Abstract
Objectives
The aim of this bibliometric analysis was to highlight potential future areas for the practical application of research on rheumatic heart disease (RHD), considering past and current research efforts.
Methods
A systematic search was conducted in the WoSCC to find articles and reviews focused on RHD published between 2013 and 2024. Microsoft Excel 2019 was used to chart the annual productivity of research relevant to RHD, while ArcGIS (version 10.8) was employed to visualize the global distribution of publications. Analysis tools such as CiteSpace (version 6.1.R6) and VOSviewer (version 1.6.18) were utilized to identify the most prolific countries or regions, authors, journals, and resource-, intellectual-, and knowledge-sharing in RHD research, and to perform co-citation analysis of references and keywords. Additionally, the Bibliometrix R Package was used to analyze topic dynamics.
Results
From the search, a total of 2,428 publications were retrieved. In terms of countries or regions, the United States was the most productive country (566, 23.31%). As for institutions, most publications have been contributed by the University of Cape Town (149, 6.14%). Regarding authors, Jonathan R. Carapetis produced the most published works, and he received the most co-citations. The most prolific journal was identified as the International Journal of Cardiology (70, 2.88%). The study published in Circulation received the most co-citations. Keywords with ongoing strong citation bursts included “surgical treatment” and “valvular heart disease”.
Conclusion
Despite the rapid advancements in the field of RHD research, future efforts should prioritize strengthening collaboration among national institutions to facilitate information dissemination. Current research on RHD mainly focuses on prognosis of patients. While, the emerging research trends in RHD encompass treatment strategies for complications, including atrial fibrillation (AF), heart failure (HF), and infective endocarditis, as well as screening strategies for RHD and surgical interventions for patients with rheumatic mitral valve disease.
Keywords: Rheumatic heart disease, Bibliometric study, Atrial fibrillation, Heart failure, Surgical options
Introduction
Rheumatic heart disease (RHD) is the result of an autoimmune response triggered by Group A ß-hemolytic streptococcus, which is characterized as inflammatory-fibrotic injury in the cardiac valve [1]. This condition causes more than 10 million disability-adjusted life-years every year, accounting for most deaths from valvular heart disease worldwide [2]. As a neglected disease, it presents significant challenges for global health systems, particularly in low-income settings [3], causing a high disease burden. RHD can lead to severe adverse health outcomes, including heart failure (HF), cardioembolic stroke, and premature death [4]. Despite being eminently preventable, RHD remains the most common cause of cardiovascular disease and early mortality globally in children and young adults [5].
Currently, the clinical management of RHD faces numerous unresolved issues. In low- and middle-income countries, diagnosis primarily relies on echocardiography, more advanced diagnostic screening methods should be explored [6]. There are no definitive treatment guidelines for various complications associated with RHD, such as atrial fibrillation (AF), HF, and infective endocarditis [3]. Furthermore, for patients with rheumatic mitral valve stenosis, choosing whether valve replacement or valve repair provides more benefits requires meticulous evaluation [7].
To identify critical issues for future research, bibliometrics, an approach for examining academic publications, is widely used to comprehensively reveal the research status, features, evolution, and emerging trends in specific fields. Tools like CiteSpace and VOSviewer software, visualization analysis software for bibliometric analysis, automatically display interactive visual networks through analyzing records of scientific publications [8]. However, the bibliometric study on RHD remains a void. To fill this knowledge gap, this study aimed to conduct the first in-depth survey of RHD research over the past decade (2013 to 2024) via bibliometric analysis to uncover the difficult and pressing research issues related to this field, and provide new sights for future related research.
Methods
Data sources and searches
The Web of Science Core Collection (WoSCC) database is the most frequently used database in bibliometrics research and covers prestigious and influential journals, which are favoured by academic researchers [9, 10]. Thus, it was chosen to identify all pertinent publications in our study. Records related to RHD were extracted from the WoSCC database for the period from January 1, 2013, to May 31, 2024. Due to time constraints, the data for 2024 are still incomplete; therefore, the literature from 2024 has not been adequately represented in the analysis. To enhance indexing, search terms were derived from the Medical Subject Headings library and were developed in consultation with a medical librarian. The search strategy was as follows: TS = (“rheumatic heart disease” OR “rheumatic heart-disease” OR “rheumatic mitral” OR “rheumatic aortic” OR “rheumatic tricuspid” OR “rheumatic pulmonary” OR “bouillaud disease” OR “bouillauds disease”). Both research articles and reviews were considered invaluable for this study [11]. A language restriction was applied, considering only English-language publications. The retrieved electronic records were saved as plain text files and stored in download_txt format. In the process of article screening, the two researchers mainly screened articles independently without interfering with each other, excluding those papers that were not relevant to the topic or whose article type was not an article or review, to confirm the selected literature. Any disagreements between the paired researchers were resolved through discussing with the other researcher after reading all the articles.
Data analysis
Descriptive statistics were used to analyze the data. All identified documents were imported into CiteSpace (version 6.1.R6), and VOSviewer (version 1.6.18). We used CiteSpace to conduct collaboration analysis (of countries or regions, institutions), co-citation analysis of references, and burst detection of keywords. Using VOSviewer software, we performed visualization analysis of authors and co-cited authors, co-citation analysis of journals, and clustering analysis of keywords. The dynamics of topics were visualized using the Bibliometrix R Package. ArcGIS (version 10.8) was employed to visualize the global distribution of publications. The analysis function in the Web of Science database was used to summarize external characteristics, including the number of publications and citations each year. We employed the analysis function in Citespace, setting the unit of analysis to either “country” or “institution.” To enhance visualization clarity, we focused on countries or institutions with more than 20 publications. Additionally, we established the unit of analysis as “reference” and conducted cluster analysis on the references. In VOSviewer, we performed citation analysis, utilizing “authors” or “sources” as the unit of analysis, concentrating on those with more than 10 publications. Furthermore, we used the co-occurrence analysis function of VOSviewer, setting the unit of analysis to “all keywords.” In order to improve image clarity, we focused on keywords that appeared more than 30 times.
Results
The development trend of publication output
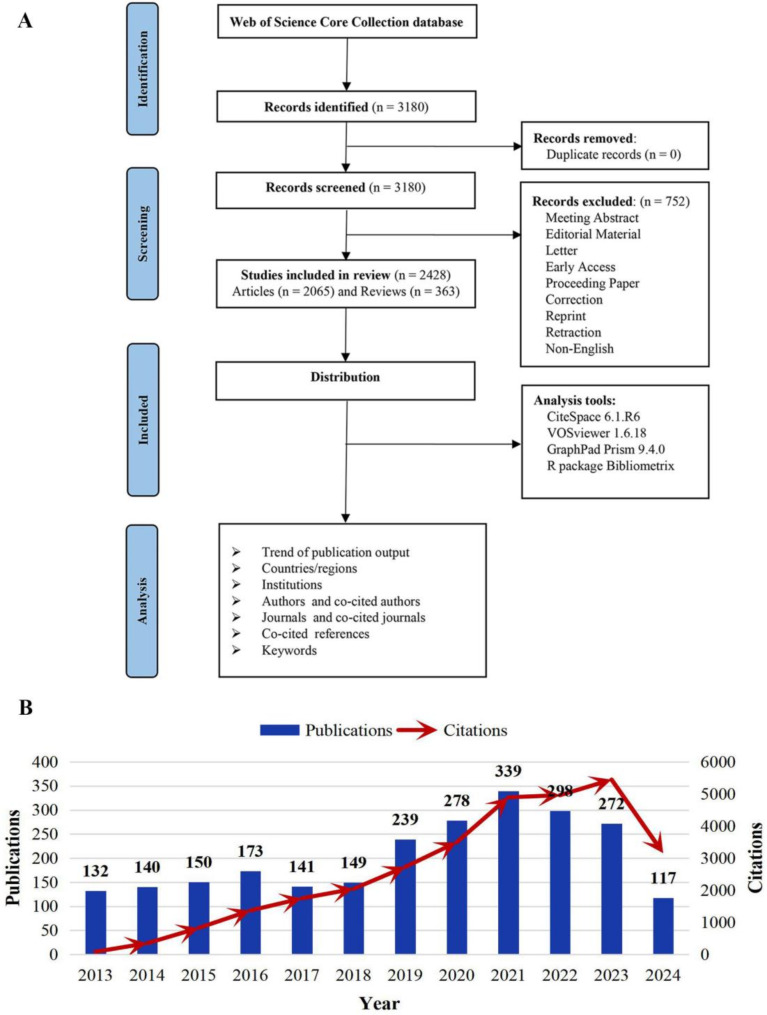
Our retrieval process, depicted in Fig. 1A, included 2428 publications concerning RHD published from 2013 to early 2024. Of these, 2065 were articles (85.05%), and 363 were reviews (14.95%). The number of annual publications reflected the development trend in this field (Fig. 1B). The output of publications showed a steady upward trend from 2013 to 2016, but the annual growth was relatively small. A significant rise in publications was noted from 2017 to 2021. However, there was no further breakthrough in the annual number of publications in the last two years. Correspondingly, citations steadily increased from 82 in 2013 to 4964 in 2022, and then surged to 5474 in 2023.
Fig. 1.
