Abstract
Objective
The primary aim of this study is to examine the prevalence of ankle osteoarthritis in patients with achondroplasia and to assess the impact of surgical correction of lower limb alignment on this prevalence. The secondary aim is to identify radiographic parameters associated with ankle osteoarthritis.
Design
This retrospective cohort study included 134 patients (268 ankles) who visited our institution between March 2014 and February 2023. Lower limb alignment was assessed using the mechanical axis deviation, lateral distal tibial angle, anterior distal tibial angle, and talar tilt angle. Ankle osteoarthritis was evaluated using the Van Dijk Osteoarthritis score and modified Kellgren–Lawrence (K-L) scale by 2 experienced orthopedic surgeons.
Results
The prevalence of ankle osteoarthritis in our study cohort was 29%, and that of advanced ankle osteoarthritis defined by Van Dijk Osteoarthritis scale III or modified K-L grade 4 was 0.8% (aged <40 years, 22%, and 0%; aged ≥40 years, 42% and 2%, respectively). Talar tilt angle was the only radiographic parameter that showed a significant correlation with the degree of ankle osteoarthritis (Van Dijk Osteoarthritis score, rs = 0.403, P < 0.001; modified K-L grade, rs = 0.385, P < 0.001).
Discussion
The prevalence of ankle osteoarthritis in achondroplasia is moderate, but the progression to advanced stages is uncommon. Ankle osteoarthritis in achondroplasia is strongly associated with increased talar tilt angle. This finding emphasizes caution regarding ankle osteoarthritis in achondroplasia with a nonparallel tibiotalar articular surface. Clinicians should, therefore, consider regularly assessing the talar tilt angle in patients with achondroplasia.
Keywords: arthritis, FGFR3, malalignment, tibial osteotomy, radiograph
Introduction
Achondroplasia is a congenital skeletal dysplasia resulting from a gain-of-function mutation in the FGFR3 gene. 1 With an incidence of 1 in 26,000 live births, it develops by sporadic or autosomal dominant transmission. 2 Its characteristic features include disproportionate short-limbed rhizomelic dwarfism, lumbar and foramen magnum stenosis, frontal bossing, and normal intelligence.3,4
Genu varum, bowing of the lower limbs, and joint laxity are also common in achondroplasia, with an incidence reported at 50% to 60%.5,6 Owing to the severity of these deformities, there has been ongoing concern regarding the possibility of developing osteoarthritis in adulthood among patients with achondroplasia. Despite the malalignment of the lower limbs, degenerative osteoarthritis is known to rarely occur in achondroplasia, and osteoarthritis in achondroplasia is not considered a prevalent problem.3,7,8 Recent animal studies suggest that activation of FGFR3 may confer protection against the development of osteoarthritis.9,10
However, to date, no comprehensive study has been conducted to confirm the association between osteoarthritis and achondroplasia, other than expert opinions or fragmentary clinical observations. Recognizing the need for more substantial evidence, this study was designed with the primary aim of investigating the prevalence of ankle osteoarthritis in patients with achondroplasia; and assessing whether the surgical correction of lower limb alignment influences this prevalence. In addition, a secondary aim of this study was to identify specific radiographic parameters that may be associated with the development and severity of ankle osteoarthritis in achondroplasia. We hypothesized that the prevalence of ankle osteoarthritis in achondroplasia would be uncommon as it is currently recognized and affected by concurrent ankle joint alignment.
