Abstract
Background
Dietary patterns influence children and adolescents’ health not only in the present but also in their adulthood. Family characteristics and functioning play a crucial role in food choices and are important modifiable factors for early interventions aimed at preventing unhealthy diets.
Objective
The study aimed to analyze the dietary patterns of Chinese children and adolescents and explore their associations with family characteristics and functioning.
Methods
6276 participants aged 6 to 17 years were recruited for the multicenter cross-sectional study through cluster sampling. Food intake, family characteristics, and family function were assessed. Dietary patterns were identified through factor analysis based on food intake data, and a multiple logistic regression model was used to investigate the associations between dietary patterns, family characteristics, and family functioning.
Results
Three distinct dietary patterns were identified: the “Diverse dietary pattern” (characterized by a rich diet and balanced nutrition), the “Fast food concentrated dietary pattern” (primarily consisting of fried foods, sugary drinks, processed meats, and other junk food), and the “Traditional dietary pattern” (mainly vegetables and grains). Girls, those living in rural areas, and those with better family functioning were more likely to adhere to the “Diverse dietary pattern” (p < 0.01). Girls, primary school students, and those with lower educated mothers tended to have higher adherence to the “Traditional dietary pattern” (p < 0.01). High adherence to the “Fast food concentrated dietary pattern” were associated with boys, older age, Han ethnicity, family dysfunction, living with both parents, being an only-child, having a better educated father, lower family income, and higher pocket money (p < 0.01).
Conclusion
Children and adolescents from different family backgrounds exhibit distinct dietary patterns, highlighting the importance of early screening and intervention tailored to these varying family characteristics. Among the modifiable family factors, better family functioning stands out as a key area of focus for promoting and sustaining healthy dietary patterns in Chinese children and adolescents.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-21068-6.
Keywords: dietary patterns, family function, family characteristics, children, adolescents
Introduction
Dietary patterns primarily focus on the interactions between nutrients and foods [1]. Dietary pattern analysis takes into account the complexity of diets, considering multiple food categories rather than individual foods or nutrients, and can reveal how different nutrients combine with various foods [2, 3]. Among the various methods, factor analysis is one of the most classical approaches to diet pattern analysis [4] with its continuity offering distinct advantages over other methods [5]. As children and adolescents grow, they are prone to developing unhealthy lifestyle behaviors, such as poor dietary habits [6, 7]. These detrimental eating habits are often interconnected, typically beginning in infancy or adolescence and persisting into adulthood [7, 8], with long-term negative effects on health [7]. Similarly, adolescents who adopt unhealthy dietary habits are at a significantly higher risk of becoming overweight or obese [9, 10]. According to recent figures for 2020 [11], approximately 340 million children and adolescents worldwide, aged 5 to 19 years, and over 38 million children under the age of five, were overweight or obese. A study examining the nutritional transition in China over the past decades [12] revealed that the dietary patterns of the Chinese population have undergone a continuous transformation, gradually shifting from a traditional diet focused on vegetables and grains to a modern diet characterized by high intake of refined grains and meat. These significant changes in dietary patterns may contribute to the rise of unhealthy eating habits and obesity among children and adolescents [13].
Furthermore, in a family environment, dietary patterns are established during a child’s early years and are influenced by parental behaviors and family characteristics [14]. Previous studies have shown that adolescent diet quality and nutritional health are closely linked to family factors such as parental education [14–16], family structure [17], number of siblings [17–19], family socioeconomic status [20, 21], and parental age [22]. Previous research has shown that children and adolescents with better family functioning tend to have positive perceptions of their families’ behavior [23], as well as the warmth and love they receive from their parents [24], both of which are associated with healthier eating patterns [25, 26]. Exploring the variability in food choices and dietary habits among adolescents with different family characteristics and functioning can aid in early dietary pattern screening and intervention tailored to diverse family backgrounds. However, existing studies in China are limited by a lack of multicenter research with large sample sizes among children and adolescents. To address this gap, we conducted the current study to investigate the dietary patterns of Chinese children and adolescents and examine their associations with family characteristics and functioning.
Materials and methods
Study design and participants
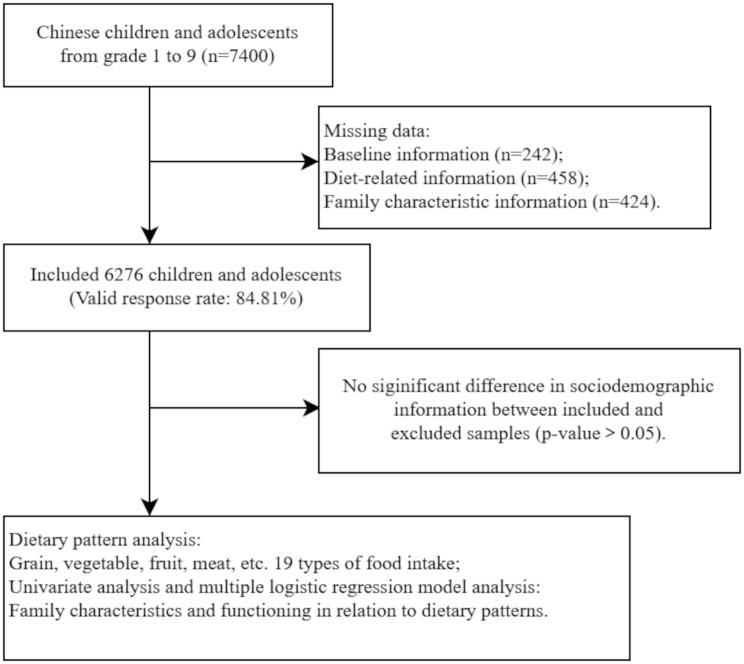
This was a prospective multicenter cross-sectional study conducted in June 2022, as part of the third wave of the Chengdu Positive Child Development (CPCD) survey [27]. Participants included children and adolescents in grades 1 to 9 from 5 primary and secondary schools in Chengdu City, Sichuan Province, China. Cluster sampling method was employed: initially, five public schools located in the city center and the northern and southern suburbs were selected through convenience sampling; subsequently, students in grades 1 through 9 in these schools were recruited. A total of 7400 students were recruited, and 6276 of them completed the study with no missing data, resulting in a valid response rate of 84.81% (Fig. 1). No differences were found in basic information between the included and excluded samples.
