Abstract
Background
The study aims to investigate the application of surgical vaginoscopy via a no-touch hysteroscopic approach for the management of female genital polyps. The primary objective is to assess the feasibility of this technique in treating intrauterine pathologies in both pregnant and non-pregnant women.
Methods
A total of forty-six patients diagnosed with genital polyps underwent operative vaginoscopy at a university-affiliated hospital between April 1, 2017 and May 31, 2023. A retrospective analysis was conducted on the collected data, encompassing patient complaints, clinical presentations, surgical outcomes, and pathological diagnoses. Additionally, the success rate of the vaginoscopic procedures was determined.
Results
Forty-six patients with an average age of 33.0 ± 8.8 years were included in this study. Among them, 25 were non-pregnant (3 with and 22 without a sexual history). The most common clinical manifestation was irregular vaginal bleeding (11/25, 44%) followed by conscious vaginal protrusion (10/25, 40%). Among the 21 pregnant patients, the main symptom was irregular vaginal bleeding during pregnancy (100%). The postoperative pathological diagnoses included 11 endometrial polyps, 33 cervical polyps, 1 multiple vaginal polyps, and 1 vaginal stump polyps. The coincidence rate between the intraoperative vaginoscopic diagnosis and postoperative pathological diagnosis was 100%. Among the non-pregnant patients, 11 were diagnosed with endometrial polyps, with an average length of 2.2 ± 1.2 cm, 1 patient had vaginal residual polyps after total hysterectomy, with a polyp length of 0.3–0.7 cm, and 1 had multiple vaginal polyps, with a length of 0.5–3 cm. Twelve patients had cervical polyps with an average length of 3.4 ± 1.2 cm. Twenty-one pregnant patients were diagnosed with cervical polyps, the average length of 2.4 ± 1.4 cm. All patients successfully underwent vaginoscopic surgery, for an average surgical duration of 23.5 ± 14.9 min, a bleeding volume of 1–10 mL(4.5 ± 3.4 mL), and an average hospitalisation of 2.7 ± 1.3 days. Throughout the surgical procedures, no complications were encountered, including water intoxication or uterine perforation. Postoperatively, no patients experienced discomforts such as fever or moderate to severe abdominal pain. Furthermore, all non-pregnant women were monitored for a two-month period following surgery, and throughout this interval, there were no reports of abnormal vaginal bleeding, unusual vaginal discharge, or abdominal pain. None of the 21 pregnant women experienced abnormal vaginal bleeding after the surgery. Nineteen of them delivered at full term, and one underwent caesarean delivery at 31 weeks owing to placental abruption. All the newborns had Apgar scores of 10, 10, and 10, and one had a miscarriage at 18 weeks of gestation.
Conclusion
Vaginoscopic surgery through no-touch hysteroscope represents a minimally invasive and highly effective method for addressing female reproductive tract polyps. This approach holds significant clinical value, particularly in the management of cervical polyps during pregnancy.
Keywords: Vaginoscopy, Genital polyps, Minimally invasive approach
Background
Genital polyps are common reproductive tract diseases that occur in approximately 7.8–50% of women. The size and number of polyps vary, and their clinical manifestations are diverse. Cervical polyps occur in approximately 2–5% of cases, often presenting without noticeable early symptoms [1]. They are sometimes detected incidentally during routine physical examinations. However, as polyps enlarge, they may cause symptoms such as contact bleeding, irregular genital bleeding, and vaginal mucositis. Additionally, cervical polyps during pregnancy may proliferate due to hormonal changes, heightening the risk of vaginal bleeding and adverse pregnancy outcomes, including miscarriage, chorioamnionitis, and premature birth [2–4]. Endometrial polyps are characterized by the localized overgrowth of endometrial glands and stroma, forming pedunculated, polyp-like structures that protrude into the uterine cavity. These polyps are relatively common and are typically benign, with only around 1% progressing to malignancy. However, they can cause symptoms such as abnormal uterine bleeding, infertility, pregnancy complications, and abdominal pain [5]. Some endometrial polyps are asymptomatic and are often detected incidentally during ultrasound examinations, discovered during gross examination after a hysterectomy performed for unrelated conditions, or identified through pathological analysis following diagnostic curettage.
The traditional blind curettage technique relies on doctors using curettes to remove endometrial lesions based solely on clinical experience. However, this method is often less effective for lesions located in the uterine fundus and corners. Repeated scraping can damage the endometrium, significantly increasing the risk of postoperative infection, uterine adhesions, and infertility. Additionally, the missed diagnosis rate with blind curettage can be as high as 50–80% [6]. Consequently, this approach is no longer recommended. Hysteroscopy is a powerful tool for the diagnosis of endometrial lesions, making it easy to identify and treat the affected lesions [7, 8]. Hysteroscopic cervical and endometrial polypectomy is the preferred surgical treatment for symptomatic cervical and endometrial polyps, offering advantages such as minimal invasiveness, convenience, rapid recovery, and effective therapeutic outcomes. With the advances of hysteroscopic instruments, Lee et al. has demonstrated the feasibility of polypectomy with a manually driven hysteroscopic tissue removal (HRT) device [8]. Conscious patients with intrauterine disease can also be performed hysteroscopic surgeries [9], and for diagnostic hysteroscopy, the pain is mild and there is no significant difference of visual analog scale (VAS) between room temperature and warmed normal saline solution as distension medium [10]. Although hysteroscopy is often considered as a costly tool, Okohue et al. has successfully performed hysteroscopic surgeries in treating intrauterine diseases in a low-budget hysteroscopy unit, providing a foundation for implementing hysteroscopy surgery in resource scarce setting [11]. There may be indisputable that benefits and convenient of hysteroscopy in the current management of intrauterine disease in clinical practice [7].
