Abstract
Background
The Mustard and Senning operations for dextro-transposition of the great arteries (D-TGA) establish a biventricular physiology with a subaortic right ventricle (sRV). While prolonged QRS has been associated with worse prognosis in these patients, current echocardiographic tools fall short in adequately assessing the (mal)performance and function decline of the sRV during follow-up. The present study is the first to characterize Myocardial Work (MW) indices of the sRV in D-TGA patients after Mustard/Senning repair.
Methods and results
All adult D-TGA patients at follow-up in the University Hospital of Leuven between 2018 and 2022 were screened for inclusion. We retrospectively collected the most recent electrocardiogram parameters, 2D echocardiographic images and serum biomarkers’ values. Offline calculations of MW indices were performed. We established correlations between all variables and categorized patients into QRS<120 ms and QRS≥120 ms for further analysis. A total of 51 D-TGA patients were included (13 Mustard, 33 male, 39 ± 6 years). QRS duration increased with age and was correlated with sRV dimensions and serum levels of troponins (R = 0.42, p < 0.01) and NT-proBNP (R = 0.31, p = 0.03). However, no significant correlation was found between QRS duration and intraventricular desynchrony or conventional functional echocardiographic parameters. QRS prolongation was associated with a deterioration in septal, but not lateral, MW parameters. Patients with QRS≥120 ms had significantly larger ventricles and higher levels of troponins and NT-proBNP.
Conclusion
QRS prolongation after Mustard/Senning repair is linked to ventricular dilatation and worse performance, particularly affecting the septal wall. Global and regional MW analysis may be useful to assess the subclinical deterioration of sRV function.
Keywords: Subaortic right ventricle, Myocardial work, Transposition of the great arteries, Congenital, Pressure-strain loops, Strain
Abbreviations
| BP | blood pressure |
| CW | constructive work |
| D-TGA | dextro-Transposition of the great arteries |
| EF | ejection fraction |
| EDA | end diastolic area |
| EDV | end diastolic volume |
| ESA | end systolic area |
| ESV | end systolic volume |
| FAC | fractional area change |
| GCW | global constructive work |
| GLS | global longitudinal strain |
| GWW | global wasted work |
| GWE | global work efficiency |
| GWI | global work index |
| IQR | inter quartile range |
| LV | left ventricle |
| MW | myocardial work |
| PSL | pressure-strain loop |
| RV | right ventricle |
| sRV | subaortic right ventricle |
| TTE | transthoracic echocardiography |
| TAPSE | tricuspid annular plane systolic excursion |
| WW | wasted work |
1. Introduction
Transposition of the great arteries (TGA) accounts for approximately 6 % of all congenital heart diseases with a male to female sex ratio that varies between 1.5:1 and 3.2:1 [1,2]. TGA is often an isolated finding, however, approximately 30–50 % of patients also present with associated congenital heart defects [3].In cases of dextro-TGA (D-TGA) the combination of atrioventricular concordance with ventriculoarterial discordance results in 2 parallel and unconnected blood circuits necessitating early surgical intervention. The Mustard and Senning operations are two types of atrial switch repair that aim to correct blood flow at the atrial level establishing a biventricular physiology in which a subaortic right ventricle (sRV) supports the systemic circulation. Although the arterial switch operation replaced this approach in the 90s, there are still adult patients who underwent Mustard or Senning procedures requiring ongoing cardiac surveillance [4].
Long-term complications including baffle leaks, arrhythmias, QRS prolongation, tricuspid regurgitation (TR) or heart failure are frequently encountered following atrial switch repair [5,6]. In patients with a sRV, chronic pressure overload leads to right ventricle (RV) dilatation and hypertrophy while progressive tricuspid valve regurgitation causes chronic volume overload. Unfortunately, the absence of reference values and adequate diagnostic tools to assess sRV function, makes it difficult to determine the moment when this progressive physiological remodelling transitions into ventricular dysfunction [[7], [8], [9]].
Transthoracic echocardiography (TTE) is the primary diagnostic method for evaluating sRV function [10]. However, there is currently no straight evidence indicating which echocardiographic parameter has the highest reliability and greatest prognostic value. Tissue Doppler imaging with global longitudinal strain (GLS) analysis, is a highly advanced and promising tool for analysing myocardial function [11]. Yet it remains a load-dependent parameter that proves challenging to interpret in a sRV exposed to chronic pressure and volume overload.
Non-invasive Myocardial Work (MW) indices derived from left ventricle (LV) pressure–strain loops (PSL) can overcome the limitation associated with load-dependency by incorporating estimated LV pressure into their calculation [12,13]. Additionally, different MW parameters provide complementary information that can contribute to a more comprehensive analysis of ventricular function and physiology. The global work index (GWI) is derived from the area of the sRV PSL and reflects the total work calculated from tricuspid valve closure to tricuspid valve opening. On the other hand, the global constructive work (GCW) represents the work performed by the sRV contributing to ventricular ejection during systole. Conversely, the global wasted work (GWW) is the work performed by the sRV that does not contribute to ventricular ejection. As such, the global work efficiency (GWE) is defined as the ratio of GCW divided by the sum of GCW and GWW. Initially, this principle was applied to the RV by Butcher et al. [14] in a cohort of patients with pulmonary hypertension. More recently, the relationship between RV PSL-derived MW and contractility has been shown in patients with pulmonary hypertension and validated with invasive pressure-volume analysis [15].
The present explorative study seeks to describe MW indices of the sRV in a cohort of adult D-TGA patients with the aim of gaining a deeper understanding of its evolution following Mustard/Senning repair. Additionally, we pursue to identify sensitive echocardiographic determinants that can assess sRV function over the long-term follow up of these patients.
