Abstract
Objective
Although Mammotome-assisted minimally invasive resection (MAMIR) has been widely accepted for treating breast benign nodules, the procedure remains very technical and challenging. The present study aimed to assess the efficacy of norepinephrine application in MAMIR concerning intraoperative hemorrhage, postoperative pain and postoperative hospitalization.
Methods
A total of 306 patients with breast nodules admitted at the Xishan people’s Hospital of Wuxi City between June 2021 and July 2023 were included in this retrospective cohort study. The patient’s age, comorbidities (hypertension and diabetes), and characteristics of the breast nodule (number, unilateral or bilateral nature, inner quadrant volume and total volume) were all meticulously documented. Operation time, intraoperative hemorrhage, postoperative hospitalization and Visual analogue scale(VAS) score (postoperative 6-hour pain score) were recorded. Based on the application of norepinephrine, patients were categorized into non-NPP(norepinephrine) and NPP group. Univariate and multivariate analyses were performed to estimate the odds ratio (OR) and the 95% confidence intervals (CIs) for outcomes.
Results
A total of 155 who accepted MAMIR were included in this study. The NPP group exhibited reduced intraoperative bleeding, diminished postoperative pain, and a shorter duration of hospitalization (p < 0.05). Univariable analysis indicated that usage of norepinephrine during operation helped to reduce intraoperative hemorrhage (OR = 0.14, 95%CI: 0.07–0.31), alleviate postoperative pain(OR = 0.03, 95%CI: 0.01–0.09) and shorten hospital stay(OR = 0.50, 95%CI: 0.26–0.95). Furthermore, multivariate analysis identified the usage of norepinephrine during MAMIR as an independent factor associated with reducing intraoperative hemorrhage (OR = 0.11, 95%CI: 0.05–0.26) and relieving postoperative pain (OR = 0.02, 95%CI: 0.004–0.08) after adjusting for other factories.
Conclusions
Norepinephrine could help to reduce postoperative hospitalization and intraoperative hemorrhage, also relieve postoperative pain for breast benign nodules resection, which was an independent protective factor for relieving postoperative pain and reducing intraoperative hemorrhage.
Keywords: Breast nodules, Norepinephrine, Mammotome, Minimally invasive surgery, Retrospective study
Introduction
Breast tumors are a common disease in women, with a wide spectrum of pathologies, ranging from benign hyperplasia, high-risk lesions, and precancerous lesions to invasive malignant tumors [1, 2]. Relatively, benign breast masses or nodules are the most common in clinical practice [3]. Although benign breast tumors do not invade surrounding tissues or endanger life, they can interfere with breast function and affect the normal life of female patients [4]. Surgical resection is commonly the most useful treatment approach to remove breast nodules. However, conventional open resection makes it difficult to remove smaller breast masses, especially those with a diameter of less than 1 cm. Moreover, conventional open resection causes significant trauma and postoperative scars that affect aesthetics, causing permanent psychological barriers for female patients [5, 6].
With the application of Mammotome-assisted minimally invasive resection (MAMIR), benign breast tumors less than 3 cm can be treated with a minimally invasive procedure [6]. The principle is to perform MAMIR on breast nodules under ultrasound guidance based on the relevant principles of vacuum negative pressure suction, which is less invasive and has better cosmetic effects, therefore it is favored by the majority of female patients [7].
However, regardless of whether the conventional open resection or MAMIR methods are used, the intraoperative hemorrhage, postoperative pain and hospitalization caused by the surgery still affect the treatment effect of benign breast nodules. A clinical report indicated that submucosal injection of norepinephrine (1:500) can separate the mucosa from the muscle plane, which was beneficial for laparoscopic duodenal ampulla resection [8]. Another prospective randomized controlled study found that the administration of norepinephrine can also prevent postoperative hemorrhage after endoscopic submucosal dissection [9]. Previously, a randomized controlled prospective rats postoperative pain model study found that local infiltration anesthesia mixed with norepinephrine, levobupivacaine and dexibuprofen can reduce postoperative pain [10]. In fact, there have been reports in China using the same concentration of norepinephrine to reduce bleeding in bladder tumor resection and knee replacement operations, but there have been no reports of its application in the surgical treatment of benign breast tumors [11, 12]. Importantly, one study described that after activation by norepinephrine, ATF1 coordinates the activation of nuclear pluripotency factors MYC/NANOG and mitochondrial biogenesis regulatory factors NRF1/TFAM, thereby coordinating nuclear reprogramming and mitochondrial regeneration, enhancing tumor stemness, and promoting tumor progression [13]. Therefore, in the process of MAMIR treatment for benign breast nodules, the rational use of norepinephrine may improve the surgical effect and reduce intraoperative hemorrhage and pain caused by surgery.