Literature search process, and the changes in the annual publication volume in this field. A Literature search and screening flowchart. B Trends in the growth of publications worldwide from 2013 to early 2024
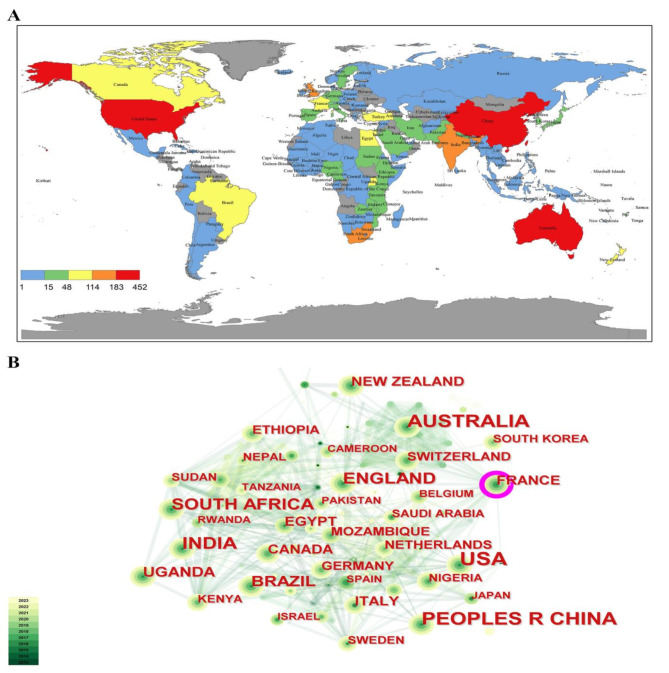
Distribution of countries/regions
In the past decade, 124 countries/regions have contributed to the research of RHD (Fig. 2A). The top three countries with the highest publication output were the United States (n = 566), Australia (n = 346) and China (n = 345), accounting for more than half of the total global publications (Table 1). South Africa, and India also made substantial contributions, each producing more than 200 articles. Nevertheless, since 2013, most countries have generated fewer than 10 publications, and some regions have yet contributed any research in this area (Fig. 2A).
Fig. 2.
The number of publications and co-occurrence network of countries/regions. A The geographical heat map of RHD-related publications. B The map of scientific research cooperation relationship between countries or regions
Table 1.
Top 10 productive countries regarding the research on RHD
| Rank | Country | Centrality | Count (%) | ACI* | H-index |
|---|---|---|---|---|---|
| 1 | USA† | 0.06 | 566 (23.31%) | 19.90 | 57 |
| 2 | Australia | 0.03 | 346 (14.25%) | 24.30 | 44 |
| 3 | China | 0.03 | 345 (14.21%) | 12.29 | 37 |
| 4 | South Africa | 0.01 | 308 (12.69%) | 33.01 | 36 |
| 5 | India | 0.04 | 200 (8.24%) | 19.56 | 30 |
| 6 | England | 0.08 | 155 (6.38%) | 26.54 | 38 |
| 7 | Brazil | 0.01 | 137 (5.64%) | 19.89 | 26 |
| 8 | Uganda | 0.09 | 102 (4.20%) | 24.48 | 24 |
| 9 | Turkey | 0.00 | 81 (3.35%) | 6.8 | 12 |
| 10 | France | 0.17 | 63 (2.59%) | 25.89 | 34 |
*ACI, average citations per item; †USA, the United States of America
The visual representation used circles to denote countries, with larger nodes indicating higher output. Lines between nodes represented collaborative ties, with thicker lines indicating closer cooperation. Purple-rimmed circles indicate the countries with high centrality, highlighting the significance of these countries in the network (Fig. 2B). The centrality of France and Uganda were 0.17, and 0.09 respectively, indicating that these countries established cooperation with many regions and played an important role in studying RHD. Of note, Turkey ranked high in the total amount of articles but low in the centrality. This may be related to the academic atmosphere in different countries and regions.
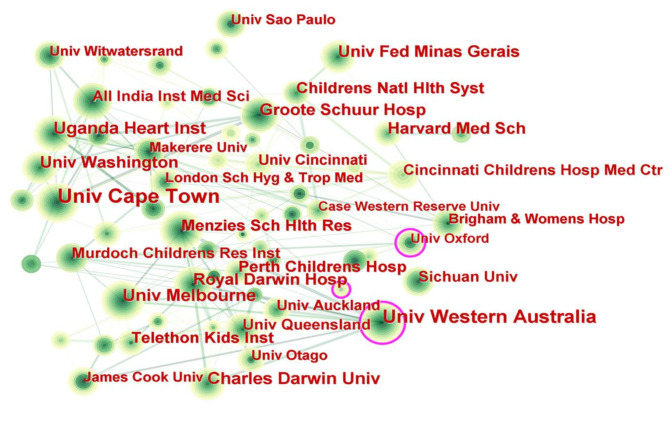
Distribution of institutions
Over the past decade, more than 500 institutions have successively carried out research on RHD (Fig. 3). Among them, the University of Cape Town (n = 149) was the most productive (Table 2), followed by the University of Western Australia (n = 147) and the Uganda Heart Institute (n = 71). More than one-third of the top ten institutions with the largest number of publications were from Australia. Regarding the cooperation between institutions, we found that institutions with higher centrality were primarily from Africa and North America, such as the University of Cape Town, the University of Washington, and Harvard Medical School, highlighting the extensive collaborative networks in these regions. In contrast, institutions like Royal Darwin Hospital, despite a high publication count, showed lower centrality and engaged primarily in internal cooperation, particularly with the University of Western Australia. Most institutions, however, were relatively dispersed in their collaborative networks.
Fig. 3.
Collaboration of institutions in the field of RHD
Table 2.
Top 10 productive institutions regarding the research on RHD
| Rank | Institution | Centrality | Count (%) | ACI* | H-index |
|---|---|---|---|---|---|
| 1 |
University of Cape Town (South Africa) |
0.10 | 149 (6.14%) | 41.51 | 36 |
| 2 | University of Western Australia (Australia) | 0.08 | 147 (6.05%) | 29.79 | 30 |
| 3 |
Uganda Heart Institute (Uganda) |
0.06 | 71 (2.92%) | 27.39 | 19 |
| 4 | Federal University of Minas Gerais (Brazil) | 0.04 | 68 (2.80%) | 22.35 | 17 |
| 5 |
Charles Darwin University (Australia) |
0.02 | 65 (2.68%) | 23.47 | 25 |
| 6 |
University of Melbourne (Australia) |
0.04 | 64 (2.64%) | 47.69 | 24 |
| 7 |
University of Washington (USA†) |
0.09 | 62 (2.56%) | 38.82 | 20 |
| 8 |
Harvard Medical School (USA) |
0.11 | 60 (2.47%) | 25.56 | 20 |
| 9 |
Royal Darwin Hospital (Australia) |
0.01 | 55 (2.27%) | 17.48 | 18 |
| 10 |
Groote Schuur Hospital (South Africa) |
0.06 | 48 (1.98%) | 41.94 | 27 |
*ACI, average citations per item; †USA, the United States of America
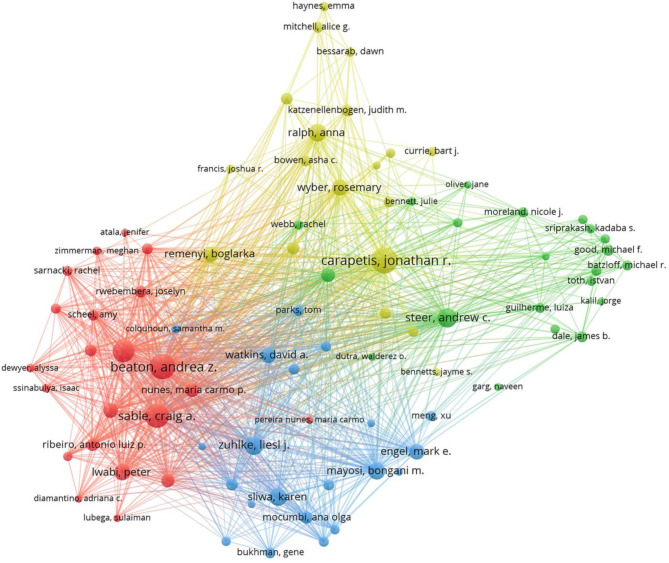
Authors and co-cited authors
A total of 11,476 authors have been involved in RHD research over the past decade. Table 3 details the top 10 most productive authors, with four from Australia, and three from South Africa. The most productive author was Jonathan R. Carapetis (n = 90) from the University of Western Australia, followed by Andrea Beaton (n = 76) from Cincinnati Children’s Hospital Medical Center, the United States and Craig A Sable (n = 75) from the Children’s National Health System, the United States. In line with closeness of connections, the collaboration of the top 88 most productive authors was divided into 4 clusters (Fig. 4). Co-cited authors are defined as those who are cited by one or more articles at the same time. Among the top 10 co-cited authors (Table 4), five authors were co-cited more than 500 times. Jonathan R. Carapetis (n = 1146) from the University of Western Australia ranked first, followed by Bo Remenyi (n = 634) from the Charles Darwin University in Australia.
Table 3.