The no-touch hysteroscopy (vaginoscopy) eliminates the need for cervical dilation, a vaginal speculum, or cervical forceps, thereby significantly reducing pain during the surgical procedure. This innovative technology facilitates the placement of the hysteroscope to visualize the vagina, cervix, and uterine cavity. Subsequently, hysteroscopic surgical instruments are introduced through the operation channel. This approach not only makes it easier to preserve the hymen but also increases patient comfort and acceptance of the procedure [12].
This study retrospectively analysed the clinical data of 46 female patients with reproductive tract polyps, with aims to evaluate the feasibility and efficacy of no-touch hysteroscope in the management of these diseases in both pregnant and non-pregnant patients.
Methods
Patients
We collected clinical data from 46 female patients with genital polyps who underwent vaginoscopic surgery between April 2017 and May 2023, and conducted a retrospective analysis of patients clinical manifestations, surgical results, pathological results, and treatment. Senior gynaecologists performed all surgeries.
The inclusion and exclusion criteria were as follows:
For pregnant patients
The inclusion criteria were as follows: (1) Repeated irregular vaginal bleeding, (2) Presented to our hospital for prenatal examination and delivery, (3) Gynaecological examination suggesting bleeding caused by cervical polyps, (4) Normal TCT (Thinprep Cytology Test) and HPV within the past year, (5) No vaginitis.
The exclusion criteria for pregnant women were specified as follows: (1) Patients with a submucosal myoma that has prolapsed, (2) Patients who were unable to complete the required follow up, (3) Patients with obstetric complications, including threatened miscarriage, placental abruption, placenta previa, and threatened preterm labor.
-
(2)
For non-pregnant patients
The inclusion criteria were as follows: (1) Aged 18–48 years, (2) Female without a history of sexual activity, (2) Presence of irregular vaginal bleeding, (3) Patients with suspicious endometrial polyps on ultrasound and ineffective oral progesterone treatment for 3 cycles, (4) Patients with suspected vaginal polyps or cervical polyps during physical examination, (5) In addition to the aforementioned inclusion criteria, considering the advantages of no-touch hysteroscope and its accuracy in diagnosing vaginal lesions, we included 2 postmenopausal patients on a voluntary basis (1 with irregular vaginal bleeding after hysterectomy, 1 with postmenopausal vaginal bleeding), and 1 patient of childbearing age with sexual life presented with symptoms suggesting the prolapse of polyps from the vagina, (6) Normal TCT and HPV within the past year for patients with sexual life, (7) No vaginitis.
The exclusion criteria were defined as follows: patients suspected of having endometrial cancer, cervical cancer, or those with concurrent severe dysfunction of the liver, kidneys, or cardiopulmonary system were not eligible for the study.
This study was approved by the Ethics Committee of Beijing Tiantan Hospital Affiliated to Capital Medical University and written informed consent was obtained from all subjects (IRB Number: KY2023-135–02).
Operative technique
A 7- mm/8.5-mm rigid hysteroscope was used to perform vaginoscopic surgery, with 5% glucose (monopolar) or 0.9% physiological saline (bipolar). The dilation pressure was maintained at 100–120 mmHg (1 mmHg = 0.133 kPa) at a flow rate of 300 mL/min. For non-pregnant patients with endometrial or cervical polyps, phloroglucinol (a myotropic, non-atropine, non-papaverine antispasmodic agent, which could act on the uterus by relaxing the cervix and relieving spasmodic contractions of the uterine smooth muscle) was administered intravenously for 3–15 min for ripping the cervix preoperatively.
The patient was placed in the bladder lithotomy position, strictly following aseptic requirements, and a 0.5% iodophor disinfectant was used to sterilise the vulva. The vaginoscopy procedure was conducted with the following specific steps: under the guidance of transabdominal ultrasonography, the hysteroscope was introduced without the use of a vaginal speculum or cervical forceps, and without the need for cervical dilation. The hysteroscope was gently placed through the hymenal fissure under direct vision, allowing for a complete exposure of the vaginal wall, vault, cervix, and vagina. In non-pregnant patients, the hysteroscope was carefully advanced into the cervical canal from the external os. The cervical canal was meticulously observed, and entry into the uterine cavity was achieved through the natural anatomical opening of the cervix. A comprehensive examination of the entire uterine cavity was then systematically performed (Fig. 1). Non-pregnant patients underwent surgery under propofol intravenous anaesthesia using unipolar electrocautery, with an endometrial polypectomy power of 80 W and coagulation power of 60 W; cervical polypectomy and coagulation power of 30 W for monopolar hysteroscopy; and 200 W for bipolar hysteroscopy for cutting and coagulation. After the hysteroscope was inserted into the vagina, cervix, or uterine cavity, vaginoscopic polypectomy was performed in the same manner as traditional hysteroscopy. By closing the labia majora and labia minora, as well as with the dilation pressure and flow velocity, the outflow of perfusion fluid from the vaginal orifice could be reduced, thus to distend the vagina.
