Abstract
Objectives
Transition from pediatric to adult health services is a difficult and common problem in many medical specialties, particularly in mental health, fraught with pitfalls that threaten its success and disrupt the continuity of care. However, there is a lack of research on this topic. The aim of this study was to characterize the perceptions of Portuguese physicians who are responsible for direct intervention in this process—child and adolescent psychiatrists (CAP) and adult psychiatrists (AP)—and to explore the possibilities for improvement.
Methods
A qualitative methodology was adopted, using thematic analysis to evaluate results, participants were selected using a convenience sampling of CAPs and APs in Lisbon area, 28 APs and 18 CAPs expressed interest in participating.
Saturation point was reached after interviewing eight CAPs and 13 APs, and the interviews were first listened to and transcribed, then NVivo software was used to facilitate coding of data.
Results
Many young people transition informally to adult services. Relying on the commitment of doctors, families, and patients is common in clinical discharge to general practitioners, who then make psychiatric referrals. A formal and standardized transition process was not found. Two-thirds of the respondents thought that transition services were useful, while others thought that such services were not needed and had no positive effect on the quality of care. However, all agreed that in the absence of transition protocols, informal transfers provided the best results.
Conclusions
All participants agreed on the importance of a seamless transition to ensure the continuity of care and that developing transition strategies to improve communication between pediatric and adult services would be beneficial. Some participants considered this issue for the first time. This suggests that the situation in Portugal is similar to that in other countries, highlighting a lack of awareness of the importance of transition process for patient outcomes.
Keywords: adolescent psychiatry, adult psychiatry, transition process, care continuity, Portugal, qualitative study
Graphical Abstract
1. Introduction
The transition process should focus on the medical, psychosocial, and educational/vocational needs of adolescents and young adults with chronic illnesses when they move from pediatric to adult health services,1 However, the process is not followed in the majority of situations; McPheeters2 found that in the US, approximately 750,000 young people transition to adult services each year across all medical specialties, but only less than half transition successfully. The percentage is even lower for people with mental illness,3 with the age group of 16–18 years being particularly vulnerable.4
A transition process creates the circumstances to preventively address the risks with evidence-based interventions5. However, engagement between mental health services is disproportionately low for patients in this age group,6, 7 suggesting a failure to recognize their specific need because they are neither children, nor fully adults.8
The development of transition services is important because a traditional organization of mental health services is faced with challenges in transition as the needs of those moving from pediatric to adult health services are not thoroughly considered.1 Consequently, they may not find an equivalent in adult services and the continuity of care is lost, with breaks in treatment and the potential for consequent decompensation resulting in negative consequences.
Therefore, a strategically planned transition process should be designed5 allowing for earlier intervention.9 New challenges, such as the COVID-19 pandemic with increased isolation and the number of transitional age youth (TAY) affected, have led to the emergence of new techniques, such as telemedicine, to respond to these issues.10 However, many physicians still have difficulties in considering transition as a process with therapeutic purposes, confusing transfer—a bureaucratic process (a person is discharged from one service to another when they reach the age of 18)—with transition—that aims to ensure continuity of care and coordination with interagency service systems (i.e. education, employment and community living).11, 12
In Portugal, child and adolescent psychiatry and adult psychiatry are specialties with their own status, operating autonomously and using different intervention methods, with little exchange between them, even if they are physically located in the same hospital. Therefore, the transition of young people from one specialty to another may not be without challenges as communication between the two is hampered by a lack of protocols or other ways of streamlining the exchange of clinical information.
The outcomes of the transition process in Portugal are unknown. However, given the lack of global literature on the subject and lack of transition protocols, we thought it would be of great interest to know the reality in Portugal, because of the impact that a poorly planned transition has on the prognosis of the disease. Breaks in treatment continuity leads to young people lost in transition.13 Many adult services are unsure of how to deal with TAY, even in terms of the characteristics of the illnesses they present (they have more experience with older people than with TAY).14 Therefore, the establishment of rigid age boundaries in the organization of services and a lack of protocols to allow a seamless transition between services are important reasons for the creation of transition services,15 which can reduce the loss of treatment continuity, the duration of untreated illness (DUP) and morbidity,13 in others areas of health, not just mental illness.12
This study aimed to characterize the perceptions of Portuguese child and adolescent and adult psychiatrists about the transition process in mental health and the possibilities for improvement.
2. Methods
The development of the interview guide began with in-depth research of articles and books about the transition of services in several medical specialties when people reach adulthood, with a greater emphasis on Psychiatry. Then, interview scripts were developed and discussed, with meetings and exchange of ideas with child psychiatrists and adult psychiatrists working in a transition service in Lisbon, which at that time had more than two years of experience in the field. These physicians mentioned the main difficulties they had when treating patients between the ages of 16 and 20 years old who had already been through other services and gave suggestions for more consistent questions.
From this exchange of ideas with those doctors, who did not take part in the interviews that were latter included in the study, a first draft of the questions to be applied was built, pointing to the need for small differences in the questions for AP’s and CAP’s.
Their input assisted with the development of interview topics, which were adapted for each specialty group as presented in Table 1.
Table 1.
Examples of the differences between questions for CAPs and APs interviews.
|
Experience of child psychiatric services CAPs – “Referring to situations you are familiar with professionally, do you know when these young people were first seen by you? (How old was the patient, who referred them, and did anyone else see them before you?” APs – “What do you usually do when a young person who has been seen for the first time in child and adolescent psychiatry comes to your consultation/hospital and is transferred to adult psychiatry?” Period of transition CAPs – “Referring to situations with which you are professionally familiar, do you think that, in general, young people who are referred to child psychiatry have clinical reasons for being referred?” APs – “Referring to situations with which you are professionally familiar, do you think that, in general, adolescents who are referred from child psychiatry to adult psychiatry have an advantage in most situations?” First experiences in the adult psychiatric service CAPs and APs - In your opinion, what are the differences between adolescent and adult psychiatric services?; What do you think are the best and worst points? Impact of transition CAPs and APs - In your opinion, do you think that the change in the type of service where the patient is followed has a significant impact on them? As far as you know, do you think that there are often breaks or long gaps in follow-up when this transition is made? Thoughts about the existence of transition services CAPs and APs - Do you think it would be advantageous to have transitional services, where technicians with experience in child psychiatry and technicians with experience in psychiatry would work, looking after people between the ages of 15 and 25, ensuring continuity of care and preparing for the change of services? Why? In some questions, if felt it was relevant, we could follow up with other questions, such as Can you tell me more about this? Can you give me an example of what you said? How did you feel about it? |
Invitations were sent to potential participants in AP and CAP services of eight hospitals in the Lisbon area; 28 APs and 18 CAPs responded affirmatively to participate in the study. Ultimately, the number of doctors to be interviewed was determined by data saturation.16, 17, 18, 19, 20
2.1. Study design and participants
Qualitative methodology using a thematic approach emerged as the most appropriate for our purpose because it aims to describe and understand particular experiences rather than to predict them; therefore, it was suitable for this study, given that the research topic is little known in Portugal and that it is important to understand the contours and characteristics of the dynamics involved.
