Abstract
Background
Giant coronary artery aneurysms are rare conditions with potentially devastating consequences. We report a case of the largest documented giant right coronary artery (RCA) aneurysm to date.
Case presentation
A 57-year-old male patient visited our outpatient clinic for abdominal pain and exertional dyspnea. Computed tomography identified a 10.2 × 9.8 cm RCA aneurysm with RCA pressure waves were similar to aortic pressures. After discussion by the cardiac team, elective resection with ligation of the proximal and distal ends of the RCA was performed due to the presence of adequate collaterals.
Conclusion
We highlight the challenges related to the management of patients presenting with giant coronary artery aneurysms. Optimal management strategies and outcomes for such rare cardiovascular conditions implies the need for standardised management guidelines.
Keywords: Coronary artery aneurysm, Pericardial cyst, Dysnea, Coronary vessel anomaly, Pressure wave
Background
RCA aneurysm can lead to severe complications limiting cardiac output due to compression of the right heart, manifesting with dyspnea, abdominal pain and dyspepsia [1]. Potential complications include myocardial ischemia, thromboembolism, spontaneous rupture leading to cardiac tamponade, and sudden death. The pathophysiology of giant coronary artery aneurysm (CAA) remains to be elucidated. In adults, atherosclerosis accounts for approximately 50% of CAA cases, followed by Kawasaki disease, congenital heart disease, trauma, Ehlers-Danlos syndrome, Marfan syndrome, Takayasu arteritis, polyarteritis nodosa, syphilitic aortitis, scleroderma, systemic lupus erythematosus, Behçet disease, and fibromuscular dysplasia [2]. Giant CAA (> 5 cm in diameter) comprise a rare subset of CAA with an incidence 0.02% [3]. These aneurysms most commonly affects the RCA proximal part (85%). The mechanism for aneurysmal formation is proposed to the relatively low pressures around the right atrium although that might explain the larger size and not the higher prevalence [4].
Case presentation
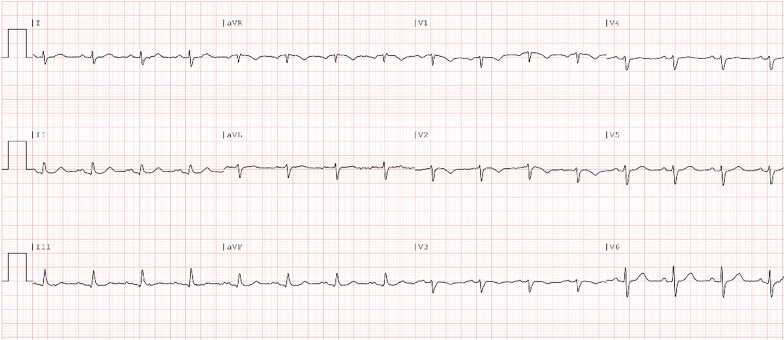
A 57-year-old white man was evaluated at our outpatient clinic for episodes of dyspnea persisting for several months, particularly while climbing one flight of stairs and fast walking. The patient denied any history of chest pain, palpitations, dizziness. Blood pressure was 107/69 mm Hg, heart rate was 74 beats/min, respiratory rate was 12/minute, and temperature was 36.8 ºC (98.24 ºF). Initial electrocardiographic assessment showed sinus rhythm, poor R wave progression and T wave inversion at leads V1-4 (Fig. 1). Laboratory tests revealed elevated levels of γGT, alkaline phosphatase, and bilirubin, along with a mild increase in fasting glucose. The patient referred a year-long abdominal pain, nausea and dyspepsia treated with esomeprazole without symptoms relief. In addition, the patient referred a 4 kg weight loss. Mild smoking habit. The patient family history is significant for early-onset of ischemic heart disease. The patient denied history of chest trauma or Kawasaki disease.
Fig. 1.
