Abstract
Background:
Prenatal myelomeningocele (MMC) repair offers significant benefits over traditional postnatal repair, as demonstrated by the Management of Myelomeningocele Study trial. We characterize the current specialist involvement in prenatal and postnatal MMC repair.
Methods:
The top 50 US News Children’s Hospitals for Neonatology and Neurology/Neurosurgery were queried, resulting in 67 unique hospitals. Specialties involved in MMC repair were extracted via hospital websites and surveys.
Results:
Among the 58 hospitals included, only 18 (31%) offered both prenatal and postnatal MMC repair, and the remaining 40 (69%) offered postnatal repair only. Of the 40 hospitals offering postnatal repair only, neurosurgeons (n = 38), orthopedic surgeons (n = 34), and urologists (n = 33) were most often included. Of the 18 hospitals with prenatal repair, neurosurgeons (n = 18) and maternal–fetal medicine specialists (n = 14) were most commonly involved. Prenatal teams had pediatric and fetal surgeons involved more often than postnatal teams (P = 0.011 and P = 0.035, respectively). Only 7 prenatal teams included fellowship-trained fetal surgeons. Teams led by fetal surgeons always included neurosurgeons (n = 7) and maternal–fetal medicine specialists (n = 7) and were least likely to include plastic surgeons (n = 1).
Conclusions:
These data emphasize both the delayed adaptation of fetal repair of MMC by major children’s hospitals and lack of fellowship-trained specialists involved; only 31% of the major children’s hospitals offer prenatal repair of MMC, with only 39% of those hospitals being led by a fellowship-trained fetal surgeon. These data highlight the need for additional teams trained in prenatal MMC repair as well as the standardization of fetal surgery fellowships to allow for the development of prenatal repair teams.
Takeaways
Question: What is the current status of practice and specialist involvement in prenatal repair of spina bifida in the United States?
Findings: Only 31% of the major children’s hospitals in the United States offer prenatal repair of myelomeningocele (MMC) and only 39% of those hospitals are led by a fellowship-trained fetal surgeon. These data emphasize both the delayed adaptation of fetal repair of MMC by major children’s hospitals and lack of fellowship-trained specialists involved.
Meaning: Our study highlights the need for additional teams trained in prenatal MMC repair and the standardization of fetal surgery fellowships to allow for the development of prenatal repair teams.
INTRODUCTION
Myelomeningocele (MMC), the most severe form of spina bifida, is characterized by incomplete neural tube closure causing protrusion of a fluid-filled sac and causes lasting disabilities.1 Postnatal repair within 48 hours has been the conventional treatment for MMC but is often complicated by the development of a hydrocephalus, necessitating the placement of a cerebrospinal fluid shunt.2 In 2011, a landmark randomized controlled trial, Management of Myelomeningocele Study (MOMS), suggested a shift to in utero repair for improved patient outcomes.3 Substantial data have demonstrated that prenatal surgery reduces the need for shunting and improves neurosurgical, motor, and urological outcomes, although at an increased risk of uterine dehiscence and preterm delivery.4–6 Fetoscopic repair is a promising alternative to open prenatal MMC repair aimed at lowering maternal risks.7 Over the past few decades, immense progress has occurred in the treatment of MMC that has decreased the debilitating impacts of MMC from infancy through transition to adulthood.
With the shift in treatment of MMC to prenatal and fetoscopic repair comes increasing complexity of treatment. Recent paradigm shifts have been introduced in training and maternal–fetal medicine (MFM) with the development of 2-year fellowships in fetal or perinatal surgery. Only 7 of these programs exist in the United States, with the first being established in 1990 at the Children’s Hospital of Pennsylvania, and none of which are American College of Graduate Medical Education accredited. They aim to provide clinical and research experience designed for the treatment of complex fetal abnormalities such as prenatal repair of MMC. However, there is great variability in the eligibility and research experience of the fellowship programs. Research requirements range from 0 to 2 years, and some have inclusion or exclusion criteria based on the completion of MFM or pediatric surgery training.