A convenience sampling was used, and semi-structured interviews were conducted with psychiatrists from the public health sector in the district of Lisbon.
2.2. – Interviews
The same interviewer conducted all interviews. The interview questions (11 open-ended questions) were derived from two main research questions:
-
1.
What are the doctors’ experiences in transition from child psychiatric services to psychiatry in terms of planning, collaboration between services, and intervention strategies?
-
2.
How do the professionals think that the introduction of a service specializing in the treatment of people aged 15–25 would change the realities of the transition process?
The study was conducted over a 12-month period in 2020 and included psychiatrists working in different locations, as shown in Table 2, Table 3, the number of doctors to be interviewed was determined by the saturation point17, 18, 19, 20, 21 that was reached after interviewing eight CAPs and 13 APs and an inductive thematic saturation was used for the threshold.
Table 2.
ADULTS PSYCHIATRISTS INTERVIEWED (AP).
| AGE | GENDER | Professional Experience (years) | HOSPITAL | |
|---|---|---|---|---|
| AP – 1 | 42 | F | 11 | GENERAL |
| AP – 2 | 34 | M | 4 | PSYCHIATRIC |
| AP – 3 | 59 | F | 30 | GENERAL |
| AP – 4 | 38 | M | 7 | PSYCHIATRIC |
| AP – 5 | 65 | F | 31 | PRIVATE; NGO |
| AP – 6 | 34 | M | 4 | GENERAL |
| AP – 7 | 38 | F | 7 | PSYCHIATRIC |
| AP – 8 | 32 | M | 2 | PSYCHIATRIC |
| AP – 9 | 42 | F | 10 | PSYCHIATRIC |
| AP – 10 | 59 | F | 23 | GENERAL |
| AP – 11 | 40 | F | 9 | PSYCHIATRIC |
| AP – 12 | 37 | F | 5 | PSYCHIATRIC |
| AP – 13 | 63 | M | 31 | GENERAL |
| AVERAGE | 44,8 | 13,4 |
Table 3.
CHILD AND ADOLESCENT PSYCHATRISTS INTERVIEWED (CA).
| AGE | GENDER | Professional Experience (years) | HOSPITAL | |
|---|---|---|---|---|
| CA – 1 | 63 | F | 31 | CENTRAL |
| CA – 2 | 58 | F | 25 | REGIONAL |
| CA – 3 | 47 | F | 16 | CENTRAL |
| CA – 4 | 55 | M | 23 | REGIONAL |
| CA – 5 | 34 | F | 4 | CENTRAL |
| CA – 6 | 33 | M | 2 | REGIONAL |
| CA – 7 | 38 | F | 4 | CENTRAL |
| CA – 8 | 49 | F | 18 | REGIONAL |
| AVERAGE | 47,1 | 15,4 |
All interviews were conducted in the hospital and were recorded.
2.3. Sample
The eight CAPs—six women and two men—had an average age of 47.1 years (range 33–63 years) and 15.4 years of professional experience as a specialist (range: 2–31 years). The 13 APs—eight women and five men—had an average age of 44.8 years (range: 32–65 years) and 13.4 years of professional experience as a specialist (range: 2—31 years). An informed consent form was presented to each participant, who read and signed it, after being assured that the data collected in the interviews would be anonymous, with no personal identifiable information, and that the interview recording would be deleted after data collection.
2.4. - Data analysis
Thematic analysis (TA)21 was considered the most appropriate method of data analysis, as it was a qualitative method that aimed to identify, analyze, and report patterns (themes) in the data22 and is achieved by discovering recurring themes in the text. It allows the emergence of themes not anticipated by the interviewer, facilitating the perception of what child and adolescent psychiatrists (CAPs) and adult psychiatrists (APs) understand by transition and its meaning for TAY.23
Each interview lasted between 25 and 35 minutes and was analyzed by reading the transcript. The data were analyzed by the researcher, that listened to the recordings and transcribed the responses and their nuances, identifying the main themes with the support of another researcher experienced in qualitative analysis. The entire process of analysis was carried out jointly with a discussion of ideas, and it was always possible to reach a consensus accepted by both sides. NVivo software (NVivo 12) was used to provide an organized template of data extraction. Analysis began as each one was completed, the interviews were the sole source of data collection and were transcribed verbatim24 and codes were defined after the interviews were completed.
The interviewees discussed their perceptions of the transition process, its impact on disease progression, and whether a transition service involving both CAPs and APs would add value.
3. Results (main themes)
Data analysis revealed three main themes (transition, adult psychiatry, and adolescent psychiatry) with 12 sub-themes; five from “transition,” three from “adult psychiatry,” and four from “adolescent psychiatry.”
Table 4.
THEMES and SUBTHEMES.
| Transition |
No formal transition Realized informal transition Impact of transition on the patient's life Existence of a transition service Other suggestions for improvement |
| Adult Psychiatry |
Follow up Patient's adaptation process Inpatient services |
| Child Psychiatry |
Follow up Working model Referrals that do not make sense Family participation |
3.1. Transition
Participants described transitions can be either formal or informal. One of the types described was formal transition that implies clinical discharge from CAP to AP psychiatry consultation with no contact between the services involved. Informal transition implies an informal and direct transition. Communication between services is handled in different ways. Experiences in the transition phase vary due to these types of formal and informal transition outcomes.
Respondents did not identify organized, formal transition programs that included protocols, regular meetings between the adolescent service and the adult service or other consolidated forms of communication between services or hospitals.
The sub-themes in “Transition” were: No formal transition (clinical discharge), realized informal transition, impact of transition on the patient's life (how does the change affect the patient and their life?), existence of a transition service (suggestions for improvement) and other suggestions for improvement
3.1.1. No formal transition (clinical discharge)
Most patients are informed of their discharge, usually by the doctor in charge, at the last visit or just before the last visit and there is an abrupt and sudden interruption of treatment; “Sometimes they don’t know why they are in a psychiatric service” told an AP and another one strengthened this idea by deepening it “many patients come particularly poorly referred and most of the time, without even understanding why, because the reasons for clinical discharge were not adequately explained to the patients.” In most cases, they were referred to general practitioners (GPs). Only in cases of serious illness, a greater care was taken to ensure transition "Sometimes they ended up booking faster, it happened a few times, because they saw that it was a really serious situation" (CAP).
