lack of systematic reviews and meta-analyses that have explored the pooled prevalence and associated factors of depression among refugees in East Africa. This study aims to investigate the pooled prevalence of depression and its associated factors among refugees living in East Africa.
Methods
A systematic search was conducted across several databases, including PubMed/MEDLINE, CINAHL, ScienceDirect, African Journals of Online (AJOL), and Google Scholar. The quality of the included studies was assessed using a Joanna Briggs Institute (JBI) quality appraisal tool. Statistical analysis was carried out using STATA-17 software packages, and a meta-analysis was conducted using a random-effects model. Heterogeneity among the studies was assessed using the I2 statistic. Publication bias was evaluated using the DOI plot, Luis Furuya Kanamori (LFK) index, and Egger’s test. For associated factors of depression, effect sizes (odds ratio) with 95% confidence intervals were analyzed.
Result
A total of eight studies involving 6,388 participants were included in this systematic review and meta-analysis, all of which were assessed to have a low risk of bias. The pooled prevalence of depression was 50.60%, with a 95% CI (35.49%, 65.71). Regarding factors associated with depression; being female [(OR = 2.01; 95% CI (1.06, 3.82)], having poor social support [OR 5.88; 95% CI (2.53, 13.67)], and experienced eight or more traumatic events [OR = 3.31;95% CI (1.74, 6.31) were positively associated factors with depression.
Conclusion
The pooled prevalence of depression among refugees in East Africa was found to be significantly high. Female participants, poor social support, and experienced eight or more traumatic events were factors affecting depression among refugees in East Africa. Therefore, policymakers and health personnel in East Africa should prioritize addressing the needs of female participants, individuals with poor social support, and those who have experienced eight or more traumatic events.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-024-06371-1.
Keywords: Depression, Refugees, East Africa
Introduction
Depression is a common mental health disorder characterized by a persistent low mood or sadness, along with a loss of interest or pleasure in activities you once enjoyed [1]. It can also involve feelings of guilt, worthlessness, and difficulty concentrating [1]. Sleep, appetite, and energy levels are often disrupted, making it hard to complete daily tasks [2, 3]. Refugees are more susceptible to psychological distress, psychosomatic complaints, and clinical mental disorders, including depression and post-traumatic stress disorder, compared to other populations, such as individuals in stable housing, voluntary migrants, or the general population in host countries [4–7]. The global burden of depression increased from 172 million in 1990 to 25,8 million in 2017, with the highest rates in Lesotho (6.59 per 1000) and lowest in Myanmar (1.28 per 1000) [8]. Recent estimates indicate that refugees experience depression at two to four times the rate compared to the general population [9–11].
A global study estimated that 31.5% of such refugees experience depression [12]. Specifically in East Africa, research consistently shows a higher prevalence of depression among refugees compared to the general population [3, 13]. Studies report a range of 20–55%, with variations likely due to methodological differences and the specific refugee groups studied [14, 15]. Female refugees appear to be particularly vulnerable, with higher reported depression rates compared to males [16, 17], potentially due to gender-based violence and unequal access to resources. The consequences of depression among refugees are far-reaching, impacting individuals, families, and society as a whole. It can lead to a shortened lifespan, decreased quality of life, increased healthcare costs, and lower educational achievement and workplace productivity [18].
Refugees in East Africa, particularly from countries like South Sudan, the Democratic Republic of Congo (DRC), Rwanda, and others, face various stressors such as displacement, loss, violence, and uncertainty, leading to a significant mental health burden, including depression [19–21]. Depression among refugees can impede their integration into host communities, overall well-being, and productivity within society [22]. Factors contributing to depression in refugees include prolonged displacement, which increases rates due to chronic stress and uncertainty [23, 24]. Urban camps often show higher rates than rural ones, driven by limited support networks and isolation [25, 26]. Violence within camps is another major risk factor [26, 27]. Additionally, many refugee camps in East Africa face limited resources, poor sanitation, and food insecurity, exacerbating stress and psychological distress and increasing the risk of depression [28, 29].
Comprehensive data on depression among refugees in East Africa is urgently needed to address this critical public health concern. Despite its significant burden, summarizing data on the epidemiology of depression is scarce, leaving key challenges unexplored, including the interplay of pre- and post-displacement hardships, socioeconomic struggles, and cultural stigma [30]. Fear of discrimination and limited awareness further hinder help-seeking behaviors [31]. Uneven research distribution, especially in conflict-affected countries like South Sudan and Somalia, skews burden estimates and overlooks vulnerable groups such as lesbian, gay, bisexual, transgender, and intersex (LGBTQ+) individuals and female-headed households, who face unique stressors [12, 32, 33]. Additionally, inconsistencies in diagnostic tools and assessment methods complicate comparisons and meta-analyses, highlighting the need for standardized, inclusive, and region-specific research [12].
This systematic review and meta-analysis will provide robust estimates of depression prevalence among refugees, focusing on studies employing standardized research methods. It will examine the interplay of pre-displacement trauma, displacement experiences, host nation policies, and access to resources as key factors influencing mental health outcomes. In addition to identifying risk factors, the review will assess culturally relevant interventions for preventing and treating depression within this vulnerable population. Insights into refugees’ coping mechanisms and resilience strategies will help design effective mental health programs. By comparing outcomes across countries with varying asylum and integration policies, the analysis aims to inform more effective resettlement strategies. Ethical considerations, such as informed consent and cultural sensitivity, will be prioritized to ensure the integrity and inclusivity of research involving vulnerable groups.
Review questions
The following review questions provide a framework for this systematic review and meta-analysis:
-
i.
What is the pooled prevalence of depression among refugees in East Africa?
-
ii.
What are the associated factors for depression among refugees in East Africa?
Materials and methods
Reporting
The results of this systematic review and meta-analysis were prepared and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [34]. The protocol has been registered in the PROSPERO database with a registration number of CRD42024496728.
Study design, settings, and search strategies
We conducted a systematic review and meta-analysis to estimate the pooled prevalence of depression and identify associated factors among refugees in East Africa. A comprehensive search for relevant literature was conducted to identify published and unpublished studies. We searched electronic databases including PubMed/Medline, CINAHL, ScienceDirect, AJOL, and Google Scholar. Additionally, we searched online repository library centers for unpublished theses and dissertations. To capture potentially relevant gray literature, we reviewed the reference lists of included studies and consulted with content experts for their insights. The search strings or terms stemmed from the following keywords: depression, refugees, and East Africa. In the advanced search databases, the search strategy was built based on the above-mentioned terms using “Medical Subject Headings (MeSH)” and “Title/Abstract” by linking “AND” and “OR” Boolean operator terms, as appropriate. The details of the database search strategies are found in Supplementary File 1. The search was conducted between March 2 and April 29, 2024, and it included all papers published up to April 29, 2024.
Measurement outcome variables
This review had two outcomes: the primary outcome was to determine the pooled prevalence of depression among refugees in East Africa while the secondary outcome was to identify the factors associated with depression. Independent variables were sex (female vs. male), social support (poor social support vs. good social support), and cumulative traumatic events ( vs.
vs.  .
.
Eligibility criteria
The study included all refugee populations without age restrictions, focusing on articles reported in English. Eligible studies comprised observational designs that reported the prevalence of depression and were conducted specifically in East Africa. Both published and unpublished studies were considered. However, studies on non-refugee populations, those not addressing the primary outcomes of interest, and articles in languages other than English were excluded. Additionally, conference proceedings, interventional studies, qualitative research, commentaries, editorial letters, case reports, case series, and monthly or annual police reports were not included in the analysis.
Search guide
The “CoCoPop search guide” framework was employed to design a systematic and comprehensive search strategy, ensuring alignment with the study’s objectives. The framework focused on three core components: Outcome/Condition, which targeted depression; Population, encompassing all refugee populations; and Context/Setting, restricted to East Africa. By structuring the search strategy around these elements, the guide facilitated the identification of relevant studies, ensuring consistency and precision in capturing data specific to the epidemiology of depression among refugees in East Africa. This approach was integral to the conception and execution of the search strategies in the study.