Electrocardiographic evaluation at first consultation
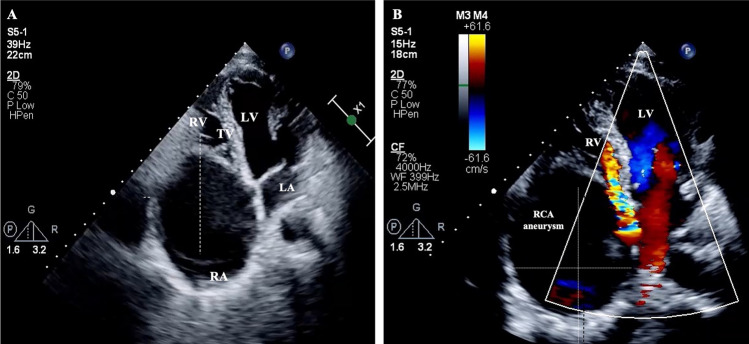
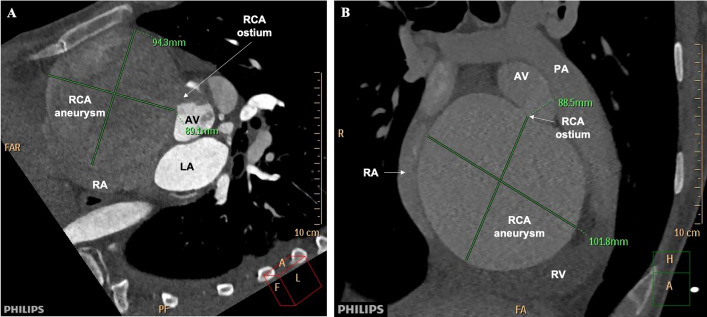
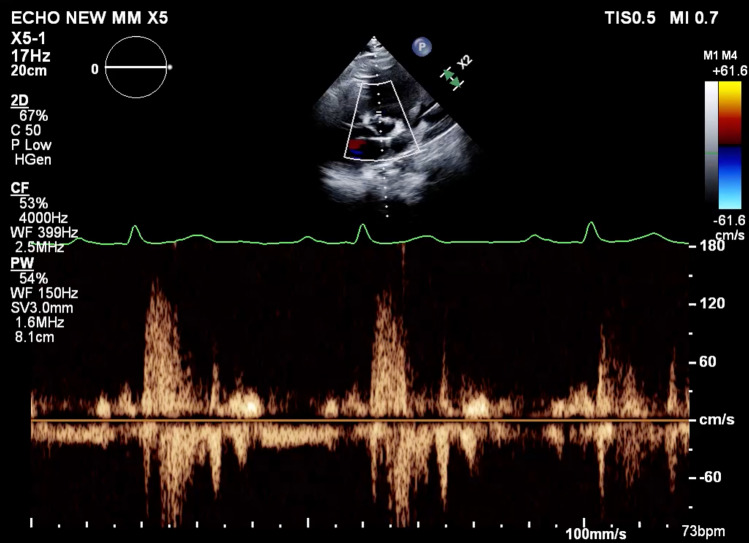
The patient was transferred to the Emergency Department for immediate cardiac echocardiography and computed tomography (CT) evaluation. Initial echocardiographic assessment showed extrinsic compression of the right atrium (RA) and ventricle (RV) (Fig. 2A). Additional findings included, reduced left ventricular (LV) size and mild global LV systolic dysfunction, with a left ventricular ejection fraction (LVEF) of less than 50%, mild RV diastolic dysfunction, mild to moderate tricuspid regurgitation, and mild pulmonary hypertension (Fig. 2B). The echocardiographic evaluation showed an oval-shaped hypoechoic structure suggestive of a pericardial cyst. Subsequently, CT angiography revealed giant right coronary artery (RCA) aneurysm, measuring up to 10.2 × 9.8 cm, in transverse and anteroposterior dimensions, respectively (Fig. 3A). The RCA collaterals from the left coronary system and the left coronary arteries were normal by CT angiography. Reference RCA measured both proximal and distal to the aneurysm was significantly narrowed due to compression by the aneurysm (< 3.0 mm), a large ostial RCA was also observed. The RCA aneurysm caused a significant mass effect with compression of the right atrium and right ventricle (Fig. 3B). Interestingly, pressure waves, carried with a 4F JR4 catheter, were similar to aortic pressures (Fig. 4). Small pericardial effusion was also observed.
Fig. 2.
Echocardiographic assessment of A apical 4 chamber demonstrating RA aneurysm compression. B Apical four-chamber color Doppler inflow of mitral and tricuspid valves demonstrating high velocity flow through tricuspid valve distorted by the RCA aneurysm. RA, right atrium. LA, left atrium. RV, right ventricle. LV, left ventricle. TV, tricuspid valve. RCA, right coronary artery
Fig. 3.
