Abstract
Background
Specialised forensic mental health provision for young people with mental disorders and high-risk behaviours has developed significantly in the UK. Despite this, research on the young people within secure settings remains limited. Adolescents in secure settings exhibit higher levels of mental disorders and have complex needs. This study aims to compare the demographic characteristics of patients discharged from an adolescent medium secure unit (AMSU) to different discharge destinations: community, another hospital, or custodial setting.
Methods
A retrospective study was conducted using data from 155 patients admitted to a UK AMSU from 2008 to 2021. Demographic data, clinical information and Millon Adolescent Clinical Inventory (MACI) scores were extracted from electronic health records. A descriptive statistical method was used to report observational differences in patient characteristics between discharge locations. Statistical analysis included Chi-squared tests and AVOVA testing.
Results
Patients discharged to different settings exhibited distinct demographic and clinical characteristics. Those discharged to custodial settings were predominantly male and often transferred from custodial settings. Those discharged to other hospitals were mostly females with a diagnosis of Borderline Personality Disorder. The community-discharged group had a higher frequency of admissions from other hospitals under civil sections. Multiple variables were found to be statistically significant in relation to discharge location including gender and age at discharge. Findings of the MACI were not statistically significant in relationship with discharge location.
Conclusions
The study enhances understanding of healthcare transitions from AMSUs. The influence of diagnoses, particularly personality disorders, and their connection to admission duration is explored, as is the influence of this on transitioning patients across care settings. The impact of trauma-informed, attachment focussed models of care in regards transitions from AMSUs is also examined. Despite diversity in discharge locations, self-reported personality questionnaires show consistent outcomes, demonstrating psychological similarities across groups. Further research is needed to understand post-discharge trajectories enabling targeted interventions and improved care pathways.
Keywords: Forensic, Adolescent, Psychiatry, Discharge
1. Introduction
In the United Kingdom (UK), the provision of psychiatric healthcare to address the mental health needs of young people with mental disorders and high-risk behaviours has evolved into specialised forensic mental health services. These services operate at the intersection of mental health and the legal/criminal justice systems, encompassing work in prisons and other secure or closely supervised environments, as well as community-based interventions to identify and support high risk individuals with mental health needs. These teams offer therapeutic interventions while providing specialist formulation, care planning and risk management advice to other services.1
Over recent decades, significant development in these services has led to the establishment of specialist community teams, in addition to adolescent medium and low secure forensic psychiatric hospitals.1 These secure hospitals are integral parts of the secure estate within the UK, alongside detention facilities under the Youth Justice system, and Secure Children's Homes. The term "secure estate" encompasses settings restricting a young person's liberty such that they cannot leave at will, incorporating additional security measures beyond what's available in open residential, educational or mental health units.2 Both medium and low security psychiatric hospitals employ heightened levels of physical, procedural and relational security measures compared to standard adolescent psychiatric hospitals.
Secure units primarily admit young people who pose the highest levels of risk to others, including potential for physical harm, sexually aggressive behaviour, or maladaptive fire setting with the potential to endanger lives. Patients include those who have committed serious offenses, as well as those with complex presentations primarily associated with challenging behaviours, being a risk to themselves and others, self-harming tendencies, and vulnerability. Adolescent secure units admit patients from 12 to 18 years, all of whom are detained under the Mental Health Act 1983 as amended 2007 (MHA). Admission can occur regardless of whether the patient has a history of committing an offence. In cases where an offence has been committed, admission is possible, irrespective of the issue of criminal responsibility at the time of the offence.
Adolescents admitted to secure settings exhibit notably higher levels of mental disorders, emotional dysregulation, emerging personality disorders, and neurodevelopmental needs compared to their counterparts in the community.3 Consequently, substantial resources are required to meet their highly complex needs.4 Despite this, research on adolescents within secure settings remains limited, and there exists a gap in understanding the transitions of the adolescents from these secure settings.3, 4 Understanding these areas is crucial, as the decisions regarding a young person's discharge destination upon leaving an Adolescent Medium Secure Unit (AMSU) are primarily guided by the treating healthcare team and their assessment of the young person's mental health and risk profile. This includes those who are subject to sections of the MHA requiring judicial approval for alterations in the level of restriction, as it is the healthcare team's duty to make recommendations to facilitate these decisions. To date, research within adolescent medium secure settings has primarily focussed on retrospective cohort studies examining the clinical and personality characteristics of admitted patients and investigating differences between female and male patients.3, 5, 6, 7 However, long term outcomes for those discharged from AMSU's remain unknown, as well as potential distinctions among cohorts transitioning into the community, another hospital setting, or custody.
To begin addressing this knowledge gap, the objective of this paper is to compare and contrast the characteristics of patients discharged from an AMSU, focussing on three destinations: i) discharge to the community, ii) transfer to another hospital, or iii) placement in a custodial setting. Enhancing the understanding of these patients and the differences among those transitioning to different discharge destinations will contribute to a more comprehensive understanding of transitions from medium secure adolescent hospitals.
2. Methods
2.1. Study design
This retrospective study was designed using data gathered from 2008 to 2021 at the AMSU at Southern Health National Health Service (NHS) Foundation Trust.
2.2. Clinical setting
The AMSU is part of the UK’s network of medium secure forensic adolescent hospitals. It cares for mixed-gender adolescent patients primarily from the southern region of England. Consisting of 20 beds, the unit admits adolescents who have either come from custodial settings or presented to a hospital with evidence of posing a risk to themselves and/or others to an extent that cannot be managed in lower security settings. Since its establishment in 2008, the AMSU has admitted over 160 patients.
