Abstract
BACKGROUND:
Despite oxygen therapy guidelines, suboptimal practices prevail among front-line resident doctors, highlighting knowledge and attitudinal barriers. Mixed-methods research can inform tailored quality improvements. This study aimed to assess the knowledge, attitudes, and practices of resident doctors regarding oxygen therapy, determine associated factors quantitatively, and explore experiences, barriers, and enablers qualitatively.
MATERIALS AND METHODS:
This was a convergent parallel mixed-methods study conducted at a tertiary teaching hospital. An analytical cross-sectional survey of 410 resident doctors assessed knowledge, attitudes, and practices using a questionnaire. Qualitative phenomenology entailed in-depth interviews with 30 participants analyzing experiences and perspectives. Integration enabled corroborating and complementing findings. Logistic regression analysis and thematic analysis were used to make themes and subthemes.
RESULTS:
Most demonstrated suboptimal knowledge (78% or 320/410 good), attitudes (61.7% or 253/410 positive), and practices (47.8% or 196/410 good). Significant factors were gender, experience, workload perceptions, and device familiarity. Males had 5.5 times higher odds of good knowledge (adjusted odds ratio (AOR) 5.5, 95% confidence interval (CI) 3.25–10). Those perceiving workload impact had 13 times higher odds of positive attitudes (AOR 13, 95% CI 9.4–20.9). Qualitative themes highlighted inadequate skills and time constraints as barriers and protocolization and decision tools as enablers.
CONCLUSION:
Gaps exist in knowledge, attitudes, and practices regarding oxygen therapy among resident doctors attributable to varied factors. Tailored quality improvement strategies addressing demonstrated barriers, such as enablement workshops, order set integration, and pulse oximetry audits, are recommended based on mixed-methods insights.
Keywords: Attitude of health personnel, knowledge, oxygen therapy, physicians, practice patterns, quality improvement, teaching hospital
Introduction
Oxygen therapy forms an essential component of care across medical and surgical specialties for managing hypoxemia due to diverse etiologies.[1] Even transient periods of hypoxemia can adversely impact outcomes, and optimal oxygen administration requires precise titration of administration devices and flow rates based on continuous monitoring.[2] Despite the existence of clinical practice guidelines on evidence-based oxygen therapy, multiple studies globally highlight prevalent gaps in knowledge, attitudes, and practices among healthcare providers—including inaccurate assessments, inappropriate prescriptions, and the tendency for oxygen overuse without clear benefit.[3,4]
Resident doctors comprise the front-line medical care providers in hospitals, and their knowledge and compliance with oxygen therapy guidelines can directly impact patient outcomes and safety. However, evidence from limited studies in developing nations indicates considerable lacunae and barriers that exist in their proper prescription and delivery of oxygen treatment.[5] Beyond the assessment of knowledge gaps, vital to improving practices is an in-depth exploration of perceptions, beliefs, experiences, and behaviors that underpin suboptimal oxygen administration. This necessitates going beyond quantification and using qualitative inquiry to illuminate contextual factors and pragmatic solutions from the resident doctor’s perspective.
Despite the availability of evidence-based guidelines, suboptimal practices are widely prevalent, highlighting the need for contextual inquiry and solutions.[2] As front-line care providers, evaluating the perspectives of resident doctors can provide insights into improving training, monitoring, and tailoring contextually appropriate quality improvement initiatives for oxygen therapy in resource-limited hospitals. Quantifying knowledge attitudes and practices and their influencing factors through surveys, along with lived experiences from interviews, can lead to pragmatic recommendations through this explanatory mixed-methods approach.
Mixed-methods studies allow a holistic understanding of complex interventions by combining the strengths of quantitative assessments of practices and their statistical correlates along with qualitative exploration of real-world enablers, barriers, and potential improvements.[6] This pragmatic approach bridges critical evidence-practice gaps for translating guidelines to context-specific solutions.[7] However, there is a lack of mixed-methods studies evaluating oxygen therapy delivery in resource-limited hospital contexts, considering provider perspectives. This study aimed to assess the knowledge, attitudes, and practices of resident doctors regarding oxygen therapy and quantify their self-reported determinants using a survey. Complementarily, in-depth interviews elicited experiences, perceived barriers, and facilitators to inform tailored quality improvement strategies.
