Abstract
Background
With advancements in imaging testing and surgical procedures, an increasing number of nodules with smaller diameters and deeper locations have been deemed suitable for surgical intervention. The preoperative localization of these nodules has become essential. In this retrospective single-center study, we aimed to compare the effectiveness and patient comfort associated with the use of a four-hook needle versus a hook-wire needle for preoperative localization. Additionally, we sought to evaluate the impact of different patient postures on localization effectiveness.
Methods
We retrospectively analyzed the data of 692 patients following preoperative CT-guided localization. The patients were categorized into different groups based on the type of localization needles used and their respective postures during localization.
Results
There was no statistical difference in total complications between the four-hook needle group and the hook-wire needle group (P > 0.05). The chest pain score in the four-hook needle group was lower than the hook-wire needle group (P = 0.001). The incidence of decoupling in the four-hook needle group was significantly lower than the hook-wire needle group (P < 0.05). The four-hook needle group had better performance in terms of localization operation time, operation time, intraoperative bleeding and first-day drainage (P < 0.05). Compared with the supine and lateral groups, the prone posture group had better performance in total complications and localization operation time, and worse performance in decoupling and chest pain (P < 0.05).
Conclusions
The four-hook needle has better effectiveness on localization and comfort in patient than the hook-wire needle, which is worthy of clinical promotion and application. The patient’s different postures during localization procedure may affect the localization results.
Keywords: Four-hook needle, Hook-wire needle, Localization postures, Pulmonary nodules, Preoperative localization
Introduction
With the increasing clinical application of low-dose computed tomography (LDCT) imaging, more microscopic pulmonary nodules can be detected at an early stage [1]. Although most of the pulmonary nodules are considered benign, there is an increasing number of malignant pulmonary nodules being detected by LDCT [2]. Advances in imaging testing and surgical procedures have led to an increase in the identification of smaller diameter and deeper located nodules that require surgical intervention. However, many of these pulmonary nodules are very difficult to palpate during video-assisted thoracic surgery (VATS). Therefore, preoperative localization has become a key step [3], including methods such as methylene blue, barium, intraoperative ultrasonography, and the increasingly utilized localization needles [4–6].
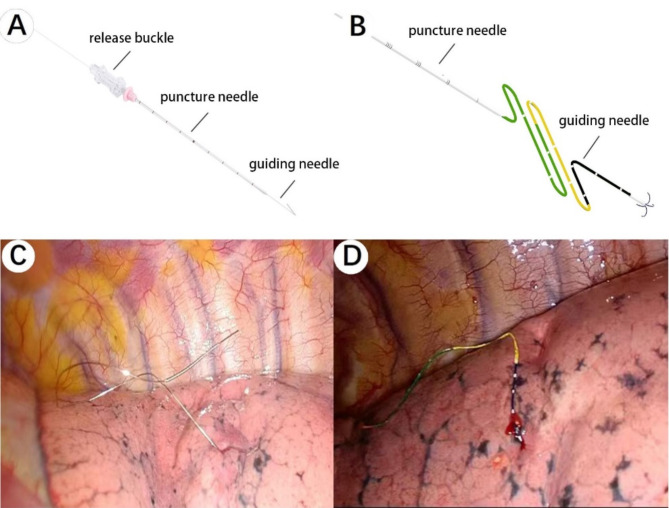
Localization needles are primarily divided into hook-wire needle and four-hook needle, which can be operated under CT guidance. The head of the needles anchor near the pulmonary nodule with the tail exposed on the surface of the lung parenchyma [7]. This facilitates both the surgeon’s determination of approximate nodule location during VATS and allows for easier specimen location determination by pathologists [8, 9]. The schematic diagram of the two localization needles is shown in Fig. 1A-B.
Fig. 1.
Intraoperative situation of localization device. A: Schematic diagram of hook-wire needle; B: Schematic diagram of four-hook needle; C: Intraoperative picture after localization of hook-wire needle; D: Intraoperative picture after localization of four-hook needle;
At the beginning of VATS, two types of localization needles can be found on the surface of lung parenchyma as shown in Fig. 1C-D. In recent years, there has been a shift towards using four-hook needle over hook-wire needle for CT-guided preoperative localization due to studies showing that hook-wire needle may cause severe pain and is prone to displacement or decoupling [4, 10–12]. This study aims to investigate differences between four-hook needle and hook-wire needle in terms of effectiveness and patient comfort using new reference indicators. Additionally, we seek to verify whether patient posture during localization has any effect on effectiveness and comfort levels.