Methods
Patient Selection
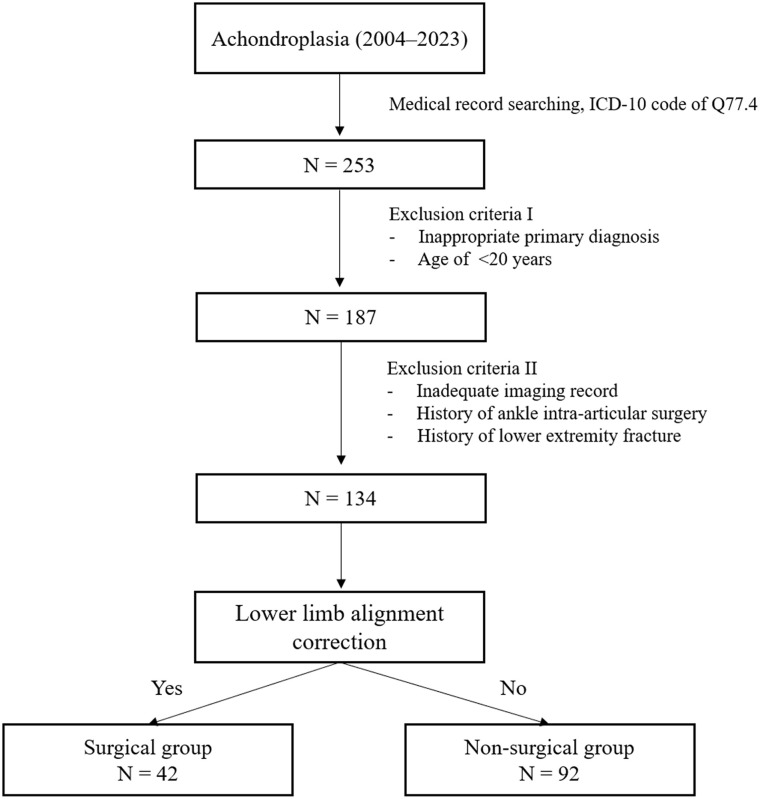
After obtaining approval from the local ethics committee in March 2023, we conducted an electronic medical record search of the patients who had visited our institution (University Hospital’s Department of Orthopaedic Surgery) between March 2014 and February 2023 and identified 253 patients with ICD-10 (International Classification of Diseases 10th Revision) code Q77.4, indicating achondroplasia. Among these patients, those who did not undergo genetic evaluation and those younger than 20 years were excluded. Patients with missing imaging data (e.g., weight-bearing lower-extremity radiographs), a history of lower-extremity fractures, or ankle intra-articular surgery were also excluded. After applying the exclusion criteria, 134 patients were included in this study ( Fig. 1 ). Retrospective data extraction was conducted by an author who was not involved in radiographic measurements or osteoarthritis assessments.
Figure 1.
Flow diagram of the study.
To investigate the effect of limb alignment correction on the development of ankle osteoarthritis, the enrolled patients were categorized into 2 groups. The surgical group included patients who underwent surgical treatments that affected the radiological parameters of lower limb alignment, including femoral or tibial corrective osteotomy, limb lengthening, or guided growth surgeries. The remaining patients who did not undergo surgical treatment were defined as the nonsurgical group.
Evaluation of Ankle Osteoarthritis
The primary outcome of this study, the degree of ankle osteoarthritis, was evaluated radiographically using the Van Dijk Osteoarthritis score and the modified Kellgren and Lawrence (K-L) scale.11-13 The Van Dijk osteoarthritis grades are as follows: grade 0, normal joint or subchondral sclerosis; grade I, osteophytes without joint space narrowing; grade II, joint space narrowing with or without osteophytes; and grade III, subtotal/total disappearance or deformation of the joint space. The original K-L scale has been used to evaluate osteoarthritis in various joints, and the modified version has been validated specifically for the radiological assessment of ankle posttraumatic osteoarthritis.11,14,15 The grades for modified K-L scale are as follows: grade 0, no radiographic features of osteoarthritis are present; grade 1, osteophytes of doubtful meaning on the medial or lateral malleolus, rare tibial sclerosis, joint space width unimpaired; grade 2, definite osteophytes on the medial malleolus, joint space width unimpaired; grade 3, definite osteophytes on the medial and/or lateral malleolus, moderate (<50%) joint space width narrowing; grade 4, definite osteophytes on medial and lateral malleoli as well as tibiotalar joint margins, severe (>50%) to complete joint space narrowing, constant tibiotalar sclerosis. In this study, advanced ankle osteoarthritis was defined as grade III according to the Van Dijk Osteoarthritis scale and grade 4 according to the modified K-L scale.16-18 The grades of the Van Dijk Osteoarthritis and modified K-L scales for each patient were determined independently by 2 orthopedic surgeons, and disagreements were resolved through discussion between the 2 evaluators to reach a consensus.