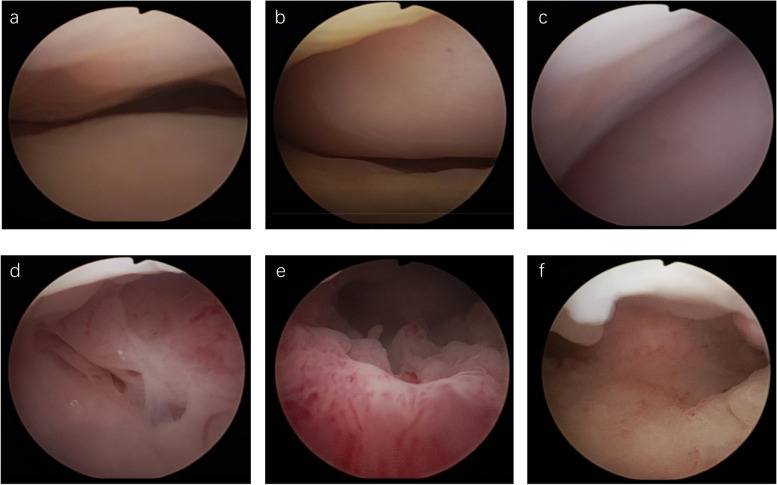
Fig. 1.
The basic procedure of vaginoscopy in non-pregnant patients. a Examine the vagina under vaginoscopy; b Expose the cervix and fornix; c Examine the fornix; d Detect endocervix; e Introduce the hysteroscope into uterine cavity; f Detect the uterine cavity
For pregnant patients, the hysteroscope did not penetrate the cervical canal too deep, it was placed in the external os. Bipolar polypectomy was performed without anaesthesia in the conscious state, and the coagulation power was 200 W.
Surgical complications, such as hemorrhage and damage to adjacent bladder and rectal tissues, are possible concerns. However, with procedures meticulously executed under direct vision, bolstered by the guidance of transabdominal ultrasound and stringent hemostasis control, these complications are largely preventable.
Effect observation.
The primary outcomes assessed for vaginoscopic surgery encompassed several key metrics: success rate, blood loss during surgery, duration of the procedure, and overall therapeutic efficacy. Postoperative evaluations involved vigilant monitoring for fever, abdominal pain, and infections in both the urinary and reproductive tracts. For pregnant patients, additional assessments were conducted to evaluate the occurrence of miscarriages, premature births, and recurrent vaginal bleeding.
Statistical analysis
SPSS software (version 25.0) was used for the statistical analysis. Measurement data are reported as the mean ± standard deviation, and count data are reported as the frequency or frequency (percentage).
Results
Characteristic of patients
Clinical manifestations of patients
The average age of 46 patients was 33.0 ± 8.8 years. Twenty-five were non-pregnant, and of these, 3 had a history of sexual activity, 22 were virgins, and 21 were pregnant (the gestational week was between 12 and 34 weeks, and average week was 19.4 ± 6). Characteristics of patients were reported in Table 1.
Table 1.
Characteristics of study groups
| Patients characteristics | ||
|---|---|---|
| Characteristics | Non-pregnant | Pregnant |
| Age (years) | 34.12 ± 11.2 | 36.61 ± 4.25 |
| BMI ( kg/m²) | 21.78 ± 3.74 | 23.1 ± 3.56 |
| Average gravida (number of times)a | 1.33 | 1.5 |
| Average parity (number of times)a | 0.67 | 0.19 |
| Irregular vaginal bleeding (n) | 11 | 21 |
| Conscious vaginal protrusion (n) | 10 | / |
| Cervical polyps founded by physical examination (n) | 2 | / |
| Postmenopausal vaginal bleeding (n) | 1 | / |
| Vaginal bleeding after total hysterectomy (n) | 1 | / |
aFor non-pregnant patients, the average time of gravida and parity was calculated in patients with sexual life
In non-pregnant patients, the principal clinical manifestations were as follows: irregular vaginal bleeding was observed in 11 cases, 10 cases of conscious vaginal protursion, 2 cases of cervical polyps identified during physical examination, 1 case of postmenopausal vaginal bleeding, and 1 case of vaginal bleeding following a total hysterectomy. The 21 pregnant patients in the study experienced recurrent episodes of intermittent vaginal bleeding throughout their pregnancies. Early in the first trimester, ultrasonography was employed to confirm intrauterine pregnancy. Cervical polyps were identified as a potential source of bleeding after other possible causes were excluded, including threatened miscarriage, inevitable miscarriage, complete miscarriage, placenta previa, placental abruption, premature birth, and vaginitis. The gestational age at surgery for the pregnant patients was 12–34 weeks, the maximus gestational age was 34 weeks, and 1 case with hypothyroidism, 1 case with thyroiditis, 2 cases with concomitant history of asthma, and 2 cases with concomitant mild anemia.