Information and methodology
General information
This is a retrospective study including 1237 hospitalized patients with pulmonary nodules who underwent VATS in the Department of Thoracic Surgery of Hebei General Hospital from August 2017 to May 2023. Exclusion Criteria are as follows: (1) Patients without preoperative localization; (2) Incomplete imaging data; (3) Patients with underlying diseases that increase the risk of localization, such as pneumothorax, pleural effusion, pleural adhesions, and pulmonary fibrosis. A total of 692 patients were enrolled, of whom 235 (34.0%) were men and 457 (66%) women. The average age was 56 years and the average pulmonary nodule diameter was 8.5 mm. According to the different localization methods, patients were divided into hook-wire group (n = 256) and four-hook group (n = 436). According to the different postures of patients at the time of localization, they were divided into supine group (n = 105), lateral group (n = 338) and prone group (n = 199).
Instruments and materials
X-ray computerized tomography equipment (SOMATOM Definition Flash, Siemens AG, Germany). Hook-wire needle (Bard Healthcare Science (Shanghai) Ltd., Shanghai, China), composed of puncture needle, guiding needle (single barb structure and metal tail), pusher, release buckle, and protection tube. Four-hook needle (Ningbo Sheng Jie Kang Biological Technology Co., Ltd., Ningbo, China), composed of puncture needle, guiding needle (tri-colored suture and four-hook anchor), pusher, release buckle, and protection tube. Both puncture needles are constructed from medical-grade stainless steel featuring a centimeter scale measuring a total length of 9 centimeters. The tri-colored suture is non-absorbable medical suture where different colors indicate different depths in the localization process. The four-hook anchor is made of nickel-titanium memory alloy wire.
Localization procedure
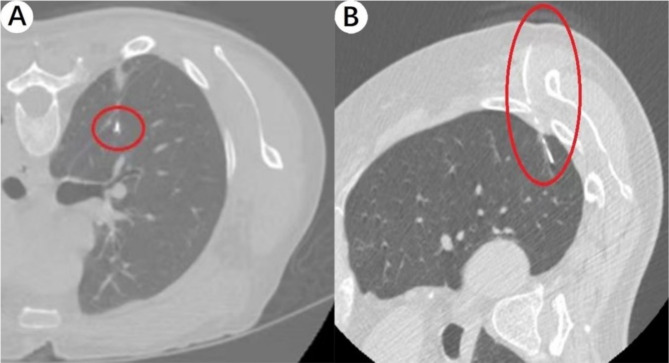
In this study, chest CT was performed using Siemens 64-slice dual-source CT (Somatom Definition) by experienced professional radiologists. The technical parameters used for the Siemens 64-slice dual-source CT were as follows: a collimator thickness of 0.6 mm and an interlayer space of 1 mm. After obtaining the chest CT images, the doctors from the Department of Thoracic Surgery at Hebei General Hospital conducted the clinical operation. The three doctors involved in this study had completed at least 100 preoperative localization cases before. Based on the preoperative CT images, an appropriate position range was determined, and localization markers were placed on the body surface. A CT scan was then performed to determine the insertion position and depth. Local infiltration anesthesia was administered after routine disinfection. The needle was guided by CT through the chest wall and pleura into lung tissue near the nodule. Generally, we chose to locate either upper or lower layers of the pulmonary nodule, and anchored its inner core head using a releaser before withdrawing it. A subsequent CT review was conducted to complete the localization process. VATS was performed on the same day after localization. The CT performance of four-hook needle and hook-wire needle after localization is shown in Fig. 2A-B.
Fig. 2.