2. Methods
2.1. Patient population
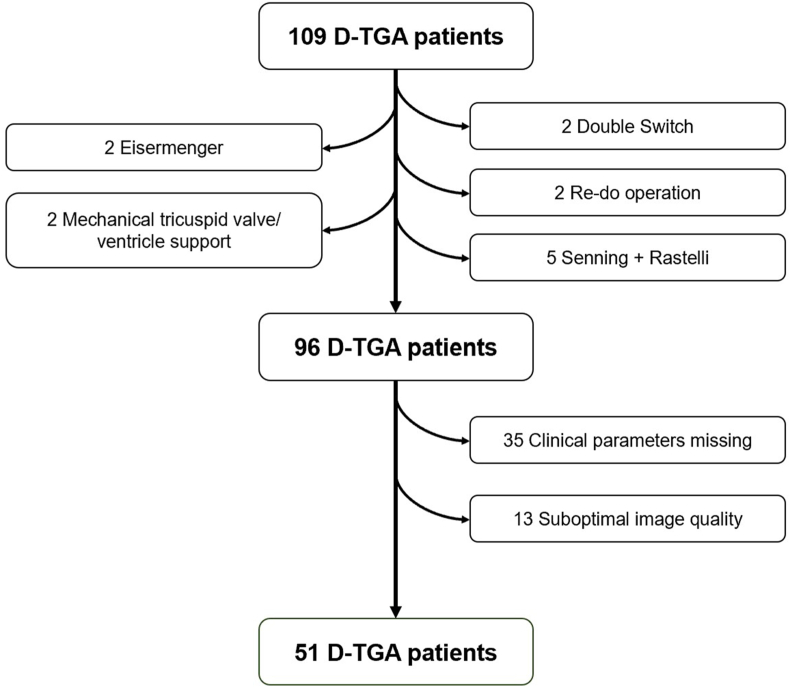
All D-TGA patients who had undergone atrial switch repair at follow-up in the University Hospital of Leuven between 2018 and 2022 were retrospectively screened (Fig. 1).Patients with double switch, a redo Mustard/Senning operation or a combination of Senning and Rastelli, Eisenmenger syndrome, a mechanical tricuspid valve or mechanical ventricular support were excluded. Furthermore, we excluded patients who either lacked echocardiographic images or had images of suboptimal quality and those with missing clinical parameters for MW calculation at the time of examination. In order to assure the highest-level accuracy in the calculation of MW parameters, only patients with BP measurements taken on the same day as the TTE were included in the analysis. In cases where multiple measurements were available on the same day, we calculated the average in order to avoid relying on isolated high or low values. This study was approved by the local Ethics Committee of the University Hospital of Leuven (s66145).
Fig. 1.
Flow chart of the patients' screening for inclusion in the study.
2.2. Data collection
All data were collected retrospectively from the latest available clinical reports. Parameters to evaluate cardiac electrical activity were obtained from the last available electrocardiogram and included heart rate (HR), PR interval, QRS duration and QTc interval. For the assessment of sRV function we analysed the most recent 2D echocardiographic images including M-mode, Doppler and tissue Doppler acquisitions. These images were analysed offline for calculation of both morphological and functional characteristics. The following dimensional variables were measured in a 4-chamber view: end systolic area (ESA), end diastolic area (EDA), end systolic volume (ESV), end diastolic volume (EDV) and stroke volume (SV). In addition to dimensional measurements, we assessed various functional variables for the sRV, including tricuspid annular plane systolic excursion (TAPSE), annular s’ and fraction area change (FAC) as well as ejection fraction (EF) using the Simpson's method and GLS. Furthermore, we evaluated mechanical desynchrony by utilizing the regional strain curves to compute the time-to-peak difference between the septal and lateral walls [16]. Finally we recorded the most recent serum levels of troponins and NT-proBNP.
2.3. Myocardial work calculation
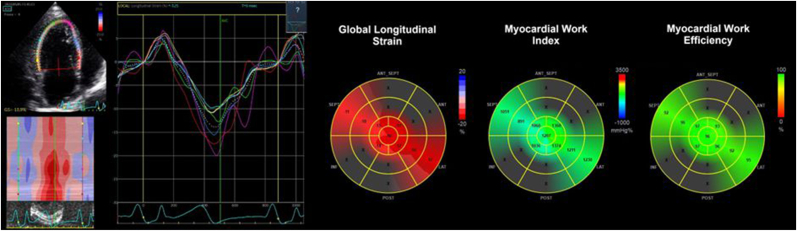
The software originally developed for the assessment of LV MW by 2D speckle tracking echocardiography was applied to the sRV for calculation of the MW indices following the methodology of Butcher et al. [17] and Russel et al. [13]. A RV-focused apical four-chamber view was used to obtain sRV GLS. In contrast with Butcher et al., the RV pressure was not measured using invasive right heart catheterization. Like Russel et al. did for the LV, we estimated the sRV intraventricular pressure by associating the peripheral arterial blood pressure (BP) with cardiac event times derived from tricuspid and aortic valve opening and closure. RV strain, non-invasive BP, measured at the brachial artery and valve events were integrated for MW calculation [18]. The global MW values were obtained as average from all myocardial segments from the apical four-chamber view (Fig. 2). Additionally, regional MW values for the lateral and septal wall separately were recorded.
Fig. 2.
Illustrative example of Myocardial Work calculation in a sRV. A RV-focused apical four-chamber view was used to obtain the sRV regional strain curves and calculate the global average. We estimated the sRV intraventricular pressure curve by associating the brachial arterial blood pressure with cardiac valve events. MW was automatically calculated by the software which integrates the sRV strain and non-invasive estimated intraventricular pressure. The regional MW values were presented in a color-coded bull's eye and the global MW values were obtained as average from all myocardial segments from the apical four-chamber view.