Top 10 productive authors in the field of RHD
| Rank | Author | Institution (Country) | Documents | ACI* | H-index |
|---|---|---|---|---|---|
| 1 | Carapetis, Jonathan R | University of Western Australia (Australia) | 90 | 50.49 | 32 |
| 2 | Beaton, Andrea Z | Cincinnati Children’s Hospital Medical Center (USA†) | 76 | 39.68 | 21 |
| 3 | Sable, Craig A. | Children’s National Health System (USA) | 75 | 25.22 | 20 |
| 4 | Okello, Emmy | Uganda Heart Institute (Uganda) | 62 | 24.76 | 20 |
| 5 | Steer, Andrew C. | Royal Children’s Hospital Melbourne (Australia) | 47 | 61.89 | 24 |
| 6 | Zühlke, Liesl Joanna | University of Cape Town (South Africa) | 44 | 43,69 | 21 |
| 7 | Sliwa, Karen | University of Cape Town (South Africa) | 38 | 31.29 | 17 |
| 8 | Ralph, Anna | Charles Darwin University (Australia) | 38 | 22.06 | 17 |
| 9 | Mayosi, Bongani | University of Cape Town (South Africa) | 33 | 84.23 | 24 |
| 10 | Wyber, rosemary | University of Western Australia (Australia) | 32 | 32.55 | 15 |
*ACI, average citations per item; †USA, the United States of America
Fig. 4.
Cooperation network among the authors
Table 4.
Top 10 co-cited authors in the field of RHD
| Rank | Co-cited author | Institution (Country) | Co-citations | H-index |
|---|---|---|---|---|
| 1 | Carapetis, Jonathan R | University of Western Australia (Australia) | 1146 | 32 |
| 2 | Remenyi, Bo | Charles Darwin University (Australia) | 634 | 12 |
| 3 | Marijon, Eloi | Université Paris Cité (France) | 619 | 12 |
| 4 | Watkins, David | University of Washington (USA†) | 605 | 14 |
| 5 | Beaton, Andrea | Cincinnati Children’s Hospital Medical Center (USA) | 517 | 21 |
| 6 | Guilherme, Luiza | Universidade de São Paulo (Brazil) | 467 | 7 |
| 7 | Zühlke, Liesl Joanna |
University of Cape Town (South Africa) |
420 | 18 |
| 8 | Sliwa, Karen |
University of Cape Town (South Africa) |
380 | 15 |
| 9 | Steer, Andrew C | National Institutes of Health (USA) | 340 | 33 |
| 10 | Cunningham, Madeleine W. | University of Oklahoma Health Sciences Center (USA) | 288 | 15 |
†USA, the United States of America
Journals and co-cited academic journals
A total of 2428 articles concerning RHD were published in 757 journals, and the top 10 active journals were listed in Table 5. The International Journal of Cardiology ranked first in the publication output (n = 70, 2.88%), followed by Frontiers in Cardiovascular Medicine (n = 53, 2.18%) and the Cardiovascular Journal of Africa (n = 49, 2.02%). Among the top 10 journals, three are from the United States, and four are from the United Kingdom. Among these journals, 9 have impact factors below 5, and the majority of them are not categorized in JCR Q1, indicating that high-quality journals have paid less attention to the field of RHD.
Table 5.
Top 10 productive journals in the field of RHD
| Rank | Journal | Publications (%) | Country | IF# (2023) | SCImago journal rank | JCR* | H-index |
|---|---|---|---|---|---|---|---|
| 1 | International Journal of Cardiology | 70 (2.88%) | Ireland | 3.2 | 1.126 | Q2 | 146 |
| 2 | Frontiers in Cardiovascular Medicine | 53 (2.18%) | Switzerland | 2.8 | 0.863 | Q2 | 69 |
| 3 | Cardiovascular Journal of Africa | 49 (2.02%) | South Africa | 0.7 | 0.302 | Q4 | 42 |
| 4 | Cureus Journal of Medical Science | 46 (1.89%) | USA† | 1.0 | / | Q3 | / |
| 5 | Global Heart | 40 (1.65%) | The United Kingdom | 2.9 | 1.022 | Q2 | 46 |
| 6 | PloS ONE | 39 (1.61%) | USA | 2.8 | 0.839 | Q1 | 435 |
| 7 | BMC Cardiovascular Disorders | 37 (1.52%) | The United Kingdom | 1.9 | 0.646 | Q3 | 71 |
| 8 | Echocardiography–a journal of cardiovascular ultrasound and allied techniques | 36 (1.48%) | USA | 1.6 | 0.384 | Q3 | 57 |
| 9 | BMJ Open | 32 (1.32%) | The United Kingdom | 2.4 | 0.971 | Q1 | 160 |
| 10 | Heart | 30 (1.24%) | The United Kingdom | 5.1 | 1.736 | Q1 | 207 |
*JCR, Journal Citation Reports; #IF, Impact Factor; †USA, the United States of America
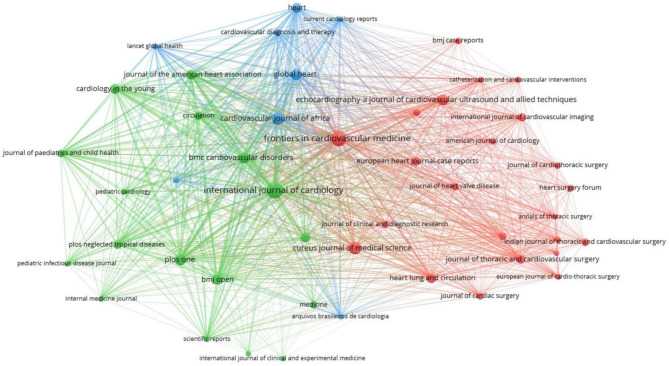
The number of citations of a journal indicates its influence in the research field, as shown in Fig. 5. According to the colour of cluster analysis, comprehensive medical periodicals such as Plos One and BMJ Open are all located in the green cluster; Academic journals in the field of heart research, such as Lancet Global Heart, and Heart are located in the blue cluster, while academic journals in the field of cardiac surgery research, such as the Journal of Thoracic and Cardiovascular Surgery, the Journal of Cardiac Surgery are located in the red cluster. In the top ten co-cited journals (Table 6), six have impact factors greater than 5, and all of these journals are classified as Q1. Among them, the Lancet has the highest impact factor, reaching 98.4, showing the high quality of articles related to RHD and the academic significance of this research.
Fig. 5.
VOSviewer network visualization map of the co-citation of journals
Table 6.
Top 10 co-cited journals in the field of RHD
| Rank | Journal | Citations | Country | IF# (2023) | SCImago journal rank | JCR* | H-index |
|---|---|---|---|---|---|---|---|
| 1 | Circulation | 4866 | USA† | 35.5 | 8.415 | Q1 | 570 |
| 2 | Journal of the American College of Cardiology | 2605 | USA | 21.7 | 8.762 | Q1 | 394 |
| 3 | Lancet | 2214 | The United Kingdom | 98.4 | 12.113 | Q1 | 700 |
| 4 | New England Journal of Medicine | 2091 | USA | 96.2 | 20.544 | Q1 | 933 |
| 5 | European Heart Journal | 2009 | The United Kingdom | 37.6 | 4.091 | Q1 | 265 |
| 6 | Heart | 1607 | The United Kingdom | 5.1 | 1.736 | Q1 | 165 |
| 7 | International Journal of Cardiology | 1369 | Ireland | 3.2 | 1.126 | Q2 | 108 |
| 8 | Journal of Thoracic and Cardiovascular Surgery | 1239 | USA | 4.9 | 1.744 | Q1 | 180 |
| 9 | American Journal of Cardiology | 1091 | USA | 2.3 | 0.950 | Q2 | 206 |
| 10 | PloS One | 1057 | USA | 2.9 | 0.839 | Q1 | 268 |
*JCR, Journal Citation Report; #IF, Impact Factor; †USA, the United States of America
Co-cited references
Research frontiers refer to emerging trends or the development of new topics. When two references were cited in the reference list of a third paper, they established a co-citation relationship. The clustering labels assigned to co-cited references can reflect the forefront of research in specific medical fields. We analyzed 776 co-cited references, and the top 10 were displayed in Table 7. The article “The global burden of group A streptococcal diseases” in the Lancet Infectious Diseases (IF = 36.4) ranked first with co-citation counts of 327, followed by the article “Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015” published in the New England Journal of Medicine (IF = 96.2) with co-citation counts of 304. Regarding the topics across these highly co-cited references, the echocardiographic diagnosis and screening of RHD are particularly prominent. The top ten co-cited articles have all been published in first-class journals such as the Lancet and New England Journal of Medicine. Furthermore, CiteSpace was used to generate co-cited network and cluster analyses by us (Fig. 6). Co-cited references were divided into 18 clusters, such as echocardiographic prevalence (#0), infective endocarditis (#4), pregnant woman (#7), heart failure (#10), rheumatic mitral stenosis (#11), and valve surgery (#14). In a word, echocardiographic prevalence, infective endocarditis, heart failure, and valve surgery are the emerging research trends in RHD.
Table 7.
