Summary
We report the case of a 60-year-old man diagnosed with unilateral, solitary, extramedullary plasmacytoma located in the right lacrimal sac fossa, with no systemic involvement. This rare plasma cell dyscrasia is usually found in the respiratory tract. Clinical and radiological features of the mass and histopathological results are described. The patient was successfully treated with complete surgical excision. There were no clinical or radiological indications of disease recurrence at 10 months’ follow-up.
Introduction
Extramedullary plasmacytoma (EMP) is a rare, malignant, plasma cell dyscrasia that occurs most commonly in the head and neck region, accounting for 1% of all head and neck malignancies.1 EMP originates from submucosal areas with an abundance of plasma cells, such as the respiratory tract, nasopharynx, and paranasal sinuses.2–4 EMP presents most commonly as a solitary lesion, usually in the fifth or sixth decade of life, with a male:female ratio of 4:1.1–5
Case Report
A 60-year man presented at Advanced Eye Centre, Post Graduate Institute of Medical Education and Research, Chandigarh, India, with a painless mass in the right lacrimal sac fossa of 11 months’ duration. The mass was insidious in onset and progressive. On examination, the mass was nontender, immobile, and firm on palpation. It measured 21 × 17 mm, with distinct superomedial margins. The mass extended into the bony lacrimal sac fossa (Figure 1A–B). The fluorescein dye disappearance test was positive in the right eye, and regurgitation on pressing the lacrimal sac was negative. The absence of epiphora, a mass that was firm to hard, and negative ROPLaS led to suspicion of lacrimal sac tumor. The rest of the ophthalmic examination was normal, including visual acuity and ocular motility. There were no masses or lumps elsewhere in the body on systemic examination and no lymphadenopathy.
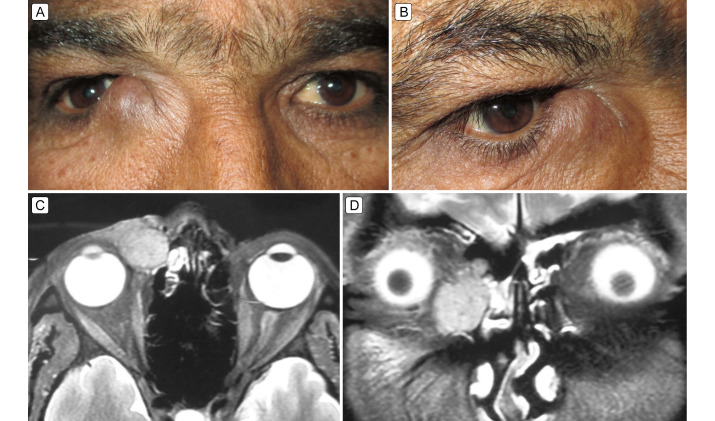
Figure 1.
A, The right lacrimal sac region shows an oval, grape-sized mass (25 × 21 mm) extending above the medial canthal tendon, pushing it superiorly; the right globe shows mild lateral displacement. B, Oblique view showing overlying skin with a bluish appearance, stretched, and free from mass. C, Contrast-enhanced magnetic resonance imaging (axial section) of the orbits showing a well-defined hyperintense mass in the lacrimal sac fossa, with mild lateral globe dystopia; there is regional ethmoid sinus hyperintensity. D, Coronal section showing a mass in the lacrimal sac region, with free nasolacrimal duct. The surrounding ethmoid sinus haze is indicated.
Contrast-enhanced magnetic resonance imaging (MRI) of the orbits revealed a heterogeneous, hyperintense (on both T1- and T2-weighted images), multilobulated mass (Figure 1C–D) measuring 25 × 20 mm in the right lacrimal sac region, with mild ethmoid sinus hyperintensity. No extension of the mass was documented in the scans.
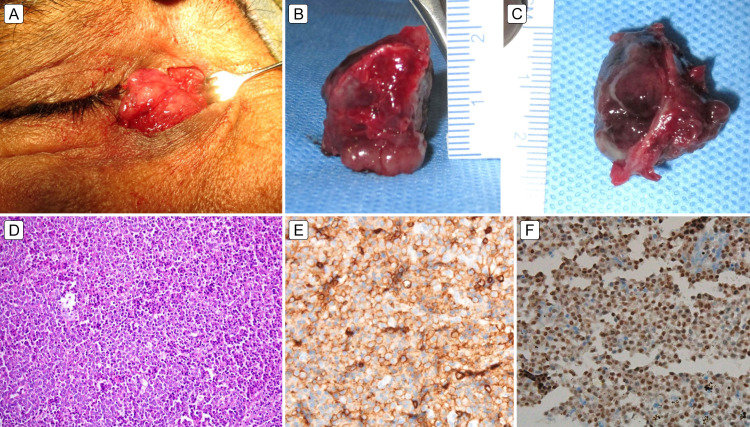
A clinical-radiological working diagnosis of a right lacrimal sac tumor was made. A right dacryocystectomy was performed under local anesthesia (Figure 2A–C), with punctum and canalicular cauterization. Histopathological examination showed sheets of plasma cells with eccentrically placed nuclei (Figure 2D). The plasma cells were atypical and showed moderate nuclear polymorphism, with prominent nucleoli. The immunohistochemistry showed membranous positivity for CD38 (Figure 2E), nuclear positivity for MUM1 (Figure 2F), and negativity for cytokeratin EBER-ISH. The features were suggestive of anaplastic plasmacytoma of the right lacrimal sac.