Selection of studies
We used EndNote X9, a reference management software, to collect and organize the initial search results, manage citations, and efficiently remove duplicates. To ensure article relevance, we employed a rigorous three-step screening process. In the first two steps, both authors (AHS & AAS) independently reviewed titles and abstracts against the predefined eligibility criteria using EndNote. Titles deemed relevant then progressed to the third stage, where we reviewed the full text of the articles. Only studies approved by both authors were included for final data extraction. Any disagreements between the reviewers were resolved through discussion, and if necessary, by consulting a third reviewer (BFK). We documented the reasons for excluding studies to create a transparent and verifiable final list for data analysis.
Data extraction and management.
Two independent authors (AHS and AAS) extracted data from eligible articles using a standardized format based on the Joanna Briggs Institute (JBI) data extraction form for systematic reviews and research syntheses [35, 36]. To ensure consistency and accuracy, the authors first pilot-tested the data extraction process on a subset of articles in Microsoft Excel before proceeding with the full dataset.
Study characteristics (first author, publication year, country, study design, sample size), response rate, quality rating, depression assessment tool, and prevalence of depression were included in the data extraction form. Disagreements during extraction were actively resolved for consensus, with a third reviewer (BFK) consulted if needed, ensuring the highest accuracy and consistency in capturing all crucial information.
Quality assessment of the studies
Two independent reviewers (AHS and AAS) critically evaluated each study using the Joanna Briggs Institute (JBI) tool [37–39] checklists for analytical cross-sectional and cohort study studies. To ensure consistent quality assessment, any disagreements between the two initial reviewers were addressed by revisiting the study together. If necessary, a third reviewer (BFK) was brought in to reach final appraisal scores.
Data processing and statistical analysis
We used Microsoft Excel to extract the necessary data from the studies. Then, we imported this data into the STATA version 17 statistical software program to analyze the combined results. Measuring heterogeneity based on statistical findings, outcome presentations, and methodologies was done using the I2 statistic and a chi-squared test by Cochran’s Q statistic with a 5% significance level [40]. I2 values of 25%, 50%, and 75% are considered indicative of low, moderate, and high heterogeneity, respectively [41]. According to the results of the statistical test, there was significant heterogeneity among the included original studies (I2 = 99.4%, p < 0.001), hereafter, the random-effects meta-analysis model [42] was used to estimate the pooled prevalence of depression and its associated factors.
We performed subgroup analysis to address two key questions. First, we aimed to see if subgrouping the data could reduce the natural variability (random variation) seen in the original study’s results (point estimates). Second, we wanted to explore how the rate of failure (fluctuates) differed between subgroups within the study population. Additionally, we employed sensitivity analysis by using the leave-one-out method to assess the influence of potential outliers on our findings. Furthermore, publication bias was assessed using the DOI plot [43], Luis Furuya Kanamori (LFK) index [44], and Egger’s test. For the LFK index, a value falling outside the range of -1 to 1 was interpreted as indicating asymmetry, which suggests the presence of publication bias. For the associated factors, we reported odds ratios, their corresponding confidence intervals, and p-values to effectively demonstrate the strength and direction of the relationships between depression and its associated factors.
Results
Exploration of studies
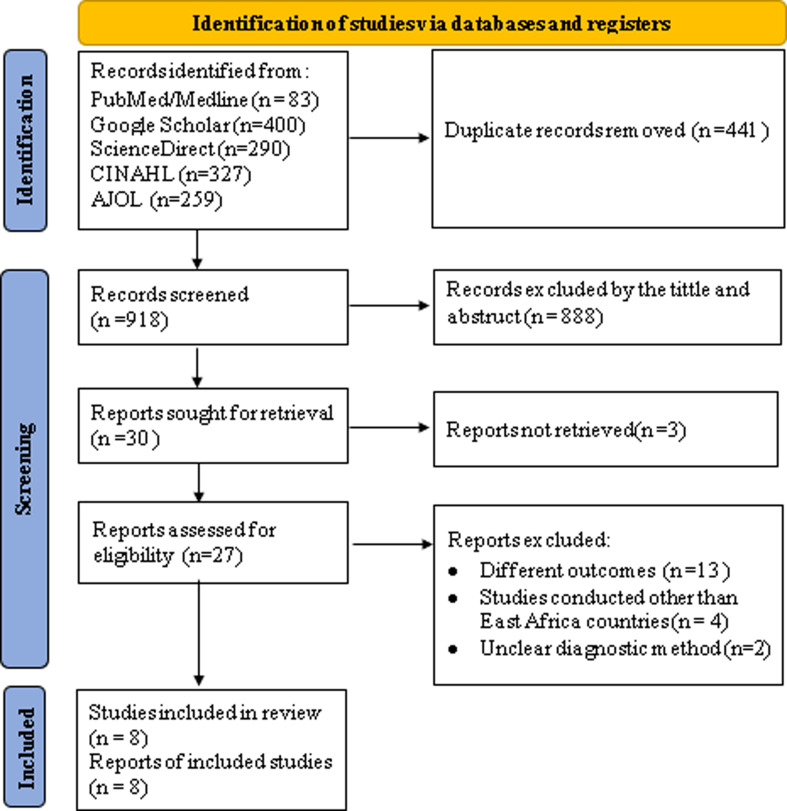
A total of 1359 articles were identified using various electronic databases such as PubMed, Google Scholar, ScienceDirect, CINAHL, and African Journals of Online (AJOL). Of these initial articles, there were about 919 non-duplicated articles (records screened). From the remaining articles, 889 articles were excluded after a review of their titles and abstracts, and 3 additional articles were excluded after we were unable to retrieve the full reports. Then, 27 potentially full-text articles were assessed for eligibility based on the pre-set criteria and 19 articles were further excluded due to different reasons [45–63]. Ultimately, 8 articles met the eligibility criteria and were included in the final meta-analysis to determine the prevalence and associated factors of depression (Fig. 1).
Fig. 1.
PRISMA flow diagram of screened and the selection process of studies on the pooled prevalence of depression and associated factors among refugees in East Africa, 2024
Quality of included studies
The methodological quality scores for the eight studies included in this review were assessed using the JBI quality assessment tool. Seven of these studies were cross-sectional, and one was a cohort study. Studies were considered high quality if they scored ≥ 6 for cross-sectional studies and ≥ 9 for the cohort study. The eight studies that met the specified criteria were included in the final systematic review and meta-analysis (Table 1).
Table 1.
Joanna Briggs Institute (JBI) critical appraisal of the included studies, 2024
| Included Articles | Criterion No (items included to appraise analytical cross-sectional studies) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total (%) | Overall quality |
| Ali et al. [64] | 2023 | √ | √ | √ | √ | √ | √ | √ | √ | 100 | High | |||
| Berhe et al. [65] | 2021 | √ | √ | √ | X | √ | √ | √ | √ | 87.5 | High | |||
| Feyera et al. [66] | 2015 | √ | √ | √ | √ | √ | √ | √ | √ | 100 | High | |||
| Roberts, B. et al.[61] | 2008 | X | √ | √ | √ | X | √ | √ | √ | 75 | High | |||
| Melese et al. [67] | 2024 | √ | √ | √ | √ | √ | √ | √ | √ | 100 | High | |||
| Gebreyesus et al. [68] | 2024 | √ | √ | √ | √ | √ | √ | √ | √ | 100 | High | |||
| Misghinna et al. [69] | 2020 | √ | √ | √ | X | X | √ | √ | √ | 75 | High | |||
| Logie, C. H et al. [70] | 2022 | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | 100 | High |
| √= Yes, criterion fulfilled, X= No, criterion not fulfilled | ||||||||||||||
For cross-sectional (Item 1: Were the criteria for inclusion in the sample clearly defined? Item 2: Were the study subjects and the setting described in detail? Item 3: Was the exposure measured validly and reliably? Item 4: Were objective, standard criteria used for measurement of the condition? Item 5: Were confounding factors identified? Item 6: Were strategies to deal with confounding factors stated? Item 7: Were the outcomes measured validly and reliably? Item 8: Was appropriate statistical analysis used?) and for the cohort -study we considered a JBI 11 items
Characteristics of the included studies
Seven cross-sectional studies and one cohort study were included in the final systematic review and meta-analysis and were published between 2008 and 2024. Among the included studies, four studies were conducted in Ethiopia [65–68], three in Uganda [61, 69, 70], and one in Somalia [64]. In this review and meta-analysis, a total of 6,388 participants were involved to determine the pooled prevalence of depression and associated factors with a minimum sample size of 374 [69] and a maximum of 1990 [68].