2.4. Statistical analysis
Descriptive data are reported as the mean ± sd for normally distributed continuous variables and as median [IQR] for continuous variables without normal distribution. Normality testing was performed by graphical analysis with histograms and QQ-plots. Pearson R correlation value between all continue variables was obtained. Based on previous studies reporting the association between QRS prolongation and sudden cardiac death in Mustard/Senning patients [19,20], QRS duration was used to categorize patients in two groups; QRS<120 ms and QRS≥120 ms. Intergroup differences were determined using the T-test and Mann-Whitney U test for continue variables with or without normal distribution respectively. To identify clinically relevant differences between the study groups, the logarithmic transformation was applied to NT-proBNP and MW parameters. This was necessary as these variables exhibited either an exponential distribution or extensive range of values with a difference of more than 1000 units between the lowest and highest value. For all tests, a p-value below 0.05 was considered statistically significant. The Bonferroni correction was applied in order to adjust for multiple testing. All statistics analysis were performed using SPSS for Windows Version 25 (SPSS, IBM headquarters, Armonk, NY, USA).
3. Results
3.1. Study population
In our final analysis a total of 51 patients (18 male, 39 ± 6 years) were included in the final analysis. Patients’ baseline characteristics are summarized in Table 1. Troponin and NT-proBNP were missing in 4 patients. Additionally, only troponin was missing in 3 patients. Only 5 patients had a pacemaker and none of them was pacing-dependent. Additionally, during the most recent pacemaker interrogation before inclusion the percentage pacing was 0 %. Atrial fibrillation was present in 2 patients. For the myocardial work analysis in these patients, images of the three apical views with similar HR were selected. While TR more than moderate was found to be present in 62 % of the patients, we did not find a significant difference in the prevalence of TR in patients with QRS<120 ms vs those with QRS≥120 ms. Moreover, there is currently a lack of available data on the potential effect of TR on the myocardial work analysis of the right ventricle.
Table 1.
Patient's baseline characteristics for the whole study population and for each group separately.
| TOTAL | QRS<120 ms | QRS≥120 ms | |
|---|---|---|---|
| N (male %) | 51 (65) | 33 (55) | 18 (83) |
| Age, mean±sd | 39 ± 6 | 38 ± 6 | 41 ± 6 |
| Mustard, n(%) | 13 (25) | 5 (15) | 8 (44) |
| Senning, n(%) | 38 (75) | 28 (85) | 10 (56) |
| Diabetes mellitus, n(%) | 0 | 0 | 0 |
| Arterial hypertension, n(%) | 1 (2) | 1 (3) | 0 |
| Dyslipidemia, n(%) | 1 (2) | 0 | 1 (6) |
| Obesity, n(%) | 4 (8) | 3 (9) | 1 (6) |
| Palpitations, n(%) | 15 (29) | 7 (21) | 8 (44) |
| Sinus rhythm, n(%) | 40 (78) | 27 (82) | 13 (72) |
| Atrial fibrillation, n(%) | 2 (4) | 1 (3) | 1 (6) |
| Right bundle branch block, n(%) | 11 (22) | 2 (6) | 9 (50) |
| Grade tricuspid valve regurgitation ≥ moderate, n(%) | 31 (62) | 21 (63) | 10 (56) |
| Atrio-ventricular block, n(%) | 3 (6) | 0 | 3 (17) |
| NYHA class 1 | 41 (80) | 29 (88) | 12 (67) |
| NYHA class 2 | 10 (20) | 4 (12) | 6 (33) |
| Beta-blocker, n(%) | 18 (35) | 11 (33) | 5 (28) |
| RAAS inhibitor, n(%) | 19 (37) | 11 (33) | 8 (44) |
| Diuretics, n(%) | 8 (16) | 4 (12) | 4 (22) |
| Anticoagulants, n(%) | 13 (25) | 4 (12) | 9 (50) |
| Statins, n(%) | 2 (4) | 1 (3) | 1 (6) |
NYHA: New York Heart Association, RAAS: renin-angiotensin-aldosterone system.
3.2. Correlations
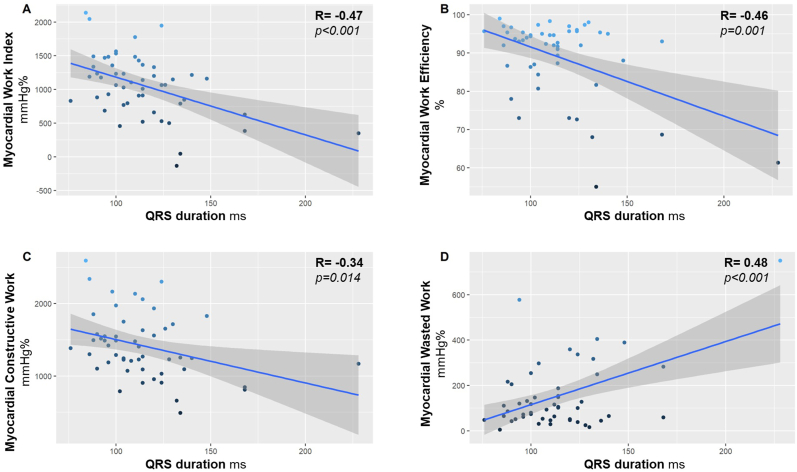
The positive correlation between QRS duration and age advocates for an increase in electromechanical dissociation in parallel with age. Additionally, QRS duration correlated with several sRV morphological features such as the EDA, ESA, ESV, EDV as well as with the serum levels of troponins and NT-proBNP (Table 2). However, we did not find any significant correlation between QRS duration and parameters related to intraventricular mechanical desynchrony or sRV function such as TAPSE, annular s’, EF and GLS. Still, a weak correlation was found between QRS duration and FAC. Interestingly, we discovered a significant correlation between the global MW parameters and the QRS duration with the exception of GCW. When looking at regional MW analysis, we found that all septal MW parameters, correlated with the QRS duration (Fig. 3) whereas this correlation was not observed for the lateral MW parameters.