2.3. Data extraction and management
A sample size of 155 patients meeting the study’s eligibility criteria was obtained. These criteria included patients admitted to the unit who had subsequently been discharged, from its opening in 2008 until May 2021. Eight patients were deemed ineligible as they were still inpatients. No other exclusion criteria were applied. Data were extracted from the electronic health records (EHRs) of all eligible patients and recorded in an Excel template. Statistical analysis was conducted using TableOne, an open-source package in Python.8 Discharge destination's relationship with categorical variables was analysed using Chi-squared test of independence, while continuous variables were analysed using the one-way ANOVA test.
2.3.1. Ethical considerations
As a service evaluation, NHS Trust approvals were obtained before conducting the study. Since the data used in this study was extracted from routine clinical records, patient consent was not required. Access to patient data for the purpose of this evaluation, was restricted to the researchers affiliated with the AMSU, who had previously established access.
2.4. Variable selection
Demographic data collected included biological gender, ethnicity, child-care status, age at admission and discharge. The childcare status was defined in relation to looked after children (LAC). In the UK, LAC refers to children who have been in the care of their local authority for over 24 hours. This is primarily due to parents being unable to meet a child's needs, the parents own needs preventing them from providing adequate care or due to the child being at significant risk of harm from another. LAC include those subject to a court-directed care order, where the local authorities take legal responsibility for the child (Section 31 Children Act 1989), children looked after by the local authorities with voluntary agreement from their parents with parental responsibility remaining with the parents (Section 20 Children Act 1989), and Care Leavers, legally defined as individuals who have been in the care of the local authority for a period of 13 weeks or more spanning their 16th birthday. All children in custody awaiting trial automatically become LAC under UK law, for these children, their LAC status was recorded as that prior to them entering custody.
Clinical information extracted from EHRs included duration of stay, the section of the MHA under which they were detained, diagnosis, referral source, and details of discharge, including place of discharge and MHA status at discharge, and Millon Adolescent Clinical Inventory (MACI) scores.9 Diagnoses were provided by Consultant Psychiatrists based on a multidisciplinary team assessment, using ICD-10.10
The MACI is a self-report inventory, specifically tailored for adolescent populations to identify, understand, and predict a range of psychological difficulties. Responses are clustered into three scales: personality patterns, expressed concerns and clinical syndromes. The personality patterns scale consists of 15 items examining for the presence of enduring personality traits and characteristics, with items including 'oppositional' and 'borderline'. The 8 items in the expressed concerns scale examine for areas of concern and emotional distress as expressed by the adolescent and includes items such as 'family discord' and 'peer insecurity'. The clinical syndromes scale aims to identify clinical symptoms and potential psychological disorder, it has 7 items including 'substance abuse' and 'depressive affect'. For each MACI item, a score of 75 indicates clinical significance, representing the top 15% of the general population, while a score of 85 indicates clinical prominence, representing the top 10%. As an actuarial measure, statistical normative comparison can be made between respondents. The MACI has shown good internal consistency and test-retest reliability.11 External validity with other relevant instruments showed high correlations.11
3. Results
3.1. Demographic characteristics and discharge destination
The majority of patients discharged to a custodial setting were male (89.9%), while females constituted a larger proportion (59.7%) in the group discharged to other hospitals. The Chi-square test of independence indicated a statistically significant relationship between gender and discharge destination (p = <0.001) (Table 1). Both age on admission and at discharge also showed a statistically significant association with discharge destination (p = 0.022 and p = <0.001, respectively). There were no substantial variations in ethnicity across the three discharge groups, with the sample predominately consisting of White British individuals (81.9%). Chi-squared tests for ethnicity and child-care status did not show statistical significance.
Table 1.
Table of Demographic Characteristics.
| Overall | Community | Hospital | Prison | p-value | |
|---|---|---|---|---|---|
| N | 155 | 69 | 67 | 19 | |
| Age On Admission, mean (SD) | 16.1 (1.2) | 15.8 (1.3) | 16.2 (1.1) | 16.5 (1.0) | 0.022 |
| Age On Discharge, mean (SD) | 16.9 (1.4) | 16.3 (1.5) | 17.6 (0.9) | 16.8 (1.1) | < 0.001 |
| Gender, n (%) | < 0.001 | ||||
| Male | 86 (55.5) | 42 (60.9) | 27 (40.3) | 17 (89.5) | |
| Female | 69 (44.5) | 27 (39.1) | 40 (59.7) | 2 (10.5) | |
| Ethnicity, n (%) | 0.523 | ||||
| White British | 127 (81.9) | 55 (79.7) | 56 (83.6) | 16 (84.2) | |
| Black/Black British | 10 (6.5) | 7 (10.1) | 3 (4.5) | ||
| Asian | 7 (4.5) | 4 (5.8) | 2 (3.0) | 1 (5.3) | |
| Other/Mixed | 11 (7.1) | 3 (4.3) | 6 (9.0) | 2 (10.5) | |
| Looked after child status, n (%) | 0.052 | ||||
| No | 76 (49.0) | 36 (52.2) | 35 (52.2) | 5 (26.3) | |
| Yes - Full Care Order | 55 (35.5) | 24 (34.8) | 20 (29.9) | 11 (57.9) | |
| Yes - Section 20 | 17 (11.0) | 8 (11.6) | 6 (9.0) | 3 (15.8) | |
| Yes - Leaving Care | 6 (3.9) | 6 (9.0) | |||
| Unknown | 1 (0.6) | 1 (1.4) | |||
Legend. Demographic factors of sample compared by discharge destination. Chi-squared tests for the following variables may be invalid due to the low number of observations: Ethnicity, Looked after child status.
