Abstract
Purpose
The incidence and mortality of hepatocellular carcinoma (HCC) and its underlying etiologies in China are still unclear. Therefore, this study used the Global Burden of Disease (GBD) 2021 to evaluate the incidence and mortality of HCC and its underlying etiologies in China.
Methods
We extracted the incident cases, incidence rate, deaths, and mortality rate of HCC and its underlying etiologies in China in 1990 and 2021 from the GBD database. In addition, we used joinpoint regression analysis to assess the trend of the incidence rate and mortality rate of HCC and its underlying etiologies in China from 1990 to 2021.
Results
The incidence of HCC in China climbed from 96,434.35 in 1990 to 196,636.59 in 2021, while the number of deaths rose from 94,937.12 in 1990 to 172,068.40 in 2021. From 1990 to 2021, the age-standardized incidence rate (ASIR) and age-standardized mortality rate (ASMR) of HCC in China decreased by 0.31 (95% CI: 0.23, 0.39) and 0.79 (95% CI: 0.28, 1.30), respectively. ASIR demonstrated a decreasing trend in HCC caused by different etiologies, such as HCC due to hepatitis B (HCCDHB), HCC due to hepatitis C (HCCDHC), and HCC due to other causes (HCCDOC), but an increasing trend in HCC due to alcohol use (HCCDAU) and HCC due to NASH (HCCDNASH). Between 1990 and 2021, ASMR showed a downward trend in HCCDHB, HCCDHC, and HCCDOC, while the trend in HCCDAU and HCCDNASH was not significant.
Conclusions
In the past 30 years, although the overall incidence rate and mortality of HCC in China have declined, the proportion of HCCDAU and HCCDNASH has increased due to the increasingly serious problems of alcoholism and obesity. Therefore, interventions are needed to address the issues of alcohol consumption and obesity in order to control the incidence of HCCDAU and HCCDNASH.
Keywords: hepatocellular carcinoma, incidence, mortality, disease burden, joinpoint regression, China
Introduction
Hepatocellular carcinoma (HCC) accounted for about 910,000 new cases and 930,000 fatalities globally in 2020, rendering it the sixth most common cancer and the second most common cause of cancer-related deaths worldwide.1,2 The majority of HCC is found in nations with underdeveloped economies, including some in East Asia, North Africa, and West Africa. 3 On the contrary, China, which has the second largest economy in the world, only has 20% of the world’s population but is seen to be a major HCC country due to the reason that cases and deaths there account for almost 50% of the global population. 3 HCC surged from third place in 2018 to second place in 2020 in terms of causes of tumour death, according to reports, even if its frequency in China remained seventh among the most prevalent tumours. 4 Hence, there have been slight changes in the epidemiology of HCC in China.
Hepatitis B virus (HBV), hepatitis C virus (HCV), alcohol abuse (AU), and non-alcoholic steatohepatitis (NASH) are among the known primary etiologies of HCC. Nevertheless, during the past few decades, the proportion of the etiologies mentioned above has shifted. 5 Although viral hepatitis remains a major cause of HCC worldwide, the rising incidence of AU and obesity as a result of economic and cultural changes, as well as dietary habits, has resulted in a considerable increase in the proportion of alcohol and NASH associated HCC. 6 However, it is unclear whether the trend of changes in the previously mentioned etiologies is consistent across China.
Regular evaluation of the epidemiological features of HCC on a global or regional scale can provide a reference for HCC treatment and prevention. We therefore assess the illness burden of HCC and its possible etiologies in China, as well as the evolving trends over the previous 30 years, based on the most recent updated data from the Global Burden of Disease (GBD) 2021. 7
Methods
Data Source
GBD is a vast database compiled by international health research institutions that is used to evaluate and analyze the effects of hazards, illnesses, and injuries on health both nationally and internationally. The incidence case, age-standardized incidence rate (ASIR), mortality, and age-standardized mortality rate (ASMR) of HCC in China were retrieved for each gender (male and female) and age (14 age groups, ranging from under 20 to over 80 years old) between 1990 and 2021. The GBD database categorizes the etiologies of HCC into 5 groups: HCC due to hepatitis B (HCCDHB), HCC due to hepatitis C (HCCDHC), HCC due to AU (HCCDAU), HCC due to NASH (HCCDNASH), and HCC due to other causes (HCCDOC). The above database’s estimated values are all represented as 95% uncertainty intervals (UI). This research report followed the STROBE guidelines. 8
Statistical Analysis
To assess the changes in the incidence and mortality rates of HCC across various genders and etiologies from 1990 to 2021, we used a joinpoint regression analysis. The fundamental idea behind joinpoint regression analysis was to use various connection points to split the study period into distinct periods. 9 Then, using the grid point with the lowest mean square error as the segmentation point, fit and optimize the connection points to assess how a particular disease changed throughout the study period. 9 The prevalence of infectious disorders, chronic diseases, and tumors is mostly studied using jointpoint regression. Because most tumor incidence and mortality rates follow a Poisson distribution, a logarithmic linear model was selected for this investigation.
We uniformly adopt models with 4 connection points (5 line segments) to reduce the possibility of changing trends during the study period and to make table drawing easier. Besides, the majority of the models constructed in this study were optimal when there were 4 connection points. Trends in incidence and death rates were measured using the annual percentage change (APC) and its 95% CI. The average APC (AAPC) and its 95% CI were used to quantify the changing trend in incidence and mortality rates between 1990 and 2021. The 95% CI excluding zero indicates that the results of APC or AAPC were statistically significant. APC or AAPC >0 signified an increase in incidence and death rates for a given period, and vice versa. Joinpoint regression software (version 4.9.1.0) was used to perform the joinpoint analysis.
Results
The Disease Burden of Hepatocellular Carcinoma and Its Etiologies in China
The incidence of HCC and its underlying etiologies in China in 1990 and 2021 are shown in Tables 1 and 2, respectively. The incidence of HCC in China increased from 96,434.35 cases in 1990 to 196,636.59 cases in 2021. From 10.58 per 100,000 people in 1990 to 9.52 per 100,000 people in 2021, the corresponding ASIR declined. Between 1990 and 2021, the number of HCCDHB incidents grew from 63,118.39 to 118,664.63. From 6.58 per 100,000 people in 1990 to 5.73 per 100,000 people in 2021, the corresponding ASIR fell. Between 1990 and 2021, the amount of HCCDHC incidents increased from 14,422.25 to 36,427.20. From 1.94 per 100,000 people in 1990 to 1.78 per 100,000 people in 2021, the associated ASIR fell. Between 1990 and 2021, the number of HCCDAU incidents increased from 7499.99 to 20,463.70. From 0.84 per 100,000 people in 1990 to 0.94 per 100,000 people in 2021, the corresponding ASIR rose. Between 1990 and 2021, the amount of HCCDNASH incident cases increased from 4056.85 to 11,292.71. From 1990 to 2021, the corresponding ASIR grew from 0.48 per 100,000 people to 0.54 per 100,000 people. From 5067.76 incident cases in 1990 to 9235.20 in 2021, the number of HCCDOC incident cases grew. From 0.54 per 100,000 people in 1990 to 0.45 per 100,000 people in 2021, the corresponding ASIR fell.
