Abstract
Background
As many as 95% of individuals across the lifespan with autism spectrum disorder (ASD) have at least one comorbidity. While research focused only on the health of autistic adolescents is limited, we do know that fewer than 14% of these youth receive appropriate transition services to self-manage their health. These limitations have resulted in poor outcomes and premature mortality. Little is known about how parents and their adolescent children address this health burden.
Objective
The objective of this study is twofold. First to compare the perceptions of adolescents with ASD and their parents regarding adolescents’ contextual and process variables (depressive symptoms, health knowledge, health communication/planning, self-efficacy, self-determination) and health self-management (HSM) behavior. The second is to examine social facilitation for HSM behaviors in adolescents with ASD and their parents.
Methods
In this community-based study, an online survey was used to compare the perspectives of 40 adolescents with ASD aged 12 to 22 years and their parents on the adolescents’ HSM behaviors. Contextual and process variable measures (PROMISE, Starx, General Self-efficacy Scale, AIR Self-determination Scale, Social Facilitation Questionnaire) were completed by both adolescents (adolescent/pediatric version) and parents (parent version).
Results
Descriptive analysis indicated that parents were teaching self-management to adolescents for monitoring and preventing illness, including medication knowledge and how to talk to their doctor. The largest differences were found between parents’ and adolescents’ perceptions regarding teaching and learning about independent management of existing health conditions. Additionally, adolescents rated their self-efficacy (t (38) = 3.62, p < .001) and self-determination (t (39) = 4.55, p < .001) significantly higher than their parents did.
Conclusions
This study contributes perspectives on what parents and adolescents are doing to enhance adolescents’ health self-management. Adolescence is a developmental period of social facilitation when parents may teach their adolescent children with ASD to self-manage their health and when those adolescents may learn to do so. During this period, providers should offer adequate planning and guided training to support parents and their adolescent children with ASD to improve adolescents’ self-management behaviors and improve health outcomes for this vulnerable population.
Keywords: Autism spectrum disorder, Facilitating health care transition, Adolescent health self-management
1. Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental condition that affects communication and social relationships in 1 in 36 eight-year-olds in the United States.1, 2 While research examining health among adolescents with ASD is limited, studies examining the health of individuals with ASD in general suggest as many as 95% of the population have at least one co-occurring physical, mental, or developmental condition.2, 3 Youth with ASD have greater health risks than those without ASD, including youth with other special health care needs.4, 5, 6 Epilepsy, for example, affects approximately 33% of individuals with ASD as opposed to only 1% to 2% of the general population7; approximately 84% of individuals with ASD report at least one gastrointestinal (GI) disorder, and GI disorders are 8 times more common in youth with ASD than in other children; and approximately 42% of the ASD population report anxiety, whereas only 3% of typically developing children and 15% of adults in the general population do so.7, 8, 9, 10, 11 The heightened risk for comorbidities in those with ASD contributes to a higher rate of premature mortality related to untreated or undertreated health conditions than in typically developing peers.6, 12 In a 20-year longitudinal study of individuals with ASD, 6.4% died an average of 38.5 years prior to their life expectancy.12 Causes of death were attributed to comorbidities, accidents, and complications relating to medication side effects.
Adolescents with ASD are included among the 14.1 million U.S. youth with special health care needs. These youth are defined as those at increased risk for physical, developmental, or emotional health conditions and require health and supportive services at an increased rate when compared to other typically developing youth.13, 14 However, unlike most other such youth with special health care needs, adolescents with ASD and their families must manage the challenges of both their autism disorder (communication challenges, executive functioning deficits, sensory hyposensitivity or hypersensitivity) and comorbidities. Furthermore, most youth with ASD require twice as many supporting services (e.g., psychiatry, occupational therapy, speech therapy) as do other youth with special health care needs.15 Meeting the health needs of youth with ASD requires coordination among multiple specialists and health care providers, which may be one reason unmet health care needs are four times more likely among youth with ASD than among typically developing peers and two times more likely than among youth with other disabilities.15
Health self-management (HSM) is an effective strategy in the health care transition process to address potential poor health outcomes and increased health demands16, especially among adolescents with ASD.17, 18 HSM in the health care transition process addresses the development and coordination of condition-specific knowledge and beliefs, as well as self-regulation skills and abilities to manage acute, chronic, and preventative health care in a consistent, prolonged manner. Given the significant number of acute and chronic health conditions experienced by individuals with ASD, early engagement in managing their health is warranted. The guidelines for HSM during adolescents’ transition to adult health responsibilities emphasize self-determination, self-management, family engagement, and need for parents to support youth in building knowledge about their own health so that they can make health care decisions.16 These guidelines as proposed by the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians suggest introduction of health care transition to adulthood to all youth by age 12 years in a supported family-centered environment.19 Unfortunately, transition service as it is described by the American Academy of Pediatrics is often unclear, incomplete, or introduced too late to support an effective transition to adult services.19, 20 In the 2016–2017 National Survey of Children and Youth with Special Health Care Needs, which included children with ASD, less than 14.6% of youth aged 12 to 17 years and their families were reported to have received transition services needed for adolescents’ transition to adult health care.21 Given the lack of clear guidance for transition, many parents carry a large burden for their children's health care.22 Parents of youth with ASD are often left to coordinate treatment from several specialty providers simultaneously, with poor communication and collaboration among providers.22, 23, 24
Additionally, parents’ perceptions of their children’s ability to deal with complex situations may be related to parents’ encouragement of their children in decision making and increased responsibility.25 In provider-implemented and parent-mediated interventions for children with ASD, children’s social engagement and parents’ self-efficacy have significantly improved with early engagement of parents in supportive role development.26 Parents of children with ASD also struggle with their own transition to the new role of coordinator as they let go of long-held responsibilities.27, 28, 29 Therefore, understanding parents’ perspectives on their children’s self-management abilities and skills should provide valuable insight into parents’ ability to support their children’s autonomy through social facilitation.
To date, little is known about how adolescents with ASD and their families manage their health condition(s). Literature and research exploring the perspectives of individuals with ASD are limited.30 A qualitative meta-synthesis of literature from 1980 to 2014 on the lived experiences of individuals with ASD found only 33 articles that presented the first-person perspectives of adults, adolescents, or children.31 Current research often relies on the perspectives of providers, families, and/or caregivers for much of our understanding of autism. This lack of ASD-specific research on the perspectives of those with ASD limits our understanding of autism and serves as a barrier to evidenced-based practice.
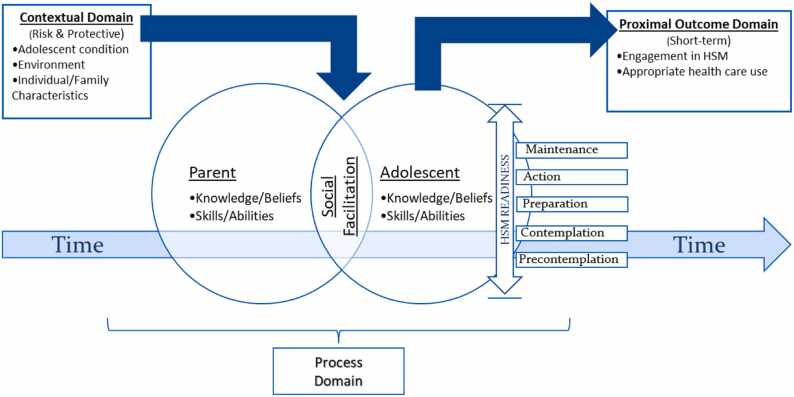
In this community-based study, we examine the psychological concept of social facilitation among adolescents with ASD and their parents, a key component in the Adolescent Health Self-Management Model.32 The concept of social facilitation suggests individual performance is improved when other people are present rather than the individual acting alone.14 Here, we define social facilitation as the shared relationship between adolescents and their parents to enhance the adolescent’s capacity to engage in HSM behavior (Fig. 1). It includes social influence, social support, and negotiated collaboration within the parent–child relationship.29, 33 In this study, social facilitation thus represents what parents do to support and prepare their adolescent children with ASD to self-manage their own health and what these adolescents do to learn how to take care of their health.