Table 2.
Pearson R correlation coefficient with QRS duration.
| QRS duration | p-value | |
|---|---|---|
| Ventricle Dimensions (sRV) | ||
| End systolic area | 0,449 | 0,001 |
| End diastolic area | 0,405 | 0,003 |
| End systolic volume | 0,428 | 0,002 |
| End diastolic volume | 0,416 | 0,002 |
| Biomarkers | ||
| TnT | 0,421 | 0,004 |
| NT-proBNP | 0,314 | 0,032 |
| Ventricle Function (sRV) | ||
| TAPSE | −0,088 | 0,541 |
| Annular s' | −0,276 | 0,093 |
| FAC | −0,314 | 0,025 |
| EF (a4C) | −0,184 | 0,197 |
| GLS (a4c) | 0,137 | 0,337 |
| INTRAVENTRICULAR DYSYNCHRONY (sRV) | ||
| Time-to-peak lateral | 0,331 | 0,017 |
| Peak strain lateral | −0,064 | 0,656 |
| Time-to-peak septal | 0,150 | 0,293 |
| Peak strain septal | 0,301 | 0,032 |
| Desynchrony lateral-septal | −0,146 | 0,306 |
| GLOBAL MYOCARDIAL WORK | ||
| Global Work Index | −0,297 | 0,035 |
| Global Work Efficiency | −0,393 | 0,004 |
| Global Constructive Work | −0,255 | 0,071 |
| Global Wasted Work | 0,393 | 0,004 |
| LATERAL MYOCARDIAL WORK | ||
| Myocardial Work Index | 0,094 | 0,511 |
| Myocardial Work Efficiency | −0,089 | 0,535 |
| Constructive Work | 0,033 | 0,816 |
| Wasted Work | 0,099 | 0,488 |
| SEPTAL MYOCARDIAL WORK | ||
| Myocardial Work Index | −0,474 | <0,001 |
| Myocardial Work Efficiency | −0,462 | 0,001 |
| Constructive Work | −0,343 | 0,014 |
| Wasted Work | 0,481 | <0,001 |
a4C: apical 4-chamber view, EF: ejection fraction, FAC: fractional area change, GLS: global longitudinal strain, NT-proBNP: N-terminal pro-brain natriuretic peptide, sRV: subaortic right ventricle, TAPSE: tricuspid annular plane systolic excursion, TnT: Troponins T.
Fig. 3.
Correlation between QRS duration and the different septal MW parameters.
After Bonferroni adjustment, only the correlation between the QRS duration and septal MW index and septal WW was still statistically significant. Therefore, a potential type I error cannot be excluded for the resting correlations found.
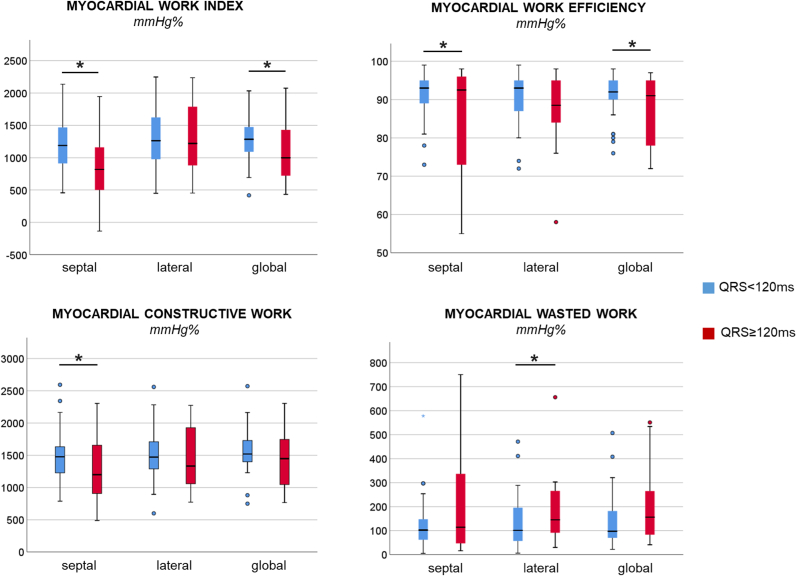
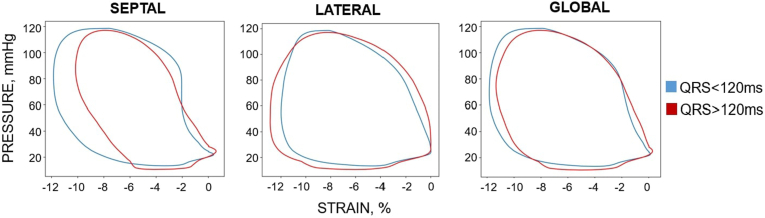
3.3. Normal vs prolonged QRS duration
Patients with a prolonged QRS had significantly larger sRV compared to patients with a normal QRS duration while no notable differences between the two groups were observed regarding mechanical desynchrony parameters (Table 3). Despite the substantially higher serum levels of troponins and NT-proBNP in the QRS≥120 ms group, no intergroup difference was found in terms of LV functional parameters (EF and GLS). Interestingly, when evaluating global and regional MW parameters significant intergroup differences were observed for MW index, MW efficiency, CW and WW, particularly in the septal region (Fig. 4, Table 3) Additionally, the mean septal PSL, which is used to determine septal MW parameters, showed a reduce surface area in patients with a QRS duration ≥120 ms compared to patients with normal QRS duration (Fig. 5). When applying Bonferroni adjustment for multiple testing, the intergroup difference remained statistically significant for ESA and ESV but not for the other variables including MW parameters.
Table 3.