CT performance after localization. A: CT performance after localization of four-hook needle; B: CT performance after localization of hook-wire needle;
Statistical indicators
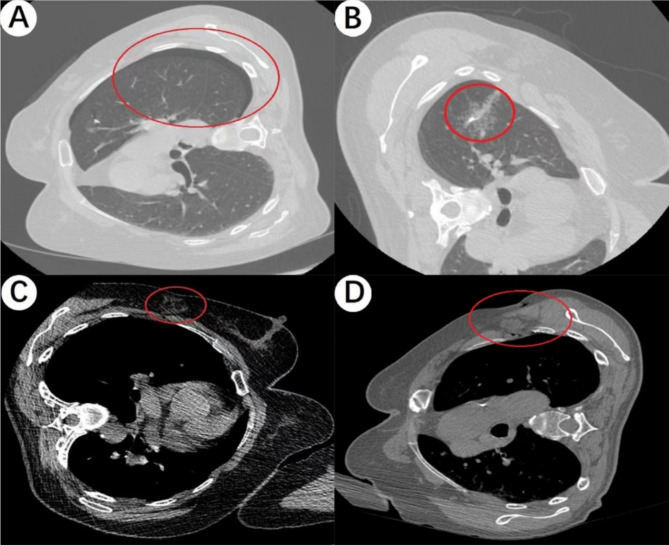
We collected data on localization-related complications, decoupling, localization operation time, chest pain scores, operation time, intraoperative bleeding, and first-day drainage. Decoupling was defined as the localization needle being found in the chest cavity but not attached to the lung parenchyma or significantly displaced during VATS. Localization-related complications were categorized as subcutaneous and intrathoracic complications, including hemorrhage and pneumothorax. Subcutaneous hemorrhage and subcutaneous emphysema were identified as visible near the needle on CT images at the time of localization (Fig. 3A-B). Additionally, parenchymal hemorrhage and pneumothorax were defined as those near the needle on CT images (Fig. 3C-D). Localization operation time referred to the duration from the first recorded CT scan to the last one. Operation time was defined as the total duration of the VATS procedure. First-day drainage referred to the amount of drainage from all indwelling drains placed during VATS within the first day after surgery. Each patient’s pain level was assessed by a nurse using a visual pain scale ranging from 0 (no pain) to 10 (most severe pain) following localization.
Fig. 3.
Associated complications are shown on CT images after localization. A: Pneumothorax on CT image after localization. B: Parenchymal hemorrhage on CT image after localization. C: Subcutaneous hemorrhage on CT image after localization. D: Subcutaneous emphysema on CT image after localization
Statistical methods
The statistical analysis was conducted using SPSS 26.0 software. The count data was presented as the number of cases and percentage (%), and analyzed using the chi-square test. All metrological data in this study were analyzed as non-normal distributions using the Mann-Whitney U test and the Kruskal-Wallis test. A significance level of P < 0.05 was considered statistically significant.
Results
Results related to the localization procedure
In relation to complications, the four-hook group had 171 cases (39.2%) of subcutaneous complications, 106 cases (24.3%) of intrathoracic complications, and a total of 232 cases (53.2%) with complications. The hook-wire group had 111 cases (43.4%) of subcutaneous complications, 75 cases (29.3%) of intrathoracic complications, and a total of 152 cases (59.4%) with complications. There was no significant difference in the incidence of complications between the two groups (P > 0.05). Specifically, in the four-hook group there were 56 cases (12.8%) of pneumothorax, 51 cases (11.7%) of parenchymal hemorrhage, 88 cases (20.2%) of subcutaneous hemorrhage, and 107 cases (24.5%) of subcutaneous emphysema, while in the hook-wire group there were 49(9.2%), 31(11.8%), 74(28.9%) and 58(22.7%) cases respectively for pneumothorax, parenchymal hemorrhage, subcutaneous hemorrhage, and subcutaneous emphysema. There were significant differences in subcutaneous hemorrhage and pneumothorax between the two groups (P < 0.05), while parenchymal hemorrhage and subcutaneous emphysema showed no statistical difference (P > 0.05). The localization operation time was recorded as being on average 9 min (range:7–11) in the four-hook group compared to 10 min (range:8–14) in the hook-wire group which showed a statistically significant difference (P = 0 0.001). Additionally, the chest pain score was lower in the four-hook group at an average of 2 (range:1–3) compared to 3 (range:2–5) in the hook-wire group with a significant statistical difference (P = 0.001). The results related to the localization procedure are shown in Table 1.
Table 1.
