Abstract
Objective
At present there is no clear, cohesive, and comprehensive theoretical understanding of the role of core beliefs in the development of disordered eating. The present study aimed to develop and test a theoretical model outlining important processes and pathways from core beliefs to eating disorder (ED) behaviours. It also aimed to explore potential differences (or similarities) in contributions of four core belief dimensions to the development and maintenance of ED symptomatology.
Method
Data were collected from a sample of 800 non-clinical participants. Path analysis was conducted to test general and multi-dimensional models. Indirect effects were calculated for all possible pathways from ED core beliefs to dietary restraint, objective binge eating, and compensatory behaviours.
Results
The hypothesised model demonstrated poor to acceptable fit to the data. Modifications were made to the general model to improve fit, remove non-significant paths and add theoretically and statistically relevant paths. All indirect effects of possible pathways from core beliefs to ED behaviours were significant. A multi-dimensional version of the model was tested with four core belief dimensions. This model identified differences in pathways from each core belief dimension to ED symptoms.
Discussion
This study extends the current understanding of the role of core beliefs in the development and maintenance of disordered eating, by building upon previous theoretical models and empirical literature. We present a general core beliefs model of disordered eating, and preliminary findings regarding differences in the processes and pathways from four key core belief dimensions to ED behaviours.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-024-01167-w.
Keywords: Eating disorders, Core beliefs, Symptoms, Theory, Model, Processes
Plain language summary
This study extends our current understanding of how core beliefs in eating disorders relate to the development of key disordered eating symptomatology. We present a comprehensive model, which builds upon previous theoretical and empirical understandings of the processes and pathways from core beliefs to dietary restraint, objective binge eating, and compensatory behaviours. We also present preliminary findings regarding potential differences in the processes that explain the relationship of four critical core belief dimensions relevant to eating disorders in contributing to the development of these behaviours.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-024-01167-w.
Introduction
Core beliefs are sets of cognitive constructs that have received increased theoretical and empirical attention in recent decades and which have been identified as important features in eating disorder (ED) development and maintenance processes [1–3]. Core beliefs can be defined as a set of deeply held, pervasive and persistent, unconditional beliefs about oneself, others, or the world [4, 5]. Beck [6] originally proposed that early negative life experiences are central to the formation of these beliefs, and as such the cognitive content of these beliefs are often negative, maladaptive or dysfunctional. Although it has been suggested that core beliefs in EDs will often represent global negative evaluations of the self [1], various dimensions of core beliefs have been identified as particularly prevalent or important in the development and maintenance of disordered eating [7, 8].
Potential factors contributing to limitations in the treatment of EDs have been well-documented [9]. Most evidence-based treatments focus on maintenance factors over aetiological factors, and the cognitive focus of treatment primarily is often on thoughts and attitudes relating to food, weight and shape, with less attention paid to challenging and correcting global, deeply entrenched beliefs [3, 9, 10]. In addition to low remission rates, high comorbidity in EDs indicates that it is important to move beyond the dominant focus of treatment on ‘surface-level’ cognitions, and behaviours involved in ED maintenance, suggesting that factors implicated in the development of EDs, such as unhelpful core beliefs, should become a more critical focus of treatment [11].
At present, the literature lacks a clear, comprehensive, and wholistic understanding of of how core beliefs and various core belief dimensions relate to the development and maintenance of disordered eating symptoms. Various theoretical ED models attempt to capture cognitive factors akin to ‘core beliefs’, using concepts such as ‘schema’, ‘core low self-esteem’, or ‘negative self-beliefs’. Although the terms ‘core belief’ and ‘schema’ have often been used interchangeably in the literature [10], schemas are proposed to include both unconditional cognitive content (i.e., core beliefs), conditional beliefs, as well as other cognitive processes and behaviours [12], [13]). Similarly, low self-esteem has been conceptualised as a broad, pervasive theme or pattern, consisting of various types of cognitions (e.g., core beliefs, assumptions, and predictions) as well as emotions ([14]; [5].
In order to form a clear and comprehensive theoretical understanding of the critical role of core beliefs in the processes and pathways that best explain ED symptomatology, several seminal models of disordered eating that have been advanced, and also informed the development of effective interventions [9] will be reviewed. Despite important differences in terminology and constructs outlined above, the theoretical models that broadly include a ‘core belief’ (or similar) component are presently considered, including the 1) the transdiagnostic maintenance model of eating disorders [15], 2) the cognitive model of bulimia nervosa [16], 3) the integrated cognitive and behavioural model of binge eating [17], and 4) the schema-focused cognitive behavioural model of eating disorders [12].
The transdiagnostic maintenance model of eating disorders
The transdiagnostic maintenance model of EDs suggests that ‘core low self-esteem’, defined as an unconditional, often pervasive, negative views of the self, contributes to an increasingly dysfunctional schema for self-evaluation [15]. This schema includes the over-evaluation of achieving ‘perfectionism’, which then contributes directly to the over-evaluation of eating, weight, shape, and their control. This over-evaluation is hypothesised to lead to restriction, dieting and other behaviours designed to control weight, which in turn results in either binge eating and compensatory behaviours, or low weight and ‘starvation syndrome’. The transdiagnostic ED model also includes a general mood intolerance component, proposed to further impact both binge eating and compensatory behaviours.
Although this model has been influential in informing CBT for EDs [18], and has also been validated several times in various populations [19–23], close examination of these studies indicates that no studies have operationalised core low self-esteem with a measure that reflects a set of unconditional beliefs about the self. Typically, measures have been utilised that reflect more general affective evaluations of the self, such as the Rosenberg Self Esteem Scale [24] or the Eating Disorders Inventory III low self-esteem subscale [25]. Further, although the construct of ‘core low self-esteem’ was originally conceptualised to convey pervasive, negative views of the self [15], this model does not attempt to recognise the importance of other core belief dimensions that may be important in the development of disordered eating symptomatology. Finally, and importantly, this framework does not attempt to examine formulation in a longitudinal manner with specific recognition or inclusion of developmental factors, nor does it make advancements in understanding the role of various types of cognition in the development and maintenance of EDs [1].
The cognitive model of bulimia nervosa
The cognitive model of bulimia nervosa (BN) is a second-generation theory that attempts to address some of the limitations of the transdiagnostic maintenance model, by including developmental factors and other important cognitive constructs and content [1, 16]. Cooper and colleagues proposed that early, negative childhood experiences may lead to the development of maladaptive, negative self-beliefs (e.g., I’m worthless), which, when triggered, activate underlying assumptions or negative automatic thoughts about eating, weight and shape [16]. The idea of ‘negative self-beliefs’ is similar to that of core low self-esteem outlined in Fairburn et al.’s [15] maintenance model, however, was instead conceptualised as a critical predisposing or developmental factor. Negative automatic thoughts are then proposed to trigger emotional states which commonly precede binge eating (e.g., anxiety, stress, depression), which in turn trigger meta-cognitive beliefs about eating, including positive, negative and permissive beliefs, ultimately resulting in binge eating and purging behaviours [16].
The cognitive model of BN offers an enhanced understanding of how negative self-beliefs or core beliefs contribute to the development of bulimic pathology, and includes other key cognitive content not considered in the other models (e.g., meta-cognitive beliefs about eating). There is evidence in support of several processes in this model in both clinical and non-clinical populations [26, 27], and this model has led to the development of an integrated meta-cognitive and cognitive therapy for treating BN and binge eating [28]. Nonetheless, this framework only addresses bulimic and binge eating pathology. It does not attempt to address how core beliefs lead to the development of restrictive pathology, nor does it acknowledge important pathways to binge eating and compensatory behaviours via restrictive eating (i.e., behavioural processes).
Integrated cognitive and behavioural model of binge eating
Recently, an integrated cognitive and behavioural model of binge eating was proposed in order to conceptualise important processes and pathways to binge eating [17]. The integrated cognitive and behavioural model integrates components from previous theoretical models and empirical research and includes critical cognitive, emotion-related, and behavioural variables implicated in binge eating. The model indicates two predominant pathways from ‘core low self-esteem’ to binge eating via either dietary restraint or meta-cognitive beliefs about binge eating (positive, negative and permissive beliefs). Additionally, the model indicates that negative affect and difficulties with emotional regulation can serially mediate the effect of core low self-esteem on binge eating through both of these pathways (i.e., dietary restraint or eating belief pathways).