Fig. 1.
Flow chart for inclusion of study participants
Data collection
Data collection took place on-site in June 2022 and included both a “Student questionnaire” and a “Parent questionnaire”. Students completed the “Student questionnaire” in the classroom with the assistance of school teachers and researchers, and submitted it directly afterward. The “Parent questionnaire” was taken home by students, completed by their caregivers, and returned to school the following day. Participants voluntarily submitted a printed informed consent form before data collection. To ensure effective and reliable data gathering, all research personnel underwent standardized training before entering the institution, and standardized explanations were provided whenever participants had questions about the items. For the food frequency questionnaire, detailed examples were included for each food category to aid student comprehension. Completion times were approximately 10–20 min for the “Student questionnaire” and 5 min for the “Parent questionnaire”.
Measurement tools
Our data collection tools included a “Student questionnaire” and a “Parent questionnaire”. The “Student questionnaire” comprised 3 sections: sociodemographic information, family function, and food frequency. The “Parent questionnaire” covered sociodemographic information and family characteristics.
The “student questionnaire”
Sociodemographic information
A self-designed data collection form was used to gather students’ sociodemographic information. The form included five items: gender (boy or girl), age (in years), grade (1st to 9th), ethnicity (Han or Minority), and pocket money (≤ 20 yuan per week, 21–50 yuan per week, or > 50 yuan per week).
The Chinese family assessment instrument (C-FAI)
The Chinese Family Assessment Instrument (C-FAI) [28] was used to evaluate family function. This scale consists of 33 items covering seven aspects: parental concern, child filial piety, parental marriage, parental control, communication, conflict, and harmony. The C-FAI score ranges from 33 to 165, with higher scores indicating greater family function. C-FAI has been widely used within the Chinese population, demonstrating strong reliability in China, with Cronbach’s alpha coefficients ranging from 0.93 to 0.98 [29]. It has also been tested in primary school students, including those in lower grades [30].
Food frequency
A simplified version of the Food Frequency Questionnaire (FFQ) was used to retrospectively assess the food intake of the study population over the past month. This included 19 food items based on common dietary foods from the China Food Composition Table [31] and previous studies [32, 33]: refined grains, coarse grains, dark-colored vegetables, light-colored vegetables, melons, berries, citrus fruits, drupe fruits, legumes, nuts, eggs, dairy products, livestock meats, poultry, processed meats, seafood, sugar-sweetened drinks, fried foods, and desserts. Participants reported intake frequency on a five-point scale (≥ 2 times/day, 1 time/day, 3–4 times/week, 1–2 times/week, < 1 time/week), which was recalculated to weekly frequencies (e.g.,1 time/day was converted to 7 times/week).
The “parent questionnaire”
Sociodemographic information
Parental sociodemographic information included three items each for both father and mother: age (in years), education level (middle school or below, high school, technical school, college or above), and occupation (farmer, worker, technical personnel, leader, staff, self-employed, unemployed).
Family characteristics
Familial characteristics included four aspects: residential district (urban or rural), family income (≥ 2000 yuan/month, 2000–5000 yuan/month, 5000-10,000 yuan/month, 10,000–20,000 yuan/month, > 20,000 yuan/month), number of children (one-child or multi-child), and household composition (living with both parents, single parent, or grandparent).
Statistical analysis
Statistical analysis was conducted using SPSS Statistics for Windows, version 26.0. Means and standard deviations (SD) were used to describe numerical variables, and proportion for categorical variables. Dietary patterns were derived using exploratory factor analysis, incorporating 19 food groups. The Kaiser–Meyer–Olkin (KMO) criterion and Bartlett’s test were used to evaluate the data’s suitability for factor analysis. Dietary patterns were identified based on an eigenvalue > 1, factor interpretability, the scree plot, and variance explained > 5%. Patterns were named according to food items with factor loadings greater than 0.5. Factor scores for each pattern were calculated for each individual using principal component analysis with varimax rotation. The median value dichotomized factor scores for each dietary pattern: participants scoring above the median were classified as high adherents, while those below were classified as low adherents.
The Chi-squared test (or analysis of variance) was used to compare the frequency distribution (or mean distribution) of categorical (or continuous) variables. Variables that showed statistical significance in the univariate analysis were included in a multivariable logistic regression model with backward selection to explore independent associations between family characteristics, family function, and dietary patterns. Additionally, based on both data-driven results and theory-based hypotheses, certain variables, such as age and other sociodemographics, were included in the multivariable models regardless of their significance in the univariate analysis. Adjusted odds ratios (OR) with corresponding 95% confidence intervals (CI) were reported. All statistical tests were two-tailed, and a p-value of less than 0.05 was considered statistically significant.
Ethical consideration
This study was reviewed and approved by the Ethics Committee of Sichuan University (K2020025). All study participants volunteered to participate, and both participants and their guardians were informed of the study objectives, procedures, privacy protections, potential risks, and data retention policies before signing informed consent. Participants were also informed of their right to withdraw from the study at any stage without any negative consequences.
Results
Socio-demographics, family characteristics and functioning
A total of 6276 pairs of students and their caregivers completed the entire study. Their demographic information, family characteristics, and family functioning are presented in Table 1. The sample was nearly evenly split between boys (3199 boys, 51%) and girls (3077 girls, 49%), with 99.2% identifying as Han ethnicity. Among the children and adolescents, 4156 were in grades 1 to 6 (66.2%), and 2120 were in grades 7 to 9 (33.8%). The average age of the children and adolescents was 9.7 ± 2.3 years, while the average ages of their fathers and mothers were 38.7 ± 6.0 and 36.1 ± 5.7 years, respectively. The average family functioning score was 59.4 ± 23.6.
