Abstract
Background
Nigeria is an epicenter for Lassa fever. Ebonyi state is located in the South-Eastern region of Nigeria where a high burden of Lassa fever has been reported. Therefore, this study was designed to assess the epidemiology of Lassa fever, its seasonality, trend, and mortality predictors in Ebonyi state, South-East, Nigeria.
Method
We analyzed data extracted from Ebonyi State Integrated Disease Surveillance and Response (IDSR) system over five years (2018–2022). A total of 1578 reported Lassa fever cases were captured in the IDSR out of which 300 were laboratory-confirmed. Data were analyzed using descriptive statistics, additive time series model, quadratic equation, and logistic regression model (α0.05). Spatial distribution of reported Lassa fever cases was conducted using Arc G.I.S.
Results
The mean age of the individuals with the reported cases of Lassa fever was 29.4 ± 17.8 years. Lassa fever showed a seasonal trend across the years. The quadratic model provided the best fit for predicting Lassa fever cumulative cases (R2 = 98.4%, P-value < 0.05). Projected cases of Lassa fever for the year 2023 were 123 in the 1st quarter, 23 in the 2nd quarter, 42 in the 3rd quarter, and 17 in the 4th quarter. The seasonality index was + 70.76, -28.42, -9.09, and -33.2 in the 1st, 2nd, 3rd, and 4th quarters respectively. The reported cases of Lassa fever followed a declining trend (slope = -0.1363). Farmers were 70% less likely to die from Lassa fever compared to those not working (aOR:0.3, CI: 0.17–0.83). The hot spots for Lassa fever were Abakaliki and Ezza Local Government Areas.
Conclusion
Although the reported Lassa fever cases followed a declining trend in Ebonyi state, there was a seasonality in the disease pattern. Being a farmer was protective against the risk of dying from Lassa fever. While efforts to eliminate and mitigate the spread of the disease in Ebonyi state should be strengthened, more attention should target the peak period of the disease.
Keywords: Lassa fever, Time series analysis, Seasonality, Ebonyi State
Background
Lassa fever (LF) is a viral hemorrhagic fever and an acute infectious zoonotic disease endemic in West Africa and the stability of its virus occurs when the relative humidity in the atmosphere decreases [18]. The disease usually presents with mild symptoms such as fever, bleeding gum, vomiting, and chest pain [25]. About 80% with clinical manifestation of Lassa virus have no symptoms, but 1 in 5 infections result in severe disease [35]. The Lassa virus is transmitted to humans by handling infected rats or through foods/household items contaminated by infected rats’ urine and feces. Person-to-person infections and laboratory transmission can also occur, particularly in healthcare settings in the absence of adequate infection prevention and control measures [35]. The morbidity and mortality associated with Lassa fever is high particularly if the disease is not early detected for necessary treatment. Ebonyi state is located in the South-Eastern region of Nigeria where a high burden of Lassa fever has been reported. Therefore, realizing goal 3 of the Sustainable Development Goals (SDGs) might be unrealizable in Ebonyi state if appropriate preventive and control interventions are not instituted.
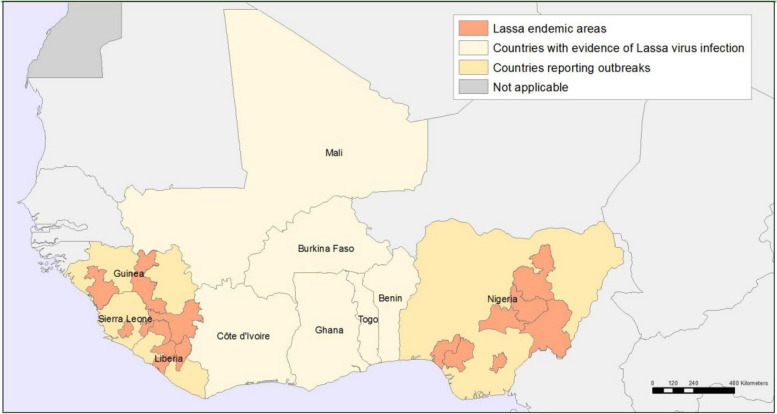
According to World Health Organization, Lassa fever is endemic in West African countries like Benin, Côte d’Ivoire, Ghana, Guinea, Liberia, Mali, Nigeria, Sierra Leone and Togo (Fig. 1). In this African sub-region, 58 million population are at risk of the disease, with cases ranging from 100,000 to 300,000 and estimated deaths being 5,000 each year [35]. Lassa fever accounts for 6.0% of fevers, 0.7% of hospital admissions, 40% of Case Fatality Rate (CFR), and almost a quarter of maternal mortality during its peak in West Africa [12]. There is also evidence of 80–95% fetal and neonatal death, with children experiencing lower attack rates than adults [21]. The actual incidence rate of Lassa fever in Nigeria is unknown, but its seroprevalence is around 21%, and its CFR ranges from 3.0% to 42.0% and it remained consistently between 20 and 25% in the last two years [10, 11].
Fig. 1.
Geographic distribution of Lassa fever in West Africa. Source: http://www.who.int/emergencies/diseases/lassa-fever/geographic-distribution
Lassa fever outbreak can occur at any time in a year but its transmission is often at its peak during the dry season due to varying interactions between humans and rodents during this period [30]. Research has shown that increased temperatures tend to increase the number of Lassa fever incidences [18], while rainfall has a detrimental impact on Lassa virus transmissibility. The dry season in Nigeria is a notable period for the migration of rodents into homes due to bush burning, thereby, facilitating their contact with food materials like grains, rice, and beans [4]. It has also been established that poor housing conditions can provide a favorable environment for rodents to thrive and thus promote their ability to infect humans through interaction with their feeding items [8]. Environmental factors such as sanitation, overcrowding, deforestation, hunting of rodents, and bush burning provide conducive environments for the spread of the Lassa fever virus in endemic communities. Living in open spaces typical of a village and urban slum setting brings about the rodents' close contact with humans and food materials [4]. Socioeconomic conditions and cultural beliefs that are the principal causes of delays in seeking healthcare or lack of access to healthcare services by infected individuals are challenges to mitigating the spread of Lassa fever in Ebonyi state. In addition, the lack of Lassa fever testing capacity and ignorance of the disease infection prevention and control practices by many health facilities contribute to its spread in Ebonyi state [3]. Research has established that health conditions like HIV, TB, and Cancer predisposed individuals with higher risks of Lassa fever infection [5].