The integrated cognitive behavioural model provides a novel conceptualisation of hypothesised pathways between core low self-esteem and binge eating symptomatology. Strengths of this model include its inclusion of several important pathways to binge eating, via meta-cognitive beliefs, affective states, and dietary restraint. It contains similarities to both the transdiagnostic maintenance model of EDs and cognitive model of BN, whilst partially addressing some of the shortcomings of these models, or elements not addressed in previous models [15, 16]. However, this model was specifically created to conceptualise binge eating, and as such does not attempt to include or address other key disordered eating symptoms, such as compensatory behaviours [17]. Although dietary restraint was considered in the model, no indirect or direct pathways or effects to this variable were tested, as the authors only tested the overall model. Furthermore, other key variables considered in previous models, such as perfectionism [15] and negative thoughts or preoccupation with food, weight and shape [15, 16], were not features of this model.
Schema-focused cognitive behavioural model of eating disorders
The schema-focused cognitive behavioural model of eating disorders was developed in attempt to clearly delineate the role of schema level representations in the development of different eating pathology [12]. The schema-focused model proposes that the content of core beliefs or belief dimensions are similarly critical across EDs but that ‘schema processes’ differ in the development of restrictive and bulimic pathology [12]. These schema processes function to regulate affect (i.e., reduce negative affective), via the mechanism of either schema compensation or schema avoidance [12]. Waller and colleagues hypothesised that in restrictive eating, schema compensation occurs as a function of primary avoidance of negative affective states and schema activation [12]. Conversely, in bulimic pathology, schema avoidance occurs as a function of secondary avoidance of negative affective states, where resulting behaviours (i.e., purging) serve a function to temporarily avoid the negative state induced by schema activation [12].
Though distinct in their focus, Waller et al. [12] identified similarities between their newly developed model and Fairburn et al. [15] maintenance model and proposed that the two may be potentially complementary. For example, Waller et al. [12] suggested ‘core low self-esteem’ may be similar to ‘defectiveness core beliefs’, that ‘perfectionism’ is similar to ‘unrelenting standards core beliefs, and that ‘mood intolerance/affect regulation’ is similar to ‘schema avoidance’. However, despite this suggestion, no research has tested the compatibility of these models by combining their key variables and processes, in order to conceptualise the role of core beliefs in the development of disordered eating symptomatology. Further, despite the use of the term ‘schemas’ when referring to unconditional core beliefs, this term is frequently utilised in assessment tools (e.g., the Young Schema Questionnaire) to typically include various other constructs, such as conditional beliefs and assumptions, affective evaluations, and behaviours [29].
Assessing and differentiating core belief dimensions and their role in key disordered eating symptomatology
It has been suggested that core beliefs in EDs often represent global negative evaluations of the self [1]. Core beliefs in EDs have previously been assessed using a general, negative self-beliefs subscale [30]. However, more recent advancements in this area have identified a number of core belief dimensions of particular potential significance to the development and maintenance of disordered eating, as well as providing theoretically consistent and psychometrically valid ways to operationalise these dimensions [7, 8, 31]. These dimensions include 1) Self-loathing, 2) Abandoned/Deprived, 3) Demanding/Needing help or support, and 4) Unassertive/Inhibited unconditional negative core beliefs. Several studies have validated the importance of self-loathing, feeling abandoned or isolated, believing oneself to be demanding, needing help, or being unassertive or emotionally inhibited for individuals with clinical ED symptomatology or sub-clinical disordered eating cognitions and behaviours [7, 8, 27, 31].
However, despite recent research identifying core belief domains that are specifically related to EDs, there is very little understanding of how these different core beliefs dimensions differentially (or similarly) influence the development of diverse disordered eating symptoms and behaviours. None of the aforementioned models have attempted to examine the processes and pathways from diverse core belief dimensions to critical ED behaviours, such as dietary restraint, binge eating, or compensatory behaviours. Although there have been clear associations between ED-related core beliefs and ED symptomatology [7, 8, 27, 31], at present the literature lacks; 1) a clear, cohesive, and comprehensive understanding of how ED core beliefs influence the development of critical ED symptoms, and 2) clarity regarding the potentially differential (or similarities in the) influence of diverse ED core belief dimensions on disordered eating behaviours.
Current Study
Each of the reviewed theoretical models has contributed to our understanding of how core beliefs (or comparable constructs) impact the development of disordered eating symptomatology. However, as noted by both Cooper [1] and Waller [12], there is need for cognitive theories to continue to evolve, as well as to improve conceptualisations of EDs by integrating theoretical models. In attempt to create a clear, cohesive, and comprehensive theoretical understanding of how ED core beliefs influence the development of disordered eating symptoms, we have reviewed key pathways and processes from previous models and attempted to build upon their strengths as well as to address key limitations. The present study had two primary aims.
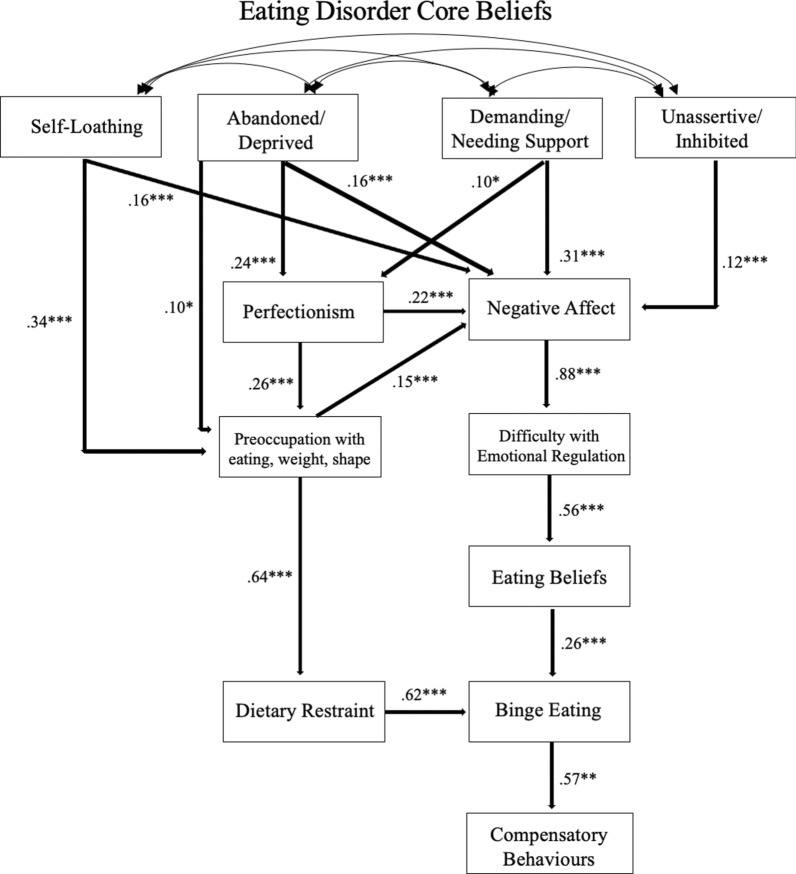
Firstly, we aimed to develop and test a general theoretical model outlining the important processes and pathways from ED core beliefs to core ED symptomatology and behaviours. This hypothesised model is displayed in Fig. 1. We predicted that the hypothesised model (Fig. 1) would demonstrate acceptable fit to the data. Within the general model, specific pathways to core ED behavioural symptomatology were tested by calculating indirect effect of various paths from ED core beliefs to 1) dietary restraint, 2) objective binge eating (OBE), and 3) compensatory behaviours.
Fig. 1.
Hypothesised Core Beliefs Model of Disordered Eating
Secondly, we aimed to conduct exploratory analysis into the potential differences in contributions of different core belief dimensions to the development of varied ED symptomatology, in order to assess whether processes and pathways were similar between ED core beliefs. To do so, tested a multi-dimensional version of the general model, by assessing the relative strengths of relationships of four important ED core belief dimensions (‘Self-Loathing’, ‘Abandoned/Deprived’, Demanding/Needing support’, and ‘Unassertive/Inhibited’) to established pathways to ED symptomatology, whilst controlling for the presence of each of the other core belief dimensions included the model.
Method
Participants and procedure
All procedures performed in studies involving human participants were in accordance with the ethical standards of The University of Sydney Human Research Ethics Committee (Project Code: 2022/856), including informed consent and debriefing participants after their participation. Participants were undergraduate psychology students, recruited through the University of Sydney’s online psychology research participation system, who voluntarily participated in exchange for course credit. All participants were provided with a participant information statement with information regarding the aims of this study, provided informed consent to participate, then voluntarily completed an online test battery of questionnaires using Qualtrics Survey Software. From the larger test battery, each of the measures described in the measures section and demographic information were collected and analysed in the present study.