Hemodynamic, anatomical and functional characteristics of de whole study population and per group.
| ALL |
QRS<120 |
QRS≥120 |
p-value |
|
|---|---|---|---|---|
| mean ± sd median [IQR] |
mean ± sd median [IQR] |
Mean ± sd median [IQR] | ||
| General | ||||
| Age, years | 39 ± 6 | 38 ± 6 | 41 ± 6 | 0,184 |
| Systolic blood pressure, mmHg | 125 ± 16 | 128 ± 17 | 121 ± 13 | 0,148 |
| Diastolic blood pressure, mmHg | 76 ± 13 | 79 ± 13 | 70 ± 11 | 0,014 |
| Body Surface Area, m2 | 1,9 ± 0,2 | 1,9 ± 0,2 | 1,8 ± 0,2 | 0,518 |
| Ecg Parameters | ||||
| Heart rate, bpm | 68 ± 13 | 69 ± 15 | 66 ± 9 | 0,480 |
| PR interval, ms | 166 ± 33 | 154 ± 25 | 191 ± 36 | 0,003 |
| QRS duration, ms | 114 ± 26 | 100 ± 10 | 139 ± 26 | <0,001 |
| QTc interval, ms | 433 ± 34 | 422 ± 28 | 453 ± 37 | 0,004 |
| Ventricle Dimensions (sRV) | ||||
| End systolic area, cm2 | 23 ± 7 | 20 ± 5 | 28 ± 8 | <0,001 |
| End diastolic area, cm2 | 32 ± 7 | 29 ± 5 | 36 ± 7 | 0,002 |
| End systolic volume, ml | 68 ± 31 | 57 ± 19 | 88 ± 39 | <0,001 |
| End diastolic volume, ml | 109 ± 38 | 95 ± 29 | 135 ± 39 | 0,001 |
| Stroke volume, ml | 41 ± 17 | 38 ± 18 | 47 ± 14 | 0,046 |
| Biomarkers | ||||
| TnT, ng/l | 6 [4,8] | 6 [4,8] | 9 [5,23] | 0,030 |
| NT-proBNP, ng/l | 258 [164, 432] | 247 [144, 346] | 308 [174, 977] | 0,045∗ |
| Intra-Ventricle Dysynchrony | ||||
| Time-to-peak lateral, s | 0,41 ± 0,06 | 0,40 ± 0,05 | 0,42 ± 0,07 | 0,325 |
| Peak strain lateral, % | −13,95 ± 4,58 | −13,85 ± 4,29 | −14,14 ± 5,21 | 0,845 |
| Time-to-peak septal, s | 0,37 ± 0,06 | 0,36 ± 0,04 | 0,37 ± 0,09 | 0,807 |
| Peak strain septal, % | −12,61 ± 4,14 | −13,28 ± 3,59 | −11,40 ± 4,86 | 0,161 |
| Desynchrony lateral-septal, s | −0,04 ± 0,07 | −0,04 ± 0,05 | −0,06 ± 0,09 | 0,114 |
| Ventricle Function (sRV) | ||||
| TAPSE, mm | 13 ± 3 | 13 ± 4 | 12 ± 3 | 0,143 |
| Annular s' | 6 ± 2 | 6 ± 2 | 5 ± 2 | 0,072 |
| FAC, % | 28 ± 11 | 30 ± 12 | 24 ± 8 | 0,016 |
| EF (a4C), % | 39 ± 12 | 40 ± 12 | 37 ± 12 | 0,467 |
| GLS (a4C), % | −13 ± 4 | −13 ± 3 | −12 ± 5 | 0,381 |
| Global Myocardial Work | ||||
| Global Work Index, mmHg% | 1200 ± 385 | 1268 ± 327 | 1073 ± 455 | 0,043° |
| Global Work Efficiency, % | 92 [84, 95] | 92 [89, 96] | 91 [78, 95] | 0,031° |
| Global Constructive Work, mmHg% | 1515 ± 378 | 1572 ± 349 | 1409 ± 416 | 0,103° |
| Global Wasted Work, mmHg% | 109 [70, 206] | 97 [69, 187] | 157 [79, 272] | 0,166° |
| Lateral Myocardial Work | ||||
| Myocardial Work Index, mmHg% | 1313 ± 428 | 1300 ± 378 | 1336 ± 519 | 0,935° |
| Myocardial Work Efficiency, % | 92 [86, 95] | 93 [86, 96] | 89 [84, 95] | 0,184° |
| Constructive Work, mmHg% | 1489 ± 415 | 1494 ± 382 | 1480 ± 481 | 0,741° |
| Wasted Work, mmHg% | 120 [69, 199] | 101 [57, 197] | 146 [89, 271] | 0,040° |
| Septal Myocardial Work | ||||
| Myocardial Work Index, mmHg% | 1065 ± 466 | 1199 ± 388 | 819 ± 506 | 0,007° |
| Myocardial Work Efficiency, % | 93 [87, 95] | 93 [88, 95] | 93 [72, 96] | 0,014° |
| Constructive Work, mmHg% | 1421 ± 450 | 1508 ± 412 | 1261 ± 482 | 0,049° |
| Wasted Work, mmHg% | 102 [52, 216] | 102 [57, 151] | 114 [47, 343] | 0,374° |
a4C: apical 4-chamber view, ECG: electrocardiogram, EF: ejection fraction, FAC: fractional area change, GLS: global longitudinal strain, NT-proBNP: N-terminal pro-brain natriuretic peptide, sRV: subaortic right ventricle, TAPSE: tricuspid annular plane systolic excursion, TnT: Troponins T. °logarithmic scale.
Fig. 4.
Regional and global Myocardial Work parameters according to QRS duration. (logarithmic scale, ∗p ≤ 0.05).
Fig. 5.
Global and regional pressure-strain loops van de sRV according to QRS duration.