The Nigeria Centre for Disease Control (NCDC) has documented yearly incidences of Lassa fever in different states with Ebonyi state having the highest annual increase [22]. Several studies have reported trend analysis of Lassa fever with a specific study focused on the epidemiological pattern in Nigeria from 2015 – 2021, revealing a notable decline during the annual peak seasons, particularly from weeks 1 to 13, with a significant 75% reduction in incidence observed between 2020 and 2021 [26]. Another study reported spatial clustering of Lassa fever between 2017 and 2021 with an increasing trend followed by a decline in 2021 [9] and Statistical and mathematical models have been used in studies to describe the trend of Lassa fever in Nigeria [6, 7, 20]. However, these studies were in most situations conducted at the national level with very few in Ebonyi state. Examining seasonality and using mathematical models to predict the cases of Lassa fever remain a grey research area in Ebonyi state. Forecasting model has been used to mitigate the spread of infectious disease like Ebola, COVID-19, Cholera, and Measles [23]. However, literature is scarce on its utilization for Lassa fever. Therefore, the formulated forecasting model in the current study will be suitable to fight against Lassa fever in Ebonyi state and could be adapted in the fight against the disease in other settings.
The current study was conceptualized and implemented against the backdrop of limited research on Lassa fever in Ebonyi state being a high-risk state for the disease in Nigeria. The outcome of the study will provide valuable insight for the establishment of early warning mechanisms capable of identifying potential outbreaks. Additionally, this will facilitate the optimal allocation of resources for the prevention and control of the disease, particularly in high-risk areas in Ebonyi state. The specific objectives of the study are to describe the epidemiology of Lassa fever in Ebonyi state by person, place, and time and to examine the factors associated with Lassa fever mortality in Ebonyi state. It also examined the trend and identified the model of best fit for predicting the future occurrence of Lassa fever cases in the state.
Methods
Study area
The study was carried out in Ebonyi state, South East, Nigeria. The 2023 projected population of the state using the 2006 housing and population census figure as the base year was 3,027,452 (View of the researchers)The people living in the state are mostly agrarian and the majority live in rural areas. The most common vegetation in the state is tree shrubs and its vegetation is a mixture of savannah and semi-tropical forest. There are thirteen Local Government Areas (LGAs) in the state namely, Abakaliki Afikpo North, Afikpo South, Ebonyi, Ezza North, Ezza South, Ikwo, Ishielu, Ivo, Izzi, Ohaozara, Ohaukwu, and Onicha. The state has thirteen general hospitals, six mission hospitals, 417 primary healthcare centers, and 119 private hospitals/clinics [33]. There is a Lassa fever virology treatment centre in Ebonyi state situated in Alex Ekwueme Federal University Teaching Hospital, Abakaliki. Ebonyi state has a humid tropical climate and the dry season is usually between December and January.
Disease surveillance system in Nigeria
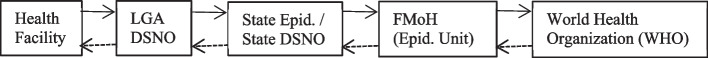
Integrated Disease Surveillance and Response (IDSR) aimed to promote coherent use of resources by integrating and streamlining common disease surveillance activities. Nigeria began efforts towards implementing the IDSR strategy in June 2000 after its adoption by the World Health Organization (WHO), at present, all 36 states in Nigeria and the Federal Capital Territory are currently implementing IDSR [16]. The Nigeria IDSR strategy articulates the available resources to collect data on notifiable diseases from a single focal point at each level (Community, health facilities, LGA, State, and Federal) (Federal Ministry of Health, 2009). The LGA level is the main focus of the IDSR system in Nigeria because it is the first level in the Nigerian health system. The information flow in the Nigerian IDSR system is from the health facility to the LGA using IDSR reporting forms. The LGA collates and forwards the data to the State Ministry of Health (SMoH), which also collates and forwards the data to the Epidemiology Division of the Federal Ministry of Health (FMoH). However, at LGA and state levels, analysis and feedback to health facilities are executed as shown in Fig. 2 (Federal Ministry of Health, 2009). The data for this study were accessed at the state level. The Federal Ministry of Health (FMoH) has listed 40 communicable and non-communicable diseases and public health-related conditions which were grouped into three categories; epidemic-prone diseases, diseases targeted for eradication and elimination, and other diseases of public health importance for the IDSR system in Nigeria. The selection was based on the following criteria; the main cause of high morbidity and mortality in the country, epidemic potential, surveillance required internationally, availability of effective control and preventive intervention for addressing the public health problem they pose, which could be easily identified using simple case definition and have intervention programmes supported by the WHO for prevention and control, eradication or elimination of the diseases (Federal Ministry of Health, 2009).
Fig. 2.
Flow of Integrated Disease Surveillance and Response (IDSR) data in Nigeria. Source: National technical guidelines for integrated diseases surveillance and response, Nigeria
During the 2014–2015 Ebola outbreak in West Africa, the Surveillance Outbreak Response Management and Analysis System (SORMAS) was developed (SORMAS Flyer). Since then, SORMAS has expanded to accommodate other diseases including monkeypox, Lassa fever, and COVID-19. This digital early warning and disease management system platform receives inputs from those involved in surveillance and presents this data to users throughout the health system to drive a comprehensive strategy and response [17]. The IDSR system in Nigeria partly runs on the Surveillance Outbreak Reporting Management and Analysis System (SORMAS) platform, especially for immediately notifiable or epidemic-prone diseases like Lassa fever. Ebonyi state surveillance reporting system flows from the communities to the health facilities (private and public). From the Health facility to the Local government area comprising the Head of Health, the Disease surveillance Notification officer (DSNO), and then the State epidemiologist.
Study design and data source
Cross-sectional and analytical designs were used for the study. Secondary data analysis was conducted based on the Lassa fever data extracted from the Ebonyi State Integrated Disease Surveillance and Response (IDSR) database which is usually updated daily from 2018 – 2022.
Data analysis and management
Relevant variables were sorted, extracted, and cleaned using Statistical Package for the Social Sciences (SPSS) version 21.0 and Microsoft Excel. These included age, sex, location, LGAs, date of onset of the disease, laboratory results, and outcome. Data were analysed using STATA version 16. Frequencies and proportions were used to summarize the data, while Chi-square analysis was used to examine the association between the disease outcome and the explanatory variables. The factors influencing Lassa fever mortality were examined using the logistic regression model (α0.05).
The trajectory of the reported cases of Lassa fever was assessed using a time series model to ascertain whether there is seasonality in the occurrence of the disease or not. The Lassa fever’s data for 2018, 2019, 2020, 2021, and 2022 were aggregated in 3 months reflecting the quarters in a year as 1st quarter (January to March), 2nd quarter (April- June), 3rd quarter (July – September), 4th quarter (October – December). The data was decomposed and the quarterly estimates were used to describe the trend. This was done by computing the 3-quarter moving average to eliminate seasonal and irregular variations from the data. The number of cases in a quarter was represented by and the trendline was obtained using the simple average method.
| 1 |
To obtain the seasonal variation (SV) in the data, the additive model was used based on the pattern exhibited by the observed reported Lassa fever cases () and is given by:
| 2 |
The additive model was decomposed because the parameters describing the time series are not changing over time which is the case for the additive model applied to the data. This is with the view to separating the time series into several factors: trend, seasonal, cyclical, and irregular variations. This parameter describing the series does not change over time with the assumption that the variation in the trend is constant over some time and as such, the plot of the smoothed data for each year follows an additive time series model.