Top 10 highly co-cited publications in the field of RHD
| Rank | Title | Citation | Year | Journal | Type | IF# (2023) |
|---|---|---|---|---|---|---|
| 1 | The global burden of group A streptococcal diseases | 327 | 2005 | Lancet Infectious Diseases | Review | 36.4 |
| 2 | Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015 | 304 | 2017 | New England Journal of Medicine | Article | 96.2 |
| 3 | World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease–an evidence-based guideline | 295 | 2011 | Nature Reviews Cardiology | Review | 41.7 |
| 4 | Rheumatic heart disease | 203 | 2012 | Lancet | Review | 98.4 |
| 5 | Prevalence of rheumatic heart disease detected by echocardiographic screening | 197 | 2007 | New England Journal of Medicine | Article | 96.2 |
| 6 | Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study) | 193 | 2015 | European Heart Journal | Article | 37.6 |
| 7 | Acute rheumatic fever and rheumatic heart disease | 141 | 2016 | Nature Reviews Disease Primers | Review | 76.9 |
| 8 | Revision of the Jones Criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: a scientific statement from the American Heart Association | 121 | 2015 | Circulation | Article | 35.5 |
| 9 | Echocardiography screening for rheumatic heart disease in Ugandan schoolchildren | 117 | 2012 | Circulation | Article | 35.5 |
| 10 | Position statement of the World Heart Federation on the prevention and control of rheumatic heart disease | 109 | 2013 | Nature Reviews Cardiology | Review | 41.7 |
#IF, Impact Factor
Fig. 6.
Reference analysis in the field of RHD
Keyword analysis
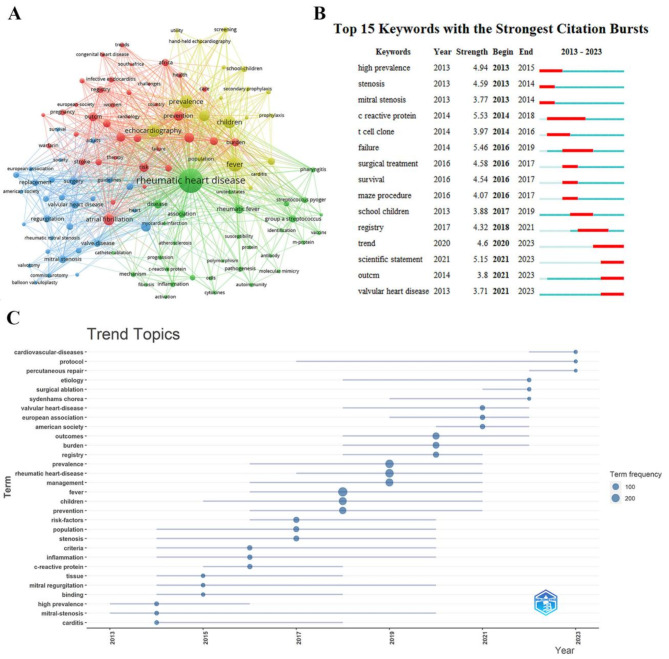
The research hotspots and future directions in the field of RHD were partially reflected in the analysis of keywords (Fig. 7A). The results show high-frequency keywords with specific meanings included fever (n = 299), echocardiography (n = 226), children (n = 209), atrial fibrillation (n = 132), surgery (n = 94), stroke (n = 66), repair (n = 50), and pregnancy (n = 49). These keywords represent the past, current or future hotspots in the field. As illustrated in Fig. 7A, the result suggests that the clusters should be divided into the following four domains: (1) RHD is a cardiac valve disorder that develops as a result of the progression of rheumatic fever, which occurs due to an infection caused by group A streptococcus bacteria through the respiratory tract or skin. Targeted treatment against group A streptococcus is of utmost importance in effectively managing the progression of this disease. (green cluster including “rheumatic fever”, “group a streptococcus”, “mechanism”, “polymorphism”, “pharyngitis”, “c-reactive protein”); (2) It is the most common acquired heart disease in children worldwide, and early diagnosis and screening using echocardiography are crucial. (yellow cluster including “echocardiography”, “children”, “prophylaxis”, “diagnosis”, “carditis”, “screening”); (3) The selected surgical techniques available for RHD include interventional, surgical repair, mechanical valve, and bioprosthetic valve replacement. (blue cluster including “mitral stenosis”, “regurgitation”, “valvotomy”, “replacement”, “ballon valvuloplasty”); (4) There are currently no guidelines for postoperative medication for the prevention of complications. (red cluster including “prevention”, “cardiac surgery”, “risk”, “stroke”, “warfarin”, “therapy”, “infective endocarditis”, “atrial fibrillation”).
Fig. 7.
Keyword analysis. A VOSviewer cluster visualization of keywords. B Top 15 keywords with the strongest citation bursts. C The evolution of keyword trends
The top 15 keywords with the strongest citation burst are shown in Fig. 7B. Additionally, we displayed the evolution of keyword trends in Fig. 7C, showing the changes in research topics over time. The analysis reveals that keywords such as high prevalence, carditis, inflammation, risk-factors, and c-reactive protein indicated that the epidemiology and mechanisms of RHD were the hot topics in the past; while keywords like trend, valvular heart disease, and outcomes inferred that the prognosis of patients with RHD were the hotspots studied in RHD at present.
Discussion
General information
The trend of annual publication outputs illustrates that the development of this field in the past decade can be segmented into an initial slow rise followed a more rapid increase. This variation in the pace of development may be attributed to improvements in diagnostic techniques, notably the vital role of echocardiographic screening which has significantly enhanced the accuracy of RHD diagnosis and emphasized the burden of the disease. The two Global RHD Registry (REMEDY) studies conducted in 2015 and 2016 documented high rates of disability and premature mortality in some African and Asian countries [12, 13]. In response to the global burden of RHD, the World Health Organization (WHO) adopted a resolution in May 2018 aimed at revitalizing global and national efforts towards RHD prevention and control [14]. Since then, scholars’ activity in this domain has surged significantly. However, the resolution only sought to ensure access to primary and secondary prevention and did not mention the critical role of surgical care for RHD, which is a condition that highly relies on surgical intervention [5]. This oversight may result in inadequate care for patients with RHD, particularly in regions with limited surgical resources. Furthermore, the trends and hotspots identified in this study emphasize the crucial role of surgical treatment in the management of RHD. The omission of this aspect in the WHO resolution may indicate a disconnect between policy-making and clinical needs, highlighting the necessity of strengthening global health policies regarding surgical care for RHD. Consequently, future resolutions should comprehensively address the treatment needs of RHD, including surgical care, to ensure that all patients have access to essential medical services. Severe and chronic structural changes in the valves represent a major cause of mortality associated with RHD. A notable lack of awareness often leads to delayed diagnosis of advanced valve pathology, rendering many patients ineligible for potentially beneficial surgical interventions. Therefore, early screening appears particularly important. Although valve replacement surgery provides initial benefits for patients, it also poses significant challenges in managing postoperative complications [15]. It is concerning that the growth in annual publication output has stagnated since last year, signalling a bottleneck in RHD research development, particularly as the increasing cumulative risk of postoperative complications in RHD patients poses ongoing challenges due to the absence of optimal management strategies [16].
Regarding the collaborative networks among countries, institutions, and authors, it can be observed that academic resources in low- and middle-income countries still lag behind those in high-income countries. For example, Brazil and Turkey, as representatives of low- and middle-income countries, have shown significant publication output worldwide. However, their international influence in this field remains relatively weak, as evidenced by their almost isolated status in the collaborative network. Institutions from South Africa, exemplified by the University of Cape Town, have established extensive collaborative networks with institutions from various countries, making significant contributions to RHD research. Moreover, researchers in South Africa, such as Liesl Joanna Zühlke and Bongani Mayosi from the University of Cape Town, have established collaborative relationships with scholars from various countries. Consequently, the region has emerged as a leader in RHD research. As for the collaborative networks of high-income countries, institutions in Europe and the Americas maintain strong connections. However, compared with scholars from Europe and the United States, Australian scholars have exhibited greater activity in collaborations within this field in recent years. For example, Emma Haynes and Asha C Bowen from the University of Western Australia have conducted research on community-based primary prevention and management of RHD [17] and the development of Group A streptococcus vaccines [18].
The comprehensive results of publication output and citations indicate that Circulation holds a reputation as the most influential journal in the field. It serves as an authoritative source for cardiovascular research and is responsible for publishing clinical practice guidelines endorsed by the American College of Cardiology/American Heart Association. These guidelines cover a range of topics, including the management of valvular heart diseases and primary prevention of cardiovascular diseases [19, 20]. Furthermore, Circulation is dedicated to publishing pioneering research in certain unexplored areas of RHD, such as latent RHD: identifying the children at the highest risk of unfavourable outcomes [21], and pregnancy outcomes in women with rheumatic mitral valve disease [22].
Research hotspots
Based on the results of keyword clustering and citation analysis, the following suggestions are proposed for future research hotspots in the field of RHD.