Whereas the distribution of prenatal versus postnatal care offered to children diagnosed with MMC is evolving, it has been almost 13 years since the MOMS was published, and it remains unclear how many of our major children’s hospitals offer prenatal care of meningomyelocele. Moreover, because repair for MMC is time-sensitive and technically challenging, large pediatric hospitals are typically the only institutions to offer the most effective prenatal intervention.8 The present study was performed to characterize the current state of MMC repair at the major children’s hospitals in the United States. We characterized the care teams and specialists involved in prenatal and postnatal MMC repair at various US children’s hospitals to report on the current status of practice for MMC treatment. Examining the physicians’ specialties involved at the time of diagnosis and treatment of MMC, along with their training and experience, may present an opportunity to optimize the composition of these teams as fetal repair of MMC becomes more widespread. Potentially leveraging increased appreciation of the experience and specialists required to provide the highest level of fetal care and surgery will be critical to increase accessibility and optimize care for children and mothers diagnosed with MMC.
METHODS
Inclusion Criteria
The publicly available top 50 US News Children’s Hospitals for Neonatology and top 50 for Neurology and Neurosurgery were queried, totaling 100 hospitals with 33 overlapping between the lists, resulting in 67 unique hospitals that were searched for MMC repair information. These lists were used because our study sought to explore the practice of MMC repair in major US hospitals. The criterion for inclusion was to be on either one of the aforementioned top 50 hospitals lists. If a hospital did not offer MMC repair or the information could not be obtained from our data collection protocol, then they were excluded from the study.
Collection Methods
Data regarding specialist involvement were gathered in 2 steps. First, hospital websites were reviewed for publicly available data on specialist teams involved in either prenatal or postnatal MMC repair. Second, a structured survey was sent to the hospitals, requesting additional details on specialist involvement that were not available on the hospital website. The survey asked if the hospital offered prenatal, postnatal, or fetoscopic MMC repair; which specialists are involved in either repair; and what training surgeons received for fetoscopic repair. If the team involved a fetal surgeon, details on where the surgeon had completed a 2-year fetal surgery fellowship were collected. Follow-up was conducted via email and phone call. Bias from variability in data reporting was attempted to be mitigated by confirming specialties through phone or email. If information was not available via website, email, or phone, the hospital was excluded from the study.