The response rates in the included primary studies ranged from 94.5% in northern Uganda [61] to 100% in Dabat town, northwest Ethiopia [67], and Kampala, Uganda [69, 70]. Regarding prevalence, the lowest prevalence (28.9%) of depression was reported in a study done in Kampala, Uganda [70], whereas the highest prevalence (81.2%) was reported in a study done in the Tigray region in Ethiopia [68] (Table 2).
Table 2.
Summary of the characteristics of eight studies included in the systemic review and meta-analysis on prevalence and associated factors of depression among refugees in East Africa, 2024
| Authors | Publication year | Country | Refugees come from |
Study design | Sample size | Response rate (%) | PoD(%) | Risk of bias | Tool |
|---|---|---|---|---|---|---|---|---|---|
| Ali et al. [64] | 2023 | Somalia | IDPs | CS | 401 | 99.5 | 59.4 | Low | HSC-25 |
| Berhe et al. [65] | 2021 | Ethiopia | Eritrean | CS | 800 | 98.3 | 37.8 | Low | PHQ-9 |
| Feyera et al. [66] | 2015 | Ethiopia | IDPs | CS | 847 | 98.1 | 38.3 | Low | PHQ-9 |
| Roberts, B. et al.[61] | 2008 | Uganda | IDPs | CS | 1210 | 94.5 | 67 | Low | HSC-25 |
| Melese et al. [67] | 2024 | Ethiopia | Eritrean | CS | 399 | 100 | 45 | Low | DASS-21 |
| Gebreyesus et al. [68] | 2024 | Ethiopia | IDPs of Tigray | CS | 1990 | 98.7 | 81.2 | Low | PHQ-9 |
| Misghinna et al. [69] | 2020 | Uganda | IDPs | CS | 374 | 100 | 46.5 | Low | DSM-5 |
| Logie, C. H et al. [70] | 2022 | Uganda | IDPs | CoS | 367 | 100 | 28.9 | Low | PHQ-9 |
IDPs = internally displaced persons; CS = cross-sectional study; CoS = cohort study; PoD; prevalence of Depression
Risk of bias assessment
Concerning the quality of the included studies, seven studies [61, 64–69] were assessed based on the JBI checklist for cross-sectional studies, and the remaining one study [70] was based on the JBI checklist for cohort studies. According to this quality assessment criterion, all studies included are classified as having a low risk of bias (Table 2).
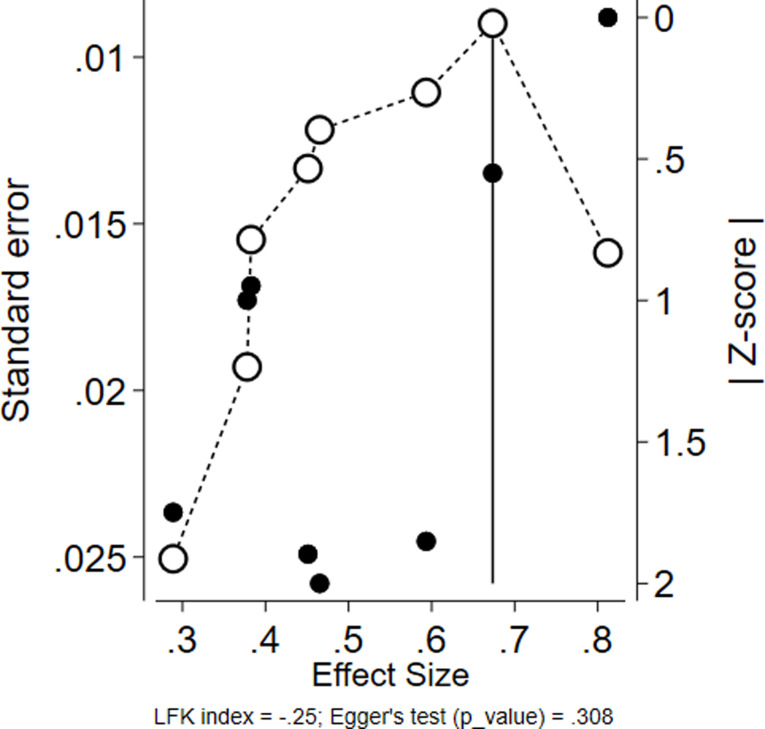
Result of publication bias assessment
To assess potential publication bias, we utilized the DOI plot [43] and the Luis Furuya-Kanamori (LFK) index [44]. Egger’s test results (p = 0.308) were not statistically significant (p > 0.05), indicating no strong evidence of publication bias for the estimated pooled prevalence of depression. Additionally, the LFK index value (-0.25) fell within the acceptable range of -1 to 1, confirming symmetry in the DOI plot and supporting the absence of publication bias in the included studies (Fig. 2).
Fig. 2.
PAssessment of publication bias of included studies using Doi plot and LFK index among refugees in East Africa, 2024
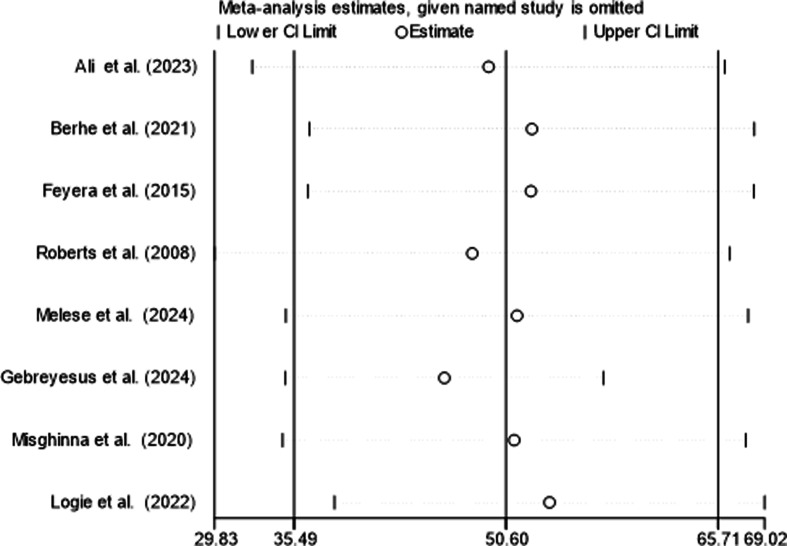
Sensitivity analysis test
The result of the leave-one-out method for the evaluation of sensitivity analysis revealed that there is no significant influence of individual studies on the pooled prevalence of depression, demonstrating the robustness of the result (Fig. 3).
Fig. 3.