3.1.1.1. Often the discharge to the family doctor is the beginning of the "loss of the patient in the system" - a phrase frequently used by the professionals interviewed. “In cases where the connection to the adult service is poor or non-existent (they are often from another geodemographic area) there is difficulty in booking a psychiatry appointment and a clinical discharge is made to Primary Health Care” (CAP). Loss can happen in different phases and involves breakdowns in treatment because of several reasons: the patient is discharged with only verbal information to contact the family doctor or is informed about the need to continue treatment and the doctor-in-charge writes a card to the GP
As respondents noted, too much time elapses between consultation with the GP and the AP, so the information about the patient is lost, from CAP to GP or from GP to AP which complicates future work for both the patient and the doctor and further treatment.
Some CAPs are more careful and continue to follow their patients until they have secured a psychiatry consultation "ideally, at least the last CAP consultation should be done in conjunction with the adult psychiatrist”, or at least other CAP’s maintain partial availability “I'm always available if there's anything… if you need a prescription, even if you've already been discharged… there's no problem."
It also happens that the transition is through the hospital, because of a worsening of the disease: those patients admitted to adult psychiatry through hospitalization/inpatient care, were discharged from child psychiatry without direct referral to adult psychiatry before the hospitalization occurred.
Corroborating the realities described, several doctors interviewed emphasized the idea that treatment breakdowns often occur when switching from CAP to AP and were mentioned several times in the interviews: "mostly due to difficulties in accessing the new service, long waiting times, or bureaucratic procedures” (CAP).
Several reasons were highlighted for clinical discharge without direct referral to adult psychiatry. Area of residence was identified as a crucial factor in determining the aftercare service, as it depends on the patient's location or health center area.
A CAP said, “If it's in my hospital's area of residence, we make a direct referral to colleagues, if it's not, we have to make a clinical summary for the family doctor, and it's the family doctor who makes the referral to the hospital in the area of residence, because often the areas of CAP and AP are not coincident”. Lack of knowledge was cited as another reason as many patients consider clinical discharge without a direct referral as a general clinical discharge and do not make an appointment with a family doctor or an AP and “patients often show up decompensated at the consultation or emergency room because they thought that once they were discharged from CAP they didn't need to keep regular psychiatric appointments”. Lack of unified and protocolized procedure was cited by several doctors as an important reason for the failure of the transition. Another factor cited was the lack of adherence by either the patient or family by not taking the medication as prescribed or attending appointments, because the patient or their family do not consider it necessary to continue therapy.
3.1.2. Realized informal transition
This type of transition as described by respondents represents transitions in which the patient undergoes an informal and direct transition from paediatric to adult psychiatry. The information given to the patient and family varies greatly, and the professionals' opinions were sometimes contradictory; some mentioned that in most situations the patient is well-informed, while others mentioned the opposite. Area of residence as referred to with lack of formal transition, is a crucial factor. If the patient's area of residence is the same as the CAP and AP services, then as a respondent noted, "I ask for an adult psychiatry appointment, internally” (CAP), if the disease is more severe that results in a clinical justification to speed up the scheduling process "I ended up making an appointment more quickly.” Proximity between services was mentioned as a reason influencing direct transition, as a participant identified if "two colleagues received internal requests, so I knew that patient would be referred to one of them, and in serious cases, I talk to them" (CAP)
3.1.3. Impact of transition on the patient's life (how does the change affects the patient’s life?)
The impact mentioned varied depending on the type of transition. Professionals indicated that when the transition is similar to a clinical discharge (with referral to the family doctor) with long breaks in treatment, exacerbation of the disease, and even admission, it has a large and negative impact on the patient's life; when it is informal and direct, there is less impact.
“The changes in the doctor-patient relationship and in the understanding of the illness, lead to a major impact on patient's life” (AP). Ten of the 13 psychiatrists stated that the impact on the patient was great.
3.1.4. Existence of a transition service (suggestions for improvement)
Participants were asked about how a service specializing in the treatment of people aged between 15 and 25 in which CAPs and APs collaborate would change the reality they experienced in the transition process.
Five APs and four CAPs stated that they found a transition service useful, because they think that “a transition service also makes it possible to better manage the expectations of parents/caregivers, to involve patients more in their therapeutic project and to facilitate the subsequent transition to an adult service” as a respondent stated (AP).
Two CAPs and one AP thought that it was not useful “It is a patch due to the inability to create child and adolescent psychiatry services, not as something that has to be done like this…" (CAP). However, the latter group also recognized changes were needed that facilitated the implementation of transition model of care to facilitate transfer from paediatric to adult mental health services. For them, the idea of transition service was more of a fix to the real problem, which is the organization of transition in general and communication between services. The remaining nine had no clear idea about this solution; however, all agreed that this issue needs to be improved.
Specific points that could be improved by the transition service, according to those who in favour of it should start with better communication between services (if it's improved several positive effects would be observed in the transition as mentioned below): Greater safety for both the professionals and the patients. Everyone would be more aware of what is happening and what needs to be done next.
Better knowledge about the patient, a CAP stated that "The patient himself can be introduced and get to know and be in a transitional space that he already knows. If he's admitted at seventeen and has to be admitted at twenty, he knows that's where he's going and I think that gives him a certain security, I think that was important."; while one AP felt that "…an approach focused on the needs of each case…, patient safety and adherence to treatment, which is often lost in this transition".
If communication between the services involved is more fluid it also allows a better knowledge about the patient: "What interventions have been carried out, what is the family context, what has been the psychopharmacology (…) it’s easier for the psychiatrist to have more reliable information and to ascertain the problem of patient and family. " (AP).
Sharing experiences was mentioned by most doctors as very important for patient treatment: "Sharing experiences in a bidirectional way can help everyone learn from each other" (CAP). "From sharing experiences, we can improve and adapt our work” (AP).
Adequate preparation for the patient's discharge will make the transition process more likely to be successful, as stated by a CAP: "the transition is carried out in an organized two-way communication, it will help both the CAP and the family to prepare the young person's discharge and this new stage".
The proximity and communication between teams was considered central to an ideal transition and was highlighted mainly by AP’s. One AP said that "…communication is easy when the two services are part of the same department"; while another mentioned AP that "If people are working in different departments there's no contact, everyone ends up working for themselves and communication doesn't flow". This reality seems to demonstrate the need for transition protocols to be followed by all those involved.
