Abstract
Background
Long-term hyperopia shift is a rare complication following cataract surgery, presenting significant clinical challenges in analysis and management.
Case presentation
A 52-year-old female with a history of high myopia and laser-assisted in-situ keratomileusis (LASIK) surgery presented with decreased vision in her left eye at the very fifth year after cataract surgery. The spherical equivalent in her left eye had increased to + 6.63 D. After thorough evaluation, the patient underwent secondary piggyback intraocular lens (IOL) implantation in the ciliary sulcus, resulting in high satisfaction.
Conclusions
This case of long-term hyperopia shift following cataract and LASIK surgeries provides valuable insights into potential etiologies and interventions for this uncommon complication.
Keywords: cataract surgery, LASIK surgery, hyperopia, high myopia, case report
Background
Cataract, a leading cause of vision impairment and blindness worldwide, is effectively treated through surgery. Postoperative refractive stability is crucial for improved quality of life. While refraction typically stabilizes at one week post-surgery, long-term hyperopia shift is a rare complication that warrants attention [1].
Case presentation
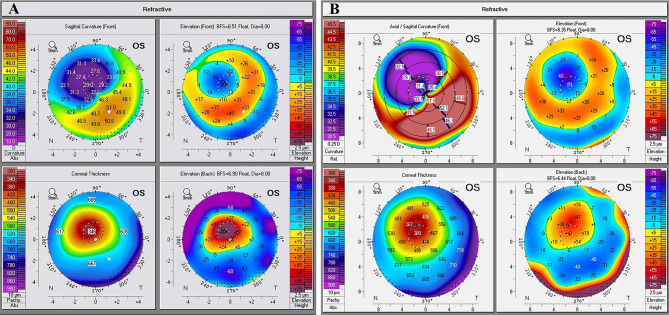
A 52-year-old female patient with a two-year history of complaints of decreased vision in the left eye was referred to ophthalmology. The patient had a history of extremely high myopia in both eyes and had undergone laser-assisted in-situ keratomileusis (LASIK) surgery in both eyes, with an eccentric small optical zone in the left eye, 20 years before (Fig. 1A). Moreover, seven years prior to the ophthalmology referral, she had undergone cataract surgery in both eyes. Both eyes implanted single-piece hydrophilic IOLs (Akreos MI60, Bausch and Lomb, New York, USA) using the Haigis-L formula to predict a -1.0D refractive target. The left eye had a UCVA of 20/100 and a BCVA of 20/40, with a refraction of + 2.5 diopter sphere (DS)/+1.0 diopter cylinder (DC)  at three months post-cataract surgery. At 12 months post-cataract surgery, the patient underwent yttrium aluminum garnet (YAG) laser posterior capsulotomy in both eyes due to posterior capsular opacification. The spherical equivalent (SE) of the left eye remained stable (+ 3.00 D to + 3.38 D) for four years postoperatively, while it suddenly increased to + 6.63 D at the fifth year and + 6.13 D at the seventh year post-surgery (Table 1, Fig. 1B). The right eye’s BCVA and SE remained stable throughout the seven-year period (Table 1). Examination revealed normal cornea, anterior chamber, IOL position, and fundus. The patient was diagnosed with long-term hyperopia shift in the left eye following cataract surgery.
at three months post-cataract surgery. At 12 months post-cataract surgery, the patient underwent yttrium aluminum garnet (YAG) laser posterior capsulotomy in both eyes due to posterior capsular opacification. The spherical equivalent (SE) of the left eye remained stable (+ 3.00 D to + 3.38 D) for four years postoperatively, while it suddenly increased to + 6.63 D at the fifth year and + 6.13 D at the seventh year post-surgery (Table 1, Fig. 1B). The right eye’s BCVA and SE remained stable throughout the seven-year period (Table 1). Examination revealed normal cornea, anterior chamber, IOL position, and fundus. The patient was diagnosed with long-term hyperopia shift in the left eye following cataract surgery.
