Summary
A 4-year-old girl presented with an enlarging, congenital, intrascleral cyst of the left eye. Intraoperative anterior segment optical coherence tomography was used to visualize and to assess the extent of the cyst, facilitating safe excision. The cyst was completely removed, and the defect was covered with an amniotic membrane graft, with a good outcome.
Introduction
Congenital intrascleral epithelial cysts are rare ocular lesions that are usually found at the limbus, with extension to the cornea.1 The cyst is thought to result from abnormal sequestration of conjunctival epithelium into the sclera during embryological development.2,3 When stable, these cysts may be observed4; however, excision is warranted for progressively enlarging and vision-threatening lesions.1–3 Because these cysts are typically diagnosed in young children, preoperative evaluation and imaging may be limited by patient cooperation. We present the case of a young girl with an enlarging, congenital, intrascleral cyst excised under the guidance of anterior segment optical coherence tomography (AS-OCT).
Case Report
A 4-year-old girl presented at Emory Eye Center with a cystic lesion in the nasal aspect of the left eye. The cyst was noted by her mother shortly after birth. The mother reported transient fluctuations in the size of the cyst, overall enlargement over the years, but no associated symptoms. There was no prior eye trauma or surgery. Birth, maternal, developmental, and family histories were noncontributory. On ocular examination, visual acuity was 20/20 in each eye. Cycloplegic refraction was +1.00 +0.25 ×80 in the right eye and +1.00 +1.00 ×70 in the left eye. Intraocular pressure was 14 mm Hg in the right eye and 11 mm Hg in the left eye. Slit-lamp examination showed an intrascleral cyst (∼10 mm × 4.5 mm) extending to the nasal limbus of the left eye. The rest of the ocular examination was normal in both eyes.
Ultrasound biomicroscopy of the left eye confirmed the presence of a nasal intrascleral cyst, although the extent of corneal and anterior chamber involvement was difficult to assess because of limited patient cooperation. A decision to excise was made because of concern for enlargement of the cyst and resulting vision loss in the affected eye.
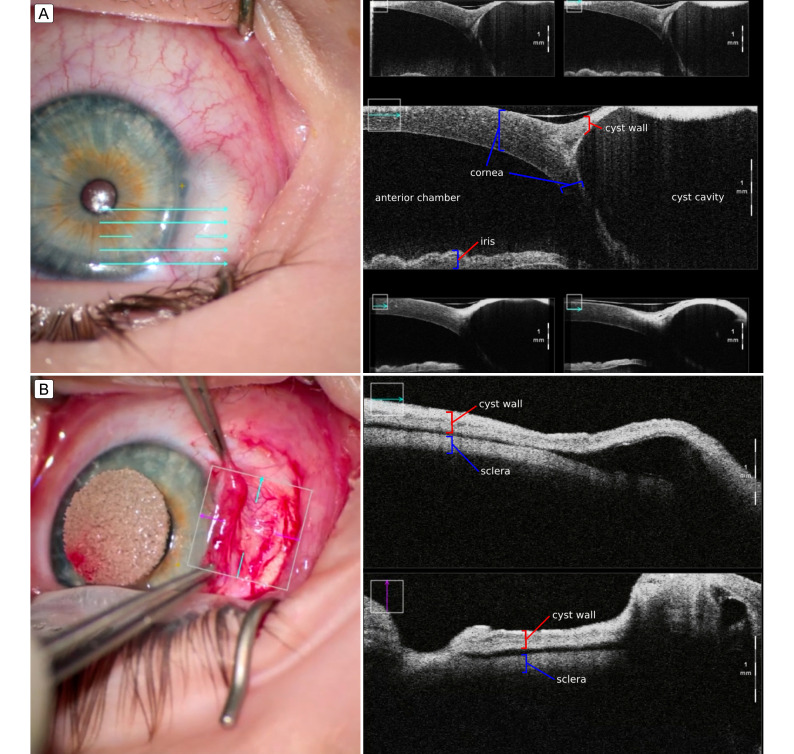
AS-OCT was performed after anesthetic induction to determine whether a connection existed between the cyst and the anterior chamber (Figure 1A). After confirming the absence of communication, the conjunctiva was opened to expose the lesion following the nasal border of the cyst. Episcleral vessels at the edge of the cyst were cauterized. Cyst rupture occurred as the lesion was dissected from the sclera, with no noted shallowing of the anterior chamber. AS-OCT was useful in helping to delineate the cyst wall from the scleral bed (Figure 1B). Cyst wall excision was completed using a crescent knife and Wescott scissors. Once hemostasis was achieved with light cautery, an amniotic membrane graft was sutured over the defect with interrupted 8-0 polyglactin 910 sutures (Figure 2A). Histopathology confirmed an intrascleral cyst lined by nonkeratinized, stratified squamous epithelium.
Figure 1.
Anterior segment optical coherence tomography (AS-OCT) was used to guide intraoperative decisions during intrascleral cyst excision. Preoperative AS-OCT confirmed the absence of a connection between the anterior chamber and the intrascleral cyst (A). Intraoperative AS-OCT helped to delineate the cyst wall from the scleral bed (B).
