Summary:
In this article, our technique for deep inferior epigastric pedicle dissection utilizing a midline fascial incision is described. Approaching these vessels via a midline facial incision provides facile access to the retrorectus space bilaterally, utilizes a dissection plane that facilitates preservation of nerve and muscle fibers, and allows for both efficient and ergonomic pedicle dissection. This method is safe and easily reproducible and may reduce abdominal donor site morbidity in deep inferior epigastric perforator flap breast reconstruction.
Takeaways
Question: Is approaching the deep inferior epigastric perforator (DIEP) pedicle through a midline fascial incision a better dissection technique?
Findings: Approaching the DIEP pedicle through a midline fascial incision is safe, easily reproducible, and may decrease donor site morbidity by decreasing muscle splitting and facilitating preservation of innervation.
Meaning: This approach to DIEP flap harvest may improve surgical efficacy and donor site outcomes in DIEP flap breast reconstruction.
INTRODUCTION
The evolution of autologous breast reconstruction is defined by technical innovations leading to decreased donor site morbidity and improved surgical efficiency. Perhaps the most significant step forward in this progression was popularization of the deep inferior epigastric perforator (DIEP) flap.1 As surgeons gained expertise in this procedure, further refinements have been aimed at minimizing fascial incisions and protecting rectus muscle innervation.2–5 Nonetheless, many of these techniques have not gained widespread adoption, perhaps due to educational barriers or lack of reproducibility. In this article, our technique for DIEP pedicle dissection through a midline fascial incision is described. This method is safe and easily reproducible and may reduce abdominal donor site morbidity in DIEP flap breast reconstruction.
DESCRIPTION OF SURGICAL TECHNIQUE
Flap elevation begins with usual isolation of perforators. In our practice, indocyanine green angiography is routinely performed to assist in perforator selection. Selected perforators are then dissected from the fascia and through their intramuscular course with care to preserve crossing nerves. Once intramuscular dissection is complete, a midline facial incision along the linea alba is made, as seen in Figure 1. Of note, when a medial perforator is selected, the facial incision used to dissect the perforator is typically carried into the midline facial incision, whereas when a lateral perforator is selected, a fasciotomy is made to free the perforator, it is dissected through the muscle, and at that point the remaining dissection is completed in the retrorectus space via the separate midline fasciotomy.
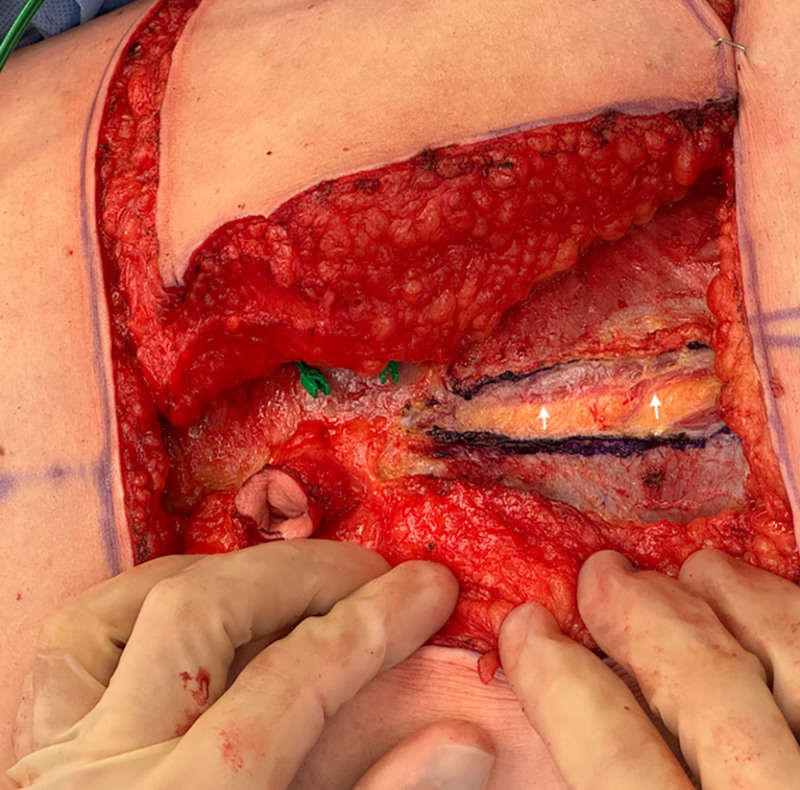
Fig. 1.