Preoperative Computed Tomography Angiography of the aneurysm. A Short axis view of the base of the heart in the arterial phase of contrast injection demonstrating the ostium of the RCA with non-enhanced blood backflow into the aorta and partially enhanced RCA aneurysm compressing the right atrium. B Short axis view at the level of the bifurcation of the pulmonary artery in venous phase demonstrating homogenous enhancement of large RCA aneurysm compressing and distorting the right atrium and ventricle. RV, right ventricle. LA, left atrium. RA, right atrium. TV, tricuspid valve. AV, aortic valve. PA, pulmonary artery. RCA, right coronary artery
Fig. 4.
Parasternal long axis pulse wave Doppler at the ostium of the RCA demonstrating systolic flow into the large aneurysm
Upon evaluation by the cardiac team, it was determined that percutaneous coronary intervention and stenting was not feasible due to the size of the RCA aneurysm, the high risk of rupture, ostial location and the ill-defined anatomy of the proximal part of RCA based on cardiac CT, coronary angiography and Cardiac Gated CTA. In addition, the right PDA branch was also small and narrowed with collaterals from the left system, unfit for a grafting upon assessment by the cardiac CT and coronary angiography. Therefore, the patient was referred for aneurysmectomy. Prior to surgery, regular blood pressure monitoring and anxiety treatment was implemented. For adequate cardiac surgery and aneurysm decompression a mild hypothermic femoral bicaval cardiopulmonary bypass was performed. Intraoperative findings confirmed the presence of a giant aneurysm (Fig. 5). Elective aneurysm resection was followed by closure of the right coronary sinus and RCA ligation at the proximal and distal ends. The right coronary ostium was dilated and oval-shaped. The ostium was closed primarily from within the root with a few 5–0 Prolene sutures and externally with 4–0 pledgeted sutures. No RCA bypass graft distal to the right coronary artery was required due to adequate collaterals from the left system to the distal RCA. Myocardial protection was achieved through antegrade and retrograde custodiol cardioplegia. Histopathologic examination of the aneurysm revealed a 2 mm thick coronary wall, hyalinization and obliteration of the vascular wall, severe calcified atherosclerotic plaques, mild focal chronic inflammation, and a fibrin thrombus. Echocardiographic evaluation immediately after surgery showed normal LV size and function with a calculated LVEF of 65%. Severe RA dilatation, moderate RV dysfunction, tricuspid regurgitation and mild elevated pulmonary artery pressure persisted after surgery. Minimal pericardial effusion and bilateral pleural effusion was also noted. The pharmacological management included diuretics, nonsteroidal anti-inflammatory drugs and statins. Two months after surgery, echocardiographic assessment indicated normal left and right ventricle function and size, mild increase in left and right atrial size, mild tricuspid regurgitation and pulmonary hypertension. The patient is currently doing well and remains asymptomatic.
Fig. 5.
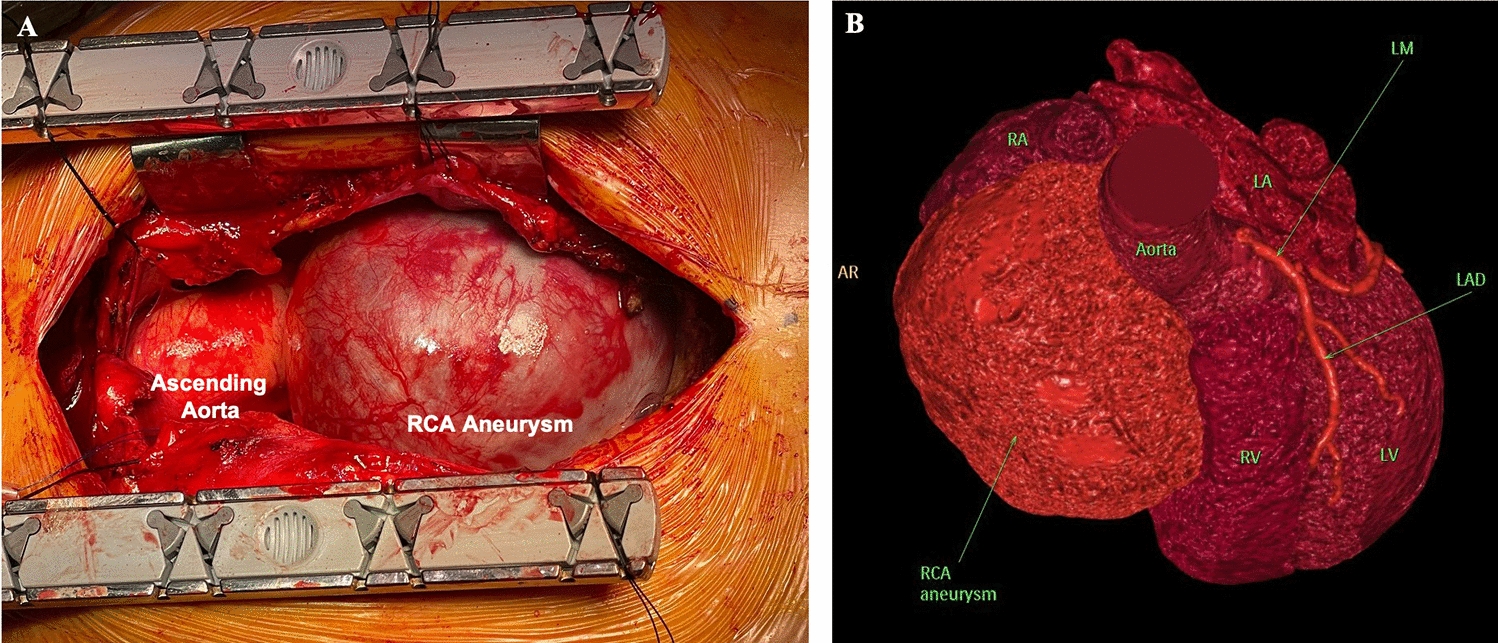