Table 1.
The Number and Incidence Rate of Hepatocellular Carcinoma and Its Underlying Etiologies in China in 1990.
| Overall | Hepatocellular Carcinoma Due to Hepatitis B | Hepatocellular Carcinoma Due to Hepatitis C | Hepatocellular Carcinoma Due to Alcohol Use | Hepatocellular Carcinoma Due to NASH | Hepatocellular Carcinoma Due to Other Cause | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | |
| Both | 96,434.35 (80,970.60, 113,768.66) | 10.58 (8.94, 12.43) | 63,118.39 (52,017.87, 75,226.51) | 6.58 (5.45, 7.84) | 14,422.25 (11,688.21, 17,539.40) | 1.94 (1.57, 2.32) | 7499.99 (5772.02, 9563.40) | 0.84 (0.66, 1.07) | 4056.85 (3237.49, 4977.60) | 0.48 (0.38, 0.58) | 5067.76 (4016.85, 6304.76) | 0.54 (0.43, 0.66) |
| Femlae | 26,225.22 (20,940.93, 31,755.09) | 6.04 (4.82, 7.28) | 9910.86 (7731.49, 12,322.23) | 2.14 (1.67, 2.66) | 8268.76 (6411.30, 10,161.78) | 2.13 (1.66, 2.61) | 2591.40 (1924.27, 3344.60) | 0.59 (0.43, 0.75) | 1931.27 (1465.97, 2400.29) | 0.45 (0.34, 0.55) | 2474.93 (1859.22, 3162.47) | 0.53 (0.40, 0.67) |
| Male | 70,209.13 (56,752.31, 85,768.18) | 15.06 (12.20, 18.24) | 53,207.53 (42,644.94, 65,059.04) | 11.01 (8.88, 13.40) | 6153.49 (4661.25, 7878.17) | 1.68 (1.31, 2.09) | 4908.59 (3691.89, 6547.27) | 1.12 (0.84, 1.45) | 2125.58 (1631.29, 2729.53) | 0.50 (0.39, 0.64) | 2592.83 (2001.92, 3354.05) | 0.54 (0.42, 0.69) |
UI: uncertainty interval; NASH: Non-alcoholic steatohepatitis; ASIR: age-standardized incidence rate.
Table 2.
The Number and Incidence Rate of Hepatocellular Carcinoma and Its Underlying Etiologies in China in 2021.
| Overall | Hepatocellular Carcinoma Due to Hepatitis B | Hepatocellular Carcinoma Due to Hepatitis C | Hepatocellular Carcinoma Due to Alcohol Use | Hepatocellular Carcinoma Due to NASH | Hepatocellular Carcinoma Due to Other Cause | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | Incidence Cases (95% UI) | ASIR Per 100,000 (95% UI) | |
| Both | 196,636.59 (158,273.06, 243,557.68) | 9.52 (7.72, 11.78) | 118,664.63 (92,279.81, 153,555.83) | 5.73 (4.48, 7.38) | 36,427.20 (28,403.62, 44,839.52) | 1.78 (1.41, 2.18) | 20,463.70 (15,239.13, 27,295.73) | 0.94 (0.71, 1.25) | 11,292.71 (8663.08, 14,313.98) | 0.54 (0.42, 0.68) | 9235.20 (7034.47, 11,874.65) | 0.45 (0.34, 0.57) |
| Femlae | 52,848.43 (41,045.47, 67,025.70) | 4.89 (3.82, 6.18) | 16,822.07 (12,386.23, 22,196.51) | 1.56 (1.16, 2.07) | 19,924.28 (15,197.93, 25,487.43) | 1.81 (1.39, 2.31) | 6579.11 (4820.34, 8696.52) | 0.58 (0.43, 0.77) | 5133.09 (3874.44, 6818.26) | 0.47 (0.35, 0.62) | 4153.79 (3057.60, 5491.58) | 0.39 (0.29, 0.51) |
| Male | 143,788.16 (108,926.76, 193,830.93) | 14.34 (10.93, 19.18) | 101,842.56 (76,298.12, 137,860.95) | 10.04 (7.60, 13.49) | 16,502.92 (12,102.56, 22,376.81) | 1.75 (1.29, 2.33) | 13,884.60 (9568.75, 19,670.88) | 1.33 (0.93, 1.85) | 6159.62 (4347.41, 8447.05) | 0.63 (0.45, 0.84) | 5081.41 (3624.03, ) 7319.05 | 0.51 (0.36, 0.72) |
UI: uncertainty interval; NASH: Non-alcoholic steatohepatitis; ASIR: age-standardized incidence rate.
The mortality of HCC and its underlying etiologies in China in 1990 and 2021 were shown in Tables 3 and 4, respectively. China had 94,937.12 HCC deaths in 1990; by 2021, that figure had risen to 172,068.40. From 10.75 per 100,000 people in 1990 to 8.35 per 100,000 people in 2021, the corresponding ASMR declined. Between 1990 and 2021, the number of deaths attributed to HCCDHB increased from 61,414.52 to 100,193.63. From 6.53 per 100,000 people in 1990 to 4.83 per 100,000 people in 2021, the corresponding ASMR was reduced. Between 1990 and 2021, the amount of deaths attributed to HCCDHC rose from 15,268.45 to 34,899.08. From 2.16 per 100,000 people in 1990 to 1.74 per 100,000 people in 2021, the corresponding ASMR decreased. Between 1990 and 2021, the number of deaths in HCCDAU increased from 7574.50 to 18,371.09. From 1990 to 2021, the corresponding ASMR fell from 0.87 per 100,000 people to 0.85 per 100,000 people. Between 1990 and 2021, the number of deaths from HCCDNASH grew from 4128.19 to 10,409.34. In 1990, the corresponding ASMR was 0.50 per 100,000 people; by 2021, it had climbed to 0.51 per 100,000 people. From 4981.34 cases in 1990 to 8033.49 cases in 2021, the incidence of HCCDOC rose. From 0.54 per 100,000 persons in 1990 to 0.39 per 100,000 people in 2021, the equivalent ASMR fell.
Table 3.