The model is as follows:
| 3 |
Yt is the observed quarterly Lassa fever data in time t, Tt = the trend component in time t: St = the seasonal component in time t, and Ct is the cyclical component in time t. Tt is the irregular variation in time t. The quarterly pattern of the smoothed Lassa fever cases in each year showed no indication of C and Yt. Therefore, = 0 and Y = 0. Equation (3) is then transformed to . The smoothed monthly reported cases of Lassa fever () was aggregated for each quarter of the year. A 3-point moving average method was used to determine the trend line for the quarterly data by eliminating the irregular fluctuations from the data. The trend line was deseasonalized using , which was used to generate the seasonal index.
| 4 |
| 5 |
| 6 |
Year i = 1,2,3,4: Quarter j = 1, 2,3 4.
Where L is the number of years where the St is available, and r is 4, the number of quarters in a year. The adjusted seasonal index (ASI) was used to assess the seasonality of Lassa fever each year. A quarter with a higher ASI is expected to experience a higher number of cases of Lassa fever.
The model of best fit among the mathematical models (Linear, Logarithmic, Inverse, Quadratic, Cubic, Compound, Power, S, Growth, Exponential, and Logistics) was assessed for the prediction of Lassa fever cases in Ebonyi State. Among these mathematical equations, the quadratic model was adjudged as the model of best fit for predicting the reported cases of Lassa fever in Ebonyi state. The quadratic model describes a relationship between a dependent variable (y) and an independent variable (x) in which the dependent variable behavior is characterized by a quadratic Eq. (7):
| 7 |
where; a, b, and c are the coefficients that determine the shape and position of the equation and represents the random error in the model.
The quadratic model was built on the assumption that the relationship between the dependent (y) and independent variable (x) follows a quadratic pattern, that is, characterized by a parabolic curve. As with linear and exponential models, it is assumed that the errors () are independent of each other. Each data point’s error should not be influenced by the errors of other data points. The variance of the errors should be constant across all levels of the independent variable (x). The spread of the residuals (differences between observed and predicted values) should be roughly the same for all values of x. Quadratic models may not fit perfectly to all datasets but the assumption that can be accurately represented by a quadratic function can be assessed through the model evaluation technique.
Ethical approval
Ethical approval for the permission to use the surveillance data was received from Ebonyi State Ministry of Health (EBSHREC/01/04/2022–02/04/2024). Confidentiality of the data was maintained.
Results
Table 1 shows the association between the socio-demographic characteristics of reported Lassa fever cases and survival status. Among the deceased Lassa fever cases, an observed fluctuation over the five years was reported. There was an increase in the percentage of deaths from 18.5% in the year 2018 to 40.8% in the year 2019. Notable fluctuations were observed over the subsequent years.
Table 1.
Percentage distribution of Lassa fever cases according to survival status by background characteristics in Ebonyi State, 2018–2022
| Variables | Outcome | - value | p-value | |
|---|---|---|---|---|
| Dead | Alive | |||
| Sex | ||||
| Male | 34.2 (50) | 65.7 (96) | 0.272 | 0.602 |
| Female | 31.3 (41) | 68.7 (90) | ||
| Age group | ||||
| 0–4 | 42.8 (3) | 57.1 (4) | 7.829 | 0.166 |
| 5–14 | 50.0 (7) | 50.0 (7) | ||
| 15–24 | 21.0 (8) | 78.9 (30) | ||
| 25–34 | 25.0 (11) | 75.0(34) | ||
| 35–49 | 30.9 (22) | 69.0 (49) | ||
| 50 + | 39.9 (39) | 60.6 (60) | ||
| Occupation | ||||
| Not working | 27.1 (25) | 72.8 (67) | 7.061 | 0.133 |
| Business | 42.8 (18) | 57.1 (24) | ||
| Farmer | 45.6 (21) | 54.3 (25) | ||
| Healthcare worker | 25.0 (5) | 75.0 (15) | ||
| Others | 31. (14) | 68.8 (31) | ||
| Years | ||||
| 2018 | 18.5 (13) | 81.4 (57) | 13.598 | 0.009** |
| 2019 | 40.8 (20) | 59.1 (29) | ||
| 2020 | 29.5 (26) | 70.4 (62) | ||
| 2021 | 47.3 (9) | 52.6 (10) | ||
| 2022 | 45.1(23) | 54.9 (28) | ||
| Senatorial District | ||||
| Ebonyi South | 26.6 (4) | 73.3 (11) | 3.209 | 0.360 |
| Ebonyi Central | 41.2(26) | 58.7 (37) | ||
| Ebonyi North | 30.2 (60) | 69.7 (134) | ||
**p < 0.01
Table 2 shows the binary logistic regression of factors associated with mortality due to Lassa fever in Ebonyi State, 2018 – 2022. Farmers were 70% less likely to die from Lassa fever compared to the unemployed (aOR:0.3, CI: 0.17—0.83). Additionally, there was an 80% reduction in death of Lassa fever cases in 2019 (aOR: 0.2, CI: (0.11- 0.72, p = 0.008), 2021(aOR: 0.2, CI: 0.09—0.92) and 2022 (aOR 0.2, CI: 0.11—0.74) compared to year 2018.
Table 2.