Sensitivity analysis to determine a single study effect on the pooled prevalence of depression among refugees in East Africa, 2024
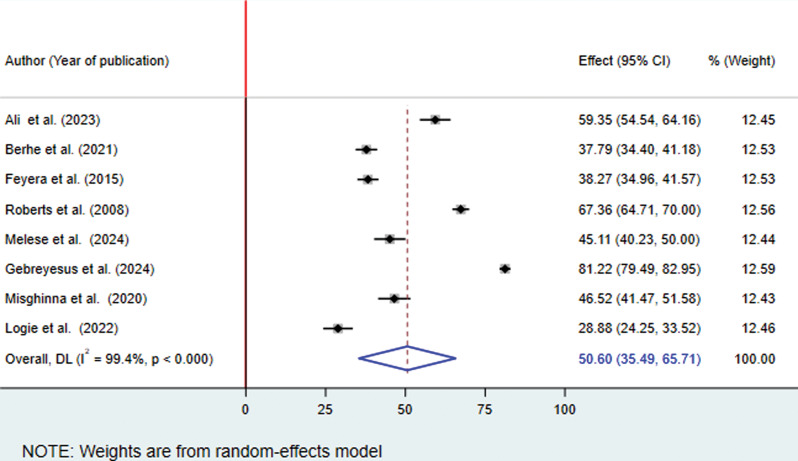
The result of the estimated pooled prevalence of depression among refugees in East Africa
The pooled prevalence of depression among refugees in East Africa was 50.60% (95% CI: 35.49, 65.71). Given the statistically significant heterogeneity observed between studies (I² = 99.4%, p < 0.001), we applied a random-effects meta-analysis model to estimate the pooled prevalence of depression among refugees in East Africa (Fig. 4).
Fig. 4.
Forest plot showing the pooled prevalence of depression among refugees in East Africa, 2024
Subgroup analysis
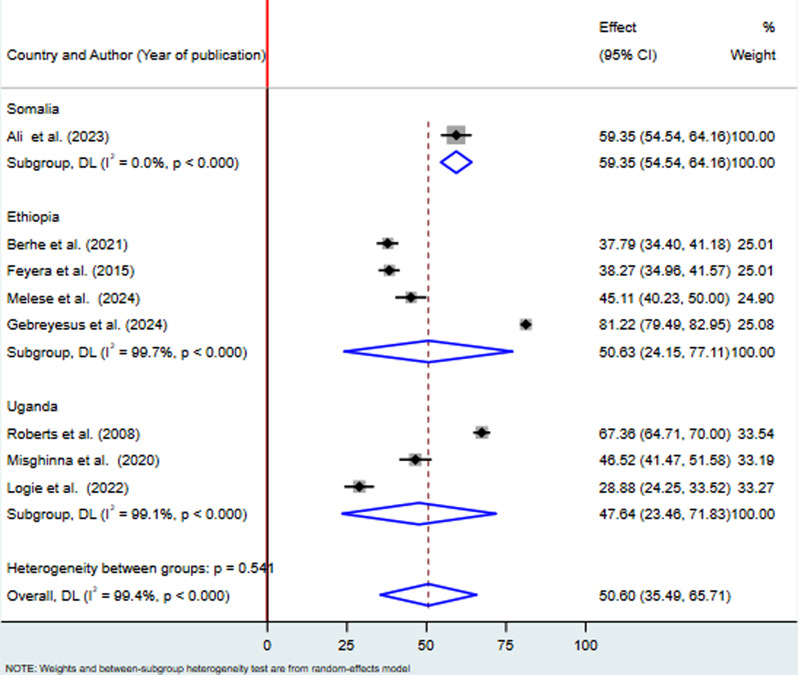
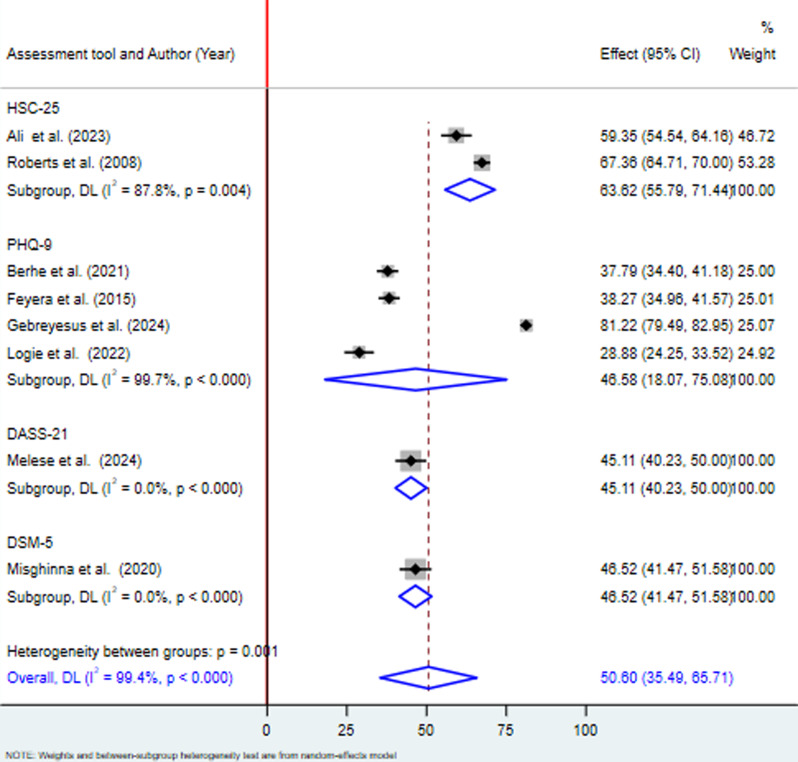
To explore potential variations, we conducted a subgroup analysis based on the countries and assessment tools used in the included studies. Regarding the pooled prevalence by country the lowest pooled prevalence of depression among refugees was reported in Uganda 47.64% (95% CI 23.46, 71.83; I2 = 99.1%, p < 0.001) and the highest was in Ethiopia 50.63% (95% CI 24.15, 77.11; I2 = 99.7%, p < 0.001). The results also indicated that there was a significant level of heterogeneity in the studies conducted in both countries. Since the study conducted in Somalia County was a single study, there was no heterogeneity test (Fig. 5). Moreover, two articles were conducted with HSC-25, around four articles were conducted with PHQ-9, one article was conducted with DASS-21, and one study was conducted with a DSM-5. The pooled prevalence of depression by using HSC-25 and PHQ-9 was 63.62% with 95% CI (55.79, 71.44) and 46.58% with 95% CI (18.07, 75.08) respectively. The heterogeneity of each tool, HSC-25, and PHQ-9 was significant (I2 = 87.8, Q = 8.18, df = 1, P < 0.004), and (I2 = 99.7, Q = 1063.43, df = 3, p < 0.001) respectively. Since the study conducted by the DASS-21 and by the DSM-5 assessment tools was a single study, there was no heterogeneity test (Fig. 6).
Fig. 5.
Forest plot presenting subgroup analysis by country for the pooled prevalence of depression among refugees in East Africa, 2024
Fig. 6.
Forest plot presenting subgroup analysis by assessment tool for the pooled prevalence of depression among refugees in East Africa, 2024
Associated factors of depression among refugees in East Africa
In this systematic review and meta-analysis, five studies were used to identify factors associated with depression among refugees in East Africa [61, 64–67].
Association between depression and female participants
Four studies were included to reveal the association between depression and female participants [61, 65–67]. There was a significant association between female participants and depression. The finding showed that female participants were about 2 (OR = 2.01, 95%, CI: 1.06, 3.82; I2 = 94.3%, p = 0.001) times more likely to have depression when compared to male participants (Table 3).
Table 3.
A result of factors associated with depression among refugees in East Africa, 2024
| Variables | Pooled OR (95%CI) | Number of studies included | I2 with p-values |
|---|---|---|---|
| Sex | |||
| Male | 1.00 | ||
| Female | 2.01(1.06, 3.82) | 4 | 94.3%, p < 0.001 |
| Social support | |||
| Good | 1.00 | ||
| Poor | 5.88(2.53, 13.67) | 2 | 82.7%, p < 0.016 |
| Cumulative traumatic events | |||

|
1.00 | ||

|
3.31(1.74, 6.31) | 3 | 88.6%, p < 0.001 |
Certainty of evidence using GRADE approach
Association between depression and social support
Two studies were carried out in this meta-analysis [65, 67]. The pooled odds ratio (OR) demonstrated that the odds of depression were significantly higher in participants who had poor social support than in participants who had good social support (OR = 5.88, 95%, CI: 2.53, 13.67) (I2 = 82.7%, p = 0.016) (Table 3).
