Abstract
Background: Primary percutaneous coronary intervention (PCI) is crucial in managing acute ST-segment elevation myocardial infarction (STEMI), emphasizing the importance of optimal myocardial reperfusion.
Objective: The goal of this research was to determine how loading doses of rosuvastatin and atorvastatin affected the flow rate of thrombolysis in myocardial infarction (TIMI) immediately post-perfusion thrombolysis in patients undergoing primary PCI.
Methodology: This prospective, comparative study was carried out over a one-year period (January 2023 to December 2023) in Pakistan. Data was gathered from patient interviews and electronic medical records for adult patients receiving primary PCI. Interventional cardiologists who were blinded to the evaluation of the immediate post-perfusion TIMI flow conducted statistical analysis to compare the results between the two statin groups.
Results: Both groups had good procedural success rates: 184 patients (92.00%) in the group using rosuvastatin and 179 patients (89.50%) in the group on atorvastatin (p = 0.284). A comparable use of auxiliary equipment was seen, with 103 patients (51.50%) and 97 patients (48.50%) in the atorvastatin group and 108 patients (54.00%) and 92 patients (46.00%) in the rosuvastatin group, respectively (p = 0.53). There were no notable variations in the immediate post-perfusion TIMI flow grades either, with p-values of 0.532 for normal flow and 0.421 for no-reflow. The two groups' mean lengths of hospital stays were comparable, measuring 3.5 days (± 1.2) for the rosuvastatin group and 3.8 days (± 1.3) for the atorvastatin group (p = 0.321).
Conclusion: Rosuvastatin and atorvastatin had comparable rapid post-perfusion TIMI flows in the initial PCI participants, indicating that they may be used interchangeably to maximize myocardial reperfusion in acute STEMI.
Keywords: atorvastatin, cardiovascular outcomes, myocardial reperfusion, pci, rosuvastatin, stemi
Introduction
Acute ST-segment elevation myocardial infarction (STEMI) remains a significant contributor to cardiovascular morbidity and mortality worldwide, with its prevalence continuing to rise due to lifestyle factors and an aging population [1,2]. Primary percutaneous coronary intervention (PCI) is the gold standard for managing STEMI, aimed at rapidly restoring coronary artery patency to salvage ischemic myocardium and reduce the risk of adverse cardiac events such as heart failure or recurrent myocardial infarction [3]. Despite advancements in procedural techniques and adjunct pharmacotherapy, achieving optimal myocardial reperfusion remains essential to improving clinical outcomes and reducing STEMI-related mortality [4].
The thrombolysis in myocardial infarction (TIMI) flow grade is a critical indicator of coronary reperfusion after PCI, offering a standardized measure to assess the restoration of blood flow in the infarct-related artery [5]. Higher TIMI flow grades post-PCI are correlated with better patient prognoses, including improved left ventricular function, reduced adverse cardiac events, and enhanced long-term survival rates [6,7]. Thus, optimizing TIMI flow during PCI is crucial to ensuring favorable outcomes in patients with acute STEMI [8].
Statin therapy plays a vital role in the secondary prevention of cardiovascular events due to its serum cholesterol level-lowering and pleiotropic effects, such as anti-inflammatory, antioxidant, and endothelial-stabilizing properties [9,10]. These additional effects of statins may further enhance myocardial reperfusion, making them a critical component of the therapeutic regimen in STEMI management [11]. Among the statins, atorvastatin and rosuvastatin are frequently used due to their proven efficacy in reducing cardiovascular morbidity and mortality [12].
However, while the safety and serum cholesterol level-lowering capabilities of both rosuvastatin and atorvastatin are well-documented, there remains limited data on their comparative effects on immediate post-perfusion TIMI flow in patients undergoing primary PCI [13]. Understanding these differences is clinically relevant, as optimizing the loading dose of statins before PCI could significantly influence myocardial reperfusion and subsequent patient outcomes. Given the increasing incidence of STEMI, refining pharmacotherapy to enhance reperfusion strategies is of the utmost importance.
This study seeks to bridge the existing knowledge gap by directly comparing the effects of loading doses of rosuvastatin versus atorvastatin on immediate post-perfusion TIMI flow in STEMI patients undergoing primary PCI. By evaluating whether one statin offers superior benefits in this critical setting, the research aims to optimize acute management strategies, enhance reperfusion outcomes, and potentially reduce the burden of cardiovascular disease. The evidence generated could guide pharmacological decisions to improve patient outcomes in the management of acute STEMI.
