Abstract
Background:
Distal radius fractures (DRFs) are some of the most common injuries suffered by the elderly; however, there are varied opinions on management. As there is limited research on patient factors affecting functional outcomes in conservatively managed patients with DRFs, this study aimed to find predictive factors for functional outcomes in such patients.
Methods:
Patients with DRFs satisfying the inclusion criteria were managed with closed reduction and slab followed by cast application. Radiological parameters (radioulnar angulation, dorsal tilt, radial height, and ulnar variance) and functional scores (patient-rated wrist evaluation [PRWE] score, Short Form 8 questionnaire [SF-8], and QuickDASH [Disabilities of the Arm, Shoulder, and Hand]-9) were recorded prereduction, postreduction, at the time of cast removal, and in follow-up visits. Patient factors such as underlying diseases were also recorded, and correlations were analyzed using appropriate software.
Results:
Patients with diabetes (43.33% of patients) and those with loss in radial height through the course of treatment were found to have poorer functional outcomes (P-values less than .05 for all functional scores—PRWE, QuickDASH-9, SF-8—except SF-8 at 12 weeks). Patients younger than 60 years were also found to have better functional outcomes at 24 weeks (for PRWE: P-value = .048, for QuickDASH-9: P-value = .032, and for SF-8: P-value = .026).
Conclusion:
Conservative management plays a major role in the treatment of DRFs, despite the increasing trend of operative management. Diabetes was found to be a predictor of poorer functional outcomes; however, further research is needed to determine the role of these and other factors in detail.
Keywords: wrist, anatomy, distal radius, fracture/dislocation, trauma, diagnosis, outcomes, research and health outcomes, post traumatic, arthritis, non operative management
Introduction
Distal radius fractures (DRFs) are among the most common fractures suffered by the elderly in cases of wrist trauma due to low-energy impacts (such as a fall on the outstretched hand) and account for approximately 17.5% of all adult fractures. 1 There are conflicting opinions regarding DRFs in the elderly population. There are various fracture patterns, with many modalities of treatment, and multiple comparisons have been made between surgical and nonsurgical treatment. Although the management of these cases is quite varied, closed reduction with cast immobilization remains an affordable and successful method of treatment for DRFs, especially in older individuals with low physical demands. The collective evidence largely supports nonoperative management in the elderly population even though reduction may be more anatomical in cases managed operatively. 2
Radiographic parameters of successful or acceptable union may not always correlate with functional outcome and there is no consensus. Minor radiological malalignments have been found in follow-up radiographs of cases treated with closed reduction and cast application; however, it has been seen that many fracture reductions which may not be acceptable radiologically are, in fact, functionally quite acceptable for the older population. 3 There is, however, a dearth of studies regarding the predictors of functional outcomes in nonoperatively managed DRFs. Such literature would enable us to formulate targeted treatment plans, explain prognosis, and proceed with the appropriate rehabilitation of such patients. This study aimed to assess for any correlation between patient factors and reduction-related radiological parameters, and the functional outcomes in nonoperatively treated extra-articular DRFs in elderly patients.
Materials and Methods
The study was conducted from March 2021 to June 2022, in an Urban Tertiary Care Hospital in India, after obtaining ethical clearance from the Institutional Ethics Committee. Sample size was calculated to be 23 (for a power of 80%) based on a study by Amorosa et al. 4 Convenient sampling was used and all patients aged 50 years or more with extra-articular, unilateral, or bilateral fractures of the distal radius (with or without ulnar styloid involvement, ie: AO classification 23A2 and 23A3, with all subtypes) were included in the study. Patients with pre-existing bony abnormalities (hypoplastic, deformed, associated tumor(s), signs of infection, advanced arthritic joints, skeletal dysplasia, signs of old fracture, pathological fracture), neuromuscular disorders, delayed presentation (more than 2 weeks old), associated ipsilateral upper limb fractures (forearm, humerus, clavicle, scapula), and patients who did not consent to participate in the study were excluded. AO Type C (articular) fractures and irreducible fractures were also excluded.