Binary logistic regression of factors associated with Lassa fever-related mortality in Ebonyi State, 2018 - 2022
| uOR(95% C.I) | p-value | aOR(95% C.I) | p-value | |
|---|---|---|---|---|
| Sex | ||||
| Female | 1.0 | |||
| Male | 0.8(0.51-1.40) | 0.522 | ||
| Age group | ||||
| 0-4 | 1.0 | |||
| 5-14 | 0.7(0.12-4.66) | 0.758 | ||
| 15-24 | 2.8(0.52-15.21) | 0.230 | ||
| 25-34 | 2.3(0.44-11.99) | 0.316 | ||
| 35-49 | 1.5(0.33-7.73) | 0.560 | ||
| 50+ | 1.1(0.29-5.95) | 0.882 | ||
| Occupation | ||||
| Not working | 1.0 | 1.0 | ||
| Business | 0.4(0.22-1.00) | 0.052 | 0.6(0.27-1.41) | 0.261 |
| Farmer | 0.4(0.20-0.88)*** | 0.022 | 0.3(0.17-0.83) *** | 0.017 |
| Healthcare worker | 1.1(0.36-3.40) | 0.842 | 1.1(0.36-3.75) | 0.788 |
| Others | 0.8(0.39-1.85) | 0.689 | 0.7(0.34-1.76) | 0.553 |
| Year | ||||
| 2018 | 1.0 | 1.0 | ||
| 2019 | 0.2(0.27-1.28) ** | 0.003 | 0.2(0.11-0.72) ** | 0.008 |
| 2020 | 0.5(0.27-1.28) | 0.185 | 0.6(0.24-1.47) | 0.267 |
| 2021 | 0.2(0.86-0.70) ** | 0.009 | 0.2(0.09-0.92) *** | 0.036 |
| 2022 | 0.2(0.11-0.56) ** | 0.001 | 0.2(0.11-0.74) *** | 0.010 |
| Senatorial District | ||||
| Ebonyi South | 1.0 | |||
| Ebonyi Central | 0.5(0.16-2.12) | 0.471 | ||
| Ebonyi North | 0.9(0.28-3.20) | 0.270 | ||
*p<0.001; **p <0.01; ***p <0.05
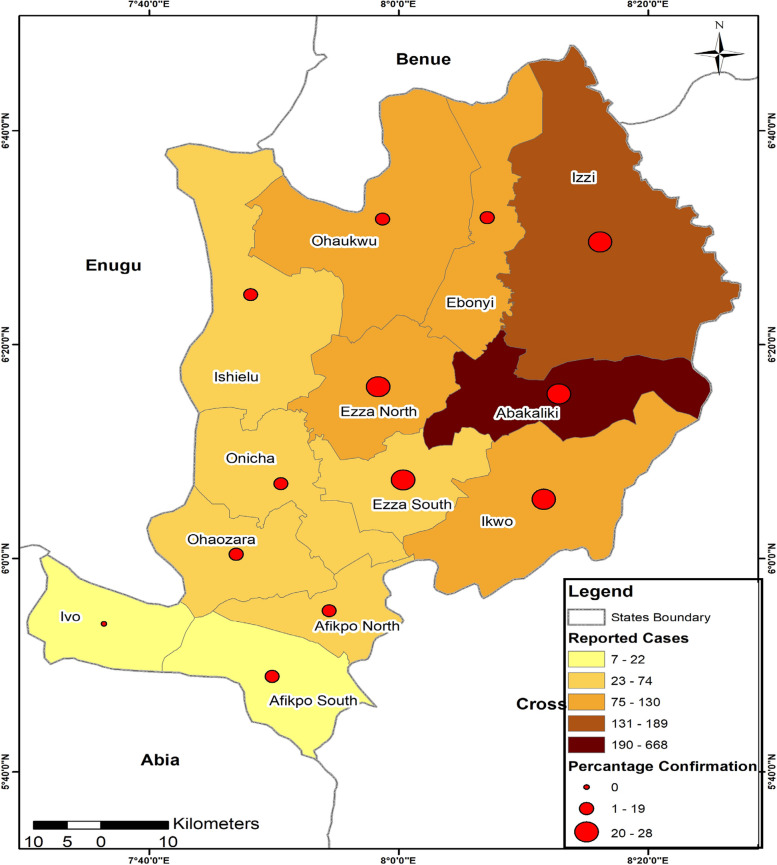
Figure 3 represents the geographical distribution of reported and confirmed Lassa fever cases by local government areas in Ebonyi State, 2018 – 2022. The trend indicates variations in the reported and confirmed cases across the LGAs. Abakaliki LGA reports the highest number of reported LF cases (668), while Ivo LGA represents the lowest (7). Ezza North and Ezza South show similar percentages of Lassa fever confirmed cases (28%).
Fig. 3.
Geographical Distribution of Reported and Confirmed Lassa Fever Cases by Local Government Areas in Ebonyi State, 2018 – 2022
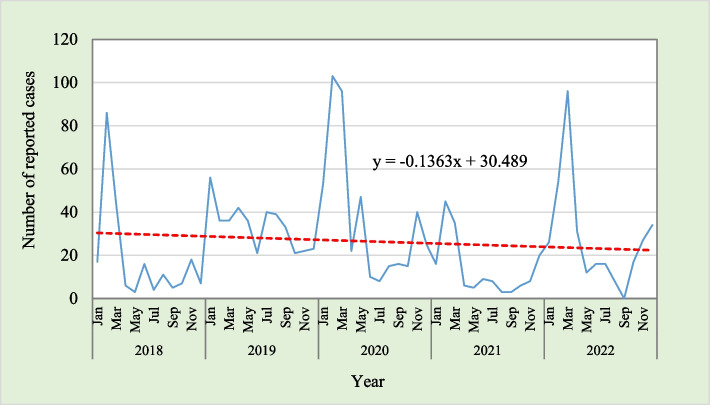
The data as presented in Fig. 4 shows the monthly number and trend line of reported cases of Lassa-fever over 5 years, 2018–2022. A declining trend in the number of reported cases of Lassa fever was observed over the years with the rate of decrease being, β = -0.1363. The data also revealed that 1.01% of the variation in the Lassa-fever data can be accounted for by time.
Fig. 4.
Monthly Number and Trend Line of Reported Cases of Lassa-Fever in Ebonyi State, 2018 – 2022
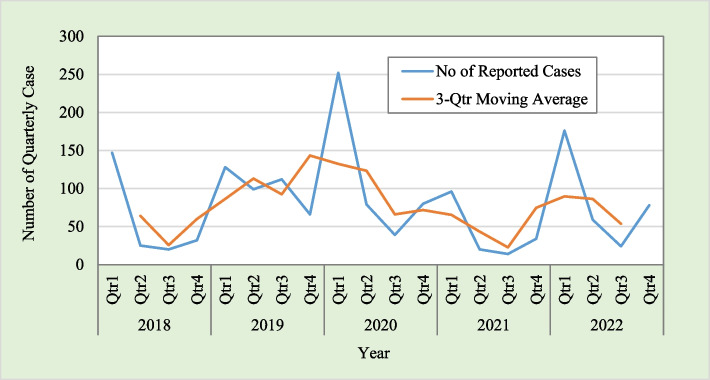
The quarterly number and 3-quarter moving average of reported cases of Lassa-Fever from 2018 to 2022 are depicted in Fig. 5. The data revealed seasonal patterns in the quarterly reported number of cases of Lassa-Fever and showed evidence of a higher number of cases in a particular period of the year across the years under investigation.
Fig. 5.
Quarterly number and 3-Quarter Moving Average of Reported Cases of Lassa-Fever in Ebonyi State, 2018 – 2022
The data presented in Table 3 represents the quarterly number of Lassa-Fever reported cases and the trend obtained through the moving average method. The seasonal variation was obtained as a difference between the number of cases per quarter and the three-quarter moving averages.
Table 3.