Assessment of Lower Limb Alignment
As a secondary outcome of this study, the radiographic assessments of lower limb alignment were performed by measuring the mechanical axis deviation (MAD), lateral distal tibial angle (LDTA), anterior distal tibial angle (ADTA), and talar tilt angle (TTA) ( Fig. 2 ). On the weight-bearing anteroposterior radiograph, MAD was determined as the perpendicular distance between the mechanical axis of the lower extremity and the center of the knee joint. 19 On the same radiograph, the LDTA was measured as the angle between the tibial axis and tibial plafond, and TTA was measured as the angle between the tibial plafond and the talar dome. On the weight-bearing lateral radiograph, the ADTA was measured as the angle between the axis of the tibia and a line drawn between the anterior and posterior margins of the tibial plafond to represent the articular surface of the distal aspect of the tibia.20,21 Reference values for the MAD, LDTA, ADTA, and TTA were set to 10 mm, 89°, 80°, and 0°, respectively.22,23 Two orthopedic surgeons performed measurements, and the average values obtained from both were used for statistical analysis.
Figure 2.
Radiographic parameters for the assessment of lower limb alignment. MAD, mechanical axis deviation; LDTA, lateral distal tibial angle; ADTA, anterior distal tibial angle; TTA, talar tilt angle.
Statistical Analyses
Data normality was determined using the Kolmogorov–Smirnov test. The independent t-test was used to compare the following continuous variables: age, body mass index, MAD, LDTA, ADTA, and TTA. The chi-square test or Fisher’s exact test was used to compare the following categorical variables: sex, grades of Van Dijk Osteoarthritis and K-L scales. Spearman’s rank correlation analysis was used to identify the correlation between lower limb alignment and ankle osteoarthritis. The radiographic parameters for lower limb alignment were converted to the absolute value of the difference from the reference value. Interobserver reliabilities for the grades of the Van Dijk Osteoarthritis and K-L scales were assessed by calculating the kappa coefficient (κ), and the values were judged as follows: poor (<0.2), fair (0.21-0.40), moderate (0.41-0.60), substantial (0.61-0.80), and almost perfect (>0.81). 24 The interobserver reliability of lower limb alignment measurement was determined using the intraclass correlation coefficient (ICC), with the following criteria applied for interpretation: poor (<0.5), moderate (0.5-0.75), good (0.75-0.9), and excellent (>0.9). 25 Statistical analyses were performed using SPSS software version 23.0 (IBM, Armonk, New York), and statistical significance was set at values of P < 0.05.
Results
Of the 134 patients, 42 (31.3%) were included in the surgical group, and 92 (68.7%) in the nonsurgical group. In the surgical group, the average time elapsed after lower-extremity correction was 104 ± 67.8 months (range = 20-203 months). Among the patients, 6 (14.3%) underwent distal femoral corrective osteotomy for varus deformity, 7 (16.6%) underwent proximal tibial corrective osteotomy for varus deformity, 2 (4.8%) had simultaneous distal femoral and proximal tibial corrective osteotomy for varus deformity, 24 (57.2%) underwent limb lengthening with correction using an external fixation device, and 3 (7.1%) underwent guided growth surgeries, including hemiepiphysiodesis. No statistically significant differences in patient characteristics were observed between the 2 groups ( Table 1 ). Among the patients, 10 in the surgical group and 37 in the nonsurgical group were aged ≥40 years. When the 2 groups were stratified based on the age of 40 years, no differences in sex, age, or body mass index were observed between the groups.
Table 1.
Characteristics of the Study Patients.
| Total (134 patients) | Surgical group (42 patients) | Nonsurgical group (92 patients) | P | |
|---|---|---|---|---|
| Sex | 0.122 | |||
| Male | 66 (49) | 18 (43) | 50 (54) | |
| Female | 68 (51) | 24 (57) | 42 (46) | |
| Age, years | 32.7 ± 10.3 | 30.4 ± 8.4 | 36.4 ± 12.9 | 0.349 |
| BMI, kg/m2 | 26.7 ± 5.4 | 26.8 ± 5.8 | 25.2 ± 5.3 | 0.572 |
Data are presented as mean ± standard deviation or number of patients (%).