(1) Treatment of complications of RHD
Patients with RHD have varying degrees of valvular damage. Research has shown that 20% of patients with symptomatic valve disease also have concomitant AF [15], which is associated with a high risk of stroke and systemic embolism ranging from 0.4 to 4.2% per year [23, 24]. Due to the elevated stroke risk in patients with RHD-associated AF, early clinical trials conducted in Europe and America targeting anticoagulation in patients with AF, as well as contemporary randomized trials using direct oral anticoagulants (DOACs) for stroke prevention, have both excluded individuals with RHD associated AF [25–27]. Currently, there is a lack of sufficient clinical evidence to support clinical decisions regarding the combination of RHD-associated AF. Nevertheless, the 2020 European Society of Cardiology guidelines continue to recommend the use of vitamin K antagonists (VKAs) for stroke prevention in this specific patient population [28]. In low- and middle-income countries, it is challenging to achieve the optimal range of international normalized ratio (INR) when using VKAs to treat patients with RHD-associated AF. Given these challenges, there is a pressing need for DOACs suitable for RHD-associated AF that do not require INR monitoring. In recent years, rivaroxaban, a DOAC that does not require monitoring of INR, has shown benefits for patients with non-valvular AF; however, whether the same benefits exist for patients with RHD-associated AF remains to be confirmed. Recently, a randomized controlled trial (RCT) involving 4,565 patients with RHD-associated AF recruited from 24 countries demonstrated that VKAs were associated with lower rates of composite outcome of stroke, systemic embolism, myocardial infarction, or vascular (cardiac or non-cardiac) or unknown cause death than rivaroxaban therapy, without a higher rate of bleeding, and was effective beyond 3 years [29]. This evidence appeared to support the recommendations outlined in the guidelines [28]. A previous meta-analysis compared data from four oral anticoagulants for stroke prevention or systemic embolism events in patients with AF. The results showed that rivaroxaban was not inferior to warfarin in preventing stroke in patients with non-valvular AF, and it significantly reduces the risk of hemorrhagic stroke, leading to a 10% reduction in mortality for patients with AF [30, 31]. Although this study provided important insights into the role of rivaroxaban in reducing the risk of bleeding in patients with non-valvular AF, it was crucial to note that these results were not necessarily applicable to RHD-associated AF.
In the studies conducted on valvular and non-valvular AF [32], why do VKAs show inconsistent bleeding risks compared with rivaroxaban? The underlying reasons for this phenomenon still need further clarification. Additionally, the incidence of valve replacement surgery or valvuloplasty is similar between the VKAs group and the rivaroxaban group, and VKAs therapy has not been proven to slow down the progression of heart valve deterioration in patients with RHD [29]. From the perspective of valve progression in patients with RHD, it is still unclear which treatment is superior between VKAs and rivaroxaban in the management of RHD-associated AF. In the future, large-scale RCTs of different anticoagulant therapies will still be needed to explore the optimal treatment strategy for patients with RHD-associated AF.
In RHD, inflammation and fibrosis of central cardiac and valve tissue are the main manifestations [33]. Mitral stenosis, caused by valve fibrosis, can increase left atrium and pulmonary pressure, leading to the main complaint of HF [4]. Currently, there are no specific treatment guidelines for the management of HF in patients with RHD. In clinical practice, the treatment of HF in patients with RHD mainly focuses on symptomatic management, and there is no targeted treatment available for the key pathological mechanism of fibrosis in HF in patients with RHD [34]. The 2022 AHA/ACC/HFSA HF management guidelines recommend the use of SGLT2 inhibitors in adults with HF and confirmed that SGLT2 inhibitors were the preferred medications for treating HF [35]. Dapagliflozin, an SGLT2 inhibitor, has been shown in multiple studies to treat HF through the anti-fibrotic pathway [36, 37]. It is unknown whether it plays a role in inhibiting fibrosis or improving heart function in patients with RHD with mitral stenosis. Recently, an RCT involving 33 patients with RHD with mitral stenosis in Indonesia demonstrated that dapagliflozin improved net atrioventricular compliance, mitral valve mean pressure gradient parameter, and NT-pro-BNP levels, thereby enhancing left atrial function. However, even with the use of dapagliflozin, ongoing fibrosis was indicated by fibrosis biomarkers such as circulating carboxy-terminal propeptide of type I procollagen, the ratio between matrix metalloproteinase 1 and tissue matrix metalloproteinase inhibitors 1, suggesting that dapagliflozin does not act through the fibrosis pathway in patients with RHD with mitral stenosis [38]. In this study, the anti-fibrotic effects of dapagliflozin in the treatment of HF caused by RHD with mitral valve stenosis were not confirmed. The fibrotic signalling pathway in RHD is still under investigation, and other pathways may have effects beyond what is currently known. Research has shown that various cytokines and signalling pathways, such as angiotensin II, TGF-β, MAPK, and miR-145-5p/S1PR1, are involved in cardiac fibrosis in RHD [39–41]. Angiotensin II may induce cardiac fibrosis by increasing the binding of IL-33 and sST2, activating the TGF-β/MAPK/Smad signalling pathway to promote inflammation, cell proliferation, differentiation, and extracellular matrix remodelling [39]. Therefore, angiotensin-converting enzyme inhibitors are considered potential targeted drugs for fibrosis related to RHD [42]. However, the role of angiotensin-converting enzyme inhibitors in RHD cases is still under study and has not been confirmed [43]. In addition, an animal experiment has shown that LINC00707, a lncRNA, can inhibit cardiac fibrosis in RHD by targeting miR-145-5p/S1PR1, providing a basis for the clinical development of targeted drugs [41]. In recent years, the role of traditional Chinese medicine in combating cardiac fibrosis has been increasingly confirmed. The main active compound of Salvia miltiorrhiza, Salvianol, can counteract myocardial tissue fibrosis in rats with myocardial infarction by regulating the level of miR-618 [44]. Berberine, an extract from Coptis chinensis, can inhibit angiotensin II-induced cardiac fibrosis by down-regulating the activity of cyclin-dependent kinase 2 [45]. Astragaloside IV can inhibit cardiac fibrosis by targeting miR-135a and activating the TGF-β/Smads pathway [46]. This provides a new possibility for the traditional Chinese medicine treatment of fibrosis in RHD. In the future, extensive research is still needed on the key pathological mechanism of fibrosis in HF caused by RHD with mitral valve stenosis, as well as the exploration of more targeted therapeutic drugs.
In addition, apart from complications like AF and HF, infective endocarditis is also commonly seen as a complication of RHD [47]. However, there are currently no large-scale clinical RCT studying this, which is an area that needs to be explored in future research.
(2) Screening strategies for RHD
Subclinical valve lesions of RHD detected in the early stages are reversible. Before the valve lesions become irreversible, the risk of developing late-stage valve heart disease can be minimized through antibiotic prophylaxis [48]. Echocardiography serves as the most critical diagnostic tool for identifying this preventable and treatable disease, playing a valuable role in detecting the presence of subclinical diseases that require prompt treatment or follow-up evaluation [49]. Portable and rapid echocardiography can help determine the disease burden and establish referral pathways in RHD screening, providing policy information for expanding RHD control programs [50]. M-mode and two-dimensional transthoracic echocardiography can assess atrial function, size, and valve function [51]. Continuous echocardiography can monitor RHD progression and evaluate the effectiveness of valve replacement surgery [52]. Three-dimensional echocardiography provides additional anatomical and morphological functional information for patients with rheumatic valve disease [53]. Recently, Cardiovascular magnetic resonance (CMR) has been proven to be capable of performing many of the aforementioned applications, and multi-parametric CMR has been used for the diagnosis and management guidance of patients with RHD in small sample sizes [54]. The advantage of CMR in RHD, particularly when ultrasound imaging is suboptimal, lies in its ability to provide accurate and reproducible information about tissue characteristics such as myocardial fibrosis without relying on adequate acoustic windows and operator experience. For instance, in a study involving three patients with chronic RHD, CMR was found to be associated with late gadolinium enhancement in the atrial wall [55]. In the future, CMR may play an increasingly important role in the evaluation and management of patients with RHD. However, its utility may be limited in its utility for assessing RHD in countries with a high RHD prevalence due to testing costs and limited expertise. A simpler, more functional, and cost-effective testing method is eagerly awaited by many high-prevalence countries.
(3) Surgical strategies for rheumatic mitral valve
Common pathological changes in rheumatic mitral stenosis include commissural fusion, tendon fusion and shortening, leaflet thickening, and fusion [56]. Percutaneous mitral balloon commissurotomy (PMBC) is recommended by the American College of Cardiology/American Heart Association as an intervention for rheumatic mitral stenosis [20], but appropriate surgical procedures must still be chosen when contraindications such as valve calcification and mitral regurgitation are present. Mitral valve replacement (MVR) and mitral valve repair (MVP) are the most widely used and effective surgical methods for rheumatic mitral stenosis. Major complications associated with mechanical valve replacement include thrombosis, thromboembolism, and bleeding [57], which require long-term anticoagulation after surgery with regular monitoring of the INR. For special populations such as young pregnant women, anticoagulant therapy after MVR surgery is susceptible to the effects of maternal stroke and adverse fetal outcomes [57]. Additionally, there is controversy surrounding the optimal starting dose and duration of postoperative anticoagulation. The American College of Chest Physicians recommends an initial dose of 5-10 mg/day for individuals requiring long-term anticoagulation [58]. However, when the dosage exceeds 5 mg, most patients surpass the upper limit of the therapeutic range, potentially leading to inconsistent anticoagulation therapy and increasing the risk of bleeding and delayed INR response [59]. Many clinical practices thus favour using lower-dose warfarin. A prospective, single-blind, RCT conducted in the United States compared the time to achieve target INR, time within the therapeutic range, and occurrence of bleeding/thromboembolic events between post-MVR patients who received an initial warfarin dose of 5 mg or 3 mg. The results indicated that in post-MVR patients, the time to achieve target INR was shorter with an initial dose of 5 mg than with 3 mg, and the use of 5 mg warfarin as an initial dose significantly reduced the cost of bridging with enoxaparin, while bleeding events were comparable [60]. A Canadian study also confirmed these findings [61]. Further profound research on the initial dose and duration of anticoagulation therapy after MVR is necessary to guide clinical practice. In addition, the mismatch between mechanical valves and patients raises the risk of patient mortality [62]. Improving the compatibility between mechanical valves and the body is also a challenging area of research. Biological heart valves are costly and prone to early degeneration. For young women of childbearing age, there is a significantly higher likelihood of requiring early reoperation [63].