Answering questions: In a process like this, which can be complex and go wrong, there must be channels to clarify things for patients and families. This will be easier if services communicate more with each other and can improve future treatments: A CAP clarified that "Any doubts that may arise for colleagues who are in charge of cases"
Patient comfort and well-being was another important improvement resulting from the creation of a transition service, because it could give better information about the illness to the patient and their family, some patients, according to AP’s, say things like this: “ they (the CAP service) just said to the patient that he couldn't be followed there anymore"; or "They didn't explain anything to him, he left and stopped taking medication for a year". It helps to develop trust with the patient, because a major problem with an abrupt transition with poor communication is the patient's lack of trust in the new service. The transition should be smoother, and the patient can get to know the new doctor, preferably in joint meetings, and slowly build their trust. Although the importance of the Family involvement is a frequent topic in the discussion, only once was it clearly mentioned by a CAP "… since they have a very active presence in the child psychiatry consultation and is often asked to intervene".
A transition service could ensure a greater security for patients and family, both CAPs and APs agree that this topic is important: "The patient themselves can be introduced and can get to know you and be in a transition space that he already knows, that gives them a certain security” (CAP). Breaks in follow-up exacerbate the disease and can be avoided by continuity of treatment "…an approach focused on the needs of each case…, patient safety and adherence to treatment, which is often lost in this transition."(AP)
3.1.5. Other suggestions for improvement of transition
The interviewees made other suggestions for how a transition service could reduce the impact of this change, pointing out that they could provide a Closer contact at the consultation level between doctors in urgent situations minimizing breakdowns, relapses, and exacerbations of illnesses “streamlining the ways in which patients can contact doctors and other technicians, improving accessibility and a minimization of impact on prognosis” (CAP). “Patients sometimes mention the difficulty of contacting me in crisis situations” (AP).
Most of the doctors interviewed agreed that there should be different criteria for the transition (other criteria for changing doctors or services), apart from age, which are perhaps more decisive than the fact that they have reached the age of 18.
As one respondent observed, "Transition from CAP to AP services does not go hand in hand with the growth process, as there is often a mismatch between young people who are still being followed in CAP and others in AP service because of an administrative procedure"(AP), Another respondent (CAP) cited “More attention to patient's individual needs and development, which strengthens the patient's confidence and adherence to treatment, minimizing breaks due to the patient's lack of cooperation”. An AP added to this idea that “If discharges or transfers were given with the main emphasis on the patient's individual stage of development and less on their age, this clinical attitude would make it possible to better clarify some doubts that may arise, for example, whether defiant behavior is a normal phase of adolescence or an early symptom of a developing mental illness.”
Suggestions offered by respondents included, sending the summary with the patient's clinical information, regarding the reason for the follow-up, treatments carried out, their response, the patient's most recent condition, etc. could ensure that the doctor and the patient do not have to start from scratch. "I think that when discharging a patient who has had a long process in child psychiatry and goes on to psychiatry, the minimum is to have a detailed report" (AP).
A child psychiatrist's statement on another topic reflects the opinion of most of the doctors interviewed: "In the case of outpatient care, I believe that the existence of reference technicians for the transition of cases, not necessarily doctors, but mental health nurses or social workers, would be an asset to ensure adherence to services, clinical recommendations and to support families in the transition process" (CAP). A respondent (AP) offered this input " it would also help make a better transition with more gradual integration, because transition is often abrupt and aggressive, patients encounter problems; therefore”, the transition should be smoother with no complete break with child psychiatry.
"It would be important for there to be a transition period between the two services, before the patient is discharged from our consultation, in which the patient would have contact with the two doctors responsible for monitoring and other technicians involved (and it would be possible to have some consultations together). The patient should have the opportunity to familiarize themselves with the new physical space" (CAP).
Local liaison in the same department seems to be an important key point for a successful transition since there are no protocoled procedures. Interviewees, both CAP and AP, who said they worked in a clinic where child and adult psychiatry exist within the same department reported better and "unique" communication, information, cooperation, and smoother transitions.” This has an impact on prevention of breakdowns, better proximity, communication and knowledge between doctors, regular liaison sessions between services, and greater trust from patients”.
Several CAPs emphasized the importance of keeping appointments until the patient has an AP appointment directly to prevent breaks in follow-up. "Is important to be able to wait in our service, to keep the appointments, until they have the adult psychiatry appointment".
Involvement of AP’s with a vocation was suggested by both CAP and AP’s: "A psychiatrist with a greater vocation for younger people might be more interesting, someone who has some availability and a more accessible language for young people" (CAP), “someone with a more empathetic approach to young people, which will promote greater adherence to therapy on the part of the young person and their family." (AP).
The need for a standardized mental health plan for the transition process specifically addresses one of the reasons for no formal transition (Lack of unified and protocolized procedure) when patients are clinically discharged. This was the opinion of most CAP’s and AP’s "Within the scope of the National Mental Health Plan, criteria and guidelines should be organized to standardize the transition process, and there should be a simplified and uniform process for transitioning services within the hospital referral network"(CAP). Very important for the interviewed is to have a global vision of care, the patient seen as a whole; it is less about the separate worlds of child and adult psychiatry and more about prioritizing the patient's well-being. Realizing the global vision includes aligning child and adult psychiatry approaches in the use of medication or the amount of care and help versus self-responsibility with which patients are treated. A respondent shared, “people are very focused on the work they're doing and on a lot of bureaucracy, and sometimes they're also focused on themselves and not on this continuity that is necessary." (AP)
Some doctors spoke of the need to slow down: This topic refers to the dispersion of doctors' activities among other tasks that do not allow them to devote as much time to these issues as would be desirable, and it would be good if they could slow down this dispersion "People are not always in the services because they also have to work in other settings appointments are all one after the other, it would be important to be aware and slow down to develop other types of conditions" (AP).
Several of the doctors interviewed said that the idea that patients and families have of what an adult psychiatric service is like is negatively distorted, and this is a topic that also needs to be worked on change in the patient's image of the service(s): “Investing in changing the organization of services, so that both psychiatric services come closer and move towards becoming a continuum” (AP) “adapting services to people and not the other way around” (CAP)
A respondent shared, “If more care were taken in the way of referral to the Psychiatry consultation, the change of service would go better “In terms of people who are never hospitalized, perhaps we should think about another form of referral, better than the one we have now” (CAP): ".
3.2. Adult psychiatry
Regarding adult psychiatry, the interviewees emphasized that the differences in the approach to the illness and the patient between CAP and AP should not be so different, especially in patients of transitional age
The sub-themes in adult psychiatry were: Follow-up; Patient's adaptation process; Inpatient services
3.2.1. Follow-up
Regarding follow-up, one the points that emerged from the interviews was about Consultations that are reported to be less frequent and shorter than that in child psychiatry, due to greater pressure on care (number of patients to see) and young people's lesser need or opposition to family presence “because they're older, they don't want their parents to be there” (AP). The information given and the explanation of the illness seem to be clearer than those in child psychiatry, as a CAP explained: "In adult psychiatry, the autonomy of the young person is favored and promoted, and the family has a more secondary place".