Operation related parameters of the two groups
| Variables | Hook-wire(n = 256) | Four-hook (n = 436) |
P |
|---|---|---|---|
|
Subcutaneous hemorrhage Subcutaneous emphysema |
74(28.9%) 58(22.7%) |
88(20.2%) 107(24.5%) |
0.009 0.574 |
| Parenchymal hemorrhage | 31(12.1%) | 51(11.7%) | 0.871 |
|
Pneumothorax Subcutaneous complications Intrathoracic complications Total complications localization operation time(min) Chest pain scores |
49(19.1%) 111(43.4%) 75(29.3%) 152(59.4%) 10(8–14) 3(2–5) |
56(12.8%) 171(39.2%) 106(24.3%) 232(53.2%) 9(7–11) 2(1–3) |
0.026 0.285 0.150 0.115 0.001 0.001 |
Results related to VATS
There were 22 (5.0%) decoupling patients in the four-hook group and 25 (9.7%) in the hook-wire group, ndicating a significant difference between the two groups (P < 0.05). The median operation time in the four-hook group was 84 (65-138.75) minutes, compared to 100 (65–170) minutes in the hook-wire group, which was statistically different between the two groups (P < 0.05). The median intraoperative bleeding was 10 (10–20) ml in the four-hook group and 12 (10–50) ml in the hook-wire group, with a significant difference (P = 0.001). The median first-day drainage was 125 (80–200) ml in the four-hook group, and 175 (100–275) ml in the hook-wire group, with statistical differences between the two groups (P = 0.001). The results related to VATS are shown in Table 2.
Table 2.
Surgery related parameters of the two groups
| Variables | Hook-wire n = 256 |
Four-hook n = 436 |
P |
|---|---|---|---|
|
Decoupling operation time(min) |
25(9.7%) 100(65–170) |
22(5.0%) 84(65-138.75) |
0.017 0.016 |
| intraoperative bleeding(ml) | 12(10–50) | 10(10–20) | 0.001 |
| first-day drainage(ml) | 175(100–275) | 125(80–200) | 0.001 |
Results related to different postures
There were 69 (65.7%), 227 (58.5%) and 88 (44.2%) cases in the supine group, lateral group and prone group, respectively. The results showed significant differences in total complications among the three groups (P = 0.001). The median localization operation time was 9(8–11) in the supine group, 9(7–13) in the lateral group, and 9(7–11) in the prone group, with statistical differences among groups (P < 0.05). The median chest pain scores also showed statistically significant differences (P = 0.001), which were 2(1–3), 2(1–3), and 4(2–5) in the supine, lateral and prone groups respectively. There were 7 (6.7%), 18 (4.6%) and 22 (11.1%) decoupling cases in the three groups, with statistical differences (P < 0.05). There were no statistically significant differences in operation time, intraoperative bleeding, and first-day drainage among the supine, lateral and prone groups (P > 0.05). Results related to different postures are shown in Table 3.
Table 3.
Posture related parameters of the three groups
| Variables | Supine n = 105 |
Lateral n = 388 |
Prone n = 199 |
P |
|---|---|---|---|---|
|
Total complications localization time(min) Chest pain scores |
69(65.7%) 9(8–11) 2(1–3) |
227(58.5%) 9(7–13) 2(1–3) |
88(44.2%) 9(7–11) 4(2–5) |
0.001 0.035 0.001 |
|
Decoupling operation time(min) |
7(6.7%) 85(60–145) |
18(4.6%) 90(67.5–150) |
22(11.1%) 85(65–139) |
0.014 0.356 |
| intraoperative bleeding(ml) | 10(10–30) | 10(10–30) | 10(10–20) | 0.673 |
| first-day drainage(ml) | 145(75–220) | 150(100–225) | 150(90–250) | 0.491 |
Discussion
Lung cancer is one of the most prevalent forms of cancer, with the number of deaths from lung cancer on the rise [13]. VATS is currently the main effective treatment for lung cancer [14]. With advances in imaging testing and surgical procedures, there has been an increase in the surgical indications for nodules with smaller diameters and deeper locations. Preoperative localization has become a crucial step for VATS, with localization needles being the most commonly used method by thoracic surgeons. In the past few years, hook-wire needle was widely utilized for CT-guided localization prior to VATS. However, studies have shown that the hook-wire needle has significant disadvantages such as causing patient discomfort and decoupling. As a result, the four-hook needle has emerged and been widely used these years. Depending on the location of the patient’s pulmonary nodule and the clinician preference, patients are generally positioned in one of three postures for localization: supine, lateral, r prone.
In this study, we conducted a retrospective analysis depending on two types of localization needles and three different postures. New reference indicators were utilized to include overlooked factors such as increased subcutaneous complications. Previous studies typically used total drainage as a reference indicator [15], but this measure varied depending on when drainage tubes were removed and could greatly affect results. Therefore, we changed our reference indicator to focus on first day drainage as it better represents surgical trauma compared to total drainage measurements.