BMI, body mass index.
Ankle Osteoarthritis
In our study cohort, the prevalence of ankle osteoarthritis and advanced ankle osteoarthritis was 29% and 0.8%, respectively. When comparing ankle osteoarthritis between the 2 groups based on the age of 40 years, 22% of patients aged <40 years showed ankle osteoarthritis, but none exhibited advanced ankle osteoarthritis. Furthermore, no significant difference in the degree of ankle osteoarthritis according to the osteoarthritis grading system was observed between the 2 groups ( Table 2 ). In the group aged ≥40 years, 42% of the patients showed ankle osteoarthritis, and 2% of the patients exhibited advanced ankle osteoarthritis. Similar to those aged <40 years, the degree of ankle osteoarthritis did not differ between the 2 groups ( Table 3 ). The kappa coefficient was 0.522 (moderate reliability) for the Van Dijk Osteoarthritis scale and 0.326 (fair reliability) for the K-L scale. Body mass index (BMI) did not show any correlation with the degree of ankle osteoarthritis in achondroplasia.
Table 2.
Assessment of Ankle Osteoarthritis in Patients With Achondroplasia Aged <40 Years in the Surgical and Nonsurgical Groups.
| Total (174 ankles) | Surgical group (64 ankles) | Nonsurgical group (110 ankles) | P | |
|---|---|---|---|---|
| Van Dijk score | 0.527 | |||
| 0 | 153 (88) | 54 (84) | 99 (90) | |
| I | 17 (10) | 8 (13) | 9 (8) | |
| II | 4 (2) | 2 (3) | 2 (2) | |
| III | 0 (0) | 0 (0) | 0 (0) | |
| K-L scale | 0.419 | |||
| 0 | 136 (78) | 46 (72) | 90 (82) | |
| 1 | 22 (13) | 11 (17) | 11 (10) | |
| 2 | 12 (7) | 5 (8) | 7 (6) | |
| 3 | 4 (2) | 2 (3) | 2 (2) | |
| 4 | 0 (0) | 0 (0) | 0 (0) |
Data are presented as number of patients (%). K-L, Kellgren and Lawrence.
Table 3.
Assessment of Ankle Osteoarthritis in Patients With Achondroplasia Aged ≥40 Years in the Surgical and Nonsurgical Groups.
| Total (94 ankles) | Surgical group (20 ankles) | Nonsurgical group (74 ankles) |
P | |
|---|---|---|---|---|
| Van Dijk score | 0.270 | |||
| 0 | 67 (71) | 12 (60) | 55 (74) | |
| I | 23 (25) | 7 (35) | 16 (22) | |
| II | 2 (2) | 1 (5) | 1 (1) | |
| III | 2 (2) | 0 (0) | 2 (3) | |
| K-L scale | 0.201 | |||
| 0 | 54 (58) | 8 (40) | 46 (62) | |
| 1 | 16 (17) | 4 (20) | 12 (16) | |
| 2 | 20 (21) | 7 (35) | 13 (18) | |
| 3 | 2 (2) | 1 (5) | 1 (1) | |
| 4 | 2 (2) | 0 (0) | 2 (3) |
Data are presented as number of patients (%).
K-L, Kellgren and Lawrence.
Lower Limb Alignment
A comparison of lower limb alignment between the surgical and nonsurgical groups revealed significant differences in LDTA and MAD, with both showing P < 0.001. Alignment values in the surgical group were closer to normal ranges, reflecting the effect of surgical correction ( Table 4 ). The ICC values of MAD, LDTA, ADTA, and TTA were 0.882, 0.906, 0.891, and 0.926, respectively, indicating good to excellent reliability.
Table 4.