Table 1.
Characteristics of the participants (n = 6276)
| Characteristics | n (%) or Mean ± SD |
|---|---|
| Gender | |
| Boy | 3199 (51.0) |
| Girl | 3077 (49.0) |
| Ethnicity | |
| Han | 6223 (99.2) |
| Minority | 53 (0.8) |
| Age (years) | 9.7 ± 2.3 |
| District | |
| Urban | 4172 (66.5) |
| Rural | 2104 (33.5) |
| Education level | |
| Primary school | 4156 (66.2) |
| Middle school | 2120 (33.8) |
| C-FAI a score | 59.4 ± 23.6 |
| Children dimension | |
| Only-child family | 2168 (34.5) |
| Multi-child family | 4108 (65.5) |
| Household composition | |
| Two-parent | 4411 (70.3) |
| Single-parent | 1147 (18.3) |
| Grand-parent | 718 (11.4) |
| Family income (yuan/monthly) | |
| ≤ 2000 | 455 (7.2) |
| 2001–5000 | 1538 (24.5) |
| 5001–10,000 | 2680 (42.7) |
| 10,001–20,000 | 1166 (18.6) |
| > 20,000 | 437 (7.0) |
| Pocket money (yuan/weekly) | |
| ≤ 20 | 4371 (69.6) |
| 21–50 | 1494 (23.8) |
| > 50 | 411 (6.5) |
| Father’s age (years) | 38.6 ± 6.1 |
| Mother’s age (years) | 36.0 ± 5.7 |
| Father’s occupation | |
| Farmer | 578 (9.2) |
| Worker | 2029 (32.3) |
| Technical personnel | 452 (7.2) |
| Leader | 917 (14.7) |
| Staff | 940 (15.0) |
| Self-employed | 1106 (17.6) |
| Unemployed | 254 (4.0) |
| Mother’s occupation | |
| Farmer | 679 (10.8) |
| Worker | 682 (10.9) |
| Technical personnel | 591 (9.4) |
| Leader | 542 (8.6) |
| Staff | 1537 (24.5) |
| Self-employed | 1054 (16.8) |
| Unemployed | 1191 (19.0) |
| Father’s education | |
| Middle school and below | 2743 (43.7) |
| High school | 1600 (25.5) |
| Technical school | 670 (10.7) |
| College and above | 1263 (20.1) |
| Mother’s education | |
| Middle school and below | 2868 (45.7) |
| High school | 1477 (23.5) |
| Technical school | 722 (11.5) |
| College and above | 1209 (19.3) |
Note: Categorical variables are described as n (%) and continuous variables are described as Mean ± SD. a means the Chinese Family Assessment Instrument
The family characteristics of the study participants were as follows: Households in urban areas were about twice as common as those in rural areas. Around two-thirds of the families were multiple-child households (65.5%), and the majority of children and adolescents lived with their parents (70.3%). In terms of financial status, most household had a monthly income below 10,000 yuan. Most children and adolescents received less than 50 yuan in weekly pocket money, with 69.6% receiving less than 20 yuan. The most common occupations for fathers and mothers were workers (32.3%) and staff (24.5%), respectively. It is noteworthy that the fathers’ group included a higher proportion of leaders, while the mothers’ group had a higher percentage of unemployed individuals (16.1%). The educational distribution for fathers and mothers was similar, with approximately half of each group having completed only middle school or less.
Dietary patterns
The Kaiser-Meyer Olkin (KMO) statistic was 0.918, and the p-value for Bartlett’s test of sphericity was less than 0.001, indicating that the dietary frequency data were suitable for factor analysis.
Factor analysis of the reported consumption of 19 food items revealed three distinct dietary patterns, which together explained 59.7% of the total variation. Ten dietary variables loaded onto factor 1, which accounted for 42.2% of the cumulative variance. This pattern was characterized by high intake of various fruits, vegetables, and eggs, followed by higher consumption of nuts, legumes, and dairy products, and was thus named the “Diverse dietary pattern”. Factor 2 had the greatest loading on five variables and explained 11.4% of the cumulative variance. This pattern was associated with a high consumption of processed meats, seafood, fried foods, sugar-sweetened drinks, and desserts, and was termed the “Fast food concentrated dietary pattern”. The third factor, which accounted for 6.1% of the cumulative variance, was mainly composed of grains and vegetables, key components of the traditional Chinese diet, and was named the “Traditional dietary pattern”. The rotated component matrix, eigenvalues, and the proportion of variance explained are presented in Table 2.
Table 2.
Factor-loading matrix for dietary patterns
| Food items | Factors | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Refined grains | 0.085 | 0.170 | 0.756 |
| Coarse grains | 0.187 | 0.153 | 0.719 |
| Dark-colored vegetables | 0.589 | -0.017 | 0.504 |
| Light-colored vegetables | 0.640 | -0.026 | 0.464 |
| Melon fruits | 0.737 | 0.132 | 0.193 |
| Berry fruits | 0.760 | 0.237 | 0.093 |
| Citrus fruits | 0.761 | 0.230 | 0.081 |
| Drupe fruits | 0.699 | 0.343 | 0.070 |
| Legumes | 0.652 | 0.387 | 0.121 |
| Nuts | 0.637 | 0.455 | 0.036 |
| Eggs | 0.661 | 0.204 | 0.178 |
| Dairy products | 0.598 | 0.163 | 0.280 |
| Livestock meats | 0.474 | 0.121 | 0.423 |
| Poultry meats | 0.415 | 0.445 | 0.303 |
| Processed meats | 0.311 | 0.725 | 0.109 |
| Seafood | 0.353 | 0.722 | 0.077 |
| Sugar-sweetened drinks | 0.124 | 0.834 | 0.098 |
| Fried foods | 0.113 | 0.846 | 0.082 |
| Desserts | 0.146 | 0.770 | 0.152 |
| Initial eigenvalues | 8.024 | 2.164 | 1.149 |
| % of cumulative variance | 42.2 | 53.6 | 59.7 |
Note: Boldface represents food items with a factor loading > |0.500|, which are the main contributors and representative of the character of each pattern
Dietary pattern scores by sociodemographic factors and summary of intake for 19 food items
The mean (SD) of dietary pattern scores by participants’ sociodemographic factors are presented in Table 3. For boys, the scores of the “Diverse dietary pattern”, “Fast food concentrated dietary pattern”, and “Traditional dietary pattern” were 0.056 ± 1.038, 0.057 ± 1.037, and 0.060 ± 1.022, respectively. In the girls’ group, these scores were − 0.058 ± 0.952, -0.059 ± 0.943, and 0.063 ± 0.973. The Han Chinese group had higher mean scores on the “Diverse dietary pattern” and lower scores on both the “Fast food concentrated dietary pattern”, and “Traditional dietary pattern” compared to the minority group. Older participants showed the highest mean score on the “Fast food concentrated dietary pattern”, while younger participants had the highest mean score on the “Traditional dietary pattern”. Additionally, participants from urban areas had the highest mean score of 0.032 ± 1.005 on the “Diverse dietary pattern”, whereas those from rural areas had the lowest. Primary school students had the lowest mean score on the “Traditional dietary pattern”, and middle school students had the lowest on the “Fast food concentrated dietary pattern”. Furthermore, Table S1 summarizes the intake of 19 food items and the mean value differences in adherence to each dietary pattern.
