Abstract
Objective
This study aimed to simulate patient transportation to a mechanical thrombectomy (MT)-capable hospital within 60 minutes, taking into account patient volume (demand side of healthcare) and hospital capacity to accept patients (supply side of healthcare).
Methods
Simulations were conducted in Hyogo Prefecture, Japan. The estimates of the annual number of patients with stroke eligible for MT in 2020 were based on the incidence of stroke by age group and the percentage of patients with stroke indicated for MT in existing publications. Patients were then randomly placed on a 1 km2 mesh map. The patients were randomly generated 100 times using R software (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria). Hospitals were selected based on 2 criteria: (1) actual provision patterns (39 hospitals) and (2) consolidated patterns (12 hospitals). Simulations were performed using ArcGIS Pro (version 10.8; Esri, Redlands, CA, USA) and Network Analyst extension (Esri) in 3 cases: (1) number of patients estimated from the population in 2020 transported to hospitals that provided MT, (2) number of patients estimated based on the 2020 population transported to selected hospitals in the case of consolidation, and (3) number of patients estimated based on 2040’s projected population and transportation to the selected hospitals.
Results
In Case 1, the estimated annual number of patients undergoing MT in 2020 was 976. The average number of patients undergoing MT and transported was 961, indicating that 98% (961/976) of the total generated patients could be transported within 60 min. In Case 2, the average number of patients undergoing MT and transported was 940, indicating that 96.3% (940/976) of the total patients could be transported within 60 min. In Case 3, the average number of patients undergoing MT and transported was 1184, showing that 95.1% (1184/1244) of the total generated patients could be transported within 60 min. A few patients in rural areas and remote islands required longer transport times.
Conclusion
The simulations showed that patient estimates from the incidence of cerebral infarction by age group and the percentage of patients with stroke indicated for MT were similar to the actual values. The simulation was closed to reality when both the supply and demand sides of healthcare were considered. Thus, this simulation study informs future healthcare policy by demonstrating the geographic distribution of human and capital resources and potential cost reduction through consolidation, taking into account demographic changes.
Keywords: mechanical thrombectomy, healthcare supply and demand, patient transport simulation, hospital consolidation, GIS
Introduction
Stroke is the fourth leading cause of death in Japan and the leading cause of death in older adults.1) The incidence of stroke by age group is higher in older adults2) than in any other demographics, and the number of patients is expected to increase as the older adult population grows. Stroke is the second most common cause of public long-term care needs and economic strain.3)
In December 2016, the Japanese Circulation Society and the Japan Stroke Society jointly announced the “Five-Year Plan to Conquer Stroke and Cardiovascular Disease”4) to improve care through human resource development, healthcare system enhancement, nationwide registration, public awareness campaigns, and research. In 2021, the “Second Five-Year Plan to Conquer Stroke and Cardiovascular Disease”5) was released to continue the project. The Second Five-Year Plan succeeds the First Five-Year Plan. It was formulated with 2 additional goals: (1) to reduce the age-adjusted mortality rate from stroke and cardiovascular diseases by 5% compared with the 2020 rate and (2) to further increase healthy life expectancy during the 5 years of the plan.
Thrombolytic therapy with intravenous tissue plasminogen activator and mechanical thrombectomy (MT) with stent retrievers and aspiration catheters have been utilized to improve healthy life expectancy in acute stroke care. A meta-analysis of 5 randomized controlled trials on MT was published in 2016.6) Here, they reported that the addition of MT to medical therapy, including intravenous tissue plasminogen activator, for acute stroke due to occlusion of a large anterior circulation artery significantly improved disability at 90 days, compared with medical therapy alone.
In Japan, the Japan Stroke Society, the Japan Neurosurgical Society, and the Japanese Society for Neuroendovascular Therapy (JSNET) have jointly published guidelines for properly using cerebral thrombus retrieval devices.7) These guidelines state that MT must be performed by a neuroendovascular specialist or a physician with experience equivalent to that of a specialist. In Japan, certification by JSNET is required to become a neuroendovascular specialist.7) In addition to the physician, the procedure requires the participation of several other medical staff. Thus, hospitals must secure adequate human resources with specialties, as well as capital resources such as medical equipment and dedicated rooms for endovascular treatments. With the enormous cost of installing and maintaining treatment facilities and the limited number of human resources, it is important to plan the efficient allocation of treatment centers and consider both demand- and supply-side factors of endovascular treatments.