3.2. Referral and admission factors
Across the entire sample, the highest proportion of admissions were from secure psychiatric hospitals (36.1%). Young Offenders Institutes (YOIs) followed closely behind, accounting for 25.8% of admissions (Table 2a). This pattern was consistent among individuals discharged to the community and those discharged to other hospitals. However, among patients discharged to custodial settings, an overwhelming majority (94.7%) had been admitted from the youth justice part of the secure estate, encompassing YOIs and Secure Training Centres (STC) and Secure Children Homes (SCH).
Table 2a.
Comparison of Referral Source and Admission Factors to Discharge Location.
| Discharge Locations |
|||||
|---|---|---|---|---|---|
| Overall | Community | Hospital | Prison | p-value | |
| N | 155 | 69 | 67 | 19 | |
| Referral Source, n (%) | 0.001 | ||||
| Adolescent general psychiatric unit | 16 (10.3) | 10 (14.5) | 6 (9.0) | ||
| Adolescent psychiatric intensive care unit | 12 (7.7) | 8 (11.6) | 4 (6.0) | ||
| Adolescent secure psychiatric unitA | 56 (36.1) | 24 (34.8) | 31 (46.3) | 1 (5.3) | |
| Adult general psychiatric unit | 6 (3.9) | 4 (5.8) | 2 (3.0) | ||
| Community - Children’s home | 1 (0.6) | 1 (1.5) | |||
| Community - Home | 5 (3.2) | 3 (4.3) | 2 (3.0) | ||
| Community - Residential school | 1 (0.6) | 1 (1.4) | |||
| Community - Supported accommodationB | 1 (0.6) | 1 (1.4) | |||
| Secure Children’s HomeC | 9 (5.8) | 4 (5.8) | 4 (6.0) | 1 (5.3) | |
| Secure Training CentreD | 8 (5.2) | 3 (4.3) | 2 (3.0) | 3 (15.8) | |
| Young Offenders InstituteE | 40 (25.8) | 11 (15.9) | 15 (22.4) | 14 (73.7) | |
| Section on Admission, n (%) | < 0.001 | ||||
| Section 2F | 22 (14.2) | 16 (23.2) | 6 (9.0) | ||
| Section 3G | 74 (47.7) | 36 (52.2) | 38 (56.7) | ||
| Section 37H | 9 (5.8) | 5 (7.2) | 4 (6.0) | ||
| Section 37/41I | 2 (1.3) | 2 (3.0) | |||
| Section 47/49J | 19 (12.3) | 5 (7.2) | 4 (6.0) | 10 (52.6) | |
| Section 48/49K | 29 (18.7) | 7 (10.1) | 13 (19.4) | 9 (47.4) | |
| Length Of Stay, mean (SD) | 333.3 (326.4) | 253.3 (241.5) | 477.6 (380.0) | 115.1 (97.9) | < 0.001 |
| Median | 246 | 193 | 371 | 77 | |
Legend. Comparison of Referral and Admission factors by discharge destination. Chi-square test of independence shows significant relation for all the factors (p-value <0.001), but with a warning that expected count < 5.
Notes
Adolescent psychiatric inpatient hospitals with additional levels of physical, procedural and relational security measures.
Accommodation with support for 16- and 17-year-old looked after children and care leavers, where they live semi-independently.
Licenced by court to deprive adolescents in their care of their liberty. Adolescents are either sentenced or awaiting trial/sentencing through the justice system or placed due to local authority concerns a person is a serious risk to themselves or others.
Place of detention for 12–17 years olds, typically used for younger adolescents or older adolescents deemed vulnerable.
Prisons for 15–21 year olds.
Civil section, allowing for detention for assessment and treatment for up to 28 days.
Civil section, allowing for detention for treatment of mental disorder.
Forensic section, a hospital order imposed when a person is convicted of an imprisonable offence but is admitted to psychiatric hospital, or placed under guardianship of a local social services authority, instead of receiving a custodial sentence.
Forensic section, the addition of a restriction order to the Section 37, imposing additional restrictions to protect the public from serious harm.
Forensic section, allowing for the transfer of a sentenced prisoner to hospital.
Forensic section, allowing for the transfer of a prisoner awaiting trial or sentencing to hospital.
To be eligible for admission and treatment within an AMSU, all patients must be detained under the MHA. In the subgroups discharged to the community and to another hospital, higher numbers of patients were admitted under civil sections rather than forensic sections (Table 2a). Forensic sections are those which cover the sections in Part III of the MHA which informs the management of persons concerned in criminal proceedings or under sentence, whereas civil sections, are those within part II of the MHA and provide for someone to be detained in hospital under a legal framework for an assessment and treatment of mental disorder. The majority of patients were admitted under Section 3, accounting for 52.2% of community admissions and 56.2% of hospital admissions. All patients discharged to a custodial setting were initially admitted under forensic sections, with 52.6% under Section 47/49 and 47.4% under Section 48/49.
Alongside referral source and section on admission, length of stay was also shown to have a statistically significant relationship to discharge destination (Table 2a). Those discharged to prison had the shortest mean length of stay (77 days) while those discharged to another hospital had the longest (371 days).