Materials and methods
Study design and settings
The Abbasi Shaheed Hospital (Karachi) and Lady Reading Hospital (Peshawar), tertiary care facilities for cardiovascular treatment in Pakistan, were the sites of this research. The patients who presented with acute STEMI and had primary PCI were included in the trial, which ran from January 2023 to December 2023.
Inclusion and exclusion criteria
Adult patients (either gender) who received primary PCI throughout the length of the trial and who presented with acute STEMI were included in the study. Exclusions from the study included patients with renal impairment (estimated glomerular filtration rate < 30 ml/minute/1.73 m2), liver dysfunction (alanine transaminase or aspartate transaminase levels more than three times the upper limit of normal), history of statin intolerance or allergic reactions, and contraindications to statin therapy.
Sample size
A power analysis with an impact size of 0.5, a power of 80%, and a statistical significance level of 0.05 served as the basis for calculating the sample size. To identify statistically significant changes in immediate post-perfusion TIMI flow between the two research groups, a minimum sample size of 400 patients was required.
Data collection
Clinical information was gathered prospectively from electronic medical records and patient interviews. This information included demographics, medical history, test results, and procedure specifics. By using angiography, skilled interventional cardiologists blinded to the patients' statin assignment evaluated the immediate post-perfusion TIMI flow. Standardized data collection forms were used to guarantee accuracy and uniformity in the data-gathering process.
Dosage administration
Statins, such as atorvastatin and rosuvastatin, were administered according to established procedures that were customized for each patient. When necessary, rosuvastatin was recommended at a loading dose of 10 mg for quick therapeutic benefits in addition to the usual daily dosage of 20 mg. In a comparable manner, 40 mg of atorvastatin was first prescribed daily, with a loading dose of 20 mg added for any required fast-acting effects.
Statistical analysis
Descriptive statistics were used to describe the operational parameters and baseline features. Frequencies and percentages were used to describe data that is categorical, while mean ± standard deviation or median with interquartile ranges were used to display variables that are continuous. Between-group analyses were carried out using appropriate statistical methods, such as chi-square tests for categorical data and independent t-tests for continuous variables. P-values were considered highly significant if they were less than 0.05.
Ethical approval
The study received ethical approval from the Institutional Review Boards (IRBs) of Lahore Medical and Dental College, Lahore, Pakistan, Abbasi Shaheed Hospital, Karachi, Pakistan, and Lady Reading Hospital, Peshawar, Pakistan.
Results
The baseline characteristics of patients receiving primary PCI in the atorvastatin and rosuvastatin groups are shown in Table 1. The average age of the rosuvastatin group was 62.4 (± 8.3) years, with 118 patients (59.00%) under 65 and 82 patients (41.00%) over 65. The distribution of patients' genders revealed that 151 patients (75.50%) were males, while 49 of the patients (24.50%) were females. Of the comorbidities, 116 patients (58.00%) had hypertension, 83 (41.50%) had diabetes mellitus, and 42 (21.00%) had a history of smoking. Of the patients, 93 (46.50%) had a history of dyslipidemia, 54 (27.00%) had a history of myocardial infarction (MI), 27 (13.50%) had a history of PCI, and 16 (8.00%) had a history of coronary artery bypass grafting (CABG). The mean age of the atorvastatin group was 63.1 years (± 7.9), with 84 patients (42.00%) and 116 patients (58.00%) being younger than 65. There were 46 girls (23.00%) and 154 men (77.00%) in the gender distribution. Comorbidities comprised diabetes mellitus in 92 individuals (46.0%), hypertension in 109 people (54.50%), and a past of smoking in 36 individuals (18.00%). Dyslipidemia was noted in 98 patients (49.00%), MI in 48 patients (24.0%), PCI in 33 patients (16.50%), and CABG in 21 patients (10.50%).
Table 1. Patient overview and initial features.