Of the 884 that responded to the survey, 800 participants completed all the measures of interest and were subsequently included in analyses (74.9% female; mean age = 20.43 years, SD = 4.44 years; Ethnic Background, 55.3% Asian, 30.5% Caucasian, 9.8% Other, 3.4% Middle Eastern, and 1% as Indigenous Australian). To ensure sufficient statistical power was obtained, we obtained the minimum sample sizes suggested based off a variety of sources from several simulation studies, and guidelines for conducting structural equation models (SEM; [32–34]). [35–37]).
In this sample, 3.6% of participants reported that they had been given a formal diagnosis of anorexia nervosa (AN) by a health professional, 2% a diagnosis of BN, 1.4% a diagnosis of binge eating disorder (BED), and 1.5% a diagnosis of another ED (e.g., other specified feeding or eating disorder [OSFED], eating disorder not otherwise specified [EDNOS], unspecified feeding or eating disorder [UFED], etc.). The lifetime prevalence rates in the current sample are in the expected range, with a recent review finding the global lifetime prevalence of any ED ranges from approximately 0.74 to 8.4% [38]. Using an EDE-Q cut-off score of 2.5 or higher, 24.6% of the sample were considered ‘ED-symptomatic’. This criterion has previously been used with the intention of exploring individuals with a presence of both clinical and sub-clinical (or prodromal) symptomatology [8, 31], Ro et al., 2015), based on literature suggesting that optimal EDE-Q clinical cut-off scores vary from 1.68 to 2.93 [39–42],Ro et al., 2015; [43], as compared to the more exclusionary clinical cut-off of 4.0 [18, 44]. Further, the ‘ED-symptomatic’ rate (24.6%) in the present sample is also comparable to the findings from a recent review indicating the prevalence of ‘disordered eating’ in Australian samples to be 25.7% [38].
The relevant EDE-Q items were used to assess OBE and compensatory behaviours. Of the included participants, 29% reported having experienced at least four binge eating episodes accompanied by the experience of loss of control over their eating in the last 28 days (range = 0 to 58), and 25.2% reported having experienced at least four episodes of compensatory behaviours (i.e., purging, use of laxatives or exercising in a compulsive manner) in the last 28 days (range = 0 to 84).
Measures
Depression anxiety stress scales (DASS-21)
In order to assess ‘negative affect’, the present study utilised the DASS-21[45]. The DASS-21 is a 21-item self-report questionnaire that examines symptoms of depression, anxiety and stress, by asking participants to rate items according to how much each statement applied to them over the past week on a scale of 0 (Did not apply to me at all) to 3 (Applied to me very much or most of the time) (e.g., ‘I felt I wasn’t worth much as a person’). Scores ranged from 21 to 84, where higher scores reflect higher negative affect. This measure has demonstrated good psychometric properties cross-culturally [46]. In the present study, the overall DASS-21 demonstrated acceptable internal consistency (Ω = 0.94).
Difficulties in emotion regulation scale brief version (DERS-16)
In order to assess ‘Difficulties with Emotional Regulation’, the DERS-16 was utilised in the present study [47]. The DERS-16 is a 16-item self-report questionnaire measuring emotional regulation difficulties, that asks participants to rate items according to how much each statement applies to them from a scale of 1 (Almost never) to 5 (Almost always) (e.g., ‘When I am upset, I feel out of control’). Scores range from 1–5, where higher scores reflect greater difficulties in emotion regulation. It has demonstrated good psychometric properties in both clinical and community samples [47], as well as compared with other DERS versions [48]. In the present study, the DERS-16 demonstrated acceptable internal consistency (Ω = 0.94).
Eating beliefs questionnaire 18 (EBQ-18)
The EBQ-18 was used in order to assess ‘eating beliefs’ in the current study [49]. The EBQ-18 is a self-report questionnaire that examines positive, negative and permissive meta-cognitive beliefs about binge eating (e.g., ‘Once I start eating, I can’t stop’). Items are rated on a scale from Strongly disagree (1) to Strongly agree (5). Scores range from 1–5, The EBQ-18 has demonstrated validity, reliability and clinical utility [49, 50]. The overall EBQ-18 demonstrated acceptable internal consistency in our sample (Ω = 0.92).
Eating disorder core beliefs questionnaire revised (ED-CBQ-R)
To assess ED core beliefs, the present study utilised the ED-CBQ-R, a 15-item self-report measure that assesses core beliefs relating to EDs [8]. The ED-CBQ-R contains four subscales, reflecting four dimensions of core beliefs,‘Self-loathing, ‘Unassertive/Inhibited, ‘Demanding/Needing help and support’, and ‘Abandoned/Isolated’. Items (e.g., ‘selfish’) are rated on a 7-point scale (Feels very much untrue [1] to Feels very much true [7]), where higher scores reflect higher ED core beliefs. The ED-CBQ-R has previously demonstrated acceptable internal consistency (α or Ω = 0.73 to 0.92) and construct validity [8, 31], as well as the overall ED-CBQ-R and each of the four subscales in the present study (Ω = 0.78 to 0.92).
Eating disorder examination questionnaire (EDE-Q)
The EDE-Q was utilised to assess ‘preoccupation with eating, weight and shape’, ‘dietary restraint’, ‘binge eating’, and ‘compensatory behaviours’ [51]. This gold-standard measure is a 28-item self-report questionnaire that assesses the frequency and severity of ED symptoms experienced 28 days prior to assessment. To measure preoccupation with eating, weight and shape, we utilised an overall mean score from the eating concerns, weight concerns and shape concerns subscales. Items were rated on a 7-point scale (No days [0] to Every day [6]). The preoccupation score (Ω = 0.95) and dietary restraint subscale (Ω = 0.86) had acceptable internal consistency. Further, item 13 was utilised to measure OBE (frequency over the last 28 days), and a combined score from items 16, 17 and 18 utilised to measure compensatory behaviours (i.e., purging, use of laxatives, and exercising in a ‘compulsive’ manner).
Frost multidimensional perfectionism scale – brief (FMPS-B)
The FMPS-B was utilised to assess ‘Perfectionism’ in the current study [52]. This scale is a brief 8-item assessment tool measuring perfectionism (striving and evaluative concerns, e.g., ‘I have extremely high goals’), where items are rated on a 5-point scale (Strongly disagree [1] to Strongly agree [5]). The FMPS-B has demonstrated good internal consistency and construct validity in community and clinical samples [52], and when utilised as an overall perfectionism construct in the current study had acceptable internal consistency (Ω = 0.80).
Statistical Analyses
Statistical analyses were carried out using IBM Statistical Package for Social Sciences (SPSS) Statistics (version 26.0) predictive analytics software and R Project for Statistical Computing [53]. Internal consistency of scales utilised were assessed using McDonald’s Omega (Ω) (values > 0.70 and < 0.95 were considered acceptable [36, 54],). Demographic characteristics were examined, data distribution was examined for all variables to assess for violations of normality assumptions, descriptive statistics reported, and Kendall’s Tau (τ) correlations to examine the relationships between all included variables.
To test the hypothesised general theoretical model, path analysis was conducted in R using weighted least squares with a mean and variance adjusted test statistic (WLSMV) as the robust estimation method. The structural model (i.e., relationships between observed variables) was specified as outlined in Fig. 1. The following values were utilised to evaluate model fit: comparative fit index (CFI) or Tucker-Lewis index (TLI) of ⩾ 0.95 was considered good and ⩾ 0.90 acceptable, and an RMSEA value of ⩽ 0.050 considered good and ⩽ 0.080 acceptable [55–58]. Post-hoc modifications to the hypothesised model were conducted to improve model fit, guided by theoretical rationale, significance of paths, and overall model fit. Standardised regression coefficients, and the indirect effects of various paths from core beliefs to ED symptomatology (dietary restraint, binge eating, and compensatory behaviours) were calculated and reported. In order to examine our secondary aim, path analysis was conducted using the aforementioned process to test the exploratory multi-dimensional model, where all four dimensions of ED core beliefs were correlated within the model.
Results
Descriptive Statistics and Correlations
A series of Shapiro–Wilk tests revealed that each of the included variables were not normally distributed (ps < 0.01). All variables were significantly positively correlated with all other included variables (τ = 0.08** to 0.68**). See Table 1 for all descriptive statistics (mean and standard deviations) for each included variable, as well as correlations between variables.
Table 1.