Intra- and interobserver variability were calculated using intraclass coefficient (ICC) and the standard error of measurements (Table 4). While a slightly higher intra- and interobserver variability was observed for GWE and GWW compared to GWI and GCW, the Interclass Correlation Coefficient (ICC) was excellent (>0.9) for intra-observer variability in all MW parameters. By contrast, for the interobserver variability, ICC was good (>0.8) for GWE and GWW and excellent for GWI and GCW.
Table 4.
Intra- and interobserver variability for MW analysis of the sRV.
| Intra-observer variability |
Inter-observer variability |
|||||
|---|---|---|---|---|---|---|
| ICC |
Bias | Limits of agreement | ICC |
Bias | Limits of agreement | |
| (95 % CI) | (95 % CI) | |||||
| GWI, mmHg% | 0.982 | 13.1 ± 69.8 | −123.8 to 150.0 | 0.974 | −43.4 ± 107.6 | −245.3 to 176.5 |
| (0.929–0.996) | (0.895–0.994) | |||||
| GCW, mmHg% | 0.962 | −44.8 ± 85.6 | −212.6 to 123.0 | 0.946 | 23.0 ± 126.6 | −225.2 to 271.2 |
| (0.848–0.991) | (0.784–0.987) | |||||
| GWW, mmHg% | 0.934 | 37.2 ± 52.7 | −66.1 to 140.5 | 0.821 | 28.1 ± 47.6 | −65.1 to 121.3 |
| (0.735–0.984) | (0.281–0.956) | |||||
| GWE, % | 0.944 | −2.0 ± 3.2 | −8.3 to 4.3 | 0.890 | −1.8 ± 2.44 | −6.6 to 2.9 |
| (0.776–0.986) | (0.558–0.973) | |||||
GCW, global constructive work; GWE, global work efficiency; GWI, global work index; GWW, global wasted work; ICC, Interclass Correlation Coefficient.
4. Discussion
To the best of our knowledge, this study sets the first attempt to describe global and regional MW parameters in D-TGA patients who have undergone Mustard/Senning repair and have a sRV. The main results of our analysis can be summarized as follows: 1- There is an age-related increase in QRS duration in D-TGA patients which is associated with a dilatation of the sRV but not with a more pronounced mechanical desynchrony. 2- D-TGA patients with prolonged QRS and overloaded sRV exhibit higher levels of cardiac biomarkers. 3- MW parameters, as opposed to conventional echocardiographic parameters for assessment of RV or LV function, are closely linked to QRS duration. 4- Patients with prolonged QRS duration show more pronounced impairment in septal MW parameters whereas lateral MW parameters remain relatively unaffected. These findings shed new light on the relationship between QRS duration, sRV function, and MW parameters in D-TGA patients following Mustard/Senning repair.
4.1. Assessment of the sRV function by myocardial work
Prolonged QRS duration is a well-known documented phenomenon following Mustard/Senning repair and has been associated with the deterioration of the sRV function [19,21]. Also QRS fragmentation has been shown to have an impact on the post-surgical survival as demonstrated by Helsen et al. [22] However, our analysis could not prove a significant correlation between conventional echocardiographic parameters and QRS duration. It is worth noting that the anatomical and physiological differences between the ventricles pose a challenge for using conventional echocardiographic parameters designed for assessing normal RV and LV function to properly evaluate the sRV function [23,24]. By contrast, our study manifests the potential advantages of employing global and regional MW analysis for this purpose, as it incorporates the peripheral arterial BP into the assessment of sRV function. Notably, three MW parameters -GWI, GWE and GWW- progressively worsen with QRS prolongation.
Even though the calculation of MW may be primarily influenced by fibre shortening rather than by afterload, the use of MW parameters and components offer a more comprehensive assessment of the sRV performance compared to GLS and TAPSE. To date, PSL-derived MW analysis has been investigated in various pathologies like pulmonary hypertension [25], atrial septum defect [26]and advanced heart failure [27]. However, clear reference values are still lacking due to the limited data available. Additionally, while normal MW values have been determined for the LV, these values cannot be directly applied to sRV. Therefore, further research is warranted to understand the clinical significance of different MW values in sRV.
Of note, while lateral MW did not show a correlation with QRS duration, the septal MW parameters, particularly wasted work (WW), displayed the highest correlation. This finding suggests that sRV dysfunction and eventual failure may originate at the septum and might be related to the subpulmonary LV function (Fig. 5) [28,29]. The pressure and volume overload experienced by the sRV will cause preferentially the free wall to stretch leading to an increase in size of the RV chamber and bowing of the septum toward the left side. Ultimately this process can lead to septal hypokinesia and dysfunction [30]. Although a considerable number of patients presented with at least moderated TR, its potential impact on MW parameters of the sRV, remains uncertain and warrants further investigation.
The prevalence of atrial fibrillation could make the MW analysis complicate and less reliable. However, Liu and colleagues [31] demonstrated that the calculation of MW parameters is feasible in various types of atrial fibrillation. Additionally, the proportion of patients with atrial fibrillation in our study population was very limited. It should be noted that the cardiac index measured in our study population falls below the normal range. This might be related to several factors. On the one hand, our calculation of the ventricular volume relays on one single 2D-image and the complex geometry of the sRV makes it challenging to acquire high quality images for accurate measurements. On the other hand, this may also indicate impaired contractility of the systemic right ventricle ultimately leading in the long term to a depressed cardiac performance.
4.2. The impact of QRS prolongation on sRV function
While mechanical desynchrony did not directly correlate with QRS prolongation, the regional MW analysis has unveiled discrepancy in the performance between the septal and lateral wall in patients with QRS≥120 ms compared to those with normal QRS duration. Patients with QRS≥120 ms were characterized by lower septal CW, MW index and MW efficiency. This finding contrasts with the previous correlation analysis which primarily linked septal WW to QRS duration.