Materials and Methods
Study design and setting
A mixed-methods study was conducted on the resident government doctors working in the tertiary care hospital, in Gujarat, during January–June 2023. The quantitative aspect, employing an analytical cross-sectional design with a convergent parallel approach, enabled a comprehensive understanding of the prevalence of good knowledge, attitudes, and practices. The qualitative facet, grounded in phenomenology, was used and provided depth by exploring individual experiences, barriers, and facilitators related to oxygen therapy among resident doctors involved in its application.
Study participants and sampling
All resident doctors irrespective of their departments working in the tertiary care hospital in Gujarat who were available in the study period and who gave consent were included. Participants who did not give consent to participate in the study were excluded.
The single population proportion formula was used to determine the sample size. It was calculated by considering 95% confidence interval (CI), a 5% margin of error, and 54.6% as a proportion of knowledge level about oxygen therapy.[8]
n = z2(p) (1 − p) d2, where n—sample size and p—proportion (50%).
d – Precision (0.05)
3.84*54.6*45.4/25 = 390
Using a stratified random (by clinical and nonclinical departments) sampling technique, all resident doctors were invited to participate in the study.
So, we got a sample size of 410.
In the qualitative arm: Resident doctors involved in oxygen therapy were enrolled through a Purposive sampling technique (30 participants for maximum variation.)
Data collection tool and technique
The consent was obtained through electronic forms. The assessment was performed with a self-structured questionnaire containing 25 questions that tested knowledge, attitude, and practice regarding oxygen therapy. Two data collectors will be employed in the data collection process. A self-administered questionnaire was prepared and used in the English language. The data collection tool was prepared from different literature, which was performed on the same topic abroad.[8] A total of six knowledge, six attitude, and six practice questions were used. The sum of correct responses for the six knowledge questions and six practice questions will be computed and expressed as the mean score to categorize whether study participants have good or poor knowledge and practice, respectively. Similarly, attitude was measured on a 5-point Likert scale and expressed as the mean score to categorize whether study participants have a positive or negative attitude. The reliability of the tool was checked using the reliability coefficient (Cronbach’s alpha) and was 0.82 for all knowledge, attitude, and practice questions. In the qualitative arm, semi-structured in-depth interviews were conducted to explore barriers, facilitators, experiences, and perspectives about oxygen therapy.
Ethical consideration
Ethical clearance and permission to conduct the research were obtained from the ethical research committee of the college. Written informed consent was presented and obtained from each study participant ((EC/NEW/INST/2021/1896) ref 01/01/2023).
Statistical analysis
The data were analyzed using Statistical Package for the Social Sciences (SPSS) version 20. Frequencies and percentages summarized categorical sociodemographic and work-related variables. Knowledge, attitudes, and practices were categorized as good vs poor, positive vs negative, and good vs poor based on the mean scores of the relevant questionnaire sections.
Bivariate logistic regression analyzed associations between explanatory variables and outcomes. Statistically significant factors (P ≤ 0.2) were entered into multivariate models to determine independent predictors. Adjusted odds ratios (AORs) with 95% CIs assessed the strength of associations. P ≤ 0.05 was considered statistically significant.
Additionally, interaction terms between gender and experience, departments and device familiarity, and experience and workload perception were added to regression models to evaluate effect modification. Linear regression modeling further explored predictors of higher attitude scores.
For qualitative data, transcripts underwent systematic coding and thematic analysis using content analysis methodology. The text was organized into categories, which were further condensed into major themes related to barriers, enablers, experiences, and perspectives regarding oxygen therapy delivery. Quantitative and qualitative findings were merged to achieve a complementary convergence of results.
Operational Definitions
Knowledge
Knowledge: Study participants who scored the mean score and above (≥4) on the knowledge questions were considered to have good knowledge of oxygen therapy, whereas those who scored below the mean score (<4) were considered to have poor knowledge.
Attitude
Attitude: Participants who answered ≥21 (mean score) of the attitude questions were considered to have a positive attitude toward oxygen therapy and <21 were considered to have a negative attitude.