The availability of health professionals other than doctors, such as nurses, psychologists and occupational therapists is perceived differently by patients at CAP and AP, with the idea that those who work at CAP are more available than those who work at AP, as doctors of both specialties stated "In AP, the consultation time is significantly shorter, about a third of what is possible in adolescent psychiatry, and it can be perceived by young people and families as of less interest, or possibly less investment in each individual situation" (CAP).
On Accessibility outside of appointment times, patients and their families feel there are differences between CAP and AP, to the disadvantage of the latter. They don't seem to understand, or it isn't explained to them, that changing the registry is natural. The accessibility acknowledged by some AP “is lower in adult psychiatry than in child and adolescent psychiatry”. Accessibility can support “in emergency situations and thus prevent breaks in treatment” (CAP).
On illnesses most AP believe that the illnesses treated in adult psychiatry “are often more serious and clinically clearly definable disorders” that although they say it can be an opinion that can be somewhat subjective.
Assessment of illness information (or lack of) from CAP is another point mentioned several times by the APs: "When possible, before the first actual observation of the patient, I consult the clinical information that is available electronically, when it exists, but sometimes we just can't get it” and concerning Prescribed medication “Adult psychiatry prescribes more quickly and more medication in general” (AP). “Some patients are not satisfied and want to take less medication” (CAP). This seems to depend on the individual case, but it is generally considered by patients that it is not well explained. The same for Family participation which, as has already been mentioned is less in adult psychiatry than in child and adolescent psychiatry; however, the family can participate at the patient's individual request: "in adolescent psychiatry, intervention is also often carried out with schools, which helps school technicians to deal with the problems and specificities of these young people, this work could also be done with employers"(CAP). Most young patients value that in AP there is a practice that leads to Empowering young people so important decisions for the patient's life are made more individually, although not uniformly. Some like it this way and it helps them to mature, while others prefer to keep a record similar to that of child psychiatry, with a greater presence of parents. “In adult psychiatry, patients are expected to have more personal responsibility, in the form of taking appointments, making central decisions individually” (AP).
3.2.2. Patient's adaptation process
This aspect differs according to individual cases: “in some cases the adolescent adapts well and relatively easily and in other cases has great difficulty adapting and feels very uncomfortable in adult psychiatry” (AP). This topic seems related to the quality of the transition, which means the involvement and motivation of patients and their families, as well as professionals from both specialties (CAP and AP). Particularly in the professionals’ group, the care that was taken in transmitting clinical information and ensuring that this information reached those who can most effectively prevent a break in the continuity of care, (in the more usual allocation of competences AP’s are the most decisive.
3.2.3. Inpatient services
The assessment of the service depends on the patients’ needs. Those who are ready for adult psychiatry in terms of their level of development, perceive the service as being better, others feel that child and adolescent psychiatry service is better. This topic seems also related to the quality/care of transition programming.
One AP described some experiences of young people who had been discharged from CAP “ they often feel a little afraid that I’m not able to understand that some of the things they feel are still part of adolescence and I’m only used talking to adults’ and another AP cited a patient who, after being discharged from CAP, had already been in an inpatient AP service “he told me that he felt better now because he was with people of his own age, when he was in another adult inpatient service there were lots of old people and on the other hand in child psychiatry he was one of the oldest”.
3.3. Child psychiatry
Regarding child psychiatry, the interviewees emphasized, as in adult psychiatry that the differences in the approach to the illness and the patient between CAP and AP should not be so different, although some acknowledge that their opinions may not be completely in line with reality due to their lack of knowledge of how the other specialty works in many aspects.
The sub-themes in “Child Psychiatry” were:
Follow-up; Working model; Referrals that do not make sense (or are unnecessary); Family participation
3.3.1. Follow-up
The service environment in child and adolescent psychiatry is more understanding, time-consuming, affable, and caring than that in adult psychiatry. "It was divided by age, so in that respect it was very good” (CAP). Nine interviewees (three APs and six CAPs) agreed with this premise that the environment in CAP is friendlier than in AP, while only two had the opposite view "They find this whole environment very 'chilled out' and prefer the adult side" (AP). Therefore, the assessment depends on the needs and stage of development of each patient.
The availability of technicians was rated better in child and adolescent psychiatry than in adult psychiatry. "In the adult psychiatry, the time we have for consultation is significantly less, about a third of what is possible in adolescent psychiatry, and this aspect has the disadvantage of being perceived by young people and families as less interest, or possibly less investment in each individual situation." (AP). Likewise, accessibility outside of appointment times is lower in AP than in CAP. “Patients sometimes mention the difficulty of contacting their doctors in crisis situations, even by phone" (CAP)
The topic prescribed medication also came up in the interviews, with some differences in relation to the AP, namely when a CAP stated that in the child psychiatry consultation there is less recourse to the use of psychotropic drugs “with psychotherapeutic approaches being favored”. In another sense, the AP’s feel differently about this issue "In CAP psychopharmacological treatment is sometimes symptomatic, not focused on the nosological entity, and it is not uncommon to see young people with severe depression not medicated with antidepressants" (AP).
The topic consultations also appeared under child psychiatry but are evaluated differently by CAPs and APs. The idea of “consultations in child psychiatry take longer than that in adult psychiatry” was translated by CAPs and APs with opposite meanings, the former see it as indispensable, the latter as unnecessary.
3.3.2. Working model
This also ties in with another subtheme mentioned, which is the working model that, according to CAPs, “consists of more psychotherapeutic interventions, with less use of medication and greater involvement of the community (parents, school, etc.)” and with the difficulties that are found by doctors like capacities of the professionals "Often it is the child psychiatrist who liaises with the schools, educational services, sometimes even sports clubs or play centers; it ends up being a very exhausting job for the child psychiatrist", the lack of parental support that does not occur frequently, however, when it does, it is a problem because a minor patient depends on family support for treatment.
The lack of community support was also mentioned by several CAPs but also some APs and is related to references that do not make sense. “In families with difficult backgrounds and problems, community help could often pick up and support the young person; however, due to the lack of support, young people end up in child psychiatry, although this does not really make sense, because the young person needs support in life and not necessarily a psychiatrist or psychologist” (CAP) which is inseparable from another topic highlighted by several interviewees, the definition of what is mental illness in children, a critical issue that is at the root of other problems (breakdowns in follow-up and worsening of illnesses). It often seems difficult to define what mental illness is in children.