It would be useful to conduct simulations that consider the geographic distribution of patients and the capacity of the facilities to receive them. These results can be incorporated into the design of resource allocation in health policy settings. Several studies have simulated the transport of patients with stroke in certain areas to calculate the transport time to the nearest facility from the patients’ location.8,9) These studies provide information on the proportion of patients who can access appropriate interventions within a certain time after stroke onset.
However, these studies only considered the demand-side perspective of healthcare and did not consider the supply-side circumstances. These studies assumed that patients were transported to the nearest hospital without considering each hospital’s capacity to provide specialty care. In a real setting, the selection of the treatment site takes into account various factors, such as estimated transportation time, the number of healthcare professionals, and the number of catheterization rooms. If the simulation is performed without taking into account the capacity of the receiving facility, many patients may be transported to the nearest facility, even if the nearest facility is inadequately equipped to receive patients because of a lack of medical specialists and co-medical staff.
In this study, we constructed a simulation model of the transport of patients with stroke to the hospital, considering both the demand- and supply-side factors that previous studies have often overlooked. The estimated number of patients indicated for MT was calculated using census data on the population, the incidence of cerebral infarction by age group,2) and the percentage of patients indicated for cerebral thrombectomy in previously reported data10,11) (which was not used in previous studies). For the supply side, the simulated patients with stroke on the Geographical Information System (GIS) were transported to a hospital, taking into account both transportation time and facility capacity. This study aimed to simulate the transport of patients with stroke in actual settings and provide more practical and valuable information for planning resource allocation.
Materials and Methods
Patients and outcomes
This study simulated a hypothetical cohort using the projected 2020 population of Hyogo Prefecture (Japan) obtained from National Institute of Population and Social Security Research (based on the 2015 census).12) Hyogo Prefecture is located in western Japan, to the west of Osaka City (Osaka Prefecture), which has the third largest population in Japan. The northern part of the prefecture faces the Sea of Japan and is mountainous, with most of the area being a depopulated region. The southern part of the prefecture faces the Seto Inland Sea, and the majority of the population is concentrated in the southeastern part of the prefecture. Furthermore, the study aimed to (1) simulate transport to a facility with a proven track record of MT treatment, (2) simulate transport to a consolidated facility (a hypothetical central facility intended for the consolidation of thrombectomy procedures, aimed at the effective utilization of medical resources and ensuring sufficient physician experience. This can be considered a facility that, at present, performs the highest number of thrombectomy procedures within the secondary medical area), and (3) simulate a cohort using the projected population for 2040 in a facility-consolidated pattern. For this simulation, the maximum transport time was set at 60 min. The simulation took into account the patient location (demand) and facility capacity (supply) to determine the number of patients transported to each facility. Data on annual Hyogo Prefecture MT procedures were acquired through collaboration with the Japan Stroke Society. Since this was a simulation study using published statistical data and data from previously published papers, approval by the Ethics Board is not required.
Patient generation
The incidence rates by age group in epidemiological surveys were used to estimate the number of patients with cerebral infarctions. Nationwide data on age-specific incidence rates were unavailable in Japan. Therefore, the number of patients was estimated by extrapolating age group-specific incidence rates over 10 years in Iwate Prefecture, Japan.2)
As this estimate includes patients ineligible for MT, the number of eligible patients was calculated by multiplying the estimate by the percentage of patients eligible for MT based on existing reports.10) Patients were then randomly placed on a 1 km2 mesh map provided by the Statistics Bureau of Japan for each patient based on population density.8) The patients were randomly generated 100 times using R software (version 4.1.2), a language and environment for statistical computing. (R Foundation for Statistical Computing, Vienna, Austria [https://www.R-project.org/])
Hospital selection
Two sets of facilities with a proven track record of MT procedures were selected as follows: (1) all hospitals where MT was provided in 2020 (total of 39 hospitals) and (2) the hospital with the largest number of patients undergoing MT in each secondary medical region (a total of 12 hospitals). However, 2 hospitals were selected from the Kobe and Hanshin-Minami medical regions because of their large populations.
Capacity setting
Each hospital’s maximum MT capacity was based on its actual 2020 patient numbers. Each simulation assumed a percentage increase in patients with MT per hospital to accommodate all generated patients.