Comparison of Lower Limb Alignment Between Patients With Achondroplasia in the Surgical And Nonsurgical Groups.
| Total (268 ankles) | Surgical group (84 ankles) | Nonsurgical group (184 ankles) | P | |
|---|---|---|---|---|
| MAD, cm | 17.3 ± 19.6 | 8.1 ± 14.8 | 21.6 ± 20.0 | <0.001 |
| LDTA, ° | 103.9 ± 11.5 | 93.9 ± 124 | 108.4 ± 7.4 | <0.001 |
| ADTA, ° | 84.8 ± 7.8 | 83.5 ± 11.1 | 85.4 ± 5.8 | 0.076 |
| TTA, ° | 1.3 ± 1.8 | 1.4 ± 1.9 | 1.3 ± 1.8 | 0.554 |
Data are presented as mean ± standard deviation. The results in bold are considered statistically significant (P < 0.05).
MAD, mechanical axis deviation; LDTA, lateral distal tibial angle; ADTA, anterior distal tibial angle; TTA, talar tilt angle.
Correlation Between the Lower Limb Alignment and Ankle Osteoarthritis
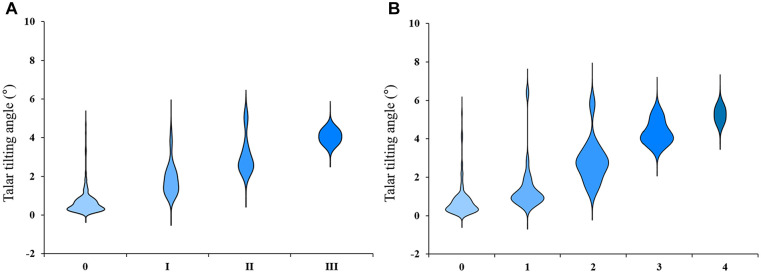
The TTA was the only radiographic parameter that exhibited a statistically significant correlation with the degree of ankle osteoarthritis, consistent across all age groups and grading systems for ankle osteoarthritis (Van Dijk Osteoarthritis score, rs = 0.403, P < 0.001, modified K-L grade, rs = 0.385, P < 0.001) ( Fig. 3 and Table 5 ).
Figure 3.
Violin plot illustrating the relationship between talar tilting angle and ankle osteoarthritis in achondroplasia patients: (A) Van Dijk Osteoarthritis Score and (B) modified Kellgren and Lawrence scale.
Table 5.
Correlation Between Lower Limb Alignment and Ankle Osteoarthritis in Patients With Achondroplasia.
| MAD | LDTA | ADTA | TTA | |
|---|---|---|---|---|
| Age <40 years (174 ankles) | ||||
| Van Dijk scale | rs = –0.152 P = 0.145 |
rs = 0.062 P = 0.550 |
rs = 0.074 P = 0.508 |
rs = 0.510 P < 0.001 |
| K-L scale | rs = –0.168 P = 0.105 |
rs = 0.082 P = 0.431 |
rs = 0.102 P = 0.363 |
rs = 0.515 P < 0.001 |
| Age ≥40 years (94 ankles) | ||||
| Van Dijk scale | rs = 0.077 P = 0.315 |
rs = 0.042 P = 0.583 |
rs = 0.072 P = 0.371 |
rs = 0.306 P < 0.001 |
| K-L scale | rs = 0.115 P = 0.129 |
rs = 0.046 P = 0.550 |
rs = 0.098 rs = 0.226 |
rs = 0.252 P = 0.001 |
The results in bold are considered statistically significant (P < 0.05).
MAD, mechanical axis deviation; LDTA, lateral distal tibial angle; ADTA, anterior distal tibial angle; TTA, talar tilt angle; K-L, Kellgren and Lawrence.
Discussion
Achondroplasia presents as severe malalignment of the ankle joint; however, its impact on the development of ankle osteoarthritis has not been extensively studied. To address this issue, we performed a retrospective cohort study to investigate the prevalence of ankle osteoarthritis and identify radiographic parameters that correlated with the progression of ankle osteoarthritis. The primary finding of this study indicated that the prevalence of ankle osteoarthritis in patients with achondroplasia was 29%, with 0.8% of patients developing advanced ankle osteoarthritis. The TTA demonstrated a significant correlation with ankle osteoarthritis, which appeared to progress as the absolute TTA value increased. These results emphasize the importance of careful monitoring of patients with achondroplasia, particularly those with nonparallel tibiotalar articular surfaces, because they are more likely to develop advanced ankle osteoarthritis.