Descriptive statistics and Kendall’s Tau correlations for all included variables
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Eating Disorder Core Beliefs | 2.93 (1.23) | ||||||||||||
| 2. Self-loathing | 2.26 (1.48) | 0.63** | |||||||||||
| 3. Unassertive | 3.30 (1.50) | 0.63** | 0.38** | ||||||||||
| 4. Demanding | 3.49 (1.50) | 0.66** | 0.43** | 0.44** | |||||||||
| 5. Abandoned | 2.67 (1.53) | 0.68** | 0.48** | 0.44** | 0.47** | ||||||||
| 6. Perfectionism | 3.24 (0.77) | 0.22** | 0.17** | 0.13** | 0.18** | 0.24** | |||||||
| 7. Preoccupation | 1.76 (1.37) | 0.35** | 0.34** | 0.24** | 0.28** | 0.31** | 0.26** | ||||||
| 8. Negative Affect | 40.91 (12.79) | 0.51** | 0.41** | 0.37** | 0.44** | 0.46** | 0.29** | 0.35** | |||||
| 9. Difficulty with Emotional Regulation | 2.63 (0.93) | 0.43** | 0.34** | 0.32** | 0.41** | 0.38** | 0.32** | 0.32** | 0.54** | ||||
| 10. Eating Beliefs | 2.20 (0.77) | 0.31** | 0.30** | 0.24** | 0.27** | 0.26** | 0.08** | 0.30** | 0.29** | 0.29** | |||
| 11. Restraint | 1.41 (1.49) | 0.18** | 0.20** | 0.11** | 0.14** | 0.16** | 0.20** | 0.53** | 0.18** | 0.16** | 0.15** | ||
| 12. Binge Eating | 3.41 (6.02) | 0.15** | 0.16** | 0.11** | 0.14** | 0.13** | 0.12** | 0.24** | 0.16** | 0.15** | 0.28** | 0.22** | |
| 13. Compensatory Behaviours | 3.46 (7.24) | 0.16** | 0.18** | 0.10** | 0.12** | 0.16** | 0.13** | 0.32** | 0.17** | 0.13** | 0.14** | 0.24** | 0.24** |
Preoccupation refers to preoccupation with eating, weight and shape. SD = Standard Deviation. **p < .01 (two-tailed)
General Model
Path Analysis
The proposed path model (Fig. 1) was fitted to the data in R using WLSMV estimation, in order to obtain overall model fit statistics, to test each of the proposed pathways and their relative strengths whilst accounting for each of the other variables in the model, and to calculate indirect paths from ED core beliefs to disordered eating behaviours (dietary restraint, OBE, and compensatory behaviours. The proposed path model demonstrated poor to acceptable fit to the observed data (see Table 2). Post-hoc modifications were utilised to remove non-significant paths and improve model fit guided by post-hoc theoretical modifications. The first modification included removing both non-significant paths from ‘Difficulty with Emotional Regulation’ to ‘Binge Eating’ and ‘Compensatory Behaviours’. This improved model fit slightly for the TLI and RMSEA (See Table 2).
Table 2.
Model fit indices for the general and multi-dimensional proposed and final models
| χ2 (df) | CFI | TLI | RMSEA [90% CI] | |
|---|---|---|---|---|
| General Model | ||||
| Hypothesised Model | 553.82 (25) | 0.925 | 0.892 | 0.110 [0.102, 0.118] |
| Modification 1 | 435.18 (27) | 0.925 | 0.900 | 0.105 [0.097, 0.114] |
| Modification 2 | 268.49 (26) | 0.959 | 0.943 | 0.082 [0.073, 0.091] |
| Modification 3: Final Model | 207.49 (24) | 0.969 | 0.954 | 0.075 [0.065, 0.084] |
| Multi-dimensional Model | ||||
| Final Model | 238.66 (39) | 0.980 | 0.970 | 0.061 [0.054, 00.69] |
Comparative fit indices: CFI = Comparative fit index; TLI = Tucker-Lewis index; RMSEA = root mean square error of approximation; CI = confidence interval; χ2(df) = chi-square (degrees of freedom)
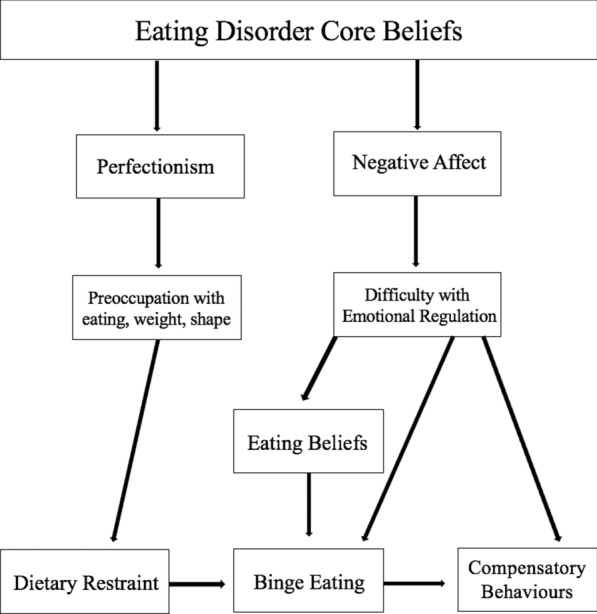
Further modifications were guided by theoretical rationale and were included if added paths were significant and/or increased model fit. The second modification included adding a path from ‘Eating disorder core beliefs’ to ‘Preoccupation with eating, weight, shape’, which resulted in improvements in model fit across all indices (Table 2). The third and final modifications involved adding two paths from both ‘Perfectionism’ and ‘Preoccupation with eating, weight, shape’ to ‘Negative affect’. No other modifications improved model fit or added significant paths to ED behaviours. Overall, fit statistics were improved compared to the proposed model, and the final model provided a more nuanced understanding of the pathways from ED core beliefs to disordered eating behaviours, based on post-hoc theoretical considerations and subsequent retention of statistically significant paths. See Fig. 2 for the final, general model, including standardised regression coefficients for significant paths. The newly developed model was referred to as the core beliefs model of disordered eating.
Fig. 2.
Final Core Beliefs Model of Disordered Eating. Regression coefficients were standardised. ** p < .01, *** p < .001
Indirect effects were calculated within the total, general model, for all possible indirect pathways from ED core beliefs to each of the three ED behaviours: dietary restraint, OBE, and compensatory behaviours. Both possible indirect paths from ED core beliefs to restraint were significant (p < 0.001). All six possible indirect paths from ED core beliefs to OBE were significant (p < 0.05), with paths containing between two and five serial mediating variables. All six possible indirect paths from ED core beliefs to compensatory behaviours were significant (p < 0.05), with paths containing between two and six serial mediating variables. See Table 3 for details of each of the serial mediating variables included in each path, and unstandardised and standardised indirect effects.
Table 3.