All 46 patients successfully underwent vaginoscopic surgery; 33 underwent cervical polypectomy (12 were non-pregnant, 21 were pregnant), 11 underwent endometrial polypectomy under vaginoscopy (10 were virgins, and 1 was postmenopausal), and 2 underwent vaginoscopic polypectomy (1 with residual vaginal polyps after total hysterectomy and 1 with multiple vaginal polyps). Patients who underwent endometrial polypectomy, including a virgin with challenging cervical access, required dilation without the need for a vaginal speculum, ensuring that the patient's hymen remained intact. All non-pregnant patients with endometrial or cervical polyps were intravenously administered phloroglucinol for 3–15 min before surgery to soften the cervix, and operations were done under abdominal ultrasound monitoring.
There were no complications during or after the surgery, with an average hospital stay of 2.7 ± 1.3 days, an average surgical time of 23.5 ± 14.9 min, and an average surgical blood loss of 4.5 ± 3.4 mL, as estimated by visual inspection. None of the patients experienced water intoxication, uterine perforation, or damage to the adjacent organs (bladder, ureter, or intestinal canal). Pain was evaluated by VAS ranging from 0–2 points one hour after surgery. None of the patients had fever, moderate or severe abdominal pain, abnormal vaginal discharge, or postoperative discomfort postoperatively.
-
(2)
Postoperative pathological diagnosis
Among the 25 non-pregnant patients, 3 had a sexual history, of whom 2 were postmenopausal women diagnosed with endometrial polyp and inflammatory polyps of the vaginal stump after total hysterectomy, and one was diagnosed with multiple vaginal polyps during her child-bearing years. In total, 22 patients had no history of sexual activity; 10 of whom were diagnosed with endometrial polyps, the remaining 12 patients were diagnosed of cervical polyps. All 10 endometrial polyps patients with no history of sexual activity were administered combined oral contraceptives or progesterone postoperatively. In addition, all 21 pregnant patients were diagnosed with cervical polyps, 6 of whom had stromal with decidual degeneration (Table 2). The diagnoses made through vaginoscopy and pathology were found to be in perfect concordance, with an accuracy rate of 100%.
Table 2.
Diagnosis of 46 patients with genital polyps
| Cases(n) | ||
|---|---|---|
| Diagnosis | Non-pregnant | Pregnant |
| Cervical polyps | 12 | 21 |
| Endometrial polyps | 11 | / |
| Polyps of the vaginal stump | 1 | / |
| Vaginal polyps | 1 | / |
Among the 12 non-pregnant patients diagnosed with cervical polyps, 2 had multiple polyps, while 10 had a solitary polyp. The size of the cervical polyps varied, with lengths ranging from 1.2 to 5 cm, and an average length of approximately 3.4 ± 1.2 cm. In the case of the 11 patients with endometrial polyps, 3 had multiple endometrial polyps, and 8 had single endometrial polyps. The average size of the endometrial polyps was 1– 4 cm, with an average length of 2.2 cm ± 1.2 cm. Twenty-one pregnancies were complicated by cervical polyps, including 19 patients with single cervical polyps and two with multiple cervical polyps. The size of cervical polyps was 1–5 cm, with an average length of 2.4 ± 1.4 cm.
-
(3)
Follow-up
Non-pregnant patients underwent postoperative follow-up for two months, during which no instances of abnormal vaginal bleeding or secretions were detected. In total, 21 pregnant patients had been followed up. Among them, 20 had completed their pregnancies without any reported abnormal vaginal bleeding. Nineteen of these patients had full-term deliveries, while one underwent a caesarean section at 31 weeks due to placental abruption. In that case, the neonate had an Apgar score of 10, indicating a healthy status. Additionally, one patient experienced a miscarriage at 18 weeks of pregnancy.
Discussion
Advantages of vaginoscopy
Hysteroscopy is the gold standard for the diagnosis of intrauterine diseases. Compared to traditional hysteroscopy, vaginoscopy has the following advantages. (1) The use of a vaginal speculum or the application of traction and fixation with cervical forceps is unnecessary. Patients can be examined in a more relaxed state, which not only prevents iatrogenic stimuli from triggering genital muscle spasms and mental stress, facilitating the procedure, but also significantly alleviates pain during hysteroscopy [13–15]. (2) Vaginoscopy is a straightforward procedure that significantly reduces the risk of hymenal injury. Moreover, unencumbered by the constraints of a vaginal speculum, the hysteroscope can navigate the natural curvature of the cervical canal and uterus, providing a more direct path into the uterine cavity. This flexibility allows for a broader range of motion, enhancing the examination's effectiveness. Vaginoscopic approach is ideal for virgins, and older women with vaginal stenosis [16]. In paediatric patients, the insertion of foreign bodies into the vagina causes persistent discharge, infection, and even tissue fibrosis, and vaginoscopy is the optimal strategy for diagnosis and treatment of vaginal foreign bodies [17].