PCI: percutaneous coronary intervention; CABG: coronary artery bypass grafting
| Characteristic | Rosuvastatin group | Atorvastatin group | |
| Age (years) | Mean ± SD | 62.4 ± 8.3 | 63.1 ± 7.9 |
| Age group categories n (%) | < 65 years | 118 (59.00%) | 116 (58.00%) |
| ≥ 65 years | 82 (41.00%) | 84 (42.00%) | |
| Gender categories n (%) | Male | 151 (75.50%) | 154 (77.00%) |
| Female | 49 (24.50%) | 46 (23.00%) | |
| Comorbidities n (%) | Hypertension | 116 (58.00%) | 109 (54.50%) |
| Diabetes mellitus | 83 (41.50%) | 92 (46.00%) | |
| Smoking | 42 (21.00%) | 36 (18.00%) | |
| History of dyslipidemia | 93 (46.50%) | 98 (49.00%) | |
| Previous myocardial infarction | 54 (27.00%) | 48 (24.00%) | |
| Previous PCI | 27 (13.50%) | 33 (16.50%) | |
| Previous CABG | 16 (8.00%) | 21 (10.50%) | |
Procedure information for primary PCI patients is shown in Table 2, which is divided into groups based on statin therapy. According to the American College of Cardiology and the American Heart Association (ACC/AHA) criteria, 139 patients (69.50%) in the rosuvastatin group and 131 patients (65.50%) in the atorvastatin group had type A lesions (p = 0.421). With 184 patients (92.00%) in the rosuvastatin group and 179 patients (89.50%) in the atorvastatin group (p = 0.284), both groups had good procedural success rates. Similarities were also seen in the use of stents and angioplasty balloons among the dual groups: 108 patients (54.00%) and 92 patients (46.00%) in the group taking rosuvastatin, and 103 patients (51.50%) and 97 patients (48.50%) in the group using atorvastatin, respectively (p = 0.53).
Table 2. Achievement rates and procedural features.
ACC/AHA: American College of Cardiology/American Heart Association
| Procedural details | Rosuvastatin group | Atorvastatin group | p-value | |||
| n | % | n | % | |||
| Lesion complexity (ACC/AHA) | Type A | 139 | 69.50 | 131 | 65.50 | 0.421 |
| Type B | 61 | 30.50 | 69 | 34.50 | ||
| Procedural success | Successful | 184 | 92.00 | 179 | 89.50 | 0.284 |
| Unsuccessful | 16 | 8.00 | 21 | 10.50 | ||
| Adjunctive devices used | Angioplasty balloon | 108 | 54.00 | 103 | 51.50 | 0.53 |
| Stent | 92 | 46.00 | 97 | 48.50 | ||
The TIMI flow grades immediately after perfusion in individuals treated with atorvastatin or rosuvastatin are shown in Table 3. Grade 0, which indicates no perfusion; grade 1, which indicates penetration without perfusion; Grade 2, which indicates partial perfusion; and normal flow are the four categories into which the TIMI flow grades are divided. Six patients (3.00%) had grade 1, five patients (2.50%) had grade 2, and 184 patients (92.00%) had normal flow in the rosuvastatin group. Five patients (2.50%) had grade 0. The atorvastatin group, in contrast, consisted of 179 patients (89.50%) with normal flow, eight patients (4.00%) with grade 1, seven patients (3.50%) with grade 2, and six patients (3.00%) with grade 0. The p-values, which are 0.421 for no-reflow and 0.532 for normal flow, show the statistical significance of the differences between the two groups.
Table 3. TIMI flow grades following instantaneous perfusion.