Table 3.
Mean (SD) of dietary pattern scores by sociodemographic factors (n = 6276)
| Sociodemographic factors | Diverse dietary pattern scores | Fast food concentrated dietary pattern scores | Traditional dietary pattern scores |
|---|---|---|---|
| Gender | |||
| Boy | 0.056 (1.038) | 0.057 (1.037) | 0.060 (1.022) |
| Girl | -0.058 (0.952) | -0.059 (0.943) | 0.063 (0.973) |
| Ethnicity | |||
| Han | 0.001 (0.999) | -0.002 (0.993) | -0.002 (0.999) |
| Minority | -0.063 (0.921) | 0.195 (1.010) | 0.171 (1.161) |
| Age (years) | |||
| Median & below | -0.002 (1.054) | -0.071 (0.985) | 0.054 (1.039) |
| Above median | 0.002 (0.941) | 0.070 (0.996) | -0.053 (0.958) |
| District | |||
| Urban | 0.032 (1.005) | -0.016 (0.990) | 0.015 (1.007) |
| Rural | -0.062 (0.983) | 0.031 (0.998) | -0.029 (0.987) |
| Education level | |||
| Primary school | -0.003 (0.945) | 0.041 (0.999) | -0.060 (0.961) |
| Middle school | 0.006 (1.097) | -0.081 (0.976) | 0.118 (1.063) |
Note: Dietary pattern scores are described as Mean (SD)
Family characteristics and functioning associated with adherence to dietary patterns
Family characteristics and functioning associated with adherence to the three dietary patterns in the univariate analysis are presented in Table S2. According to the results of multivariable analysis, high adherence to the “Diverse dietary pattern” was significantly correlated with gender, district, C-FAI score, and mother’s occupation (p < 0.05). Children and adolescents living in rural and with better family functioning were more likely to adhere to the “Diverse dietary pattern”. Additionally, children whose mothers were leaders showed higher adherence to the “Diverse dietary pattern” compared to those whose mothers were unemployed. High adherence to the “Fast food concentrated dietary pattern” was associated with gender, age, ethnicity, family type, children’s dimensions, C-FAI score, pocket money, family income and father’s education (p < 0.05). Children and adolescents with high adherence to the “Fast food concentrated dietary pattern” were predominantly of Han ethnicity, older, and more likely to be the only-child. They also tended to have lower monthly family income, more pocket money, poorer family functioning, and higher levels of father’s education. Children living with both parents were more likely to adhere to the “Fast food concentrated dietary pattern” compared to those living with grandparents. High adherence to the “Traditional dietary pattern” was associated with gender, the student’s education level, and mother’s education (p < 0.01). Children and adolescents with high adherence to the “Fast food concentrated dietary pattern” were mostly primary school students and had mothers with lower levels of education. Boys showed higher adherence to the “Fast food concentrated dietary pattern” than girls, while girls exhibited greater adherence to the “Diverse dietary pattern” and the “Traditional dietary pattern”. Table 4 presents the variables associated with dietary pattern adherence in the multivariable analysis.
Table 4.