Indirect effects for pathways to ED symptomatology in general and multi-dimensional models
| Pathways: general model | Unstandardised indirect effect | Standardised indirect effect | p-value |
|---|---|---|---|
| Dietary Restraint | |||
| 1: EDCB → PRE → DR | 0.307 | 0.256 | < 0.001 |
| 2: EDCB → PERF → PRE → DR | 0.070 | 0.058 | < 0.001 |
| Objective Binge Eating | |||
| 3: EDCB → PRE → DR → OBE | 0.329 | 0.156 | < 0.001 |
| 4: EDCB → NEG → DER → EB → OBE | 0.158 | 0.075 | < 0.001 |
| 5: EDCB → PERF → PRE → DR → OBE | 0.075 | 0.035 | < 0.001 |
| 6: EDCB → PRE → NEG → DER → EB → OBE | 0.013 | 0.006 | 0.007 |
| 7: EDCB → PERF → NEG → DER → EB → OBE | 0.019 | 0.009 | 0.001 |
| 8: EDCB → PERF → PRE → NEG → DER → EB → OBE | 0.003 | 0.008 | |
| Compensatory Behaviours | 0.001 | ||
| 9: EDCB → PRE → DR → OBE → CB | 0.513 | 0.087 | < 0.001 |
| 10: EDCB → NEG → DER → EB → OBE → CB | 0.247 | 0.042 | < 0.001 |
| 11: EDCB → PERF → PRE → DR → OBE → CB | 0.117 | 0.020 | < 0.001 |
| 12: EDCB → PRE → NEG → DER → EB → OBE → CB | 0.021 | 0.004 | 0.007 |
| 13: EDCB → PERF → NEG → DER → EB → OBE → CB | 0.029 | 0.005 | 0.001 |
| 14: EDCB → PERF → PRE → NEG → DER → EB → OBE → CB | 0.005 | 0.001 | 0.010 |
| Pathways: Multi-dimensional Model | Unstandardised Indirect Effect | Standardised Indirect Effect | p-value |
|---|---|---|---|
| Dietary Restraint | |||
| 1: SL → PRE → DR | 0.237 | 0.239 | < 0.001 |
| 2: A/D → PRE → DR | 0.066 | 0.068 | 0.030 |
| 3: A/D → PERF → PRE → DR | 0.046 | 0.048 | < 0.001 |
| 4: D/NS → PERF → PRE → DR | 0.022 | 0.022 | 0.009 |
| Objective Binge Eating | |||
| 5: SL → PRE → DR → OBE | 0.251 | 0.147 | < 0.001 |
| 6: SL → NEG → DER → EB → OBE | 0.035 | 0.021 | 0.009 |
| 7: SL → PRE → NEG → DER → EB → OBE | 0.012 | 0.007 | 0.009 |
| 8: U/I → NEG → DER → EB → OBE | 0.025 | 0.015 | 0.011 |
| 9: A/D → PRE → DR → OBE | 0.070 | 0.042 | 0.042 |
| 10: A/D → PERF → PRE → DR → OBE | 0.049 | 0.029 | < 0.001 |
| 11: A/D → NEG → DER → EB → OBE | 0.031 | 0.019 | 0.006 |
| 12: A/D → PRE → NEG → DER → EB → OBE | 0.003 | 0.002 | 0.104 |
| 13: A/D → PERF → NEG → DER → EB → OBE | 0.012 | 0.007 | 0.004 |
| 14: A/D → PERF → PRE → NEG → DER → EB → OBE | 0.002 | 0.001 | 0.014 |
| 15: D/NS → PERF → PRE → DR → OBE | 0.023 | 0.014 | 0.015 |
| 16: D/NS → NEG → DER → EB → OBE | 0.066 | 0.039 | 0.001 |
| 17: D/NS → PERF → NEG → DER → EB → OBE | 0.006 | 0.003 | 0.030 |
| 18: D/NS → PERF → PRE → NEG → DER → EB → OBE | 0.001 | 0.001 | 0.053 |
| Compensatory Behaviours | |||
| 19: SL → PRE → DR → OBE → CB | 0.408 | 0.083 | < 0.001 |
| 20: SL → NEG → DER → EB → OBE → CB | 0.058 | 0.012 | 0.006 |
| 21: SL → PRE → NEG → DER → EB → OBE → CB | 0.019 | 0.004 | 0.009 |
| 22: U/I → NEG → DER → EB → OBE → CB | 0.041 | 0.009 | 0.009 |
| 23: A/D → PRE → DR → OBE → CB | 0.114 | 0.024 | 0.041 |
| 24: A/D → PERF → PRE → DR → OBE → CB | 0.079 | 0.017 | < 0.001 |
| 25: A/D → NEG → DER → EB → OBE → CB | 0.051 | 0.011 | 0.006 |
| 26: A/D → PRE → NEG → DER → EB → OBE → CB | 0.005 | 0.001 | 0.099 |
| 27: A/D → PERF → NEG → DER → EB → OBE → CB | 0.020 | 0.004 | 0.003 |
| 28: A/D → PERF → PRE → NEG → DER → EB → OBE → CB | 0.004 | 0.001 | 0.016 |
| 29: D/NS → PERF → PRE → DR → OBE → CB | 0.038 | 0.008 | 0.017 |
| 30: D/NS → NEG → DER → EB → OBE → CB | 0.107 | 0.022 | < 0.001 |
| 31: D/NS → PERF → NEG → DER → EB → OBE → CB | 0.009 | 0.002 | 0.027 |
| 32: D/NS → PERF → PRE → NEG → DER → EB → OBE → CB | 0.002 | < 0.001 | 0.054 |
A/D = Abandoned/Deprived; CB = Compensatory Behaviours; D/NS = Demanding/Needing support; DER = Difficulty with Emotional Regulation; DR = Dietary Restraint; EB = Eating Beliefs; EDCB = Eating Disorder Core Beliefs; NEG = Negative Affect; OBE = Objective Binge Eating; PERF = Perfectionism; PRE = Preoccupation with eating, weight, shape; SL = Self-Loathing; U/I = Unassertive/Inhibited
Multi-dimensional Model
Path Analysis
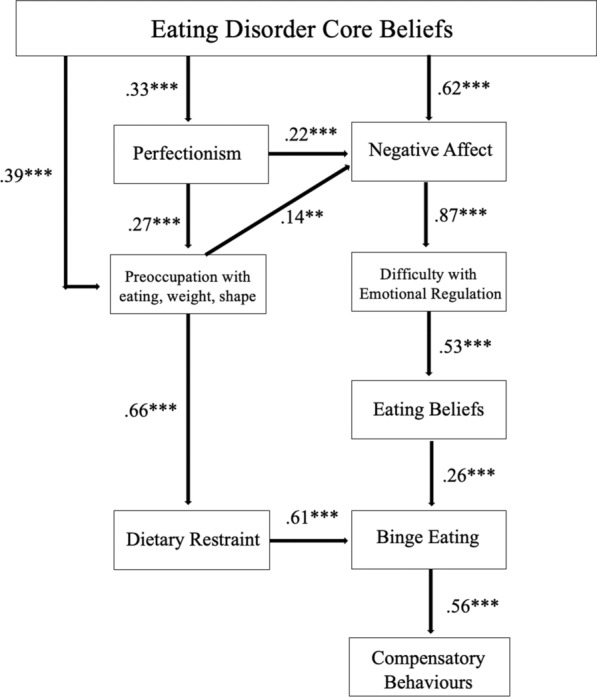
To investigate the secondary aim of the current study, an exploratory test of the newly developed ‘core beliefs model of disordered eating’ was conducted with a multi-dimensional model of core beliefs. This involved a simultaneous test of four dimensions of ED core beliefs; ‘Self-loathing’, ‘Abandoned/Deprived’, Demanding/Needing support’, and ‘Unassertive/Inhibited’. The model was tested in R using WLSMV estimation, where all four ED core belief dimensions were correlated, in order to test the relative strength of paths from each ED core belief dimension to other variables in the model and ultimately to ED symptomatology, whilst controlling for the presence of each of the other core belief dimensions included the model. This was important in order to examine any potential differences in pathways to various disordered eating behaviours, or whether these processes were similar between core belief dimensions.
The multi-dimensional model demonstrated superior fit to the observed data compared to the general model, with good fit to the observed data for all indices, except for RMSEA which indicated acceptable fit (see Table 2). However, the multi-dimensional model (Fig. 3) demonstrated some differences to the general model (Fig. 2). Firstly, the path from ‘Self-loathing’ was significant to ‘Preoccupation with eating, weight, shape’ and ‘Negative affect’, but not to ‘Perfectionism’. Moreover, the paths from ‘Demanding/Needing support’ were only significant to both ‘Perfectionism’ and ‘Negative affect’, but no longer directly to ‘Preoccupation with eating, weight, shape’. The paths from Unassertive/Inhibited’ were no longer significant to ‘Perfectionism’, ‘Preoccupation with eating, weight, shape’, only to ‘Negative affect’. Only the paths from ‘Abandoned/Deprived’ were significant to all variables as in the general model, that is, ‘Perfectionism’, ‘Preoccupation with eating, weight, shape’, and ‘Negative affect’. See Fig. 3 for the tested multi-dimensional model, including standardised regression coefficients for significant paths.
Fig. 3.
Multi-dimensional model outlining specific processes and pathways from core belief dimensions to eating disorder symptomatology. Straight arrows represent significant paths, labelled with standardised regression coefficients. Curved arrows represent correlations. * p < .05, ** p < .01, *** p < .001
Indirect effects were calculated within the total, multi-dimensional model, for all possible indirect pathways from ED core beliefs to each of the three ED behaviours: dietary restraint, OBE, and compensatory behaviours. Each possible indirect path from ‘Self-Loathing’, ‘Abandoned/Deprived’ and ‘Demanding/Needing support’ to restraint were significant (p < 0.05). Of 14 possible indirect paths from ED core beliefs to OBE, 12 were significant (p < 0.05); one path from ‘Unassertive/Inhibited’ to OBE, three paths from ‘Self-loathing’ to OBE, five paths from ‘Abandoned/Deprived’ to OBE, and three paths from ‘Demanding/Needing support’ to OBE. Of 14 possible indirect paths from ED core beliefs to compensatory behaviours, 12 were significant (p < 0.05); one path from ‘Unassertive/Inhibited’ to compensatory behaviours, three paths from ‘Self-loathing’ to compensatory behaviours, five paths from ‘Abandoned/Deprived’ to compensatory behaviours, and three paths from ‘Demanding/Needing support’ to compensatory behaviours. See Table 3 for details of each of the serial mediating variables included in each path, and unstandardised and standardised indirect effects.