The results indicated that while there was no significant difference between the two groups in the overall incidence of complications, the use of a four-hook needle was associated with a lower likelihood of specific complications such as subcutaneous hemorrhage (20.2%) and pneumothorax (12.8%), compared to the hook-wire needle (28.9% and 49.1%, P < 0.05). Previous studies have also reported lower complication rates with the four-hook needle compared to the hook-wire needle [11]. Both localization needles generally exhibit similar performance during localization procedures, causing minimal damage to the thoracic cage and lung parenchyma due to their small size. Therefore, our results are considered credible.
Furthermore, our study revealed that chest pain scores were lower in the four-hook group than in the hook-wire group, and that decoupling occurred less frequently in the former group than in the latter. The hook-wire needle features a single barb structure with a metal tail which may lead to higher decoupling rates and increased pain due to movement of its head part or exposure of its skin surface portion. On the contrary, the head of the four-hook needle is deposed of 4 small metal hooks which provide more secure anchoring within lung tissue, reducing decoupling occurrences. Additionally, its linear tail structure with markings can be easily constricted into the chest cavity, thereby minimizing chest pain.
The four-hook group demonstrated a shorter time of localization and operation procedure, as well as less intraoperative bleeding and first-day drainage compared to the hook-wire needle group in our study. As a retrospective study, we observed that hook-wire needles were predominantly used in earlier years, while the four-hook needles were primarily utilized in recent years. The variations in the reference data mentioned above may be attributed to the improvement of technical proficiency among clinicians. However, it is unclear whether the differences are due to variances in localization hooks or clinician surgical proficiency, and this aspect is not further discussed in this study, which represents a limitation of our research.
In this study, we conducted an investigation into the impact of different patient postures on the localization results for the first time. Our findings revealed that body posture did indeed affect the localization results in certain aspects. The analysis indicated significant variations in total complications among the three groups, with a lower incidence observed in the prone posture group compared to the other posture groups. Additionally, it was found that the prone group had a shorter localization operation time than the other groups. However, it is worth noting that individuals in the prone group reported stronger chest pain and a higher incidence of decoupling compared to those in other groups. This may be attributed to the more drastic change in posture after localization, as well as potential friction in the tail of the device when lying flat before operation. When assuming a prone posture, the puncture point is located on the back, which has more muscles. Passing through denser muscles may result in less bleeding and emphysema than passing through loose fatty tissue, but it may also cause more intense pain. There were no statistically significant differences among the three groups in terms of operation time, intraoperative bleeding, and first-day drainage. The complications associated with localization are generally not severe. Therefore, in order to achieve a lower incidence of pain and decoupling, clinicians can appropriately select the prone posture or a more suitable lateral posture during localization based on patient-specific factors.
There are certain limitations in this study. Firstly, it is important to note that this is a retrospective study and as such, it may not have been able to fully account for the influence of other factors on the results. Additionally, it should be noted that this is a single-center study. Therefore, further validation of our findings would necessitate prospective and large-scale multicenter studies.
Conclusions
The four-hook needle demonstrates superior effectiveness in terms of localization and patient comfort compared to the hook-wire needle, making it a worthy candidate for clinical promotion and application. It is important to note that the patient’s different postures during the localization procedure may have an impact on the accuracy of the localization results.
Acknowledgements
Not applicable.
Author contributions
WZM, LB, DGC and XX completed the main design and conception of the study. ZHF, ZXP, and XWF complete the collection of clinical data. WZM and ZHZ complete the collection of data. ZHF and ZXP collected the pathological data of patients. ZQT and HZH integrate the data. WZM, ZHZ, and XWF analyze and interpret the data. LB processes the data graphics. WZM and HZH drafted the first draft of the article, and DGC and XX made final revisions to the article. All authors have read and approved the final manuscript.
Funding
This research was funded by the Key Research and Development Program of Hebei Province (grant no. 22377790D).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Hebei General Hospital (no. 2023140). Retrospective information was recorded by the Hebei General Hospital Medical Record System, which dispensed with the requirement for informed patient consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zengming Wang, Bin Li, Guochen Duan and Shun Xu contributed equally to this work.
Contributor Information
Guochen Duan, Email: duanguoc@126.com.
Shun Xu, Email: xushuncmu@sina.com.