According to the recent systematic review, 8.8% of the normal older adult population showed radiographic signs of ankle osteoarthritis and 1.9% showed advanced ankle osteoarthritis that represented severe joint space narrowing. 26 In this study, 42% of patients with achondroplasia aged ≥40 years exhibited radiographic signs of ankle osteoarthritis. However, the prevalence of advanced ankle osteoarthritis in achondroplasia aged ≥40 years was only 2.0%, which was comparable to that of the normal population. These findings indicate that although patients with achondroplasia are more susceptible to ankle osteoarthritis than normal older adults, the likelihood of developing advanced ankle osteoarthritis is not higher. We believe that these findings support the previous view that achondroplasia does not significantly increase the risk of developing advanced osteoarthritis, and that osteoarthritis is, therefore, not a major concern for the population of patients with achondroplasia.3,7
In the present study, TTA was the only radiographic parameter that demonstrated a significant correlation with ankle osteoarthritis. The TTA represents the parallelism of the tibiotalar articular surface, and it increases when there is a ligament imbalance around the ankle joint. These findings indicate that joint space integrity, rather than skeletal deformities, such as tibial bowing or varus, is a major contributing factor to the development of ankle osteoarthritis in achondroplasia. In fact, in the comparison between the surgical and nonsurgical groups, no significant difference in the degree of ankle osteoarthritis was observed between the 2 groups, even though MAD, LDTA, and ADTA improved after lower limb correction surgery. Previous studies have also highlighted that increased TTA is a risk factor for ankle osteoarthritis.27,28 Therefore, our findings emphasize the importance of ankle ligament balance and suggest proactive correction through ligament surgery in cases where ligament imbalances with nonparallel tibiotalar articular surfaces are present in the ankles of patients with achondroplasia.29,30
The strengths of this study lie in the facts that a large number of patients were included, the degree of osteoarthritis was objectively assessed using radiographic parameters, and the study focused on a broad range of deformities in both the surgical and nonsurgical groups. However, this study has several limitations. First, the modified K-L scale used to assess ankle osteoarthritis was originally formulated for the varus ankle joint and may not fully capture all ankle deformities such as valgus ankle joints, observed in some of our study patients. This may be the reason for the low kappa coefficient of the modified K-L scale. To compensate for this, the Van Dijk Osteoarthritis scale was also used; however, the low reliability of the modified K-L scale is considered a limitation of this study. Second, in the surgical group, the mean postoperative follow-up period was 8.7 years, which may not be adequate in determining whether the improved radiographic parameters influenced the progression of ankle osteoarthritis or not. Given that most patients were in their 30s or younger at the time of surgical intervention, it could be argued that a longer follow-up period was necessary. Third, we investigated the prevalence of ankle osteoarthritis by categorizing the study population based on the age of 40. This was decided upon on the basis of a previous report on trends in the incidence and prevalence of osteoarthritis. 31 However, this age standard may be relatively young. Although the average life span of patients with achondroplasia is approximately 10 years less than that of the general population,32,33 additional analysis targeting older age groups such as those in their 60s or 70s is necessary. Unfortunately, the small sample size of elderly patients in this study restricted this analysis. To address this limitation, we plan to conduct a long-term follow-up of the study cohort to assess outcomes over extended postoperative periods and into advanced age.
Conclusion
Patients with achondroplasia are prone to ankle osteoarthritis; however, the likelihood of developing advanced ankle osteoarthritis does not appear to be higher than in the general population. Our study found a significant association between TTA values and ankle osteoarthritis, emphasizing the importance of recognizing osteoarthritis in achondroplasia, especially in cases with a nonparallel tibiotalar articular surface. These findings may inform future research on clinical management and joint preservation strategies in this population.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author Contributions: Won Seok Choi: Data curation, formal analysis, and writing—original draft.
Joung Woo Shin: Data curation, investigation, and methodology.