Fig. 1.
Corneal topography images of the left eye obtained from Pentacam which was measured before cataract surgery (A) and seven years post-cataract surgery (B)
Table 1.
Clinical Parameters of the patient before and after cataract surgery
| Parameters | Baseline | 1d | 3 m | 5y | 7y | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| OD | OS | OD | OS | OD | OS | OD | OS | OD | OS | |
| BCVA | 0.5 | 0.2 | 0.8 | 0.3 | 0.8 | 0.5 | 0.8 | 0.5 | 0.8 | 0.5 |
| DS (D) | -7.50 | -17.00 | + 0.75 | 0.00 | + 1.00 | + 2.50 | + 1.25 | + 6.00 | + 1.25 | + 5.50 |
| DC (D) | -2.00 | -2.25 | + 1.50 | + 1.50 | + 1.00 | + 1.00 | + 1.25 | + 1.25 | + 1.25 | + 1.25 |
| SE (D) | -8.50 | -18.13 | + 1.50 | + 0.75 | + 1.5 | + 3.0 | + 1.88 | + 6.63 | + 1.88 | + 6.13 |
| AL (mm) | 30.95 | 32.10 | 31.40 | 32.28 | ||||||
| K1 (D) | 33.80 | 32.10 | 34.1 | 32.8 | 34.0 | 33.8 | ||||
| K2 (D) | 36.20 | 35.70 | 37.5 | 37.6 | 36.9 | 38.5 | ||||
| Kavg (D) | 34.90 | 33.80 | 35.7 | 35.4 | 34.70 | 36.0 | ||||
| ACD (mm) | 2.65 | 2.88 | 5.11 | 5.16 | ||||||
BCVA = best-corrected visual acuity; DS = diopter sphere; DC = diopter cylinder; SE = spherical equivalent; AL = axial length; Kavg = Average central corneal curvature; ACD: anterior chamber depth
Discussion and conclusions
Long-term hyperopia shift is a rare complication following cataract surgery. The first reason is posterior shift of the IOL over time and leading to an increase in the anterior chamber depth (ACD). Previous studies have found that capsular contraction syndrome leads to the posterior displacement of the IOL, capsule fibrosis, and an increased ACD [2]. Although no capsular shrinkage or contraction was observed in this patient, the postoperative ACD was significantly higher than the predicted ACD calculated using published formulas [3] (4.37 mm predicted vs. 5.16 mm postoperatively). Previous studies found that capsular contraction syndrome and refractive change can occur in IOLs of various materials, such as polymethylmethacrylate, silicone, and acrylic. However, the likelihood of IOL deformation and decentration may be increased while utilizing flexible material IOLs. The patient was implanted with single-piece hydrophilic IOLs, which was constructed of flexible materials that may have contributed to the IOL’s posterior shift [4]. Still, the change in the postoperative ACD was bilateral and symmetrical. The SE of the patient’s right eye remained stable at + 1.50 D. Therefore, the shift in the ACD could not completely explain the hyperopia state.
The flattening of the cornea or the posterior pole of the eyeball can also lead to acquired hyperopia. However, there was no significant difference in our patient’s mean corneal curvature over the seven-year period following the cataract surgery (Fig. 1). While the patient’s Kmax was determined to be abnormally high which may be caused by decentered ablation and resulted in an unusually flat and steep curvature. Post-LASIK corneal ectasia is also characterized by an increase in corneal curvature, while it leads to an exacerbation of myopia and astigmatism, rather than hyperopia. In our patient, there was little change observed in the corneal curvature or the front and back elevations, which eliminates the possibility of corneal ectasia. Despite this, it must be noted that the abnormally high Kmax could have led to an error in the IOL power calculation.
Furthermore, the flattening of the posterior pole and the shortening of the axial length may also contribute to a hyperopia shift. However, the fundus appeared normal in the patient, as confirmed by B-scan ultrasound and optical coherence tomography. And no significant difference was observed in this patient’s axial length over the seven years (Table 1).