Fig. 1.
Adolescent Health Self-Management Model.
This study addresses two aims. The first is to compare the perspectives of adolescents with ASD and their parents on HSM behavior—the perceptions of adolescents and their parents regarding adolescents’ contextual and process variables (depressive symptoms, health knowledge, health communication/planning, self-efficacy, self-determination) and HSM behavior. The second is to examine social facilitation for HSM behaviors in adolescents with ASD and their parents, by considering what parents do to prepare their children to transition to HSM, what adolescents with ASD do to transition to HSM, and what parents perceive as barriers to transitioning their adolescent children with ASD to HSM.
2. Method
For this community-based study we used an online survey to compare adolescents’ and parents’ perspectives on adolescents’ HSM behaviors. The findings presented here focus on depressive symptoms, health knowledge, health communication/planning, self-efficacy, self-determination, HSM behavior, and social facilitation. A power analysis for bivariate correlation recommended a minimum sample size of 30 for the study, assuming α = .05 and a power of 0.80, for an effect size of r = .47.34
2.1. Participants
A convenience sample of 40 adolescents with ASD aged 12 to 22 years and 40 parents/caregivers (40 dyads) were recruited from agencies and organizations supporting individuals with ASD and their families. The adolescents, with a diverse set of needs and abilities, and their parents/caregivers completed an online survey separately. Most of the parent/caregiver sample (98%) were the parent of the adolescent (only one was an aunt), so the parent/caregiver sample is referred to as consisting of parents henceforth.
The 22-item Background Information Questionnaire was completed by parents and assessed 12 parent/family related items such as parents age, sex, access to family centered care, number of children in the household, number of children having ASD in the household and 10 adolescent specific related items such as adolescents’ age, sex, age at ASD diagnosis, chronic health condition(s), level of daily impact from chronic health condition(s), if any. The sample’s characteristics are summarized in Table 1.
Table 1.
Demographic variables of adolescent and parent participants.
| CHARACTERISTIC | n | (%) | Μ | (SD) | RANGE |
|---|---|---|---|---|---|
| AGE (YEARS) | |||||
| Parent | 40 | (100) | 47.93 | (7.07) | 34 – 64 |
| Adolescent | |||||
| 12-14 years | 20 | (50) | 15.83 | (3.25) | 12 - 22 |
| 15-18 years | 9 | (22.5) | |||
| 19-22 years | 11 | (27.5) | |||
| GENDER | |||||
| Parent | |||||
| Male | 1 | (2.5) | |||
| Female | 39 | (97.5) | |||
| Adolescent | |||||
| Male | 30 | (75) | |||
| Female | 9 | (22.5) | |||
| Other | 1 | (2.5) | |||
| RACE | |||||
| Parent | |||||
| White | 34 | (85) | |||
| Black/African American | 1 | (2.5) | |||
| Asian | 1 | (2.5) | |||
| Mixed Race | 4 | (10) | |||
| Adolescent | |||||
| White | 34 | (85) | |||
| Black/African American | 1 | (2.5) | |||
| Mixed Race | 5 | (12.5) | |||
| ETHNICITY | |||||
| Parent & Adolescent | |||||
| Hispanic | 7 | (17.5) | |||
| Non-Hispanic | 33 | (82.5) | |||
| MOTHER’S EDUCATION | |||||
| Did not complete HS | 2 | (5) | |||
| High school diploma | 2 | (5) | |||
| Some college/post-HS | 15 | (37.5) | |||
| College/baccalaureate | 15 | (37.5) | |||
| Post-baccalaureate | 6 | (15) | |||
| FATHER’S EDUCATION | |||||
| Did not complete HS | 4 | (10) | |||
| High school diploma | 11 | (27.5) | |||
| Some college/post-HS | 7 | (17.5) | |||
| College/baccalaureate | 13 | (32.5) | |||
| Post-baccalaureate | 5 | (12.5) | |||
| ANNUAL HOUSEHOLD INCOME | |||||
| $25,000 or less | 5 | (12.5) | |||
| $25,001 to $50,000 | 5 | (12.5) | |||
| $50,001 to $75,000 | 5 | (12.5) | |||
| $75,001 to $100,000 | 9 | (22.5) | |||
| $100, 001 or above | 16 | (40) | |||
| AGE ASD DIAGNOSIS | 6.45 | (4.00) | 1 - 14 | ||
| YEARS SINCE DIAGNOSIS | 9.38 | (5.18) | 1 – 19.5 | ||
| ADOLESCENT’S CURRENT GRADE | |||||
| Middle School (6th – 8th) | 17 | (42.5) | |||
| High School (9th – 12th) | 13 | (32.5) | |||
| High School graduate/diploma | 5 | (12.5) | |||
| Some college/degree | 5 | (12.5) | |||
| CHRONIC HEALTH CONDITION | |||||
| Yes | 33 | (82.5) | |||
| No | 7 | (17.5) | |||
| DEPRESSION (parent report of adolescent) | 9 | (22.5) | |||
| IMPACT OF CHRONIC HEALTH CONDITION (DAILY) | |||||
| Rarely or not at all | 12 | (30) | |||
| Sometimes | 11 | (27.5) | |||
| Usually/or often | 9 | (22.5) | |||
| Always | 8 | (20) | |||
| ACCESS TO FAMILY-CENTERED CARE | |||||
| Yes | 36 | (90) | |||
| No | 4 | (10) |
Note: HS = High School
The mean age of the adolescent participants (15.83 years) was slightly skewed toward a younger age (skewness =.73, SE =.37); 50% were 12–14 years old. The sample comprised more male (75%) than female (22.5%) participants, which aligns with ASD diagnosis being four times more likely for boys than for girls. Per parent report, most of the adolescent participants had at least one comorbid health condition (83%) that impacted their daily lives mildly to significantly (70%). Anxiety was the highest rated comorbid mental health condition (63%), GI disorders were among the highest rated physical health conditions (23%), and intellectual developmental disorder was the highest rated developmental condition (13%). The median age for ASD diagnosis was 5.0 years, with a mean of 9.38 years since diagnosis. Despite study flyers being distributed across a broad array of facilities and programs caring for individuals and families having ASD, the participating parents were primarily White (85%) non-Hispanic (83%) educated mothers who were married (78%). Most parents (90%) reported access to family-centered care and private and/or public health insurance (93%). Most (63%) reported annual household incomes above $75,000.
2.2. Procedure
Following IRB approval, participants were recruited via posted flyers and presentations at agencies, organizations, and providers that supported individuals with ASD and their families living in Texas, from October 2019 to December 2020. Prospective study participants who expressed interest were screened for eligibility. Inclusion criteria for adolescents were (a) a diagnosis of ASD (per parents’ report), (b) age 12 to 22 years, (c) enrollment in 6th grade or above, (d) ability to read and write English, (e) ability to give consent/assent, and (f) having a parent/family caregiver who was able to read and write in English and who consented to participate in the study. All eligible participants received instructions about the study and its expectations as well as a copy of the parent consent and adolescent assent/consent (based on adolescents’ age) to review and keep for their records.