Sei Wook Son: Resources, supervision, and validation.
Hak Jun Kim: Conceptualization and validation.
Sang Hyeon Hwang: Resources and supervision.
Sang Geon Park: Resources, supervision, and methodology.
Young Hwan Park: Conceptualization, investigation, supervision, and writing—review & editing.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: This study was approved by the Institutional Review Board of the authors’ institutions (IRB No. 2023GR0310).
ORCID iD: Young Hwan Park  https://orcid.org/0000-0002-1732-5405
https://orcid.org/0000-0002-1732-5405
References
- 1. Naski MC, Wang Q, Xu J, Ornitz DM. Graded activation of fibroblast growth factor receptor 3 by mutations causing achondroplasia and thanatophoric dysplasia. Nat Genet. 1996;13(2):233-7. [DOI] [PubMed] [Google Scholar]
- 2. Stoll C, Dott B, Roth MP, Alembik Y. Birth prevalence rates of skeletal dysplasias. Clin Genet. 1989;35(2):88-92. [DOI] [PubMed] [Google Scholar]
- 3. Bailey JAII. Orthopaedic aspects of achondroplasia. J Bone Joint Surg Am. 1970;52(7):1285-301. [PubMed] [Google Scholar]
- 4. Ponseti IV. Skeletal growth in achondroplasia. J Bone Joint Surg Am. 1970;52(4):701-16. [PubMed] [Google Scholar]
- 5. Stanley G, McLoughlin S, Beals RK. Observations on the cause of bowlegs in achondroplasia. J Pediatr Orthop. 2002;22(1):112-6. [PubMed] [Google Scholar]
- 6. Kopits SE. Orthopedic complications of dwarfism. Clin Orthop Relat Res. 1976;114:153-79. [PubMed] [Google Scholar]
- 7. Lee ST, Song HR, Mahajan R, Makwana V, Suh SW, Lee SH. Development of genu varum in achondroplasia: relation to fibular overgrowth. J Bone Joint Surg Br. 2007;89(1):57-61. [DOI] [PubMed] [Google Scholar]
- 8. Pauli RM. Achondroplasia: a comprehensive clinical review. Orphanet J Rare Dis. 2019;14(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tang J, Su N, Zhou S, Xie Y, Huang J, Wen X, et al. Fibroblast growth factor receptor 3 inhibits osteoarthritis progression in the knee joints of adult mice. Arthritis Rheumatol. 2016;68(10):2432-43. [DOI] [PubMed] [Google Scholar]
- 10. Okura T, Matsushita M, Mishima K, Esaki R, Seki T, Ishiguro N, et al. Activated FGFR3 prevents subchondral bone sclerosis during the development of osteoarthritis in transgenic mice with achondroplasia. J Orthop Res. 2018;36(1):300-8. [DOI] [PubMed] [Google Scholar]
- 11. Holzer N, Salvo D, Marijnissen AC, Vincken KL, Ahmad AC, Serra E, et al. Radiographic evaluation of posttraumatic osteoarthritis of the ankle: the Kellgren-Lawrence scale is reliable and correlates with clinical symptoms. Osteoarthritis Cartilage. 2015;23(3):363-9. [DOI] [PubMed] [Google Scholar]
- 12. van Dijk CN, Verhagen RA, Tol JL. Arthroscopy for problems after ankle fracture. J Bone Joint Surg Br. 1997;79(2):280-4. [DOI] [PubMed] [Google Scholar]
- 13. Claessen FM, Meijer DT, van den Bekerom MP, Gevers Deynoot BD, Mallee WH, Doornberg JN, et al. Reliability of classification for post-traumatic ankle osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Park YH, Jang KS, Yeo ED, Choi GW, Kim HJ. Comparison of outcome of deltoid ligament repair according to location of suture anchors in rotational ankle fracture. Foot Ankle Int. 2021;42(1):62-8. [DOI] [PubMed] [Google Scholar]