TIMI: thrombolysis in myocardial infarction
| TIMI flow grade | Rosuvastatin group | Atorvastatin group | p-value | |||
| n | % | n | % | |||
| No-reflow | Grade 0: No perfusion | 5 | 2.50 | 6 | 3.00 | 0.421 |
| Grade 1: Penetration without perfusion | 6 | 3.00 | 8 | 4.00 | ||
| Grade 2: Partial perfusion | 5 | 2.50 | 7 | 3.50 | ||
| Normal flow | 184 | 92.00 | 179 | 89.50 | 0.532 | |
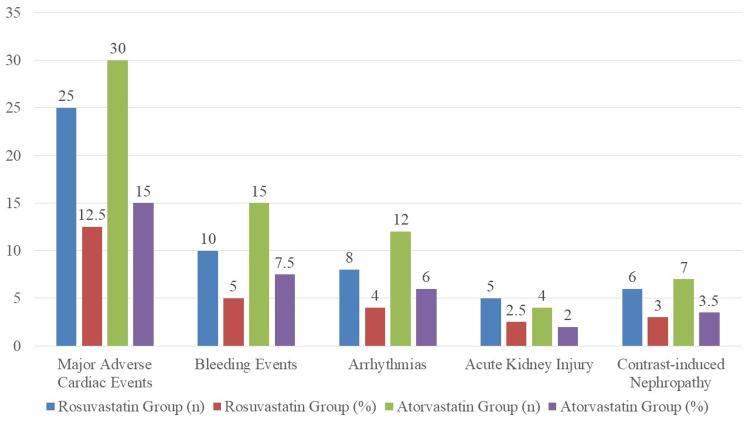
A comparison of side effects between the atorvastatin and rosuvastatin groups is shown in Figure 1. Major adverse cardiac occurrences, bleeding events, arrhythmias, acute kidney injury, and contrast-induced nephropathy are examples of adverse occurrences. Among the patients in the rosuvastatin group, there were 25 (12.50%) who had major adverse cardiac events, 10 (5.00%) who had bleeding events, eight (4.00%) who had arrhythmias, five (2.50%) who had acute kidney injury, and six (3.00%) who acquired contrast-induced nephropathy. In contrast, 30 patients (15.00%) in the atorvastatin group experienced major adverse cardiac events, 15 patients (7.50%) had bleeding events, 12 patients (6.00%) had arrhythmias, four patients (2.00%) had acute kidney injury, and seven patients (3.50%) developed contrast-induced nephropathy.
Figure 1. Comparing adverse events in the groups taking atorvastatin and rosuvastatin.
The comparison of several laboratory parameters between the atorvastatin and rosuvastatin groups is shown in Table 4. The low-density lipoprotein (LDL) cholesterol levels in the rosuvastatin and atorvastatin groups were 100.5 ± 15.3 mg/dL and 102.1 ± 14.8 mg/dL, respectively, with mean ± SD values. The interquartile range (IQR) for alaminase (ALT) was 25 (20-30) IU/L in the rosuvastatin group and 28 (22-32) IU/L in the atorvastatin group. The mean ± standard deviation (SD) values for the estimated glomerular filtration rate (eGFR) were 76.8 ± 11.2 ml/minute/1.73 m2 in the atorvastatin group and 78.2 ± 10.5 ml/minute/1.73 m2 in the rosuvastatin group. The levels of creatine kinase-MB (CK-MB) in the rosuvastatin and atorvastatin groups were 12.5 (10-15) ng/mL and 13 (11-16) ng/mL, respectively, with median (IQR) values. The mean ± SD values of troponin I levels were 6.8 ± 2.1 ng/mL in the group using rosuvastatin and 7.2 ± 2.5 ng/mL in the group taking atorvastatin. The mean ± standard deviation of hemoglobin levels in the rosuvastatin and atorvastatin groups were 13.8 ± 1.2 g/dL and 13.5 ± 1.3 g/dL, respectively. In conclusion, the mean ± standard deviation of platelet counts (x109/L) was found to be 220.4 ± 45.6 x109/L for the rosuvastatin group and 215.8 ± 42.3 x109/L for the atorvastatin group. Hemoglobin levels (p = 0.142) and ALT levels (p = 0.284) showed significant changes, but no other parameters showed any significant differences (p > 0.05).
Table 4. Comparison of laboratory parameters for the atorvastatin and rosuvastatin groups.
LDL cholesterol: low-density lipoprotein cholesterol, ALT: alanine transaminase, eGFR: estimated glomerular filtration rate, CK-MB: creatine kinase-MB
| Laboratory parameter | Rosuvastatin group | Atorvastatin group | p-value |
| LDL cholesterol (mg/dL), mean ± SD | 100.5 ± 15.3 | 102.1 ± 14.8 | 0.421 |
| ALT (IU/L), median (IQR) | 25 (20-30) | 28 (22-32) | 0.284 |
| eGFR (ml/min/1.73 m2), mean ± SD | 78.2 ± 10.5 | 76.8 ± 11.2 | 0.532 |
| CK-MB (ng/mL), median (IQR) | 12.5 (10-15) | 13 (11-16) | 0.176 |
| Troponin I (ng/mL), mean ± SD | 6.8 ± 2.1 | 7.2 ± 2.5 | 0.321 |
| Hemoglobin (g/dL), mean ± SD | 13.8 ± 1.2 | 13.5 ± 1.3 | 0.142 |
| Platelet count (x109/L), mean ± SD | 220.4 ± 45.6 | 215.8 ± 42.3 | 0.621 |
Table 5 displays clinical outcomes and the duration of hospital stay for the atorvastatin and rosuvastatin-taking groups. In the group using rosuvastatin, the average length of hospital stay was 3.5 days (± 1.2), whereas in the group on atorvastatin, it was 3.8 days (± 1.3). The statistical significance of the disparity in hospital stay duration among the two subgroups was not found, as shown by the comparison's p-value of 0.321.