Association between depression and cumulative traumatic events
A total of three articles were included in this meta-analysis [64–66]. There was a significant association between cumulative traumatic events and depression. Participants who had experienced eight or more traumatic events were more likely to have depression (OR = 3.31, 95%, CI: 1.74, 6.31; I2 = 88.6%, p = 0.001) as compared to participants who had experienced less than eight traumatic events (Table 3).
The certainty of evidence for the pooled prevalence of depression is rated as low, while the certainty for associated factors is very low. This reflects the need for additional high-quality, geographically diverse studies using standardized diagnostic tools to address the observed heterogeneity and improve the precision of effect estimates. According to GRADE recommendations [71], further research is very likely to improve confidence in the effect estimates and may result in substantial changes to these estimates (Supplementary File 2).
Discussion
This systematic review and meta-analysis were conducted in East African countries to estimate the pooled prevalence of depression and its associated factors among refugees. This study will contribute to the development of public health strategies aimed at preventing and treating depression in this vulnerable population by emphasizing early detection, culturally appropriate mental health interventions, and ongoing care to improve the overall well-being of refugees. The current study included eight studies with a total of 6,388 participants, to estimate the pooled prevalence of depression and associated factors among refugees in East Africa. This study only assessed articles performed in Ethiopia, Uganda, and Somalia due to limited study availability in other East African countries. Most of the included studies were limited by cross-sectional designs, small sample sizes, and the use of the PHQ-9 tool. However, all studies were assessed as having a low risk of bias according to the JBI tool checklists, indicating high methodological quality.
In this meta-analysis, the pooled prevalence of depression among refugees in East Africa was 50.60% (95%CI:35.49, 65.71%). The current pooled prevalence of depression in East Africa was significantly higher than that reported in a systematic review and meta-analysis of adult Syrian refugees [72] (31%), in15 countries [12] (31.5%), and in 5 countries [73] (13.81%). In addition, this finding was higher than that of a study conducted in 18 low-middle-income and high-income countries (32%) [74]. The discrepancy might be due to the severity of conflicts, East Africa has unfortunately experienced numerous protracted conflicts, some with ongoing violence. The nature and severity of these conflicts could be more impactful on mental health compared to conflicts in other regions included in the broader reviews [75]. The other possibility might be due to limited resources and support, refugees in East Africa might face greater challenges due to limited access to mental healthcare, social support systems, and basic necessities compared to refugees in other regions [76]. Furthermore, there is a possibility that the rising prevalence of depression and the predicted epidemic in developing countries may contribute to this.
Similarly, the current finding was significantly higher than the prevalence reported using fixed effect analysis in similar East African countries [3] (31%). The possible explanation for the observed variations might be due to differences in methodology. The fixed effect model assumes a single common effect size for all studies. This might underestimate the true variation in depression prevalence between countries. The random effects model acknowledges the potential for variation and provides a more conservative estimate that reflects the average effect across the included countries [77].
Significant variation (heterogeneity) in the prevalence of depression was found between the studies included in this review. To explore this variation and understand potential sources of differences, we conducted a subgroup analysis. Accordingly, the subgroup analysis of this study revealed that Uganda reported the lowest pooled prevalence of depression (47.64%) [61, 69, 70], while Ethiopia had the highest (50.63%) [65–68]. This difference might be explained by factors like the recent war in Ethiopia’s Tigray region, potentially causing greater displacement and hardship for refugees there. It is also important to consider the possibility that variations in sample sizes between studies from these countries might have influenced the observed prevalence differences.
In this review, we also investigated factors associated with depression among refugees in East Africa. Female participants, poor social support, and cumulative traumatic events were identified as factors associated with depression among refugees in East Africa.
Female participants were two times more likely to have depression than male participants. This finding is supported by studies conducted in different nations [78], North Korea [79], Lebanon [80], Greece [81], and Kenya [82]. Potential reasons for this higher prevalence may include exposure to gender-based violence, as women in conflict zones are more vulnerable to sexual assault, domestic violence, and other forms of GBV, which are significant risk factors for depression [83]. In addition, societal expectations surrounding female behavior and emotional expression may also make it more difficult for women to seek help for mental health issues [84]. Furthermore, the limited resources and challenging living conditions in refugee camps may be more burdensome for women due to childcare and household responsibilities [85].
Participants who had poor social support were about six times more likely to have depression when compared to participants who had good social support. This finding was consistent with studies conducted in different nations [78], urban Somali refugees [86], and in Ethiopia [87]. This is the fact that poor social support can lead to feelings of isolation and loneliness, which are significant risk factors for depression [88] and refugees who lack strong social connections may have difficulty accessing emotional support and feel more alone in dealing with their struggles [76]. Cultural factors might influence how social support is expressed and perceived. For example, some cultures may have a stronger emphasis on family support, while others may place more value on community connections [89].
Finally, participants who had experienced eight or more traumatic events were more likely to have depression as compared to participants who had experienced less than eight traumatic events. This finding is supported by studies conducted in different nations [90], South Korea [91], Germany [92], urban Somali refugees [86], Syrian refugee women [93], and in Somalia [64]. This might be because individuals experiencing eight or more traumas might have faced more severe or prolonged events, leading to a greater psychological impact and increased risk of depression [94] and repeated exposure to trauma can erode an individual’s resilience - the ability to cope with adversity. This can leave them feeling overwhelmed and less able to bounce back from stressful events, making them more susceptible to depression [95].
Biological and neuropsychological hypotheses suggest that trauma and depression are linked through several mechanisms. Chronic trauma can dysregulate the HPA axis, leading to elevated cortisol levels, which are associated with depression. Inflammation in the brain, caused by trauma, can disrupt mood regulation and increase the risk of depressive symptoms. Additionally, trauma may result in structural changes in key brain areas, such as the hippocampus and amygdala, which affect emotional regulation. Neurotransmitter imbalances, particularly in serotonin, dopamine, and norepinephrine, also play a critical role in both trauma and depression [96].
The finding has implications for future researchers, clinicians, and policymakers; for future researchers, the high prevalence of depression highlights a need for further investigation. More research is crucial to understand the reasons behind this and develop better management strategies. These findings emphasize the importance of screening for depression among refugees, both in healthcare institutions and community settings. The study can inform policymakers in designing and implementing effective prevention and treatment programs for depression within refugee communities and healthcare systems across East Africa.
Strengths and limitations of this study
This systematic review adheres to the PRISMA guidelines and offers a comprehensive analysis of depression prevalence and associated factors among refugees in East African countries. To minimize bias and ensure quality, we searched multiple databases and employed dual reviewer screening. The review estimates pooled prevalence rates, identifies pooled associated factors, and conducts subgroup analyses based on countries and assessment tools.
The limitations of this study include high heterogeneity among the included studies and restricted geographic coverage, with data available only from three countries (Ethiopia, Uganda, and Somalia), which may limit the generalizability of findings to other East African nations or global refugee populations. The study’s focus on English-language articles may have excluded relevant research published in other languages, and the scarcity of eligible studies from other countries in the region further narrows the geographical scope. Additionally, while the exclusion of studies using alternative outcome measurement approaches ensured methodological consistency, it may have led to the omission of valuable insights. Variability in diagnostic tools, underrepresentation of key subpopulations (e.g., LGBTQ + refugees), and imprecise estimates with wide confidence intervals due to small sample sizes further contribute to low certainty for prevalence and very low certainty for associated factors, emphasizing the need for more diverse, high-quality studies with standardized methodologies to strengthen the evidence base.
Conclusions
In this meta-analysis, the pooled prevalence of depression among refugees in East Africa was found to be significantly higher than that of host populations. The findings suggest that public health policymakers should focus on strengthening social support networks for refugees and implementing comprehensive mental health interventions, with particular attention to female refugees and those with a history of cumulative trauma. These strategies are essential for reducing depression prevalence and enhancing overall health outcomes among refugees. Therefore, regional policymakers and healthcare providers should prioritize interventions aimed at addressing the needs of female refugees, individuals with limited social support, and those who have experienced multiple traumatic events, as these factors are key contributors to mental health challenges within this population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We express our deepest gratitude to Samara University for their generous gift of free internet and library access, and all the authors of primary studies.