Prior to the COVID-19 pandemic, all participants were offered the option to complete a hard copy of the survey in person. Given the diversity of needs and abilities of individuals with ASD and to avoid limiting the study to youth with specific cognitive or communication abilities, IRB approval was obtained to provide additional support for completing the survey if needed. This support included answering questions, adding clarity, and reading questions aloud to avoid undue bias. In addition, parents were informed that adolescents had to answer survey questions independently; parents were not allowed to be proxy respondents for their children. When possible, parents were asked to provide an email address for their children so that each adolescent’s consent/assent and survey link could be sent directly to the adolescent. Although several parents initially inquired about additional support for their children, no additional parent or adolescent support was requested for completing the survey. However, prior to receiving the survey link, two parents chose to withdraw their children from the study because they did not believe that their children could complete the survey independently. Once social distancing restrictions related to COVID-19 limited face-to-face research, distance support and online survey completion became the only study options available.
Parents and adolescents received an email with an individual link to the study’s Qualtrics survey, with consent/assent forms posted at the beginning of the survey per IRB waiver of signed consent. Parents agreed to be study participants and agreed for their children to be study participants before their individual surveys began, and adolescents agreed to be study participants before their surveys began. Upon survey completion, both adolescents and parents received a $25 gift card for their time and effort.
2.3. Measures
Individual and family demographic data were obtained with a Background Information Questionnaire designed by the first author and completed by parents. Contextual, process, and proximal outcome variables were measured with widely used instruments having established reliability and validity for assessing youth with special health care needs with and without ASD. The instruments, their psychometrics, and the Cronbach alpha reliability coefficients from this study are presented in Table 2. The references in the notes at the bottom of the table contain additional psychometric information about these instruments.12, 25, 35, 36, 37, 38, 39, 40, 41, 42 Given the lack of measures designed to capture social facilitation between adolescents with ASD and their parents in the health care setting, specific questions were used to explore collaborative health behaviors in each adolescent with ASD and the adolescent’s parents. Adolescents were asked, “What does your parent do to help you learn how to manage your health?” Parents were asked, “What do you do to help your child learn how to self-manage their health?” Because the adolescents' social facilitation consisted of the transition of health management from the parent to the adolescent’s HSM, adolescents were asked, “What do you do on your own to take care of your health?” These investigator-developed questions were informed by the first author’s previous interviews with parents, were followed by dropdown menu options commonly found for all chronic health conditions.33 For instance, when asking parents what they do to prepare their child to self-manage their health, the dropdown menu included options such as: I teach my child about how to take their medications; I teach my child how to report symptoms of illness to their doctor; I teach my child how to reduce stress and manage their emotions; I’m not now teaching my child these skills because I manage their health care”. In addition, an “other” category was provided, to allow respondents to add additional information in their own words. To measure parents’ perceived barriers to transitioning health responsibility to their child, parents were asked, “What are your barriers to teaching your child how to self-manage their health?” A dropdown menu offered common barriers for parents transitioning their child to adult services.29 Participants could select a response from this dropdown menu, and again, an “other” category was provided to enable parents to elaborate on their response to this question.
Table 2.
Instruments for adolescent measures.
| Tool | Domain/Concept | Description | Items | Scoring | α |
|---|---|---|---|---|---|
| Contextual: | |||||
| PROMISa | Depressive symptoms | Negative mood, negative self-view | A: 14 P: 11 |
1 = almost never to 5 = almost always | A:.91 P:.94 |
| Process: | |||||
| Starxb | Health knowledge | Specific condition knowledge | A: 3 | 1 = nothing to 5 = a lot | A:.69 |
| Starxb | Communication/Planning | With family/provider | A: 3/3 | 1 = very hard to 5 = very easy | A:.71 |
| Starx-Pc | Health knowledge | Perception of child’s knowledge | P: 3 | 1 = nothing to 5 = a lot | P:.89 |
| Starx-Pc | Communication/Planning | Perception of child’s skill/ability | P: 3/3 | 1 = very hard to 5 = very easy | P:.83 |
| GSESd | Self-efficacy | A = Confidence in own skill/ability P = Confidence in child’s skill/ability |
A: 10 P: 10 |
1 = not at all to 4 = exactly true | A:.76 P:.80 |
| AIRe | Self-determination | A = Opportunity practice skill/ability P = Perception of child’s opportunity |
A: 24 P: 24 |
0 = not needed to 5 = always | A:.88 P:.91 |
| Proximal Outcome: | |||||
| Starxb | HSM behavior | Self-management behavior | A: 9 | 1 = never to 5 = always | A:.65 |
| Star-Pc | HSM behavior | Perception child’s self-management | P: 9 | 1 = never to 5 = always | P:.72 |
Note:
= PROMIS - emotional distress-depression-peds short form12;
= Starx health care transition readiness questionnaire for youth with chronic health condition35, 36;
= Starx-P health care transition readiness questionnaire for parent of youth with chronic health condition (child’s readiness)37;
2.4. Data analysis
All quantitative data were analyzed using IBM SPSS Statistics 26.0. Parents’ data were merged with their children’s data as the aim of this study was exploring the adolescent’s self-reported health behaviors as compared with parents’ perspective on their child’s health behaviors. Data entry was checked by a second observer to assure accuracy. A preliminary analysis was conducted to assess for missing data, establish descriptive characteristics of the sample, and estimate internal consistency reliability (Cronbach’s alphas) for all instruments. Coefficients for all measures except adolescents’ scores on subscales for health knowledge (α = .69) and HSM behavior (α = .65) were above α = .70. Apart from self-efficacy and depressive symptom measures not completed by one adolescent, all survey items had less than 4% missing data, with missingness at random. Data for the adolescent not completing the self-efficacy and depressive symptom measures was removed when analyzing results relating to these two measures. This is noted in the respective data tables. Otherwise, limited data missing at random were replaced with the average of the values of the parameter estimates derived from multiple imputation (average parameter estimates across imputation samples). Statistical significance was set at p ≤ .05.
The adolescent depressive symptom measure contained three more items than did the parent version of the measure, so raw scores were converted to standardized T-scores and interpreted symptom severity was determined using PROMIS43 tables and scales. Paired-samples t-tests were conducted to examine differences in dyad measures completed by both adolescents and parents (depressive symptoms, health knowledge, health communication/planning, self-efficacy, self-determination, HSM behavior).
When analyzing social facilitation data, descriptive statistics were used to examine the number and percentage of responses for each category in the dropdown menus provided on the survey. These findings are presented in Table 3 and fully described in the Results section. To examine the additional responses from the “other” category provided by parents and adolescents, themes were identified using a descriptive content analysis approach.44 In the preparation phase of the content analysis, data within each of the “other” categories was identified in relation to the three aspects of social facilitation: social influence, social support, or negotiated collaboration. Once identified, data was then organized, coded, and grouped into subthemes.
Table 3.