3.3. Discharge factors
Among those discharged to the community, 88.4% became informal patients, while the remaining patients were discharged under a Community Treatment Order (CTO) (Table 2b).
Table 2b.
Comparison of Factors at Point of Discharge to Discharge Location.
| Discharge Locations |
|||||
|---|---|---|---|---|---|
| Overall | Community | Hospital | Prison | p-value | |
| N | 155 | 69 | 67 | 19 | |
| Section on discharge, n (%) | < 0.001 | ||||
| Community Treatment OrderA | 8 (5.2) | 8 (11.6) | |||
| InformalB | 82 (52.9) | 61 (88.4) | 3 (4.5) | 18 (94.7) | |
| Section 3 | 40 (25.8) | 40 (59.7) | |||
| Section 37 | 12 (7.7) | 12 (17.9) | |||
| Section 37/41 | 6 (3.9) | 6 (9.0) | |||
| Section 38/41C | 1 (0.6) | 1 (1.5) | |||
| Section 45aD | 1 (0.6) | 1 (5.3) | |||
| Section 47/49 | 4 (2.6) | 4 (6.0) | |||
| Section 48/49 | 1 (0.6) | 1 (1.5) | |||
| Discharge Diagnosis, n (%) | < 0.001 | ||||
| F10-F19 Mental and Behavioural Disorders due to psychoactive substance use | 5 (3.2) | 3 (4.3) | 2 (10.5) | ||
| F20-F29 Schizophrenia, Schizotypal and Delusional Disorders | 44 (28.4) | 22 (31.9) | 18 (26.9) | 4 (21.1) | |
| F30-F39 Affective Disorders | 7 (4.5) | 2 (2.9) | 4 (6.0) | 1 (5.3) | |
| F40-F48 Neurotic, Stress Related and Somatoform Disorders | 5 (3.2) | 3 (4.3) | 1 (1.5) | 1 (5.3) | |
| F60.2 Dissocial Personality Disorder | 7 (4.5) | 1 (1.4) | 1 (1.5) | 5 (26.3) | |
| F60.3 Borderline Personality Disorder | 31 (20.0) | 8 (11.6) | 21 (31.3) | 2 (10.5) | |
| F70-F79 Intellectual Disabilities | 2 (1.3) | 1 (1.4) | 1 (1.5) | ||
| F84 Pervasive Developmental Disorders | 16 (10.3) | 4 (5.8) | 11 (16.4) | 1 (5.3) | |
| F90 Hyperkinetic Disorder | 2 (1.3) | 1 (1.4) | 1 (1.5) | ||
| F91 Conduct Disorders | 7 (4.5) | 4 (5.8) | 1 (1.5) | 2 (10.5) | |
| F92 Mixed Disorders of Conduct and Emotion | 25 (16.1) | 18 (26.1) | 7 (10.4) | ||
| F94 Disorders of social functioning with onset specific to childhood and adolescence | 1 (0.6) | 1 (1.4) | |||
| No formal diagnosis | 3 (1.9) | 1 (1.4) | 1 (1.5) | 1 (5.3) | |
| Discharge Destination, n (%) | < 0.001 | ||||
| Adolescent general psychiatric hospital | 4 (2.6) | 4 (6.0) | |||
| Adolescent low secure hospital | 4 (2.6) | 4 (6.0) | |||
| Adolescent medium secure hospital | 5 (3.2) | 5 (7.5) | |||
| Adult general psychiatric hospital | 4 (2.6) | 4 (6.0) | |||
| Adult high secure hospital | 1 (0.6) | 1 (1.5) | |||
| Adult low secure (autism specialist) hospital | 4 (2.6) | 4 (6.0) | |||
| Adult low secure hospital | 24 (15.5) | 24 (35.8) | |||
| Adult medium secure hospital | 20 (12.9) | 20 (29.9) | |||
| Community - Unspecified | 4 (2.6) | 4 (5.8) | |||
| Emergency accommodationE | 2 (1.3) | 2 (2.9) | |||
| Family Residence | 38 (24.5) | 38 (55.1) | |||
| Residential Care/Children's Home | 8 (5.2) | 8 (11.6) | |||
| Residential School | 3 (1.9) | 3 (4.3) | |||
| Secure Training Centre | 1 (0.6) | 1 (5.3) | |||
| Secure rehabilitation unitF | 1 (0.6) | 1 (1.5) | |||
| Supported accommodation | 14 (9.0) | 14 (20.3) | |||
| Young Offenders Institute | 18 (11.6) | 18 (94.7) | |||
Legend. Comparison of discharge factors by discharge destination. Chi-square test of independence shows significant relation for all the factors (p-value <0.001), but with a warning that expected count < 5.
Notes
Part of the MHA whereby on discharge a person is subject to conditions which enables them to be recalled to a hospital if there is deterioration in their mental health while in the community.
Not detained under mental health act.
Forensic section, an interim hospital order which can be given when a person is convicted of an imprisonable offence other than murder, where there is evidence that it may be appropriate for a hospital order under Section 37 to be made, and allows for a period of assessment to deem if this is appropriate.
Forensic section, whereby a person is sentenced to prison with a hospital direction such that an individual is initially detained to hospital for treatment of their mental disorder before transfer to prison.
Interim, temporary accommodation supplied by local authority.
Rehabilitation psychiatric unit for individuals with complex and enduring mental health needs which focus on longer term support with the aim for discharge into community settings. Secure units have higher levels of security to ensure safety and to manage risk.