Simulation
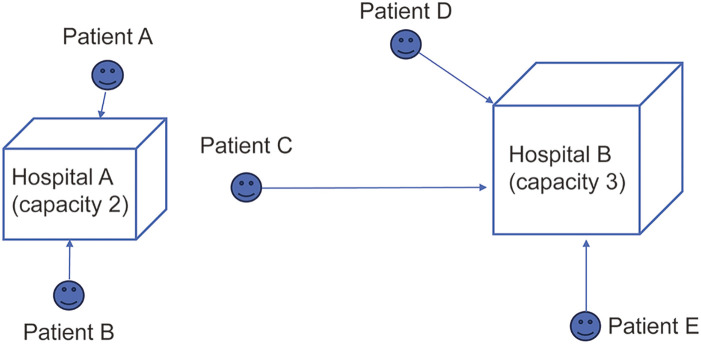
Simulations were performed using ArcGIS Pro 3.2 (Esri, Redlands, CA, USA) and Network Analyst extension (Esri). Road Network 2022 (Esri) was used as the road information required for the simulation. The built-in “Maximize Coverage Capacity” mode was used to simulate the transportation of each patient, taking into account both supply- and demand-side factors. The “Maximize Coverage Capacity” mode is an analysis method based on the maximum coverage location problem (MCLP) with capacity limits.13) MCLP is currently the most frequently cited location modeling method. The detailed mathematical modeling method is explained elsewhere.14) The “Maximum Coverage Capacity” mode prioritizes maximizing patient coverage, sending patients to the nearest hospital with available capacity up to its limit. Figure 1 illustrates the transfer of 5 patients with stroke (A–E) to 2 hospitals (A and B) with capacities of 2 and 3 patients, respectively. Patients A and B were sent to the nearest hospital (A), and patients D and E were sent to the nearest hospital (B). However, patient C was sent to Hospital B, which has available capacity, rather than the nearest Hospital A, which was already full.
Fig. 1. A case of 5 patients’ transportation to 2 hospitals under the Maximize Coverage Capacity mode.
The transport simulation was repeated 100 times using the maximum coverage model. Subsequently, the mean value of the 100 transport simulations was used as the result.
Results
Validity of estimated number of patients
The estimated annual number of patients treated with MT in 2020 was 976, based on the projected population in 2020 according to the 2015 census, the age-group-specific incidence of cerebral infarction in an epidemiological study,2) and the previously reported indication rates10) for MT, as described in the Materials and Methods section. The actual number of MT procedures performed in Hyogo Prefecture in 2020 and 2021 were 843 and 940, respectively. Thus, the patient generation process based on the extrapolated data represented the actual number of patients undergoing MT.
All facilities with a proven track record of MT for the 2020 population
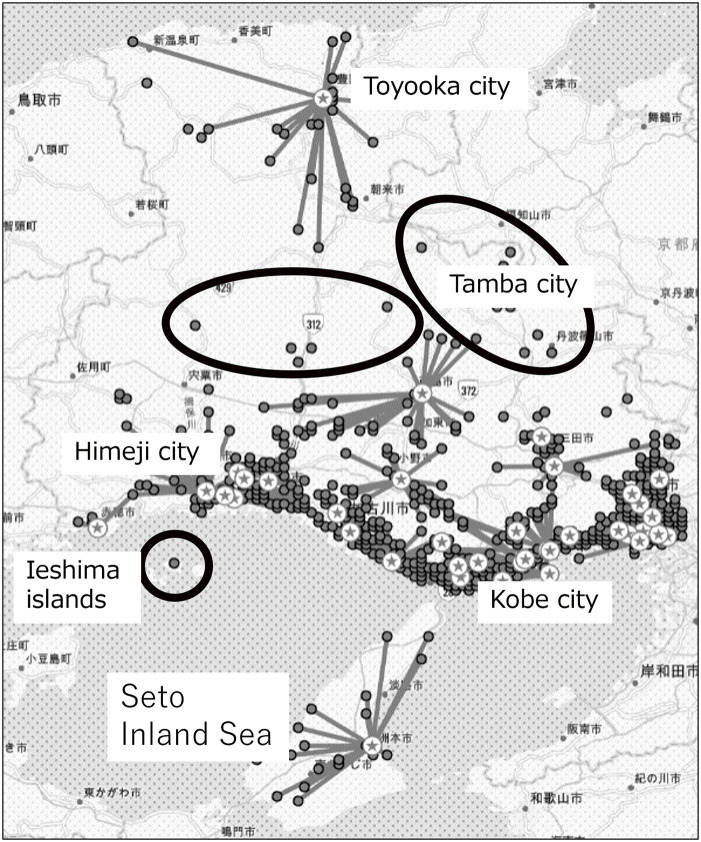
In this simulation, patients undergoing MT were transported to one of the facilities where the treatment was performed. In all, 39 facilities had proficiency in MT in 2020. After 100 simulations, the total number of transported patients was 961, indicating that 98% of the patients (n = 976) could be transported within 60 min. Figure 2 shows the details of the transport simulations. Furthermore, patients who could not be transported within 60 min (n = 15) lived in the black circles in the Middle Eastern parts of Hyogo Prefecture (near the border between Hyogo and Kyoto Prefectures), including Tamba City. The black circles, which were located in the central and western parts of Hyogo Prefecture, include Fukuzaki City, Ichikawa City, and Shisou City. The black circle in the Seto Inland Sea includes the Ieshima Islands, belonging to Himeji City. The Seto Inland Sea in Japan is surrounded by the main islands of Honshu, Shikoku, and Kyushu. From an economic perspective, the coastal areas host major cities like Hiroshima and Kobe.