This retrospective study aims to explore the efficacy of norepinephrine application in MAMIR in the treatment of benign breast nodules, to provide a basis for optimizing minimally invasive surgical treatment of benign breast masses/nodules in clinical practice.
Methods
Study design and patients
Patients with breast nodules admitted at the Xishan People’s Hospital of Wuxi City between June 2021 and July 2023 were included in this retrospective cohort study. Patients were separated into two groups: non-NPP (MAMIR was performed after implementing local infiltration anesthesia with lidocaine) and NPP group (MAMIR was performed after implementing local infiltration anesthesia with mixed lidocaine and norepinephrine solution). The need for written informed consent was waived by the Xishan People’s Hospital of Wuxi City Ethics Committee due to the retrospective nature of the study (No. xs2024ky001).
Inclusion criteria were the following
(1) those who underwent MAMIR either non-NPP or NPP; (2) aged 18–75 years; (3) with benign breast nodules by physical examination, color ultrasound, mammography and histopathology according to bi-RADS classification criteria [14]; (4) the diameter of a single nodule no more than 3 cm (≤ 3 cm).
Exclusion criteria were the following
(1) patients undergoing surgery who converted to conventional open resection; (2) rapid intraoperative pathology suggested a malignant tumor; (3) uncorrectable coagulation disorders; (4) pregnant women.
The study complied with the Declaration of Helsinki and was approved by the Ethics Committee of the Xishan People’s Hospital of Wuxi City (No. xs2024ky001). The requirement for informed consent was waived.
Surgical technique
All surgeries were completed by the same surgical team. The patient is positioned supine for the examination of the lesion using ultrasound. A suitable location is selected and marked for incision. Standard disinfection procedures are carried out, followed by subcutaneous administration of local anesthesia. (A) Non-NPP group was treated as follow: diluted lidocaine (0.01 g/ml) was used for local infiltration anesthesia to both upper and lower areas of the lesion as well as along the puncture pathway with ultrasound guidance. (B) NPP group was treated as follows: 2 ml diluted lidocaine (0.01 g/ml) for local skin anesthesia. Subsequently, 8 ml diluted lidocaine (0.01 g/ml) and 42 ml norepinephrine solution (1:200,000) were mixed into a 50 ml solution which was then used for local infiltration anesthesia to both upper and lower areas of the lesion as well as along the puncture pathway with ultrasound guidance. At last, surgical procedures for MAMIR were performed as previously published [6, 7].
Data collection
Data collection and follow-up were carried out for both non-NPP and NPP groups. Following data were included: age, hypertension, diabetes, resected nodules, bilateral nodules, inner quadrant volume, total nodules’ volumes, operation time, postoperative 6-hour pain score intraoperative hemorrhage and postoperative hospitalization. Patients in both groups were regularly followed up for at least 1 month via telephone or outpatient clinic.
Statistical analysis
The data were analyzed using SPSS 22.0 (IBM, Armonk, NY, USA). The continuous data were expressed as means ± standard deviations and analyzed using Student’s t-test. Categorical data were presented as frequencies and scores and were analyzed using Fisher’s exact test. Univariate and multivariate analyses were performed to estimate the odds ratio (OR) and the 95% confidence intervals (CIs) for intraoperative hemorrhage, VAS score during postoperative 6 h and postoperative hospitalization (days), including age, hypertension, diabetes, operation time, resected nodules, bilateral nodules, inner quadrant volume and total nodules’ volumes. Meanwhile, postoperative 6-hour pain score was classified into mild pain and moderate pain based on median Visual analogue scale(VAS) score. The data of hospitalization was dichotomized into two groups using median value as the cut off in logistic regression analysis.P value less than 0.05 indicated statistical significance.