Factors associated with dietary patterns in multivariable analysis (p < 0.05)
| Dietary pattern | Factor | Multivariable | OR (95% CI) |
|---|---|---|---|
| Diverse dietary pattern | Gender | Boys | 0.86 (0.78, 0.95) ** |
| Girls# | 1.00 | ||
| District | Urban | 0.87 (0.78, 0.98) * | |
| Rural# | 1.00 | ||
| C-FAIa score | above median | 1.34 (1.21, 1.48) *** | |
| Median & below# | 1.00 | ||
| Mother’s occupation | Leader | 1.27 (1.02, 1.58) * | |
| Unemployed# | 1.00 | ||
| Fast food concentrated dietary pattern | Gender | Boys | 1.84 (1.76, 1.93) ** |
| Girls# | 1.00 | ||
| Ethnicity | Han | 2.15 (1.19, 3.89) * | |
| Minority# | 1.00 | ||
| Age (years) | above median | 1.60 (1.38, 1.85) *** | |
| Median & below# | 1.00 | ||
| Household composition | Grand-parent | 0.77 (0.64, 0.94) ** | |
| Two-parent# | 1.00 | ||
| Children dimension | Multi-child family | 0.87 (0.78, 0.98) * | |
| Only-child family# | 1.00 | ||
| Father’s education | High school | 1.24 (1.07, 1.43) ** | |
| Technical school | 1.38 (1.18, 1.61) *** | ||
| College and above | 1.21 (1.00, 1.47) * | ||
| Middle school and below# | 1.00 | ||
| C-FAIa score | above median | 0.58 (0.53, 0.65) *** | |
| Median & below# | 1.00 | ||
| Pocket money (yuan/weekly) | 20–50 | 1.61 (1.49, 1.75) *** | |
| ≤ 20# | 1.00 | ||
| Family income (yuan/monthly) | 5001-10,000 | 0.76 (0.61, 0.95) * | |
| 10,001–20,000 | 0.73 (0.59, 0.90) ** | ||
| > 20,000 | 0.76 (0.60, 0.95) * | ||
| ≤ 2000# | 1.00 | ||
| Traditional dietary pattern | Gender | Boys | 0.83 (0.75, 0.92) *** |
| Girls# | 1.00 | ||
| Education level | Middle school | 0.83 (0.71, 0.97) * | |
| Primary school# | 1.00 | ||
| Mother’s education | High school | 0.82 (0.68, 0.99) * | |
| College and above | 0.75 (0.61, 0.92) ** | ||
| Middle school and below# | 1.00 |
Note: a means the Chinese Family Assessment Instrument. CI, confidence interval. * p < 0.05, ** p < 0.01, *** p < 0.001. # denotes the reference group
Discussions
This prospective multicenter cross-sectional study examined the dietary patterns in relation to different family characteristics and functioning among Chinese children and adolescents, and sought to explore the associations between family factors and adherence to various dietary patterns. Our findings contributed to the existing literature in several ways: three distinct dietary patterns—the “Diverse dietary pattern”, the “Fast food concentrated dietary pattern”, and the “Traditional dietary pattern”—were identified, highlighting the presence of unhealthy dietary patterns and emphasizing the need for regular screening of dietary habits among youth to ensure balanced nutrition. Furthermore, family function and other family characteristics were found to be associated with these patterns, offering insights for targeted interventions to improve children’s nutritional status based on their family backgrounds, while also underscoring the crucial role of family function in children’s nutrition and health.
We identified three types of dietary patterns, which are supported by published evidence. Based on factor analysis, we named the dietary pattern characterized by a balanced higher consumption of vegetables, fruits, nuts, legumes, eggs, and dairy products the “Diverse dietary pattern”. This aligns with findings from previous studies [34–36]. Such dietary patterns have previously been referred to “vegetables and fruits”, “nutritional” or “protective” dietary patterns [19, 37, 38], all of which emphasize the health benefits of these diets. In contrast, the “Fast food concentrated dietary pattern” identified in our study was characterized by a higher intake of processed meats, seafood, sugar-sweetened drinks, fried foods, and desserts-foods that are highly popular among adolescents and children. Other researchers have similarly labeled this dietary pattern as “risky”, “Western”, or “junk food” [38–40], as it includes processed foods, sugary substances and fried foods, all of which have a known negative influence on the growth and development of children and adolescents. Finally, the “Traditional dietary pattern” was characterized by a higher consumption of vegetables and grains. In the traditional Chinese diet, vegetables and grains play a central role, with variations in the types of coarse grains, refined grains, and vegetables chosen by different families [13].
Consistent with previous studies [41, 42], we found that boys were more likely to adhere to the “Fast food concentrated dietary pattern”, while girls showed greater adherence to the “Diverse dietary pattern” and the “Traditional dietary pattern”. Due to changes in hormone levels and physical development, boys were generally more active in their food choices and consumption, particularly favoring processed foods and sugar-sweetened drinks that are high in calories, sugar, and salt [43, 44]. During adolescence, girls tended to focus more on healthy eating and maintaining a slim body, often driven by concerns about their appearance and body shape [36, 45]. Several studies [42, 46] have also supported the conclusion that youth age is positively correlated with adherence to the “Fast food concentrated dietary pattern”. Junk foods such as desserts, sugary drinks, and fried foods are particularly appealing to children [47], while Chinese parents often believed that younger children need to consume more grains and vegetables due to their growth and development needs [48]. This belief also explains why primary school students were more likely to follow the “Traditional dietary pattern” than middle school students.
Family plays a crucial role in shaping the dietary patterns of children and adolescents [38]. C-FAI scores were positively correlated with the “Diverse dietary pattern” and negatively correlated with the “Fast food concentrated dietary pattern”. This suggests that children experiencing more familial dysfunction are more likely to adopt poor dietary habits. A qualitative study from Chile [49], conducted in a low socioeconomic context, indicated that family relationships and food practices are complex phenomena. It found that families in which members were better able to express emotions and feelings often derive greater health benefits from their food choices.
The varying roles of parents in child health have been described in previous studies [38, 42, 50]. Our findings show that children with fathers who have higher levels of education were more likely to adhere to the “Fast food concentrated dietary pattern”. In contrast, children and adolescents with less educated mothers were more inclined to follow the “Traditional dietary pattern”, while those with mothers of higher social status were more likely to follow the “Diverse dietary pattern”. Several studies [22, 51] have reached similar conclusions, highlighting that parental literacy and cultural knowledge are foundational to good dietary quality and nutrition for children and are significantly associated with better parental feeding practices. Similarly, a study by G Appannah et al. [15] found that lower-educated women tended to have less diversity in child feeding and were more likely to adhere to dietary practices rooted in tradition. A systematic review [52] indicated that the level of economic development in a country affects the relationship between education and obesity, with lower-income countries showing a stronger positive correlation. Additionally, children and adolescents in rural areas were more likely to follow the “Diverse dietary pattern” than those in urban areas, likely due to the availability of healthier, more diverse natural foods [53].
In contrast to other research findings [16, 54, 55], our study found that students living with parents were more likely to adopt the “Fast food concentrated dietary pattern” than those living with grandparents. Tara et al. [56] pointed out that parental stress and parenting-related stress were each significantly associated with children’s fast-food consumption, particularly among younger parents. The amount of children’s weekly allowance was positively associated with a tendency for unhealthy eating patterns, which aligns with the conclusions of a three-year longitudinal study of Chinese adolescents [48] which found that an increased allowance was linked to a higher risk of adopting the “Fast food concentarted dietary pattern” as well as overweight and obesity. Our study also found that children from higher-income families had lower adherence to the “Fast food concentrated dietary pattern”. Shi et al. [38] noted that families with higher incomes likely have better consumption levels, offering a greater variety of food options, thus improving the overall quality of children’s eating habits and nutritional intake. Furthermore, this study found that children from one-child families were more likely to adhere to the “Fast food concentrated dietary pattern”. This finding is consistent with the findings of Gao et al. [57], who found that children from one-child families consumed more high-sugar and high-fat foods. However, it contrasts with, Meller et al. [19], who concluded that the number of siblings was positively correlated with adherence to the junk food pattern.