Abbreviations
- AJOL
African Journals of Online
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- DASS-21
Depression, Anxiety, and Stress Scale
- DSM-5
Diagnostic and Statistical Manual of Mental Disorder
- GBV
Gender-Based Violence
- GRADE
Grading of Recommendations, Assessment, Development, and Evaluations
- HSC-25
Hopkins Symptom Checklist
- JBI
Joanna Briggs Institute
- LGBTQ+
Lesbian, Gay, Bisexual, Transgender and Intersex
- LMIC
Low- and Middle-Income Countries
- MeSH
Medical Subject Headings
- PHQ-9
patient health questionnaire
- PRISMA
Preferred Reporting Items for Systematic Review and Meta-Analysis
- PTSD
Post-Traumatic Stress Disorder
Author contributions
AHS, AAS and BFK were design, analysis and interpretation of data; and responsible for the drafting of the article. AHS, AAS, BFK, AHM and MGM were involved in acquisition of data, analysis and interpretation of data. All authors read and approved the final manuscript.
Funding
No grants or funding were received from any public, private, or nonprofit sectors for this review.
Data availability
All data generated or analyzed during this study are available from the corresponding author with a reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Organization WH, Depression. 2023. https://www.who.int/news-room/fact-sheets/detail/depression
- 2.Tareke SA, Lelisho ME, Shibeshi AH, Muze MQ, Jabir YN, Wolde KS et al. Depressive symptoms among residents of south Wollo Zone in Northern Ethiopia after the liberation of invasion of TPLF led force. Heliyon. 2023;9(2). [DOI] [PMC free article] [PubMed]
- 3.Pozuelo JR, Bradenbrink R, Stierna MF, Sterck O. Depression, violence and socioeconomic outcomes among refugees in East Africa: evidence from a multicountry representative survey. BMJ Ment Health. 2023;26(1). [DOI] [PMC free article] [PubMed]
- 4.Feyera F, Mihretie G, Bedaso A, Gedle D, Kumera G. Prevalence of depression and associated factors among Somali refugee at melkadida camp, southeast Ethiopia: a cross-sectional study. BMC Psychiatry. 2015;15(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giacco D, Laxhman N, Priebe S, editors. Prevalence of and risk factors for mental disorders in refugees. Seminars in cell & developmental biology. Elsevier; 2018. [DOI] [PubMed]
- 6.Disney L, McPherson J. Understanding refugee mental health and employment issues: implications for social work practice. J Social Work Global Community. 2020;5(1):2. [Google Scholar]
- 7.Organization WH. World report on the health of refugees and migrants. 2022.
- 8.Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the Global Burden of Disease study. J Psychiatr Res. 2020;126:134–40. [DOI] [PubMed] [Google Scholar]
- 9.Frankova I, Scheeres K, Menculini G, Cikrikcili U, Matei IC, Fellinger M, et al. Forcibly displaced persons and mental health: a survey of the experiences of Europe-wide psychiatry trainees during their training. Transcult Psychiatry. 2023;60(1):167–75. Epub 2022/11/08. doi: 10.1177/13634615221135421. PubMed PMID: 36344237. [DOI] [PubMed] [Google Scholar]
- 10.Verhagen IL, Noom MJ, Lindauer RJL, Daams JG, Hein IM. Mental health screening and assessment tools for forcibly displaced children: a systematic review. Eur J Psychotraumatol. 2022;13(2):2126468. PubMed PMID: 36212114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.AMADI D. Resilience in African female refugees and internally displaced persons (IDPs) living with mental health issues. 2021.
- 12.Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med. 2020;17(9):e1003337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berhe SM, Azale T, Fanta T, Demeke W, Minyihun A. Prevalence and predictors of Depression among Eritrean refugees in Ethiopia: a cross-sectional survey. Psychol Res Behav Manag. 2021;14:1971–80. PubMed PMID: 34916858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vigneswaran D, Quirk J. Quantitative methodological dilemmas in urban refugee research: a case study of Johannesburg. J Refugee Stud. 2013;26(1):110–6. [Google Scholar]
- 15.Sulaiman-Hill CMR, Thompson SC. Sampling challenges in a study examining refugee resettlement. BMC Int Health Hum Rights. 2011;11(1):2. 10.1186/1472-698X-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jensen MA. Gender-based violence in refugee camps: understanding and addressing the role of gender in the experiences of refugees. Inquiries J. 2019;11(02).
- 17.Tastsoglou E, Petrinioti X, Karagiannopoulou C. The gender-based violence and precarity nexus: asylum-seeking women in the Eastern Mediterranean. Front Hum Dynamics. 2021;3:660682. [Google Scholar]
- 18.Stecher C, Cloonan S, Domino ME. The Economics of Treatment for Depression. Annu Rev Public Health. 2024;45. [DOI] [PubMed]
- 19.Nowak AC, Nutsch N, Brake T-M, Gehrlein L-M, Razum O. Associations between postmigration living situation and symptoms of common mental disorders in adult refugees in Europe: updating systematic review from 2015 onwards. BMC Public Health. 2023;23(1):1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abera S, Niguss T, Tesfahun E, Mulu T, Kindu B, Tulu M. Prevalence of Mental disorders and factors associated with it among Ethiopian migrant returnees from the Middle East. 2023.
- 21.Knappe F, Filippou K, Hatzigeorgiadis A, Morres ID, Tzormpatzakis E, Havas E, et al. Psychological well-being, mental distress, metabolic syndrome, and associated factors among people living in a refugee camp in Greece: a cross-sectional study. Front Public Health. 2023;11:1179756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fennig M, Denov M. The impact of trauma, flight and protracted displacement on the mental health of Eritrean refugees living in Israel: an exploratory study of coping strategies. SSM-Mental Health. 2022;2:100102. [Google Scholar]
- 23.Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, et al. Common mental health problems in immigrants and refugees: general approach in primary care. CMAJ. 2011;183(12):E959–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siriwardhana C, Stewart R. Forced migration and mental health: prolonged internal displacement, return migration and resilience. Int Health. 2013;5(1):19–23. [DOI] [PubMed] [Google Scholar]
- 25.Logie CH, Okumu M, Mwima S, Hakiza R, Chemutai D, Kyambadde P. Contextual factors associated with depression among urban refugee and displaced youth in Kampala, Uganda: findings from a cross-sectional study. Confl Health. 2020;14:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Logie CH, Okumu M, Mwima S, Hakiza R, Irungi KP, Kyambadde P, et al. Social ecological factors associated with experiencing violence among urban refugee and displaced adolescent girls and young women in informal settlements in Kampala, Uganda: a cross-sectional study. Confl Health. 2019;13(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frounfelker RL, Islam N, Falcone J, Farrar J, Ra C, Antonaccio CM, et al. Living through war: Mental health of children and youth in conflict-affected areas. Int Rev Red Cross. 2019;101(911):481–506. [Google Scholar]
- 28.Torre C. Think positive, save a life? Resilience and Mental Health Interventions as Political Abandonment in a Refugee settlement in Northern Uganda. Civil Wars. 2023:1–27.
- 29.Scharpf F, Masath FB, Mkinga G, Kyaruzi E, Nkuba M, Machumu M, et al. Prevalence of suicidality and associated factors of suicide risk in a representative community sample of families in three east African refugee camps. Soc Psychiatry Psychiatr Epidemiol. 2024;59(2):245–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. Stigma and discrimination related to mental illness in low-and middle-income countries. Epidemiol Psychiatric Sci. 2015;24(5):382–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sickel AE, Seacat JD, Nabors NA. Mental health stigma update: a review of consequences. Adv Mental Health. 2014;12(3):202–15. [Google Scholar]
- 32.Nematy A, Namer Y, Razum O. Lgbtqi + refugees’ and asylum seekers’ mental health: a qualitative systematic review. Sexuality Res Social Policy. 2023;20(2):636–63. [Google Scholar]
- 33.Patanè M, Ghane S, Karyotaki E, Cuijpers P, Schoonmade L, Tarsitani L et al. Prevalence of mental disorders in refugees and asylum seekers: a systematic review and meta-analysis. Global Mental Health. 2022:1–14. [DOI] [PMC free article] [PubMed]
- 34.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 35.Joanna Briggs Institute. Reviewers’ Manual: 2017 edition. Australia. 2017. 2019.