Results
Characteristics of the patients
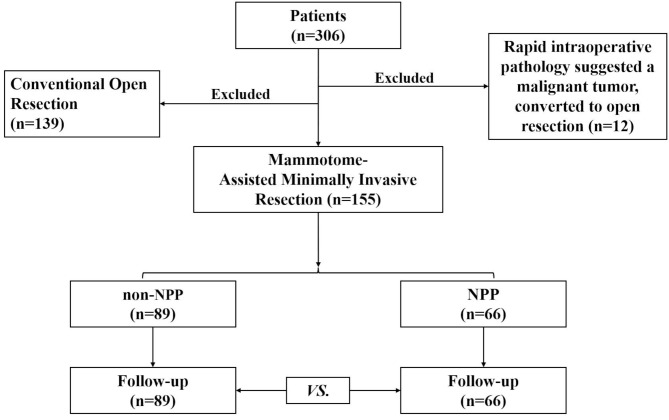
A total of 306 patients were diagnosed with breast nodules at Xishan People’s Hospital of Wuxi City. Among these patients, 139 were excluded due to conventional open resection, another 12 were excluded because rapid intraoperative pathology suggested a malignant tumor and converted to open resection. Finally, a total of 155 who accepted MAMIR were included in this study from June 2021 to July 2023 based on the exclusion and inclusion criteria. Among of them, 89 patients were treated with non-norepinephrine (non-NPP group), the other 66 patients were treated with norepinephrine (NPP group) (Fig. 1).
Fig. 1.
Detailed surgery flow diagram
No statistically significant differences were detected between-group in parameters, such as age, hypertension, diabetes, resected nodules, bilateral nodules, inner quadrant volume and total nodules’ volumes (all P > 0.05, Table 1).
Table 1.
Analysis of the intraoperative and postoperative characteristics
| Items | non-NPP (n = 89) | NPP (n = 66) |
|---|---|---|
| Age, mean ± SD, year | 40.29 ± 11.74 | 42.42 ± 11.2 |
| Hypertension | ||
| No | 80 (89.9) | 58 (87.9) |
| Yes | 9 (10.1) | 8 (12.1) |
| Diabetes | ||
| No | 84 (94.4) | 66 (100) |
| Yes | 5 (5.6) | 0 (0) |
| Resected nodules, median (IQR) | 2 (1,2) | 2 (1,3) |
| Bilateral nodules, median | ||
| No | 56 (62.9) | 43 (65.2) |
| Yes | 33 (37.1) | 23 (34.8) |
| Inner quadrant volume, median (IQR), mm3 | 0 (0,88) | 0 (0,40) |
| Total nodules’ volume, median (IQR), mm3 | 507 (196,864) | 323.75 (209.25,535.75) |
Abbreviations: SD,standard deviation; IQR, interquartile ranges
Notes: P-values less than 0.05, were boldly marked and italicized font, indicating statistical significance
Analysis of the intraoperative and postoperative characteristics
Compared to the non-NPP group, the operative time was similar in the NPP group, and no statistical differences. However, statistically significant differences were detected between the two groups in the intraoperative hemorrhage, postoperative hospitalization, and VAS score [15] during postoperative 6 h(P < 0.05, Table 2).
Table 2.