The Death Cases and Mortality Rate of Hepatocellular Carcinoma and Its Underlying Etiologies in China in 1990.
| Overall | Hepatocellular Carcinoma Due to Hepatitis B | Hepatocellular Carcinoma Due to Hepatitis C | Hepatocellular Carcinoma Due to Alcohol Use | Hepatocellular Carcinoma Due to NASH | Hepatocellular Carcinoma Due to Other Cause | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Death Cases (95% UI) | ASMR Per 100,000 (95% UI) | Death Cases (95% UI) | ASMR Per 100,000 (95% UI) | Death Cases (95% UI) | ASMR Per 100,000 (95% UI) | Death Cases (95% UI) | ASMR Per 100,000 (95% UI) | Death Cases (95% UI) | ASMR Per 100,000 (95% UI) | Death Cases (95% UI) | ASMR Per 100,000 (95% UI) | |
| Both | 94,937.12 (79,884.26, 111,526.73) | 10.75 (9.12. 12.61) | 61,414.52 (50,743.20, 73,121.84) | 6.53 (5.42, 7.76) | 15,268.45 (12,408.43, 18,500.42) | 2.16 (1.77, 2.60) | 7574.50 (5858.01, 9677.17) | 0.87 (0.69, 1.10) | 4128.19 (3292.97, 5067.91) | 0.50 (0.40, 0.61) | 4981.34 (3957.32, 6185.17) | 0.54 (0.43, 0.67) |
| Femlae | 26,633.11 (21,349.83, 32,258.36) | 6.33 (5.08, 7.64) | 9890.15 (7689.56, 12,250.70) | 2.18 (1.70, 2.70) | 8905.90 (6905.99, 10,947.11) | 2.38 (1.87, 2.93) | 2659.16 (1975.72, 3432.94) | 0.61 (0.46, 0.78) | 1995.03 (1515.24, 2481.62) | 0.48 (0.36, 0.59) | 2461.60 (1848.28, 3118.74) | 0.54 (0.41, 0.67) |
| Male | 68,304.01 (55,234.66, 83,128.05) | 15.19 (12.32, 18.36) | 51,524.37 (41,304.99, 62,899.38) | 10.96 (8.85, 13.33) | 6362.55 (4834.83, 8108.07) | 1.85 (1.46, 2.28) | 4915.34 (3680.40, 3680.40) | 1.15 (0.87, 1.49) | 2133.16 (1636.88, 2744.31) | 0.53 (0.41, 0.67) | 2519.75 (1949.35, 3259.83) | 0.54 (0.42, 0.69) |
UI: uncertainty interval; NASH: Non-alcoholic steatohepatitis; ASMR: age-standardized mortality rate.
Table 4.
The Death Cases and Mortality Rate of Hepatocellular Carcinoma and Its Underlying Etiologies in China in 2021.
| Overall | Hepatocellular Carcinoma Due to Hepatitis B | Hepatocellular Carcinoma Due to Hepatitis C | Hepatocellular Carcinoma Due to Alcohol Use | Hepatocellular Carcinoma Due to NASH | Hepatocellular Carcinoma Due to Other Cause | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality Number (95% UI) | ASMR per 100,000 (95% UI) | Mortality Number (95% UI) | ASMR Per 100,000 (95% UI) | Mortality Number (95% UI) | ASMR Per 100,000 (95% UI) | Mortality Number (95% UI) | ASMR Per 100,000 (95% UI) | Mortality Number (95% UI) | ASMR Per 100,000 (95% UI) | Mortality Number (95% UI) | ASMR Per 100,000 (95% UI) | |
| Both | 172,068.40 (139,621.29, 212,495.94) | 8.35 (6.80, 10.29) | 100,193.63 (77,721.19, 129,138.37) | 4.83 (3.76, 6.19) | 34,899.08 (27,412.63, 42,964.74) | 1.74 (1.38, 2.12) | 18,371.09 (13,652.97, 24,251.63) | 0.85 (0.64, 1.12) | 10,409.34 (8036.34. 13,179.82) | 0.51 (0.39, 0.64) | 8033.49 (13,652.97, 24,251.63) | 0.39 (0.30, 0.49) |
| Femlae | 49,605.44 (38,616.99, 62,668.34) | 4.57 (2.57, 5.76) | 15,128.73 (11,158.75, 19,855.58) | 1.40 (1.04, 1.84) | 19,635.40 (15,057.49, 24,848.52) | 1.80 (1.39, 2.28) | 6118.90 (4471.69, 8144.01) | 0.54 (0.40, 0.73) | 4894.87 (3668.73, 6557.52) | 0.45 (0.34, 0.60) | 3735.44 (2761.27, 4949.11) | 0.35 (0.26, 0.46) |
| Male | 122,462.95 (93,115.19, 164,815.76) | 12.40 (9.46, 16.55) | 85,064.90 (63,905.26, 114,759.77) | 8.48 (6.42, 11.29) | 15,263.68 (11,223.29, 20,714.20) | 1.69 (1.27, 2.26) | 12,198.19 (8488.63, 17,015.00) | 1.19 (0.85, 1.62) | 5514.47 (3894.58, 7542.17) | 0.58 (0.41, 0.78) | 4298.05 (3031.95, 6204.21) | 0.43 (0.31, 0.62) |
UI: uncertainty interval; NASH: Non-alcoholic steatohepatitis; ASMR: age-standardized mortality rate.
In 2021, the incident cases and ASIR of HCC in males were higher than those in females, and the same was true for deaths and ASMR. For HCCDHC, the number of incident cases, deaths, ASIR, and ASMR of females was higher than that of males. For HCC caused by other etiologies, males have higher incident cases, deaths, ASIR, and ASMR than females.