A detailed history was taken along with a thorough clinical examination, and patient factors including underlying medical conditions (eg, hypertension, diabetes, endocrine abnormalities), age, sex, hand dominance, and side of the fracture were recorded. Prereduction radiographs were assessed to classify fracture patterns. Functional scores (patient-rated wrist evaluation [PRWE], Disabilities of the Arm, Shoulder, and Hand-9 [QuickDASH-9], Visual Analogue Scale [VAS] for pain, and the Short Form 8 [SF-8] questionnaire) were also recorded prereduction (post-injury) to obtain a baseline.5 -7
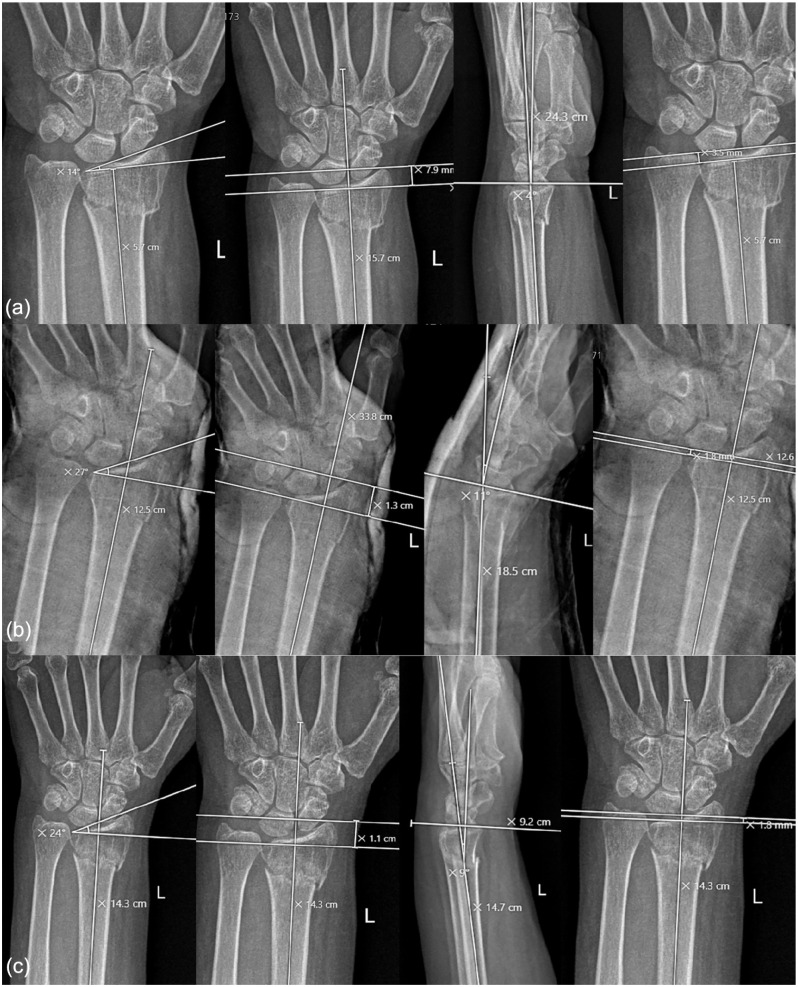
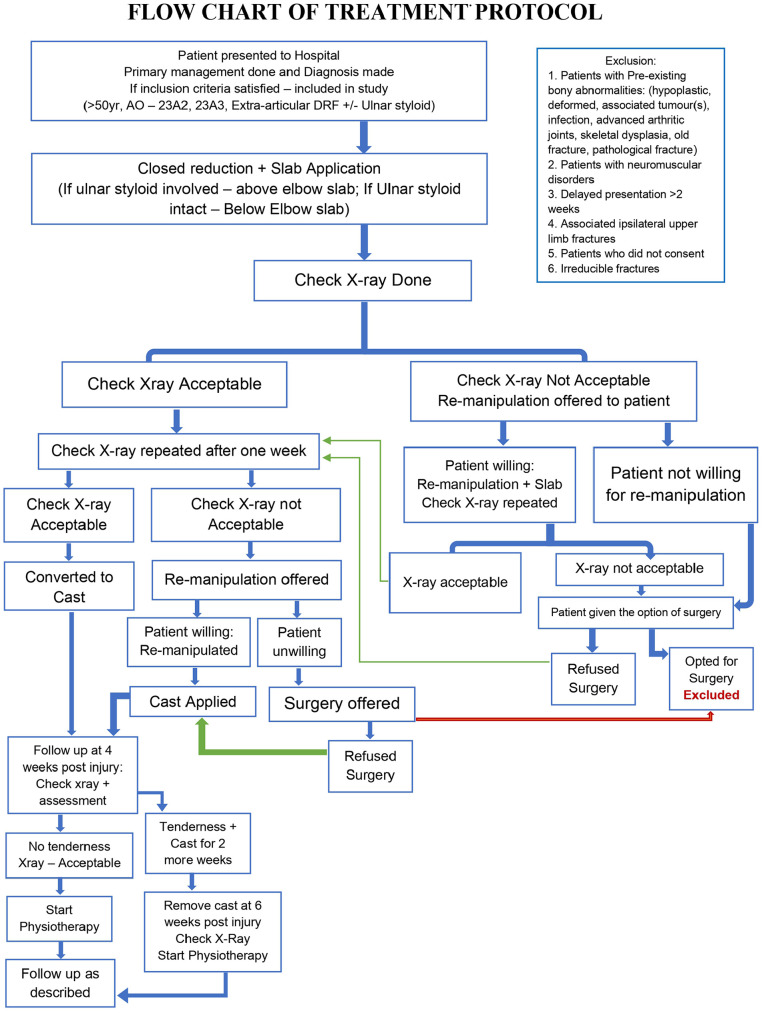
Reductions were performed by 3 doctors in a standard manner, 8 under analgesic cover, and with informed consent. The patient was positioned supine with the arm in pronation and traction and counter traction were applied. A third doctor would first milk the fracture and then apply an upward and radially directed force to position the wrist in palmar flexion and ulnar deviation to attempt reduction, followed by slab application. A point to note is that all patients with ulnar styloid involvement received above elbow slabs and casts.9,10 Check radiographs were done immediately postreduction to confirm acceptability by studying the change in radiological parameters of alignment (angulation, ulnar variance, radial height, and radioulnar inclination) between prereduction and postreduction radiographs (Figure 1). A single re-manipulation attempt was given if the reduction was unacceptable. Following slab application, management was performed according to the protocol shown in Figure 2. Range of motion and functional scores were recorded at follow-up visits after cast removal at 12 and 24 weeks. Radiological parameters described above were also recorded at cast removal according to the protocol in Figure 2.