- 36.Joanna Briggs Institute. data extraction form for review for systematic reviews and research syntheses,. 2014.
- 37.Institute JB. Critical appraisal tools 2020.
- 38.Institute JB. Joanna Briggs Institute Reviewers’ Manual: 2017 edition. Australia: The Joanna Briggs Institute; 2017. 2019.
- 39.Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synthesis. 2020;18(10):2127–33. [DOI] [PubMed] [Google Scholar]
- 40.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–29. [Google Scholar]
- 41.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. [DOI] [PubMed] [Google Scholar]
- 42.Berkey CS, Hoaglin DC, Mosteller F, Colditz GA. A random-effects regression model for meta‐analysis. Stat Med. 1995;14(4):395–411. [DOI] [PubMed] [Google Scholar]
- 43.Furuya-Kanamori L, Barendregt JJ, Doi SA. A new improved graphical and quantitative method for detecting bias in meta-analysis. JBI Evid Implement. 2018;16(4):195–203. [DOI] [PubMed] [Google Scholar]
- 44.Furuya-Kanamori L, LFK. Stata module to compute LFK index and Doi plot for detection of publication bias in meta-analysis. 2021.
- 45.Betancourt TS, Speelman L, Onyango G, Bolton P. A qualitative study of mental health problems among children displaced by war in northern Uganda. Transcult Psychiatry. 2009;46(2):238–56. 10.1177/1363461509105815. Epub 2009/06/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Devries KM, Fabbri C, Allen E, Barongo V, Shayo E, Greco G, et al. Preventing violence against children in schools (PVACS): protocol for a cluster randomised controlled trial of the EmpaTeach behavioural intervention in Nyarugusu Refugee camp. BMC Public Health. 2019;19(1):1295. 10.1186/s12889-019-7627-y. Epub 2019/10/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ertl V, Pfeiffer A, Schauer-Kaiser E, Elbert T, Neuner F. The challenge of living on: psychopathology and its mediating influence on the readjustment of former child soldiers. PLoS ONE. 2014;9(7):e102786. 10.1371/journal.pone.0102786. Epub 2014/07/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fabbri C, Rodrigues K, Leurent B, Allen E, Qiu M, Zuakulu M et al. The EmpaTeach intervention for reducing physical violence from teachers to students in Nyarugusu Refugee Camp: A cluster-randomised controlled trial. PLoS Med. 2021;18(10):e1003808. Epub 2021/10/05. doi: 10.1371/journal.pmed.1003808. PubMed PMID: 34606500; PubMed Central PMCID: PMCPMC8489723 following competing interests: the EmpaTeach intervention was developed by KR at the International Rescue Committee and MK, GTE, and ADF at the Behavioral Insights Team. They have provided input into study design but final decisions on study design and procedures were taken by KD. [DOI] [PMC free article] [PubMed]
- 49.Getnet B, Medhin G, Alem A. Symptoms of post-traumatic stress disorder and depression among Eritrean refugees in Ethiopia: identifying direct, meditating and moderating predictors from path analysis. BMJ Open. 2019;9(1):e021142. 10.1136/bmjopen-2017-021142. Epub 2019/01/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Getnet B, Alem A. Validity of the Center for Epidemiologic Studies Depression Scale (CES-D) in Eritrean refugees living in Ethiopia. BMJ Open. 2019;9(5):e026129. 10.1136/bmjopen-2018-026129. Epub 2019/05/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lamkaddem M, Essink-Bot ML, Deville W, Gerritsen A, Stronks K. Health changes of refugees from Afghanistan, Iran and Somalia: the role of residence status and experienced living difficulties in the resettlement process. Eur J Public Health. 2015;25(6):917–22. 10.1093/eurpub/ckv061. Epub 2015/04/12. [DOI] [PubMed] [Google Scholar]
- 52.Lincoln AK, Lazarevic V, White MT, Ellis BH. The impact of Acculturation Style and Acculturative hassles on the Mental Health of Somali Adolescent Refugees. J Immigr Minor Health. 2016;18(4):771–8. 10.1007/s10903-015-0232-y. Epub 2015/06/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Logie CH, Okumu M, Malama K, Mwima S, Hakiza R, Kiera UM et al. Examining the substance use, violence, and HIV and AIDS (SAVA) syndemic among urban refugee youth in Kampala, Uganda: cross-sectional survey findings. BMJ Glob Health. 2022;7(Suppl 5). Epub 2022/07/08. 10.1136/bmjgh-2021-006583. PubMed PMID: 35798442; PubMed Central PMCID: PMCPMC9263932. [DOI] [PMC free article] [PubMed]
- 54.Meffert SM, Marmar CR. Darfur refugees in Cairo: mental health and interpersonal conflict in the aftermath of genocide. J Interpers Violence. 2009;24(11):1835–48. Epub 2008/10/24. doi: 10.1177/0886260508325491. PubMed PMID: 18945917; PubMed Central PMCID: PMCPMC6777844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meffert SM, Musalo K, Abdo AO, Alla OA, Elmakki YO, Omer AA, et al. Feelings of betrayal by the United Nations High Commissioner for refugees and emotionally distressed Sudanese refugees in Cairo. Med Confl Surviv. 2010;26(2):160–72. PubMed PMID: 20718287; PubMed Central PMCID: PMCPMC6777846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meyer SR, Steinhaus M, Bangirana C, Onyango-Mangen P, Stark L. The influence of caregiver depression on adolescent mental health outcomes: findings from refugee settlements in Uganda. BMC Psychiatry. 2017;17(1):405. 10.1186/s12888-017-1566-x. Epub 2017/12/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Muller LRF, Gossmann K, Hartmann F, Buter KP, Rosner R, Unterhitzenberger J. 1-year follow-up of the mental health and stress factors in asylum-seeking children and adolescents resettled in Germany. BMC Public Health. 2019;19(1):908. 10.1186/s12889-019-7263-6. PubMed PMID: 31286909; PubMed Central PMCID: PMCPMC6615278. Epub 2019/07/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mumin FI, Wesonga FD, Handuleh JIM, White RG, Mor SM. COVID-19 and its prevention in internally displaced person (IDP) camps in Somalia: impact on livelihood, food security and mental health. BMC Public Health. 2022;22(1):2414. 10.1186/s12889-022-14878-z. Epub 2022/12/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stress Disorder and Depression Among Women at Ekerenyo Camp for the Internally Displaced (2).pdf>.
- 60.<prevalence-of-depressive-disorders-and-associated-demographic-factors-among-refugees-amidst-covid19-in-nakivale-refugee-.pdf>.