For patients discharged to custodial settings, the majority were informal patients, as on return to a custodial setting, Sections 47/49 and 48/49 are rescinded and return occurs as an informal patient. In the subgroup discharged to another hospital, most patients were under civil sections at discharge (59.7% on a Section 3). Of the 35.9% discharged under a forensic section, the most frequent sections were Section 37 and Section 37/41.
Among all subgroups, the broadest spectrum of diagnoses was observed in the group discharged to the community (Table 2b). The Chi-square test of independence showed significant relationships for both section at discharge and discharge diagnosis in relation to discharge destination, however interpretation is restricted due to an anticipated count of 5.
3.4. MACI profiles
Overall, 61% of patients had completed a MACI assessment; 58% of the community group, 69% in the custodial group, and 63% in the hospital group. The aim is for assessment to occur at the start of admission, however practically it would occur as soon as a young person was willing to or able to engage. Therefore, the MACI results represent the psychological profiles of young people at varying timepoints in their admission. Non-completion was seen in cases of patient refusal or inability to engage due to the severity of their mental health difficulties. The MACI data are divided into three scales; personality patterns, expressed concerns, and clinical syndromes.
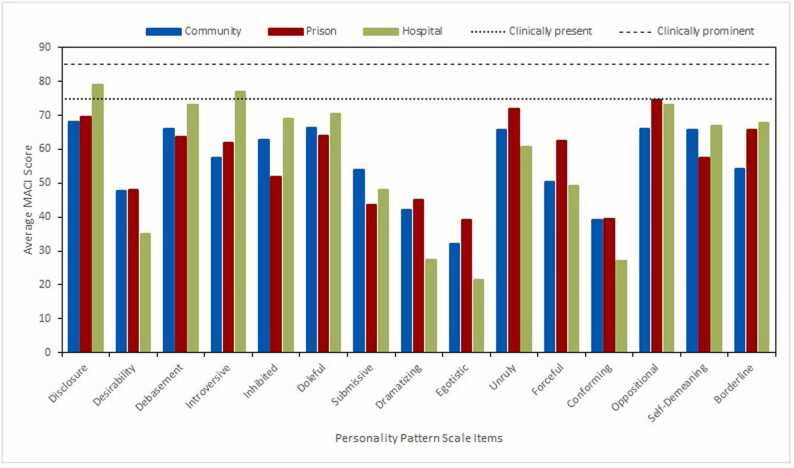
3.4.1. Personality patterns scales
In the subgroup discharged to hospital, ‘Disclosure’ and ‘Introversive’ were the only items across all subgroups in this scale where the average exceeded the clinically significant threshold of 75 (Fig. 1). The Chi-square test of independence indicated that the relationship between personality patterns and discharge location was statistically non-significant: X2 (95, N = 23k) = 29.8, p = 0.372.
Fig. 1.
MACI Personality Patterns Scale: Average Scores.
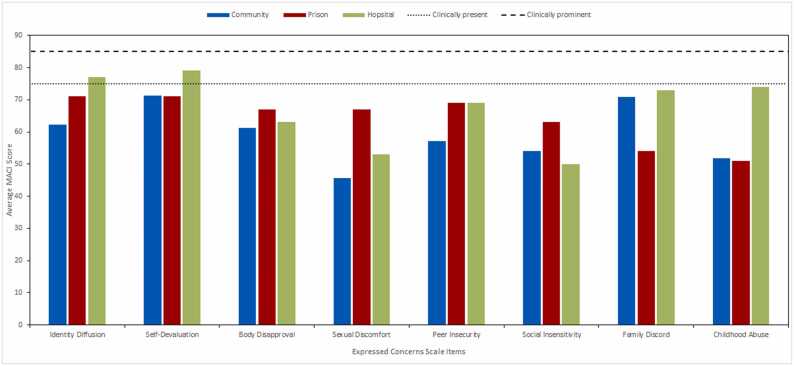
3.4.2. Expressed concern scales
In this scale, the average score of the items ‘Identity Diffusion and ‘Self-Devaluation’ exceeded the clinically significant threshold of 75 in the hospital subgroup (Fig. 2). The Chi-square test of independence showed that the relationship between expressed concern factors and discharge location was statistically non-significant, X2 (14, N = 95) = 19.8, p = 0.13.
Fig. 2.
MACI Expressed Concerns Scales: Average Scores.
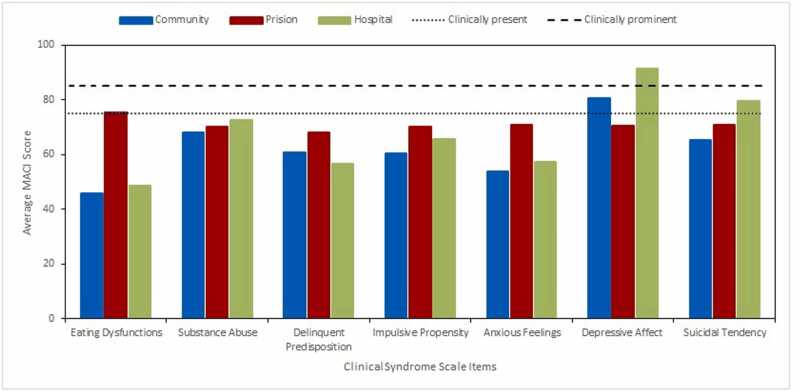
3.4.3. Clinical syndrome scales
This scale had the highest number of items with mean scores exceeding the clinically significant threshold of 75. In the community subgroup, ‘depressive affect’ exceeded this threshold, while ‘suicidal tendency’ exceeded it in the hospital subgroup. Additionally, ‘depressive affect’ in the hospital subgroup was the only item with an average exceeding the clinical prominence threshold (Fig. 3). The Chi-square test of independence showed that the relationship between clinical syndrome scales and discharge location was statistically non-significant, X2 (12, N = 95) = 10.3, p = 0.588.