Strengths and limitations
The strength of this study lies in its large sample size and the use of whole-group sampling, which included schools from different orientations and levels of economic development in the region, ensuring better sample representation. Additionally, we collected valuable data on important adolescent behaviors and current dietary habits, including the frequency of food intake. The questionnaire included questions for both parents and students, which enhanced the breadth, accuracy, and completeness of the data collected. This approach allowed us to describe children’s family characteristics and functioning in detail and to explore the mechanisms linking these family factors to their dietary patterns. Ultimately, this study provides valuable insights and evidence to inform future recommendations and interventions focused on diet and health for adolescents from diverse family backgrounds and functioning.
However, there were several limitations to our study. Firstly, students were asked to recall their food frequency over the past month, which may have introduced recall bias. Secondly, this study recruited participants using a whole cluster sampling method in Chengdu City, Sichuan Province, Southwest China. Compared to simple random sampling, cluster sampling may introduce larger sampling errors, and the limited geographic and cultural scope of our sample may constrain the generalizability of these findings. Therefore, caution is advised when applying these results to other regions in China with differing economic and cultural backgrounds. Additionally, school lunches were provided to participants. Although the influence of these meals may be limited due to the similarity in food options, future studies should aim to clarify and minimize this factor as much as possible. Thirdly, the proportion of younger children in our sample might lead to inaccuracies in completing the self-administered questionnaires. While no critical concerns arose during the data collection, future research should consider incorporating objective measurements, such as nutritional markers. Lastly, our study was conducted in June 2022, during the ongoing COVID-19 pandemic. Although schools, workplaces, and daily life were not as strictly confined by the Chinese government as before, public fear of the pandemic may have influenced our results, suggesting the need for future longitudinal research to further explore these factors.
Conclusions
Overall, this study highlights the dietary patterns associated with different family characteristics and functioning among Chinese children and adolescents, contributing to the understanding of the link between family factors and dietary habits. The identification of three distinct dietary patterns—the “Diverse dietary pattern”, the “Fast food concentrated dietary pattern”, and the “Traditional dietary pattern”—underscores the importance of routine screening for dietary patterns, considering the diverse family backgrounds of children and adolescents, to promote balanced nutrition and health. Additionally, improving family functioning should prioritized in efforts to help Chinese children and adolescents establish and maintain healthy dietary patterns.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Author contributions
SQ Luo, SJ Liao and BR Luo were responsible for the study conception, design and methodology; SQ Luo and SJ Liao analyzed data and wrote the paper; L Zhao provided this data; WL Ma was responsible for the data curation; AQ Xiong provided constructive suggestions; BR Luo and L Zhao were responsible for reviewing and editing. All authors have reviewed and approved the published version of the manuscript.
Funding
This research was funded by the Hong Kong Polytechnic University (grant number 19H0642) and the Science and Technology Department of Sichuan Province, China (grant number 2020JDKP0021).
Data availability
Data detailed in the manuscript will not be made publicly available because private information of participants was included, but are available upon request from the corresponding author.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was carried out in compliance with the Helsinki Declaration, and it was authorized by Sichuan University’s Ethics Committee with registration number K2020025.
Consent to participate
All participants were volunteered to participate in this study survey.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shiqi Luo and Shujuan Liao contributed equally as the first author.
Contributor Information
Biru Luo, Email: hxnurs@163.com.
Li Zhao, Email: zhaoli@scu.edu.cn.
References
- 1.Newby PK, Tucker KL. Empirically Derived Eating Patterns Using Factor or Cluster Analysis: A Review. Nutr Rev. 2004;62(5):177–203. [DOI] [PubMed] [Google Scholar]
- 2.Shu L, Shen XM, Li C, Zhang XY, Zheng PF. Dietary patterns are associated with type 2 diabetes mellitus among middle-aged adults in Zhejiang Province, China. Nutr J. 2017;16(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Horn L. Eating pattern analyses: the whole is more than the sum of its parts. J Am Diet Assoc. 2011;111(2):203. [DOI] [PubMed] [Google Scholar]
- 4.Hong X, Ye Q, Wang Z, Yang H, Chen X, Zhou H, Wang C, Chu W, Lai Y, Sun L, et al. Reproducibility and validity of dietary patterns identified using factor analysis among Chinese populations. Br J Nutr. 2016;116(5):842–52. [DOI] [PubMed] [Google Scholar]
- 5.DiBello JR, Kraft P, McGarvey ST, Goldberg R, Campos H, Baylin A. Comparison of 3 methods for identifying dietary patterns associated with risk of disease. Am J Epidemiol. 2008;168(12):1433–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, Mitra R, O’Reilly N, Spence JC, Vanderloo LM, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Activity. 2020;17(1):85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pujia R, Ferro Y, Maurotti S, Khoory J, Gazzaruso C, Pujia A, Montalcini T, Mazza E. The Effects of COVID-19 on the Eating Habits of Children and Adolescents in Italy: A Pilot Survey Study. 2021, 13(8):2641. [DOI] [PMC free article] [PubMed]
- 9.Herrera A, Sarmiento C. Overweight and obesity: Family factors, diet, and physical activity in school children from middle to high socioeconomic level in Cali, Colombia. Biomedica: revista del Instituto Nac de Salud. 2022;42(Sp 1):100–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, Jia P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes. 2020;10(6):e12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Organization WH. Obesity and overweight. 2020.