Fig. 2. Results of transport simulation to facilities with treatment experience in 2020 only. The gray circle indicates the patient’s point of origin, and the star indicates the treatment facility. The lines extending from the gray circle to the star indicate the results for each type of transport. Gray circles that do not extend to the star indicate patients who could not be transported within 60 min as some patients could not be transported within 60 min in the central part of the prefecture.
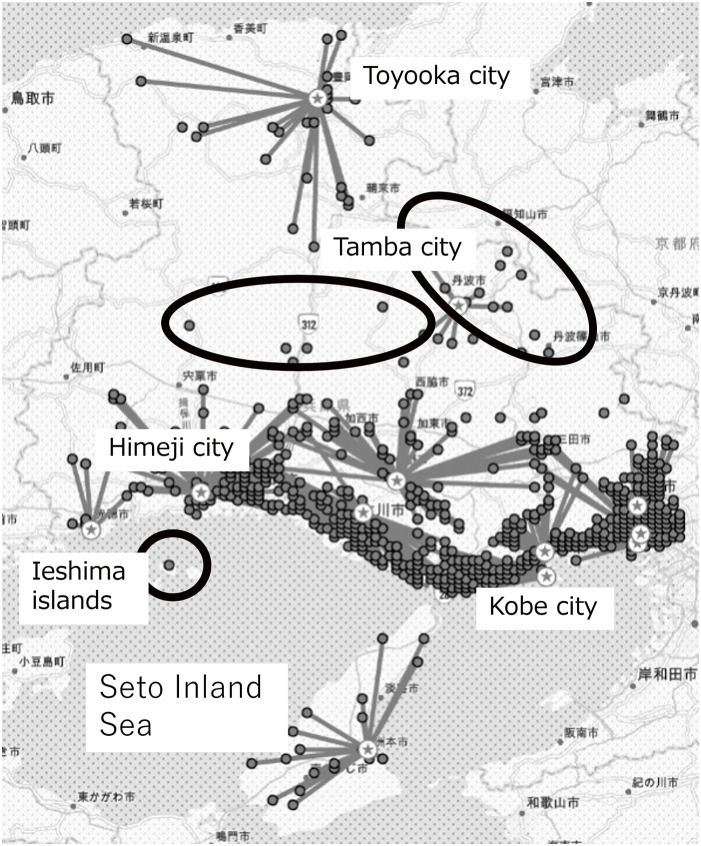
Facility-consolidated pattern for the 2020 population
In this simulation, the transport destination hospitals were limited to the more experienced hospitals. In each secondary medical care area, only facilities with the most patients undergoing MT were selected to accept patients. The 2 most experienced facilities were selected from 2 heavily populated areas: the Kobe Medical Care Area and the Hanshin-Minami Medical Care Area. Patients receiving MT were transported to 12 hospitals in 10 secondary medical areas. Furthermore, as the current hospitals could not accommodate all the patients, their capacity was increased by 100% to handle 1032 patients. The total number of patients transported was 940, indicating that 96.3% of the patients (n = 976) could be transported within 60 min. Figure 3 shows the details of the transport simulations. In this simulation, patients who could not be transported within 60 min (n = 36) lived in the thick black circular areas. In this simulation, as in simulation 1, the black circle denotes areas located in the middle right of Hyogo Prefecture (near the border of Hyogo and Kyoto Prefecture), which includes Tamba City. The thick black line circle denotes areas in the central and western parts of Hyogo Prefecture, including Fukuzaki City, Ichikawa City, and Shisou City. The thick black circle in the Seto Inland Sea includes the Ieshima Islands, which belong to Himeji City.