Post-hoc path analyses were conducted to examine whether the general model (Fig. 2) and its paths were significant if each ED core belief dimension was tested in isolation. Although this was not a specific theoretical or statistical aim of the present study, it was considered important to test each ED core belief dimension separately to assess their ongoing theoretical relevance. This was considered important given the interesting variation in paths from ED core beliefs to ED behaviours, whilst controlling for the presence of each of the other core belief dimensions. Results suggested that when tested in isolation, all four general ED core belief models (one for each dimension) displayed acceptable to good model fit (see Supplementary Table 1). Supplementary Table 2 reports all standardised path coefficients.
Discussion
The present study aimed to develop and test a general theoretical model outlining the important developmental and maintenance processes and pathways from ED core beliefs to core ED symptomatology and behaviours, as well as exploring the potential differential impact of, or pathways from various core belief dimensions to dietary restraint, OBE, and compensatory behaviours. A final, general core beliefs model of disordered eating was presented (Fig. 2). The hypothesised model displayed poor to acceptable fit to the data. As such, several post-hoc modifications were made which increased model fit and added theoretical richness to the final model. This included removing two non-significant paths and adding three statistically and theoretically significant paths.
The final model indicates that core beliefs can lead to the development of disordered eating symptomatology in several ways. Firstly, negative core beliefs can increase perfectionistic attitudes, tendencies and behaviours, which in turn contributes to over-evaluating the importance of eating, weight and shape whilst evaluating the self. This scheme for self-evaluation shares similarities with previous theory and empirical research [15], Wade et al., [59]), whereby body weight and shape can become a means of ‘self-definition’ or ‘compensation’ for perfectionistic beliefs or tendencies in response to the activation of maladaptive core beliefs. The model also indicates that ED core beliefs can increase preoccupation, including in the absence of perfectionism to mediate this relationship. This relationship has been seen in previous empirical tests of Fairburn’s et al. [15] maintenance model [19, 20]. This preoccupation with eating, weight and shape contributes to increased dietary restraint, which in turn predicts OBE and subsequent compensatory behaviours.
Additional paths were added to improve the theoretical depth of early paths, guided by post-hoc theoretical and statistical rationale. Although it has not been specifically proposed in previous theoretical ED models, the relationship between perfectionism and negative affect (e.g., depressive symptomatology) has been well-established [60]. As such, the path from ‘Perfectionism’ to ‘Negative affect’ adds theoretical richness to early paths that have not been specifically proposed in seminal ED models. Similarly, a path was added from ‘Preoccupation with eating, weight and shape’ to ‘Negative affect’, to support the established relationship between increased negative thoughts, concerns or preoccupations, and the negative affective states that are often subsequently experienced (e.g., depression, anxiety, stress [16]).
However, even in the absence of perfectionism or preoccupation with eating, weight and shape, negative core beliefs were shown to relate to increased disordered eating symptomatology. This outcome is in alignment with previous theory which outlines similar processes [12, 16]. This model demonstrated that ED core beliefs can trigger or relate to increased negative affect, which then facilitates increased difficulties with emotional regulation. Difficulties in regulating negative affective states can then trigger unhelpful meta-cognitive beliefs about eating. In turn, greater meta-cognitive beliefs (i.e., positive, negative and permissive about binge eating) lead to increased binge eating, which in turn can trigger increased compensatory behaviours. The pathway described has similarities to those proposed in the cognitive model of BN [16] and the integrated cognitive behavioural model of binge eating [17]. However, unlike these models, it includes other important cognitive and behavioural elements, that is, perfectionism, and preoccupation with eating, weight, shape, and dietary restraint. Moreover, the two (major) sequences of processes from ED core beliefs to dietary restraint, binge eating, and compensatory behaviours, somewhat resemble that of the schema avoidance and schema compensation processes proposed by Waller [12]. However, there is greater nuance in this model in pathways from ED core beliefs to other important elements (e.g., various types of cognitions) that are not explicitly outlined or described in the schema-focussed theory.
Altogether, the model contains similarities to established and recent theoretical models with a construct akin to a ‘core belief’. The final model also attempts to integrate all key processes, create cohesion, and theoretical richness, and to provide a conceptualisation of how ED core beliefs relate to the development and maintenance of disordered eating symptomatology via several pathways. Several of these paths have never been theoretically proposed in current ED models, nor theoretically tested. For example, the path from ‘Eating disorder core beliefs’ to ‘Binge eating’, through five serial mediators (‘Perfectionism’, ‘Preoccupation with eating, weight, shape’, ‘Negative affect’, ‘Difficulty with emotional regulation’, and ‘Eating beliefs’). Importantly, all indirect effects calculated for all possible pathways from ED core beliefs to all three key ED symptomatology were significant. This indicates that ED core beliefs can be related to increases in ED behaviours through several paths. For example, ED core beliefs can result in increased dietary restraint, binge eating and compensatory behaviours through pre-occupation with eating, weight and shape, both with and without increased perfectionism as a mediator of this process. Additionally, ED core beliefs can result in increases in binge eating and compensatory behaviours both with and without mediating increases in negative affect, difficulties in emotional regulation and eating beliefs. Overall, it is evident that there are many pathways that may relate to the development of ED symptoms.
The multi-dimensional version of the model tested hypothesised pathways and highlights the ways in which different core beliefs dimensions may potentially differ in their strength of relationship to other constructs and proposed processes in the model. For example, ‘self-loathing’ core beliefs predicted increased ‘preoccupation with eating, weight and shape’ and ‘negative affect’, but whilst controlling for the other core belief dimensions did not directly predict ‘Perfectionism’. Further, all indirect effects for all possible paths tested from ‘Self-loathing’ to dietary restraint, OBE, and compensatory behaviours were significant. Further, ‘Abandoned/Deprived’ beliefs predicted greater ‘Perfectionism’, ‘Preoccupation with eating, weight, shape’, and ‘Negative affect’. This may suggest that this dimension of maladaptive core beliefs is a particularly strong contributor to the development of core eating disordered pathology as compared to the other core belief dimensions.
When examining the significant indirect effects of specific paths, ‘Abandoned/Deprived’ predicted greater ED behaviours through all major pathways: 1) through increased perfectionism, which in turn increased pre-occupation with food, weight and shape, 2) through increased perfectionism which in turn increases negative affect, difficulties in emotional regulation and eating beliefs, 3) through negative affect directly, or 4) through pre-occupation with food, weight and shape directly. Only two indirect effects were not significant.
‘Demanding/Needing support’ core beliefs directly predicted both greater ‘Perfectionism’ and ‘Negative affect’ in the multi-dimensional model and displayed almost all significant indirect path to all three ED behaviours. Similar to ‘Abandoned/Deprived’ beliefs, only two indirect effects were not significant. Interestingly, whilst controlling for the effects of the other three core belief dimensions, ‘Unassertive/Inhibited’ core beliefs only displayed a significant pathway to ‘Negative affect’. It is possible that this dimension is particularly important to the internalising symptomatology that often co-occurs with ED symptomatology. However, the specific nuances and differences found between these processes and pathways were indeed based on exploratory analyses and are, as such, preliminary findings that should be examined again in additional samples before strong conclusions can be drawn. Although post-hoc supplementary analyses reinforced the ongoing importance of these beliefs in the development of disordered eating (i.e., when tested in isolation), in order to assess and potentially reinforce their unique contributions and relationships with other variables, these outcomes should be examined again in relevant samples.
Strengths, Limitations and Future Research
The present study had several empirical strengths and made some important theoretical contributions. We presented a general core beliefs model of disordered eating, which highlights the critical pathways from ED core beliefs to important behavioural ED symptomatology, dietary restriction, OBE, and compensatory behaviours. This is the first model to bring focus to the importance of core beliefs in development of EDs, as well as highlight the differential processes and pathways that may lead to various core ED symptoms. This general model allows future study to test and explore not only the model in its entirety, but additionally to test specific paths and processes, depending on the relevance for specific disorders or symptom profiles (e.g., AN restrictive subtype without a binge-purge [BP] cycle, or BED without compensatory behaviours). The presentation of various indirect effect pathways allows for partial tests of the model to be conducted in samples where it is either not possible or not relevant to test the model in its entirely. Furthermore, this is the first study to present preliminary differences in early processes from different core belief dimensions to ED behaviours.