Figure 1.
Radiographs showing various radiological parameters and measurements at (a) prereduction, (b) postreduction, and (c) cast removal.
Figure 2.
Flowchart of the treatment protocol. DRF = distal radius fracture.
Data entry was done using MS Excel 2019, and statistical analysis was done using MS Excel 2019 and SPSS ver. 29.0, using appropriate correlation tests such as Spearman correlation test.
Results
There were a total of 30 patients, with 24 women and 6 men. The mean age of the study group was found to be 58.87 ± 8.278 years. The age range was 50 to 81 years. Out of the total of 30 cases, 16 (53.3%) cases had fractures affecting the right wrist, and 14 (46.7%) had fractures affecting the left wrist. There were no bilateral fractures. Of the 30 cases, 4 (13.3%) were AO classification 2R3A2.1 (simple extra-articular fractures), 18 (60%) were 2R3A2.2 (Colle fracture), and 8 (26.7%) were 2R3A3.3 (extra-articular DRF fractures with metaphyseal comminution). A total of 13 patients (43.3%) had Frykman type I fractures (DRF not associated with ulnar styloid fracture) and 17 patients had Frykman type II fractures (DRF associated with ulnar styloid fractures). In total, 21 patients had comorbidities while 9 did not. Fractures united by 12 weeks in all cases.
The mean prereduction parameters were as follows: angulation = 11.93 degrees dorsal ± 8.87, ulnar variance = 0.66 ± 1.89 mm, and radioulnar inclination = 13.77 ± 6.52 degrees.
The mean postreduction parameters were as follows: angulation = 5.07 degrees palmar ± 6.76, ulnar variance = 0.12 ± 1.30 mm, radioulnar inclination = 22.03 ± 4.21 degrees, and radial height = 11.36 ± 1.56 mm. These values indicated acceptable reductions.
The mean radiological parameters at cast removal were as follows: angulation = 4.90 degrees palmar ± 6.467, ulnar variance = 0.15 ± 1.291 mm, radioulnar inclination = 21.60 ± 4.288 degrees, and radial height = 10.85 ± 1.663 mm. This demonstrates that even in patients with circumferential casting, a certain degree of loss of reduction does occur.
Functional scoring showed the following result: mean PRWE score at 12 weeks was 25.82 ± 9.98 and at 24 weeks was 17.90 ± 8.48. The mean QuickDASH-9 score at 12 weeks was 24.14 ± 11.14 and at 24 weeks was 13.59 ± 8.35. The mean VAS score at 6 weeks was 4.27 ± 1.57, at 12 weeks was 2.17 ± 1.12, and at 24 weeks was 0.80 ± 1.06. The mean SF-8 score at 12 weeks was 15.13 ± 3.36 and at 24 weeks was 11.00 ± 3.34. The decreasing scores indicate functional improvement over time.
The presence of diabetes mellitus (43.33% of patients) had a significant impact on functional scores, with poorer outcomes reported by those affected (P-value less than .05 for all scores—PRWE, SF-8, and QuickDASH-9) at 12 and 24 weeks except SF-8 at 12 weeks. Such a correlation was not found in the presence of any other comorbid condition. Table 1 outlines these results.
Table 1.
Presence of Diabetes Correlated With Functional Outcome Scores at 12 and 24 Weeks.
| Functional scores | DM | N | Mean | Standard deviation | P-value |
|---|---|---|---|---|---|
| PRWE 12 weeks | No | 17 | 22.09 | 7.48 | .016 |
| Yes | 13 | 30.69 | 10.98 | ||
| PRWE 24 weeks | No | 17 | 15.18 | 6.59 | .042 |
| Yes | 13 | 21.46 | 9.57 | ||
| QuickDASH-9 after 12 weeks | No | 17 | 20.57 | 7.59 | .043 |
| Yes | 13 | 28.81 | 13.48 | ||
| QuickDASH-9 after 24 weeks | No | 17 | 10.68 | 5.80 | .026 |
| Yes | 13 | 17.40 | 9.80 | ||
| SF-8 at 12 weeks | No | 17 | 14.24 | 2.84 | .095 |
| Yes | 13 | 16.31 | 3.73 | ||
| SF-8 at 24 weeks | No | 17 | 9.82 | 2.67 | .025 |
| Yes | 13 | 12.54 | 3.60 |
Note. DM = diabetes mellitus; PRWE = patient-rated wrist evaluation; DASH = Disabilities of the Arm, Shoulder, and Hand; SF = Short Form. Bold values indicate significant results, p<0.05.