Fig. 3. Results of transport simulation in the case of consolidated facilities. As in simulation 1, gray circles indicate patients, and stars indicate treatment facilities (transport destination). Patients who cannot be transported within 60 min are dispersed around the central part of the prefecture.
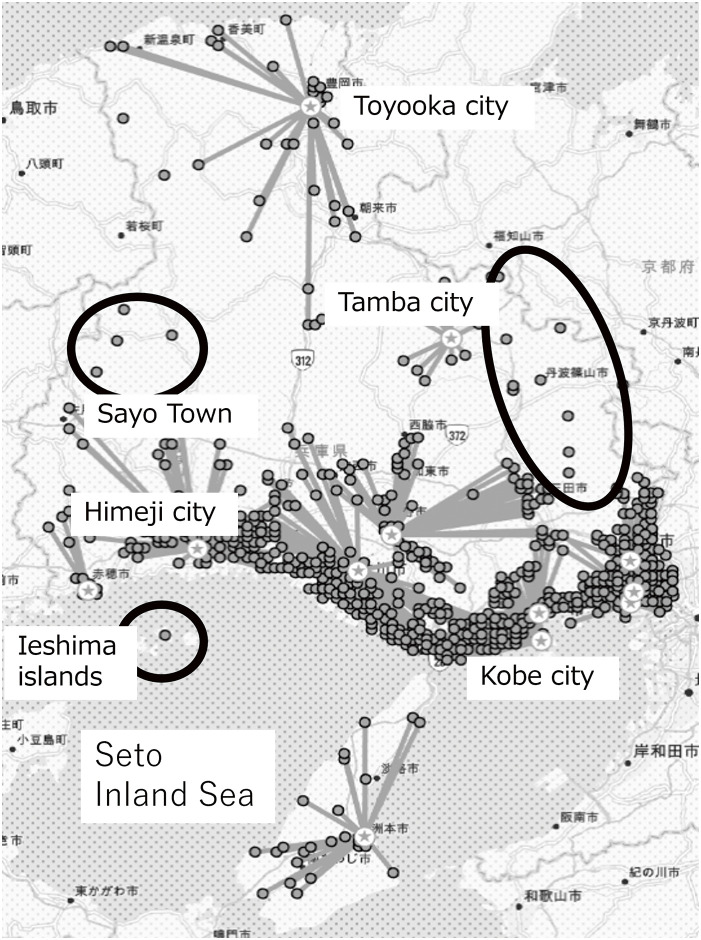
Facility-consolidated pattern for the 2040 forecasted population
This simulation was based on the forecasted population of each municipality in 2040 rather than the 2020 population, as was used in the 2 simulations above. Transport destination hospitals were selected in the same manner as in simulation 2. The number of patients generated by the 2040 population projection was 1244, a 27.5% increase from those generated by the 2020 population. The capacity was set to 1290 cases, 150% of the actual number, to accommodate all generated patients. The total number of patients transported was 1184, indicating that 95.1% of the total number of patients (n = 1244) could be transported within 60 min. Figure 4 shows the details of the transport simulations. Here, patients who could not be transported within 60 min (n = 60) lived in thick black circles. The results of this simulation were similar to those of simulations 1 and 2. The patients who could not be transported within 60 min were in Tamba City, Sayo City, and Ieshima Island, as they are located within the thick black line circles.
Fig. 4. Simulation results of consolidating facilities and transporting estimated patients based on the projected population of 2040. Similar to simulation 1, gray circles indicate patients, and stars indicate transport facilities. Patients who could not be transported within 60 min were those residing in the Mid-Eastern and Mid-Western parts of the prefecture.
In the first simulation with all hospitals, specialists handled an average of 8.5 cases per person (median 7). In the second simulation, consolidating facilities increased the workload per specialist at designated centers to an average of 16.8 cases (median 16.7).
Discussion
This study simulated the transport of patients undergoing MT in Hyogo Prefecture. This study showed that in Hyogo Prefecture, most patients could receive MT treatment even with the current number of hospitals and specialists. In the simulation with a limited number of facilities, the number of patients per hospital would need to be doubled; however, it was found that most patients could be transported within 60 min, even in this scenario. Thus, consolidating MT-providing hospitals with an increased capacity for MT treatment in each hospital would result in the same capacity for patient acceptance. Furthermore, in simulation (3), which considers future demographic changes, 95% of the patients can be transported with the same facility-consolidated pattern as in simulation (2). Thus, even if the number of MT patients increases in the elderly population by 2024, almost all patients can be accepted by consolidated facilities with an enlarged capacity to provide MT.