However, these contributions must also be placed in the context of the limitations of this study. Primarily, this research was conducted using cross-sectional data. Therefore, although the model was developed from well-established literature regarding empirical and theoretical relationships between key included variables, the causality of processes cannot be strictly inferred from the current data. Currently, outcomes only represent a preliminary test of the model. Future longitudinal research should investigate the proposed processes and their development over time. Future research could also consider ecological momentary assessment to test state-level processes proposed, as well as maintenance processes that were not tested in the current model. The current model was a recursive model and highlighted only the developmental pathways and processed from ED core beliefs to ED symptomatology. Future ecological momentary assessment or experimental research could further test and develop the model (e.g., a non-recursive model) by examining both developmental and maintenance processes.
Further, although the measures utilised to operationalize each of the key variables included in the model were all psychometrically validated measures, it would be beneficial for a future test of the model to utilise different assessment tools to explore the stability of the model whilst using alternate measures, given these tools possess adequate psychometric properties. Moreover, the post-hoc modifications to the hypothesised model were not tested with new data in the present study. It is therefore considered important that both final models, be explicitly tested in an independent sample in future study. Finally, this study used a sample of undergraduate university students. Although our sample contained levels of disordered eating symptomatology and clinical ED diagnoses comparable to global and Australian prevalence rates [38], it remains critical that the model is tested, either in whole or in part, in relevant treatment seeking or clinical populations with sufficient sample sizes, or with a sample of individuals self-reporting a current ED diagnosis. It would also be interesting to validate and compare this model in those with prodromal or sub-clinical EDs, and between those with different diagnostic status (e.g., AN-BP subtype compared to BED).
Future research should consider validation of both the general and multi-dimensional model in both a general and in specific ED populations, as well as to focus on examining the specific nuances in processes. Further, it is also possible that these four dimensions of core beliefs may relate to specific behaviours differently in specific ED populations. For example, AN-BP or BN samples may demonstrate a greater number of significant indirect pathways to compensatory behaviours, where this non-clinical sample did not. Thus, future investigation into these specific pathways is certainly warranted.
Conclusions
This study extends the current understanding of the role of core belief in the development of disordered eating, by building upon previous theoretical models and empirical literature. We present a general, core beliefs model of disordered eating, and preliminary findings regarding differences in processes and pathways from four key core belief dimensions to ED behaviours. It is hoped that processes and pathways presented in this model are tested in relevant populations and that this study has provided a comprehensive way to understanding the critical role of core beliefs in development of disordered eating symptomatology. Bearing in mind that core beliefs are considered a developmental factor arising from early experience, identification of such beliefs and utilisation of these as targets will be valuable in both the prevention and early intervention space, as well as in clinical treatment and research.
Supplementary Information
Author contributions
AH and MA were involved in the conception of the study. AH conducted the literature review, conceptualised the hypothesised versions of the theoretical model, collected and analysed the data, and prepared the first draft of the manuscript. Subsequent versions of the theoretical model and manuscript were refined in collaboration with AB and MA. All authors read and approved the final theoretical models and manuscript.
Funding
The authors declare that they did not receive funding for this study.
Availability of data and materials
The data using during the current study is available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved as part of a larger Higher Degree Research project (‘Negative core beliefs in eating disorders’: Approval number 2022/856) by the University of Sydney Human Research Ethics Committee. All participants were provided with a participant information statement and provided their consent to participate in the study. All participants read a Participant Information Statement allowing them to make an informed choice as to whether they wanted to participate in the research or not. They were informed that they could also cease participation at any stage with no penalty to them. The ethics of the consent procedure was approved as above. Participants consented to their data being used for research purposes and consented to unidentifiable aggregate data to be published.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cooper MJ. Cognitive theory in anorexia nervosa and bulimia nervosa: progress, development and future directions. Clin Psychol Rev. 2005;25(4):511–31. 10.1016/j.cpr.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Jones CJ, Leung N, Harris G. Dysfunctional core beliefs in eating disorders: a review. J Cognit Psychoth Int Quart. 2007;21(2):156–71. 10.1891/088983907780851531. [Google Scholar]
- 3.Maher A, Cason L, Huckstepp T, Stallman H, Kannis-Dymand L, Millear P, Mason J, Wood A, Allen A. Early maladaptive schemas in eating disorders: a systematic review. Eur Eat Disord Rev. 2022;30(1):3–22. 10.1002/erv.2866. [DOI] [PubMed] [Google Scholar]
- 4.Beck AT, Freeman E. Cognitive therapy of personality disorders. London: The Guilford Press; 1990. p. 470. [Google Scholar]
- 5.Young JE, Klosko JS, Weishaar ME. Schema therapy: a practitioners guide. New York, NY, USA: The Guilford Press; 2003. [Google Scholar]
- 6.Beck AT. Cognitive therapy and the emotional disorders. Cham: International Universities Press; 1976. [Google Scholar]
- 7.Fairchild H, Cooper M. A multidimensional measure of core beliefs relevant to eating disorders: Preliminary development and validation. Eat Behav. 2010;11(4):239–46. 10.1016/j.eatbeh.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Hatoum AH, Burton AL, Abbott MJ. Assessing negative core beliefs in eating disorders: revision of the eating disorder core beliefs questionnaire. J Eating Dis. 2022;10(18):542. 10.1186/s40337-022-00542-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pennesi JL, Wade TD. A systematic review of the existing models of disordered eating: Do they inform the development of effective interventions? Clin Psychol Rev. 2016;43:175–92. 10.1016/j.cpr.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Pugh M. A narrative review of schemas and schema therapy outcomes in the eating disorders. Clin Psychol Rev. 2015;39:30–41. 10.1016/j.cpr.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 11.Levinson CA, Cusack C, Brown ML, Smith AR. A network approach can improve eating disorder conceptualization and treatment. Nature Rev Psychol. 2022;1(7):419–30. 10.1038/s44159-022-00062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waller G, Kennerley H, Ohanian V. Schema-focused cognitive-behavioral therapy for eating disorders. In: Riso LP, du Toit PL, Stein DJ, Young JE, editors. Cognitive schemas and core beliefs in psychological problems: a scientist-practitioner guide. NJ: American Psychological Association; 2007. p. 139–75. [Google Scholar]
- 13.Young JE, Brown G. Young schema questionnaire. In: Young JE, editor. Cognitive therapy for personality disorders: A schema-focused approach. 2nd ed. Sarasota: Professional Resource Press/Professional Resource Exchange; 1994. p. 63–76. [Google Scholar]
- 14.Fennell MJV. Low self Esteem: a cognitive perspective. Behav Cogn Psychother. 1997;25(1):1–25. 10.1017/S1352465800015368. [Google Scholar]
- 15.Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav Res Ther. 2003;41(5):509–28. 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- 16.Cooper MJ, Wells A, Todd G. A cognitive model of bulimia nervosa. Br J Clin Psychol. 2004;43(1):1–16. 10.1348/014466504772812931. [DOI] [PubMed] [Google Scholar]
- 17.Burton AL, Abbott MJ. Processes and pathways to binge eating: Development of an integrated cognitive and behavioural model of binge eating. J Eat Disord. 2019;7:18. 10.1186/s40337-019-0248-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fairburn CG, Cooper Z, O’Connor M. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008. [Google Scholar]
- 19.Allen KL, Byrne SM, McLean NJ. The dual-pathway and cognitive-behavioural models of binge eating: prospective evaluation and comparison. Eur Child Adolesc Psych. 2012;21(1):51–62. 10.1007/s00787-011-0231-z. [DOI] [PubMed] [Google Scholar]
- 20.Dakanalis A, Timko CA, Clerici M, Zanetti MA, Riva G. Comprehensive examination of the trans-diagnostic cognitive behavioral model of eating disorders in males. Eat Behav. 2014;15(1):63–7. 10.1016/j.eatbeh.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Hoiles KJ, Egan SJ, Kane RT. The validity of the transdiagnostic cognitive behavioural model of eating disorders in predicting dietary restraint. Eating Behav. 2012;13(2):123–6. 10.1016/j.eatbeh.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Lampard AM, Tasca GA, Balfour L, Bissada H. An evaluation of the transdiagnostic cognitive-behavioural model of eating disorders. Eur Eat Disord Rev. 2013;21(2):99–107. 10.1002/erv.2214. [DOI] [PubMed] [Google Scholar]
- 23.Murray SB, Rieger E, Karlov L, Touyz SW. An investigation of the transdiagnostic model of eating disorders in the context of muscle dysmorphia. Eur Eat Disord Rev. 2013;21(2):160–4. 10.1002/erv.2194. [DOI] [PubMed] [Google Scholar]
- 24.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 25.Garner, D. M. (2004). Eating Disorder Inventory – 3. Professional manual. Lutz: FL.