Fig. 3.
MACI Clinical Syndrome Scales: Average Scores.
4. Discussion
4.1. Patients Transferred to Other Psychiatric Hospitals
The subgroup of patients transferred to another hospital upon discharge exhibited a higher proportion of females, with Borderline Personality Disorder emerging as the prevailing diagnosis within this category. This finding aligns with prior studies of this AMSU population that found a greater incidence of Borderline Personality Disorder among females compared with males. 3, 6 Notably, this predominantly female group exhibited the longest length of stay, corroborating prior research indicating prolonged admissions for female patients, where there were higher rates of Borderline Personality Disorder.3
The current clinical consensus, as mirrored in the National Institute for Health and Care Excellence (NICE) guidance for Borderline Personality Disorder, only favours inpatient treatment in situations of crisis management where there exists a significant risk to the patients’ life.12 This approach stems from concerns that hospitalisation may inadvertently escalate risks, through acute symptomatic deterioration, and escalated maladaptive behaviours such as self-harm, violence, and rule violations, ultimately resulting in prolonged admissions. 13,14 This pattern has been consistently observed at the AMSU, and is supported by the longer admissions in patients discharged to other hospitals, particularly where Borderline Personality Disorder is the dominant diagnosis.
This subgroup also exhibited the highest average age at discharge, a likely consequence of patients remaining within the AMSU beyond the anticipated transition to an adult hospital. The complexity of their presentations often hindered the identification of suitable alternative care options, occasionally resulting in extending their stay past 18 years of age. The severity of challenges encountered by this subgroup was also underscored by the MACI profiles. Five out of the six instances where an average score reached the clinical significance threshold, and the sole instance of an item’s average score attaining clinical prominence occurred within this subgroup discharged to other hospitals. This is suggestive of the level and frequency of complexity that sits within the group, however the chi-square test of independence indicated a statistically non-significant relationship between all MACI scales and discharge location. This demonstrates that items within the MACI should not be used clinically as an indicator as to the likely discharge destination or be used in isolation to inform transition decisions, however instead should help inform the understanding of risk a young person presents to themselves and others, which clinically drives decisions around discharge.
4.2. Patients transferred to custodial setting
The majority of patients discharged to custodial settings after an AMSU admission were male. This aligned with fact that that 94.7% of these young people were initially admitted from custodial settings, a setting predominantly populated by males. In the year ending March 2022, 97% of children in the secure estate in England and Wales, encompassing YOIs, STCs and SCHs were male. 15
All patients discharged to custodial settings had been initially admitted under forensic sections, specifically Section 48/49 or 47/49 of the MHA. Despite an overall reduction in the number of under 18's in custody, the unchanging rate of adolescent prisoners transferred to psychiatric hospitals in England and Wales suggests an increasingly complex cohort of offenders, some with severe psychiatric difficulties.16 The 2022 Mental Health Bill's proposal of a 28-day time limit for acutely ill prisoners to be transferred to hospital from prison for ongoing treatment may lead to an increase in the rate of adolescent prisoners transferred to AMSU’s in the future.17
This subgroup exhibited a higher proportion of LAC, compared to the other discharge settings. Within this group 73.7% were LAC on admission, 59.7% under full care orders. LAC have been shown to have experienced high rates of adversity including abuse, neglect, exposure to violence and inconsistent care, which not only elevate the likelihood of developing mental illnesses but also is significantly associated with interpersonal and self-directed violence. 18, 19, 20, 21, 22 Given the elevated rates of mental health disorders among LAC and children in custody, it's possible that the higher rates of LAC discharged to custodial settings stem from this shared predisposition.2, 23, 24
This subgroup exhibited the shortest median length of stay (77 days). Reasons for returning a patient to custody post-AMSU admission are varied. There may have been sufficient improvement in their mental health to allow a return to custodial settings, a failure to engage in therapeutic work or through the decision of the clinical team not to recommend a Section 37 hospital order at the point of sentence. Occasionally patients are transferred to hospital to undertake detailed assessment work that cannot be easily completed in custody and then returned to custody with recommendations regarding mental health treatment. The process of returning a child or young person to custody from hospital has been outlined by the Department of Health and can occur after a discharge planning meeting has occurred and with the agreement of the Ministry of Justice or following a sentencing hearing at court when a Section 37 hospital order has not been made.25 This process is quicker than finding a suitable community placement or an alternative appropriate hospital bed and will be contributing to the shorter length of stay in this cohort. The prevalence of Dissocial Personality Disorder diagnoses within this group, which has limited evidence supporting hospital admissions for its treatment, and the availability of custodial discharge options for risk monitoring and control, may also contribute to the shorter admissions observed in this subgroup.26
4.3. Patients discharged to community settings
A substantial percentage (45%) of patients transitioned to community settings, primarily family addresses or supported accommodation. This discharge process can be protracted, involving use of Section 17 leave, which allows for detained patients to be granted leave of absence from the hospital, before a discharge planning meeting (Section 117 meeting) convenes, involving staff from the AMSU and the receiving mental health team.