Table 5. Hospital stay duration and clinical outcomes.
| Hospital stay duration (days) | Rosuvastatin group | Atorvastatin group | p-value |
| Mean ± SD | 3.5 ± 1.2 | 3.8 ± 1.3 | 0.321 |
Discussion
The immediate post-perfusion TIMI flow is a crucial determinant of myocardial reperfusion and clinical outcomes following primary PCI in acute STEMI patients [14]. Our study found comparable rates of achieving optimal TIMI flow between atorvastatin and rosuvastatin groups (92.00% vs. 89.50%), which aligns with previous research indicating similar efficacy in restoring coronary flow [15,16]. This suggests that both statins are effective options in the acute setting, providing clinicians with flexibility based on patient-specific factors. Additionally, procedural success rates and lesion complexity were similar across groups, reinforcing the role of statins in optimizing PCI outcomes by stabilizing plaques and enhancing coronary flow [17,18].
Regarding safety, both statins demonstrated a similar adverse event profile. The rates of serious adverse cardiac events, bleeding episodes, and renal complications did not significantly differ between the two groups, which is in agreement with the existing literature showing that atorvastatin and rosuvastatin are generally well-tolerated in high-risk cardiovascular patients [19,20]. For instance, bleeding rates were slightly lower in the rosuvastatin group (5.00% vs. 7.50%), but this difference was not statistically significant. The low incidence of adverse renal events and arrhythmias further confirms the safety of these agents when used at high doses during the acute phase of STEMI management.
Interestingly, our findings on comparable clinical outcomes align with studies that reported no substantial differences in myocardial perfusion or adverse events when comparing high-dose regimens of various statins in acute coronary syndromes [15,21]. However, some evidence suggests that rosuvastatin might have a marginal advantage due to its more potent anti-inflammatory effects, although this was not statistically significant in our cohort [22]. Future research, especially large-scale randomized trials, would be beneficial to determine if such differences might impact long-term outcomes.
Beyond the immediate pharmacological effects, social determinants of cardiovascular health, as highlighted in studies like that of Borkowski et al., play a pivotal role in patient outcomes [23]. In regions like Pakistan, where our study was conducted, factors such as socioeconomic status, limited access to timely medical care, and disparities in healthcare resources significantly influence the prognoses of STEMI patients. These systemic barriers can lead to delayed interventions, which in turn may compromise the benefits of pharmacological therapies. Addressing these social inequities, along with optimizing acute pharmacotherapy, could lead to better health outcomes.
Strength and limitation
The present study possesses several strengths, notably its prospective design and comparative approach, which significantly reduce recall bias and enhance the reliability of collected data. By directly comparing the effects of loading doses of rosuvastatin and atorvastatin on immediate post-perfusion TIMI flow, the study offers valuable insights into optimizing acute management strategies for STEMI patients undergoing primary PCI. The blinded evaluation of TIMI flow by interventional cardiologists further strengthens the study’s methodological rigor, reducing the risk of assessment bias. However, a key limitation is the lack of randomization in patient allocation, which introduces the potential for selection bias, as patients were assigned to either statin therapy based on clinical practice or physician discretion rather than a randomized process. Statistical adjustments were employed to mitigate this limitation, and blinding was utilized during the evaluation of primary outcomes.
Future perspective
Although this study provides insights into the acute effects of atorvastatin and rosuvastatin on immediate myocardial reperfusion in STEMI patients, future research should focus on assessing the long-term impact of these statins on mortality, recurrent cardiovascular events, and overall patient survival. Additionally, an analysis of specific patient subgroups-such as those defined by age, comorbidities (e.g., diabetes, hypertension), and genetic markers-could provide valuable insights into whether certain populations derive greater benefit from one statin over the other. Investigating the mechanistic differences between statins, especially their effects on endothelial function, plaque stability, and inflammation, will also help further refine treatment strategies in the acute coronary syndrome setting. A randomized controlled trial design would be essential to minimize bias and strengthen the evidence supporting the clinical use of statins in STEMI management.