Application of vaginoscopic surgery in female reproductive tract polyps
Celibate women can experience symptoms such as irregular vaginal bleeding and secretions. However, some traditional habits and cultures, particularly concerns about hymen integrity, often limit gynaecological examinations, which can delay diagnosis. Vaginoscopy has expanded the capabilities of hysteroscopic procedures. By carefully inserting the hysteroscope into the vagina, a liquid medium can be introduced, allowing for magnified visualization without the use of a speculum. This approach facilitates timely diagnosis and treatment of vaginal and intrauterine conditions.
In this study, 22 celibate women experienced abnormal bleeding or vulvar secretions that seriously affected their daily lives. No complications or hymen damage were observed during the operation, reducing the psychological burden on patients and families. The first recurrence rate after hysteroscopic polypectomy is 24.35% [18], so oral progesterone or short-term contraceptive pills were administered in ten virgin patients with endometrial polyps to suppress the recurrence after surgery. None of the patients developed fever or abnormal bleeding after surgery, and 12 patients were diagnosed with cervical polyps. Facing challenges in accessing the cervix in a virgin patient with endometrial polyps, we utilized transabdominal ultrasonography to guide our efforts, based on operators’experience, we carefully attempted to clamp and gradually dilate the cervix without the use of a speculum. The approach was successful, and the hymen of the virgin patient remained unscathed. It is possible that the use of micro instruments could further minimize the need for dilation in such delicate procedures. Asexual patients are prone to mental stress and anxiety due to factors such as age and traditional thoughts. Therefore, preoperative communication and humane care should be provided.
The decline in estrogen levels in postmenopausal women and cervical atrophy cause the original squamocolumnar junction to retract into the often narrow and curved cervical canal, and increasing the risk of diagnostic challenges, including missed or incorrect diagnoses. Traditional hysteroscopy often overlooks lesions in the vagina and cervical canal, whereas vaginoscopy allows for the direct insertion of a hysteroscope through the vagina, offering an unobstructed view of the vaginal walls, cervical canal, and uterine cavity. This technique facilitates the performance of biopsies or lesion excision under direct visualization, thereby enhancing the precision of tissue sampling and significantly reducing the likelihood of overlooking pathologies [19]. In this study, there were two menopausal women: one with postmenopausal vaginal bleeding who was diagnosed with endometrial polyps, and another with abnormal vaginal bleeding 10 years after total hysterectomy. Vaginoscopy revealed clusters of polyps approximately 0.3-0.7 cm in length in the vaginal stumps. In addition, one patient of reproductive age had conscious external genital protrusion, and vaginoscopy revealed multiple polyps of 0.5-3 cm length in the vagina that were simultaneously removed. For patients presenting with vaginal strictures, challenges in cervical exposure, or vaginal pathologies, vaginoscopy offers the advantage of fully exposing the vagina and cervix. This approach not only enhances the success rate of diagnostic examinations but also improves the efficacy of therapeutic interventions.
Cervical polyps, which can lead to abnormal bleeding, vaginal discharge, and mucosal inflammation, warrant surgical intervention upon confirmation of diagnosis. During pregnancy, physiological changes may cause rapid growth of cervical polyps, with larger ones potentially protruding or even detaching from the vaginal orifice, significantly increasing the risk of vaginal bleeding and infection. The management of cervical polyps during pregnancy remains controversial. Wakimoto et al. conducted a study on 4,172 pregnant women, in which 92 patients had cervical polyps (discovered during the first 12 weeks of pregnancy and did not undergo polypectomy). Results showed that pregnant women with cervical polyps had a higher incidence of spontaneous premature birth before 34 weeks of pregnancy than did those without cervical polyps (5.4% vs. 0.7%, P < 0.01). They hypothesised that cervical polyps detected during the first 12 weeks of pregnancy were risk factors for premature birth and were related to premature birth before 34 weeks [20]. Our previous study suggested that, compared with those in the conservatively treated group, the incidences of premature birth, infection, recurrent vaginal bleeding, and premature rupture of membranes after hysteroscopic cervical polypectomy during pregnancy were lower, which could reduce the occurrence of pregnancy complications [21]. Polypectomy is feasible for patients with recurrent vaginal bleeding caused by cervical polyps during pregnancy for whom conventional conservative treatment is ineffective. However, hysteroscopic removal of cervical polyps during pregnancy is controversial, and evidence about this topic is scarce. A recent meta-analysis revealed that removal of decidual or endocervical polyps is related to an increased risk of pregnancy loss and preterm birth [22]. Pregnancy is a long process for which additional data and inclusion in multi-centre studies are needed in the future to summarise and explore the impact of cervical polypectomy during pregnancy period. Vaginoscopy can also be used to electrically remove polyps from the pedicle to reduce recurrence, making it an ideal method for removal cervical polyps. In this study, 21 pregnant women (12–34 weeks) experienced recurrent vaginal bleeding symptoms during pregnancy, and were suspected of cervical polyps. Vaginoscopic surgery was performed, and postoperative pathology revealed cervical polyps, six of which cases were stromal with decidual transformation. Since the postoperative pain in pregnant patients in our study was either mild discomfort or no pain at all, and no analgesics were given.