In all the simulations, few patients in remote locations, such as the Tamba City area, the areas surrounding Fukuzaki City, Sayo Town, and the Ieshima Islands, could not be transported to any hospital within 60 min. It is preferable to consider transportation by doctor helicopters instead of ambulance cars in these areas. Hyogo Prefecture designates priority areas for transport requests using helicopters, and the above areas are included in the priority area.15) Another option is to construct new facilities near these areas. However, taking into account the low overall needs in these areas, the construction of new stroke care centers might not be justified if the costs of human and capital resources are high. Therefore, it is necessary to study the costs and effectiveness of consolidating facilities in the future.
Simulation studies of patient transport have been conducted in the previous literature, but these studies considered only the demand side of healthcare. This study considers both the demand and supply sides by explicitly setting the capacity of the receiving facility. This study provides detailed information on the capacities that need to be reinforced if the number of facilities is consolidated in both present and future populations. It is important to construct quantitative evidence to design consolidated present facilities because it is more difficult for policymakers to consolidate than disperse and increase the number of facilities.
In this simulation, the upper limit of the transport time from the point of patient occurrence to the hospital was set to 60 min. According to emergency statistics published in 2021,16) the average time from the time of a call to arrival at the scene of an emergency in Hyogo Prefecture was 8.6 min, and the average transport time was 37.9 min. As 92.9% of the cases were transported within 60 min, it was appropriate to set the transport time to 60 min in this simulation. It is recommended that MT be performed within 6 h of onset (not within 6 h until reperfusion) in Japanese Guidelines for Mechanical Thrombectomy if clinical symptoms and imaging results meet the requirements.7) A hospital in Akashi City, Hyogo Prefecture used a similar simulation and reported a mean onset-to-hospitalization time of 69 min, a mean door-to-puncture time of 67 min, and a mean onset-to-reperfusion time of 3 h and 20 min.17) Akashi City is located in southern Hyogo Prefecture, to the west of Kobe City, the capital of Hyogo Prefecture. The population is approximately 300000. Another hospital in Yokohama City, Kanagawa Prefecture, reported a mean onset to reperfusion time of 5 h and 4 min,18) with a median time of 3 h and 4 min. Yokohama City is the capital of Kanagawa Prefecture and is located about 30 km south of downtown Tokyo. With a population of approximately 3.75 million, it is the second-largest city in Japan. The authors also reported a mean door-to-puncture time of 1 h and 26 min. In Nara prefecture, a hospital reported a mean door-to-puncture time of 2 h and 2 min and a mean puncture-to-reperfusion time of 35 min.19) Nara prefecture is located in the center of the Kinki region in the western part of the Japanese archipelago and lies east of Osaka, Japan’s third largest city. The northern part of the prefecture is an urban area, while the southern part is a sparsely populated area.
Thus, transport times and door-to-puncture times vary depending on the region and facility; however, these domestic reports show that the recommendation of initiating MT within 6 h of onset by the Japanese guidelines is being achieved.
Even in reports using nationwide emergency transport data, the transport time was 32 min20); therefore, setting a longer transport time could result in a simulation that does not reflect the actual situation. Based on the actual transport times, we believe that it is appropriate to set the transport time to 60 min and conduct the analysis.
Quality improvement collaboratives (QIC) of the workflow in stroke care can improve the quality of care by shortening the time to reperfusion,21,22) assuming the time from onset to puncture remains unchanged. If the door-to-puncture time can be shortened, then more time can be allocated for transportation. Even in the facility-consolidated cases, the number of patients per physician was lower than the recommended number of patients in other countries. Physicians at U.S. thrombectomy-capable stroke centers and comprehensive stroke centers were required to perform 15 cases of MT in the past 12 months or 30 cases in the past 24 months.23) In this study, only 3 of 39 facilities (7.7%) met the U.S. criteria in 2020 (actual value). Even in the facility-consolidated case, 5 of 12 (41.7%) facilities did not meet the standards (simulated value). The facility-consolidation scenario in this study may be insufficient if the quality of the MT is volume-dependent. Recently, research has been progressing to expand the indications to perform MT for large vessel occlusion (LVO) with extensive ischemic lesions,24) medium vessel occlusion (MeVO),25) and basilar artery thrombotic occlusion.26) If MT is actively performed for these lesions, the number of patients is expected to increase significantly. In our simulations, the number of patients was estimated by multiplying the population by age group with the incidence of stroke by age group and the rate of MT implementation based on published papers on all strokes. If the indications for MT are expanded, it will be possible to estimate the number of patients by changing the implementation rate. If updated papers on the rate of implementation are published in the future, it will be possible to estimate the number of patients and perform simulations using that data.