Conclusions
The results demonstrated no significant differences between atorvastatin and rosuvastatin in terms of achieving optimal TIMI flow, procedural success rates, lesion complexity, adverse events, laboratory parameters, length of hospital stay, or overall clinical outcomes. Both statins showed comparable effectiveness and safety profiles, suggesting that they may be used interchangeably in the acute STEMI setting. These findings underscore the clinical importance of statin therapy in primary PCI for acute STEMI patients, as both atorvastatin and rosuvastatin contribute to myocardial reperfusion and potentially improve patient outcomes. These results could inform clinical practice and guidelines, reinforcing the use of either statin as a valuable therapeutic option in the management of acute STEMI, thereby helping to optimize patient care and treatment strategies.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study. IRB of Lahore Medical and Dental College (LMDC) issued approval LM&DC 30656-21/2023.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Sajjad Ullah Khan, Ahmed Jamal Chaudhary, Sana Iqbal, Nisar Ahmad Khan, Anshaal Furrukh, Shah Bano, Muhammad Nasir Ali, Afaq Ali
Critical review of the manuscript for important intellectual content: Sajjad Ullah Khan, Sana Iqbal, Anshaal Furrukh, Shah Bano, Afaq Ali
Supervision: Sajjad Ullah Khan
Acquisition, analysis, or interpretation of data: Ahmed Jamal Chaudhary, Sana Iqbal, Nisar Ahmad Khan, Anshaal Furrukh, Shah Bano, Muhammad Nasir Ali, Afaq Ali
Drafting of the manuscript: Ahmed Jamal Chaudhary, Nisar Ahmad Khan, Muhammad Nasir Ali, Afaq Ali
References
- 1.Comparative Study between safety and efficacy of pharmacoinvasive strategy and primary percutaneous coronary angioplasty in patients presenting by acute ST segment elevation myocardial infarction. Samia M, Ahmed GS, Ayman A, Yasser H. J Cairo Univ. 2019;87:705–712. [Google Scholar]
- 2.Procedural volume and outcomes after primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction in Kerala, India: report of the Cardiological Society of India-Kerala primary percutaneous coronary intervention registry. Jabir A, Mathew A, Zheng Y, et al. J Am Heart Assoc. 2020;9:0. doi: 10.1161/JAHA.119.014968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acute coronary syndromes (ACS)-unravelling biology to identify new therapies-the microcirculation as a frontier for new therapies in ACS. Vaidya K, Tucker B, Patel S, Ng MK. Cells. 2021;10:2188. doi: 10.3390/cells10092188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Therapy in ST-elevation myocardial infarction: reperfusion strategies, pharmacology and stent selection. Singh V, Cohen MG. Curr Treat Options Cardiovasc Med. 2014;16:302. doi: 10.1007/s11936-014-0302-9. [DOI] [PubMed] [Google Scholar]
- 5.Coronary no-reflow after primary percutaneous coronary intervention-current knowledge on pathophysiology, diagnosis, clinical impact and therapy. Ndrepepa G, Kastrati A. J Clin Med. 2023;12:5592. doi: 10.3390/jcm12175592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. van 't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Circulation. 1998;97:2302–2306. doi: 10.1161/01.cir.97.23.2302. [DOI] [PubMed] [Google Scholar]
- 7.The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. Antman EM, Cohen M, Bernink PJ, et al. JAMA. 2000;284:835–842. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 8.Short-term safety and long-term benefits of stent postdilation after primary percutaneous coronary intervention: results of a cohort study. Saadat N, Saadatagah S, Aghajani Nargesi A, et al. Catheter Cardiovasc Interv. 2020;95:1249–1256. doi: 10.1002/ccd.28396. [DOI] [PubMed] [Google Scholar]
- 9.Statin therapy for the primary prevention of cardiovascular disease: pros. Razavi AC, Mehta A, Sperling LS. Atherosclerosis. 2022;356:41–45. doi: 10.1016/j.atherosclerosis.2022.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Novel concepts of statin therapy for cardiovascular risk reduction in hypertension. Varughese GI, Patel JV, Lip GY, Varma C. Curr Pharm Des. 2006;12:1593–1609. doi: 10.2174/138161206776843304. [DOI] [PubMed] [Google Scholar]