Data Analysis
Systematic measures were taken to ensure consistency and accuracy in data collection. Detailed spreadsheets were kept to track each hospital’s specialist involvement and survey status. All specialist data collected fit into the standardized 10 specialties presented in this study. Data collectors were trained to follow a standardized protocol, and software tools were used to ensure consistency in the analysis of data across all sources. Data were analyzed using binomial tests comparing the proportion of specialists for a specialty between prenatal and postnatal repair. χ2 analyses were also conducted to compare the distribution of specialties between prenatal and postnatal repair. Statistical significance was established for a P value of less than 0.05.
RESULTS
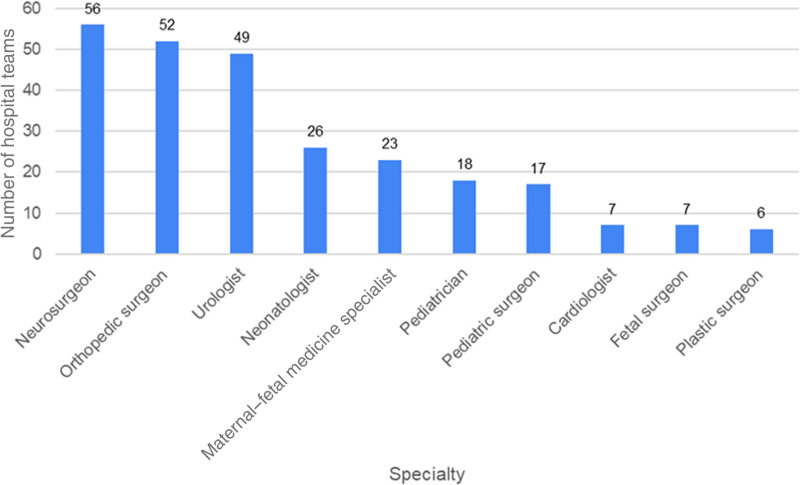
Specialties Involved in All Cases of MMC Repair
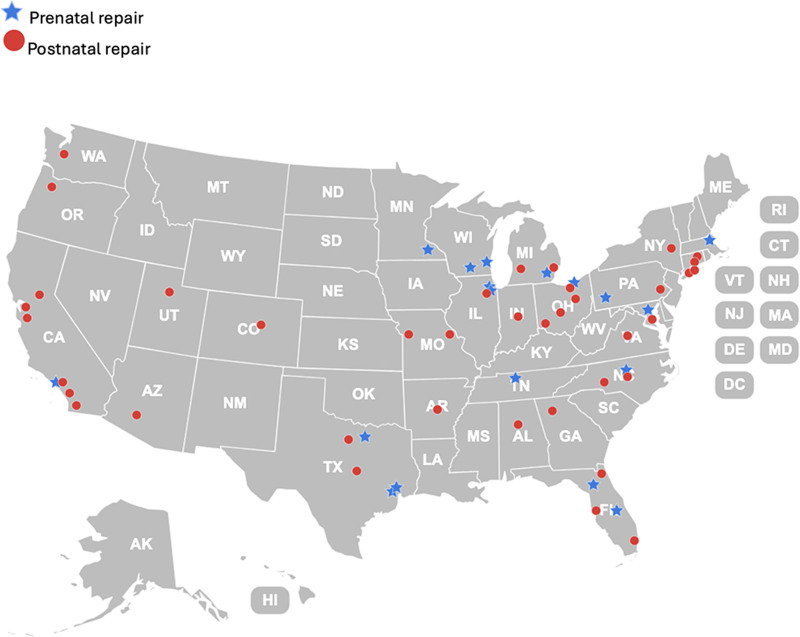
A total of 58 hospitals that offered either prenatal or postnatal MMC repair were included in the study (Fig. 1). Figure 2 depicts the specialty distribution for all 58 hospitals offering MMC repair. Neurosurgeons (n = 56), orthopedic surgeons (n = 52), and urologists (n = 49) were most often involved for all hospitals that offered MMC repair. Cardiologists (n = 7), fetal surgeons (n = 7), and plastic surgeons (n = 6) were least often involved in MMC repair.
Fig. 1.
Map of hospitals offering prenatal (n = 18) versus postnatal repair (n = 40) in the United States. Prenatal repair hospitals are indicated by the blue star and postnatal by a red circle.
Fig. 2.
Specialties involved in all cases of MMC repair (n = 58 hospitals). A total of 58 hospitals offered MMC repair, and teams from all 58 hospitals are included in Figure 1.
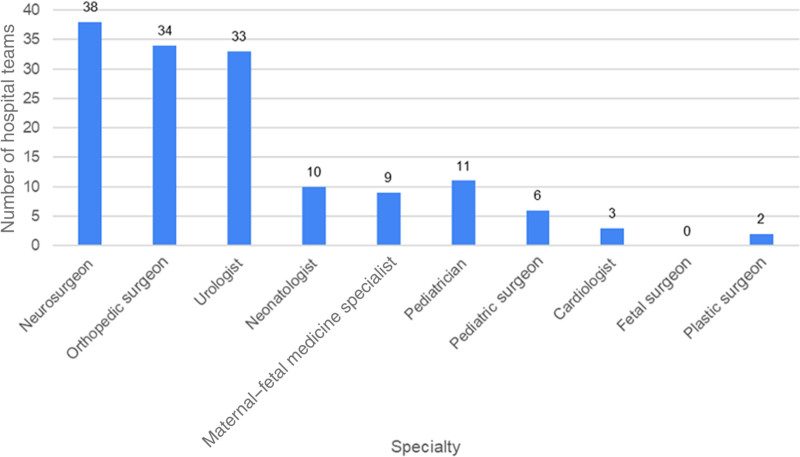
Specialty Distribution for Hospitals With Postnatal Care Only
Of the 58 hospitals, 40 (69%) offered postnatal repair only. Among these 40 hospitals, neurosurgeons (n = 38), orthopedic surgeons (n = 34), and urologists (n = 33) were most often included on the teams (Fig. 3). Cardiologists (n = 3), plastic surgeons (n = 2), and fetal surgeons (n = 0) were least often involved in postnatal MMC repair of the 40 hospitals that offered only postnatal MMC repair.
Fig. 3.
Specialties involved in hospitals only offering postnatal MMC repair (n = 40 hospitals). A total of 40 hospitals offered postnatal MMC repair only, and teams from these 40 hospitals are included in Figure 2.