Among those discharged to the community, a higher frequency of admissions from other hospitals and under civil sections was observed. A smaller proportion came from secure settings under forensic sections, potentially indicating cases where individuals have been admitted while in custody awaiting trial and their case has been dropped or those who complete their sentence during admission, enabling community discharge. The 2022 Mental Health Bill's proposed introduction of supervised community discharge for restricted patients, may further enhance community discharge rates for those from custodial settings.17 Most community-discharged patients were informal while a minority were subject to CTOs. The limited use of CTO's might reflect efficacy concerns across multiple countries.27
4.4. Impact of a Trauma-Attachment Model of Care on Transitions
The AMSU operates based on a trauma informed-attachment focussed model of care, which recognises the importance of young people establishing relationships within a system which is able to provide consistent care. The model aims to minimise caregiver disruption, enabling young people to experience new relational experiences crucial for development, similar to those found in healthy parent-child relationships. Notably, caregiver disruption has been linked to increased rates of restraints, self-harming behaviours, and suicide attempts in inpatient settings.28
The trauma-attachment model most clearly impacts transitions within the groups discharged to another hospital and those transitioning to the community. For those discharged to another hospital, 79% are discharged to an adult psychiatric hospital, which mandate a minimum admission age of 18 years. This highlights that for this group, the majority of discharges occur during the transition from adolescent and adult healthcare systems. This practice aligns with reports of positive transition outcomes between adolescent and adult secure services when stability and security is prioritised, and number of transitions is minimised.29, 30
This emphasis on minimising transitions is also evident in the frequency of the young people being discharged directly to a community setting from the AMSU. This practice contrasts with adult forensic services, where such occurrences are infrequent. In adult services, it is common to transfer patients to lower security settings before community discharge. This underscores a notable divergence between patient pathways in adolescent versus adult inpatient secure services.29, 31
4.5. Strengths
This study contributes insights into a specialised field of psychiatric practice - medium secure services for adolescents. The study extends the knowledge base of existing research by demonstrating statistically significant distinctions in patient characteristics among different discharge settings from the AMSU. This paper confirms prior findings regarding diagnosis prominence and length of stay among specific groups, offering a comprehensive understanding, and how this impacts transitions from the AMSU.3, 6, 7 Importantly, this study signifies differences between adolescent and adult inpatient secure service discharge pathways, emphasising the practical implications of a trauma-informed, attachment focussed model on transition decisions. Notably, the examination of MACI scores did not establish statistically significant relationships with discharge locations.
4.6. Limitations
This study's strengths could be enhanced by incorporating data from multiple AMSU's to improve its generalisability and address the difficulties with insufficient minimum expected counts which hindered statistical test feasibility. Despite this, the findings from this AMSU are likely to be reflective of other UK AMSU's due to the wide geographical area covered by each unit. More caution would need to be used if applying these findings to settings outside the UK, due to the likely differences in the structure and functioning of adolescent psychiatric services internationally. MACI profile results, although informative, are limited by a completion rate of 61%, potentially not representing the entire cohort.
5. Conclusion
The study's findings enrich our understanding of healthcare transitions from AMSUs.
Exploration of the potential influence of diagnoses, particularly focussing on personality disorders, and their interconnectedness with the duration of admission enhances understanding of the challenges in transitioning patients across care settings. Furthermore, the impact of a trauma-informed, attachment focussed model of care on transition decisions has been examined. Importantly despite the diversity in discharge locations, there emerges a remarkable convergence of outcomes from the self-reported personality questionnaires where no statistical significance was identified. This observation demonstrates the nuanced psychological similarities that transcend the distinct discharge groups.
Despite the complexity and elevated risk factors associated with these young people, the predominate discharge location was to the community. The imperative for future research is undeniable. As health care transitions from AMSU to community settings carry inherent risks, we advocate for in-depth investigation through longitudinal studies or comprehensive surveillance initiatives. These would enable an understanding of the trajectory of these patient's post-discharge, ultimately informing the development of targeted interventions and refined care pathways.
Funding
This study was sponsored by Southern Health NHS Foundation Trust. SS and GD are supported by NIHR RCF. The study sponsors had no input in the study design, data extraction, analyses and interpretation of data, nor in the writing of the manuscript and in the decision to submit the paper for publication. This research did not receive any specific grant(s) from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Generative (AI) and AI-assisted technologies in the writing process
During the preparation of this work the authors used Open AI in order to improve readability of the text. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Ethical statement
NHS Trust approvals were obtained from the organisation. Ethics approval was not required as this was a service evaluation project. Consent to participate was not applicable, given that this was a service evaluation using routinely collected clinical data.
CRediT authorship contribution statement
Jones Charlotte: Writing – review & editing, Writing – original draft, Methodology, Investigation, Conceptualization. Hill Simon A: Writing – review & editing, Writing – original draft, Supervision, Methodology, Investigation, Conceptualization. Dibben Louise: Methodology, Investigation, Conceptualization. Sana Sajid: Writing – review & editing, Visualization, Conceptualization. Shetty Suchith: Resources, Formal analysis. Phiri Peter: Writing – review & editing, Supervision, Methodology. Majeed Selma: Formal analysis.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors acknowledge support from Southern Health NHS Foundation Trust.
Data availability
The data that has been used is confidential.