Trend Analysis of Hepatocellular Carcinoma and Its Etiologies in China from 1990 to 2021
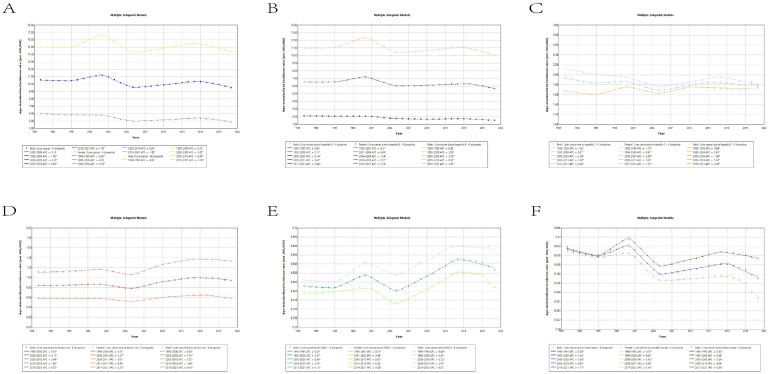
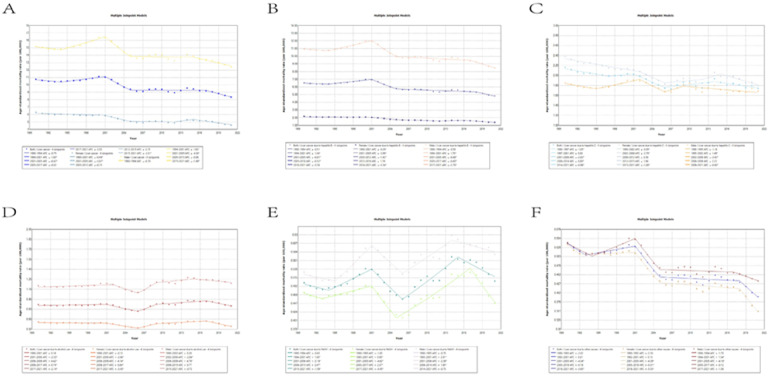
Table 5, Table 6, Figures 1, and 2 exhibited the jointpoint regression analysis of ASIR and ASMR for HCC and its etiology in China from 1990 to 2021. The ASIR and ASMR of HCC in China decreased by 0.31 (95% CI: 0.23, 0.39) and 0.79 (95% CI: 0.28, 1.30) between 1990 and 2021, respectively. Between 2000 and 2005, ASIR decreased at the highest rate (APC: −3.39, 95% CI: −3.60, −3.19), whereas ASMR decreased at the highest rate (APC: −4.42, 95% CI: −6.34, −2.45) between 2001 and 2005. Nonetheless, the ASIR of HCC demonstrated an increasing tendency from 2005 to 2016 (APC: 0.83, 95% CI: 0.78, 0.89). In both ASIR and ASMR, women’s HCC declined more between 1990 and 2021 than did men’s. It is noteworthy to notice that between 2000 and 2005, the ASIR of both male and female HCC saw the most significant fall. The greatest decrease in ASMR was seen in both male and female HCC from 2001 and 2005.
Table 5.
Joinpoint Regression Analysis of Age-Standardized Incidence Rate of Hepatocellular Carcinoma and Its Underlying Etiologies in China From 1990 to 2021.
| Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | 1990-2021 AAPC (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Genders | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | ||
| Hepatocellular carcinoma | Both | 1990-1995 | −0.19 (−0.43, 0.05) | 1995-2000 | 1.60* (1.35, 1.86) | 2000-2005 | −3.39 (−3.60, −3.19) | 2005-2016 | 0.83 (0.78, 0.89) | 2016-2021 | −1.70 (−1.99, −1.40) | −0.31 (−0.39, −0.23) |
| Female | 1990-1995 | −0.63 (−0.93, −0.34) | 1995-2000 | −0.03 (−0.38, 0.32) | 2000-2005 | −3.10 (−3.37, −2.82) | 2005-2016 | 0.83 (0.76, 0.90) | 2016-2021 | −1.95 (−2.28, 1.61) | −0.64 (−0.73, −0.54) | |
| Male | 1990-1995 | −0.02 (−0.22, 0.18) | 1995-2000 | 2.32 (2.09, 2.54) | 2000-2005 | −3.27 (−3.45, −3.09) | 2005-2015 | 0.90 (0.85, 0.95) | 2015-2021 | −1.14 (−1.34, −0.94) | −0.10 (−0.17, −0.04) | |
| Hepatocellular carcinoma due to hepatitis B | Both | 1990-1995 | −0.03 (−0.47, 0.41) | 1995-2000 | 2.11 (1.60, 2.62) | 2000-2005 | −3.74 (−4.15, −3.32) | 2005-2017 | 0.43 (0.33, 0.54) | 2017-2021 | −2.48 (−3.40, 1.56) | −0.44 (−0.61, −0.27) |
| Female | 1990-2001 | −0.31 (−0.44, −0.18) | 2001-2004 | −4.09 (−5.48, −2.69) | 2004-2009 | −1.24 (−1.72, −0.75) | 2009-2016 | 0.51 (0.21, 0.81) | 2016-2021 | −2.26 (−2.77, −1.75) | −0.97 (−1.15, −0.78) | |
| Male | 1990-1995 | 0.08 (−0.24, 0.40) | 1995-2000 | 2.50 (2.14, 2.86) | 2000-2005 | −3.50 (−3.87, −3.31) | 2005-2016 | 0.62 (0.54, 0.71) | 2016-2021 | −1.82 (−2.26, −1.38) | −0.26 (−0.37, −0.15) | |
| Hepatocellular carcinoma due to hepatitis C | Both | 1990-1995 | −1.02 (−1.43, −0.61) | 1995-2000 | 0.37 (−0.15, 0.90) | 2000-2005 | −2.09 (−2.56, −1.62) | 2005-2013 | 1.20 (1.01, 1.39) | 2013-2021 | −0.42 (−0.63, −0.22) | −0.25* (−0.39, −0.11) |
| Female | 1990-1994 | −1.15 (−1.52, −0.77) | 1994-2000 | −0.61 (−0.84, −0.38) | 2000-2005 | −2.08 (−2.35, −1.81) | 2005-2015 | 1.08 (1.01, 1.16) | 2015-2021 | −1.25 (−1.46, −1.03) | −0.50 (−0.59, −0.41) | |
| Male | 1990-1995 | −0.89 (−1.49, −0.29) | 1995-2000 | 2.00 (1.17, 2.84) | 2000-2005 | −1.69 (−2.40, −0.98) | 2005-2010 | 1.60 (0.96, 2.25) | 2010-2021 | −0.20 (−0.39, −0.00) | 0.09 (−0.13, 0.31) | |
| Hepatocellular carcinoma due to alcohol use | Both | 1990-2000 | 0.35 (0.21, 0.48) | 2000-2005 | −2.15 (−2.64, −1.66) | 2005-2010 | 3.44 (2.98, 3.01) | 2010-2015 | 1.80 (1.33, 2.27) | 2015-2021 | −0.87 (−1.18, −0.55) | 0.43 (0.28, 0.57) |
| Female | 1990-2000 | −0.01 (−0.16, 0.14) | 2000-2005 | −2.27 (−2.76, −1.78) | 2005-2011 | 3.01 (2.65, 3.37) | 2011-2017 | 0.90 (0.53, 1.27) | 2017-2021 | −2.72 (−3.38, −2.05) | 0.02 (−0.13, 0.17) | |
| Male | 1990-2000 | 0.56 (0.42, 0.70) | 2000-2005 | −1.91 (−2.41, −1.41) | 2005-2010 | 3.72 (3.25, 4.19) | 2010-2015 | 1.66 (1.17, 2.15) | 2015-2021 | −0.44 (−0.80, −0.09) | 0.64 (0.49, 0.79) | |
| Hepatocellular carcinoma due to NASH | Both | 1990-1995 | −0.29 (−0.65, 0.07) | 1995-2000 | 2.37 (1.90, 2.85) | 2000-2005 | −2.94 (−3.37, −2.51) | 2005-2015 | 2.74 (2.60, 2.87) | 2015-2021 | −1.10 (−1.40, −0.80) | 0.51 (0.38, 0.64) |
| Female | 1990-2021 | 0.53 (0.34, 0.72) | 2001-2005 | −3.94 (−5.04, −2.82) | 2005-2015 | 3.02 (2.79, 3.24) | 2015-2019 | −0.58 (−1.99, 0.86) | 2019-2021 | −5.60 (−9.13, −1.94) | 0.18 (−0.15, 0.51) | |