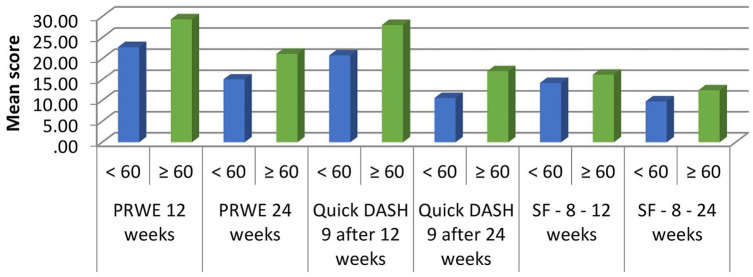
Functional scores at 24-week follow-up were lower for patients younger than 60 years, indicating a better outcome in this group of the population studied (for PRWE: P-value = .048, for QuickDASH-9: P-value = .032, and for SF-8: P-value = .026; Figure 3).
Figure 3.
Comparison of mean functional scores at 12 and 24 weeks with the age group of patients: x-axis—functional scores at 12 and 24 weeks for age groups (less than 60 and 60 or more years) and y-axis—mean functional score as a number.
Note. PRWE = patient-rated wrist evaluation; DASH = Disabilities of the Arm, Shoulder, and Hand; SF = Short Form.
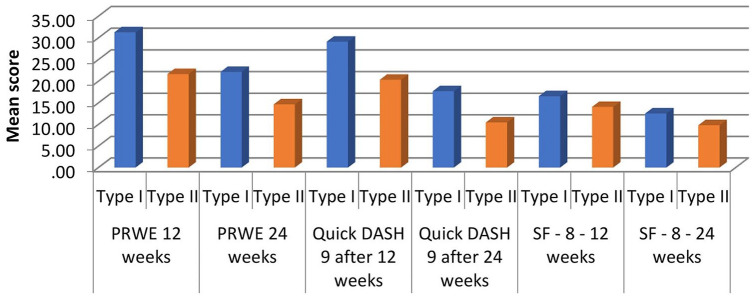
Frykman type II injuries (ie, those with ulnar styloid involvement) had a better outcome than Frykman type I injuries (ie, those without ulnar styloid involvement) in our study as shown in Figure 4.
Figure 4.
Correlation of functional scores with Frykman classification of the fracture at initial presentation: x-axis—functional scores at 12 and 24 weeks for Frykman type I and II and y-axis—mean functional score as a number.
Note. PRWE = patient-rated wrist evaluation; DASH = Disabilities of the Arm, Shoulder, and Hand; SF = Short Form.
Four patients (13.33%) in the study group developed complications. One patient developed complex regional pain syndrome (CRPS), which resolved over time with physiotherapy and supportive treatment. Three patients developed stiffness and were managed with physiotherapy and counseling. A total of 26 patients did not develop any complications and had an uneventful follow-up period.
Spearman correlation was used to analyze the relationship between radiological parameters of alignment of the distal radius and functional scores. We found that there was no significant correlation between prereduction parameters and functional outcome scores at 12 and 24 weeks (P > .05). A significant inverse correlation was found between postreduction radial height and VAS at 12 weeks (P-value = .018), and between postreduction radioulnar inclination and SF-8 score at 24 weeks (P-value = .007). However, the overall functional outcome did not correlate directly with postreduction parameters.
There was a significant inverse correlation between radial height at the time of cast removal and functional outcome scores. Thus, there is a direct correlation between the maintenance of radial height and a better functional outcome (P-value < .05 for all scores except VAS at 24 weeks, for which the P-value was .06). Loss of radial height between reduction and cast removal adversely affected the outcome at 12 and 24 weeks (P-value < .05). Radioulnar inclination at cast removal significantly correlated with SF-8 scores (P-value < .05) and approached a significant relationship with QuickDASH-9 at 24 weeks (P-value = .062). Loss of radioulnar inclination was found to be a significant factor for functional scores PRWE, QuickDASH-9, and SF-8 at 12 and 24 weeks (P-value < .05) but not for VAS at any time. Changes or loss of reduction in ulnar variance and angulation were not correlated with functional outcomes. Tables 2 and 3 show these comparisons.
Table 2.