Analysis of the intraoperative and postoperative characteristics
| Items | non-NPP (n = 89) | NPP (n = 66) | P value |
|---|---|---|---|
| Operation time, median (IQR), min | 30 (15,50) | 25 (15,30) | 0.07 |
| Intraoperative hemorrhage, median (IQR), ml | 10 (5,10) | 5 (5,5) | < 0.001 |
| Postoperative hospitalization, median (IQR), day | 3 (2,3) | 2 (2,3) | 0.017 |
| VAS score (postoperative 6-hour pain score) | < 0.001 | ||
| 2 | 0 (0) | 6 (9.1) | |
| 3 | 14 (15.7) | 34 (51.5) | |
| 4 | 14 (15.7) | 22 (33.3) | |
| 5 | 23 (25.8) | 3 (4.6) | |
| 6 | 38 (42.7) | 1 (1.5) |
Abbreviations: IQR, interquartile rangesVAS, Visual Analogue Scale
Notes: P-values less than 0.05, were boldly marked and italicized font, indicating statistical significance
Norepinephrine conduced to reduce intraoperative hemorrhage for breast benign nodules resection
The univariate analysis showed that the usage of norepinephrine during MAMIR could reduce intraoperative hemorrhage (odds ratio[OR] = 0.14, 95% confidence interval [CI]:0.07–0.31, Table 3). Furthermore, the use of norepinephrine was an independent protective factor for reducing intraoperative hemorrhage after adjusting for resected nodules and bilateral Nodules in multivariate analysis (OR = 0.11, 95%CI:0.05–0.26, Table 3).
Table 3.
Univariable and multivariable analysis of intraoperative hemorrhage for the patients
| Items | OR (95%CI) | P value | OR (95%CI) | P value |
|---|---|---|---|---|
| Age, year | 1.01(0.98–1.03) | 0.694 | ||
| Hypertension | 0.94(0.34–2.61) | 0.901 | ||
| Diabetes | 2.07(0.34–12.76) | 0.432 | ||
| Resected nodules | 1.52(1.14–2.04) | 0.004 | 1.64(1.1–2.46) | 0.015 |
| Bilateral Nodules | 2.27(1.16–4.43) | 0.016 | 1.26(0.49–3.22) | 0.626 |
| Inner quadrant volume, mm3 | 1(1–1) | 0.238 | ||
| Total nodules’ volumes, mm3 | 1(1–1) | 0.57 | ||
| Norepinephrine | 0.14(0.07–0.31) | < 0.001 | 0.11(0.05–0.26) | < 0.001 |
Notes: P-values less than 0.05, were boldly marked and italicized font, indicating statistical significance
Norepinephrine helped to alleviate postoperative pain
MAMIR has relatively small trauma and a short duration of postoperative pain, mainly on the first postoperative day. Therefore, we chose postoperative 6 h as the comparison object for evaluating postoperative pain. The univariate analysis was performed to detect the relationship between these two groups. The results described that intraoperative use of norepinephrine could help to alleviate postoperative pain within 6 h(OR = 0.03, 95%CI:0.01–0.09, Table 4). Furthermore, the multivariate analysis showed that the association between administration of norepinephrine and relieving postoperative pain remained robust after adjusting for total nodules’ volumes, operation time, and intraoperative hemorrhage (OR = 0.02, 95%CI:0.004–0.08, Table 4).
Table 4.
Univariable and multivariable analysis of VAS score during postoperative 6 h for the patients
| Items | OR (95%CI) | P value | OR (95%CI) | P value |
|---|---|---|---|---|
| Age, year | 0.98(0.95-1) | 0.089 | ||
| Hypertension | 0.73(0.26–2.09) | 0.558 | ||
| Diabetes | 5.84(0.64–53.49) | 0.119 | ||
| Resected nodules | 1.19(0.93–1.51) | 0.167 | ||
| Bilateral Nodules | 1.33(0.69–2.59) | 0.394 | ||
| Inner quadrant volume, mm3 | 1(1–1) | 0.104 | ||
| Total nodules’ volumes, mm3 | 1(1–1) | 0.001 | 1.00.(1.00-1.002) | 0.003 |
| Operation time, min | 1.02(1.01–1.04) | 0.004 | 1.01(0.98–1.03) | 0.637 |
| Intraoperative hemorrhage, ml | 1.14(1.05–1.23) | 0.001 | 1.04(0.96–1.12) | 0.381 |
| Norepinephrine | 0.03(0.01–0.09) | < 0.001 | 0.02(0.004–0.08) | < 0.001 |
Notes: P-values less than 0.05, were boldly marked and italicized font, indicating statistical significance
Norepinephrine helped to reduce postoperative hospitalization
In order to explore the factors affecting postoperative hospitalization, univariate and multivariate analysis were performed. Univariate analysis indicated that the usage of norepinephrine during operation helped to reduce postoperative hospitalization (OR = 0.5, 95%CI:0.26–0.95, Table 5). However, usage of norepinephrine during operation was not an independent factors influencing postoperative hospitalization after adjusting for bilateral nodules, operation time and intraoperative hemorrhage in multivariate analysis (OR = 0.64, 95%CI:0.31–1.29, Table 5).