Parent and adolescent responses to social facilitation questions (N = 40).
| Response | Parent n/% |
Adolescent n/% |
|---|---|---|
| What parent does to support adolescent HSM behavior | ||
| Nothing – Parent manages all health care needs | 6 (15.0) | 12 (30.0) |
| Teaches about medications | 29 (72.5) | 22 (55.0) |
| Teaches to talk to doctor | 31 (77.5) | 24 (60.0) |
| Teaches to monitor for s/s of illness | 34 (85.0) | 21 (52.5) |
| Teaches how to complete a treatment (adolescent only asked) | - | 12 (30.0) |
| Shows how to find information about health | 19 (47.5) | 24 (60.0) |
| Shows how to set-up health reminders, timers, etc. | 10 (25.0) | 17 (42.5) |
| Teaches to promote health (eat right, exercise, etc.) | 36 (90.0) | 35 (87.5) |
| Teaches to manage emotions | 37 (92.5) | 30 (75.0) |
| Teaches to set-up doctor’s appointments | 10 (25.0) | 10 (25.0) |
| Teaches how to report s/s of illness to doctor (parent only asked) | 26 (65.0) | - |
| What adolescent does to take care of own health | ||
| Nothing, parent takes care of all health needs | 10 (25.0) | |
| Talk to parent about wanting more responsibility for my health | 14 (35.0) | |
| I monitor my health for s/s that I need to contact my doctor | 19 (47.5) | |
| I schedule my own appointments with therapist | 4 (10.0) | |
| I get enough sleep, eat right, and exercise regularly | 21 (52.5) | |
| I use adaptive devices for my health | 8 (20.0) | |
| Barriers for parents to teach HSM behaviors | ||
| I never thought of teaching my child to self-manage their health | 8 (20.0) | |
| Too many other competing teaching priorities for my child | 11 (27.5) | |
| Lack of information about what to teach my child | 7 (17.5) | |
| Lack of time | 12 (30.0) | |
| Too many health concerns for my child to self-manage | 7 (17.5) | |
| No support from health care team about how to do this | 5 (12.5) | |
| Too many competing family priorities | 17 (42.5) | |
2.5. Community participation
This study had meaningful involvement in numerous ways from individuals and family members of people with ASD. The first author, a parent of an adolescent with ASD, respectfully speaks and advocates from this perspective. A local consortium group of ASD researchers, providers, individuals with ASD and family members provided feedback that informed the study design. Six parents of children with ASD were interviewed earlier about their experiences while providing health care guidance for their child, and their comments also informed this study. Finally, many thanks are extended to the family members of people with ASD who assisted in the study implementation by publicizing the study to families they know and serve. Without your support and contributions this study would not have been possible.
3. Results
3.1. Comparing adolescent and parent perspectives
The first aim of this study was to compare the perspectives of adolescents with ASD and their parents on HSM behavior. We did this by examining the adolescents’ and parents’ perceptions of the adolescents’ contextual and process variables (depressive symptoms, health knowledge, health communication/planning, self-efficacy, self-determination) and HSM behavior.
Differences in adolescents' and parents' perceptions of contextual (depressive symptoms) and process (knowledge, communication/planning, self-efficacy, self-determination) variables and HSM behaviors are presented in Table 4. Differences were statistically significant for two of the six comparative measures: self-efficacy and self-determination. Effect sizes associated with these comparisons (Cohen’s d) ranged from.20 to.72.
Table 4.
Group differences between adolescent and parent measures (N = 40).
| Measure | Adolescent M (SD) |
Parent M (SD) |
df | t | p | Cohen’s d |
|---|---|---|---|---|---|---|
| Pair 1: Depressive Symptoms | 55.14 (9.88) | 57.86 (11.17) | 38 | -1.72 | .09 | -0.26 |
| Pair 2: Health Knowledge | 11.38 (2.62) | 12.02 (2.64) | 39 | -1.70 | .10 | -0.24 |
| Pair 3: Health Comm/Plan | 18.64 (4.58) | 17.02 (5.79) | 39 | 1.85 | .07 | 0.31 |
| Pair 4: Self-Efficacy | 27.85 (4.37) | 25.10 (4.33) | 38 | 3.62 | .001 ** | 0.63 |
| Pair 5: Self-Determination | 68.21 (10.13) | 60.90 (10.31) | 39 | 4.55 | < .001 *** | 0.72 |
| Pair 6: Self-Management | 26.40 (5.71) | 25.18 (6.39) | 39 | 1.68 | .10 | 0.20 |
N = 39 for adolescent depressive symptoms and self-efficacy measures
**Significant at the 0.001 level (2-tailed) ***Significant at the < 0.001 level (2-tailed)
Due to a significant departure from normality for both self-efficacy and health knowledge as indicated by Shapiro–Wilk test, a nonparametric (Wilcoxon signed-rank) test was run, and the results were consistent with those of the t-test comparisons. The significant difference for self-efficacy scores (z (38) = 3.22, p = .001) suggests that adolescents on average perceived themselves as having greater self-efficacy than their parents did. Examination of parents’ (Μ = 60.90, SD = 10.31) and adolescents’ (Μ = 68.21, SD = 10.13) self-determination scores indicated that adolescents perceived their self-determination to be significantly higher than their parents did (t (39) = 4.55, p < .001).
Differences between the adolescents’ (Μ = 55.14, SD = 9.88) and parents’ (Μ = 57.86, SD = 11.17) mean ratings on depressive symptoms were nonsignificant (p < .10), but the differences in responses between parents and adolescents merit further consideration. Standardized T-scores are presented in Table 5. Although about half the adolescents’ depressive symptoms scores fell into the category of none to slight depressive symptoms, only 38% of parents’ scores for their children’s symptoms were in this range. The other 62% of parents rated their child’s depressive symptoms as mild to severe. However, only nine parents (22.5%) reported their child having a diagnosis of depression on the Background Information Questionnaire. As a contextual variable, adolescents having ASD and co-occurring depression may add to the complexity of learning HSM, especially if the depressive disorder is untreated or undertreated.
Table 5.
Adolescent Depressive Symptom Rating.
| PROMIS T-scores | Adolescent (N = 39) M SD |
Parents (N = 40) M SD |
|---|---|---|
| None to Slight | 21 (54%) | 15 (38%) |
| Mild | 4 (10%) | 7 (17%) |
| Moderate | 13 (33%) | 12 (30%) |
| Severe | 1 (3%) | 6 (15%) |
3.2. Social Facilitation for HSM Behaviors
The second aim of this study was to examine social facilitation for HSM behaviors in adolescents with ASD and their parents by asking what parents do to prepare their children to transition to HSM, what adolescents with ASD do to transition to HSM, and what parents perceive as barriers to transitioning their adolescent children with ASD to HSM. Most parents (31/40) expanded on their thoughts in each of the optional “other” categories presented to parents. Fewer adolescent respondents offered additional thoughts. For instance, a little over 27% (11/40) of adolescents responded to the “other” category when asked about what parents do to support their HSM and approximately 37% (15/40) responded to the “other” category asking what the adolescent does on their own to learn HSM.
3.3. What parents do to prepare their child to transition to HSM
Parents and adolescents were both asked what the parent did to help the adolescent engage in HSM behaviors (see Table 3). Both adolescents and parents reported that parents were most likely to teach the adolescent how to manage emotions (75% vs 92.5%) and engage in health-promoting behaviors (87.5% vs. 90%). Parents were more likely than adolescents to report that they taught their children how to monitor their health (85% vs. 52.5%) and take medications (72.5% vs. 55%). Adolescents were more likely to report that parents helped them find health information (60% vs. 47.5%) and set up adaptive devices (42.5% vs. 25%). The agreement between adolescents and parents was highest for one of the lowest reported aspects of teaching, how to set up doctor’s appointments (25%).