In accordance with our results, Pluymen et al. reported the association of sRV size with NT-proBNP levels and QRS duration following Mustard/Senning repair [21]. Also Roos-Hesselink and colleagues confirmed a significant increase in QRS duration over long-term follow-up accompanying deterioration in sRV function as measured by echocardiography [32]. QRS prolongation, ventricular dilatation and cardiac dysfunction represent gradual processes, stemming from the chronic pressure and volume overload on the sRV in D-TGA patients. Consequently, establishing normal cut-off values for these parameters proves challenging. Therefore, in further research, a serial assessment approach may offer a more comprehensive evaluation of sRV (mal)performance and function decline over time. Based on our results, MW analysis emerges as a potentially valuable tool for this purpose.
4.3. Limitations
This study does have certain limitations. First, it focuses on a distinctive aging patient population with post-surgical sRV and unique characteristics resulting from Mustard/Senning procedures. Consequently, this study is limited by a relatively small sample size and a single-centre design which hampers statistical analysis. Therefore, possible accidental findings need to be confirmed in larger studies. Second, MW assessment is a relatively and underexplored method that has not been extensively applied to the RV. Additionally, whereas cardiac magnetic resonance is considered the gold standard to measure RV volumes our analysis is based on TTE images, as it is a more accessible technique in the daily practice. Lastly, the advanced nature of this analysis demands high quality images which may not be readily obtainable in routine clinical practice. Given the retrospective nature of the study, the inclusion of patients was limited by the availability of suitable data. Also, potential differences between the Mustard and Senning procedure may affect outcomes among populations with different proportions.
5. Conclusion
Our study is the first to describe MW values in the sRV of D-TGA patients after Mustard/Senning repair. We have observed a post-surgical prolongation of QRS duration which aligns with a ventricular dilatation and more impaired cardiac performance. In the context of chronic pressure and volume overload, it appears that the underperformance of the sRV after Mustard/Senning repair may originate at the septal wall. Global and regional MW analysis, particularly septal MW values, emerges as a promising tool to assess subclinical sRV dysfunction. Instead of targeting direct clinical implications, our study aims to opens new perspectives for cardiac assessment in patients with a sRV. Certainly, follow-up studies are warranted to determine its prognostic value and delineate its clinical implications.
Sources of founding
A.M. reports receiving a research grant from the CardioPaTh Program.
CRediT authorship contribution statement
Ana Moya: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Sofie Verstreken: Writing – review & editing, Conceptualization. Dimitri Buytaert: Visualization, Software. Monika Beles: Methodology, Formal analysis. Elayne Kelen de Oliveira: Validation. Marc Vanderheyden: Writing – review & editing, Supervision, Investigation, Conceptualization. Alexander Van De Bruaene: Writing – review & editing, Methodology, Investigation, Conceptualization. Werner Budts: Writing – review & editing, Supervision, Methodology, Investigation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper other than one of the authors (WB) serving on the IJCCHD Editorial Board, albeit not involved with the handling of this paper.
References
- 1.Vejlstrup N., et al. Long-term outcome of mustard/senning correction for transposition of the great arteries in Sweden and Denmark. Circulation. 2015;132(8):633–638. doi: 10.1161/CIRCULATIONAHA.114.010770. [DOI] [PubMed] [Google Scholar]
- 2.Brida M., Diller G.-P., Gatzoulis M.A. Systemic right ventricle in adults with congenital heart disease. Anatomic and phenotypic spectrum and current aproach to management. Circulation. 2018;137:508–518. doi: 10.1161/CIRCULATIONAHA.117.031544. [DOI] [PubMed] [Google Scholar]
- 3.Martins P., Castela E. Transposition of the great arteries. Orphanet J Rare Dis. 2008;3(27) doi: 10.1007/978-3-319-44691-2_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moons P., Bovijn L., Budts W., Belmans A., Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. 2010;122:2264–2272. doi: 10.1161/CIRCULATIONAHA.110.946343. [DOI] [PubMed] [Google Scholar]
- 5.Kammeraad J.A.E., et al. Predictors of sudden cardiac death after mustard or senning repair for transposition of the great arteries. J Am Coll Cardiol. 2004;44(5):1095–1102. doi: 10.1016/j.jacc.2004.05.073. [DOI] [PubMed] [Google Scholar]
- 6.Khairy P. Sudden cardiac death in transposition of the great arteries with a Mustard or Senning baffle: the myocardial ischemia hypothesis. Curr Opin Cardiol. 2017;32(1):101–107. doi: 10.1097/HCO.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 7.Shah S., Gupta T., Ahmad R. Managing heart failure in transposition of the great arteries. Ochsner J. 2015;15(3):290–296. [PMC free article] [PubMed] [Google Scholar]
- 8.Van De Bruaene A., et al. Pulmonary hypertension in patients with a subaortic right ventricle: prevalence, impact and management. Heart. 2019;0:1–8. doi: 10.1136/heartjnl-2019-314756. [DOI] [PubMed] [Google Scholar]
- 9.Helsen F., et al. Right ventricular systolic dysfunction at rest is not related to decreased exercise capacity in patients with a systemic right ventricle. Int J Cardiol. 2018;260(2017):66–71. doi: 10.1016/j.ijcard.2018.03.029. [DOI] [PubMed] [Google Scholar]