Interestingly, the patient’s pupil size changed significantly after the cataract surgery (right eye: 1.5 mm pre-operatively vs. 2.64 mm post-operatively; left eye: 1.57 mm pre-operatively vs. 2.72 mm post-operatively). The patient may have experienced compensatory pupil constriction preoperatively to reveal the high-order aberrations in the pupil area. Postoperatively, the pupils of both eyes were dilated as a result of the improved binocular vision, the removal of blurring inhibition, and the reduction in early-stage inflammatory factors. However, the enlarged pupil caused a deterioration in the visual function of the patient’s left eye and the patient’s refractive error varied greatly in different regions. This was due to the irregular corneal surface and indicated poor visual fixation. Besides, the patient developed intolerable blurred vision in the left eye at 48 years old, which may have been related to a decline in the compensatory mechanisms. Therefore, the change in the IOL position, the dilated pupil size, the IOL power calculation error, and the subtle changes in the corneal curvature could all have led to the patient’s hyperopia shift.
A postoperative hyperopia shift can be treated with corneal rigid gas permeable (RGP) lenses, lamellar keratoplasty, or IOL replacement. However, due to the irregular corneal surface, the use of matching RGP lenses were not considered appropriate for our patient. Lamellar keratoplasty is unnecessary when the corneal curvature remains stable. In addition, IOL replacement is associated with a higher risk of injury, and the resultant changes in corneal refraction can be unpredictable. Based on such considerations, the decision was made to implant a piggyback IOL in the patient’s ciliary sulcus as a simpler and more effective treatment option (Fig. 2).
Fig. 2.
Anterior segment OCT images after piggyback IOL implantation in the ciliary sulcus
The SE was + 0.50 D and the BCVA was 20/50 in the patient’s left eye at six months postoperatively. No adverse events were observed. The patient expressed a high level of satisfaction with these outcomes.
We reported a case with long-term hyperopia shift following cataract surgery and laser-assisted in-situ keratomileusis (LASIK) surgery, which can provide clinicians with more clues to consider the reasons and interventions for this disease.
Abbreviations
- SE
spherical equivalent
- LASIK
laser-assisted in-situ keratomileusis
- UCVA
uncorrected visual acuity
- BCVA
best-corrected visual acuity
- DS
diopter sphere
- DC
diopter cylinder
- YAG
yttrium aluminum garnet
- TCRP
total corneal refractive power
- ACD
anterior chamber depth
Author contributions
XL.L. and YL.W. wrote the main manuscript text and C.L. prepared Figs. 1 and 2. All authors reviewed the manuscript.
Funding
This work was supported by Shanghai Eye Diseases Prevention &Treatment Center Foundation under Grant 22LC01004, and the National Natural Science Foundation of China under Grant No 82305319.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
No ethical approval required.
Consent for publication
Written informed consent was obtained from the patient to publish this article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaolei Lin and Can Li contributed equally to this work.
References
- 1.Charlesworth E, Alderson A J, Juan V, Elliott D B. When is refraction stable following routine cataract surgery? A systematic review and meta-analysis. Ophthalmic & physiological optics,2020,40(5):531–539. [DOI] [PubMed]
- 2.Kim T G, Moon S W. Hyperopic shift caused by capsule contraction syndrome after microincision foldable intraocular Lens implantation: case series. BMC Ophthalmol,2019,19(1):116. [DOI] [PMC free article] [PubMed]
- 3.Ning X, Yang Y, Yan H, et al. Anterior chamber depth-a predictor of refractive outcomes after age-related cataract surgery. BMC Ophthalmol,2019,19(1):134. [DOI] [PMC free article] [PubMed]
- 4.Liu Y L, Yang C M, Huang J Y, et al. Postoperative hyperopic shift after cataract surgery in silicone oil-filled eyes. Acta Ophthalmologica,2014,92(4). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.