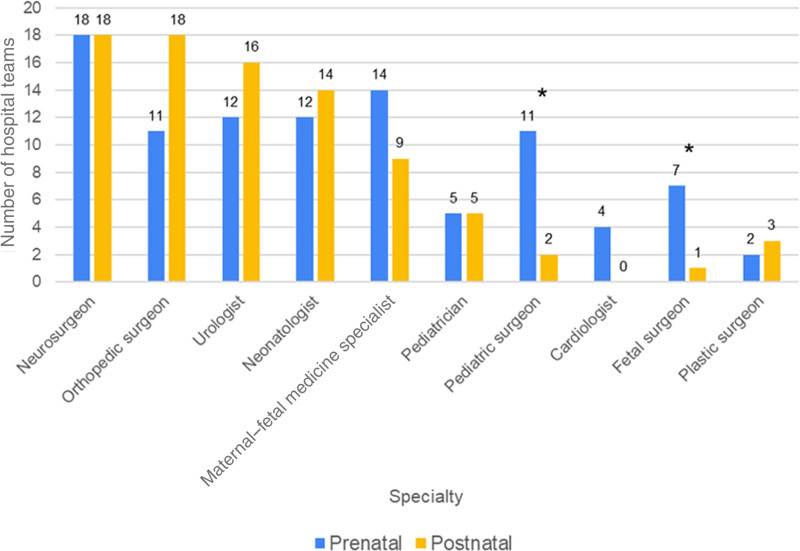
Specialty Distribution for Hospitals With Prenatal and Postnatal MMC Repair
Of the 58 hospitals, 16 (31%) offered prenatal repair of MMC, and all of these hospitals also offered postnatal MMC repair. Neurosurgeons were involved in all 18 teams for both prenatal and postnatal repair (Fig. 4). MFM (n = 14), neonatology (n = 12), and urology (n = 12) specialists were most frequently involved in prenatal repair. Orthopedic surgeons (n = 18), urologists (n = 16), and neonatologists (n = 14) were more frequently a part of postnatal repair. Fetal surgeons, pediatricians, cardiologists, and plastic surgeons were least often a part of the teams for both prenatal and postnatal repair. Ten hospitals offered prenatal fetoscopic repair of MMC, and fetal surgeons were involved 60% of the time in these teams.
Fig. 4.
Specialty distribution for hospitals offering both prenatal and postnatal MMC repair (n = 18 hospitals). A total of 18 hospitals offered both prenatal and postnatal MMC repair, and teams from these 18 hospitals are included in Figure 3. The rate of involvement of a pediatric surgeon and a fellowship-trained fetal surgeon was significantly higher in prenatal repair teams (n = 11 and n = 7, respectively) compared with postnatal repair (n = 2 and n = 1, respectively) (P = 0.011 and P = 0.035, respectively). Asterisks (*) represent a statistically significant difference.
Of the 18 hospitals, 7 (39%) that offered prenatal repair included a fellowship-trained fetal surgeon as a part of the prenatal repair team. However, the fetal surgeon remained involved in postnatal MMC repair in only 1 of the 7 hospitals. Of the 18 hospitals that offered both prenatal and postnatal repair, the rate of involvement of a pediatric surgeon and a fellowship-trained fetal surgeon was significantly higher in prenatal repair teams (n = 11 and n = 7, respectively) compared with postnatal repair (n = 2 and n = 1, respectively) (P = 0.011 and P = 0.035, respectively). The differences between MFM specialist and orthopedic surgeon involvement between prenatal and postnatal repair teams were not significant.
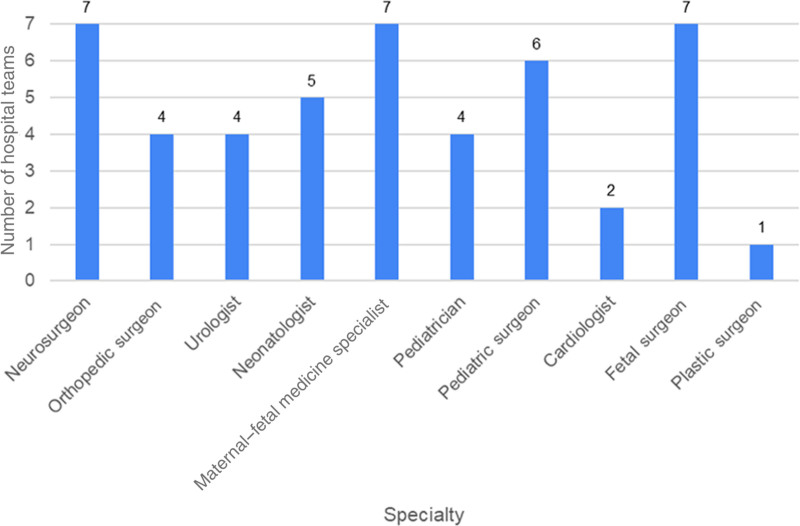
Specialties Involved in Teams Led by Fetal Surgeons
A total of 7 hospitals offered prenatal MMC repair teams led by fetal surgeons. These hospitals are Boston Children’s Hospital, Texas Children’s Hospital, Johns Hopkins Children’s Center, Children’s Memorial Hermann Hospital, Cleveland Clinic Children’s Hospital, University of Michigan Health C.S. Mott Children’s Hospital, and Ann and Robert H. Lurie Children’s Hospital. The fetal surgeons obtained fellowship training at Baylor College of Medicine (n = 3), University of California San Francisco (n = 2), and Children’s Hospital of Philadelphia (n = 2). All teams led by fetal surgeons included neurosurgeons (n = 7) and MFM specialists (n = 7) (Fig. 5). Teams offering prenatal repair of MMC were next most likely to include pediatric surgeons (n = 6) and least likely to include plastic surgeons (n = 1).