Figure 2.
A, Intraoperative image showing a bosselated surface with preserved, separated orbicularis oculi muscle fibers. The bony lacrimal sac fossa was intact, and no bony breach was noted clinically. B, The completely excised mass had a bosselated smooth bony surface (25 mm). C, The skin surface of the mass shows more irregularity (20 mm). D, Hematoxylin-eosin staining (×10) showing sheets of atypical plasma cells with eccentric nuclei with skeletal muscle infiltration. E-F, Immunohistology showing membrane positivity for CD 38 (E) And nuclear positivity for MUM1 (F).
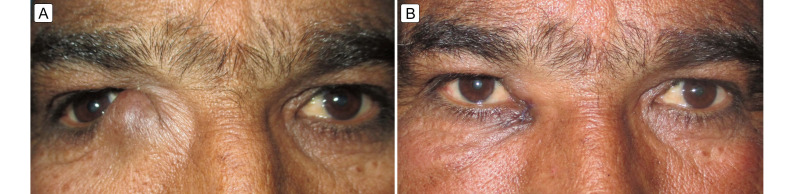
Positron emission tomography whole-body scan showed no other hypermetabolic foci in the right lacrimal sac region or elsewhere in the body. The subsequent hematology consultation and bone-marrow investigations ruled out multiple myeloma. At 10 months’ follow-up, there were no clinical or radiological indications of disease recurrence (Figure 3); however, the patient had clear fluid epiphora from the right eye, for which botulinum toxin injection into the right lacrimal gland was advised. We discussed the possibility of radiation therapy with the patient, in the event of any local recurrence.
Figure 3.
A, Preoperative image in primary gaze. B, Postoperative image shows normal-looking right lacrimal sac fossa and right globe position 2 weeks after excision.
Discussion
In a review of lymphoproliferative lesions involving the lacrimal system, Singh and Ali6 reported that the majority of lymphoma/leukemia lesions primarily involved the lacrimal sac (63%), with epiphora being the most common presenting complaint (96%), followed by swelling in the lacrimal sac region (75%). Most malignant primary tumors of the lacrimal system originate from the epithelium or the mesenchymal components of the lacrimal sac. Primary neoplasms arising from the lacrimal sac are of epithelial (75%) or nonepithelial (25%) origin. Other tumors include mesenchymal (12%), melanoma (5%), and malignant lymphoma (6%).1,2,6
EMP is an intermediate between monoclonal gammopathy of undetermined significance and multiple myeloma. It arises from the plasma cells of mucosal surfaces.7 Treatment includes surgical resection, radiotherapy, or a combined approach.1–6 Complete surgical resection is often successful in well-defined and localized masses that are amenable to resection. In our case, the tumor was localized to the lacrimal sac fossa and, based on preoperative imaging and intraoperative assessment, did not extend to the surrounding regions. Tumor growth did not extend above or displace the medial canthal tendon, perhaps due to a more prominent growth in anterior, subcutaneous direction, where it would encounter less resistance. The complete removal of the mass was achieved through blunt dissection.
EMP is a highly radiosensitive tumor, making radiation therapy a viable treatment option in solitary-defined lesions where complete surgical resection is not possible.7,8 Radiation achieves local tumor control rate of >80%-90% and decreases local relapse rate.1,2,7,8 A combined and more aggressive approach is desired in cases with more advanced diseases or recurrences. In the event of local recurrence in our patient, we may consider localized radiation therapy.