Practice
Participants who scored 3 and above (the mean score) on the practice questions were considered to have good practice and those who scored <3 were considered to have poor practice.
Results
The mean scores of the knowledge, attitude, and practice questions among the participants were 4, 21, and 3, respectively. Around 78% of the participants answered above the mean value of knowledge participants, and 47.8% answered above the mean value of the practice questions. Of the participants, 61.7% answered above the mean value of the attitude questions [Figure 1].
Figure 1.
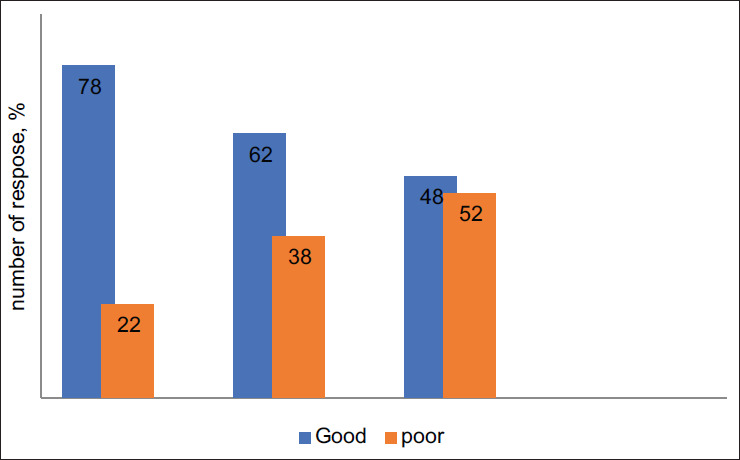
The overall results of the outcome variable for resident doctors
Table 1 provides a comprehensive overview of the sociodemographic and work-related characteristics of the 410 participants. Almost an equal distribution was observed among age groups, with 47% being 25 years or younger and 53% over 25. The majority of participants were male (70%), and a significant proportion hailed from clinical departments (69%). Additionally, the study consisted mostly of individuals with less than 5 years of experience (79%). Notably, a substantial 75% perceived workload as an influencing factor in oxygen therapy, while 60% were familiar with oxygen devices.
Table 1.
Sociodemographic and work-related characteristics (n=410)
| Variables | Category | Response, n (%) |
|---|---|---|
| Age | ≤25 years >25 years |
194 (47) 216 (53) |
| Gender | Male Female |
285 (70) 125 (30) |
| Department | Nonclinical Clinical |
126 (31) 284 (69) |
| Experience | <5 years ≥5 years |
87 (21) 323 (79) |
| Do you think workload affects oxygen therapy? | Yes No |
307 (75) 103 (25) |
| Familiar with using devices for oxygen therapy? | Yes No |
248 (60) 162 (40) |
Table 2 delves into factors correlated with knowledge about oxygen therapy. While age and department did not exhibit significant associations, noteworthy correlations were evident. Males displayed markedly higher odds of good knowledge, with an AOR of 5.5 (P < 0.001). Moreover, participants familiar with oxygen devices showed 5.4 times higher odds of good knowledge (AOR 2.3, P < 0.001). Notably, those acknowledging workload impact exhibited significantly increased knowledge, with 35 times higher odds (AOR 8, P < 0.001).
Table 2.
Factors associated with knowledge of resident doctors
| Variables | Knowledge |
COR 95%CI | AOR 95%CI | p | ||
|---|---|---|---|---|---|---|
| Good, n (%) | Poor n (%) | |||||
| Age | ≤25 year | 151 (78) | 43 (22) | |||
| >25 years | 169 (78) | 47 (22) | 1.02 0.6-1.56 | - | 0.496 | |
| Gender | Male | 200 (70) | 85 (30) | |||
| Female | 119 (95) | 6 (5) | 10 3.97-25 | 5.5 3.25-10 | <0.001* * | |
| Experience | ≥5 years | 244 (75) | 79 (25) | 2.2 1.1-4.4 | 1.8 1.09-3.3 | 0.02* |
| <5 years | 76 (87) | 11 (13) | ||||
| Department | Clinical | 220 (77) | 64 (23) | 0.89 0.5-1.49 | - | 0.345 |
| Nonclinical | 100 (79) | 26 (21) | ||||
| Familiar with oxygen | Yes | 222 (89) | 26 (11) | 5.4 3.2-9.0 | 2.3 1.2-3.82 | < 0.001** |
| devices | No | 98 (60) | 64 (40) | |||
| Do you think workload | Yes | 297 (97) | 10 (3) | 35 17.4-72 | 8.02 6.6-14 | <0.001** |
| affects oxygen therapy? | No | 23 (22) | 80 (78) | |||
*P<0.05—significant, **P<0.001—highly significant, Cl—confidence interval, AOR—adjusted odds ratio, COR—crude odds ratio
Table 3 explores factors linked to a positive attitude toward oxygen therapy. Significant associations were identified across gender, experience, department, familiarity with devices, and, notably, workload perception. The strongest correlation was observed for workload perception, with participants perceiving its impact as exhibiting a 40 times higher crude odds ratio (COR) and a 13 times higher AOR for a positive attitude (P < 0.001).