Table 5.
Univariable and multivariable analysis of postoperative hospitalization for all the patients
| Items | OR (95%CI) | P value | OR (95%CI) | P value |
|---|---|---|---|---|
| Age, year | 1.01(0.98–1.04) | 0.491 | ||
| Hypertension | 1.26(0.46–3.47) | 0.65 | ||
| Diabetes | 4.57(0.5-41.87) | 0.179 | ||
| Resected nodules | 1.28(0.99–1.66) | 0.062 | ||
| Bilateral Nodules | 2.03(1.04–3.95) | 0.037 | 1.391(0.64–3.04) | 0.409 |
| Inner quadrant volume, mm3 | 1(1–1) | 0.633 | ||
| Total nodules’ volumes, mm3 | 1(1–1) | 0.461 | ||
| Operation time- min | 1.02(1.01–1.04) | 0.005 | 1.01(0.996–1.03) | 0.140 |
| Intraoperative hemorrhage, ml | 1.08(1.01–1.15) | 0.022 | 1.04(0.98–1.11) | 0.232 |
| Norepinephrine | 0.5(0.26–0.95) | 0.035 | 0.64(0.31–1.29) | 0.210 |
| VAS score (postoperative 6,hour pain score) | ||||
| 2 | ||||
| 3 | 0.6(0.11–3.3) | 0.557 | ||
| 4 | 1(0.18–5.63) | 1 | ||
| 5 | 1.36(0.23–8.08) | 0.733 | ||
| 6 | 1.05(0.19–5.87) | 0.953 |
Abbreviations: VAS,Visual Analogue Scale
Notes: P-values less than 0.05, were boldly marked and italicized font- indicating statistical significance
Discussion
Breast tumor is a common disease that currently plagues the majority of Chinese women. The incidence of breast cancer has also increased during the last 10 years [16]. Although the current strategy for the diagnosis and treatment of breast cancer has achieved a bit of therapeutic effects, it still endangers women and causes death [17]. In fact, most of the breast nodules are benign masses. Although they are not life-threatening, they can still cause breast dysfunction and affect the normal life of women, affecting their psychology and physiology [3, 5]. For the diagnosis and treatment of benign breast nodules, surgical resection is the main approach [18]. Importantly, the gradual promotion of MAMIR has benefited the majority of female patients [14].
Herein, we added norepinephrine to assist local infiltration during preoperative local anesthesia which improved the operational details of the MAMIR approach in this study. The results showed that it can help to reduce intraoperative hemorrhage, relieve postoperative pain, and reduce postoperative hospitalization. Relatively, breast tumors are a common disease in women, while benign nodules account for the majority [3]. Although the MAMIR treatment method is widely used for benign breast nodules, no one has tried using norepinephrine to assist MAMIR in treating breast nodules. According to this study, our improved methods on this basis may help better implement the MAMIR regimen and benefit the patients.
Actually, mammotome-assisted minimally invasive technology has also been widely used in the diagnosis of breast masses and the resection of benign masses and/or nodules [2, 18, 19]. More than that, mammotome-assisted minimally invasive technology has even been used in auxiliary endoscopic breast-conserving surgery to provide auxiliary treatment for patients with early-stage breast cancer [20]. In fact, previous pieces of literature have reported that MAMIR has advantages in efficacy compared with traditional open surgery, as it can relieve postoperative pain, reduce postoperative scars, shorten hospitalization stays [7, 18], and also reduce postoperative complications [6]. Even more, there was a report that MAMIR could be applied to the case of large breast masses (diameter > 3 cm) and benefit the patient [21]. In this study, patients who received MAMIR treatment had breast benign nodules with a maximum diameter of no more than 3 cm. All patients completed MAMIR surgical treatment and were successfully discharged from the same hospital without any deaths or serious complications.