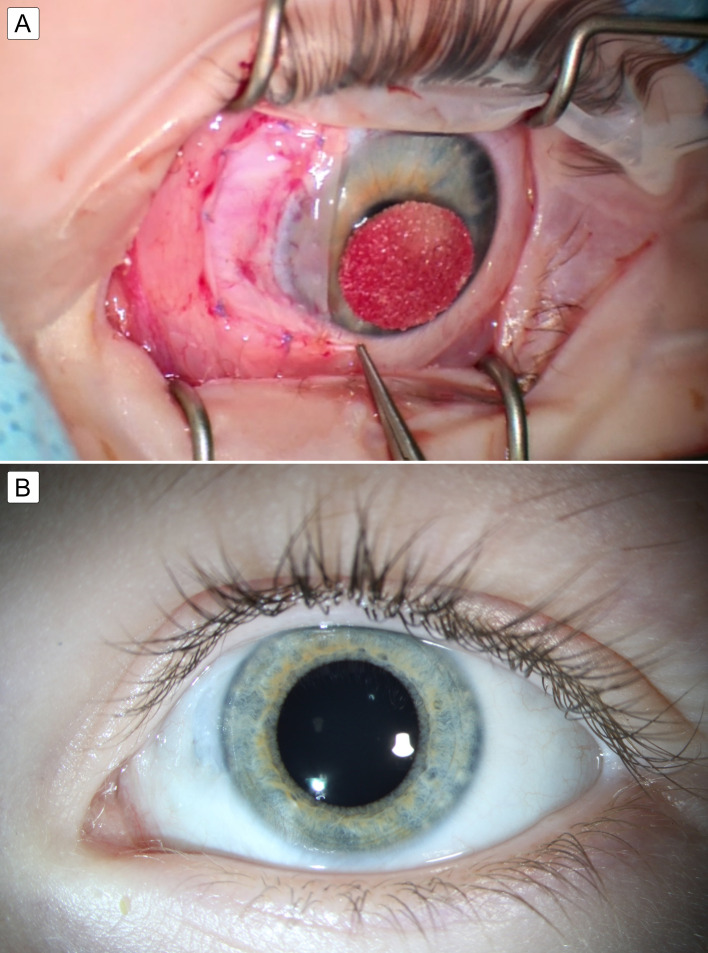
Figure 2.
A, Amniotic graft membrane sutured over the defect. B, Slit lamp photograph after 12 months showed healing and scarring of the ocular surface at the former site of the intrascleral cyst.
One year after surgery, the patient’s best-corrected visual acuity was 20/20 in both eyes (LEA chart, isolated optotypes), with a refraction of plano +1.00 ×100 in the right eye and +0.25 +1.75 ×90 in the left eye. Slit lamp examination of the left eye showed a clear cornea and a well-healed ocular surface. There was thinning of the sclera adjacent to the limbus (Figure 2B). No recurrence or complications developed within 1 year of excision.
Discussion
Intraoperative OCT enables dynamic imaging of ophthalmic surgeries, capturing the surgical process and real-time interactions between instruments and tissues. It is used to guide decision making during important steps of surgery, with the goal of optimizing surgical outcomes. Both portable and microscope-integrated OCTs have been increasingly employed in anterior segment surgeries, including corneal procedures, refractive surgeries, phacoemulsification, glaucoma surgeries. Additionally, intraoperative OCT has proved to be a valuable tool in pediatric examinations under anesthesia.5
Our case demonstrates the utility of microscope-integrated AS-OCT in surgical decision making during intrascleral cyst excision. Outpatient examination and diagnostic imaging may be challenging in young children, and imaging performed after sedation may add reliable and valuable information that can guide surgical technique. AS-OCT provides information regarding the size, depth, and extent of an intrascleral cyst. Knowledge of the presence of a communication between the cyst and the anterior chamber can alert the surgeon to potential intraoperative anterior chamber collapse. In cases where such communication is identified, a preemptive measure would involve the creation of an anterior chamber paracentesis. This procedure facilitates the injection of balanced salt solution or viscoelastic, effectively preventing the occurrence of anterior chamber collapse. Furthermore, intraoperative AS-OCT may facilitate visualization of a dissection plane to allow complete cyst wall excision, thereby decreasing the risk for recurrence. Awareness of the extent of corneal and scleral involvement also allows planning for an appropriate graft. We elected to place an amniotic membrane graft over the defect. Other surgeons have also achieved success with banked fascia lata1 and tectonic scleral grafts.2 The surgery resulted in a favorable outcome, with complete cyst excision, minimal change in refraction, and a stable, best-corrected visual acuity of 20/20.
This report underscores the utility of intraoperative AS-OCT in intrascleral cyst excision, especially for young children with limited preoperative evaluation. By providing real-time visualization during surgery, this imaging modality can aid in the precise removal of the cyst, thereby minimizing the risk of complications.
References
- 1.Akbaba M, Hacıyakupoğlu G, Uğuz A, Karslıoğlu S, Karcıoğlu Z. Congenital intrascleral cyst. Clin Ophthalmol. 2011;5:583–5. doi: 10.2147/OPTH.S19789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmood MA, Awad A. Congenital sclerocorneal epithelial cyst. Am J Ophthalmol. 1998;126:740–1. doi: 10.1016/s0002-9394(98)00128-7. [DOI] [PubMed] [Google Scholar]
- 3.Liakos GM. Intracorneal and sclerocorneal cysts. Br J Ophthalmol. 1978;62:155–8. doi: 10.1136/bjo.62.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soni T, Das S. Natural course of congenital corneoscleral cyst: 10-year follow-up. Indian J Ophthalmol. 2020;68:2217–8. doi: 10.4103/ijo.IJO_206_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Titiyal JS, Kaur M, Nair S, Sharma N. Intraoperative optical coherence tomography in anterior segment surgery. Surv Ophthalmol. 2021;66:308–26. doi: 10.1016/j.survophthal.2020.07.001. [DOI] [PubMed] [Google Scholar]