Table 3.
Factors associated with an attitude of resident doctors
| Factor variables | Attitude |
COR 95% CI | AOR 95%CI | p | ||
|---|---|---|---|---|---|---|
| Positive, n(%) | Negative n (%) | |||||
| Age | ≤25 years | 114 (59) | 80 (41) | 1.26 0.85-1.88 | - | 0.344 |
| >25 years | 139 (64) | 77 (36) | ||||
| Gender | Male | 204 (72) | 81 (28) | 3.9 2.5-6.24 | 2.4 1.2-5.4 | <0.001** |
| Female | 49 (39) | 76 (61) | ||||
| Experience | ≥5 years | 215 (66) | 108 (44) | 2.5 1.5-4.1 | 2.2 1.18-4.17 | <0.005* |
| <5 years | 38 (44) | 49 (56) | ||||
| Department | Clinical | 188 (66) | 96 (44) | 1.8 1.9-2.8 | 1.6 1.2-2.6 | <0.001** |
| Nonclinical | 65 (51) | 61 (49) | ||||
| Familiar with using devices | Yes | 187 (75) | 61 (25) | 4.4 2.9-6.8 | 3.2 2.4-5.5 | <0.001** |
| for oxygen therapy | No | 66 (40) | 96 (59) | |||
| Workload affects oxygen | Yes | 244 (79) | 63 (21) | 40.4 19.3-84 | 13 9.4-20.9 | <0.001** |
| therapy | No | 9 (9) | 94 (91) | |||
P<0.05—significant*, P<0.001—highly significant**
Table 4 elucidates factors associated with good oxygen therapy practices. Males displayed slightly higher odds of good practice (AOR 1.4, P = 0.025), while the clinical department exhibited notably higher odds (AOR 3.38, P < 0.001). Familiarity with devices demonstrated a significant positive association, yielding an AOR of 3.3 (P < 0.001). Furthermore, participants acknowledging workload impact showed significantly increased odds of good practice, with an AOR of 2.4 (P < 0.001).
Table 4.
Factors associated with the practice of resident doctors
| Factor variables | Practice |
COR 95% CI | AOR 95% CI | p | ||
|---|---|---|---|---|---|---|
| Good, n (%) | Poor n (%) | |||||
| Age | ≤25 years | 97 (50) | 97 (50) | 1.18 0.8-1.74 | - | 0.399 |
| >25 years | 99 (46) | 117 (54) | ||||
| Gender | Male | 147 (52) | 138 (48) | 1.61 1.06-2.5 | 1.4 1.01-2.6 | 0.025 * |
| Female | 49 (39) | 76 (61) | ||||
| Experience | ≥5 years | 157 (49) | 166 (51) | 1.1 0.7-1.87 | - | |
| <5 years | 39 (45) | 48 (55) | 0.53 | |||
| Department | Clinical | 165 (58) | 119 (42) | 4.2 2.5-6.7 | 3.38 2.79-10.74 | <0.001* |
| Nonclinical | 31 (25) | 95 (75) | ||||
| Familiar with using devices | Yes | 158 (53) | 90 (47) | 5.7 3.6-8.9 | 3.3 2.8-5.4 | <0.001 ** |
| for oxygen therapy | No | 38 (37) | 124 (63) | |||
| Workload affects oxygen | Yes | 162 (32) | 145 (9) | 2.2 1.5-3.85 | 2.4 1.2-4.8 | <0.001** |
| therapy | No | 34 (16) | 69 (43) | |||
P<0.05—significant*, P<0.001—highly significant**
Table 5 Interaction analysis of factors associated with oxygen therapy knowledge
Table 5.