In clinical practice, norepinephrine was often used for gastrointestinal surgery such as endoscopic submucosal dissection, or the treatment of upper gastrointestinal bleeding diseases [8, 22, 23]. However, there have been no reports on the combined use of norepinephrine during MAMIR surgery. As early as 1999, a clinical research investigation in the United States found that the combination of 2% lidocaine and vasoconstrictors (norepinephrine 1:50000 and vasopressin 0.25 IU/mL) had sedative effects on heart rate, blood pressure, arrhythmia, and ischemic response, confirming the safety of lidocaine combined with norepinephrine for local anesthesia, while the use of midazolam can significantly improve the sympathetic adrenal pressure response [24]. A previous study indicated that local application of norepinephrine (1:200,000) can reduce bleeding after total knee replacement [11], as well as the report of using the same concentration of norepinephrine combined with hemagglutination to treat bleeding after transurethral resection of bladder tumors [12]. In this study, we used the lower concentration based on previous clinical literature took the concentration (1:50,000) reported as mentioned above [24], and then diluted it by 1/4 to avoid possible breast tissue and skin damage [25, 26]. Through this retrospective observational study, it was clarified that this concentration is effective and safe for breast benign cancer. Since norepinephrine may promote tumor progression [13], this study focused on the application of norepinephrine in benign breast tumors. In fact, in the process of MAMIR treatment for benign breast masses, the diameter of the breast masses in the patients in this study was all less than 3 cm, and the auxiliary anesthesia of midazolam was not required. Simultaneously, the administration of norepinephrine in MAMIR surgery was safe and no one experienced adverse reactions. Meanwhile, on the basis of a minimally invasive approach, MAMIR with the application of norepinephrine was more effective in reducing intraoperative hemorrhage, relieving postoperative pain, and shortening hospitalization time, which is consistent with the previous study and can better improve the clinical effect of MAMIR, although previous research reports have not involved the role of norepinephrine in the treatment of breast masses with MAMIR [2, 6, 7, 18].
Therefore, although there is currently no research reported on the use of norepinephrine to assist MAMIR in the treatment of breast masses, the implementation of our research may help promote clinical implementation in various medical centers and benefit the patients.
Study limitations
The present study has some limitations, more feedback from patients undergoing this procedure is needed. Mainly, this was a retrospective study, much more data and/or prospective studies may better characterize the association between breast nodules’ volume, operation time, intraoperative hemorrhage, and length of hospitalization in MAMIR. Although a short-term follow-up was conducted without any apparent complications, further long-term follow-up remains imperative for comprehensive evaluation. Furthermore, patients were mainly from Eastern China, and there was a lack of multi-center and/or regional comparative analysis.
Conclusion
This study elaborated on the treatment of breast benign nodules in a medical center in Eastern China. Although MAMIR is a safe and effective minimally invasive strategy, it is an effective method for treating breast nodules. In this study, norepinephrine application in MAMIR was safe and effective, could help to reduce postoperative hospitalization, also an important independent predictive factor for decreasing intraoperative hemorrhage and postoperative pain. When surgeons perform breast nodule resection, norepinephrine infiltrates the surrounding tissues of the breast nodule could be a good performance, giving full play to the advantages of norepinephrine in MAMIR. However, future research directions may need to focus more on the dosage, long-term effects, and efficacy of norepinephrine to obtain better feedback and benefit more patients.
Acknowledgements
None.
Author contributions
All authors have read and approved the final manuscript. All authors declare that no artificial intelligence or assistive technologies were used during the research process. CC: designed the research and drafted the paper. YS and LY: performed research and reviewed this paper. ZX: designed the mathematical methods. JH: organized the cases and collected and analyzed the data.
Funding
This research was supported by the scientific research projects of Top Talent Support Program for Young and Middle-Aged People of Wuxi Health Committee (HB2023116).