- 12.Huang L, Wang Z, Wang H, Zhao L, Jiang H, Zhang B, Ding G. Nutrition transition and related health challenges over decades in China. Eur J Clin Nutr. 2021;75(2):247–52. [DOI] [PubMed] [Google Scholar]
- 13.Zhen S, Ma Y, Zhao Z, Yang X, Wen D. Dietary pattern is associated with obesity in Chinese children and adolescents: data from China Health and Nutrition Survey (CHNS). Nutr J. 2018;17(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Durão C, Severo M, Oliveira A, Moreira P, Guerra A, Barros H, Lopes C. Association of maternal characteristics and behaviours with 4-year-old children’s dietary patterns. Matern Child Nutr 2017, 13(2). [DOI] [PMC free article] [PubMed]
- 15.Appannah G, Pot GK, Oddy WH, Jebb SA, Ambrosini GL. Determinants of a dietary pattern linked with greater metabolic risk and its tracking during adolescence. J Hum Nutr dietetics: official J Br Diet Association. 2018;31(2):218–27. [DOI] [PubMed] [Google Scholar]
- 16.Yan SQ, Cao H, Gu CL, Xu YQ, Ni LL, Tao HH, Shao T, Tao FB. [Dietary patterns among preschoolers and its association with education level of the parents]. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2017;38(8):1060–3. [DOI] [PubMed] [Google Scholar]
- 17.Barros L, Lopes C, Oliveira A. Child and family characteristics are associated with a dietary variety index in 4-year-old children from the Generation XXI cohort. Nutr Res (New York NY). 2019;63:76–85. [DOI] [PubMed] [Google Scholar]
- 18.Golley RK, Hendrie GA, McNaughton SA. Scores on the dietary guideline index for children and adolescents are associated with nutrient intake and socio-economic position but not adiposity. J Nutr. 2011;141(7):1340–7. [DOI] [PubMed] [Google Scholar]
- 19.Meller FO, Assunção MC, Schäfer AA, Loret de Mola C, Dahly DL, Vaz JS, Barros FC. Is the number of siblings associated with dietary patterns in adolescents? The 1993 birth cohort of Pelotas (Brazil). PLoS ONE. 2017;12(3):e0174087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, Wickramasinghe K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Global health. 2017;5(3):e277–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott JA, Chih TY, Oddy WH. Food variety at 2 years of age is related to duration of breastfeeding. Nutrients. 2012;4(10):1464–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leventakou V, Sarri K, Georgiou V, Chatzea V, Frouzi E, Kastelianou A, Gatzou A, Kogevinas M, Chatzi L. Early life determinants of dietary patterns in preschool children: Rhea mother-child cohort, Crete, Greece. Eur J Clin Nutr. 2016;70(1):60–5. [DOI] [PubMed] [Google Scholar]
- 23.Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 1988;27(1):97–104. [DOI] [PubMed] [Google Scholar]
- 24.Colón-Ramos U, Monge-Rojas R, Smith-Castro V, Wang J, Cheng YI, Perreira KM, Van Horn L, Sotres-Alvarez D, Isasi CR, Gallo LC. Family function and eating behaviours among Hispanic/Latino youth: results from the Hispanic Community Children’s Health Study/Study of Latino Youth (SOL Youth). Public Health Nutr. 2021;24(5):924–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Renzaho AM, Dau A, Cyril S, Ayala GX. The influence of family functioning on the consumption of unhealthy foods and beverages among 1- to 12-y-old children in Victoria, Australia. Nutr (Burbank Los Angeles Cty Calif). 2014;30(9):1028–33. [DOI] [PubMed] [Google Scholar]
- 26.Renzaho AM, Kumanyika S, Tucker KL. Family functioning, parental psychological distress, child behavioural problems, socio-economic disadvantage and fruit and vegetable consumption among 4–12 year-old Victorians, Australia. Health Promot Int. 2011;26(3):263–75. [DOI] [PubMed] [Google Scholar]
- 27.Zhao L, Shek DTL, Zou K, Lei Y, Jia P. Cohort Profile: Chengdu Positive Child Development (CPCD) survey. Int J Epidemiol. 2022;51(3):e95–107. [DOI] [PubMed] [Google Scholar]
- 28.Siu AM, Shek DT. Psychometric properties of the Chinese Family Assessment Instrument in Chinese adolescents in Hong Kong. Adolescence. 2005;40(160):817–30. [PubMed] [Google Scholar]
- 29.Shek DTL, Ma CMS. The Chinese Family Assessment Instrument (C-FAI): Hierarchical Confirmatory Factor Analyses and Factorial Invariance. Res Social Work Pract. 2009;20(1):112–23. [Google Scholar]
- 30.Shek DTL, Leung KH, Li X, Dou D. Psychometric properties of the Chinese Family Assessment Instrument: evidence from mainland China. Front Psychol. 2023;14:1290224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang Yuexin WG. He Mei.: China food composition tables. Peking University Medical Press; 2019.