Interaction analysis of factors associated with oxygen therapy knowledge
| Variable | Adjusted OR | 95% CI | P |
|---|---|---|---|
| Gender (male vs female) | 1.7 | 1.2 to 2.5 | 0.01* |
| Experience (>5 yrs vs ≤5 yrs) | 1.3 | 0.9 to 2.1 | 0.15 |
| Department (clinical vs nonclinical) | 1.5 | 1.0 to 2.2 | 0.05 |
| Familiarity with devices (yes vs no) | 2.1 | 1.5 to 3.0 | <0.001** |
| Workload perception (yes vs no) | 1.8 | 1.2 to 2.8 | 0.01* |
| Gender x experience | 3.1 | 1.8 to 5.4 | <0.001** |
| Department x familiarity | 0.9 | 0.5 to 1.5 | 0.65 |
| Experience x workload | 1.3 | 0.7 to 2.3 | 0.42 |
P<0.05—significant*, P<0.001—highly significant **
The regression analysis identifies multiple factors independently predictive of oxygen therapy knowledge, including gender, experience, department type, device familiarity, and workload perception.
An interaction term between gender and experience reveals that the knowledge gap between males and females gets amplified with increasing experience (OR 3.1 for interaction term)—suggesting experienced male providers incrementally surpass their female counterparts.
However, interaction terms for departments with device familiarity and experience with workload were not statistically significant—implying their associations with knowledge were likely independent without synergism between terms.
Table 6 Linear regression model of factors predicting attitude score
Table 6.
Linear regression model for factors predicting oxygen therapy attitude score
| Variable | Coeff. | 95% CI | P |
|---|---|---|---|
| Gender (male) | 1.7 | 0.9 to 2.5 | <0.001** |
| Experience (>5 yrs) | 1.2 | 0.6 to 1.9 | <0.001** |
| Department (clinical) | 0.8 | 0.2 to 1.4 | 0.01* |
| Workload perception | 2.3 | 1.8 to 2.9 | <0.001** |
| Familiarity with devices | 1.5 | 1.0 to 2.1 | <0.001** |
| Age (>25 yrs) | 0.9 | 0.4 to 1.5 | 0.002* |
| Experience x workload | 0.4 | -0.2 to 1.1 | 0.19 |
| Familiarity x department | 0.3 | -0.4 to 1.1 | 0.39 |
P<0.05—significant *,P<0.001—highly significant **
Several factors demonstrate independent positive associations with higher attitude scores, including male gender, clinical department, longer experience, device familiarity, higher workload perception, and older age.
The magnitude of effects is provided through the coefficient values—such males have scored 1.7 units higher on average, and those perceiving workloads have 2.3 units higher attitudes, indicating a larger effect size.
However, the experience workload interaction term is not significant, suggesting their influences on oxygen therapy attitudes are independent and additive, rather than synergistic.
Similarly, the interaction between department and familiarity with oxygen devices lacks significance—their associations with attitude scores are likely independent without noteworthy modifying effects on each other.
In summary, these expanded regression models with interaction terms provide additional confirmation of factors predicting knowledge and attitudes, some showing potential effect modification, while others demonstrate independent relationships.
Table 7 categorizes the themes, subthemes, and participant phrases systematically, offering a clear view of the qualitative data captured in the study.
Table 7.