| Male | 1990-1995 | −0.48 (−0.77, −0.19) | 1995-2000 | 3.41 (3.01, 3.82) | 2000-2005 | −2.12 (−2.48, −1.75) | 2005-2014 | 2.41 (2.28, 2.54) | 2014-2021 | −0.21 (−0.43, 0.00) | 0.76 (0.66, 0.87) | |
| Hepatocellular carcinoma due to other cause | Both | 1990-1995 | −0.80 (−1.06, −0.55) | 1995-2000 | 1.34 (1.02, 1.65) | 2000-2005 | −3.43 (−3.71, −3.15) | 2005-2016 | 0.65 (0.57, 0.72) | 2016-2021 | −1.71 (−1.99, −1.42) | −0.53 (−0.62, −0.44) |
| Female | 1990-1995 | −0.70 (−0.99, −0.41) | 1995-2000 | 0.62 (0.27, 0.98) | 2000-2005 | −3.42 (−3.73, −3.11) | 2005-2017 | 0.28 (0.21, 0.35) | 2017-2021 | −3.44 (−3.90, −2.98) | −0.91 (−1.02, −0.81) | |
| Male | 1990-1995 | −0.88 (−1.05, −0.71) | 1995-2000 | 2.08 (1.87, 2.30) | 2000-2005 | −3.24 (−3.44, −3.05) | 2005-2015 | 0.88 (0.81, 0.94) | 2015-2021 | −0.56 (−0.73, −0.40) | −0.17 (−0.23, −0.11) | |
APC: annual percentage change; AAPC: average annual percentage change; NASH: Non-alcoholic steatohepatitis.
Table 6.
Joinpoint Regression Analysis of Age-Standardized Mortality Rate of Hepatocellular Carcinoma and Its Underlying Etiologies in China From 1990 to 2021.
| Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | 1990-2021 AAPC (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Genders | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | ||
| Hepatocellular carcinoma | Both | 1990-1994 | −0.75 (−2.64, 1.17) | 1994-2001 | 1.00 (0.17, 1.83) | 2001-2005 | −4.42 (−6.34, −2.45) | 2005-2017 | −0.02 (−0.35, 0.31) | 2017-2021 | −2.52 (−5.08, 0.10) | −0.79 (−1.30, −0.28) |
| Female | 1990-2001 | −0.44 (−0.74, −0.14) | 2001-2005 | −3.67 (−5.13, −2.18) | 2005-2012 | −0.15 (−0.76, 0.47) | 2012-2015 | 2.15 (−1.54, 5.97) | 2015-2021 | −2.31 (−3.24, −1.38) | −0.92 (−1.36, −0.47) | |
| Male | 1990-1994 | −0.70 (−2.66, 1.29) | 1994-2001 | 1.63 (0.77, 2.49) | 2001-2005 | −4.30 (−6.26, −2.29) | 2005-2015 | −0.06 (−0.47, 0.35) | 2015-2021 | −1.49 (−2.88, −0.09) | −0.60 (−1.08, −0.12) | |
| Hepatocellular carcinoma due to hepatitis B | Both | 1990-1994 | −0.51 (−2.18, 1.19) | 1994-2001 | 1.34 (0.61, 2.07) | 2001-2005 | −4.81 (−6.62, −2.97) | 2005-2018 | −0.52 (−0.80, −0.25) | 2018-2021 | −3.56 (−7.35, 0.38) | −0.97 (−1.47, −0.46) |
| Female | 1990-2001 | −0.29 (−0.54, −0.05) | 2001-2005 | −3.99 (−5.39, −2.56) | 2005-2012 | −1.42 (−1.94, −0.89) | 2012-2016 | 1.19 (−0.55, 2.97) | 2016-2021 | −3.34 (−4.37, −2.29) | −1.34 (−1.68, −0.99) | |
| Male | 1990-1994 | −0.50 (−2.25, 1.28)_ | 1994-2001 | 1.70 (0.95, 2.44) | 2001-2005 | −4.68 (−6.50, −2.83) | 2005-2017 | −0.40 (−0.69, −0.10) | 2017-2021 | −2.70 (−5.16, −0.19) | −0.81 (−1.28, −0.33) | |
| Hepatocellular carcinoma due to hepatitis C | Both | 1990-1997 | −1.05 (−1.93, −0.16) | 1997-2001 | 0.63 (−2.51, 3.87) | 2001-2006 | −2.83 (−4.51, −1.13) | 2006-2014 | 0.80 (0.00, 1.60) | 2014-2021 | −0.98 (−1.92, −0.04) | −0.64 (−1.20, −0.07) |
| Female | 1990-2002 | −0.99 (−1.28, −0.69) | 2002-2006 | −2.79 (−4.57, −0.97) | 2006-2012 | 0.56 (−0.47, 1.60) | 2012-2015 | 1.94 (−2.55, 6.62) | 2015-2021 | −1.88 (−2.89, −0.86) | −0.82 (−1.36, −0.28) | |
| Male | 1990-1995 | −1.18 (−2.81, 0.48) | 1995-2002 | 1.49 (0.23, 2.77) | 2002-2006 | −3.43 (−6.29, −0.49) | 2006-2009 | 2.22 (−4.45, 9.36) | 2009-2021 | −0.60 (−1.08, −0.13) | −0.33 (−1.14, 0.49) | |
| Hepatocellular carcinoma due to alcohol use | Both | 1990-2001 | 0.18 (−0.12, 0.49) | 2001-2006 | −2.53 (−3.77, −1.27) | 2006-2009 | 4.42 (0.41, 8.60) | 2009-2017 | 0.74 (0.20, 1.28) | 2017-2021 | −2.14 (−3.77, −0.47) | −0.02 (−0.50, 0.46) |
| Female | 1990-2001 | −0.12 (−0.41, 0.17) | 2001-2006 | −2.66 (−3.77, −1.54) | 2006-2009 | 4.14 (0.18, 8.26) | 2009-2017 | 0.84 (0.32, 1.37) | 2017-2021 | −3.43 (−5.02, −1.81) | −0.32 (−0.78, 0.15) | |
| Male | 1990-2002 | 0.28 (−0.02, 0.59) | 2002-2006 | −2.84 (−4.98, −0.66) | 2006-2009 | 4.78 (0.32, 9.43) | 2009-2015 | 0.77 (−0.21, 1.76) | 2015-2021 | −0.72 (−1.73, 0.29) | 0.20 (−0.35, 0.75) | |
| Hepatocellular carcinoma due to NASH | Both | 1990-1994 | −0.83 (−2.71, 1.08) | 1994-2001 | 1.60 (0.64, 2.57) | 2001-2006 | −3.18 (−4.85, ) | 2006-2015 | 2.47 (1.84, 3.11) | 2015-2021 | −1.59 (−2.73, −0.44) | 0.13 (−0.36, 0.61) |
| Female | 1990-1993 | −1.00 (−4.09, 2.19) | 1993-2001 | 0.90 (0.13, 1.68) | 2001-2005 | −4.62 (−7.01, −2.17) | 2005-2017 | 2.37 (1.98, 2.75) | 2017-2021 | −4.45 (−6.71, −2.15) | −0.16 (−0.71, 0.40) | |