Correlation Between Functional Scores and Radiological Parameters of Alignment: Prereduction, Postreduction, and After Removal of Cast.
| Spearman rho | Statistical Parameters | PRWE 12 weeks | PRWE 24 weeks | QuickDASH-9 after 12 weeks | QuickDASH-9 after 24 weeks | SF-8 at 12 weeks | SF-8 at 24 weeks | VAS 12 weeks | VAS 24 weeks |
|---|---|---|---|---|---|---|---|---|---|
| Prereduction angulation | Correlation coefficient | −0.002 | −0.050 | −0.063 | −0.123 | −0.239 | −0.036 | −0.102 | 0.114 |
| P-value | .993 | .793 | .743 | .517 | .204 | .850 | .590 | .549 | |
| Prereduction ulnar variance | Correlation coefficient | 0.108 | 0.133 | 0.136 | 0.079 | 0.242 | 0.338 | 0.172 | 0.217 |
| P-value | .570 | .484 | .474 | .678 | .197 | .067 | .364 | .250 | |
| Prereduction radioulnar inclination | Correlation coefficient | −0.071 | −0.023 | −0.119 | −0.106 | −0.135 | −0.354 | −0.091 | 0.011 |
| P-value | .707 | .905 | .530 | .579 | .477 | .055 | .634 | .954 | |
| Postreduction angulation | Correlation coefficient | −0.116 | −0.088 | −0.186 | −0.183 | −0.201 | −0.136 | −0.037 | 0.156 |
| P-value | .540 | .645 | .326 | .332 | .288 | .472 | .844 | .412 | |
| Postreduction ulnar variance | Correlation coefficient | 0.191 | 0.213 | 0.179 | 0.137 | 0.249 | 0.347 | 0.359 | 0.225 |
| P-value | .312 | .258 | .345 | .470 | .185 | .061 | .051 | .231 | |
| Postreduction radioulnar inclination | Correlation coefficient | −0.235 | −0.148 | −0.218 | −0.270 | −0.288 | −0.483 | −0.212 | −0.147 |
| P-value | .211 | .435 | .247 | .149 | .123 | .007 | .261 | .437 | |
| Postreduction radial height | Correlation coefficient | −0.075 | −0.117 | −0.090 | −0.050 | −0.199 | −0.047 | −0.430 | −0.164 |
| P-value | .692 | .538 | .635 | .792 | .291 | .804 | .018 | .386 | |
| Angulation at cast removal | Correlation coefficient | −0.128 | −0.106 | −0.202 | −0.200 | −0.220 | −0.152 | −0.038 | 0.142 |
| P-value | .501 | .579 | .284 | .290 | .243 | .422 | .840 | .455 | |
| Ulnar variance at cast removal | Correlation coefficient | 0.238 | 0.252 | 0.229 | 0.187 | 0.294 | 0.386 | 0.370 | 0.213 |
| P-value | .206 | .179 | .225 | .323 | .115 | .035 | .044 | .258 | |
| Radioulnar inclination at cast removal | Correlation coefficient | −0.305 | −0.227 | −0.279 | −0.345 | −0.366 | −0.532 | −0.231 | −0.150 |
| P-value | .101 | .228 | .135 | .062 | .047 | .002 | .219 | .428 | |
| Radial height at cast removal | Correlation coefficient | −0.402 | −0.442 | −0.401 | −0.391 | −0.533 | −0.397 | −0.590 | −0.347 |
| P-value | .028 | .014 | .028 | .032 | .002 | .030 | .001 | .060 |
Note. PRWE = patient-rated wrist evaluation; DASH = Disabilities of the Arm, Shoulder, and Hand; VAS = Visual Analogue Scale. Bold values indicate significant results, p<0.05.
Table 3.
Correlation Between Change in Radiological Parameters and Functional Scores at 12 and 24 Weeks.
| Spearman rho | Statistical Parameters | Change in angulation | Change in ulnar variance | Loss of radioulnar inclination | Loss of radial height |
|---|---|---|---|---|---|
| VAS 12 weeks | Correlation coefficient | 0.101 | −0.070 | 0.303 | 0.349 |
| P-value | .597 | .712 | .103 | .059 | |
| VAS 24 weeks | Correlation coefficient | 0.207 | 0.097 | 0.155 | 0.369 |
| P-value | .272 | .612 | .413 | .045 | |
| PRWE 12 weeks | Correlation coefficient | 0.190 | −0.187 | 0.569 | 0.691 |
| P-value | .314 | .323 | .001 | .001 | |
| PRWE 24 weeks | Correlation coefficient | 0.249 | −0.140 | 0.574 | 0.711 |
| P-value | .185 | .461 | .001 | .001 | |
| QuickDASH-9 after 12 weeks | Correlation coefficient | 0.200 | −0.179 | 0.366 | 0.719 |
| P-value | .290 | .344 | .047 | .001 | |
| QuickDASH-9 after 24 weeks | Correlation coefficient | 0.220 | −0.179 | 0.507 | 0.753 |
| P-value | .243 | .343 | .004 | .001 | |
| SF-8 at 12 weeks | Correlation coefficient | 0.211 | −0.210 | 0.582 | 0.672 |
| P-value | .263 | .265 | .001 | .001 | |
| SF-8 at 24 weeks | Correlation coefficient | 0.175 | −0.160 | 0.528 | 0.786 |
| P-value | .354 | .397 | .003 | .001 |
Note. VAS = Visual Analogue Scale; PRWE = patient-rated wrist evaluation; DASH = Disabilities of the Arm, Shoulder, and Hand; SF = Short Form.