Twenty-one patients had no abnormal vaginal bleeding after surgery, including 20 patients who gave birth and 1 patient at 18 weeks of gestation who had a miscarriage 3 weeks after surgery. The patient had no fever, lower abdomen pain, or external genital odor, we hypothesized that the miscarriage might not be caused by intrauterine infection after surgery. However, the specific reasons for the embryo failure remained unclear. Although the probability of infection and miscarriage caused by hysteroscopic surgery is low, the operator should be extremely cautious when counselling patient about risks and benefits. Currently, there is no clear evidence regarding the timing of surgery for cervical polyps during pregnancy, and further research is needed. In this study, pregnant patients with cervical polyps were successfully removal without anaesthesia, reducing the discomfort caused by speculum, and the patients and their families were highly satisfied.
Precautions during hysteroscopic surgery under vaginoscopy
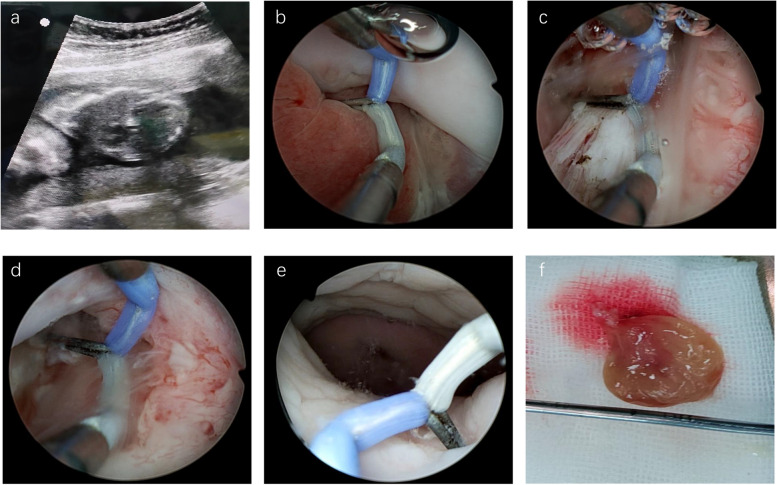
Guraslan et al. previously reported 38% patients experience moderate pain and 5% showed serve pain [23]. Vaginoscopy can significantly reduce patient discomfort, enhance the convenience of hysteroscopic diagnosis, and improve patient satisfaction. For non-pregnant patients, following the concept of 'timely diagnosis and immediate treatment,' the removal of cervical or endometrial polyps via vaginoscopy is comparable to traditional hysteroscopic polypectomy once the hysteroscope enters the uterine cavity. For pregnant patients, cervical polyps are removed to prevent irregular bleeding or infection, and a circular electrode is first used to observe the appearance of polyps and determine the location of resection. The needle-shaped electrode is then used for slow electrocoagulation and removal of the polyp tissue at the external os (as shown in Fig. 2 and the surgical procedure is shown in the video). The operative technique limits the depth of hysteroscope insertion into the cervical canal, reducing the risk of premature membrane rupture. Additionally, with abdominal ultrasound guidance, the procedure can be performed without anesthesia, allowing pregnant women to undergo surgery while the observation of a normal fetal heartbeat helps alleviate their anxiety.
Fig. 2.
Basic operative procedures of cervical polypectomy via vaginoscopy for pregnant patients. a Abdominal ultrasound to monitor fetal heart during operation; b Needle shaped electrode was placed at the cervical external; c Coagulation of the cervical polyps at the external os; d Resection of the cervical polyp and electrocoagulation for hemostasis; e: The cervical polyp was removed; f The resected polyp
During pregnancy, vaginoscopic resection of cervical polyps is conducted with low-pressure dilation, maintaining approximately 100–120 mmHg, to minimize the risk of excessive water pressure during entry into the uterine cavity and to reduce the likelihood of reflux infection. Proper water pressure management is essential during these procedures. This technique, performed without anesthesia and using a no-touch hysteroscopic approach without a speculum, significantly reduces patient pain and discomfort. Cervical polypectomy during pregnancy has traditionally been performed using methods such as oval forceps clamping or loop ligation, these procedures require the use of a speculum, which can often cause significant discomfort to the patient and may even necessitate anesthesia to ensure the smooth completion of the surgery. Furthermore, these techniques are associated with suboptimal hemostasis and prolonged surgical time, increasing the risk of postoperative infection. Compared to these modalities, bipolar electrosurgical polypectomy through vaginoscopy offered several advantages, including rapid execution, enhanced safety, minimal bleeding, and reduced pain in pregnant patients. This approach not only simplifies and accelerates the procedure but also ensures adequate hemostasis, reducing the incidence of postoperative vaginal bleeding and infection. Additionally, patients can remain fully conscious during the procedure, experience minimal to no pain.