An “other” category enabled parents and adolescents to describe additional strategies that parents employed to support adolescents’ HSM behavior in their own words. Descriptive content analysis revealed several subthemes in relation to what parents are doing to prepare their child to transition to HSM. These subthemes included: lack of expectation to assume responsibility, active engagement and collaboration, and lack of supportive transition resources. The first subtheme was a lack of expectation that the adolescent would assume responsibility for their health and was demonstrated by several adolescents stating they were too young to assume health responsibilities. One adolescent stated, “I’m 14 so I feel like I’m a bit young”. Another remarked, “for a lot of this I’m too young to be able to do this on my own, even if I didn’t have autism”. Still another commented; “I like mom to do a lot of doctor stuff.” Parents also seemed to struggle with this transition as one parent stated, “I really didn’t think of that until answering this survey.” Further supporting this subtheme, multiple parents and adolescents reported that the parent was currently managing all health care needs (15% and 30%, respectively).
Parents’ statements about their active engagement and collaboration with their adolescent children in social facilitation constituted the second subtheme. For instance, one parent remarked, “We’re in the process of learning these things and transitioning to more independence”. Another parent stated, “[Child’s Name] always asks questions about medications and treatment”. Still another wrote, “I don’t teach so much at this point so much as reinforce previously taught lessons.” Parents were also teaching their children self-advocacy for relating to their health. Comments from several parents included: “I try to encourage her to speak up for herself now that she is a legal adult because no one really cares what her mother has to say now. It’s all about her.” The last subtheme emerged regarding parents’ concern for their children’s transitioning successfully to adult responsibilities without the presence of supporting services. Parents wrote, “I am not confident as he reaches adulthood he will manage his health needs adequately”, and another stated, “There is currently no system outside of Mom to teach him how to self-manage his health.”
3.4. What adolescents with ASD are doing to transition to self-manage their health
Descriptive statistics for each category in the survey’s pull-down menu are presented in Table 3. Some adolescents reported that they did nothing on their own and relied on parents to manage their health (25%), whereas others sought more involvement (35%). As ways to manage their health, adolescents most often reported that they took steps to promote good health (52.5%), followed by regularly monitoring their health for signs and symptoms of illness (47.5%). In the adolescents’ open text responses, a recurring subtheme reflected adolescents were seeking independence. Several adolescents shared their actions toward independence. One wrote, “I learn a lot on my own from books and the internet. I currently scribe for a family practice doctor so I’ve been learning a lot from her too”. Another stated, “While I may need a reminder or two every so often, I basically take care of my life with an exception being driving.” Others identified a need to take on more responsibility stating: “I need to be more active” and “I need to do more.”
3.5. What parents perceive as barriers to transitioning their adolescents with ASD to HSM
In the pull-down menu for this question, parents most frequently endorsed competing family priorities (42.5%) and lack of time (30%) as barriers to teaching HSM to their children (Table 3). For some parents, awareness (20%) or a lack of understanding about what to instruct their children were barriers (17.5%). The most prominent subtheme from parents’ free-text comments related to their child’s communication difficulties. One parent stated, “Child has difficulties with expressive verbal communication”. Another wrote, “Engaging in dialog can sometimes be cut short if she gets embarrassed or flustered.” One parent described a lack of barriers: “In some ways my son has an easier time than the rest of us because he likes to follow rules; in other words, when he decided to go gluten free—he just did it and never cheats whereas the rest of us have more trouble. We wish we had his willpower.” Lack of independent skills and abilities was a common subtheme within the perceived barriers to health transition free-text comments. Adolescents’ inability to drive themselves to appointments was a significant concern to some parents. One parent wrote, “my daughter cannot drive (too distracted)”. Another parent stated, “my child doesn’t drive so I have to schedule his appts”. A third parent commented, “another barrier is my daughter not having a driver’s license.” The final subtheme recognized by parents was the lack of supporting resources in the health transition process. For instance, some statements indicated that parents might be struggling with their own transitions: “A big barrier is making time to remember to encourage him to take over tasks rather than doing them for him”. Another wrote, “I lack the skill on ‘how’ to let go of that aspect.” A few parents expressed exhaustion as indicated by one parent who stated, “Just straight up overwhelmed. It’s hard to remember every little thing I should be doing for my children. It’s especially hard to look toward the future and making them independent when we have so much happening in the moment.”
4. Discussion
This study revealed differences between parents and adolescents in their perceptions of health self-management as well as areas of agreement between them. Research on the transition to health self-management into adulthood is limited. The lack of empirical data could suggest that adolescents with ASD may not engage in HSM behaviors, or alternatively that this phenomenon is not being studied. Examining this multifactorial process can provide a better understanding of the adolescent’s engagement, the family’s involvement, and their perspectives on support received from provider(s) for HSM behaviors. Most individuals with ASD have a comorbidity, resulting in premature mortality for many, but we know little about what individuals with ASD are doing to learn to manage their lifetime health or how best to support that process. This study therefore provides adolescents’ and parents’ perceptions of HSM behaviors in transition age youth with ASD to examine what both are doing individually and together to enhance the adolescents’ HSM behaviors.
Understanding social facilitation occurring between adolescents and their parents offers insight for the delivery of psychoeducational interventions or support to families during this vulnerable period of development. Parents of children with ASD may lack sufficient knowledge to facilitate their child’s transition to increased health responsibility. In addition, parents may not provide supportive guidance and monitoring during transition, which can hinder adolescents’ readiness to engage in HSM behaviors.22, 28, 29
Future research to better inform the social facilitation process within transition health may consider adding the health providers perspective, improved measures that better capture this phenomenon, and increased supports for researchers in both qualitative and quantitative complementary research designs to provide a holistic approach. In the extended Adolescent Health Self-Management Model32, providers play a key role in supporting both contextual variables and the social facilitation process by providing quality care, supports, and resources. Therefore, their perspective regarding understanding of the process, their role in the process, and barriers to providing this support would be valuable.
The measures used in this study were based on our existing understanding on health transition for youth with special health care needs. Given the complexity and diversity of needs for individuals with ASD, measures addressing health transition and social facilitation will need the flexibility to be more person-centered. Poor validation of these measures within the ASD population serves as a significant barrier to this research method. Guiding frameworks such as the Adolescent Health Self-Management Model, should be considered in the development of future measures and then researched to assure reliability and validity. Furthermore, previous literature regarding health transition in youth having ASD has primarily been qualitative research. While much of this early research is exploratory making qualitative work particularly important, both qualitative and quantitative research can provide complementary insight and perspective. This is especially true given social and communication challenges known to exist in autism. Some of these youth may find completing a well-designed, structured survey measure easier to communicate their need or situation.
4.1. Adolescents’ and Parents’ Perceptions
Adolescents in this study rated their self-efficacy significantly higher than did their parents. According to Bandura’s self-efficacy theory45, confidence in one’s ability to achieve a specific behavior determines the behaviors in which one will engage, how long one will engage in them, and to what extent one will do so. The higher the confidence in the adolescent’s ability to transition to more independence, the more likely the adolescent and the parent are to achieve transition into the adolescent’s responsibility. Self-efficacy in this study exemplifies the process construct, “beliefs”. Over or under confidence as suggested by the self-efficacy findings may negatively impact the adolescents’ or parents’ engagement in social facilitation and subsequently the adolescent’s readiness to engage in HSM.