- 61.Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:38. 10.1186/1471-244X-8-38. Epub 2008/05/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tol WA, Greene MC, Likindikoki S, Misinzo L, Ventevogel P, Bonz AG, et al. An integrated intervention to reduce intimate partner violence and psychological distress with refugees in low-resource settings: study protocol for the Nguvu Cluster randomized trial. BMC Psychiatry. 2017;17(1):186. 10.1186/s12888-017-1338-7. Epub 2017/05/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tol WA, Leku MR, Lakin DP, Carswell K, Augustinavicius J, Adaku A, et al. Guided self-help to reduce psychological distress in South Sudanese female refugees in Uganda: a cluster randomised trial. Lancet Glob Health. 2020;8(2):e254–63. 10.1016/S2214-109X(19)30504-2. Epub 2020/01/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ali M, Mutavi T, Mburu JM, Mathai M. Prevalence of posttraumatic stress disorder and depression among internally displaced persons in Mogadishu-Somalia. Neuropsychiatr Dis Treat. 2023:469–78. [DOI] [PMC free article] [PubMed]
- 65.Berhe SM, Azale T, Fanta T, Demeke W, Minyihun A. Prevalence and predictors of depression among Eritrean refugees in Ethiopia: a cross-sectional survey. Psychol Res Behav Manage. 2021:1971–80. [DOI] [PMC free article] [PubMed]
- 66.Feyera F, Mihretie G, Bedaso A, Gedle D, Kumera G. Prevalence of depression and associated factors among Somali refugee at Melkadida camp, Southeast Ethiopia: a cross-sectional study. BMC Psychiatry. 2015;15. 10.1186/s12888-015-0539-1.: 171. Epub 2015/07/25. [DOI] [PMC free article] [PubMed]
- 67.Melese M, Simegn W, Esubalew D, Limenh LW, Ayenew W, Chanie GS, et al. Symptoms of posttraumatic stress, anxiety, and depression, along with their associated factors, among Eritrean refugees in Dabat town, northwest Ethiopia, 2023. BMC Psychol. 2024;12(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gebreyesus A, Niguse AT, Shishay F, Mamo L, Gebremedhin T, Tsegay K, et al. Prevalence of depression and associated factors among community hosted internally displaced people of Tigray; during war and siege. BMC Psychiatry. 2024;24(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Misghinna TK, Nakimuli-Mpungu E, Abbo C, Kinyanda E, Fellowship T, Misghinna TK. Major depressive disorder and associated factors among adult refugees attending a refugee center in Kampala, Uganda. Afr J Trauma Stress. 2020;5(1):1–21. [Google Scholar]
- 70.Logie CH, Berry I, Okumu M, Loutet M, McNamee C, Hakiza R, et al. The prevalence and correlates of depression before and after the COVID-19 pandemic declaration among urban refugee adolescents and youth in informal settlements in Kampala, Uganda: a longitudinal cohort study. Ann Epidemiol. 2022;66:37–43. PubMed PMID: 34785396; PubMed Central PMCID: PMCPMC8590831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schunemann H, Brozek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations (The GRADE Working Group). http://gdt.guidelinedevelopment.org/app/handbook/handbook. html; 2013.
- 72.Nguyen TP, Guajardo MGU, Sahle BW, Renzaho AM, Slewa-Younan S. Prevalence of common mental disorders in adult Syrian refugees resettled in high income western countries: a systematic review and meta-analysis. BMC Psychiatry. 2022;22:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Blackmore R, Gray KM, Boyle JA, Fazel M, Ranasinha S, Fitzgerald G, et al. Systematic review and meta-analysis: the prevalence of mental illness in child and adolescent refugees and asylum seekers. J Am Acad Child Adolesc Psychiatry. 2020;59(6):705–14. [DOI] [PubMed] [Google Scholar]
- 74.Patanè M, Ghane S, Karyotaki E, Cuijpers P, Schoonmade L, Tarsitani L, et al. Prevalence of mental disorders in refugees and asylum seekers: a systematic review and meta-analysis. Global Mental Health. 2022;9:250–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights. 2015;15:1–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Klabbers RE, Ashaba S, Stern J, Faustin Z, Tsai AC, Kasozi J et al. Mental disorders and lack of social support among refugees and Ugandan nationals screening for HIV at health centers in Nakivale Refugee settlement in southwestern Uganda. J Global Health Rep. 2022;6. [DOI] [PMC free article] [PubMed]
- 77.Dettori JR, Norvell DC, Chapman JR. Fixed-effect vs random-effects models for meta-analysis: 3 points to consider. Global Spine J. 2022;12(7):1624–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bedaso A, Duko B. Epidemiology of depression among displaced people: a systematic review and meta-analysis. Psychiatry Res. 2022;311:114493. [DOI] [PubMed] [Google Scholar]
- 79.김연희 조영아. A study on the prevalence and the influencing factors of the mental health problems among recent migrant North koreans: a focus on 2007 entrants. Unification Policy Stud. 2010;19(2):141–74. [Google Scholar]
- 80.Naal H, Nabulsi D, El Arnaout N, Abdouni L, Dimassi H, Harb R, et al. Prevalence of depression symptoms and associated sociodemographic and clinical correlates among Syrian refugees in Lebanon. BMC Public Health. 2021;21:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Poole DN, Hedt-Gauthier B, Liao S, Raymond NA, Bärnighausen T. Major depressive disorder prevalence and risk factors among Syrian asylum seekers in Greece. BMC Public Health. 2018;18:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Musau JN, Omondi M, Khasakhala L. The prevalence of post-traumatic stress disorder (PTSD) among internally displaced persons (IDPs) in Maai Mahiu Camp in Nakuru County, Kenya. J Intern Displacement. 2018;8(1):20–33. [Google Scholar]
- 83.Hossain M, Pearson RJ, McAlpine A, Bacchus LJ, Spangaro J, Muthuri S, et al. Gender-based violence and its association with mental health among Somali women in a Kenyan refugee camp: a latent class analysis. J Epidemiol Community Health. 2021;75(4):327–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nyikavaranda P, Pantelic M, Jones CJ, Paudyal P, Tunks A, Llewellyn CD. Barriers and facilitators to seeking and accessing mental health support in primary care and the community among female migrants in Europe: a feminisms systematic review. Int J Equity Health. 2023;22(1):196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fazel M, Betancourt TS. Preventive mental health interventions for refugee children and adolescents in high-income settings. Lancet Child Adolesc Health. 2018;2(2):121–32. [DOI] [PubMed] [Google Scholar]
- 86.Swan LE, Im H. Risk and protective factors for common mental disorders among urban Somali refugee youth. J Child Adolesc Trauma. 2021;14(3):321–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Anbesaw T, Kassa MA, Yimam W, Kassaw AB, Belete M, Abera A et al. Factors associated with depression among war-affected population in Northeast, Ethiopia. BMC Psychiatry. 2024;24. [DOI] [PMC free article] [PubMed]
- 88.Erzen E, Çikrikci Ö. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry. 2018;64(5):427–35. [DOI] [PubMed] [Google Scholar]
- 89.Kaplan V, Düken ME. Mental health states of the refugee women in the 10-year visiting process: an assessment in context of the sociocultural adaptation. Middle East Curr Psychiatry. 2023;30(1):72. [Google Scholar]
- 90.Ronzani P, Stojetz W, Stammel N, Boettche M, Zardetto D, Fenzl S, et al. Prevalence of Depression and Associated Socio-economic outcomes during violent conflict: a matched analysis for Palestine using nationally Representative Survey and Conflict Event Data. medRxiv. 2024;202402:23–24303259. [Google Scholar]
- 91.Sohn JH, Lim J, Lee JS, Kim K, Lim S, Byeon N et al. Prevalence of possible depression and post-traumatic stress disorder among community dwelling adult refugees and refugee applicants in South Korea. J Korean Med Sci. 2019;34(11). [DOI] [PMC free article] [PubMed]
- 92.Nesterko Y, Jäckle D, Friedrich M, Holzapfel L, Glaesmer H. Factors predicting symptoms of somatization, depression, anxiety, post-traumatic stress disorder, self-rated mental and physical health among recently arrived refugees in Germany. Confl Health. 2020;14:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hosseini Z, Bakdash T, Ahmad S, Awaad R. Predictors of depression among Syrian refugee women: a socio-culturally relevant analysis. Int J Soc Psychiatry. 2023;69(5):1223–30. [DOI] [PubMed] [Google Scholar]
- 94.Gerber MM, Frankfurt SB, Contractor AA, Oudshoorn K, Dranger P, Brown LA. Influence of multiple traumatic event types on mental health outcomes: does count matter? J Psychopathol Behav Assess. 2018;40:645–54. [Google Scholar]
- 95.Watters ER, Aloe AM, Wojciak AS. Examining the associations between childhood trauma, resilience, and depression: a multivariate meta-analysis. Trauma Violence Abuse. 2023;24(1):231–44. [DOI] [PubMed] [Google Scholar]
- 96.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49(12):1023–39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are available from the corresponding author with a reasonable request.