Quarterly number, 3—quarter moving average, and seasonal variation of reported cases of Lassa Fever in Ebonyi State, 2018—2022
| Year | Quarter | No of Reported Cases | 3-Qtr Moving Average | SV = Y-TL |
|---|---|---|---|---|
| 2018 | Qtr1 | 147 | - | - |
| Qtr2 | 25 | 64.00 | -39.00 | |
| Qtr3 | 20 | 25.67 | -5.67 | |
| Qtr4 | 32 | 60.00 | -28.00 | |
| 2019 | Qtr1 | 128 | 86.33 | 41.67 |
| Qtr2 | 99 | 113.00 | -14.00 | |
| Qtr3 | 112 | 92.33 | 19.67 | |
| Qtr4 | 66 | 143.33 | -77.33 | |
| 2020 | Qtr1 | 252 | 132.33 | 119.67 |
| Qtr2 | 79 | 123.33 | -44.33 | |
| Qtr3 | 39 | 66.00 | -27.00 | |
| Qtr4 | 80 | 71.67 | 8.33 | |
| 2021 | Qtr1 | 96 | 65.33 | 30.67 |
| Qtr2 | 20 | 43.33 | -23.33 | |
| Qtr3 | 14 | 22.67 | -8.67 | |
| Qtr4 | 34 | 74.67 | -40.67 | |
| 2022 | Qtr1 | 176 | 89.67 | 86.33 |
| Qtr2 | 59 | 86.33 | -27.33 | |
| Qtr3 | 24 | 53.67 | -29.67 | |
| Qtr4 | 78 | - | - |
The computational procedures for the adjusted seasonal variation of the reported cases of Lassa fever in Ebonyi state are presented in Table 4. The adjusted seasonal index was highest in quarter 1 (+ 70.6), followed by quarter 3 (-9.09), then quarter 2 (-28.42), and quarter 4 (-33.24) in that order.
Table 4.
Adjusted seasonal variation of reported cases of Lassa fever in Ebonyi State, 2018—2022
| Quarter | ||||
|---|---|---|---|---|
| Year | 1 | 2 | 3 | 4 |
| 2018 | -39.00 | -5.67 | -28.00 | |
| 2019 | 41.67 | -14.00 | 19.67 | -77.33 |
| 2020 | 119.67 | -44.33 | -27.00 | 8.33 |
| 2021 | 30.67 | -23.33 | -8.67 | -40.67 |
| 2022 | 86.33 | -27.33 | -29.67 | |
| Average | 69.58 | -29.60 | -10.27 | -34.42 |
| Adjt. Factor | 1.18 | 1.18 | 1.18 | 1.18 |
| Adj.SVI | 70.76 | -28.42 | -9.09 | -33.24 |
Adjt. Adjustment, Adj.SVI Adjusted Seasonal Variation Index
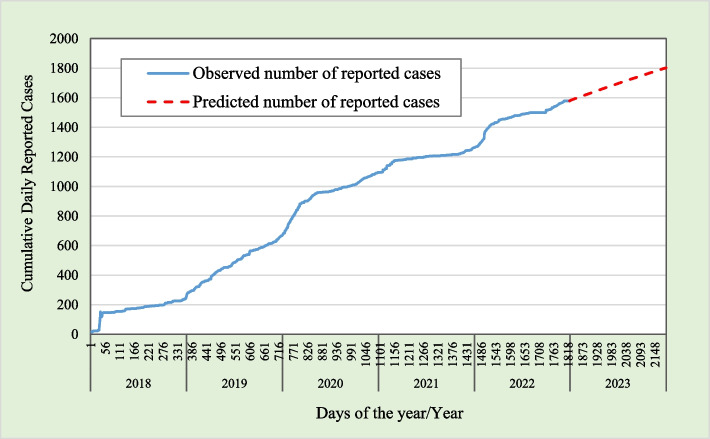
Figure 6 represents reported Lassa fever observed and fitted cumulative cases in Ebonyi state, 2018–2022 which includes all the models selected for comparison in the study. They include Linear model, Logarithmic model, Inverse model, Quadratic model, cubic model, Compound model, Power model, S model, Growth model, Exponential model, and Logistic model. Among all the selected models, only the Linear model with (R2 = 97%, p-value < 0.05), the Quadratic model (R2 = 98.2%, p-value < 0.05), and the Cubic model (R2 = 98.5%, p-value < 0.05) reported high R2. Among the three models, the Cubic model had the best fit but the cumulative Lassa fever cases show a projection with a sinusoidal curve, which is not appropriate. Therefore, a quadratic model (R2 = 98.2%, P-value < 0.05) was chosen as the best for the Lassa fever data.
Fig. 6.
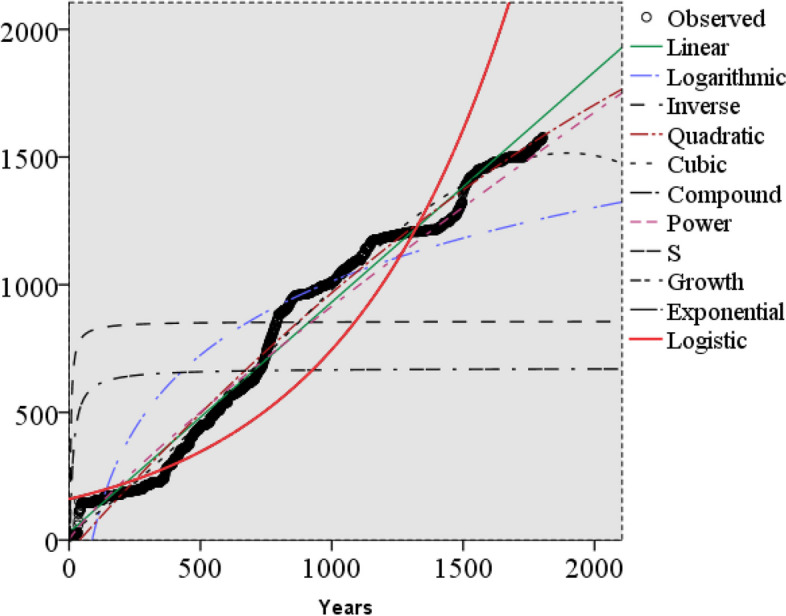
Lassa Fever Observed and Fitted Cumulative Cases in Ebonyi State, 2018–2022
Table 5 represents the summary and parameter estimates of the models selected for the study. The quadratic model was identified as the best fit to model Lassa fever reported cases. The quadratic model fits perfectly with the R-square of 98.2%, and was therefore chosen as the best for the Lassa fever data. The R-square for the cubic model was 98.5% but, its curve shows a sinusoidal curve which was inappropriate.
Table 5.