Discussion
The main objective of the study was to assess the predictors of functional outcomes of extra-articular DRFs treated with closed reduction and cast immobilization. We also measured and analyzed various functional scores and radiological parameters to assess the outcomes.
Thirty patients with extra-articular fractures of the distal end of the radius were managed with closed reduction and cast immobilization. Patients with involvement of the ulnar styloid (17 out of 30, ie, 56.7%) were treated with above elbow slabs and casts, while patients with isolated DRFs (the remaining 43.3%) were treated with below elbow slabs and casts. Li et al 11 found in 2012 that the presence or absence of an ulnar styloid fracture did not affect the outcome. According to them, the anatomical reduction of the fracture became important when there was an ulnar styloid fracture associated with the DRF. This was true for both operative and nonoperative management. 11 In our study, we found that patients who had ulnar styloid fractures had better outcomes (P-values range from .006 to .043). However, this may be a skewed finding due to the nature of treatment such fractures received. All patients with ulnar styloid fractures were treated with above elbow casts and slabs in the initial period. This may indicate that the outcome in this case is attributed to the usage of an above elbow slab or cast, which may offer greater stability at the fracture site, rather than the presence of an ulnar styloid fracture.
We found in our study that patients aged less than 60 years fared better in terms of functional outcome than patients aged more than 60 years, with P-value less than .05 for all scores. However, this is not to say that patients aged 60 and above fared badly. Overall, it was found that most of our patients had moderate to good outcomes, with a mean PRWE score of 17.90 ± 8.48 at 24 weeks. This is similar to results by Ikpeze et al, 12 Amorosa et al, 4 and Lutz et al. 13
There was an almost equal distribution of side affected in the study group, with 53.3% (16 out of 30) of patients having a right-sided fracture and 46.7% having a left-sided fracture. In our study, patients with left-sided fractures were found to have worse outcomes overall. The only relation would be in the case of the dominant hand being involved. We can theorize the reason for this outcome through cultural factors relating to the Indian subcontinent, as most people in India use their left hand for daily ablutions, so any injuries to the left wrist or hand would greatly affect activities of daily living and hence the functional outcome scores. A study by Hosokawa et al 14 found that there was no correlation between hand dominance and the outcome of nonsurgically treated DRFs. Ashe et al, 15 in 2007, found that there may be a correlation between bone response to fractures and dominance of the hand, but further studies are required to evaluate this concept.
It was found that 43.33% of the study group was affected by diabetes mellitus, either as a standalone disease or in conjunction with another disorder. One patient had diabetes with hypothyroidism, while 5 patients had co-existing diabetes and hypertension. Compared with the prevalence of diabetes in India based on the Indian Council of Medical Research India – Diabetes study, a population-based study conducted in 2017, this is a higher prevalence than expected.16,17 One possible explanation would be that individuals with diabetes are more likely to develop osteoporosis as was found by Leidig-Bruckner et al 18 and hence suffer osteoporotic fractures in areas of high risk for the same, such as the wrist and the hip. Therefore, we may deduce that in an analysis of a group of elderly patients with fractured wrists, a larger proportion may be found to be suffering from diabetes. In our study, patients with diabetes had a poorer outcome compared with individuals without diabetes (Spearman correlation: P < .05 for all functional scores used). The mean scores for patients with diabetes were as follows: PRWE at 12 weeks = 30.69 ± 10.98, PRWE at 24 weeks = 21.46 ± 9.57, QuickDASH-9 at 12 weeks = 28.81 ± 13.48, QuickDASH-9 at 24 weeks = 17.40 ± 9.80, SF-8 at 12 weeks = 16.31 ± 3.73, and SF-8 at 24 weeks = 12.54 ± 3.60. This agrees with the findings of Alsubheen et al 19 who found that in their study of 479 patients with and without diabetes, patients with diabetes had poorer outcomes and slower rates of healing and functional improvement compared with individuals without diabetes, based on the PRWE and SF-12 questionnaires (P-value less than .01).