This study had some limitations. First, patient generation was estimated by extrapolating epidemiological data on the incidence of cerebral infarction in prefectures other than Hyogo. It would be preferable to use data from the Hyogo Prefecture for a more realistic simulation, even if the simulated number of patients is similar to the actual number. Second, we determined the capacity setting of MT patients in each hospital. When evaluating a facility’s ability to accommodate patients, various factors must be taken into account. These include the quantity and working environment of attending physicians and co-medical staff, the level of overcrowding in the emergency department, and the availability of catheterization and operating rooms for providing treatment. In this research, the increase in capacity is not based on an estimation using the above-detailed supply factors but on actual numbers. In the future, it will be necessary to derive a prediction formula for capacity that includes the various factors mentioned above to provide information on the kind of intervention needed to increase capacity.
The third issue concerns temporal and seasonal variations. This simulation did not consider any road conditions at different times of the day or during different seasons. Road congestion is expected to differ during the day and night. Additionally, northern Hyogo Prefecture experiences heavy snowfall in the winter, which can significantly change road conditions and affect transportation time. Future work should include simulations that consider road conditions at different times of the day and during different seasons.
Fourth, the simulation did not consider the seasonality of patient occurrence. A National Cerebral and Cardiovascular Center study reported that the proportion of patients with cardiogenic cerebral embolisms was higher in winter when limited to elderly patients, those with cardiogenic cerebral embolisms, and those with moderate-to-severe disease.27) In this case, a tighter demand-supply balance will occur in the winter season. Future simulations should also consider seasonality on the demand side.
Conclusion
This study showed that the estimated number of patients (based on the incidence of cerebral infarction) according to age group and the percentage of cerebral thrombus retrieval therapy indicated approximate actual values and that the transport simulation was close to reality, taking both the supply and demand sides of healthcare into account.
Furthermore, it showed that the number of treatments per specialist was suitable for maintaining skills when facilities were consolidated. The results of this study are important for future medical policies in terms of the effective utilization of specialists, maintenance of skills, and cost reduction through consolidation. Therefore, further improvements in the accuracy of the simulation are required in future studies.
Funding
This research was supported by JSPS KAKENHI Grant Number 23K27823 for the cost of language editing and publication.
Disclosure Statement
The authors declare that they have no conflicts of interest.
References
- 1).Ministry of Health Law. Vital Statistics of Japan 2019. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei19/dl/15_all.pdf (in Japanese) (Accessed: June 15, 2023)
- 2).Omama S, Ogasawara K, Inoue Y, et al. Ten-year cerebrovascular disease trend occurrence by population-based stroke registry in an aging Japan local prefecture. J Stroke Cerebrovasc Dis 2020; 29: 104580. [DOI] [PubMed] [Google Scholar]
- 3).Ministry of Health LaW. Comprehensive Survey of Living Conditions. 2022. https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa22/dl/05.pdf (in Japanese) (Accessed: August 26, 2023)
- 4).The Japanese Circulation Society, the Japan Stroke Society. Five-Year Plan to Conquer Stroke and Cardiovascular Disease. 2016. https://www.j-circ.or.jp/five_year/files/five_year_plan.pdf (in Japanese) (Accessed: June 10, 2023)
- 5).The Japanese Circulation Society, the Japan Stroke Society. Second Five-Year Plan for Curing Stroke and Cardiovascular Disease. 2021. https://www.j-circ.or.jp/five_year/files/JCS_five_year_plan_2nd.pdf (in Japanese) (Accessed: June 10, 2023)