A Intraoperative Intact mid–right coronary artery giant aneurysm. RCA, right coronary artery. B 3D rendering of the heart demonstrating normal left coronary system and aneurysmatic right coronary artery compressing the right atrium and ventricle. Normal left coronary system. RA, right atrium. LA, left atrium. RV, right ventricle. LV, left ventricle. RCA, right coronary artery. LM, left main coronary artery. LAD, left anterior descending artery
Discussion
In our patient, RCA pressure measurements were identical to the systemic aortic pressure wave increasing the risk of rupture. In addition, pulmonary hypertension was observed secondary to aneurysm compression of both chambers which remained upon aneurysm resection. The patient underwent surgical aneurysmectomy which resulted in improved ventricular function.
At present, management options include pharmacological treatment with antiplatelet and anticoagulant agents, percutaneous intervention, and surgical treatment, despite no existing guidelines for the management of giant coronary aneurysm [5]. Coronary angiography remains the gold standard technique to evaluate size, shape, location of the aneurysms, as well as the degree of coronary atherosclerotic plaque formation [5].
This case highlights the challenges associated with the management of giant coronary artery aneurysms. Optimal management strategies and outcomes for such rare cardiovascular conditions implies the need for standardised management guidelines.
Abbreviations
- CAA
Coronary artery aneurysm
- CAD
Coronary artery disease
- CCT
Computed tomography, right coronary artery
Author contributions
A.O, data acquisition. E.G-C, conception and design, revision E.S, image acquisition. X.P, and M.K, image acquisition. Y.BG, supervision. All authors have read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Patient consented for participation in research.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.AbouSherif S, OzdenTok O, Taşköylü Ö, Goktekin O, Kilic ID. Coronary artery aneurysms: a review of the epidemiology, pathophysiology, diagnosis, and treatment. Front Cardiovasc Med. 2017;5(4):24. 10.3389/fcvm.2017.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crawley PD, Mahlow WJ, Huntsinger DR, Afiniwala S, Wortham DC. Giant coronary artery aneurysms: review and update. Tex Heart Inst J. 2014;41(6):603–8. 10.14503/THIJ-13-3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keyser A, Hilker MK, Husser O, Diez C, Schmid C. Giant coronary aneurysms exceeding 5 cm in size. Interact Cardiovasc Thorac Surg. 2012;15(1):33–6. 10.1093/icvts/ivs111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maiodna E, Azoury F, Chand M, Bunting L, Rosman HS, Yamasaki H. Giant right coronary artery aneurysm: an association with primary varicose veins? JACC Case Rep. 2020;2(8):1196–9. 10.1016/j.jaccas.2020.05.064.PMID:34317447;PMCID:PMC8311881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawsara A, Núñez Gil I, Alqahtani F, et al. Management of coronary artery aneurysms. J Am Coll Cardiol Intv. 2018;11(13):1211–23. 10.1016/j.jcin.2018.02.041. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.