Fig. 5.
Specialties involved in prenatal MMC repair teams led by fetal surgeons (n = 7 hospitals). A total of 7 hospitals had fetal surgeons included in prenatal MMC repair, and specialties from these 7 prenatal repairs are included in Figure 4.
DISCUSSION
Modern fetal surgery first emerged after the development of in utero interventions at the University of California San Francisco by Dr. Harrison (pediatric surgery), in collaboration with Dr. Longaker (plastic surgery) and Dr. Adzik (pediatric surgery).9 The subsequent MOMS trial proposed by Dr. Farmer has since expanded their initial research and highlighted improved outcomes of open fetal MMC repair.3 Although plastic surgery and pediatric surgery were involved in the development of these trials, this should not have any bearing on the specialties needed for prenatal repair of MMC, particularly because much of this work was completed before the researchers entering their specialties of choice. Prenatal repair has become a validated form of treatment for MMC, with demonstrated benefits over postnatal repair of MMC. However, our study identified that only 18 of the 58 (31%) major children’s hospitals surveyed offered prenatal repair of MMC, 12 years after the completion of the MOMS. Of the 18 prenatal teams, 7 included a fellowship-trained fetal surgeon, whereas 11 involved specialists who did not complete a fetal surgery fellowship. Findings also demonstrated that postnatal teams most frequently involved neurosurgeons, orthopedic surgeons, and urologists, whereas prenatal teams most frequently involved neurosurgeons and MFM specialists. Teams may have included many peripheral members listed on their websites, however the essential leads of the team will consist of those who operate on the fetus during MMC repair, including fetal surgeons, neurosurgeons, pediatric surgeons, and MFM specialists. Our study highlights the complexity of team structure as well as scarcity of prenatal repair for MMC across the United States, emphasizing a need for broader development and subsequent availability of these multidisciplinary teams.
The limitations in access to fetal MMC repair are multifactorial, including cost, availability, and safety. However, the lack of surgeon availability is the focus of our study as the delay in the adoption of prenatal MMC repair may be attributed to the lack of standardization in training. Our study identified 11 teams performing prenatal MMC without a fellowship-trained fetal surgeon, which may indicate that specialists with proper experience and training may lead teams outside of a fetal surgery fellowship program. The 7 surgeons who were fellowship-trained received training from 3 institutions: Baylor College of Medicine (n = 3), University of California San Francisco (n = 2), and Children’s Hospital of Philadelphia (n = 2) fellowships. However, there is a lack of standardization among fellowship programs, with significant variability in research emphasis and eligibility criteria across programs. One can speculate that establishing and maintaining a fetal surgery program requires substantial resources, which likely contributes to the lack of fetal surgery training programs. However, there is a scarcity of prenatal MMC repair teams, irrespective of the training of their members. Our findings suggest that teams may be led by fellowship-trained fetal surgeons, neurosurgeons, MFM specialists, or surgeons without fellowship training, which may be a recent by-product of the growing pediatric fetal surgery experience. We also found that pediatric surgeons were involved in prenatal repair at a significantly higher rate than in postnatal repair, which suggests that pediatric surgeons may be a key component of prenatal MMC repair. Recent studies have demonstrated a shortage of pediatric surgeons in the United States, which may partly contribute to the limited access to prenatal repair in US hospitals.10
A notable geographic disparity in the availability of prenatal MMC repair was observed in this study. Only 1 program on the West Coast offered prenatal repair, whereas 7 programs in the Midwest and 6 on the East Coast offered prenatal repair. Hospitals on the West Coast relied more heavily on postnatal care. These differences could be attributed to a variety of factors, including availability of academic intuitions, access to specialized providers, and disparities in healthcare infrastructure and research. Further investigation of the potential impact of these geographic disparities is crucial, as it highlights the need for increased resource allocation to ensure equitable access to prenatal MMC care across all regions of the United States. Addressing these disparities could allow for improved outcomes in a broader population affected by MMC.