3.3.3. Referrals that do not make sense (or are unnecessary)
Through the adolescent phase, various behavioral problems can emerge that "naturally" disappear with age or are signs of a serious developing mental illness. It seems difficult to predict whether a conspicuous behavior will develop into a mental illness. “I also get the feeling that nosological diagnoses are rarely made, although I understand why clinical pictures in this age group are often poorly defined, less typical” (AP), leading to referrals that do not make sense (or are unnecessary) that results from the unclear question of what mental illness in children is. Thus, the family doctor, the health center, or the court often refer to child psychiatry because they could not assess whether it is a mental illness or a reactive situation of adolescence. These referrals can lead to longer waiting lists and waiting times for even urgent cases with a clearer clinical picture. In addition, there is an extended area of responsibility for psychiatrists, as they also treat cases with reactive situations, although this is not the original task of a psychiatrist; consequently, the availability of technicians decreases.
3.3.4. Family participation
The family participation appears again as a central component in the treatment of child psychiatry and was mentioned frequently by CAP’s and AP’s although it wasn't mentioned as a main theme, “No cooperation from the patient or family” or “…a more empathetic approach to young people promote greater adherence to therapy and the therapeutic plan on the part of the young person and their family." (AP). Another AP stated that “family participation, as is the case in child psychiatry, can be important in some cases and should be improved”.
One CAP expressed the idea that, in addition to families ‘In CAP, intervention is often carried out with schools, promoting their reintegration, and I think that in adult psychiatry the same should be done for the professional reintegration of young adults.’
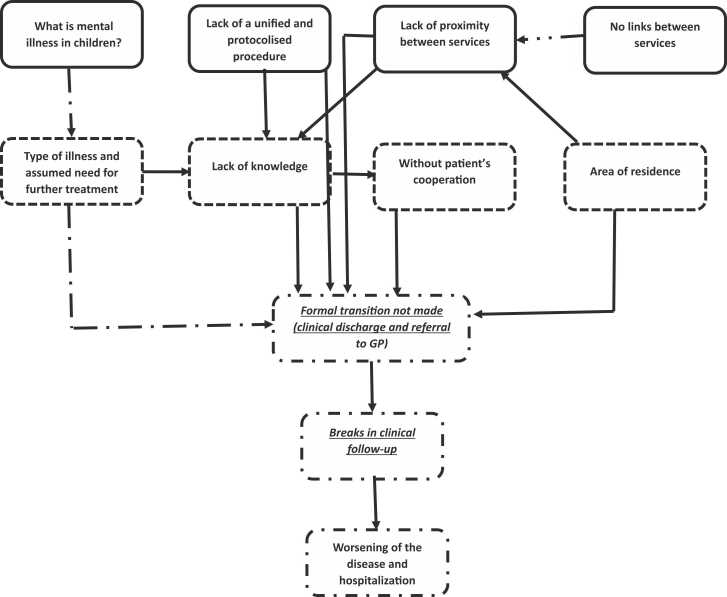
A summary of the main reasons why the transition process often goes wrong and the links between them are explained in Fig. 1 below.
Fig. 1.
MAIN REASONS FOR BREAKS IN CLINICAL FOLLOW-UP (and links between them).
 Primary reasons identified
Primary reasons identified Evolution of problems
Evolution of problems Adverse consequences.
Adverse consequences.
4. Discussion
According to Blum1 “Transition is an efficient, planned, patient-oriented process that meets the medical, psychosocial and educational/occupational needs of young people with chronic conditions” 1 some authors state that this process should start at 14 years of age25, whereas others stress that it should start at least 1 year before the transition boundary26.
Often, transition is not understood as a part of the therapeutic process, even though several authors argue that it should be, and include a period of joint care with clinical information sharing and the passing of records11 and that most of the transitions occur informally, depending on the CAP’s commitment and AP’s receptivity, because no protocols exist to ensure that this passage occurs with less disruptions, beyond youth experiences of moving from CAMHS and AMHS are influenced by concurrent life transitions and their individual preferences regarding autonomy and independence.27 The benefits of having services, or at least protocols, that deal with the transition from pediatric to adult services is an issue that is globally debated among physicians from the two specialties—child and adolescent psychiatry and adult psychiatry, literature shows that continuation of care is a complex process, with important players at policy and organizational levels, service level and at the level of individuals: patients, their families and healthcare providers 7.
A study in the European Union28 considers that the current service configuration, with distinct Child and Adolescent Mental Health (CAMHS) and Adult Mental Health Services (AMHS), is a weak link where the care pathway needs to be most robust; 43 % of the study participants reported that 25–49 % of CAMHS service users will need transitioning to AMHS and 33 % of AMHS users under 30 years had previous contact with CAMHS. Those who answered the question (14/28 countries) said that written policies for managing the interface were available in only four countries (4/14) and that only in half of the countries (14/28) transition support services were available. Another important issue is that for some conditions, there are no adult services with enough experience (e.g. autism or ADHD), making successful transfer even more difficult 29, because the adult psychiatrists usually have little experience on these conditions usually considered childhood illnesses.30
The existing services have demonstrated their consistency and usefulness in reducing disruption to the continuity of care; however, the percentage of young people who do not smoothly transition from one service to the other is more than half in most medical specialties2 and worse in psychiatry even when there are protocols, as shown in the TRACK study.3
A study concerning young people with autism spectrum disorder revealed that in 35 % of those discharged to primary care this path was unsuccessful.31
In the present study, we tried to understand how CAP and AP doctors dealt with the transition between services when a young person reaches the age of 18 and moves from a pediatric service to an adult service and whether they thought it would be beneficial to have services for young people in their late teens and early adulthood (15–25 years).
The answers we received show that this is a problem that doctors feel should be looked at in more depth, and some even said that they hadn't thought about it until now, although they felt that many young people with serious psychiatric illnesses suffered a break in the continuity of care, which they only became aware of when they arrived at the AP's appointment or when the CAP’s received a request for help from the family or the patient themselves when the illness worsened.
In the results of our interviews with Portuguese doctors, we found that the majority considered that the existence of transition services is beneficial for the quality of the therapeutic intervention. CAP’s who believed that a transition service is unnecessary or would not be useful were more vehement than AP’s who shared this position. CAPs did not have a clear knowledge about what happens in AP services; the same is true for APs in relation to adolescent psychiatry services. Neither has sufficient knowledge about the “other specialty,” leading to opinions based on stereotypes, some CAPs expressed fear about the practices followed in adult psychiatry, claiming that psychiatrists prescribe too much medication and take few nonpharmacological approaches. Additionally, some APs pointed to CAPs aversion to pursuing psychopharmacological interventions.
However, both who believed and did not believe in the transition services agreed that the organization of transition in general and the communication between services needs to be improved through the establishment of rules/protocols that structure transition as a process jointly conducted by the two specialties.