Surgeons need to undergo systematic training in vaginoscopy technology; understand and master the operating skills of this technology; prevent and treat complications [24]. The general recommendation is to independently perform hysteroscopy examinations on at least 500 patients and complete at least 100 vaginoscopic surgeries under the guidance of superiors or specialists with experience before performing the surgery independently [24]. During cervical polypectomy in pregnancy using vaginoscopy, we recommend an abdominal ultrasound examination performed by a physician for enhanced monitoring. As anesthesia is unnecessary, a physician or surgical nurse should remain attentive to the patient’s overall condition and needs throughout the procedure. Alternatively, nursing staff can provide compassionate care to ensure patient comfort. The primary goal of cervical polyp removal is to prevent further bleeding and accurately identify the optimal removal site, helping to minimize the risk of complications such as retrograde surgery and infection.
Conclusion
There are some limitations in this study. First, as a retrospective analysis, it includes a limited sample size, we plan to include more patients prospectively to better evaluate and compare the therapeutic efficacy of vaginoscopic surgery with traditional hysteroscopic surgery in treating intrauterine diseases. Second, we have not conducted a comparative study on cervical polyp surgeries at different gestational stages or with traditional hysteroscopic surgery during pregnancy. This aspect requires further exploration to offer more tailored treatment options for patients in the future.
In practice, for non-pregnant patients, the difficulty of vaginoscopic technology lies in identification of cervical os and passing cervical canal, as well as in controlling the force and direction of the inserted endoscope, which may increase the risk of side injuries. But these problems can be overcome through standardized operation training and regular practice. Based on doctor’s experience, with ultrasound guidance, doctors can also use the top of the hysteroscope to press down or lift up forcefully, slowly enter the uterine cavity, in some cases it can be successful. However, if there are difficulties in entry into cervical canal, the cervix will be expanded without using speculum under ultrasound guidance, or a probe was used to bluntly separate cervical adhesions and dilate the cervix; or using miniature scissors through the working channel by a slender hysteroscope to separate adhesions [24]. Uterine perforation is the main risk and operators should be altered.
In summary, this study suggests that vaginoscopic resection of genital polyps is minimally invasive, safe, and effective and is worth recommending. The use of intraoperative ultrasound guidance allows for precise, non-invasive, and cost-effective monitoring of instrument positioning. Vaginoscopy polypectomy shows promise for pregnant patients, with real-time fetal heartbeat monitoring helping to reduce anxiety. Advances in endoscopic surgery and the refinement of hysteroscopic instruments, including smaller instrument diameters, have broadened the range of possible hysteroscopic procedures, enabling effective treatment for cervical polyps during pregnancy and for reproductive tract abnormalities in asexual and postmenopausal women.
Acknowledgements
None.
Authors’ contributions
HX. L. and LM. F. conceived the study. All authors collected the Data. BJ. Y., WL. G. and CY. Huang. searched literature. HX. L., CX. L. and H. Z. prepared tables and figures. The first draft of manuscript was written by HX. L., LM. F. and all authors commented on previous versions of the manuscript. All authors reviewed the manuscript.
Funding
None.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Beijing Tiantan Hospital Affiliated to Capital Medical University (IRB Number: KY2023-135–02). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tanos V, Berry KE, Seikkula J, Abi Raad E, Stavroulis A, Sleiman Z, et al. The management of polyps in female reproductive organs. Int J Surg. 2017;43:7–16. 10.1016/j.ijsu.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Hirayama E, Ebina Y, Kato K, Akabane-Nakagawa K, Okuyama K. Cervical polyps in early pregnancy are a risk factor for late abortion and spontaneous preterm birth: A retrospective cohort study. Int J Gynaecol Obstet. 2022;156(1):64–70. 10.1002/ijgo.13608. [DOI] [PubMed] [Google Scholar]
- 3.Levin G, Rottenstreich A. 2nd trimester miscarriage following decidual polypectomy. Eur J Obstet Gynecol Reprod Biol. 2018;225:262–3. [DOI] [PubMed] [Google Scholar]