References
- 1.Hindley N., Lengua C., White O. Forensic mental health services for children and adolescents: rationale and development. BJPsych Adv. 2017;23(1):36–43. [Google Scholar]
- 2.Warner L., Hales H., Smith J., et al. Central and North West London NHS Foundation Trust and St George’s University of London; London: 2018. Secure settings for young people: A National scoping exercise. [Google Scholar]
- 3.Hill S.A., Brodrick P., Doherty A., Lolley J., Wallington F., White O. Characteristics of female patients admitted to an adolescent secure forensic psychiatric hospital. J Forensic Psychiatry Psychol. 2014 [Google Scholar]
- 4.McCrone P., Dhanasiri S., Patel A., et al. 1st ed.., Vol. 58. Kings Fund; London: 2008. (Paying the price). [Google Scholar]
- 5.Bailey S., Thornton L., Weaver A. The first 100 admissions to an adolescent secure unit. J Adolesc. 1994;17:207–220. [Google Scholar]
- 6.Hill A., Ferreira J., Chamorro V., Hosking A. Characteristics and personality profiles of first 100 patients admitted to a secure forensic adolescent hospital. J Forensic Psychiatry Psychol. 2019:352–366. [Google Scholar]
- 7.Hill S.A., Argent S.E., Lolley J., Wallington F. Characteristics of male patients admitted to an adolescent secure forensic psychiatric hospital. J Forensic Psychiatry Psychol. 2015;27 [Google Scholar]
- 8.Pollard T.J., Johnson A.E.W., Raffa J.D., Mark R.G. Tableone: An open source Python package for producing summary statistics for research papers. JAMIA Open. 2018;1:26–31. doi: 10.1093/jamiaopen/ooy012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Millon T., Millon C., Davis R., Grossman S. Pearson Assessment; San Antonio, TX: 2006. Millon Adolescent Clinical Inventory (MACI) [Google Scholar]
- 10.World Health Organisation. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organisation; 1992.
- 11.Pinto M., Grilo C. Reliability, diagnostic efficiency, and validity of the Millon adolescent clinical inventory: examination of selected scales in psychiatrically hospitalized adolescents. Behav Res Ther. 2004;42(12):1505–1519. doi: 10.1016/j.brat.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence [NICE]. Borderline Personality Disorder: recognition and management. London: 2009. [PubMed]
- 13.Livesley W.J. Guildford Press; New York, NY: 2003. Practical Management of Personality Disorder. [Google Scholar]
- 14.Biskin R.S., Paris J. Management of borderline personality disorder. Can Med Assoc J. 2012:1897–1902. doi: 10.1503/cmaj.112055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Youth Justice Board. Youth Justice Statistics England and Wales 2021/22. Accessed 7 November 2023. 〈https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1131414/Youth_Justice_Statistics_2021–22.pdf〉 -22.pdf (publishing.service.gov.uk);2023.
- 16.Hill S.A., Mitchell P., Leipold A. Transfers of mentally disordered adolescents from custodial settings to psychiatric hospitals in England and Wales 2004-2014. J Forensic Psychiatry Psychol. 2016:1–9. [Google Scholar]
- 17.Department of Health and Social Care. Draft Mental Health Bill. UK: DHSC; 2022.
- 18.Rahilly T., Hendry E. Promoting the wellbeing of children in care: messages from research. Lond: Natl Soc Prev Cruel Child. 2014 [Google Scholar]
- 19.Simkiss D.E. Outcomes for looked after children and young people. Paediatr Child Health. 2013;22:388–392. [Google Scholar]
- 20.Chapman D.P., Dube S.R., Anda R.F. Adverse childhood events as risk factors for negative mental health outcomes. Psychiatr Ann. 2007:359–364. [Google Scholar]
- 21.Duke N.N., Pettingell S.L., McMorris B.J., Borowsky W. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Am Acad Pediatr. 2010;125(4):778–786. doi: 10.1542/peds.2009-0597. [DOI] [PubMed] [Google Scholar]
- 22.Webb R.E., Johnson D. The association between aggression, traumatic event exposure and post traumatic stress disorder of looked after young people. Scott J Resid Child Care. 2019;18(3) [Google Scholar]
- 23.National Institute for Health and Care Excellence [NICE]. Looked after children and young people. London: 2021. [PubMed]
- 24.Youth Justice Board. Young People and the Secure Estate: Needs and Interventions; 2013.
- 25.Department of Health. Procedure for the Transfer from Custody of Children and Young People to and from Hospital under the Mental Health Act 1983 in England. London; 2010.
- 26.National Institute for Health and Care Excellence [NICE]. Antisocial Personality Disorder: prevention and management; 2013. [PubMed]
- 27.Rugkasa J. Effectiveness of Community Treatment Orders: The International Evidence. Can J Psychiatry. 2016;61(1):15–24. doi: 10.1177/0706743715620415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaltiala-Heino R., Putkonen H., Eronen M. Why do girls freak out? Exploring female rage among adolescents admitted to adolescent forensic psychiatric inpatient care. J Forensic Psychiatry Psychol. 2013;24:83–110. [Google Scholar]
- 29.Livanou M.I., Bull M., Lane R., D'Souza S., El Asam A., Singh S.P. Transition outcomes for young people discharged from adolescent medium secure services in England: A qualitative study exploring adolescents' and carers' experiences. Clin Child Psychol Psychiatry. 2021;26(4):1227–1242. doi: 10.1177/13591045211026048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wheatley M.D., Long C.G.L., Dolley O. Transitions of females from adolescent secure to adult secure services: A qualitative pilot project. J Ment Health. 2013;22(3):207–217. doi: 10.3109/09638237.2012.705921. [DOI] [PubMed] [Google Scholar]
- 31.Government of Scotland. Independent Forensic Mental Health Review: Interim Report. 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.