The interviews highlighted a persistent difficulty in distinguishing transfer from transition, as is the case in other countries where studies have been carried out on the subject, as well as in the communication between services3.
The study also showed that many doctors do not have the perception that many patients spend long periods without medical attention, because it was not clear to them that discharge from a service such as a child and adolescent psychiatry does not mean that specialized mental health care is not needed.
The data regarding Portugal is inconsistent; however, the problem exists and that it is necessary to understand what the reality to understand this problem. The low number of doctors required to achieve saturation demonstrates that the perception of the problem and the subsequent opinions on it are clearly expressed.
5. Limitations
The current study examined the transition from child and adolescent psychiatry to adult psychiatry services for TAY with mental health problems, as perceived by the psychiatrists and was conducted in the region with the largest population in Portugal, Lisbon and the Tagus Valley, where more than a third of the country's population lives and which has urban, rural and mixed areas, general hospitals and a psychiatric hospital (CHPL – Lisbon Psychiatric Hospital), which did not include the entire country of Portugal.
All the interviews were given the same weight, although there was variability in the clarity and depth of the answers, a convenience sample was used. Some doctors were unwilling to answer the questions for reasons that were not asked, out of respect for the privacy of these doctors, but some of them didn't accept the invitation, citing a lack of available time. The vast majority of those approached were interested in taking part in the study; the findings are consistent with those of studies from other countries,1, 3 but the lack of protocols and transition teams in Portugal precludes a straightforward comparison with the reality of other national health systems.
The researcher tried to appear neutral and without intervention beyond what was stated in the interviews, although there is always the possibility of not having achieved this in an absolute way, to which may be added the subjectivity that may exist in the conclusions of qualitative research.
The non-inclusion of GPs, patients and families meant that experiences other than those of psychiatrists could not be considered in the study's results and conclusions, but these are populations that we plan to include in future research, allowing a more global view of the reality of the transition of services in Portugal.
Another theme often mentioned in the interviews, the difficulty in communication between the two medical specialties, could have been explored further, with new questions to ask during the interviews, which we didn't do because they only came up during the transcription and analysis of the interviews. Further research is needed to better understand these issues so that increasingly care continuity of fewer young people are lost in the transition.
6. Conclusions
The research reveals that most doctors are unaware of what happens to a young person while transitioning from a pediatric psychiatric service to an adult one, as well as the potentially negative consequences of not ensuring the continuity of care. The physicians’ ideas exhibit a clear difference in opinions; the majority think that transition services are a good solution to the issue. The interviewees highlighted the need to improve communication between the two specialties; however, how to accomplish it remained unclear. Some of the interviewees stated that the study caused them to think about this issue for the first time and agreed that the entities and professionals involved should pay more attention to this process, however, there is a lack of research in other countries,32 despite the importance of the topic.
The need for transition protocols to ensure continuity of psychiatric care throughout this transition appears to be an unquestioned necessity and it stimulated remarkable agreement among the various professionals involved. If transition services represent a step forward in the continuity of care, close collaboration and fluid communication between pediatric and adult services are needed and must be strengthened through the development of models that consider dimensions such as autonomy, work, free time, and community participation.
A transition process involving collaboration between the professionals involved, may not be the only way for a TAY to move from a pediatric to an adult service; however, it would eventually result in greater benefits to patients through the dynamics of the services involved.33
Funding
There was no funding received or involved in conducting the study.
Ethical statement
This study protocol was reviewed and approved by Nova Medical School - Comissão de Ética, approval number [73/2018CEFCM] and by Comissão Científico Pedagógica - Lisbon Psychiatric Center (CHPL)
Declaration of Competing Interest
The author declare that he has no competing interests.
Data availability
Data will be made available on request.
References
- 1.Blum R.W., Garell D., Hodgman C.H., et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the society for adolescent medicine. J Adolesc Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. PMID: 8312295 Transition from child-centered to adult health-care systems … - PubMed. [DOI] [PubMed] [Google Scholar]
- 2.McPheeters M.L., Davis A.M., Brown R.F., Taylor J.L., Epstein R.A. Transition care for children with special health care needs. Pediatrics. 2014;134:900–908. doi: 10.1542/peds.2014-1909. 〈https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533283/〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh S.P., Paul M., Ford T., Kramer T., Weaver T. Transitions of care from child and adolescent mental health services to adult mental health services (TRACK study): a study of protocols in greater London. BMC Health Serv Res. 2008;8:135. doi: 10.1186/1472-6963-8-135. 〈https://pubmed.ncbi.nlm.nih.gov/18573214/〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Penttila M., Jaaskelainen E., Hirvonen N., Isohanni M., Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2014;205:88–94. doi: 10.1192/bjp.bp.113.127753. 〈https://pubmed.ncbi.nlm.nih.gov/25252316/〉 [DOI] [PubMed] [Google Scholar]
- 5.Meleis A.I., Sawyer L.M., Im E.O., Hilfinger M.D.K., Schumacher K. Experiencing transitions: an emerging middle-range theory. ANS Adv Nurs Sci. 2000;23:12–28. doi: 10.1097/00012272-200009000-00006. 〈https://pubmed.ncbi.nlm.nih.gov/10970036/〉 [DOI] [PubMed] [Google Scholar]
- 6.Katherine S., Azeesat B., Tresha G. APA Council on Children, Adolescents, and Their Families. 2019. APA “position statement on transitional aged youth”.〈https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-Transitional-Aged-Youth.pdf〉 [Google Scholar]
- 7.Hendrickx G., De Roeck V., Maras A., et al. Challenges during the transition from child and adolescent mental health services to adult mental health services. BJPsych Bull. 2020;44:163–168. doi: 10.1192/bjb.2019.85. 〈https://pubmed.ncbi.nlm.nih.gov/31931898/〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Royal College of Psychiatrists. Good mental health services for young people faculty report CAP/GAP/01. 2017. 〈http://www.rcpsych.ac.uk/publications/collegereports.aspx〉.