- 26.Bergin JL, Wade TD. A cross-sectional analysis of the cognitive model of bulimia nervosa. Int J Eat Disord. 2012;45(6):776–86. 10.1002/eat.22012. [DOI] [PubMed] [Google Scholar]
- 27.Young E, Cooper M. Applying a cognitive model to binge eating in a female community sample. Eat Behav. 2013;14(3):295–8. 10.1016/j.eatbeh.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Cooper, M., Todd, G., & Wells, A. (2008). Treating bulimia nervosa and binge eating: An integrated metacognitive and cognitive therapy manual. Routledge
- 29.Young JE, Brown G. Young schema questionnaire-short form; version 3 (YSQ-S3. YSQ): APA PsycTests; 2005. 10.1037/t67023-000. [Google Scholar]
- 30.Cooper M, Cohen-Tovée E, Todd G, Wells A, Tovée M. The eating disorder belief questionnaire: preliminary development. Behav Res Ther. 1997;35(4):381–8. 10.1016/s0005-7967(96)00115-5. [DOI] [PubMed] [Google Scholar]
- 31.Hatoum AH, Burton AL, Abbott MJ. Validation of the revised eating disorder core beliefs questionnaire (ED-CBQ-R) in an Australian sample. Clin Psychol. 2022. 10.1080/13284207.2022.2144717. [Google Scholar]
- 32.Carpenter S. Ten steps in scale development and reporting: a guide for researchers. Commun Methods Meas. 2018;12(1):25–44. 10.1080/19312458.2017.1396583. [Google Scholar]
- 33.Hair JF, Tomas G, Hult M, Ringle CM, Sarstedt M, Danks NP, Ray S. An introduction to structural equation modeling. In: Hair JF, Tomas G, Hult M, Ringle CM, Sarstedt M, Danks NP, Ray S, editors. Partial least squares structural equation modeling (PLS-SEM) using r: a workbook. Cham: Springer International Publishing; 2021. p. 1–29. 10.1007/978-3-030-80519-7_1. [Google Scholar]
- 34.Hoyle RH, Gottfredson NC. Sample size considerations in prevention research applications of multilevel modeling and structural equation modeling. Prev Sci. 2015;16(7):987–96. 10.1007/s11121-014-0489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. 2005;5(2):159–68. 10.1207/s15327574ijt0502_4. [Google Scholar]
- 36.Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 37.Thakkar JJ. Procedural steps in structural equation modelling. In: Thakkar JJ, editor. Structural equation modelling: Application for research and practice (with AMOS and R). Springer Singapore; 2020. p. 29–34. [Google Scholar]
- 38.Hay P, Aouad P, Le A, Marks P, Maloney D, Touyz S, Maguire S. Epidemiology of eating disorders: Population, prevalence, disease burden and quality of life informing public policy in Australia-a rapid review. J Eat Disord. 2023;11(1):23. 10.1186/s40337-023-00738-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melisse B, van Furth EF, de Beurs E. Eating disorder examination questionnaire (EDE-Q): validity and norms for Saudi nationals. Eating Weight Dis EWD. 2022;27(1):139–50. 10.1007/s40519-021-01150-3. [DOI] [PubMed] [Google Scholar]
- 40.Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ. Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. 2004;42(5):551–67. 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- 41.Mond JM, Myers TC, Crosby RD, Hay PJ, Rodgers B, Morgan JF, Lacey JH, Mitchell JE. Screening for eating disorders in primary care: EDE-Q versus SCOFF. Behav Res Ther. 2008;46(5):612–22. 10.1016/j.brat.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 42.Rica R, Solar M, Compte EJ, Sepúlveda AR. Establishing the optimal male cut-off point: confirmatory factor analysis of the eating disorder examination-questionnaire (EDE-Q) in a representative sample of Spanish university students. Eat Weight Disord. 2021. 10.1007/s40519-021-01234-0. [DOI] [PubMed] [Google Scholar]
- 43.Schaefer LM, Smith KE, Leonard R, Wetterneck C, Smith B, Farrell N, Riemann BC, Frederick DA, Schaumberg K, Klump KL, Anderson DA, Thompson JK. Identifying a male clinical cutoff on the eating disorder examination-questionnaire (EDE-Q). Int J Eat Disord. 2018;51(12):1357–60. 10.1002/eat.22972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meule A. Reconsidering the use of cut-off scores for the eating disorder examination-questionnaire. Eat Disord. 2021;29(5):480–4. 10.1080/10640266.2019.1678981. [DOI] [PubMed] [Google Scholar]
- 45.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995. [Google Scholar]
- 46.Zanon C, Brenner RE, Baptista MN, Vogel DL, Rubin M, Al-Darmaki FR, Gonçalves M, Heath PJ, Liao HY, Mackenzie CS, Topkaya N, Wade NG, Zlati A. Examining the dimensionality, reliability, and invariance of the depression, anxiety, and stress scale-21 (DASS-21) across eight countries. Assessment. 2021;28(6):1531–44. 10.1177/1073191119887449. [DOI] [PubMed] [Google Scholar]
- 47.Bjureberg J, Ljótsson B, Tull MT, Hedman E, Sahlin H, Lundh LG, Bjärehed J, DiLillo D, Messman-Moore T, Gumpert CH, Gratz KL. Development and validation of a brief version of the difficulties in emotion regulation scale: the DERS-16. J Psychopathol Behav Assess. 2016;38(2):284–96. 10.1007/s10862-015-9514-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burton AL, Brown R, Abbott MJ. Overcoming difficulties in measuring emotional regulation: assessing and comparing the psychometric properties of the DERS long and short forms. Cogent Psychol. 2022;9(1):629. 10.1080/23311908.2022.2060629. [Google Scholar]
- 49.Burton AL, Abbott MJ. The revised short-form of the Eating Beliefs Questionnaire: Measuring positive, negative, and permissive beliefs about binge eating. J Eat Disord. 2018;6:37. 10.1186/s40337-018-0224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Burton AL, Mitchison D, Hay P, Donnelly B, Thornton C, Russell J, Swinbourne J, Basten C, Goldstein M, Touyz S, Abbott MJ. Beliefs about binge eating: psychometric properties of the eating beliefs questionnaire (EBQ-18) in eating disorder, obese, and community samples. Nutrients. 2018;10(9):1306. 10.3390/nu10091306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire?. Int J Eat Disord. 1994;16:363–70. [PubMed] [Google Scholar]
- 52.Burgess AM, Frost RO, DiBartolo PM. Development and validation of the frost multidimensional perfectionism scale-brief. J Psychoeduc Assess. 2016;34(7):620–33. 10.1177/0734282916651359. [Google Scholar]
- 53.R Core Team (2023). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Australia. https://www.R-project.org/.
- 54.Dunn TJ, Baguley T, Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. 2014;105(3):399–412. 10.1111/bjop.12046. [DOI] [PubMed] [Google Scholar]
- 55.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. 10.1080/10705519909540118. [Google Scholar]
- 56.Jackson DL, Gillaspy JA Jr, Purc-Stephenson R. Reporting practices in confirmatory factor analysis: an overview and some recommendations. Psychol Methods. 2009;14(1):6–23. 10.1037/a0014694. [DOI] [PubMed] [Google Scholar]
- 57.Marsh HW, Hau KT, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing hu and bentler’s (1999) findings. Struct Equ Model. 2004;11(3):320–41. 10.1207/s15328007sem1103_2. [Google Scholar]
- 58.Schreiber JB, Stage FK, King J, Nora A, Barlow EA. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res. 2006;99(6):323–37. 10.3200/JOER.99.6.323-338. [Google Scholar]
- 59.Wade TD, O’Shea A, Shafran R. Perfectionism and Eating Disorders. In: Sirois FM, Molnar DS, editors. Perfectionism, Health, and Well-Being. NY: Springer International Publishing; 2016. p. 205–22. [Google Scholar]
- 60.Hummel J, Cludius B, Woud ML, Holdenrieder J, Mende N, Huber V, Limburg K, Takano K. The causal relationship between perfectionism and negative affect: two experimental studies. Personal Indiv Diff. 2023;200:111895. 10.1016/j.paid.2022.111895. [Google Scholar]
- 61.Rø Ø, Reas DL, Stedal K. Eating disorder examination questionnaire (EDE-Q) in Norwegian adults: discrimination between female controls and eating disorder patients. Europ Eating Dis Rev J Eating Dis Assoc. 2015;23(5):408–12. 10.1002/erv.2372. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data using during the current study is available from the corresponding author on reasonable request.