- 6).Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 7).Yamagami H, Hayakawa M, Inoue M. Guidelines for Mechanical Thrombectomy in Japan, the Fourth Edition, March 2020: A Guideline from the Japan Stroke Society, the Japan Neurosurgical Society, and the Japanese Society for Neuroendovascular Therapy. Neurol Med Chir (Tokyo) 2021; 61: 163–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Morii Y, Osanai T, Ishikawa T, et al. Cost effectiveness of drive and retrieve system in Hokkaido for acute ischemic stroke patient treatment using geographic information system. J Stroke Cerebrovasc Dis 2019; 28: 2292–2301. [DOI] [PubMed] [Google Scholar]
- 9).Freyssenge J, Renard F, Schott AM, et al. Measurement of the potential geographic accessibility from call to definitive care for patient with acute stroke. Int J Health Geogr 2018; 17: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Mokin M, Pendurthi A, Ljubimov V, et al. ASPECTS, large vessel occlusion, and time of symptom onset: estimation of eligibility for endovascular therapy. Neurosurgery 2018; 83: 122–127. [DOI] [PubMed] [Google Scholar]
- 11).Chia NH, Leyden JM, Newbury J, et al. Determining the number of ischemic strokes potentially eligible for endovascular thrombectomy: a population-based study. Stroke 2016; 47: 1377–1380. [DOI] [PubMed] [Google Scholar]
- 12).National Institute of Population and Social Security Research. Japan’s Future Population Projections by Region (2018 Estimates). https://www.ipss.go.jp/pp-shicyoson/j/shicyoson18/3kekka/Municipalities.asp (in Japanese) (Accessed: January 27, 2023)
- 13).Church R, Velle CR, ReVelle C. The maximal covering location problem. Pap Reg Sci 1974; 32: 101–118. [Google Scholar]
- 14).Murray AT. Maximal coverage location problem: impacts, significance, and evolution. Int Reg Sci Rev 2016; 39: 5–27. [Google Scholar]
- 15).Committee HPDHOC. Hyogo Prefecture Doctor Helicopter Operation Procedures, 8th Edition. 2022. https://hgmc.hyogo.jp/data/media/harima-hp/page/about/torikumi/doctorheli_procedure.pdf (in Japanese) (Accessed: October 15, 2023)
- 16).Hyogo Prefecture. Annual Report on Fire and Disaster Prevention. 2021. https://web.pref.hyogo.lg.jp/kk43/documents/r3_nenpou.pdf (in Japanese) (Accessed: October 15, 2023)
- 17).Sato F, Takahashi K, Kuga Y, et al. Efforts to shorten time from patient presentation to thrombectomy in acute ischemic stroke. Jpn J Stroke 2020; 42: 1–7. (in Japanese). [Google Scholar]
- 18).Yokohama City. Results of Mechanical Thrombectomy in the Fiscal Year 2020. 2021. https://www.city.yokohama.lg.jp/kenko-iryo-fukushi/kenko-iryo/iryo/gan/nokekkan/nou05-jisseki.files/0045_20220307.pdf (in Japanese) (Accessed: October 15, 2023)
- 19).Maeoka R, Nakagawa I, Sugie K, et al. How can the time to thrombectomy be reduced? - The challenge facing our new Stroke Care Center. Neurosurg Emerg 2018; 23: 88–93. (in Japanese) [Google Scholar]
- 20).Kurogi A, Onozuka D, Hagihara A, et al. Influence of hospital capabilities and prehospital time on outcomes of thrombectomy for stroke in Japan from 2013 to 2016. Sci Rep 2022; 12: 3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21).Lowther HJ, Harrison J, Hill JE, et al. The effectiveness of quality improvement collaboratives in improving stroke care and the facilitators and barriers to their implementation: a systematic review. Implement Sci 2021; 16: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Ren N, Ogata S, Kiyoshige E, et al. Associations between adherence to evidence-based, stroke quality indicators and outcomes of acute reperfusion therapy. Stroke 2022; 53: 3359–3368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).Stein LK, Mocco J, Fifi J, et al. Correlations between physician and hospital stroke thrombectomy volumes and outcomes: a nationwide analysis. Stroke 2021; 52: 2858–2865. [DOI] [PubMed] [Google Scholar]
- 24).Yoshimura S, Sakai N, Yamagami H, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med 2022; 386: 1303–1313. [DOI] [PubMed] [Google Scholar]
- 25).Miura M, Yoshimura S, Sakai N, et al. Endovascular therapy for middle cerebral artery M2 segment occlusion: subanalyses of RESCUE-Japan Registry 2. J Neurointerv Surg 2019; 11: 964–969. [DOI] [PubMed] [Google Scholar]
- 26).Malik A, Drumm B, D’Anna L, et al. Mechanical thrombectomy in acute basilar artery stroke: a systematic review and Meta-analysis of randomized controlled trials. BMC Neurol 2022; 22: 415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).Toyoda K, Koga M, Yamagami H, et al. Seasonal variations in neurological severity and outcomes of ischemic stroke - 5-year single-center observational study. Circ J 2018; 82: 1443–1450. [DOI] [PubMed] [Google Scholar]