While analyzing the correlation of functional outcome with radiological parameters of alignment at different times, we found that losses in radial height and radioulnar inclination were both directly related to comparatively worse functional outcomes, while angulation and ulnar variance had no significant correlation. The mean loss of radial height in our study was found to be 0.52 ± 0.80 mm, and the correlation was statistically significant for all functional and pain scores with P-value less than .05 for all scores except VAS at 6 weeks. Anzarut et al 20 also found that angulation (volar or dorsal tilt) had no significance in the outcomes of elderly patients with DRFs. 21 However, our findings related to radial height and inclination are in contrast to a study by Ranjeet et al who found no correlation between radiological parameters and functional outcomes of DRFs. Tahiririan et al 22 and Leone et al 23 found that loss in radial height and radial inclination were important predictive factors of instability, but they made no note of the functional outcomes in these patients.
Limitations/Strengths
Our study adds data to research around the factors affecting the outcome of DRFs among the elderly, in the Indian population. There are limited studies on the correlation of comorbidities and other similar patient factors with functional outcomes of such fractures, and we hope to add some insight into these areas with this study. The COVID-19 pandemic going on during the study period reduced our sample size due to various reasons, including loss of follow-up and fewer patients presenting to the outpatient department (OPD). However, the final sample had adequate power for analysis. The relatively small sample size may lead to a limited representation of the study population.
This study did not differentiate between tip and base fractures of the ulnar styloid which could influence the stability of the fracture. The treatment for all styloid fractures was uniform. The degree of glycemic control was also not assessed using HbA1c for the study group. This could have yielded additional data for correlations.
Conclusions
Based on the results of this study, we conclude that conservative treatment with casts has a major role in treating DRFs despite the trend toward operative management. We found significant correlations between the presence of diabetes, the age of the patient, and the change in radial height with the overall functional outcome of patients with DRFs. However, functional outcomes were unrelated to the overall radiological reduction quality, sex, and other factors. We also recommend patients presenting with DRFs be appropriately screened for diabetes in the OPD/emergency setting, which would help in better prognostication. Strict glycemic control should be ensured in such patients.
More studies are required to assess the efficacy and validity of predictive markers of functional outcome. These may help us individualize and streamline treatment for each patient with a DRF according to their needs.
Acknowledgments
We would like to thank Dr Junaid Nagori and Dr Anmol Dua for their role in the emergency management of the patients enrolled in the study. We would also like to thank the Department of Radiology at HIMSR for their support in providing access to the Stradus PACS system.
Footnotes
Author Contributions: Conceptualization: Neel Aggarwal, Arvind Kumar, and Javed Jameel; Methodology: Arvind Kumar, Javed Jameel, and Neel Aggarwal; Software: Neel Aggarwal, Siddhartha Sinha, and Javed Jameel; Validation: Arvind Kumar, Javed Jameel, Sandeep Kumar, and Owais A. Qureshi; Formal analysis: Siddhartha Sinha, Javed Jameel, Arvind Kumar, Javed Jameel, and Neel Aggarwal; Investigation: Neel Aggarwal, Siddhartha Sinha, Arvind Kumar, and Javed Jameel; Resources: Siddhartha Sinha, Arvind Kumar, Javed Jameel, Sandeep Kumar, and Owais A. Qureshi; Data curation: Neel Aggarwal, Siddhartha Sinha, and Arvind Kumar; Writing: Neel Aggarwal, Siddhartha Sinha, Arvind Kumar, and Javed Jameel; Writing—review & editing: Siddhartha Sinha, Sandeep Kumar, and Neel Aggarwal; Preparation, creation, and/or presentation of the published work by those from the original research group, specifically critical review, commentary, or revision—including prepublication or postpublication stages: Siddhartha Sinha, Arvind Kumar, and Javed Jameel; Visualization: Sandeep Kumar and Owais A. Qureshi; Project administration: Siddhartha Sinha, Arvind Kumar, and Javed Jameel; Funding acquisition: Not applicable.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: The authors declare that no infringement was made on the rights of the humans involved in the study. No animals were involved in this study.