EMP progresses to multiple myeloma in 15% of cases over a median time of 2–3 years.8 Patients may have poor prognosis due to incomplete resection, local recurrence, lymph node metastasis, and bone lesions, which suggest the possibility of multiple myeloma. Histopathology features of high-grade anaplastic plasmacytomas with increased vascularity are poor prognostic markers.8
EMP in the ophthalmic region has been infrequently reported, and rarely in the lacrimal sac.5,7,9 EMPs have been reported in orbital soft tissue, the ciliary body, the conjunctiva, the canaliculus, and in the epibulbar region.8–11 Orbital EMP is uncommon, and the reported cases originated from the lacrimal gland.8,9 Our literature search revealed a case of a solitary plasmacytoma arising from the lacrimal sac region that presented as a painless mass with epiphora. The diagnosis of EMP was confirmed after a nasal endoscopic biopsy, and the patient was successfully treated with radiotherapy.7 You et al11 reported a primary plasmacytoma masquerading as infectious lacrimal canaliculitis; its clinical presentation related to its mass effect.
Complete surgical excision of a clinically and radiologically well-defined and localized lacrimal sac tumor may provide satisfactory local disease control, which can be combined with localized radiotherapy for any residual tumor. In our patient, the adjuvant radiation therapy would have further negated the risk of local recurrence; however, it would have carried an added risk of radiation induced dry-eye and radiation retinopathy. Hence, radiation therapy or a combined approach can be reserved for large-sized tumors, more advanced disease, or local recurrences.
Histopathology and immunohistochemistry facilitate diagnosis: monoclonal plasma cells are positive for CD38, which is a receptor on plasma cells, and MUM1 positivity is a marker of lymphoid differentiation and upregulated in neoplastic transformation.8 Systemic screening for the active foci and long-term patient follow-up is desired to look for any local or systemic metastasis. We believe complete surgical excision of a clinically and radiologically well-defined tumor may provide local disease control. Immunohistochemistry provides the final diagnosis and systemic screening for the other active foci with follow-up is desired.
References
- 1.Sun WJ, Zhang JJ, An N, Shen M, Huang ZX, Li X. Clinical analysis of 40 multiple myeloma patients with extramedullary plasmacytoma of the head. J Int Med Res. 2016;44:1462–73. doi: 10.1177/0300060516664820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gao J, Tseng CC, Barinsky GL, et al. Analysis of the treatment and survival of sinonasal extramedullary plasmacytoma. Am J Rhinol Allergy. 2022;36:591–8. doi: 10.1177/19458924221092529. [DOI] [PubMed] [Google Scholar]
- 3.Sia DI, Cannon PS, Selva D. Extramedullary plasmacytoma arising from the lacrimal gland. Clin Exp Ophthalmol. 2010;38:895–8. doi: 10.1111/j.1442-9071.2010.02372.x. [DOI] [PubMed] [Google Scholar]
- 4.Barmas-Alamdari D, Sodhi GS, Shenouda TA. Bilateral proptosis in a case of recurring multiple myeloma: uncommon orbital presentation of plasmacytoma. Int Med Case Rep J. 2020;13:297–301. doi: 10.2147/IMCRJ.S260472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee CM, Asilnejad B, Cohen LM, et al. Solitary extramedullary plasmacytoma of the lacrimal sac with associated crystal-storing histiocytosis. Ophthalmic Plast Reconstr Surg. 2022;38:102–7. doi: 10.1097/IOP.0000000000002028. [DOI] [PubMed] [Google Scholar]
- 6.Singh S, Ali MJ. Lymphoproliferative tumors involving the lacrimal drainage system: a major review. Orbit. 2020;39:276–4. doi: 10.1080/01676830.2019.1634104. [DOI] [PubMed] [Google Scholar]
- 7.Lim J, Yoo SW, Choi KH, Lee JH. Extramedullary plasmacytoma of the lacrimal sac and duct invading the inferior meatus: an extremely rare occurrence. J Rhinol. 2012;19:80–2. [Google Scholar]
- 8.Iqbal QUA, Majid HJ. StatPearls. Treasure Island: StatPearls Publishing; 2023. Plasmacytoma. [PubMed] [Google Scholar]
- 9.Sharma S, Kaur R, Bal A, Mohindra S, Aggarwal R. Primary orbital plasmacytoman unusual presentation in an adolescent. Indian J Pathol Microbiol. 2018;61:158–9. doi: 10.4103/IJPM.IJPM_378_17. [DOI] [PubMed] [Google Scholar]
- 10.Zloto O, Vahdani K, Stack R, Verity DH, Rose GE. Periocular presentation of solitary plasmacytomas and multiple myeloma. Ophthalmic Plast Reconstr Surg. 2022;38:180–4. doi: 10.1097/IOP.0000000000002023. [DOI] [PubMed] [Google Scholar]
- 11.You JY, Glassman ML, McCormick SA, Milman T. Plasmacytoma associated with canaliculitis. Ophthalmic Plast Reconstr Surg. 2012;28:e60–2. doi: 10.1097/IOP.0b013e3182238b75. [DOI] [PubMed] [Google Scholar]