Data availability
The dataset for this study can be obtained by contacting the corresponding author (Chaobo Chen) upon reasonable request. If you have any questions, please contact bobo19820106@gmail.com.
Declarations
Ethical approval
The study was retrospective and approved by the Xishan People’s Hospital Ethics Committee to be conducted with opt-out rather than written consent. According to the ethical guidelines, the requirement for written informed consent was waived due to the retrospective nature of the study. This study was conducted in accordance with the Declaration of Helsinki of 1975 (as revised in 2013), and the protocol was reviewed and approved by the Ethics Committee of the Xishan people’s hospital of Wuxi City (No. xs2024ky001).
Competing interests
The authors declare no competing interests.
Disclosure
This paper has been uploaded to Research Square (https://www.researchsquare.com/article/rs-4511918/v1).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yafei Sun, Zipeng Xu, Jing Hu and Lina You contributed equally to this work.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. [DOI] [PubMed] [Google Scholar]
- 2.Zou SF, Tao L, Feng ZC, Wang JY, Liu L, Liang WL, Liu JN, Xu DD, Lin JY, Zhang JG, et al. A comparative study on ultrasound-guided elite, Mammotome, and core needle biopsy for diagnosing malignant breast masses. Arch Med Sci. 2022;18(2):422–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stachs A, Stubert J, Reimer T, Hartmann S. Benign breast disease in women. Dtsch Arztebl Int. 2019;116(33–34):565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weaver M, Stuckey A. Benign breast disorders. Obstet Gynecol Clin North Am. 2022;49(1):57–72. [DOI] [PubMed] [Google Scholar]
- 5.Kong X, Chen X, Jiang L, Ma T, Han B, Yang Q. Periareolar incision for the management of benign breast tumors. Oncol Lett. 2016;12(5):3259–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li R, Li J, Chen S, Xiao B, Liu L, Zhu N. Comparison of Curative Complications between Mammotome-Assisted Minimally Invasive Resection and Conventional Open Resection for Breast Neoplasm: A Retrospective Clinical Study. Biomed Res Int 2021, 2021:7739628. [DOI] [PMC free article] [PubMed] [Retracted]
- 7.Wang Y, Wang J, Liu L, Liang W, Qin Y, Zheng Z, Zou S, Xu Y, Chen C, Feng Z, et al. Comparison of curative effects between mammotome-assisted minimally invasive resection (MAMIR) and traditional open surgery for Gynecomastia in Chinese patients: a prospective clinical study. Breast J. 2019;25(6):1084–9. [DOI] [PubMed] [Google Scholar]
- 8.Cai H, Gao P, Lu F, Cai Y, Peng B. Laparoscopic Transduodenal Ampullectomy: how we have standardized the technique (with video). Ann Surg Oncol. 2023;30(2):1156–7. [DOI] [PubMed] [Google Scholar]
- 9.Lin SL, Gao PT, Ni WK, Li QL, Chen WF, Zhang YQ, Hu JW, Qin WZ, Cai MY, Ren Z, et al. Controlled hypertension under hemostasis prevents post-gastric endoscopic submucosal dissection bleeding: a prospective randomized controlled trial. Surg Endosc. 2021;35(10):5675–85. [DOI] [PubMed] [Google Scholar]
- 10.Gao Z, Cui F, Cao X, Wang D, Li X, Li T. Local infiltration of the surgical wounds with levobupivacaine, dexibuprofen, and norepinephrine to reduce postoperative pain: a randomized, vehicle-controlled, and preclinical study. Biomed Pharmacother. 2017;92:459–67. [DOI] [PubMed] [Google Scholar]
- 11.Lin W, Tiejun Y, Lin G. Local application of norepinephrine reduces bleeding in kee joint after total replacement operation. Med Aesthet Cosmetology. 2015;24(1):508–508. [Google Scholar]
- 12.Yongyan CG, Siping ZENG, et al. The Effect of Norepinephrine Combined with Hemagglutination in the treatment of postoperative hemorrhage of bladder tumor. China Continuing Med Educ. 2018;10(10):138–9. [Google Scholar]