Model summary and parameter estimates
| Model | R Square | F | Sig | Parameter Estimates | |||
|---|---|---|---|---|---|---|---|
| Constant | β1 | β2 | β3 | ||||
| Linear | 0.979 | 83,210.677 | < 0.001 | 29.564 | 0.902 | ||
| Logarithmic | 0.758 | 5622.757 | < 0.001 | -1867.459 | 417.047 | ||
| Inverse | 0.038 | 71.534 | < 0.001 | 856.801 | -3105.948 | ||
| Quadratic | 0.984 | 54,829.520 | < 0.001 | -45.781 | 1.153 | 0.000 | |
| Cubic | 0.987 | 46,700.646 | < 0.001 | 28.383 | 0.660 | 0.001 | -2.5E-007 |
| Compound | 0.813 | 7817.298 | < 0.001 | 160.514 | 1.002 | ||
| Power | 0.948 | 32,837.470 | < 0.001 | 2.223 | 0.872 | ||
| S | 0.138 | 288.417 | < 0.001 | 6.513 | -11.030 | ||
| Growth | 0.813 | 7817.298 | < 0.001 | 5.078 | 0.002 | ||
| Exponential | 0.813 | 7817.298 | < 0.001 | 160.514 | 0.002 | ||
| Logistic | 0.813 | 7817.298 | < 0.001 | 0.006 | 0.998 | ||
The data shown in Fig. 7 shows the cumulative observed and projected values for the reported Lassa fever cases in Ebonyi State from January 2023 to December 2023. The graph shows that the rate of increase in the number of projected Lassa fever cases is not constant but increasing over time from 2018 – 2022, and a total of 224 Lassa fever cases were projected for the year 2023.
Fig. 7.
Graphical Display of the Observed and Predicted Cumulative Reported Cases of Lassa Fever in Ebonyi State, 2018–2022
Discussion
The reported Lassa fever cases in Ebonyi state from 2018 to 2022 followed a downward trend. However, high number of Lassa fever cases were being reported throughout the analyzed years and its pattern of spread over the five-year period followed a fluctuating pattern. This outcome corroborates the earlier findings about the dynamics of Lassa fever and other similar infectious diseases [1, 13–15]. The observed pattern of Lassa fever cases in the current study could be attributed to relapse and variation in public health interventions, especially sensitization of the public concerning the preventive measures, preparedness, and control of the disease on yearly basis.
Literature has established that changes in the atmospheric conditions and environmental parameters can facilitates seasonal variations in the pattern of spread of infectious diseases like Ebola, COVID-19, Malaria, Measles, Rubella, etc. [31]. In the current study, the seasonality in the pattern of Lassa fever cases was established with the first quarter of the year expected to experience striking spread of the disease compared to the other quarters. This finding was in agreement with what was reported by a similar study in Nigeria [32]. The observed seasonality pattern could be attributed to the fact that the first quarter of the year is associated with a dry season and increased rodent population in Ebonyi State [4]. Dry season usually experienced in the first quarter of the year, serves as the breeding period for M.natanelsis rodents, exhibiting a strong seasonal dynamic connected to changes in food availability during that time. This period leads to unintentional human-to-human contact with rodents [4, 24]. Sylvester Chibueze et al [29] Deforestation of trees is usually practiced during the dry season resulting in habitat loss for wildlife and biodiversity loss (Chibueze, 2022a). Ecological factors such as rainfall show a relationship with the rodent habitat which serves as a significant factor in Lassa fever prevalence [24].
We found that the reported cases of Lassa fever were mostly prominent among adult aged 50 years and above. This finding was a deviation from what was found in an earlier study conducted in Ebonyi state where most suspected Lassa fever cases were reported among younger age groups [27]. The weakened immune systems and pre-existing health conditions associated with the elderly population could be responsible for this difference. The clinical and epidemiologic features of Lassa fever have previously shown that a compromised or weakened immune system serves as a predisposing factor for Lassa fever susceptibility among the elderly [19]. Higher proportion of males in both reported and confirmed cases of Lassa fever compared to females in Ebonyi state found in the present study has earlier being established in the literature [12]. The mortality associated with Lassa fever outcome over the five-year study period displays a fluctuating pattern, with an increase from 2019 to 2020, followed by a decline in 2021 and a slight increase in 2022. The COVID-19 pandemic which reduced access to healthcare services in the year 2020 and its comorbidity effect might be the possible reasons for the increased observed mortality associated with Lassa fever between 2019 and 2020. The manifestation of the intervention strategies for the COVID-19 pandemic in the year 2020 might have resulted in the reduction in Lassa fever cases observed in 2021. Farmers showed a lower risk of dying from Lassa fever compared to other work categories. This finding was similar to an outbreak investigation in Ebonyi State [27]. There is the possibility that farmers in the study area accessed local herbs as one of the treatment mechanisms for the disease. Although not validated, the nature of their daily routine activities could imply suppressing the infections associated with the disease. The reasons for reduced mortality risk among the farmers might be a good area for further research.
The data further showed variation in Lassa fever cases across the LGAs in Ebonyi state, indicating a heterogenous pattern. Urban LGAs such as Abakaliki, Izzi, and Ikwo LGA reported higher incidence of Lassa fever cases, whereas the rural LGAs including Onicha, Afikpo South, and Ivo LGAs had fewer cases. Clustering of Lassa fever cases was also observed between Abakaliki and Ebonyi local government areas over the study period. These findings were similar to what was found by Solomon [27]. The improved surveillance and capacity for testing Lassa fever cases, access to health facilities, and the poor living arrangement in the slums in the urban LGAs compared to the rural LGAs might be the possible reason for this observed rural–urban LGAs pattern. There is the likelihood that socio-economic factors such as poverty, population density, poor agricultural practices, low public awareness of Lassa fever, and cultural practices might be responsible for the variation in Lassa fever cases across the LGAs in Ebonyi State. Differentials in environmental conditions like housing conditions, hygiene practices, and sanitation [31] might be responsible for the variation observed in the number of cases of Lassa fever across the LGAs in Ebonyi state.
The quadratic equation was the model of best fit for the Lassa fever trajectory in Ebonyi state. In previous research, the quadratic model was recognized among the top-performing predictive models for Ebola and COVID-19 [2, 28, 34] using the quadratic model, a total of 224 Lassa fever cases was predicted for the year 2023 with the assumption that the prevailing public health intervention activities, disease immunity,and atmospheric, environmental, and socioeconomic conditions would be sustained throughout the period. Although the predicted number of Lassa fever cases showed a declining trend, it is noteworthy that there was no deviation between the pattern of the observed yearly reported number of cases over the five years and the predicted values Due to the infectious nature of Lassa fever and its high case-fatality rate, relevant government agencies and parastatals are doing everything possible to eradicate the disease from society. A state free from Lassa fever is desirable by any government. Therefore, the Ebonyi state government might need to strengthen its preventive and control mechanisms to ensure that the large number of predicted cases for the year 2023 do not manifest in reality.