The finding for self-efficacy in the present study is consistent with previous research suggesting that parents of adolescents with ASD often lack confidence in their child’s interpersonal skills. In a study by Locke and Mitchell46, parents accurately predicted that their children would express more confidence than the parents did themselves. Indeed, many parents of adolescents with ASD receive little, if any, formal training in health transition.47 Given the great responsibility that parents carry in managing their children’s health needs, building confidence in a child’s abilities without support may be difficult. Research on other youth with special health care needs suggests that parents’ low self-efficacy with respect to their children’s and their own abilities may keep adolescents from having the opportunity to gain necessary transition skills and abilities.48, 49
Self-determination reflects human motivation, psychological development, and well-being.50 In this study it is represented by the process variable of learned health skills and abilities. Motivation to learn skills and engage in HSM may be negatively affected if not sufficiently supported by parents. For adolescents with ASD, self-determination skills can enhance problem-solving, decision-making, goal-setting, and self-monitoring. Adolescents in this study rated their self-determination significantly higher than their parents rated them in this area. To the best of our knowledge, this is the first study to compare adolescents with ASD and their parents on adolescents’ self-determination in relation to health transition. Emerging research on self-determination in youth with ASD almost always presents the parent’s perspective, far less often the youth’s perspective.39, 51 Research has focused on other factors or outcomes (quality of life, specific measurement use, or cognitive ability) instead of on self-determination’s association with health transition. Higher rates of self-determination have been linked to positive outcomes such as quality of life, social inclusion, better employment, and independent living for youth with ASD, apart from health transition. In a study of high-school students with ASD taking part in adult transition planning, students with higher self-advocacy, who spent more time in general education and who regularly discussed post high-school plans, were more active participants in the process.52
An unexpected finding of the study was the severity of depression in adolescents in the study. Depression in youth with ASD is a commonly co-occurring disorder that compromises adaptive functioning and quality of life.53 On our Background Information form, 22.5% of adolescent participants were identified by their parents as having been diagnosed with depression. However, this study’s depressive symptom measure suggested that 36% of adolescents and 45% of parents indicated a moderate to severe level of adolescent depressive symptoms. This discrepancy suggests possible undertreatment of depression in the sample. Given the association between depression and heightened physical comorbidities (gastrointestinal problems, seizure), the presence of depressive symptoms is important.53 In a review of the literature, Hudson et al.54 found that significantly elevated lifetime rates of depression in individuals with ASD were associated with self-report more than with caregiver report; individuals with ASD are four times more likely than the general-public to experience depression in their lifetime. Adolescents with ASD and their parents should be made aware of resources to address depression, and future research exploring why they are unaware or do not seek treatment for depression is necessary.
4.2. Social facilitation in transition
Despite the absence of formal transition programs, some transition of health management from parents to their adolescent children was occurring in this sample. The level of reported motivation and active participation by the adolescents in HSM is encouraging, especially given that half of the adolescents were 12–14 years old. Over half of adolescents and close to three quarters of their parents agreed that the parents were teaching their children about medications and how to talk to their doctor. Adolescents also were learning how to monitor for and prevent illness. Unfortunately, some aspects of health transition were not being taught, perhaps due to lack of resources, support, or awareness that health transition is vital for adolescents’ future well-being. With respect to self-management, tasks such as using adaptive devices, scheduling doctor/therapy appointments, and completing treatment regimens were infrequently reported. In the only other known study to examine health transition from the perspective of parents and adolescents with ASD, independent engagement in HSM for adolescents was found to be “challenging”.55 But, as in the present study, although many parents managed most aspects of their children’s health, small steps toward independence were being made.
Adolescents’ perspectives are key to understanding their engagement in HSM behaviors. Discrepancies between parents’ and adolescents’ perspectives on HSM behaviors underscore the importance of hearing directly from adolescents about their understanding of their HSM behaviors. There appears to be some discrepancy in what adolescents’ state they are doing on their own during social facilitation. Social facilitation between adolescents and parents during health transitions warrants further research, given the current lack of formal transition services. This is especially true given that parents’ and youths’ priorities and perspectives during transition do not always align.45, 56
4.3. Study limitations
This study used a convenience sample that was relatively homogenous. Although the author approached a broad variety of institutions, services, and providers serving individuals and families with ASD in many community settings, the study sample presents as mostly White, middle-class, two-parent families living in one large southwestern state. Future studies should examine a more demographically and geographically diverse sample to provide a better representation and understanding of the autism spectrum.
The study sample was recruited via reputable providers, service centers, and institutions providing care for individuals and families having ASD. However, individual diagnosis was not independently confirmed beyond parent report. Therefore, future studies may benefit from provider confirmed ASD diagnosis. One suggestion for future recruitment may include special education programs within the school districts where diagnosis has already been established.
Given the lack of instruments designed for youth with ASD, the use of existing scales for youth with special health care needs was necessary. Although the measures in this study indicated good reliability, there is also a need to assess HSM behaviors beyond self-report. It should be noted that after the conclusion of this study a new healthcare transition measure for youth with ASD57, The Health-related Independence Measure, was published. While this measure has shown good reliability and validity, this tool is completed by parents which limits its usefulness in meeting one of the goals of this study, which was to capture the perspective of the adolescent themselves. Perhaps this is the next step for the tool.
Finally, despite clearly stated guidelines, online survey research does not guarantee that solicited responses are obtained independently or from the intended participant. Also, the requirement that the adolescent be able to “speak for themselves” by completing the online survey independently excluded individuals whose cognitive limitations precluded their participation. Future studies should explore other ways to solicit feedback from adolescents with ASD. Caregivers’ and providers’ perspectives may be helpful, but only an individual with ASD can speak to the experience of having ASD.
5. Implications for practice
Gaps in what parents are teaching and what adolescents are doing, and significant differences between parents’ and adolescents’ perceptions, reinforce the need for guidance from health professionals as adolescents move toward more independent HSM. Parents report many barriers to teaching HSM behavior. Competing family priorities was the most common barrier reported by parents (43%). For parents of children with ASD, perceived family burden has been associated with lower treatment adherence in previous studies.58 What parents teach, and whether parents teach HSM behavior, may be influenced by the perceived impact that it has on the family. Future research should explore innovative ways to provide parent teaching that do not make increased demands on over-burdened parents, such as use of on-line resources, for example. Teachers in schools have a key role to play here as well. As they build the communication and self-determination skills of adolescents with ASD, they can reinforce the importance of using these skills in the health arena as well as in other areas of the adolescents’ lives. Furthermore, in a study of post-school vocational and academic outcomes identified in youths’ individualized education plans, support services were not reliably implemented.59 Therefore, a more efficient use of skills already identified and taught may be warranted.
Furthermore, programs that support interdisciplinary care and research such as the Leadership Education in Neurodevelopmental and Related Disabilities (LEND) programs, are key in supporting this population and their families. More interdisciplinary supports and collaboration between providers may also ease the health care burden placed on parents.
6. Conclusion
This examination of the transition to increased health responsibilities for youth with ASD aligns well with research on factors impacting other types of transition. Previous research has underscored the need for guided transition services that support parents in transition as adolescents assume planned incremental responsibility for HSM.16, 19 As such, our study contributes important aspects of social facilitation and initial data targeting current transition trends occurring between adolescents with ASD and parents that may inform providers supporting these individuals and families.
CRediT authorship contribution statement
Jamie L Rock: Conceptualization, Visualization, Methodology, Writing – original draft, Formal Analysis. Heather A Becker: Validation, Formal Analysis, Supervision, Writing – review & editing
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical statement
We, Jamie L Rock and Heather A Becker, consciously assure that for the manuscript Exploring Adolescent and Parent Perspectives on Facilitating Health Self-Management in Adolescents with Autism Spectrum Disorder the following is fulfilled:
-
2)
This material is the authors' own original work, which has not been previously published elsewhere.
-
3)
The paper is not currently being considered for publication elsewhere.
-
4)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
5)
The paper properly credits the meaningful contributions of co-authors and co-researchers.
-
6)
The results are appropriately placed in the context of prior and existing research.
-
7)
All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
-
8)
All authors have been personally and actively involved in substantial work leading to the paper and will take public responsibility for its content.