References
- 1.Yoshida R, Yoshizako T, Tanaka S, et al. CT-guided color marking of impalpable pulmonary nodules prior to video-assisted thoracoscopic surgery. Clin Imaging. 2021;74:84–8. 10.1016/j.clinimag.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Y S, F X, W Z, H H, T C, Q L. Multiclassifier fusion based on radiomics features for the prediction of benign and malignant primary pulmonary solid nodules. Annals Translational Med. 2020;8(5). 10.21037/atm.2020.01.135 [DOI] [PMC free article] [PubMed]
- 3.Liu B, Gu C. Expert consensus workshop report: guidelines for preoperative assisted localization of small pulmonary nodules. J Cancer Res Ther. 2020;16(5):967–73. 10.4103/jcrt.JCRT_449_20. [DOI] [PubMed] [Google Scholar]
- 4.Lin MW, Tseng YH, Lee YF, et al. Computed tomography-guided patent blue vital dye localization of pulmonary nodules in uniportal thoracoscopy. J THORAC CARDIOV SUR. 2016. 10.1016/j.jtcvs.2016.04.052. 152 J THORAC CARDIOV SUR. [DOI] [PubMed] [Google Scholar]
- 5.Lee NK, Park CM, Kang CH, et al. CT-Guided percutaneous transthoracic localization of pulmonary nodules prior to video-assisted thoracoscopic surgery using Barium suspension. Korean J Radiol. 2012;13(6):694–701. 10.3348/kjr.2012.13.6.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kondo R, Yoshida K, Hamanaka K, et al. Intraoperative ultrasonographic localization of pulmonary ground-glass opacities. J Thorac Cardiovasc Surg. 2009;138(4):837–42. 10.1016/j.jtcvs.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Xue X, Tian F, Tang J et al. Comparison of Four-hook Needle and Memory Alloy Coil in Localization of Pulmonary Nodules. Zhongguo Fei Ai Za Zhi. 2021; 24 Zhongguo Fei Ai Za Zhi. 10.3779/j.issn.1009-3419.2021.102.30 [DOI] [PMC free article] [PubMed]
- 8.Finley RJ, Mayo JR, Grant K, et al. Preoperative computed tomography–guided microcoil localization of small peripheral pulmonary nodules: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. 2015;149(1):26–32. 10.1016/j.jtcvs.2014.08.055. [DOI] [PubMed] [Google Scholar]
- 9.Qiang Y, Zhang L, Yang N, et al. Diagnostic and therapeutic value of computed tomography guided coil placement after digital subtraction angiography guided video-assisted thoracoscopic surgery resection for solitary pulmonary nodules. Transl Lung Cancer Res. 2015;4(5):598–604. 10.3978/j.issn.2218-6751.2015.08.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iguchi T, Hiraki T, Gobara H, et al. CT fluoroscopy-guided preoperative short hook wire placement for small pulmonary lesions: evaluation of safety and identification of risk factors for pneumothorax. Eur Radiol. 2016;26(1):114–21. 10.1007/s00330-015-3815-z. [DOI] [PubMed] [Google Scholar]
- 11.Zhang X, Tsauo J, Tian P et al. Randomized comparison of the four-hook anchor device and hook-wire use for the preoperative localization of pulmonary nodules. J Thorac Cardiovasc Surg Published Online June 2023:S0022522323004592. 10.1016/j.jtcvs.2023.05.034 [DOI] [PubMed]
- 12.Chen YR, Yeow KM, Lee JY, et al. CT-guided Hook Wire localization of Subpleural Lung lesions for Video-assisted thoracoscopic surgery (VATS). J Formos Med Assoc. 2007;106(11):911–8. 10.1016/S0929-6646(08)60061-3. [DOI] [PubMed] [Google Scholar]
- 13.The Lancet. GLOBOCAN 2018: counting the toll of cancer. Lancet. 2018;392(10152):985. 10.1016/S0140-6736(18)32252-9. [DOI] [PubMed] [Google Scholar]
- 14.Congregado M, Merchan RJ, Gallardo G, Ayarra J, Loscertales J. Video-assisted thoracic surgery (VATS) lobectomy: 13 years’ experience. Surg Endosc. 2008;22(8):1852–7. 10.1007/s00464-007-9720-z. [DOI] [PubMed] [Google Scholar]
- 15.Wang JL, Xia FF, Dong AH, Lu Y. Comparison between coil and hook-wire localization before video-assisted thoracoscopic surgery for lung nodules: a systematic review and meta-analysis. Wideochir Inne Tech Maloinwazyjne. 2022;17(3):441–9. 10.5114/wiitm.2022.116396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.