- 9.Mental Health Division, Department of Health . Mental Health Division, Department of Health; London, UK: 2009. New horizons: a shared vision for mental health.〈https://www.choiceforum.org/docs/newhorizons.pdf〉 [Google Scholar]
- 10.Khetarpal S.K., Auster L.S., Miller E., Goldstein T.R. Transition age youth mental health: addressing the gap with telemedicine. Child Adolesc Psychiatry Ment Health. 2022;16:8. doi: 10.1186/s13034-022-00444-3. 〈https://capmh.biomedcentral.com/articles/10.1186/s13034-022-00444-3〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paul M., Ford T., Kramer T., Islam Z., Harley K., Singh S.P. Transfers and transitions between child and adult mental health services. Br J Psychiatry Suppl. 2013;54:s36–s40. doi: 10.1192/bjp.bp.112.119198. 〈https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/transfers-and-transitions-between-child-and-adult-mental-health-services/0C95BB2E2584E5EC901BE87562926A43〉 [DOI] [PubMed] [Google Scholar]
- 12.Stewart D., Freeman A., Law M., Healy H., Burke-Gaffney J., Forhan M., et al. The best journey to adult life. An evidence based model and best practice guidelines for the transition to adulthood for youth with disabilities. 2009. 〈https://canchild.ca/system/tenon/assets/attachments/000/000/688/original/BJAmodelandbestpracticeguidelinespdf2009.pdf〉.
- 13.McDonagh J.E., Viner R.M. Lost in transition? Between paediatric and adult services. BMJ. 2006;332:435–436. doi: 10.1136/bmj.332.7539.435. 〈https://research.manchester.ac.uk/en/publications/lost-in-transition-between-paediatric-and-adult-services〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yoon M.J., Pao M. Challenges of transitioning from pediatric to adult-oriented care. Psychiatric. 2015;32:20. 〈https://pure.johnshopkins.edu/en/publications/challenges-of-transitioning-from-pediatric-to-adult-oriented-care〉 [Google Scholar]
- 15.Leipold B., Munz M., Michéle-Malkowsky A. Coping and resilience in the transition to adulthood. Emerg Adulthood. 2019;7:12–20. 〈https://journals.sagepub.com/doi/abs/10.1177/2167696817752950〉 [Google Scholar]
- 16.Adler P.A., Adler P., Baker S.E., Edwards R. Expert voices and early career reflections on sampling and cases in qualitative research. ESRC National Centre for Research Methods, University of Southampton; Southampton, England: 2012. How many qualitative interviews is enough? pp. 8–11.〈http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf〉 [Google Scholar]
- 17.Sim J., Saunders B., Waterfield J., Kingstone T. Can sample size in qualitative research be determined a priori? Int J Soc Res Methodol. 2018;21:619–634. 〈https://www.tandfonline.com/doi/full/10.1080/13645579.2018.1454643〉 [Google Scholar]
- 18.Saunders B., Sim J., Kingstone T., et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–1907. doi: 10.1007/s11135-017-0574-8. 〈https://link.springer.com/article/10.1007/s11135-017-0574-8〉 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grady M.P. Phi Delta Kappa International; Bloomington, Indiana, US: 1998. Qualitative and action research: a practitioner handbook.〈https://www.abebooks.com/9780873678087/Qualitative-Action-Research-Practitioner-Handbook-0873678087/plp〉 [Google Scholar]
- 20.Fusch P., Ness L. Are we there yet? Data saturation in qualitative research. Qual Rep. 2015;20:1408–1416. 〈https://nsuworks.nova.edu/tqr/vol20/iss9/3/〉 [Google Scholar]
- 21.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. 〈https://www.tandfonline.com/doi/abs/10.1191/1478088706qp063oa〉 [Google Scholar]
- 22.Roulston K. Data analysis and ‘theorizing as ideology’. Qual Res Psychol. 2001;1:279–302. 〈https://www.researchgate.net/publication/249730893_Data_analysis_and_'theorizing_as_ideology'〉 [Google Scholar]
- 23.Mason M. Sample size and saturation in PhD studies using qualitative interviews. Forum Qual. Soc Res. 2010;11:19. 〈https://www.qualitative-research.net/index.php/fqs/article/view/1428〉 [Google Scholar]
- 24.Coolican H., Coolican H. Routledge; London, UK: 2009. Research methods and statistics in psychology.〈https://www.routledge.com/Research-Methods-and-Statistics-in-Psychology/Coolican/p/book/9781138708969〉 [Google Scholar]
- 25.McDonagh J.E. Transition of care: how should we do it? Paediatr Child Health. 2007;17(12):480–484. doi: 10.1016/j.paed.2007.09.007. 〈https://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(07)00256-9/fulltext〉 [DOI] [Google Scholar]
- 26.Suris J.C., Rutishauser C., Akre C. Does talking about it make a difference? Opinions of chronically ill young adults after being transferred to adult care. Arch Pedia. 2015;22(3):267. doi: 10.1016/j.arcped.2014.12.001. https://pubmed.ncbi.nlm.nih.gov/25649648/ [DOI] [PubMed] [Google Scholar]
- 27.Hickman, C.J. Strength and Limitations of a Qualitative Research Design from the perspective of a Ph.D student. December 2015 〈doi:10.13140/RG.2.1.3765.6406〉 https://www.researchgate.net/publication/286459625_Strength_and_Limitations_of_a_Qualitative_Research_Design_from_the_perspective_of_a_PhD_student.
- 28.Signorini G., Singh S.P., Marsanic V.B., et al. The interface between child/adolescent and adult mental health services: results from a European 28-country survey. Eur Child Adolesc Psychiatry. 2018;27:501–511. doi: 10.1007/s00787-018-1112-5. (https://pure.eur.nl/en/publications/the-interface-between-childadolescent-and-adult-mental-health-ser) [DOI] [PubMed] [Google Scholar]
- 29.Hall C.L., Newell K., Taylor J., Sayal K., Hollis C. Services for young people with attention deficit/hyperactivity disorder transitioning from child to adult mental health services: a national survey of mental health trusts in England. J Psychopharmacol. 2015;29:39–42. doi: 10.1177/0269881114550353. 〈https://pubmed.ncbi.nlm.nih.gov/25237121/〉 [DOI] [PubMed] [Google Scholar]
- 30.Young, S., Murphy, C.M. & Coghill, D. 2011. Avoiding the ’twilight zone’: recommendations for the transition of services from adolescence to adulthood for young people with ADHD. 11, 174. 〈https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-11-174〉. [DOI] [PMC free article] [PubMed]
- 31.Merrick H., King C., McConachie H., Parr J.R., Le Couteur A. Experience of transfer from child to adult mental health services of young people with autism spectrum disorder. BJPsych Open. 2020;6(e58):1–10. doi: 10.1192/bjo.2020.4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7345668/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Broad K.L., Sandhu V.K., Sunderji N., et al. Youth experiences of transition from child mental health services to adult mental health services: a qualitative thematic synthesis. BMC Psychiatry. 2017;17:380. doi: 10.1186/s12888-017-1538-1. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1538-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salgado J. The transition of children and adolescent healthcare services to adult healthcare services: a reality with impact on prognosis. Acta Med Port. 2022;35:161–163. doi: 10.20344/amp.15912. 〈https://europepmc.org/article/med/35320070〉 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.