MVP requires the selection of different techniques based on the specific pathological characteristics of the patient’s valve, such as subvalvular debridement, annuloplasty, and subvalvular instrumented lysis et al. [64]. The variety and complexity of rheumatic lesions make valve repair much more demanding than that of degenerative diseases, thus testing the expertise of the surgeon and the facility’s capabilities [65]. Studies have indicated that MVP has demonstrated positive results for patients with RHD, with long-term survival rates exceeding those of MVR, particularly in young patients [66, 67]. However, despite undergoing MVP surgery, the inflammatory processes associated with the disease persist postoperatively, and the underlying factors causing the disease remain unresolved. Thus, lifelong prophylactic antibiotic use is still necessary after surgery [68]. Furthermore, the evolving nature of inflammatory diseases renders the outcomes less predictable. If medical treatments targeting the rheumatic process and cardiac failure fail to stabilize the condition, the prognosis remains quite bleak for children under the age of 10–12 with severe valvular dysfunction, regardless of whether they undergo MVP or MVR [68]. In low- and middle-income countries, limited availability of skilled professionals and constrained healthcare budgets reduce the likelihood of widespread implementation of such surgery. In addition, several challenges persist regarding surgical strategies for MVP: (1) Timing of Surgery: the progressive stenosis results in reducing appropriateness of repair [68]; (2) Surgeon Expertise: when a surgeon’s expertise is insufficient, the risk of poor outcomes during attempts at repair is real [69]; (3) Patient Circumstances: some patients in rural areas and low- and middle-income countries do not have the ability of follow-up or affording re-intervention [70]; (4) Multidisciplinary Evaluation: comprehensive assessment by a multidisciplinary cardiac team is essential for improving patient outcomes [71]. To address these issues, both future clinical practice and clinical trials should focus on the following strategies: (1) Implement extensive screening initiatives in endemic regions to facilitate early symptom identification and timely surgical intervention. Additionally, incorporate advanced diagnostic modalities to determine the optimal timing for surgery [72]; (2) Advocate for increased financial investment by local governments and public health departments to provide targeted cardiac surgery training for surgeons. Promote cross-center collaboration and knowledge exchange, and establish a comprehensive evaluation system for cardiac surgeons to enhance their professional expertise [73]; (3) Conduct a thorough assessment of the patient’s background, considering their preferences, financial situation, and adherence, to develop a personalized follow-up and treatment plan [3]; (4) Establish specialized medical centers for the treatment of rheumatic heart valve disease and convene regular multidisciplinary case discussions to promote effective collaboration and knowledge sharing among multidisciplinary experts [74].
Research comparing the long-term outcomes of mechanical valve replacement, biological valve replacement, and valve repair remains limited. A recent meta-analysis of 11 studies containing a total of 5,654 patients concluded that compared with patients who undergo MVR, those who undergo MVP benefit from a higher long-term survival rate, a lower risk of early mortality, and better outcomes regarding valve-related adverse events. However, a higher risk of reoperation was observed in the MVP group [75]. In the future, a large number of RCTs are still needed to compare the clinical efficacy of MVP and MVR, in order to identify the best treatment options for patients.
Strengths and limitations
Bibliometric methods have efficiently highlighted the hot topics and trends within RHD research. To our knowledge, this is the first bibliometric analysis of RHD. However, these methods cannot replace systematic reviews due to their methodological limitations. Therefore, this review faces several limitations. Firstly, the study exclusively utilized the WoSCC database, potentially overlooking contributions from other publication sources. Secondly, bibliometric analysis does not assess the quality of literature; therefore, the inclusion of low-quality articles may compromise the analysis. Thirdly, the authors devised the search strategy for this study by consulting the MeSH vocabulary and collaborating with a medical librarian. However, some potentially relevant terms may have been overlooked, leading to the exclusion of related articles. Fourthly, this study included only English-language literature, which may have overlooked valuable findings in non-English documents, leading to incomplete data. Lastly, due to time constraints, the most recent literature from 2024 was not incorporated.
Conclusions
This comprehensive analysis indicates that research on RHD is expanding. While North America and Europe continue to wield significant academic influence, institutions in low- and middle-income countries such as South Africa and China have demonstrated substantial potential in this area. Issues such as the treatment of complications associated with RHD, including AF, HF, and infective endocarditis, as well as screening strategies for RHD and surgical treatment for rheumatic mitral valve disease, remain areas of active inquiry. These clinical challenges have attracted considerable attention recently and are poised to be pivotal focuses of future research efforts.
Abbreviations
- MI
Myocardial infarction
- WoSCC
Web of Science Core Collection
- USA
United States of America
- RHD
Rheumatic heart disease
- HF
Heart Failure
- IF
Impact Factor
- AF
Atrial fibrillation
- VKAs
Vitamin K antagonists
- MVR
Mitral valve replacement
- MVP
Mitral valve repair
Author contributions
Conceptualization: Yifan Chen, Zhonghui Jiang; Methodology: Dan Ma, Zhijie Cui; Formal analysis and investigation: Yanjiao Liu, Qinghua Pang; Writing - original draft preparation: Yifan Chen, Liuding Wang; Writing - review and editing: Zhonghui Jiang, Zhuye Gao; Funding acquisition: Zhuye Gao; Supervision: Zhuye Gao. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82274508) and the Project of China Academy of Chinese Medical Sciences (No. CI2021A00920).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yifan Chen and Liuding Wang contributed equally to this work and should be considered co-first authors.
Contributor Information
Zhonghui Jiang, Email: 1043457031@qq.com.
Zhuye Gao, Email: zhuyegao@126.com.
References
- 1.Dooley LM, Ahmad TB, Pandey M, et al. Rheumatic Heart Disease: a review of the current status of Global Research Activity. Autoimmun Rev. 2021;20(2):102740. 10.1016/j.autrev.2020.102740. [DOI] [PubMed] [Google Scholar]
- 2.Watkins DA, Johnson CO, Colquhoun SM, et al. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015. N Engl J Med. 2017;377(8):713–22. 10.1056/NEJMoa1603693. [DOI] [PubMed] [Google Scholar]
- 3.Kumar RK, Antunes MJ, Beaton A, et al. Contemporary diagnosis and management of Rheumatic Heart Disease: implications for closing the gap: a Scientific Statement from the American Heart Association. Circulation. 2020;142(20):e337–57. 10.1161/CIR.0000000000000921. [DOI] [PubMed] [Google Scholar]
- 4.Rwebembera J, Beaton AZ, de Loizaga SR, et al. The global impact of Rheumatic Heart Disease. Curr Cardiol Rep. 2021;23(11):160. 10.1007/s11886-021-01592-2. [DOI] [PubMed] [Google Scholar]
- 5.Dougherty S, Okello E, Mwangi J, et al. Rheumatic Heart Disease: Jacc Focus Seminar 2/4. J Am Coll Cardiol. 2023;81(1):81–94. 10.1016/j.jacc.2022.09.050. [DOI] [PubMed] [Google Scholar]
- 6.Gelaw TT, Yimer YA, Gesesse AA, et al. Intervention needs assessment in children with heart diseases presenting to Tibebe-Ghion Specialized Teaching Hospital, Bahir Dar, North West Ethiopia - Tip of the iceberg of the intervention gap in low-and-middle-income countries (LMICs). Int J Cardiol. 2024;412:132324. 10.1016/j.ijcard.2024.132324. [DOI] [PubMed] [Google Scholar]