- 10.Schneider M., et al. Systematic evaluation of systemic right ventricular function. J Clin Med. 2020;9(1) doi: 10.3390/jcm9010107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moya A., et al. 15-Year follow-up of regional right and left ventricular function after the Senning operation: a Colour-Doppler myocardial imaging study. Acta Cardiol. 2020;0(0):1–8. doi: 10.1080/00015385.2020.1770459. [DOI] [PubMed] [Google Scholar]
- 12.Papadopoulos K., Özden Tok Ö., Mitrousi K., Ikonomidis I. Myocardial work: methodology and clinical applications. Diagnostics. 2021;11(3):573. doi: 10.3390/diagnostics11030573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell K., et al. A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J. 2012;33(6):724–733. doi: 10.1093/eurheartj/ehs016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butcher S.C., et al. Right ventricular myocardial work characterization in patients with pulmonary hypertension and relation to invasive hemodynamic parameters and outcomes. Am J Cardiol. 2022;177(2):151–161. doi: 10.1016/j.amjcard.2022.04.058. [DOI] [PubMed] [Google Scholar]
- 15.Lakatos B.K., et al. Right ventricular pressure-strain relationship-derived myocardial work reflects contractility: validation with invasive pressure-volume analysis. J Heart Lung Transplant. 2024;43(7):1183–1187. doi: 10.1016/j.healun.2024.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Fudim M., Dalgaard F., Fathallah M., Iskandrian A.E., Borges-Neto S. Mechanical dyssynchrony: how do we measure it, what it means, and what we can do about it. J Nucl Cardiol. 2021;28(5):2174–2184. doi: 10.1007/s12350-019-01758-0. [DOI] [PubMed] [Google Scholar]
- 17.Butcher S.C., et al. Right ventricular myocardial work: proof-of-concept for non-invasive assessment of right ventricular function. Eur Heart J Cardiovasc Imaging. 2021;22(2):142–152. doi: 10.1093/ehjci/jeaa261. [DOI] [PubMed] [Google Scholar]
- 18.Smiseth O.A., Donal E., Penicka M., Sletten O.J. How to measure left ventricular myocardial work by pressure–strain loops. Eur Heart J Cardiovasc Imaging. 2020;(00):1–3. doi: 10.1093/ehjci/jeaa301. [DOI] [PubMed] [Google Scholar]
- 19.Schwerzmann M., et al. Ventricular arrhythmias and sudden death in adults after a Mustard operation for transposition of the great arteries. Eur Heart J. 2009;30(15):1873–1879. doi: 10.1093/eurheartj/ehp179. [DOI] [PubMed] [Google Scholar]
- 20.Koyak Z., et al. Sudden cardiac death in adult congenital heart disease: can the unpredictable be foreseen? Europace. 2017;19(3):401–406. doi: 10.1093/europace/euw060. [DOI] [PubMed] [Google Scholar]
- 21.Plymen C.M., et al. The relationship of systemic right ventricular function to ECG parameters and NT-proBNP levels in adults with transposition of the great arteries late after Senning or Mustard surgery. Heart. 2010;96(19):1569–1573. doi: 10.1136/hrt.2010.198648. [DOI] [PubMed] [Google Scholar]
- 22.Helsen F., et al. Appearance of QRS fragmentation late after Mustard/Senning repair is associated with adverse outcome. Heart. 2017;103(13):1036–1042. doi: 10.1136/heartjnl-2016-310512. [DOI] [PubMed] [Google Scholar]
- 23.Budts W., Scheurwegs C., Stevens A., Moons P., Van Deyk K., Vanhees L. The future of adult patients after Mustard or Senning repair for transposition of the great arteries. Int J Cardiol. 2006;113(2):209–214. doi: 10.1016/j.ijcard.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 24.Helsen F., et al. 2018. Advanced imaging to phenotype patients with a systemic right. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Butcher S.C., et al. Right ventricular myocardial work characterization in patients with pulmonary hypertension and relation to invasive hemodynamic parameters and outcomes. Am J Cardiol. 2022;177(2):151–161. doi: 10.1016/j.amjcard.2022.04.058. [DOI] [PubMed] [Google Scholar]
- 26.Wu J., et al. Noninvasive right ventricular work in patients with atrial septal defects: a proof-of-concept study. Cardiovasc Ultrasound. Dec. 2023;21(1) doi: 10.1186/s12947-023-00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landra F., et al. Right ventricular myocardial work for the prediction of early right heart failure and long-term mortality after left ventricular assist device implant. Eur Heart J Cardiovasc Imaging. Jan. 2024;25(1):105–115. doi: 10.1093/ehjci/jead193. [DOI] [PubMed] [Google Scholar]
- 28.Santens B., et al. Adverse functional remodelling of the subpulmonary left ventricle in patients with a systemic right ventricle is associated with clinical outcome. Eur Heart J Cardiovasc Imaging. May 2022;23(5):680–688. doi: 10.1093/ehjci/jeab086. [DOI] [PubMed] [Google Scholar]
- 29.Surkova E., et al. Systolic dysfunction of the subpulmonary left ventricle is associated with the severity of heart failure in patients with a systemic right ventricle. Int J Cardiol. Feb. 2021;324:66–71. doi: 10.1016/j.ijcard.2020.09.051. [DOI] [PubMed] [Google Scholar]
- 30.Saleh S., Liakopoulos O.J., Buckberg G.D. The septal motor of biventricular function. Eur J Cardio Thorac Surg. 2006;29(SUPPL. 1):126–138. doi: 10.1016/j.ejcts.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 31.Liu T., Liu H., Song Y., Huang Y., Zhang C. Quantitative assessment of left ventricular myocardial work in patients with different types of atrial fibrillation by non-invasive pressure-strain loop technique. Echocardiography. 2024;41 doi: 10.1111/echo.15801. [DOI] [PubMed] [Google Scholar]
- 32.Roos-Hesselink J.W., et al. Decline in ventricular function and clinical condition after mustard repair for transposition of the great arteries (a prospective study of 22-29 years) Eur Heart J. 2004;25(14):1264–1270. doi: 10.1016/j.ehj.2004.03.009. [DOI] [PubMed] [Google Scholar]