- 4.Romero R, Miranda J, Chaiworapongsa T, Korzeniewski SJ, Chaemsaithong P, Gotsch F, et al. Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol. 2014;72:458–74. 10.1111/aji.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nijkang NP, Anderson L, Markham R, Mancoin F. Endometrial polyps: Pathogenesis, sequelae and treatment. SAGE open medicine. 2019;7:2050312119848247. 10.1177/2050312119848247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Timmermans A, Gerritse MB, Opmeer BC, Jansen FW, Mol BW, Veersema S. Diagnostic accuracy of endometrial thickness to exclude polyps in women with postmenopausal bleeding. J Clin Ultrasound. 2008;36(5):286–90. 10.1002/jcu.20415. [DOI] [PubMed] [Google Scholar]
- 7.Wang PH. A Powerful Value of Hysteroscopy. Gynecol Minim Invasive Ther. 2018;7(4):143–4. 10.4103/GMIT.GMIT_71_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee MMH. Endometrial Polyp Removed by a Manual Hysteroscopic Tissue Removal Device. Gynecol Minim Invasive Ther. 2020;9(1):34–5. 10.4103/GMIT.GMIT_116_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yen CF, Chou HH, Wu HM, Lee CL, Chang TC. Effectiveness and appropriateness in the application of office hysteroscopy. J Formos Med Assoc. 2019;118(11):1480–7. 10.1016/j.jfma.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Sharma S, Roy KK, Rai R, Zangmo R, Malhotra N, Das A. Assessment of pain at different steps of diagnostic hysteroscopy using room temperature normal saline versus warmed normal saline solution as distension medium: A randomized controlled trial. Gynecol Minim Invasive Ther. 2022;11:41–6. 10.4103/GMIT.GMIT_5_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okohue JE, Okohue JO (2020). Establishing a Low-Budget Hysteroscopy Unit in a Resource-Poor Setting. Gynecol Minim Invasive Ther. 23;9(1):18–23. 10.4103/GMIT.GMIT_11_19. [DOI] [PMC free article] [PubMed]
- 12.Smith PP, Kolhe S, O’Connor S, Clark TJ. Vaginoscopy Against Standard Treatment: a randomised controlled trial. BJOG. 2019;126(7):891–9. 10.1111/1471-0528.15665. [DOI] [PubMed] [Google Scholar]
- 13.Di Spiezio SA, Zizolfi B, Calagna G, Florio P, Nappi C, Di Carlo C. Vaginohysteroscopy for the diagnosis and treatment of vaginal lesions. Int J Gynaecol Obstet. 2016;133(2):146–51. 10.1016/j.ijgo.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Garbin O, Kutnahorsky R, Göllner JL. Vaginoscopic versus conventional approaches to outpatient diagnostic hysteroscopy: a two-centre randomized prospective study. Hum Reprod. 2006;21(11):2996–3000. 10.1093/humrep/del276. [DOI] [PubMed] [Google Scholar]
- 15.Bettocchi S, Ceci O, Di Venere R, Pansini MV, Pellegrino A, Marello F, et al (2002) Advanced operative office hysteroscopy without anaesthesia: analysis of 501 cases treated with a 5 Fr. bipolar electrode. Hum Reprod.17(9):2435–2438. 10.1093/humrep/17.9.2435. [DOI] [PubMed]
- 16.Yıldız S, Ekin M, Cengiz H, Dağdeviren H, Kaya C. Vaginal foreign body: Successful management with vaginoscopy. J Turk Ger Gynocol Assoc. 2013;14(1):46–7. 10.5152/jtgga.2013.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bettocchi S, Selvaggi L. A vaginoscopic approach to reduce the pain of office hysteroscopy. J Am Assoc Gynecol Laparosc. 1997;4(2):255–8. 10.1016/s1074-3804(97)80019-9. [DOI] [PubMed] [Google Scholar]
- 18.Cea García J, Jiménez Caraballo A, Ríos Vallejo MDM, Zapardiel I. Retrospective Cohort Study on the Symptomatic Recurrence Pattern after Hysteroscopic Polypectomy. Gynecol Minim Invasive Ther. 2020;9(4):209–14. 10.4103/GMIT.GMIT_102_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Spiezio Sardo A, Giampaolino P, Manzi A, De Angelis MC, Zizolfi B, Alonso L, et al. The Invisible External Cervical Os. Tips and Tricks to Overcome this Challenge during In-Office Hysteroscopy. J Minim Invasive Gynecol. 2021;28(2):172–173. 10.1016/j.jmig.2020.05.027. [DOI] [PubMed]
- 20.Wakimoto T, Hayashi S, Koh I, Yamamoto R, Ishii K. Relationship between unremoved cervical polyp in pregnancy and spontaneous preterm birth. Am J Obstet Gynecol. 2022;227(6):899.e1–899.e6. 10.1016/j.ajog.2022.06.064. [DOI] [PubMed] [Google Scholar]
- 21.Huang CY, Feng LM, Yang BJ, Li CX. Applicaion of hysteroscopy in the treatment of cervical polyp during pregnancy. Chin J Laparoscopic Surg (Electronic Edition). 2021;14(02):81–4. [Google Scholar]
- 22.Riemma G, Della Corte L, Vitale SG, Cianci S, La Verde M, Giampaolino P, et al. Surgical management of endocervical and decidual polyps during pregnancy: systematic review and met-analysis. Arch Gynecol Obstet. 2023;307(3):673–80. 10.1007/s00404-022-06550-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guraslan H, Senturk MB, Dogan K, Yuksel B, Kaya C, Karacan T, et al. Diagnostic office hysteroscopy; why is it still painful procedure despite the surgical experience and mini-hysteroscope. J Obstet Gynaecol Res. 2022;48(6):1418–25. 10.1111/jog.15219. [DOI] [PubMed] [Google Scholar]
- 24.Zhang h, Wei l, Feng lm,. Chinese experts’ recommendation on vaginal endoscopy technology. J Med. 2022;57(02):129–33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.