Qualitative findings of the study
| Theme | Subtheme | Participant phrases |
|---|---|---|
| Perceived barriers to effective oxygen therapy | Inadequate training | “I don’t think we received enough hands-on training on operating oxygen devices and titrating flow rates.” “There should be periodic refreshers on guidelines because it’s easy to forget details.” |
| High workload and time constraints | “With the high patient load, it becomes difficult to spend adequate time titrating oxygen levels and deciding on the best delivery method.” “I sometimes feel rushed to move on to the next patient even if the current patient’s oxygen needs have not been fully addressed.” | |
| Suggestions for improvement | Enhanced educational opportunities | “Maybe having simulations and exercises would help cement knowledge on oxygen therapy.” “Continuing education credits for oxygen therapy updates would probably improve compliance.” |
| Protocol implementation | “Following standardized protocols on oxygen therapy may help reduce errors.” “Defaults based on best practices could help when there isn’t enough time to make fully informed custom decisions.” | |
| Attitudes and perceptions | Viewing oxygen therapy as less critical | “Oxygen administration does not seem as high a priority as some other resuscitative measures.” “I think some providers don’t fully appreciate the impacts of even transient hypoxia.” |
| Lack of self-efficacy | “I don’t feel very confident in my ability to detect subtle signs of hypoxemia.” “Choosing oxygen devices and titrating flow rates takes some experience.” | |
| Clinical inertia and deviations from guidelines | Tendency to continue previous prescriptions rather than titrating | “I often just renew what the previous provider has ordered if the patient seems stable.” “It takes effort to wean high oxygen flows down if the patient improved.” |
| Deviating from recommendations | “The guidelines don’t always align with specific clinical scenarios.” “I use workarounds that I think will work even if not following best practices.” | |
| Potential solutions and mitigation strategies | Tackling knowledge gaps | “Online training videos can standardize baseline knowledge for everybody.” “Flowcharts on protocols in break rooms remind us of best practices.” |
| Streamlining workflows | “Integrating alerts and decision tools into EMR can facilitate following guidelines.” “Standard order sets help remove redundant decision points.” |
Discussion
The key findings from the convergent quantitative and qualitative results provide vital insights into existing gaps and influential factors affecting optimal oxygen therapy delivery by front-line resident doctors in this teaching hospital. Consistent with prior reports,[9] the significant knowledge deficiencies demonstrate the need for reevaluating current training mechanisms and designing refreshers tailored to identified concept gaps regarding the dangers of hypoxemia-hyperoxemia, device specifications, and titration protocols. The concerning statistics on self-reported inappropriate attitudes and compliance additionally underscore the need for practice monitoring safeguards.[10]
In this study, around 78% had a good level of knowledge, which is greater than the reports of the South Gondar Zone Hospital (68.7%),[11] Addis Ababa, Ethiopia (36.2%),[8] and Debre Tabor General Hospital, Ethiopia (52%).[12] The discrepancy in these reports might be due to differences in study participants, study settings, and samples.
In our study, 47.8% of participants were evaluated as having a good level of practice. This finding was greater than the reports of studies conducted in Debre Tabor, Ethiopia (33%),[12] and Addis Ababa (43.4%).[8] This variation can be explained by different contributing factors, such as differences in study participants, sample size, and study period.
Another factor that has an association with practice level is the expected workload. In agreement with this finding, a study conducted in Riyadh explained that getting training, adequate supply of devices, and the workload were associated with the practice level of participants[13]
Regarding the attitude level of the current study, 61.7% of participants have a positive level of attitude toward oxygen therapy. These findings are more consistent with reports from the study performed in Addis Ababa (53.3%).[8] Participants with a poor level of knowledge are more likely to have a negative attitude toward oxygen therapy (AOR-5.610, 95% CI (3.365–9.351)).
The qualitative themes substantiate that beyond standalone knowledge limitations, ingrained workplace cultural views tend to discourage due diligence for optimal titration. The described tendencies for clinical inertia, along with insufficient appraisal of transient hypoxemia harms, demonstrate the need for protocols nudging proactive evidence implementation. Integrating cognitive aids within workflows through intradisciplinary partnerships can facilitate sustained guideline adherence as elaborated for sepsis management.[14]
Limitations
Being a single-center study, the findings may have limited generalizability. The knowledge and practice measures rely on self-reports, which can overestimate actual skills. Structured observations were not feasible, though iterative interviews allowed some verification of described behaviors.
Conclusion
In conclusion, the explanatory mixed-methods approach identified specific evidence-practice gaps among resident doctors regarding knowledge, attitudes, prescription practices, and influencing factors affecting optimal oxygen therapy. The qualitative insights provide contextual clarity on barriers amenable to tailored quality improvements for enhancing patient safety.