As for other diseases in the IDSR register, implementing the Lassa fever IDSR strategy in Nigeria has recorded some successes including operationalized response and epidemic preparedness at all tiers of government, dedicated staff, and budgetary allocation to disease surveillance. However, the IDSR faces several challenges such as inadequate trained staff, poor infrastructure and coordination, and inadequate data on reported cases of Lassa fever etc. These challenges often affect its effective implementation and more importantly, the data quality. Although the national IDSR register has a case definition for Lassa fever, the inconsistencies in case definition at the state level can lead to a higher or lower number of reported or diagnosed cases. It is not impossible that typographical errors and missing data in the IDSR form could have resulted in incomplete reporting of Lassa fever cases in the data used for the current study. The use of a large number of Lassa fever-reported cases from 2018 to 2022 is a strength of this paper, especially in its mathematical modelling aspect. However, a deviation from the predicted number of Lassa fever cases in this paper for the year 2023 is anticipated due to possible variation in the underlying assumptions of the model. Therefore, the readers should be cautious of these anticipated changes in their interpretation of the findings.
Conclusion
Lassa fever persists in both endemic and non-endemic local government areas in Ebonyi state but a declining trend was observed across the state. There was a seasonality in the pattern of spread of Lassa fever in Ebonyi state with an indication that the first and third quarters of the year are likely to witness more reported cases than other quarters. Being unemployed and aged at least 50 years predisposed individuals to higher risk of Lassa fever. The data suggests a temporal trend of the occurrence of the disease. highlighting a persistent occurrence of the disease in every year. While efforts to eliminate and mitigate the spread of the disease in Ebonyi state should be strengthened, more attention should target those periods of the year where higher number of cases is anticipated. Qualitative studies are needed to ascertain the reasons while the unemployed individuals are more at risk of contracting the disease. The lower mortality risk among some occupational groups like farmers emphasizes the need for occupational-specific intervention on Lassa fever preventive measures in Ebonyi state, Nigeria.
Acknowledgements
We thank the data originator for releasing the data for this study.
Abbreviations
- AOR
Adjusted Odd Ratio
- ASI
Adjusted Seasonal Index
- CI
Confidence Interval
- CFR
Case Fatality Rate
- IDSR
Integrated Disease Surveillance and Response
- LGA
Local Government Area
- LF
Lassa Fever
- NCDC
Nigeria Centre for Disease Control
- UOR
Unadjusted Odd Ratio
- WHO
World Health Organization
Authors’ contributions
Conception, AEA, ASA; Data extraction AEA; Data Analysis and Modelling, AEA, ASA, ATS; Draft, AEA, ASA, ATS. All authors reviewed the draft and made substantial contributions to produce the first draft of the manuscript. All authors approved the final draft of the manuscript to be published.
Funding
Financial support for this study was obtained from the European and Developing Countries Clinical Trials Partnership (EDCTP), The views, opinions, and content of this publication are those of the authors and do not necessarily reflect the views, opinions, or policies of EDCTP.
Data availability
The data could be accessed online at Nigeria Centre for Disease Control and Prevention. Interested users should visit the website and register for access and permission to use the data.
Declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained by the data originators from the Ebonyi State Ministry of Health (EBSHREC/01/04/2022–02/04/2024).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Adebowale AS, Afolabi RF, Bello S, Salawu MM, Bamgboye EA, Adeoye I, Dairo MD, Kivumbi B, Wanyana I, Seck I, Diallo I, Leye MMM, Bassoum O, Fall M, Ndejjo R, Kabwama SN, Mapatano MA, Bosonkie M, Egbende L, … Fawole OI. Spread and seasonality of COVID ‑ 19 pandemic confirmed cases in sub ‑ Saharan Africa : experience from Democratic Republic. BMC Infect Dis 2023;1–12. 10.1186/s12879-023-08168-1 [DOI] [PMC free article] [PubMed]
- 2.Adebowale AS, Fagbamigbe AF, Akinyemi JO, Obisesan OK, Awosanya EJ, Afolabi RF, Alarape SA, Obabiyi SO. The spread of COVID-19 outbreak in the first 120 days : a comparison between Nigeria and seven other countries. 2021:1–8. [DOI] [PMC free article] [PubMed]
- 3.Agbonlahor DE, Akpede GO, Happi CT, Tomori O. 52 Years of Lassa Fever Outbreaks in Nigeria, 1969 – 2020: an epidemiologic analysis of the temporal and spatial trends. 2021;105(4):974–985. 10.4269/ajtmh.20-1160 [DOI] [PMC free article] [PubMed]
- 4.Akhmetzhanov AR, Asai Y, Nishiura H. Quantifying the seasonal drivers of transmission for Lassa fever in Nigeria. Philos Transact Royal Soc B: Biolog Sci 2019;374(1775). 10.1098/rstb.2018.0268 [DOI] [PMC free article] [PubMed]
- 5.Aloke C, Obasi NA, Aja PM, Emelike CU, Egwu CO, Jeje O, Edeogu CO, Onisuru OO, Orji OU, Achilonu I. Challenges, and future perspectives. 2023;1–25. [DOI] [PMC free article] [PubMed]
- 6.Bakare EA, Are EB, Abolarin OE, Osanyinlusi SA, Ngwu B, Ubaka ON. Mathematical modelling and analysis of transmission dynamics of Lassa fever. J Appl Math 2020;2020. 10.1155/2020/6131708
- 7.Barua S, Dénes A, Ibrahim MA. A seasonal model to assess intervention strategies for preventing periodic recurrence of Lassa fever. Heliyon. 2021;7(8):e07760. 10.1016/j.heliyon.2021.e07760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonner PC, Schmidt W-P, Belmain SR, Oshin B, Baglole D, Borchert M. Poor housing quality increases risk of rodent infestation and Lassa fever in refugee camps of Sierra Leone. 2007. [PubMed]
- 9.Cadmus S, Taiwo OJ, Akinseye V, Cadmus E, Famokun G, Fagbemi S, Ansumana R, Omoluabi A. Ecological correlates and predictors of Lassa fever incidence in Ondo State , Nigeria 2017 – 2021 : an emerging urban trend. Sci Rep 2023;1–15. 10.1038/s41598-023-47820-3 [DOI] [PMC free article] [PubMed]
- 10.Centers for Disease Control and Prevention (CDC). Lassa fever: NCDC confirms 8 new infections, as death toll hits 171. The Guardian Nigeria: National.18thSept. 2022. https://www.environewsnigeria.com/lassa-fever-ncdc-confirms-eight-new-infections-as-death-toll-hits-171/.
- 11.Centers for Disease Control and Prevention (CDC). Nigeria Centre for Disease Control. 2022. https://ncdc.gov.ng/ncdc.gov.ng/.