| Male | 1990-1995 | −0.70 (−1.96, 0.58) | 1995-2001 | 2.91 (1.65, 4.19) | 2001-2006 | −2.59 (−4.22, −0.92) | 2006-2014 | 1.95 (1.25, 2.65) | 2014-2021 | −0.73 (−1.64, 0.19) | 0.35 (−0.11, 0.82) | |
| Hepatocellular carcinoma due to other cause | Both | 1990-1993 | −2.02 (−4.86, 0.89) | 1993-2001 | 0.61 (−0.05, 1.28) | 2001-2005 | −4.34 (−6.51, −2.13) | 2005-2018 | −0.18 (−0.48, 0.11) | 2018-2021 | −3.65 (−6.80, −0.38) | −1.05 (−1.56, −0.53) |
| Female | 1990-1992 | −2.56 (−8.00, 3.20) | 1992-2001 | 0.13 (−0.37, 0.63) | 2001-2005 | −4.39 (−6.43, −2.30) | 2005-1018 | −0.31 (−0.58, −0.03) | 2018-2021 | −5.53 (−8.53, −2.42) | −1.38 (−1.92, −0.83) | |
| Male | 1990-1994 | −1.70 (−3.46, 0.09) | 1994-2001 | 1.34 (0.48, 2.21) | 2001-2005 | −4.18 (−6.34, −1.96) | 2005-2017 | −0.12 (−0.47, 0.23) | 2017-2021 | −1.36 (−3.79, 1.14) | −0.69 (−1.20, −0.18) | |
APC: annual percentage change; AAPC: average annual percentage change; NASH: Non-alcoholic steatohepatitis.
Figure 1.
The trend of age-standardized incidence rate of hepatocellular carcinoma and its underlying etiologies in China from 1990 to 2021. (A) Hepatocellular carcinoma; (B) Hepatocellular carcinoma due to hepatitis B; (C) Hepatocellular carcinoma due to hepatitis C; (D) Hepatocellular carcinoma due to alcohol use; (E) Hepatocellular carcinoma due to NASH; (F) Hepatocellular carcinoma due to other cause.
Figure 2.
The trend of age-standardized mortality rate of hepatocellular carcinoma and its underlying etiologies in China from 1990 to 2021. (A) Hepatocellular carcinoma; (B) Hepatocellular carcinoma due to hepatitis B; (C) Hepatocellular carcinoma due to hepatitis C; (D) Hepatocellular carcinoma due to alcohol use; (E) Hepatocellular carcinoma due to NASH; (F) Hepatocellular carcinoma due to other cause.
Between 1990 and 2021, ASIR demonstrated a decrease in HCC caused by various etiologies, such as HCCDHB, HCCDHC, and HCCDOC, while growing in HCCDAU and HCCDNASH. Although the ASIR of HCCDAU increased from 1990 to 2021 (AAPC: 0.43, 95% CI: 0.28, 0.57), this trend was more pronounced in males (AAPC: 0.64, 95% CI: 0.49, 0.79) than in females (AAPC: 0.02, 95% CI: −0.13, 0.17). This gender difference in trend was also present in HCCDNASH’s ASIR. Meanwhile, while the ASIR of HCCDHC decreased between 1990 and 2021, this development was primarily driven by women. Between 1990 and 2021, the ASIR of HCCDHB in both males and females decreased, with females showing the most significant decline between 2001 and 2004 (APC: −4.09, 95% CI: −5.48, −2.69), and males showing the most significant decline between 2000 and 2005 (APC: −3.50, 95% CI: −3.87, −3.31). The ASIR of HCCDOC in both females and males showed a downward trend between 1990 and 2021, with females showing the most significant decrease in ASIR between 2017 and 2021 (APC: −3.44, 95% CI: −3.90, −2.98), and males showing the most significant decrease in ASIR between 2000 and 2005 (APC: −3.24, 95% CI: −3.44, −3.05).
Between 1990 and 2021, ASMR demonstrated a declining trend in HCC due to various etiologies, including HCCDHB, HCCDHC, and HCCDOC, but changes in HCCDAU and HCCDNASH were not significant. Between 1990 and 2021, there was no significant trend in ASMR changes in HCCDAU and HCCDNASH for either men or women. Although the ASMR of HCCDHC decreased between 1990 and 2021, this reduction was primarily driven by women. Between 1990 and 2021, the ASMR of HCCDHB in both females and males decreased, with the largest significant drop found in females and males between 2001 and 2005 (APC: −3.99, 95% CI: −5.39, −2.56) (APC: −4.68, 95% CI: −6.50, −2.83). Between 1990 and 2021, the ASMR of HCCDOC decreased in both females and males, with females showing the most significant decline between 2018 and 2021 (APC: −5.53, 95% CI: −8.53, −2.42) and males showing the most significant decline between 2001 and 2005 (APC: −4.18, 95% CI: −6.34, −1.96).
Discussion
This study employed research data from GBD 2021 to assess the current state and long-term trends in the incidence and mortality of HCC and its causes in China. This study found that the overall incidence rate and mortality from HCC decreased between 1990 and 2021. HCCDHB, HCCDHC, and HCCDOC incidence rates fell between 1990 and 2021, whereas HCCDAU and HCCDNASH rates increased. HCCDHB, HCCDHC, and HCCDOC showed a downward trend between 1990 and 2021, but the trends of HCCDAU and HCCDNASH were not significant during this period.