The midline fascial incision is made after identifying 2 adjacent perforators in the middle third of the left rectus muscle. The linea alba was marked and opened. The medial edge of the left rectus abdominis is seen below the fascia (arrows).
Pedicle dissection is performed from the contralateral side of the table. The medial edge of the rectus abdominis muscle is identified and lifted from the peritoneum to begin developing the retrorectus space. Weitlaner retractors are then placed with one prong on the peritoneum and the other on the rectus abdominis. The purpose of these retractors is two-fold. As the prongs are carefully spread, they assist in developing the retrorectus space by further peeling the rectus abdominis from the peritoneum. Additionally, this maneuver creates an optical window that is used for pedicle identification and dissection, as seen in Figures 2 and 3. The pedicle is easily visualized in this plane, and dissection from the selected perforator(s) superiorly to vessel origin inferiorly is completed with ligation of vascular branches and unused perforators. Of note, this optical window is ergonomic for the surgeon, who is looking across the patient and toward the contralateral pelvis for flap harvest. In bilateral cases, both pedicles are accessed via the same midline fascial incision. Figure 4 displays closed fasciotomies after the dissection depicted in Figures 2 and 3. (See figure, Supplemental Digital Content 1, which displays fasciotomies in a patient with perforators located in the middle one-third of the rectus muscle bilaterally. http://links.lww.com/PRSGO/D698.) (See figure, Supplemental Digital Content 2, which displays fascial closure in this patient. http://links.lww.com/PRSGO/D699.)
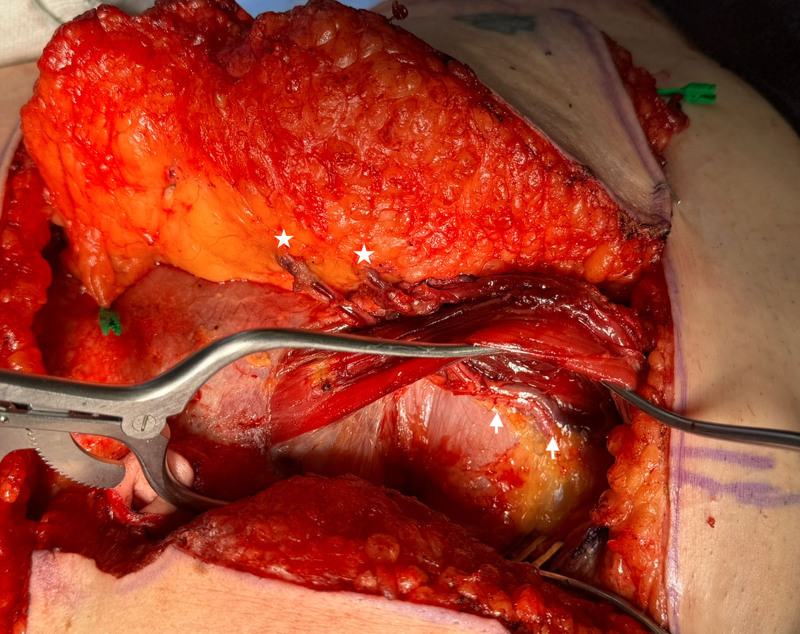
Fig. 2.
The left retrorectus space is exposed from the contralateral side of the table facilitated by Weitlaner retractors. One Weitlaner prong pushes up the rectus muscle, whereas the other prong pushes down the peritoneum creating an optical window for pedicle dissection. Two perforators can be seen coursing through the rectus and entering the flap (stars), and the pedicle can be seen in the retrorectus space coursing toward the groin (arrows).