- 12.Dalhat MM, Olayinka A, Meremikwu MM, Dan-Nwafor C, Iniobong A, Ntoimo LF, Onoh I, Mba S, Ohonsi C, Arinze C, Esu EB, Nwafor O, Oladipupo I, Onoja M, Ilori E, Okonofua F, Ochu CL, Igumbor EU, Adetifa I. Epidemiological trends of Lassa fever in Nigeria, 2018–2021. Plos One. 2022;17(12 December):2018–21. 10.1371/journal.pone.0279467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faruk AS, Adebowale AS, Balogun MS, Taiwo L, Adeoye O, Mamuda S. Temporal trend of measles cases and impact of vaccination on mortality in Jigawa State, Nigeria, 2013–2017 : a secondary data analysis. 35(Supp 1):2013–2017. 10.11604/pamj.supp.2020.35.1.19780 [DOI] [PMC free article] [PubMed]
- 14.Fatiregun AA, Adebowale AS, Fagbamigbe AF. Epidemiology of measles in Southwest Nigeria : an analysis of measles case-based surveillance data from 2007 to 2012. 2015;2014:133–140. 10.1093/trstmh/tru004 [DOI] [PubMed]
- 15.Fatiregun AA, Fagbamigbe A. Epidemiology of rubella disease in south-west nigeria : trends and projection from measles case- based surveillance data. 2018;2014. 10.1080/23120053.2014.11441571
- 16.Federal Ministry of Health (FMoH) National policy on Integrated Disease Surveillance Response in Nigeria. Abuja: Federal Ministry of Health; 2005. pp. 1–7.
- 17.Grainer C. A Software for Disease Surveillance and Outbreak Response: Insights from Implementing SORMAS in Nigeria and Ghana. Bonn, Germany: German Federal Ministry for Economic Cooperation and Development; 2020. Accessed Oct 2024.
- 18.Idi H, Lasisi KE, Abdulhameed M, Kwami AM. Determinants of Lassa fever prevalence with regards to attitudes and environmental factors in Bauchi State. J Sci Technol Educ. 2022;10(4):2022. [Google Scholar]
- 19.Ilori EA, Frank C, Dan-nwafor CC, Ipadeola O, Krings A, Ukponu W, Womi-eteng OE, Adeyemo A, Mutbam SK, Musa EO, Lasuba CLP, Alemu W, Okogbenin S, Ogbaini E, Unigwe U, Ogah E, Onoh R, Abejegah C, Ayodeji O. (2019). Increase in Lassa Fever Cases in Nigeria. 2018;25(5):2018–9. [DOI] [PMC free article] [PubMed]
- 20.Musa SS, Zhao S, Gao D, Lin Q, Chowell G, He D. Mechanistic modelling of the large-scale Lassa fever epidemics in Nigeria from 2016 to 2019: modelling the Lassa fever epidemics in Nigeria. J Theoret Biol 2020;493. 10.1016/j.jtbi.2020.110209 [DOI] [PubMed]
- 21.Nigeria Center for Disease Control. NCDC Weekly Epidemiological Report. Vol. 3. WER-Nigeria: Nigeria Center for Disease Control. 2012. pp. 8–11.
- 22.Nigeria Centre for Disease Control. Lassa fever Situation Report Epi Week 52. 2020. https://reliefweb.int/report/nigeria/ncdc-lassa-fever-situation-report-epi-week-52-21-27-december-2020. Accessed 16 Nov 2021.
- 23.Ojo MM, Gbadamosi B, Benson TO, Adebimpe O, Georgina AL. Modeling the dynamics of Lassa fever in Nigeria. J Egyptian Math Soc. 2021. 10.1186/s42787-021-00124-9. [Google Scholar]
- 24.Redding DW, Gibb R, Dan-nwafor CC, Ilori EA, Yashe RU, Oladele SH, Amedu MO, Iniobong A, Att LA, Donnelly CA, Abubakar I, Jones KE, Ihekweazu C. Geographical drivers and climate-linked dynamics of Lassa fever in Nigeria. 2020;2021:1–10. 10.1038/s41467-021-25910-y [DOI] [PMC free article] [PubMed]
- 25.Saka JM, Bintu Gubio A, Kerecvel YS, Saka AO, Oyemakinde A. Lassa fever epidemic in Nigeria - outbreak investigation, risk factors and empirical analysis from 2012 to 2016. J Commun Publ Health Nurs 2017;03(02). 10.4172/2471-9846.1000170
- 26.Secher PH, Hangaard S, Kronborg T, Korsbakke L, Hæsum E, Udsen FW, Hejlesen O, Bender C. Clinical implementation of an algorithm for predicting exacerbations in patients with COPD in telemonitoring: a study protocol for a single-blinded randomized controlled trial. 2022:1–10. [DOI] [PMC free article] [PubMed]
- 27.Solomon JG. Outbreak investigation of Lassa fever in Ebonyi State. Texila Int J Publ Health 2019;161–169. 10.21522/tijph.2013.se.19.02.art021
- 28.Stephen A, Francis A, Odunayo J, Olalekan K, Jolaoluwa E, Felix R. Situation assessment and natural dynamics of COVID-19 pandemic in Nigeria, 31 May 2020. Scientific African. 2021;12:e00844. 10.1016/j.sciaf.2021.e00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sylvester Chibueze I, Kurotimipa Frank O, Matthew Chidozie O. Lassa fever in Nigeria: social and ecological risk factors exacerbating transmission and sustainable management strategies. Int J Trop Dis 2022;5(2). 10.23937/2643-461x/1710065
- 30.Sylvester Chibueze I, Kurotimipa Frank O, Matthew Chidozie O. Lassa fever in Nigeria: social and ecological risk factors exacerbating transmission and sustainable management strategies. Int J Trop Dis 2022b;5(2). 10.23937/2643-461x/1710065
- 31.Ulor A, Ana G. Environmental determinants and markers of Lassa fever transmission in a low socioeconomic community in Akure, southwestern Nigeria. Int J Infect Dis. 2021;101:404. 10.1016/j.ijid.2020.09.1060. [Google Scholar]
- 32.Umoke MJ, Umoke PCI, Nwalieji CA, Onwe RN, Nwafor IE, Agbaje SO, Nwimo IO. Assessment of knowledge and sources of information on Lassa fever infection among the undergraduate students of Ebonyi State University, Nigeria. SAGE Open 2021;11(1). 10.1177/21582440211006382
- 33.Usuwa IS, Akpa CO, Umeokonkwo CD, Umoke M, Oguanuo CS, Olorukooba AA, Bamgboye E, Balogun MS. Knowledge and risk perception towards Lassa fever infection among residents of affected communities in Ebonyi State. Nigeria: Implications for risk communication; 2020. p. 1–10. [DOI] [PMC free article] [PubMed]
- 34.Wang G, Yao W. An application of small-world network on predicting the behavior of infectious disease on campus. Infect Dis Model. 2024;9(1):177–84. 10.1016/j.idm.2023.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.WHO. Lassa fever. https://www.who.int/news-room/fact-sheets/detail/lassa-fever. Accessed 23 June 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data could be accessed online at Nigeria Centre for Disease Control and Prevention. Interested users should visit the website and register for access and permission to use the data.