Statement of Informed Consent: Informed consent was obtained from all patients who were enrolled in the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Neel Aggarwal  https://orcid.org/0000-0002-6618-9032
https://orcid.org/0000-0002-6618-9032
Siddhartha Sinha  https://orcid.org/0000-0002-3582-5542
https://orcid.org/0000-0002-3582-5542
Arvind Kumar  https://orcid.org/0000-0002-6224-3636
https://orcid.org/0000-0002-6224-3636
References
- 1. Candela V, Di Lucia P, Carnevali C, et al. Epidemiology of distal radius fractures: a detailed survey on a large sample of patients in a suburban area. J Orthop Traumatol. 2022;23(1):43. doi: 10.1186/s10195-022-00663-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Palh H, Muhammad S, Karim K, et al. Operative versus non-operative management of distal radius fractures, in elderly patients: a retrospective study. Int J Curr Res Rev. 2022;14. doi: 10.31782/ijcrr.2022.14915 [DOI] [Google Scholar]
- 3. Hohmann E, Meta M, Navalgund V, et al. The relationship between radiological alignment of united distal radius fractures and functional and patient-perceived outcomes in elderly patients. J Orthop Surg. 2017;25(1):2309499016684976. doi: 10.1177/2309499016684976 [DOI] [PubMed] [Google Scholar]
- 4. Amorosa LF, Vitale MA, Brown S, et al. A functional outcomes survey of elderly patients who sustained distal radius fractures. Hand. 2011;6(3):260-267. doi: 10.1007/s11552-011-9327-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mehta SP, MacDermid JC, Richardson J, et al. A systematic review of the measurement properties of the patient-rated wrist evaluation. J Orthop Sports Phys Ther. 2015;45(4):289-298. doi: 10.2519/jospt.2015.5236 [DOI] [PubMed] [Google Scholar]
- 6. Gabel CP, Yelland M, Melloh M, et al. A modified QuickDASH-9 provides a valid outcome instrument for upper limb function. BMC Musculoskelet Disord. 2009;10:161. doi: 10.1186/1471-2474-10-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mishra PK, Nagar M, Gaur SC, et al. Morphometry of distal end radius in the Indian population: a radiological study. Indian J Orthop. 2016;50(6):610-615. doi: 10.4103/0019-5413.193482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Charnley J. The Closed Treatment of Common Fractures, Centenary ed. Associated East-West Press Pvt. Ltd; 2010. [Google Scholar]
- 9. Logan AJ, Lindau TR. The management of distal ulnar fractures in adults: a review of the literature and recommendations for treatment. Strategies Trauma Limb Reconstr. 2008;3(2):49-56. doi: 10.1007/s11751-008-0040-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim JK, Kim JO, Koh YD. Management of distal ulnar fracture combined with distal radius fracture. J Hand Surg Asian Pac Vol. 2016;21(2):155-160. doi: 10.1142/S2424835516400075 [DOI] [PubMed] [Google Scholar]
- 11. Li S, Chen Y, Lin Z, et al. Effect of associated ulnar styloid fracture on wrist function after distal radius. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012;26(6):666-670. [PubMed] [Google Scholar]
- 12. Ikpeze TC, Smith HC, Lee DJ, et al. Distal radius fracture outcomes and rehabilitation. Geriatr Orthop Surg Rehabil. 2016;7(4):202-205. doi: 10.1177/2151458516669202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lutz K, Yeoh KM, MacDermid JC, et al. Complications associated with operative versus nonsurgical treatment of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 2014;39(7):1280-1286. doi: 10.1016/j.jhsa.2014.04.018 [DOI] [PubMed] [Google Scholar]
- 14. Hosokawa T, Tajika T, Suto M, et al. Relationship between hand dominance and treatment outcomes for distal radius fractures in the elderly in the short-term. J Hand Surg Glob Online. 2020;2(4):212-216. doi: 10.1016/j.jhsg.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ashe MC, Khan KM, Davis JC, et al. Hand dominance and bone response after a distal radial fracture: a peripheral QCT study. J Clin Densitom. 2007;10(1):93-101. doi: 10.1016/j.jocd.2006.09.004 [DOI] [PubMed] [Google Scholar]
- 16. Atre S, Deshmukh S, Kulkarni M. Prevalence of type 2 diabetes mellitus (T2DM) in India: a systematic review (1994-2018). Diabetes Metab Syndr. 2020;14(5):897-906. doi: 10.1016/j.dsx.2020.05.040 [DOI] [PubMed] [Google Scholar]
- 17. Anjana RM, Deepa M, Pradeepa R, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585-596. doi: 10.1016/S2213-8587(17)30174-2 [DOI] [PubMed] [Google Scholar]
- 18. Leidig-Bruckner G, Grobholz S, Bruckner T, et al. Prevalence and determinants of osteoporosis in patients with type 1 and type 2 diabetes mellitus. BMC Endocr Disord. 2014;14:33. doi: 10.1186/1472-6823-14-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alsubheen SA, MacDermid JC, Walton DM, et al. The effect of diabetes on functional outcomes among individuals with distal radial fractures. J Hand Ther. 2019;32(4):476-482. doi: 10.1016/j.jht.2018.02.008 [DOI] [PubMed] [Google Scholar]
- 20. Anzarut A, Johnson JA, Rowe BH, et al. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29(6):1121-1127. doi: 10.1016/j.jhsa.2004.07.002 [DOI] [PubMed] [Google Scholar]
- 21. Ranjeet N, Estrella EP. Distal radius fractures: does a radiologically acceptable reduction really change the result. J Clin Diagn Res. 2012;6(8):1388-1392. doi: 10.7860/JCDR/2012/4567.2366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tahririan MA, Javdan M, Nouraei MH, et al. Evaluation of instability factors in distal radius fractures. J Res Med Sci. 2013;18(10):892-896. [PMC free article] [PubMed] [Google Scholar]
- 23. Leone J, Bhandari M, Adili A, et al. Predictors of early and late instability following conservative treatment of extra-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124(1):38-41. doi: 10.1007/s00402-003-0597-6 [DOI] [PubMed] [Google Scholar]