It is understood that violation of the above Ethical Statement rules may result in consequences.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Jamie L. Rock, Email: jamie.rock@wsu.edu.
Heather A. Becker, Email: hbecker@mail.nur.utexas.edu.
Data availability
Data will be made available on request.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental health disorders (5th ed.); 2013. 〈https://www.psychiatry.org/psychiatrists/practice/dsm〉.
- 2.Centers for Disease Control and Prevention. Data & statistics on autism spectrum disorder; 2023. 〈https://www.cdc.gov/ncbddd/autism/data.html〉.
- 3.Soke G.N., Maenner M.J., Christensen D., Kurzius-Spencer M., Schieve L.A. Prevalence of co-occurring medical and behavioral conditions/symptoms among 4- and 8-year-old children with autism spectrum disorder in selected areas of the United States in 2010. J Autism Dev Disord. 2018;48(8):2663–2676. doi: 10.1007/s10803-018-3521-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Croen L.A., Zerbo O., Qian Y., et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814–823. doi: 10.1177/1362361315577517. [DOI] [PubMed] [Google Scholar]
- 5.Cummings J.R., Lynch F.L., Rust K.C., et al. Health services utilization among children with and without autism spectrum disorders. J Autism Dev Disord. 2016;46(3):910–920. doi: 10.1007/s10803-015-2634-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirvikoski T., Mittendorfer-Ruz E., Boman M., Larsson H., Lichtenstein P., Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016;208(3):232–238. doi: 10.1192/bjp.bp.114.160192. [DOI] [PubMed] [Google Scholar]
- 7.Autism Speaks. Autism and health: A special report by Autism Speaks. Autism Speaks; 2017. 〈https://www.autismspeaks.org/sites/default/files/2018–09/autism-and-health-report.pdf〉.
- 8.Doshi-Velez F., Ge Y., Kohane I. Comorbidity clusters in autism spectrum disorders: an electronic health record time-series analysis. Pediatrics. 2014;133(1):e54–e63. doi: 10.1542/peds.2013-0819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fulceri F., Morelli M., Santochi E., et al. Gastrointestinal symptoms and behavioral problems in preschoolers with autism spectrum disorder. Dig Liver Dis. 2016;48(3):248–254. doi: 10.1016/j.dld.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 10.Mannion A., Leader G., Healy O. An investigation of comorbid psychological disorders, sleep problems, gastrointestinal symptoms, and epilepsy in children and adolescents with autism spectrum disorder. Res Autism Spectr Disord. 2013;7(1):35–42. doi: 10.1016/j.rasd.2012.05.002. [DOI] [Google Scholar]
- 11.Rosenfeld C.S. Microbiome disturbances and autism spectrum disorders. Drug Metab Dispos. 2015;43(10):1557–1571. doi: 10.1124/dmd.115.063826. [DOI] [PubMed] [Google Scholar]
- 12.DaWalt L.S., Hong J., Greenberg J.S., Mailick M.R. Mortality in individuals with autism spectrum disorder: predictors over a 20-year period. Autism. 2019;23(7):1732–1739. doi: 10.1177/1362361319827412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Health Resources & Services Administration, Maternal and Child Health Bureau. The National Survey of Children's Health; 2018. 〈https://www.childhealthdata.org/learn-about-the-nsch/NSCH〉.
- 14.Maternal and Child Health Bureau Health Resour Serv Adm (HRSA) 2022 (Retrieved from Children and Youth With Special Health Care Needs: https://mchb.hrsa.gov/sites/default/files/mchb/programs-impact/nsch-data-brief-children-youth-special-health-care-needs.pdf) [Google Scholar]
- 15.Karpur A., Lello A., Frazier T., Dixon P.J., Shih A.J. Health disparities among children with autism spectrum disorders: analysis of the National Survey of Children’s Health 2016. J Autism Dev Disord. 2019;49(4):1652–1664. doi: 10.1007/s10803-018-3862-9. [DOI] [PubMed] [Google Scholar]
- 16.White, P.H., Cooley, W.C., Transitions Clinical Report Authoring Group, American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians. (2018). Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics, 142(5), Article e20182587. https://doi.org/10.1542/peds.2018–2587. [DOI] [PubMed]
- 17.Lozano P., Houtrow A. Supporting self-management in children and adolescents with complex chronic conditions. Pediatrics. 2018;141(Suppl. 3):S233–S241. doi: 10.1542/peds.2017-1284H. [DOI] [PubMed] [Google Scholar]
- 18.National Institute of Nursing Research. Self-Management: Improving quality of life for individuals with chronic illness; 2016, December. 〈https://www.ninr.nih.gov/newsandinformation/iq/self-management-workshop〉.
- 19.American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians, Transitions Clinical Report Authoring Group. (2011). Clinical report—Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics, 128(1), 182–200. 10.1542/peds.2011-0969. [DOI] [PubMed]
- 20.Betz C., Ferris M., Woodward J., Okumura M., Jan S., Wood D. The health care transition research consortium health care transition model: a framework for research and practice. J Pediatr Rehabil Med. 2014;7:3–15. doi: 10.3233/PRM-140277. [DOI] [PubMed] [Google Scholar]
- 21.Data Resource Center for Child and Adolescent Health 2016–2017 Natl Surv Children’s Health. 2019 〈https://www.childhealthdata.org/browse/survey/results?q=5482&r=1&r2=45〉 [Google Scholar]
- 22.Farmer J.E., Clark M.J., Mayfield W.A., et al. The relationship between the medical home and unmet needs for children with autism spectrum disorder. Matern Child Health J. 2014;18(3):672–680. doi: 10.1007/s10995-013-1292-z. [DOI] [PubMed] [Google Scholar]
- 23.Dang K., Bent S., Lawton B., et al. Integrating autism care through a school-based intervention model: a pilot study. J Clin Med. 2017;6(10) doi: 10.3390/jcm6100097. (Article) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheak-Zamora N.C., Teti M., First J. Transitions are scary for our kids, and they're scary for us”: family member and youth perspectives on the challenges of transitioning to adulthood with autism. J Appl Res Intellect Disabil. 2015;28(6):548–560. doi: 10.1111/jar.12150. [DOI] [PubMed] [Google Scholar]
- 25.Cramm J.M., Strating M.M.H., Roebroeck M.E., Nieboer A.P. The importance of general self-efficacy for the quality of life of adolescents with chronic conditions. Soc Indic Res. 2013;113(1):551–561. doi: 10.1007/s11205-012-0110-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schertz H.H., Lester J.N., Erden E., Safran S., Githens P. Challenges and contributors to self-efficacy for caregivers of toddlers with autism. Autism. 2020;24(5):1260–1272. doi: 10.1177/1362361319899761. [DOI] [PubMed] [Google Scholar]
- 27.Agarwal R., Heron L., Burke S.L. Evaluating a postsecondary education program for students with intellectual disabilities: leveraging the parent perspective. J Autism Dev Disord. 2021;51(7):2229–2240. doi: 10.1007/s10803-020-04676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heath G., Farre A., Shaw K. Parenting a child with chronic illness as they transition into adulthood: a systematic review and thematic synthesis of parents’ experiences. Patient Educ Couns. 2017;100(1):76–92. doi: 10.1016/j.pec.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 29.Reed-Knight B., Blount R.L., Gilleland J. The transition of health care responsibility from parents to youth diagnosed with chronic illness: a developmental systems perspective. Fam Syst Health. 2014;32(2):219–234. doi: 10.1037/fsh0000039. [DOI] [PubMed] [Google Scholar]
- 30.Tesfaye R., Courchesne V., Yusuf A., et al. Assuming ability of youth with autism: synthesis of methods capturing the first-person perspectives of children and youth with disabilities. Autism. 2019;23(8):1882–1896. doi: 10.1177/1362361319831487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DePape A.-M., Lindsay S. Lived experiences from the perspective of individuals with autism spectrum disorder: a qualitative meta-synthesis. Focus Autism Other Dev Disabil. 2016;31(1):60–71. doi: 10.1177/1088357615587504. [DOI] [Google Scholar]
- 32.Rock J., Becker H. Factors for nurses assisting adolescents with autism develop health self-management. J Nurse Pract. 2021;17(4):445–452. doi: 10.1016/j.nurpra.2020.10.024. [DOI] [Google Scholar]
- 33.Ryan P., Sawin K.J. The individual and family self-management theory: Background and perspectives on context, process, and outcomes. Nurs Outlook. 2009;57(4):217–225. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Verchota G., Sawin K.J. Testing components of a self-management theory in adolescents with type 1 diabetes mellitus. Nurs Res. 2016;65(6):487–495. doi: 10.1097/NNR.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 35.Cohen S.E., Hooper S.R., Javalkar K., et al. Self-management and transition readiness assessment: concurrent, predictive, and discriminant validation of the STARx questionnaire. J Pediatr Nurs. 2015;30(5):668–676. doi: 10.1016/j.pedn.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 36.UNC School of Medicine. UNC STARx Program: About the STARx Questionnaire; 2021. https://www.med.unc.edu/transition/transition-tools/trxansition-scale/.