The prevalence and control of HBV infection in China is a sophisticated but pressing public health concern that must be addressed. In 1992, the Chinese health department performed the first national hepatitis B study to determine the prevalence of hepatitis throughout the country. The findings revealed that the positive rate of hepatitis B surface antigen in China was around 9.75%, indicating that over 120 million persons nationwide were infected with HBV. 10 As a result, China is classified as high prevalence location for hepatitis B. Then, China formally introduced the hepatitis B vaccine into the management of planned immunization. Ten years later, the Chinese government launched free hepatitis B vaccine for infants countrywide, significantly increasing the hepatitis B immunization rate for newborns. By 2015, China had achieved a 95% vaccination rate for infants with the hepatitis B vaccine, indicating considerable progress in hepatitis B prevention. 11 Hepatitis B immunization can considerably reduce the risk of HCC; this advantage can be seen within a relatively short period. In Taiwan, the incidence of HCC in children and adolescents has decreased dramatically in the 10 years since the newborn vaccination program began. 12 At the same time, a recent 30-year neonatal research in Qidong, China, found that among vaccinated individuals, the incidence of HCC fell by 84%, indicating a considerable preventive effect since early childhood. 13 In this study, the incidence rate of HCCDHB fell dramatically after 1990, which is broadly comparable with China’s hepatitis B immunization campaign that began in the 1990s.
Although only 1.6% of the Chinese population is infected with HCV, given the country’s population of 1.4 billion, this equates to around 22.4 million people. Although HCV can also cause HCC, unlike HBV, it does not integrate into the genome and instead causes liver damage, fibrosis, and cirrhosis through chronic inflammation, eventually leading to HCC. 14 HCV encoded proteins, including the core protein NS3 and NS5A, induce cell transformation and cancer growth by infecting host cells via signalling pathways. 15 According to our findings, the incidence of HCCDHC decreased in China between 1990 and 2021. Possible explanations are as follows: To begin, the government promotes citizen health awareness, such as avoiding the use of shared syringes and unsterilized tattoo and ear piercing equipment, among other things. 16 Second, since 1992, China has tested all blood donors for HCV to ensure that all blood products are thoroughly screened prior to infusion, considerably lowering the danger of HCV transmission through the blood. 17 Furthermore, while China has not approved the hepatitis C vaccine for clinical use, the use of direct-acting antiviral drugs (DAAs) such as sofosbuvir, dacatavir, and remdesivir allows clinicians to achieve a cure rate of up to 90%–99% by combining the patient’s viral genotype with specific circumstances. 18 However, the drop in the incidence rate of HCCDHC appears to be limited to women, while the incidence rate of men has remained relatively stable over the last 30 years. The causes are as follows: First, the number of cases of HCCDHC goes down because IL-6 stops Kupffer cells from responding to estrogen.19,20 Second, females have a better cell-mediated immune response and a higher clearance rate after HCV infection compared to male users. 21
The changing tendencies of HCCDAU and HCCDNASH are rarely discussed in the literature. In general, hepatitis B and C account for the majority of HCC etiologies, while alcoholism and NASH account for a small proportion. However, a recent study found that since 2010, HCCDAU and HCCDNASH have been rising. 22 China’s alcohol use has increased over the last 30 years, although the drinking rate differs by province. 23 This is strongly tied to the quick development of the economy, the rise in people’s living standards, and the acceleration of urbanization. Alcohol consumption has increased, particularly in metropolitan areas, pubs, and banquet settings. Second, as a result of economic globalization, young people are developing a preference for Western style alcoholic beverages such as wine and beer, resulting in a rapid growth in alcohol consumption among this demographic.24,25 However, because this study focuses primarily on the changes in the incidence and death trends of HCC and its causes in China from 1990 to 2021, it does not address the incidence and mortality trends of HCCDAU among young people in China during the last few decades. As a result, additional research is required in the future to corroborate this. In this study, the incidence of HCCDAU in men has increased over the last 30 years, whereas the trend in women is not significant. The explanation for this is that, while females have lower activity of alcohol dehydrogenase than males, they have a higher blood alcohol concentration, rendering them more susceptible to severe acute liver injury. 26 However, because males consume more alcohol than women, their risk of HCCDAU has increased with time. HCCDNASH is noted for having the fastest global growth between 2010 and 2019. 6 In this study, HCCDNASH also had the quickest growth rate among HCC of various etiologies. This suggests that China’s dietary pattern is becoming more global. Globalization has led to a shift in Chinese diets toward high-calorie, high-fat, and high-sugar foods. Furthermore, a lack of physical activity has increased obesity and associated metabolic illnesses, increasing the risk of HCCDNASH. However, the incidence rate of men with HCCDNASH increased, but the incidence rate of women did not change much. One probable explanation is that men and women have different fat levels. Male fat is primarily found in the abdomen, whereas females store fat beneath the skin. 27 Furthermore, abdominal fat appears to be more closely associated with NASH. 28
However, this study does have certain drawbacks. To begin, while the GBD database provided overall data on HCC throughout China, it lacked particular data for individual provinces, cities, and rural areas. It is well known that the incidence and mortality rates of HCC vary by region in China. As a result, more precise data is required to assess the incidence and mortality of HCC in various regions of China. Second, although GBD data can provide valuable insights and facilitate large-scale analysis, its potential issues, such as ecological fallacies, must be acknowledged. Third, the causes of HCC identified by GBD were classified into 5 major categories. Aside from HCCDHB, HCCDHC, HCCDAU, and HCCDNASH, HCC from different etiologies are grouped together. As a result, this study cannot provide information on the incidence and fatality rates of HCC induced by aflatoxin, parasites, or hemochromatosis. Similarly, this study did not investigate the HCC produced by the interaction of many etiologies. Third, the results provided by GBD were derived from mathematical models rather than observations. Therefore, the data produced from this study should be regarded with caution. Finally, although this study uses joint point regression analysis to analyze the change trend of HCC, it may not fully explain the confounding factors that may affect cancer incidence rate and mortality over time, such as changes in health care, screening practices or public health policies.
Conclusions
Our research has shown that from 1990 to 2021, the overall incidence rate and mortality of HCC in China declined. The incidence rate and mortality of HCCDHB, HCCDHC and HCCDOC all showed a downward trend during this period. The incidence rate of HCCDAU and HCCDNASH showed an upward trend during this period, while the trend of mortality was not significant. Therefore, interventions targeting alcohol abuse and obesity may reduce the incidence and mortality trends of HCCDAU and HCCDNASH.
Appendix.
Abbreviations
- HCC
Hepatocellular carcinoma
- HBV
Hepatitis B virus
- HCV
hepatitis C virus
- AU
alcohol abuse
- NASH
non-alcoholic steatohepatitis
- GBD
Global Burden of Disease
- ASIR
age-standardized incidence rate
- ASMR
age-standardized mortality rate
- HCCDHB
HCC due to hepatitis B
- HCCDHC
HCC due to hepatitis C
- HCCDAU
HCC due to AU
- HCCDNASH
HCC due to NASH
- HCCDOC
HCC due to other causes
- UI
uncertainty intervals
- APC
annual percentage change
- AAPC
average APC
- DAAs
direct-acting antiviral drugs
Footnotes
Author Contributions: Conceptualization, Jiaye Long and Du Wang; methodology, Jiaye Long and Shuxin Qin; software, Jiaye Long and Kai Cui; writing—original draft preparation, Jiaye Long; writing—review and editing, Zhong Li; visualization, Du Wang; supervision, Zhong Li. All authors have read and agreed to the published version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Statement
Ethical Considerations
This study did not require ethical review and approval because it used publicly available deidentified data accessed from GBD 2021.