There is also a need for greater consistency of fellowship training for fetal surgeons, which should become the mode of practice as the specialty grows. The development of ACGME-approved fetal surgery fellowships with a clinical focus may be a solution in the future as the number of teams grows. These could formalize the pool of applicants from which developing teams may wish to recruit, to allow for growth of teams offering prenatal repair. However, it is important to recognize the value of experience in those teams led by non–fellowship-trained surgeons, as these may be the pioneers in a field in which American College of Graduate Medical Education–approved clinical fellowships do not exist.
In the period before the MOMS trial, a study estimated that 919 repairs of postnatal MMC occur per year in the United States from 1998 to 2010.11 Furthermore, our institution has averaged 24 cases of prenatal and 11.3 cases of postnatal repair annually over the last 16 years. On the basis of the estimate by Kshettry et al11 of 919 repairs annually nationwide and our institution’s annual volume, we can estimate that approximately 625 cases may be treated prenatally and 294 postnatally, requiring 26 teams to perform both prenatal and postnatal MMC repair. This would require a 45% increase in the number of teams performing prenatal repair, from the 18 teams which our study identified.
It is important to acknowledge the limitations of our study. The data collection methods relied on surveys and website information, which may not have captured the complete spectrum of surgical options offered at each of the 58 hospitals surveyed. A more comprehensive investigation could involve interviews with healthcare providers and collaboration with relevant medical societies to obtain a more accurate assessment of the current landscape. To address the gaps in the availability of prenatal MMC repair, future research should focus on the relative paucity of teams that perform fetal surgery compared with those who do not. This future direction will be beneficial in understanding the landscape of MMC management and improving outcomes for affected families.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 19 December 2024.
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Yamashiro KJ, Galganski LA, Hirose S. Fetal myelomeningocele repair. Semin Pediatr Surg. 2019;28:150823. [DOI] [PubMed] [Google Scholar]
- 2.Grivell RM, Andersen C, Dodd JM. Prenatal versus postnatal repair procedures for spina bifida for improving infant and maternal outcomes. Cochrane Database Syst Rev. 2014;2014:CD008825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adzick NS, Thom EA, Spong CY, et al. ; MOMS Investigators. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364:993–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clayton DB, Thomas JC, Brock JW, III. Fetal repair of myelomeningocele: current status and urologic implications. J Pediatr Urol. 2020;16:3–9. [DOI] [PubMed] [Google Scholar]
- 5.Houtrow AJ, Thom EA, Fletcher JM, et al. Prenatal repair of myelomeningocele and school-age functional outcomes. Pediatrics. 2020;145:e20191544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Houtrow AJ, MacPherson C, Jackson-Coty J, et al. Prenatal repair and physical functioning among children with myelomeningocele: a secondary analysis of a randomized clinical trial. JAMA Pediatr. 2021;175:e205674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kabagambe SK, Jensen GW, Chen YJ, et al. Fetal surgery for myelomeningocele: a systematic review and meta-analysis of outcomes in fetoscopic versus open repair. Fetal Diagn Ther. 2018;43:161–174. [DOI] [PubMed] [Google Scholar]
- 8.Han JS, Rangwala SD, Ge BB, et al. Myelomeningocele repair at pediatric hospitals: association with routine discharge and shorter hospital stay. J Neurosurg Pediatr. 2023;32:376–383. [DOI] [PubMed] [Google Scholar]
- 9.Yamashiro KJ, Farmer DL. Fetal myelomeningocele repair: a narrative review of the history, current controversies and future directions. Transl Pediatr. 2021;10:1497–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakayama DK, Burd RS, Newman KD. Pediatric surgery workforce: supply and demand. J Pediatr Surg. 2009;44:1677–1682. [DOI] [PubMed] [Google Scholar]
- 11.Kshettry VR, Kelly ML, Rosenbaum BP, et al. Myelomeningocele: surgical trends and predictors of outcome in the United States, 1988–2010. J Neurosurg Pediatr. 2014;13:666–678. [DOI] [PubMed] [Google Scholar]