Recommendations: The following context-specific recommendations are proposed for strengthening oxygen therapy delivery based on study findings:
Competency mapping to standardized thresholds during intensive pulmonology postings
Streamlined electronic health record (EMR) order sets guiding appropriate device selection and weaning provisions
Enablement workshops for self-efficacy in the prescriber and nursing teams
Departmental pulse oximetry audits and constructive feedback processes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors express their heartfelt gratitude to the Head of the Department of Community Medicine, as well as the study participants.
References
- 1.Brown SM, Grissom CK, Moss M, Rice TW, Schoenfeld D, Hou PC, et al. Nonlinear imputation of PaO2/FIO2 from SpO2/FIO2 among patients with acute respiratory distress syndrome. Chest. 2018;153:1011–8. doi: 10.1016/j.chest.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Damiani E, Adrario E, Girardis M, Romano R, Pelaia P, Singer M, et al. Arterial hyperoxia and mortality in critically ill patients: A systematic review and meta-analysis. Crit Care. 2018;22:1–11. doi: 10.1186/s13054-014-0711-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Oxygen therapy in acute healthcare facilities: A point prevalence audit and survey of prescribing practice in Tasmania, Australia. BMC Health Serv Res. 2021;21:1–12. [Google Scholar]
- 4.Tiruvoipati R, Lewis D, Haji K, Botha J. High-flow nasal oxygen vs high-flow face mask: A randomized crossover trial in extubated patients. J Crit Care. 2017;40:63–8. doi: 10.1016/j.jcrc.2009.06.050. [DOI] [PubMed] [Google Scholar]
- 5.Chatterjee R, Kundu R, Ghosh M, Majumdar KK, Panchabhai TS, Shah D, et al. Barriers to proper oxygenation in intensive care units in India: Formative research for designing context-specific strategies. J Patient Saf. 2017;13:225–30. [Google Scholar]
- 6.Hampson T. and McKinley J. Problems posing as solutions: criticizing pragmatism as a paradigm for mixed research. Research in Education. 2023;116(1):124–138. https://doi.org/10.1177/00345237231160085. [Google Scholar]
- 7.Irwin K, Panniers T, Ponseca A. Mixed methods: The drive towards evidence-based solutions through complex interventions. J Mixed Methods Res. 2021;16:226–38. [Google Scholar]
- 8.Lemma G. Assessment of nurse’s knowledge, attitude, and practice about oxygen therapy at emergency departments of one federal and three regional hospitals in Addis Ababa [master’s thesis] Ethiopia: Addis Ababa University. 2015 [Google Scholar]
- 9.Severinghaus JW, Astrup PB. History of blood gas analysis. IV. Leland Clark’s oxygen electrode. J Clin Monit. 1986;2:125–39. doi: 10.1007/BF01637680. [DOI] [PubMed] [Google Scholar]
- 10.Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: The oxygen-ICU randomized clinical trial. JAMA. 2016;316:1583–9. doi: 10.1001/jama.2016.11993. [DOI] [PubMed] [Google Scholar]
- 11.Demilew BC, Mekonen A, Aemro A, Sewnet N, Hailu BA. Knowledge, attitude, and practice of health professionals for oxygen therapy working in South Gondar zone hospitals, 2021: A multicenter cross-sectional study. BMC Health Serv Res. 2022;22:600. doi: 10.1186/s12913-022-08011-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeleke S, Kefale D. Nurses’ supplemental oxygen therapy knowledge and practice in Debre Tabor general hospital: A cross-sectional study. Open Access Emerg Med. 2021;13:51. doi: 10.2147/OAEM.S299139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aloushan AF, Almoaiqel FA, Alghamdi RN, Alnahari FI, Aldosari AF, Masud N, et al. Assessment of knowledge, attitude, and practice regarding oxygen therapy at emergency departments in Riyadh in 2017: A cross-sectional study. World J Emerg Med. 2019;10:88. doi: 10.5847/wjem.j.1920-8642.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kleinpell RM. Promoting early identification of sepsis in hospitalized patients with nurse-led protocols. Crit Care. 2017;21:1–3. doi: 10.1186/s13054-016-1590-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