- 11.Beneficial effects of statins on seizures independent of their lipid-lowering effect: a narrative review. Amanlou A, Nassireslami E, Dehpour AR, Rashidian A, Chamanara M. Iran J Med Sci. 2023;48:13–25. doi: 10.30476/IJMS.2021.91645.2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Comparing the effectiveness of rosuvastatin and atorvastatin in preventing cardiovascular outcomes: estimates using the Archimedes model. Schuetz CA, van Herick A, Alperin P, Peskin B, Hsia J, Gandhi S. J Med Econ. 2012;15:1118–1129. doi: 10.3111/13696998.2012.704459. [DOI] [PubMed] [Google Scholar]
- 13.Clinical benefit of statin pretreatment in patients undergoing percutaneous coronary intervention: a collaborative patient-level meta-analysis of 13 randomized studies. Patti G, Cannon CP, Murphy SA, et al. Circulation. 2011;123:1622–1632. doi: 10.1161/CIRCULATIONAHA.110.002451. [DOI] [PubMed] [Google Scholar]
- 14.Admission troponin T level predicts clinical outcomes, TIMI flow, and myocardial tissue perfusion after primary percutaneous intervention for acute ST-segment elevation myocardial infarction. Giannitsis E, Müller-Bardorff M, Lehrke S, et al. Circulation. 2001;104:630–635. doi: 10.1161/hc3101.093863. [DOI] [PubMed] [Google Scholar]
- 15.Comparing the effects of loading dose of rosuvastatin vs atorvastatin on immediate post-perfusion TIMI flow in primary PCI patient. Kamran M, Mukhtar M, Ali M, Umair M, Ahmed A. Biol Clin Sci Res J. 2023;4:271. [Google Scholar]
- 16.Comparison of the treatment efficacy of rosuvastatin versus atorvastatin loading prior to percutaneous coronary intervention in ST-segment elevation myocardial infarction. Adel EM, Elberry AA, Abdel Aziz A, Naguib IA, Alghamdi BS, Hussein RR. J Clin Med. 2022;11:5142. doi: 10.3390/jcm11175142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prevention of peri-procedural myocardial injury using a single high loading dose of rosuvastatin. Cay S, Cagirci G, Sen N, Balbay Y, Durmaz T, Aydogdu S. Cardiovasc Drugs Ther. 2010;24:41–47. doi: 10.1007/s10557-010-6224-1. [DOI] [PubMed] [Google Scholar]
- 18.12-month follow-up results of high dose rosuvastatin loading before percutaneous coronary intervention in patients with acute coronary syndrome. Yun KH, Oh SK, Rhee SJ, Yoo NJ, Kim NH, Jeong JW. Int J Cardiol. 2011;146:68–72. doi: 10.1016/j.ijcard.2010.04.052. [DOI] [PubMed] [Google Scholar]
- 19.Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR* Trial) Jones PH, Davidson MH, Stein EA, et al. American journal of cardiology. 2003;92:152–160. doi: 10.1016/s0002-9149(03)00530-7. [DOI] [PubMed] [Google Scholar]
- 20.A randomised study comparing the efficacy and safety of rosuvastatin with atorvastatin for achieving lipid goals in clinical practice in Asian patients at high risk of cardiovascular disease (DISCOVERY-Asia study) Zhu JR, Tomlinson B, Ro YM, Sim KH, Lee YT, Sriratanasathavorn C. Curr Med Res Opin. 2007;23:3055–3068. doi: 10.1185/030079907x242809. [DOI] [PubMed] [Google Scholar]
- 21.Comparative effects of high-dose atorvastatin versus moderate-dose rosuvastatin on lipid parameters, oxidized-LDL and inflammatory markers in ST elevation myocardial infarction. Aydin MU, Aygul N, Altunkeser BB, Unlu A, Taner A. Atherosclerosis. 2015;239:439–443. doi: 10.1016/j.atherosclerosis.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Comparison of anti-inflammatory effect of atorvastatin with rosuvastatin in patients of acute coronary syndrome. Khurana S, Gupta S, Bhalla H, Nandwani S, Gupta V. J Pharmacol Pharmacother. 2015;6:130–135. doi: 10.4103/0976-500X.162011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Racial and socioeconomic determinants of cardiovascular health: a comprehensive review. Borkowski P, Borkowska N, Mangeshkar S, Adal BH, Singh N. Cureus. 2024;16:0. doi: 10.7759/cureus.59497. [DOI] [PMC free article] [PubMed] [Google Scholar]