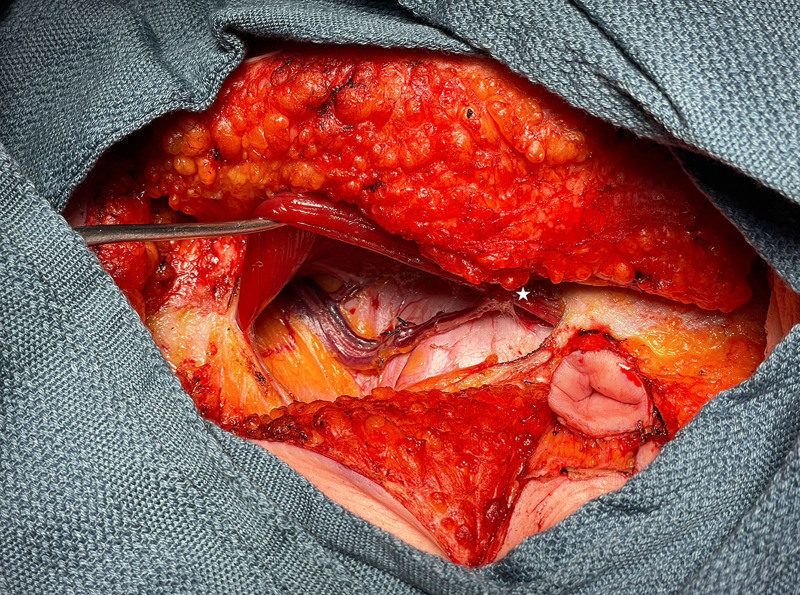
Fig. 3.
The right retrorectus space is exposed from the contralateral side of the table facilitated by a Weitlaner retractor. A septocutaneous perforator can be seen entering the flap (star), and the pedicle can be seen in the retrorectus space coursing towards the groin.
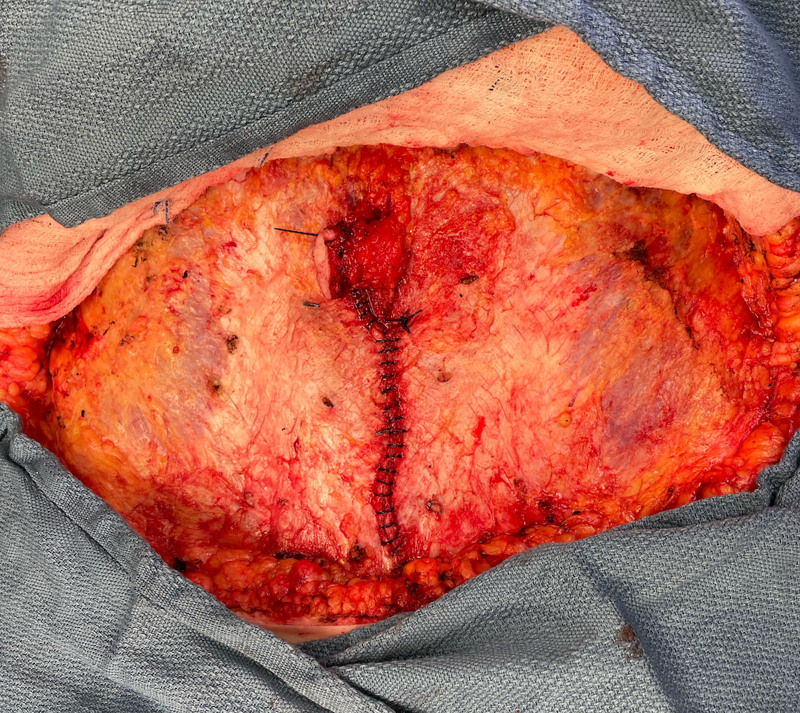
Fig. 4.
Closed fasciotomies after bilateral DIEP flaps were harvested. On the left hemiabdomen, 2 medial row perforators were selected, as pictured in Figure 2. On the right hemiabdomen, a septocutaneous perforator just inferior to the umbilicus was selected, as pictured in Figure 3. Note, there is one midline fascial incision to close.
DISCUSSION
In this article, our technique for DIEP flap pedicle dissection utilizing a midline fascial incision is described. This straightforward and easily reproducible approach provides three main benefits: (1) Facile access to the retrorectus space allows for pedicle identification, dissection, and harvest bilaterally via a single incision; (2) pedicle dissection in the retrorectus plane via a medial incision facilitates preservation of maximum muscle and crossing nerve fibers; and (3) dissecting the pedicle in the retrorectus plane via this optical window is efficient and ergonomic for the surgeon.