ORCID iD
Jiaye Long https://orcid.org/0000-0003-2821-4011
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):209-249. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 2.Long J, Chen B, Liu Z. Comparative efficacy and safety of molecular targeted agents combined with transarterial chemoembolization in the treatment of unresectable hepatocellular carcinoma: a network meta-analysis. Front Oncol. 2023;13:1179431. doi: 10.3389/fonc.2023.1179431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rumgay H, Arnold M, Ferlay J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040. J Hepatol. 2022;77(6):1598-1606. doi: 10.1016/j.jhep.2022.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J. 2021;134(7):783-791. doi: 10.1097/CM9.0000000000001474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Massarweh NN, El-Serag HB. Epidemiology of hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Cancer Control. 2017;24(3):1073274817729245. doi: 10.1177/1073274817729245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang DQ, Singal AG, Kono Y, Tan DJH, El-Serag HB, Loomba R. Changing global epidemiology of liver cancer from 2010 to 2019: NASH is the fastest growing cause of liver cancer. Cell Metabol. 2022;34(7):969-977.e2. doi: 10.1016/j.cmet.2022.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.GBD 2021 Diseases and Injuries Collaborators . Global incidence, prevalence, Years Lived with Disability (YLDs), Disability-Adjusted Life-Years (DALYs), and Healthy Life Expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133-2161. doi: 10.1016/S0140-6736(24)00757-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573-577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 9.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates [published correction appears in Stat Med 2001 Feb 28;20(4):655]. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 10.Wang H, Men P, Xiao Y, et al. Hepatitis B infection in the general population of China: a systematic review and meta-analysis. BMC Infect Dis. 2019;19(1):811. doi: 10.1186/s12879-019-4428-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang P, Zu J, Yin J, et al. The independent impact of newborn hepatitis B vaccination on reducing HBV prevalence in China, 1992-2006: a mathematical model analysis. J Theor Biol. 2015;386:115-121. doi: 10.1016/j.jtbi.2015.08.030 [DOI] [PubMed] [Google Scholar]
- 12.Chen DS. Hepatitis B vaccination: the key towards elimination and eradication of hepatitis B. J Hepatol. 2009;50(4):805-816. doi: 10.1016/j.jhep.2009.01.002 [DOI] [PubMed] [Google Scholar]
- 13.Qu C, Chen T, Fan C, et al. Efficacy of neonatal HBV vaccination on liver cancer and other liver diseases over 30-year follow-up of the Qidong hepatitis B intervention study: a cluster randomized controlled trial. PLoS Med. 2014;11(12):e1001774. doi: 10.1371/journal.pmed.1001774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heredia-Torres TG, Rincón-Sánchez AR, Lozano-Sepúlveda SA, et al. Unraveling the molecular mechanisms involved in HCV-induced carcinogenesis. Viruses. 2022;14(12):2762. doi: 10.3390/v14122762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D’souza S, Lau KC, Coffin CS, Patel TR. Molecular mechanisms of viral hepatitis induced hepatocellular carcinoma. World J Gastroenterol. 2020;26(38):5759-5783. doi: 10.3748/wjg.v26.i38.5759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alter MJ. Epidemiology of hepatitis C virus infection. World J Gastroenterol. 2007;13(17):2436-2441. doi: 10.3748/wjg.v13.i17.2436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou J, Wang FD, Li LQ, Chen EQ. Management of in- and out-of-hospital screening for hepatitis C. Front Public Health. 2023;10:984810. doi: 10.3389/fpubh.2022.984810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao Z, Chu M, Guo Y, et al. Feasibility of hepatitis C elimination in China: from epidemiology, natural history, and intervention perspectives. Front Microbiol. 2022;13:884598. doi: 10.3389/fmicb.2022.884598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naugler WE, Sakurai T, Kim S, et al. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science. 2007;317(5834):121-124. doi: 10.1126/science.1140485 [DOI] [PubMed] [Google Scholar]
- 20.Nakagawa H, Maeda S, Yoshida H, et al. Serum IL-6 levels and the risk for hepatocarcinogenesis in chronic hepatitis C patients: an analysis based on gender differences. Int J Cancer. 2009;125(10):2264-2269. doi: 10.1002/ijc.24720 [DOI] [PubMed] [Google Scholar]
- 21.Levinsson A, Zolopa C, Vakili F, et al. Sex and gender differences in hepatitis C virus risk, prevention, and cascade of care in people who inject drugs: systematic review and meta-analysis. EClinicalMedicine. 2024;72:102596. doi: 10.1016/j.eclinm.2024.102596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao G, Liu J, Liu M. Global, regional, and national trends in incidence and mortality of primary liver cancer and its underlying etiologies from 1990 to 2019: results from the global burden of disease study 2019. J Epidemiol Glob Health. 2023;13(2):344-360. doi: 10.1007/s44197-023-00109-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu A, Jiang H, Dowling R, et al. The transition of alcohol control in China 1990-2019: impacts and recommendations. Int J Drug Pol. 2022;105:103698. doi: 10.1016/j.drugpo.2022.103698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo L, Deng J, He Y, et al. Alcohol use and alcohol-related problems among adolescents in China: a large-scale cross-sectional study. Medicine (Baltim). 2016;95(38):e4533. doi: 10.1097/MD.0000000000004533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ji CY, Hu PJ, Song Y. The epidemiology of alcohol consumption and misuse among Chinese college students. Alcohol Alcohol. 2012;47(4):464-472. doi: 10.1093/alcalc/ags037 [DOI] [PubMed] [Google Scholar]
- 26.Bizzaro D, Becchetti C, Trapani S, et al. Influence of sex in alcohol-related liver disease: pre-clinical and clinical settings. United European Gastroenterol J. 2023;11(2):218-227. doi: 10.1002/ueg2.12370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fried SK, Lee MJ, Karastergiou K. Shaping fat distribution: new insights into the molecular determinants of depot- and sex-dependent adipose biology. Obesity. 2015;23(7):1345-1352. doi: 10.1002/oby.21133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lonardo A, Nascimbeni F, Ballestri S, et al. Sex differences in nonalcoholic fatty liver disease: state of the art and identification of research gaps. Hepatology. 2019;70(4):1457-1469. doi: 10.1002/hep.30626 [DOI] [PMC free article] [PubMed] [Google Scholar]