- 37.Nazareth M., Hart L., Ferris M., Rak E., Hooper S., van Tilburg M.A.L. A parental report of youth transition readiness: the parent STARx questionnaire (STARx-P) and re-evaluation of the STARx child report. J Pediatr Nurs. 2018;38:122–126. doi: 10.1016/j.pedn.2017.08.033. [DOI] [PubMed] [Google Scholar]
- 38.R. Schwarzer M. Jerusalem, Generalized Self-Efficacy scale. In J. Weinman, S. Wright, & M. Johnston, Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). NFER-Nelson; 1995.
- 39.AIR Self-Determination Assessments The University of Oklahoma. Zarrow Cent Learn Enrich. 2019 (https://www.ou.edu/education/centers-and-partnerships/zarrow/self-determination-assessment-tools/air-self-determination-assessment) [Google Scholar]
- 40.Chou Y.-C., Wehmeyer M.L., Palmer S.B., Lee J. Comparisons of self-determination among students with autism, intellectual disability, and learning disabilities: a multivariate analysis. Focus Autism Other Dev Disabil. 2017;32(2):124–132. doi: 10.1177/1088357615625059. [DOI] [PubMed] [Google Scholar]
- 41.Shogren K., Wehmeyer M., Palmer S., et al. Examining the relationship between the ARC's self-determination scale and the American Institutes of Reasearch self-determination scale. Assess Eff Interv. 2008;33(2):94–107. doi: 10.1177/1534508407311395. [DOI] [Google Scholar]
- 42.White K., Flanagan T., Nadig A. Examining the relationship between self-determination and quality of life in young adults with autism spectrum disorder. J Dev Phys Disabil. 2018;30:735–754. doi: 10.1007/s10882-018-9616-y. [DOI] [Google Scholar]
- 43.PROMIS Health Meas. 2021 (https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis) [Google Scholar]
- 44.Elos S., Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 45.Bandura A. Self-efficacy: the exercise of control. W H Freeman. 1997 [Google Scholar]
- 46.Locke K.D., Mitchell G.E. Self-perceptions, parent-perceptions, and meta-perceptions of the interpersonal efficacy of adolescents with autism spectrum disorder. Res Autism Spectr Disord. 2016;31:19–29. doi: 10.1016/j.rasd.2016.07.006. [DOI] [Google Scholar]
- 47.Cheak-Zamora N.C., Yang X., Farmer J.E., Clark M. Disparities in transition planning for youth with autism spectrum disorder. Pediatrics. 2013;131(3):447–454. doi: 10.1542/peds.2012-1572. [DOI] [PubMed] [Google Scholar]
- 48.Fishman L.N., Barendse R.M., Hait E., Burdick C., Arnold J. Self-management of older adolescents with inflammatory bowel disease: a pilot study of behavior and knowledge as prelude to transition. Clin Pediatr. 2010;49(12):1129–1133. doi: 10.1177/0009922810379042. [DOI] [PubMed] [Google Scholar]
- 49.Sawin K.J., Bellin M.H., Roux G., Buran C.F., Brei T.J. The experience of self-management in adolescent women with spina bifida. Rehabil Nurs. 2009;34(1):26–38. doi: 10.1002/j.2048-7940.2009.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 50.Deci E.L., Ryan R.M. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psychol/Psychol Can. 2008;49(3):182–185. doi: 10.1037/a0012801. [DOI] [Google Scholar]
- 51.Cheak-Zamora N.C., Maurer-Batjer A., Malow B.A., Coleman A. Self-determination in young adults with autism spectrum disorder. Autism. 2020;24(3):605–616. doi: 10.1177/1362361319877329. [DOI] [PubMed] [Google Scholar]
- 52.Griffin M.M., Taylor J.L., Urbano R.C., Hodapp R.M. Involvement in transition planning meetings among high school students with autism spectrum disorders. J Spec Educ. 2014;47(4):256–264. doi: 10.1177/0022466913475668. [DOI] [Google Scholar]
- 53.Pezzimenti F., Han G.T., Vasa R.A., Gotham K. Depression in youth with autism spectrum disorder. Child Adolesc Psychiatr Clin North Am. 2019;28(3):397–409. doi: 10.1016/j.chc.2019.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hudson C.C., Hall L., Harkness K.L. Prevalence of depressive disorders in individuals with autism spectrum disorder: a meta-analysis. J Abnorm Child Psychol. 2019;47(1):165–175. doi: 10.1007/s10802-018-0402-1. [DOI] [PubMed] [Google Scholar]
- 55.Cheak-Zamora N.C., Teti M., Maurer-Batjer A., Koegler E. Exploration and comparison of adolescents with autism spectrum disorder and their caregiver's perspectives on transitioning to adult health care and adulthood. J Pediatr Psychol. 2017;42(9):1028–1039. doi: 10.1093/jpepsy/jsx075. [DOI] [PubMed] [Google Scholar]
- 56.Rehm R.S., Fuentes-Afflick E., Fisher L.T., Chesla C.A. Parent and youth priorities during the transition to adulthood for youth with special health care needs and developmental disabilities. Adv Nurs Sci. 2012;35(3):E57–E72. doi: 10.1097/ANS.0b013e3182626180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cheak-Zamora N., Petroski G., La Manna A., Beversdorf D., Farmer J. Validation of the health-related independence for young adults with autism spectrum disorder measure-caregiver version. J Autism Dev Disord. 2021;51(6):2036–2046. doi: 10.1007/s10803-020-04690-2. [DOI] [PubMed] [Google Scholar]
- 58.Hock R., Kinsman A., Ortaglia A. Examining treatment adherence among parents of children with autism spectrum disorder. Disabil Health J. 2015;8(3):407–413. doi: 10.1016/j.dhjo.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 59.Snell-Rood C., Ruble L., Kleinert H., et al. Stakeholder perspectives on transition planning, implementation, and outcomes for students with autism spectrum disorder. Autism. 2020;24(5):1164–1176. doi: 10.1177/1362361319894827. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.