- 7.Brescia AA, Watt TMF, Murray SL, et al. Rheumatic mitral valve repair or replacement in the valve-in-valve era. J Thorac Cardiovasc Surg. 2022;163(2):591–e6021. 10.1016/j.jtcvs.2020.04.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson M, Sampson M, Barrowman N, et al. Bibliometric Analysis of Neurology Articles Published in General Medicine journals. JAMA Netw Open. 2021;4(4):e215840. 10.1001/jamanetworkopen.2021.5840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perazzo MF, Otoni ALC, Costa MS, et al. The top 100 most-cited papers in Paediatric Dentistry journals: a bibliometric analysis. Int J Paediatr Dent. 2019;29(6):692–711. 10.1111/ipd.12563. [DOI] [PubMed] [Google Scholar]
- 10.Dong R, Wang H, Ye J, et al. Publication trends for Alzheimer’s Disease Worldwide and in China: a 30-Year bibliometric analysis. Front Hum Neurosci. 2019;13:259. 10.3389/fnhum.2019.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roscoe JN, Shapiro VB, Whitaker K, et al. Classifying changes to preventive interventions: applying adaptation taxonomies. J Prim Prev. 2019;40(1):89–109. 10.1007/s10935-018-00531-2. [DOI] [PubMed] [Google Scholar]
- 12.Zühlke L, Karthikeyan G, Engel ME, et al. Clinical outcomes in 3343 children and adults with Rheumatic Heart Disease from 14 low- and Middle-Income countries: two-year follow-up of the global Rheumatic Heart Disease Registry (the Remedy Study). Circulation. 2016;134(19):1456–66. 10.1161/CIRCULATIONAHA.116.024769. [DOI] [PubMed] [Google Scholar]
- 13.Zühlke L, Engel ME, Karthikeyan G et al. Characteristics, Complications, and Gaps in Evidence-Based Interventions in Rheumatic Heart Disease: The Global Rheumatic Heart Disease Registry (the Remedy Study). Eur Heart J. 2015;36(18):1115-22a. 10.1093/eurheartj/ehu449 [DOI] [PMC free article] [PubMed]
- 14.White A. WHO Resolution on rheumatic heart disease. Eur Heart J. 2018;39(48):4233. 10.1093/eurheartj/ehy764. [DOI] [PubMed] [Google Scholar]
- 15.Vervoort D, Antunes MJ, Pezzella AT. Rheumatic Heart Disease: the role of global cardiac surgery. J Card Surg. 2021;36(8):2857–64. 10.1111/jocs.15597. [DOI] [PubMed] [Google Scholar]
- 16.Doran J, Canty D, Dempsey K, et al. Surgery for Rheumatic Heart Disease in the Northern Territory, Australia, 1997–2016: what have we gained? BMJ Glob Health. 2023;8(3):e011763. 10.1136/bmjgh-2023-011763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haynes E, Katzenellenbogen JM, Noonan S, et al. Aust N Z J Public Health. 2022;46(5):554–7. 10.1111/1753-6405.13259. Is the Australian Primary Healthcare System Ready for the Rheumatic Heart Disease Endgame Strategy? Data Synthesis and Recommendations. [DOI] [PubMed]
- 18.Cannon JW, Bowen AC. An update on the Burden of Group a Streptococcal diseases in Australia and Vaccine Development. Med J Aust. 2021;215(1):27–8. 10.5694/mja2.51126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Otto CM, Nishimura RA, Bonow RO, et al. 2020 Acc/Aha Guideline for the management of patients with Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation. 2021;143(5):e35–71. 10.1161/CIR.0000000000000932. [DOI] [PubMed] [Google Scholar]
- 20.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 Acc/Aha Guideline on the primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation. 2019;140(11):e596–646. 10.1161/CIR.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beaton A, Aliku T, Dewyer A, et al. Latent Rheumatic Heart Disease: identifying the children at highest risk of unfavorable outcome. Circulation. 2017;136(23):2233–44. 10.1161/CIRCULATIONAHA.117.029936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Hagen IM, Thorne SA, Taha N, et al. Pregnancy outcomes in women with rheumatic mitral valve disease: results from the Registry of pregnancy and Cardiac Disease. Circulation. 2018;137(8):806–16. 10.1161/CIRCULATIONAHA.117.032561. [DOI] [PubMed] [Google Scholar]
- 23.Karthikeyan G, Connolly SJ, Yusuf S. Overestimation of stroke risk in rheumatic mitral stenosis and the implications for oral anticoagulation. Circulation. 2020;142(18):1697–9. 10.1161/CIRCULATIONAHA.120.050347. [DOI] [PubMed] [Google Scholar]
- 24.Karthikeyan G. Stroke risk in Rheumatic Heart Disease. Heart. 2021;107(9):694–6. 10.1136/heartjnl-2020-318756. [DOI] [PubMed] [Google Scholar]
- 25.Halperin JL, Hankey GJ, Wojdyla DM, et al. Efficacy and safety of Rivaroxaban compared with Warfarin among Elderly patients with Nonvalvular Atrial Fibrillation in the Rivaroxaban once Daily, oral, direct factor Xa Inhibition compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (Rocket Af). Circulation. 2014;130(2):138–46. 10.1161/CIRCULATIONAHA.113.005008. [DOI] [PubMed] [Google Scholar]
- 26.Girgis IG, Patel MR, Peters GR, et al. Population Pharmacokinetics and Pharmacodynamics of Rivaroxaban in patients with non-valvular atrial fibrillation: results from Rocket Af. J Clin Pharmacol. 2014;54(8):917–27. 10.1002/jcph.288. [DOI] [PubMed] [Google Scholar]
- 27.Fischer U, Koga M, Strbian D, et al. Early Versus later anticoagulation for stroke with Atrial Fibrillation. N Engl J Med. 2023;388(26):2411–21. 10.1056/NEJMoa2303048. [DOI] [PubMed] [Google Scholar]
- 28.Hindricks G, Potpara T, Dagres N, et al. 2020 Esc guidelines for the diagnosis and management of Atrial Fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (Eacts): the Task Force for the diagnosis and management of Atrial Fibrillation of the European Society of Cardiology (Esc) developed with the Special Contribution of the European Heart Rhythm Association (Ehra) of the Esc. Eur Heart J. 2020;42(5):373–498. 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 29.Connolly SJ, Karthikeyan G, Ntsekhe M, et al. Rivaroxaban in Rheumatic Heart Disease-Associated Atrial Fibrillation. N Engl J Med. 2022;387(11):978–88. 10.1056/NEJMoa2209051. [DOI] [PubMed] [Google Scholar]
- 30.Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with Atrial Fibrillation: a Meta-analysis of Randomised trials. Lancet. 2014;383(9921):955–62. 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 31.Guimarães HP, de Barros ESPGM, Liporace IL, et al. A Randomized Clinical Trial to evaluate the efficacy and safety of Rivaroxaban in patients with Bioprosthetic Mitral Valve and Atrial Fibrillation or Flutter: Rationale and Design of the River Trial. Am Heart J. 2021;231:128–36. 10.1016/j.ahj.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Hanon O, Vidal JS, Pisica-Donose G, et al. Bleeding risk with Rivaroxaban compared with Vitamin K Antagonists in patients aged 80 years or older with Atrial Fibrillation. Heart. 2021;107(17):1376–82. 10.1136/heartjnl-2020-317923. [DOI] [PubMed] [Google Scholar]
- 33.Bright PD, Mayosi BM, Martin WJ. An immunological perspective on Rheumatic Heart Disease Pathogenesis: more questions than answers. Heart. 2016;102(19):1527–32. 10.1136/heartjnl-2015-309188. [DOI] [PubMed] [Google Scholar]
- 34.Ogbemudia EJ, Umuerri EM. Relevance of rheumatic Valvular Heart Disease in the Aetiology of Heart failure in Contemporary Times. West Afr J Med. 2021;38(3):241–5. [PubMed] [Google Scholar]
- 35.Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the management of Heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation. 2022;145(18):e895–1032. 10.1161/CIR.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 36.Jhund PS, Kondo T, Butt JH, et al. Dapagliflozin across the Range of Ejection Fraction in patients with heart failure: a Patient-Level, pooled Meta-analysis of Dapa-Hf and deliver. Nat Med. 2022;28(9):1956–64. 10.1038/s41591-022-01971-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin YW, Chen CY, Shih JY, et al. Dapagliflozin improves Cardiac Hemodynamics and mitigates Arrhythmogenesis in Mitral Regurgitation-Induced Myocardial Dysfunction. J Am Heart Assoc. 2021;10(7):e019274. 10.1161/JAHA.120.019274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asrial AA, Reviono R, Soetrisno S, et al. Effect of Dapagliflozin on patients with Rheumatic Heart Disease Mitral stenosis. J Clin Med. 2023;12(18). 10.3390/jcm12185898. [DOI] [PMC free article] [PubMed]
- 39.Ambari AM, Setianto B, Santoso A, et al. Angiotensin converting enzyme inhibitors (Aceis) decrease the progression of Cardiac Fibrosis in Rheumatic Heart Disease through the inhibition of IL-33/sST2. Front Cardiovasc Med. 2020;7:115. 10.3389/fcvm.2020.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim L, Kim DK, Yang WI, et al. Overexpression of transforming growth factor-Beta 1 in the Valvular Fibrosis of Chronic Rheumatic Heart Disease. J Korean Med Sci. 2008;23(1):41–8. 10.3346/jkms.2008.23.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao W, Huang G, Ye J. LINC00707 inhibits myocardial fibrosis and Immune Disorder in Rheumatic Heart Disease by regulating miR-145-5p/S1PR1. Biotechnol Genet Eng Rev. 2023;4:1–14. 10.1080/02648725.2023.2204598. [DOI] [PubMed] [Google Scholar]