- 16. Son KM, Hong JI, Kim DH, Jang DG, Crema MD, Kim HA. Absence of pain in subjects with advanced radiographic knee osteoarthritis. BMC Musculoskelet Disord. 2020;21(1):640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Herrera-Perez M, Valderrabano V, Godoy-Santos AL, de Cesar Netto C, Gonzalez-Martin D, Tejero S. Ankle osteoarthritis: comprehensive review and treatment algorithm proposal. EFORT Open Rev. 2022;7(7):448-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rikken QGH, Dahmen J, Stufkens SAS, Kerkhoffs G. Satisfactory long-term clinical outcomes after bone marrow stimulation of osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3525-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gordon JE, Chen RC, Dobbs MB, Luhmann SJ, Rich MM, Schoenecker PL. Interobserver and intraobserver reliability in the evaluation of mechanical axis deviation. J Pediatr Orthop. 2009;29(3):281-4. [DOI] [PubMed] [Google Scholar]
- 20. Lee WC, Moon JS, Lee K, Byun WJ, Lee SH. Indications for supramalleolar osteotomy in patients with ankle osteoarthritis and varus deformity. J Bone Joint Surg Am. 2011;93(13):1243-8. [DOI] [PubMed] [Google Scholar]
- 21. Inan M, Jeong C, Chan G, Mackenzie WG, Glutting J. Analysis of lower extremity alignment in achondroplasia: interobserver reliability and intraobserver reproducibility. J Pediatr Orthop. 2006;26(1):75-8. [DOI] [PubMed] [Google Scholar]
- 22. Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25(3):425-65. [PubMed] [Google Scholar]
- 23. Marques Luis N, Varatojo R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021;6(6):487-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74. [PubMed] [Google Scholar]
- 25. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Murray C, Marshall M, Rathod T, Bowen CJ, Menz HB, Roddy E. Population prevalence and distribution of ankle pain and symptomatic radiographic ankle osteoarthritis in community dwelling older adults: a systematic review and cross-sectional study. PLoS ONE. 2018;13(4):e0193662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Choudhury AK, Bansal S, Pranav J, Raja BS, Gupta T, Paul S, et al. Increased medial talar tilt may incite ankle pain and predispose ankle osteoarthritis after correction of severity of knee varus deformity among patients undergoing bilateral total knee arthroplasty: a prospective observation. Knee Surg Relat Res. 2024;36(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kyung MG, Cho YJ, Lee J, Lee W, Kim DY, Lee DO, et al. Relationship between talofibular impingement and increased talar tilt in incongruent varus ankle osteoarthritis. J Orthop Surg. 2021;29(3):23094990211045219. [DOI] [PubMed] [Google Scholar]
- 29. Golditz T, Steib S, Pfeifer K, Uder M, Gelse K, Janka R, et al. Functional ankle instability as a risk factor for osteoarthritis: using T2-mapping to analyze early cartilage degeneration in the ankle joint of young athletes. Osteoarthritis Cartilage. 2014;22(10):1377-85. [DOI] [PubMed] [Google Scholar]
- 30. Sakurai S, Nakasa T, Ikuta Y, Kawabata S, Moriwaki D, Ishibashi S, et al. The relationship between calcaneofibular ligament injury and ankle osteoarthritis progression: a comprehensive analysis of stress distribution and osteophyte formation in the subtalar joint. Foot Ankle Int. 2024;45(8):870-8. [DOI] [PubMed] [Google Scholar]
- 31. Swain S, Sarmanova A, Mallen C, Kuo CF, Coupland C, Doherty M, et al. Trends in incidence and prevalence of osteoarthritis in the United Kingdom: findings from the Clinical Practice Research Datalink (CPRD). Osteoarthritis Cartilage. 2020;28(6):792-801. [DOI] [PubMed] [Google Scholar]
- 32. Hecht JT, Francomano CA, Horton WA, Annegers JF. Mortality in achondroplasia. Am J Hum Genet. 1987;41(3):454-64. [PMC free article] [PubMed] [Google Scholar]
- 33. Wynn J, King TM, Gambello MJ, Waller DK, Hecht JT. Mortality in achondroplasia study: a 42-year follow-up. Am J Med Genet A. 2007;143A(21):2502-11. [DOI] [PubMed] [Google Scholar]