- 32.Gu Q, Wu Y, Feng Z, Chai Y, Hou S, Yu Z, Shen X. Dietary pattern and precocious puberty risk in Chinese girls: a case-control study. Nutr J. 2024;23(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang H, Herforth AW, Xi B, Zou Z. Validation of the Diet Quality Questionnaire in Chinese Children and Adolescents and Relationship with Pediatric Overweight and Obesity. Nutrients 2022, 14(17). [DOI] [PMC free article] [PubMed]
- 34.Shang X, Li Y, Liu A, Zhang Q, Hu X, Du S, Ma J, Xu G, Li Y, Guo H, et al. Dietary pattern and its association with the prevalence of obesity and related cardiometabolic risk factors among Chinese children. PLoS ONE. 2012;7(8):e43183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abbasi K, Beigrezai S, Ghiasvand R, Pourmasoumi M, Mahaki B. Dietary Patterns and Attention Deficit Hyperactivity Disorder Among Iranian Children: A Case-Control Study. J Am Coll Nutr. 2019;38(1):76–83. [DOI] [PubMed] [Google Scholar]
- 36.Kanellopoulou A, Kosti RI, Notara V, Antonogeorgos G, Rojas-Gil AP, Kornilaki EN, Lagiou A, Yannakoulia M, Panagiotakos DB. Dietary Patterns, Weight Perception and Obesity Status, among 10-12-Year-Old Children; an Epidemiological Study in Greece. Child (Basel Switzerland) 2021, 8(8). [DOI] [PMC free article] [PubMed]
- 37.Naja F, Hwalla N, Itani L, Karam S, Sibai AM, Nasreddine L. A Western dietary pattern is associated with overweight and obesity in a national sample of Lebanese adolescents (13–19 years): a cross-sectional study. Br J Nutr. 2015;114(11):1909–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shi XR, Chen TJ, Ma J. [Analysis of family influencing factors of dietary behavior pattern of children and adolescents]. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2020;41(8):1291–5. [DOI] [PubMed] [Google Scholar]
- 39.Sogari G, Velez-Argumedo C, Gómez MI, Mora C. College Students and Eating Habits: A Study Using An Ecological Model for Healthy Behavior. Nutrients 2018, 10(12). [DOI] [PMC free article] [PubMed]
- 40.Trujillo-Mayol I, Guerra-Valle M, Casas-Forero N, Sobral MMC, Viegas O, Alarcón-Enos J, Ferreira IM, Pinho O. Western Dietary Pattern Antioxidant Intakes and Oxidative Stress: Importance During the SARS-CoV-2/COVID-19 Pandemic. Adv Nutr (Bethesda Md). 2021;12(3):670–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kafeshani O, Sarrafzadegan N, Nouri F, Mohammadifard N. Major dietary patterns in Iranian adolescents: Isfahan Healthy Heart Program, Iran. ARYA atherosclerosis. 2015;11(Suppl 1):61–8. [PMC free article] [PubMed] [Google Scholar]
- 42.Kotova MB, Maksimov SA, Drapkina OM. Gender, Age, Family and Territorial Features of Dietary and Physical Activity Patterns in Russian Youths. Int J Environ Res Public Health 2022, 19(9). [DOI] [PMC free article] [PubMed]
- 43.Mescoloto SB, Pongiluppi G, Domene S. Ultra-processed food consumption and children and adolescents’ health. Jornal de pediatria. 2024;100(Suppl 1):S18–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Monzani A, Ricotti R, Caputo M, Solito A, Archero F, Bellone S, Prodam F. A Systematic Review of the Association of Skipping Breakfast with Weight and Cardiometabolic Risk Factors in Children and Adolescents. What Should We Better Investigate in the Future? Nutrients 2019, 11(2). [DOI] [PMC free article] [PubMed]
- 45.Schnettler B, Grunert KG, Lobos G, Miranda-Zapata E, Denegri M, Ares G, Hueche C. A latent class analysis of family eating habits in families with adolescents. Appetite. 2018;129:37–48. [DOI] [PubMed] [Google Scholar]
- 46.He Y, Luo B, Zhao L, Liao S. Influences of the COVID-19 Pandemic on Obesity and Weight-Related Behaviors among Chinese Children: A Multi-Center Longitudinal Study. Nutrients 2022, 14(18). [DOI] [PMC free article] [PubMed]
- 47.Liao X, Chen S, Su M, Zhang X, Wei Y, Liang S, Wei Q, Zhang Z. The Relationship between Dietary Pattern and Bone Mass in School-Age Children. Nutrients 2022, 14(18). [DOI] [PMC free article] [PubMed]
- 48.Ma L, Fang Z, Gao L, Zhao Y, Xue H, Li K, Wang Y. A 3-year Longitudinal Study of Pocket Money, Eating Behavior, Weight Status: The Childhood Obesity Study in China Mega-Cities. Int J Environ Res Public Health 2020, 17(23). [DOI] [PMC free article] [PubMed]
- 49.Cuevas C, Herrera P, Morales G, Aguayo L, Galvez EP. Understanding the food-family relationship: A qualitative research in a Chilean low socioeconomic context. Appetite. 2021;156:104852. [DOI] [PubMed] [Google Scholar]
- 50.Liu Y, Ma Y, Jiang N, Song S, Fan Q, Wen D. Interaction between Parental Education and Household Wealth on Children’s Obesity Risk. Int J Environ Res Public Health 2018, 15(8). [DOI] [PMC free article] [PubMed]
- 51.Costarelli V, Michou M, Panagiotakos DB, Lionis C. Parental health literacy and nutrition literacy affect child feeding practices: A cross-sectional study. Nutr Health. 2022;28(1):59–68. [DOI] [PubMed] [Google Scholar]
- 52.Cohen AK, Rai M, Rehkopf DH, Abrams B. Educational attainment and obesity: a systematic review. Obes reviews: official J Int Association Study Obes. 2013;14(12):989–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu Y, Liu C, Chen K, Li S. Parental migration and children’s dietary diversity at home: Evidence from rural China. PLoS ONE. 2023;18(12):e0291041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berge JM, Hoppmann C, Hanson C, Neumark-Sztainer D. Perspectives about family meals from single-headed and dual-headed households: a qualitative analysis. J Acad Nutr Dietetics. 2013;113(12):1632–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tan BQM, Hee JM, Yow KS, Sim X, Asano M, Chong MF. Feeding-Related Knowledge, Attitudes, and Practices among Grandparents in Singapore. Nutrients 2019, 11(7). [DOI] [PMC free article] [PubMed]
- 56.Bautista T, Fogelman N, Lartigue S, Silverman WK, Jastreboff AM, Sinha R. Association between specific types of parent stressors and fast-food consumption among parents and children. Eat Behav. 2023;49:101724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gao D, Li Y, Yang Z, Ma Y, Chen M, Dong Y, Zou Z, Ma J. The Association Between Single-Child Status and Risk of Abdominal Obesity: Result From a Cross-Sectional Study of China. Front Pead. 2021;9:697047. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data detailed in the manuscript will not be made publicly available because private information of participants was included, but are available upon request from the corresponding author.