- 42.Chockalingam A, Venkatesan S, Dorairajan S, et al. Safety and Efficacy of Enalapril in Multivalvular Heart Disease with significant mitral Stenosis–SCOPE-MS. Angiology. 2005;56(2):151–8. 10.1177/000331970505600205. [DOI] [PubMed] [Google Scholar]
- 43.Ambari AM, Setianto B, Santoso A, et al. Randomised controlled trial into the role of Ramipril in Fibrosis Reduction in Rheumatic Heart Disease: the Ramirhed Trial Protocol. BMJ Open. 2021;11(9):e048016. 10.1136/bmjopen-2020-048016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yan N, Xiao C, Wang X, et al. Tanshinone Iia from Salvia Miltiorrhiza exerts Anti-fibrotic effects on Cardiac fibroblasts and rat heart tissues by suppressing the levels of pro-fibrotic factors: the key role of miR-618. J Food Biochem. 2022;46(2):e14078. 10.1111/jfbc.14078. [DOI] [PubMed] [Google Scholar]
- 45.Che Y, Shen DF, Wang ZP, et al. Protective role of Berberine in Isoprenaline-Induced Cardiac Fibrosis in rats. BMC Cardiovasc Disord. 2019;19(1):219. 10.1186/s12872-019-1198-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wei Y, Wu Y, Feng K, et al. Astragaloside Iv inhibits Cardiac Fibrosis Via miR-135a-TRPM7-TGF-β/Smads pathway. J Ethnopharmacol. 2020;249:112404. 10.1016/j.jep.2019.112404. [DOI] [PubMed] [Google Scholar]
- 47.Alsamarrai A, Saavedra C, Bryce A, et al. Infective endocarditis in patients with Rheumatic Heart Disease: a single-centre retrospective comparative study. N Z Med J. 2022;135(1550):62–73. [PubMed] [Google Scholar]
- 48.Fairley JM, Ahmad M. Paths to Improved Rheumatic Heart Disease: screening and Prophylaxis. Cardiol Young. 2020;30(1):149–50. 10.1017/S1047951119002774. [DOI] [PubMed] [Google Scholar]
- 49.Marijon E, Ou P, Celermajer DS, et al. Prevalence of Rheumatic Heart Disease detected by Echocardiographic Screening. N Engl J Med. 2007;357(5):470–6. 10.1056/NEJMoa065085. [DOI] [PubMed] [Google Scholar]
- 50.Karki P, Uranw S, Bastola S, et al. Effectiveness of systematic echocardiographic screening for Rheumatic Heart Disease in Nepalese schoolchildren: a Cluster Randomized Clinical Trial. JAMA Cardiol. 2021;6(4):420–6. 10.1001/jamacardio.2020.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agomuoh DI, Akpa MR, Alasia DD. Echocardiography in the University of Port Harcourt Teaching Hospital: April 2000 to March 2003. Niger J Med. 2006;15(2):132–6. 10.4314/njm.v15i2.37096. [DOI] [PubMed] [Google Scholar]
- 52.Wunderlich NC, Dalvi B, Ho SY, et al. Rheumatic mitral valve stenosis: diagnosis and treatment options. Curr Cardiol Rep. 2019;21(3):14. 10.1007/s11886-019-1099-7. [DOI] [PubMed] [Google Scholar]
- 53.Vieira MLC, Branco CEB, Gazola ASL, et al. 3D Echocardiography for Rheumatic Heart Disease Analysis: Ready for Prime Time. Front Cardiovasc Med. 2021;8:676938. 10.3389/fcvm.2021.676938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mavrogeni S, Pepe A, Nijveldt R, et al. Cardiovascular magnetic resonance in Autoimmune Rheumatic diseases: a clinical Consensus Document by the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2022;23(9):e308–22. 10.1093/ehjci/jeac134. [DOI] [PubMed] [Google Scholar]
- 55.Shriki J, Talkin B, Thomas IC, et al. Delayed Gadolinium Enhancement in the Atrial Wall: a Novel Finding in 3 patients with Rheumatic Heart Disease. Tex Heart Inst J. 2011;38(1):56–60. [PMC free article] [PubMed] [Google Scholar]
- 56.Tagliari F, Correia MG, Amorim GD, et al. Clinical Features and Survival Analysis of Patients after mechanical heart valve replacement, with an emphasis on prosthetic valve thrombosis. Arq Bras Cardiol. 2022;119(5):734–44. 10.36660/abc.20210544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dalén M, Persson M, Glaser N, et al. Socioeconomic status and risk of bleeding after mechanical aortic valve replacement. J Am Coll Cardiol. 2022;79(25):2502–13. 10.1016/j.jacc.2022.04.030. [DOI] [PubMed] [Google Scholar]
- 58.Ansell J, Hirsh J, Hylek E, et al., et al. Pharmacology and Management of the Vitamin K Antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest. 2008;133(6 Suppl):s160–98. 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 59.Sanaani A, Yandrapalli S, Harburger JM. Antithrombotic Management of patients with Prosthetic Heart valves. Cardiol Rev. 2018;26(4):177–86. 10.1097/CRD.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 60.Sabry S, El Wakeel LM, Saleh A, et al. Comparison of Warfarin initiation at 3 mg versus 5 mg for anticoagulation of patients with mechanical mitral valve replacement surgery: a prospective Randomized Trial. Clin Drug Investig. 2022;42(4):309–18. 10.1007/s40261-022-01137-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chu MWA, Ruel M, Graeve A, et al. Low-dose vs Standard Warfarin after mechanical mitral valve replacement: a randomized trial. Ann Thorac Surg. 2023;115(4):929–38. 10.1016/j.athoracsur.2022.12.031. [DOI] [PubMed] [Google Scholar]
- 62.El Midany AA, Mostafa EA, Hikal T, et al. Incidence and predictors of mismatch after mechanical mitral valve replacement. Asian Cardiovasc Thorac Ann. 2019;27(7):535–41. 10.1177/0218492319869560. [DOI] [PubMed] [Google Scholar]
- 63.Mvondo CM, Pugliese M, Giamberti A, et al. Surgery for rheumatic mitral valve Disease in Sub-saharan African countries: why Valve Repair is still the Best Surgical option. Pan Afr Med J. 2016;24:307. 10.11604/pamj.2016.24.307.7504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.LaPar DJ, Ailawadi G, Isbell JM, et al. Mitral Valve Repair Rates Correlate with Surgeon and Institutional Experience. J Thorac Cardiovasc Surg. 2014;148(3):995–1004. 10.1016/j.jtcvs.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 65.Antunes MJ. Challenges in Rheumatic Valvular Disease: Surgical Strategies for Mitral Valve Preservation. Glob Cardiol Sci Pract. 2015;2015:9. 10.5339/gcsp.2015.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Krishna Moorthy PS, Sivalingam S, Dillon J, et al. Is it worth repairing rheumatic mitral valve disease in children? Long-term outcomes of an aggressive approach to rheumatic mitral valve repair compared to replacement in young patients. Interact Cardiovasc Thorac Surg. 2019;28(2):191–8. 10.1093/icvts/ivy234. [DOI] [PubMed] [Google Scholar]
- 67.McGurty D, Remenyi B, Cheung M, et al. Outcomes after rheumatic mitral valve repair in children. Ann Thorac Surg. 2019;108(3):792–7. 10.1016/j.athoracsur.2019.03.085. [DOI] [PubMed] [Google Scholar]
- 68.Antunes MJ. Repair of the rheumatic mitral valve: is the controversy over? Asian Cardiovasc Thorac Ann. 2020;28(7):374–6. 10.1177/0218492320927316. [DOI] [PubMed] [Google Scholar]
- 69.Silverman M, Padala M, Commentary. Multifaceted challenges with choosing between mitral valve repair and replacement for rheumatic heart disease. J Thorac Cardiovasc Surg. 2022;164(1):70–1. 10.1016/j.jtcvs.2020.08.035. [DOI] [PubMed] [Google Scholar]
- 70.Vervoort D, Ouzounian M, Yanagawa B. Mitral valve surgery for rheumatic heart disease: replace, repair, retrain? Curr Opin Cardiol. 2021;36(2):179–85. 10.1097/HCO.0000000000000826. [DOI] [PubMed] [Google Scholar]
- 71.Treede H, Schirmer J, Rudolph V, et al. A heart team’s perspective on interventional mitral valve repair: percutaneous clip implantation as an important adjunct to a surgical mitral valve program for treatment of high-risk patients. J Thorac Cardiovasc Surg. 2012;143(1):78–84. 10.1016/j.jtcvs.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 72.Sims Sanyahumbi A, Sable CA, Karlsten M, et al. Task shifting to clinical officer-led echocardiography screening for detecting rheumatic heart disease in Malawi, Africa. Cardiol Young. 2017;27(6):1133–9. 10.1017/S1047951116002511. [DOI] [PubMed] [Google Scholar]
- 73.Bolling SF, Li S, O’Brien SM, et al. Predictors of mitral valve repair: clinical and surgeon factors. Ann Thorac Surg. 2010;90(6):1904–12. 10.1016/j.athoracsur.2010.07.062. [DOI] [PubMed] [Google Scholar]
- 74.Rahman I, Segria CR, Trevis J, et al. Mitral valvular surgery outcomes in a centre with a dedicated mitral multi-disciplinary team. Br J Cardiol. 2024;31(1):012. 10.5837/bjc.2024.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fu G, Zhou Z, Huang S, et al. Mitral valve surgery in patients with Rheumatic Heart Disease: Repair vs. Replace Front Cardiovasc Med. 2021;8:685746. 10.3389/fcvm.2021.685746. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
Data Availability Statement
No datasets were generated or analysed during the current study.