- 13.He B, Gao R, Lv S, Chen A, Huang J, Wang L, Feng Y, Feng J, Liu B, Lei J, et al. Cancer cell employs a microenvironmental neural signal trans-activating nucleus-mitochondria coordination to acquire stemness. Signal Transduct Target Ther. 2023;8(1):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang H, Wang Q, Zhang Y, Peng Y. Value of ultrasound BI–RADS classification in preoperative evaluation of the ultrasound–guided mammotome–assisted minimally invasive resection of breast masses: a retrospective analysis. Exp Ther Med. 2023;25(4):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, Harris JD. Validation of Digital Visual Analog Scale Pain Scoring with a traditional paper-based Visual Analog Scale in adults. J Am Acad Orthop Surg Glob Res Rev. 2018;2(3):e088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lei S, Zheng R, Zhang S, Wang S, Chen R, Sun K, Zeng H, Zhou J, Wei W. Global patterns of breast cancer incidence and mortality: a population-based cancer registry data analysis from 2000 to 2020. Cancer Commun (Lond). 2021;41(11):1183–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnold M, Morgan E, Rumgay H, Mafra A, Singh D, Laversanne M, Vignat J, Gralow JR, Cardoso F, Siesling S, et al. Current and future burden of breast cancer: global statistics for 2020 and 2040. Breast. 2022;66:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang DH, Shu YL. Clinic efficacy and safety of ultrasound-guided mammotome-assisted surgery for patients with breast benign tumors. Eur Rev Med Pharmacol Sci. 2023;27(13):5985–92. [DOI] [PubMed] [Google Scholar]
- 19.Bozzini A, Cassano E, Raciti D, Disalvatore D, Pala O, Vingiani A, Renne G. Analysis of efficacy and accuracy of 2 vacuum-assisted breast Biopsy devices: Mammotome and Elite. Clin Breast Cancer. 2018;18(6):e1277–82. [DOI] [PubMed] [Google Scholar]
- 20.Xu Y, Ming J, Zhou Y, Qi X, Fan L, Jiang J. Mammotome-assisted endoscopic breast-conserving surgery: a novel technique for early-stage breast cancer. World J Surg Oncol. 2014;12:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang T, Zhu L. Mammotome-assisted removal with minimal incision of large juvenile fibroadenoma of breast: a case report. Med (Baltim). 2020;99(10):e19442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang T, Wang DN, Liu WT, Zheng ZQ, Chen X, Fang WL, Li S, Liang L, Wang BM. Hemostatic effect of topical hemocoagulase spray in digestive endoscopy. World J Gastroenterol. 2016;22(25):5831–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dong X, Li H, Zhu T. Clinical efficacy of norepinephrine combined with cimetidine in treatment of neonatal upper gastrointestinal hemorrhage and its adverse reactions. Pak J Med Sci. 2022;38(8):2215–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Middlehurst RJ, Gibbs A, Walton G. Cardiovascular risk: the safety of local anesthesia, vasoconstrictors, and sedation in heart disease. Anesth Prog. 1999;46(4):118–23. [PMC free article] [PubMed] [Google Scholar]
- 25.Christensen J, Andersson E, Sjoberg F, Hellgren E, Harbut P, Harbut J, Sjovall F, von Bruhn Gufler C, Martensson J, Rubenson Wahlin R, et al. Adverse events of peripherally administered norepinephrine during surgery: a prospective Multicenter Study. Anesth Analg. 2024;138(6):1242–8. [DOI] [PubMed] [Google Scholar]
- 26.Fechner J, El-Boghdadly K, Spahn DR, Motsch J, Struys M, Duranteau O, Ganter MT, Richter T, Hollmann MW, Rossaint R, et al. Anaesthetic efficacy and postinduction hypotension with remimazolam compared with propofol: a multicentre randomised controlled trial. Anaesthesia. 2024;79(4):410–22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset for this study can be obtained by contacting the corresponding author (Chaobo Chen) upon reasonable request. If you have any questions, please contact bobo19820106@gmail.com.