Retrorectus pedicle dissection through a midline incision limits muscular dissection because no further muscle splitting is required once the perforator is dissected through the rectus abdominis. We hypothesize that this technique may decrease donor site morbidity due to increased muscular and crossing nerve preservation, as previous studies have shown that the extent of muscular dissection correlates with this.6,7 Additionally, less need for rectus retraction may decrease postoperative pain and traction neuropraxia, potentially facilitating recovery. Further study is needed to investigate whether the presented technique significantly impacts abdominal weakness, hernia, or bulge rates compared with traditional dissection methods.
We have found this technique particularly simplifies dissection of septal perforators and perforators penetrating the most medial fibers of the rectus abdominis, such as the frequently selected periumbilical perforator. In these instances, the fascial incision made for perforator dissection is continued inferiorly as the midline fascial incision. Nevertheless, we find this technique beneficial regardless of perforator locations or configurations and use it in almost every DIEP flap. A situation when the described technique may not be beneficial is when a lateral perforator with a very long intramuscular course is selected, as it may not require much additional pedicle dissection once it exits the rectus muscle. Preoperative imaging facilitates perforator selection and dissection planning to minimize morbidity.8 We have also used this pedicle dissection technique with flaps necessitating abdominal perforator exchange and when harvesting deep inferior epigastric composite grafts through a Pfannenstiel or minitummy tuck incision for use in lumbar flap breast reconstruction.
In patients with a history of previous midline incisions such as those who have undergone exploratory laparotomy and in those with extensive scarring from cesarian section, care must be taken to avoid injury to the peritoneum, as scarring can obscure fascial planes. Nonetheless, we have not found these situations to preclude use of the presented technique. In instances where peritoneal injury has occurred, it is repaired with 0 Vicryl suture. No bowel injuries have occurred with this technique; however, caution should be used, as it is hypothetically possible. Caution should also be taken to avoid excessive force against the peritoneum when deploying Weitlaner retractors, as this could theoretically cause compression of the great vessels, particularly in very thin patients who sometimes exhibit a palpable abdominal aortic pulse through the peritoneum.
This pedicle dissection technique has been consistently utilized in our practice over the past 2 years, and we have found it to be safe and easily reproducible. We believe utilizing a midline fascial approach to pedicle dissection can minimize donor site morbidity, facilitate surgical efficiency and ergonomics, and improve outcomes in DIEP flap breast reconstruction.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 19 December 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. [DOI] [PubMed] [Google Scholar]
- 2.DellaCroce FJ, DellaCroce HC, Blum CA, et al. Myth-busting the DIEP flap and an introduction to the abdominal perforator exchange (APEX) breast reconstruction technique: a single-surgeon retrospective review. Plast Reconstr Surg. 2019;143:992–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shakir S, Spencer AB, Kozak GM, et al. Laparoscopically assisted DIEP flap harvest minimizes fascial incision in autologous breast reconstruction. Plast Reconstr Surg. 2020;146:265e–275e. [DOI] [PubMed] [Google Scholar]
- 4.Selber JC. The robotic DIEP flap. Plast Reconstr Surg. 2020;145:340–343. [DOI] [PubMed] [Google Scholar]
- 5.Martinez CA, Boutros SG. Outpatient microsurgical breast reconstruction. Plast Reconstr Surg Glob Open. 2020;8:e3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee KT, Park JW, Mun GH. Impact of rectus muscle injury during perforator dissection on functional donor morbidity after deep inferior epigastric perforator flap breast reconstruction. Plast Reconstr Surg Glob Open. 2019;7:e2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stecco C, Azzena GP, Macchi V, et al. Rectus abdominis muscle innervation: an anatomical study with surgical implications in DIEP flap harvesting. Surg Radiol Anat. 2018;40:865–872. [DOI] [PubMed] [Google Scholar]
- 8.Rozen WM, Palmer KP, Suami H, et al. The DIEA branching pattern and its relationship to perforators: the importance of preoperative computed tomographic angiography for DIEA perforator flaps. Plast Reconstr Surg. 2008;121:367–373. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.